Recent Developments in Engineering Non-Paralytic Botulinum Molecules for Therapeutic Applications
Abstract
1. Introduction
2. Mechanisms of Action of BoNTs
3. Clinical Use of BoNTs
3.1. Efficacy of BoNTs in External Gland Secretion
3.1.1. Hyperhidrosis
3.1.2. Sialorrhea
3.1.3. Hyperlacrimation
3.1.4. Facial Seborrhea
3.2. Efficacy of BoNT in Hypersensitivity
3.2.1. Overactive Bladder
3.2.2. Pain Syndromes
Chronic Migraine
Trigeminal Neuralgia
4. Adverse Effects
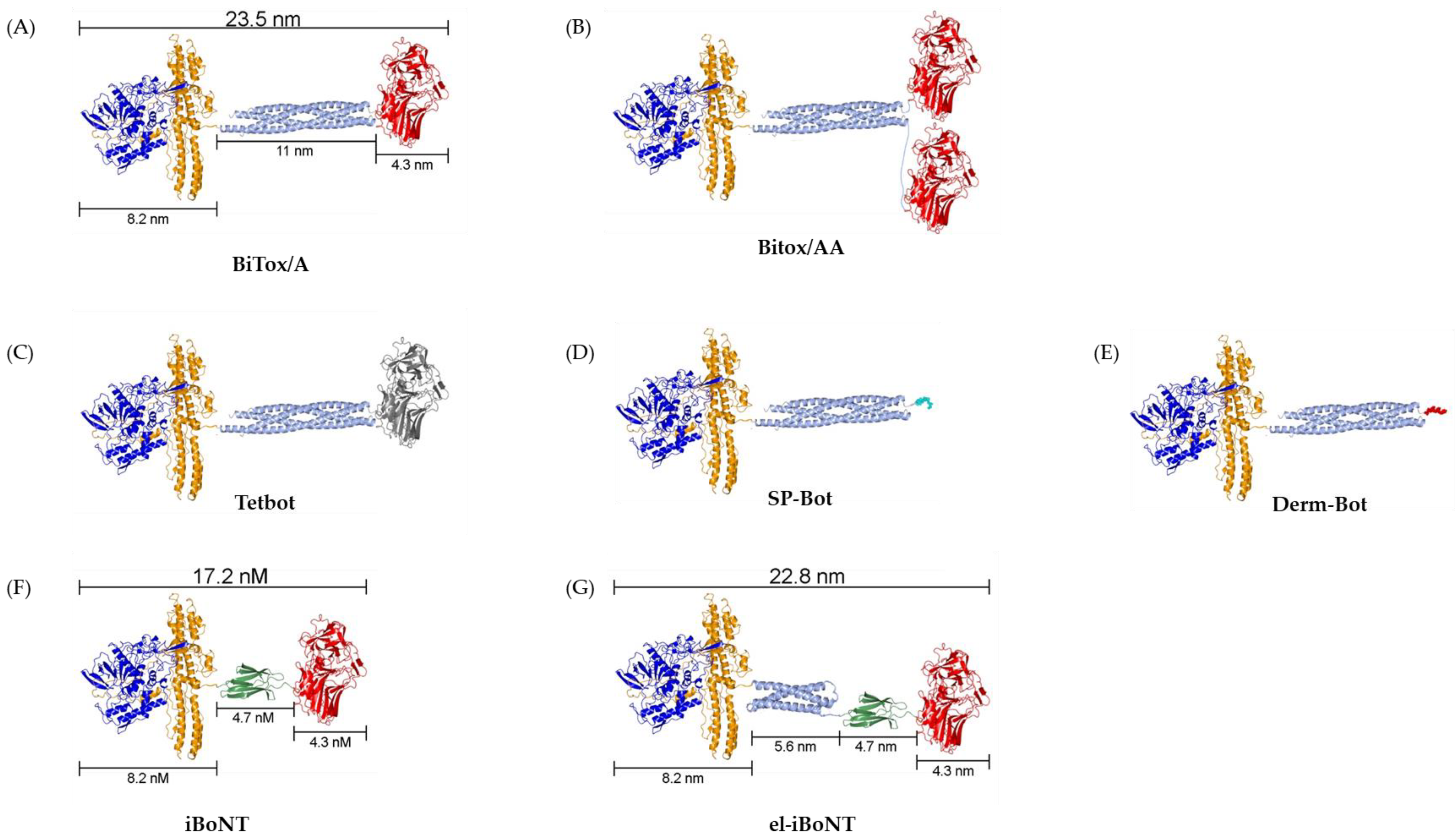
5. Novel BoNT Molecules
6. Future Directions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
List of Abbreviations
| BoNT(s) | Botulinum Neurotoxin(s) |
| SP | Substance P |
| CGRP | Calcitonin Gene-Related Peptide |
| TRPA1 | Transient Receptor Potential Ankyrin 1 |
| TRPV1 | Transient Receptor Potential Vanilloid 1 |
| P2X3 | P2X Purinoceptor 3 |
| FDA | Food and Drug Administration |
| OAB | Overactive Bladder |
| UTI | Urinary Tract Infections |
| TN | Trigeminal Neuralgia |
| HIT-6 | Headache Impact Test |
| SNARE | Soluble N-Ethylmaleimide-Sensitive Factor Attachment Protein Receptor |
| SNAP-25 | Synaptosomal-Associated Protein of 25 kDa |
| IL1β | Interleukin-1β |
| VAMP | Vesicle-Associated Membrane Protein |
| IL6 | Interleukin 6 |
| BiTox | Binary Toxin |
| BiTox/AA | Binary Toxin-AA |
| TetBot | Tetanus-Botulinum Chimera |
| CFA | Freund’s Complete Adjuvant |
| SP-Bot | Substance P-Bot |
| Derm-Bot | Dermorphin-Bot |
| el-iBoNT | Elongated Isopeptide-Bonded Botulinum Neurotoxin |
References
- Scott, A.B. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. J. Pediatr. Ophthalmol. Strabismus 1980, 17, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Tsui, J.K.; Eisen, A.; Mak, E.; Carruthers, J.; Scott, A.B.; Calne, D.B. A pilot study on the use of botulinum toxin in spasmodic torticollis. Can. J. Neurol. Sci. 1985, 12, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Marques, R.E.; Castelão, M.; Ferreira, J.; Sampaio, C.; Moore, A.P.; Costa, J. Botulinum toxin type A therapy for blepharospasm. Cochrane Database Syst. Rev. 2020, 11, CD004900. [Google Scholar] [CrossRef]
- Cariati, M.; Chiarello, M.M.; Cannistra’, M.; Lerose, M.A.; Brisinda, G. Gastrointestinal uses of botulinum toxin. In Botulinum Toxin Therapy; Springer: Cham, Switzerland, 2021; pp. 185–226. [Google Scholar] [CrossRef]
- King, A.; Quirouet, A.; Moore, C.K. Urologic applications of botulinum toxin. Clevel. Clin. J. Med. 2015, 82, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Multani, I.; Manji, J.; Hastings-Ison, T.; Khot, A.; Graham, K. Botulinum toxin in the management of children with cerebral palsy. Pediatr. Drugs 2019, 21, 261–281. [Google Scholar] [CrossRef]
- Martina, E.; Diotallevi, F.; Radi, G.; Campanati, A.; Offidani, A. Therapeutic use of botulinum neurotoxins in dermatology: Systematic review. Toxins 2021, 13, 120. [Google Scholar] [CrossRef] [PubMed]
- Muñoz Lora, V.R.M.; Del Bel Cury, A.A.; Jabbari, B.; Lacković, Z. Botulinum toxin type A in dental medicine. J. Dent. Res. 2019, 98, 1450–1457. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Jost, W. Botulinum toxin treatment of secretory disorders. Mov. Disord. 2004, 19 (Suppl. S8), S137–S141. [Google Scholar] [CrossRef]
- Park, J.; Park, H.J. Botulinum toxin for the treatment of neuropathic pain. Toxins 2017, 9, 260. [Google Scholar] [CrossRef]
- Rossetto, O.; Pirazzini, M.; Fabris, F.; Montecucco, C. Botulinum Neurotoxins: Mechanism of Action. In Botulinum Toxin Therapy; Springer: Cham, Switzerland, 2021; pp. 35–47. [Google Scholar] [CrossRef]
- Beranger, T.; Pierache, A.; Loffer, Z.; Tiffreau, V.; Ferri, J.; Nicot, R. Efficacy of injections of botulinum toxin-A for improving drooling and quality of life in disabled patients. Ann. Phys. Rehabil. Med. 2020, 63, 568–569. [Google Scholar] [CrossRef]
- Welch, M.J.; Purkiss, J.R.; Foster, K.A. Sensitivity of embryonic rat dorsal root ganglia neurons to Clostridium botulinum neurotoxins. Toxicon 2000, 38, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Cui, M.; Khanijou, S.; Rubino, J.; Aoki, K.R. Subcutaneous administration of botulinum toxin A reduces formalin-induced pain. Pain 2004, 107, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Blumenfeld, A.; Silberstein, S.D.; Dodick, D.W.; Aurora, S.K.; Turkel, C.C.; Binder, W.J. Method of injection of onabotulinumtoxinA for chronic migraine: A safe, well-tolerated, and effective treatment paradigm based on the PREEMPT clinical program. Headache J. Head Face Pain 2010, 50, 1406–1418. [Google Scholar] [CrossRef] [PubMed]
- Burstein, R.; Zhang, X.; Levy, D.; Aoki, K.R.; Brin, M.F. Selective inhibition of meningeal nociceptors by botulinum neurotoxin type A: Therapeutic implications for migraine and other pains. Cephalalgia 2014, 34, 853–869. [Google Scholar] [CrossRef] [PubMed]
- Yiangou, Y.; Facer, P.; Ford, A.; Brady, C.; Wiseman, O.; Fowler, C.J.; Anand, P. Capsaicin receptor VR1 and ATP-gated ion channel P2X3 in human urinary bladder. BJU Int. 2001, 87, 774–779. [Google Scholar] [CrossRef] [PubMed]
- Apostolidis, A.; Popat, R.; Yiangou, Y.; Cockayne, D.; Ford, A.P.D.W.; Davis, J.B.; Dasgupta, P.; Fowler, C.J.; Anand, P. Decreased sensory receptors P2X3 and TRPV1 in suburothelial nerve fibers following intradetrusor injections of botulinum toxin for human detrusor overactivity. J. Urol. 2005, 174, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Luvisetto, S.; Vacca, V.; Cianchetti, C. Analgesic effects of botulinum neurotoxin type A in a model of allyl isothiocyanate-and capsaicin-induced pain in mice. Toxicon 2015, 94, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Matak, I.; Bach-Rojecky, L.; Filipović, B.; Lacković, Z. Behavioral and immunohistochemical evidence for central antinociceptive activity of botulinum toxin A. Neuroscience 2011, 186, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Chen, S. Clinical uses of botulinum neurotoxins: Current indications, limitations and future developments. Toxins 2012, 4, 913–939. [Google Scholar] [CrossRef]
- Heckmann, M.; Ceballos-Baumann, A.O.; Plewig, G. Botulinum toxin A for axillary hyperhidrosis (excessive sweating). N. Engl. J. Med. 2001, 344, 488–493. [Google Scholar] [CrossRef]
- Karlqvist, M.; Rosell, K.; Rystedt, A.; Hymnelius, K.; Swartling, C. Botulinum toxin B in the treatment of craniofacial hyperhidrosis. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 1313–1317. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, R.; Quddus, A.; Baker, D.M. Treatment of primary craniofacial hyperhidrosis: A systematic review. Am. J. Clin. Dermatol. 2015, 16, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Jongerius, P.H.; Hoogen, F.J.V.D.; Limbeek, J.V.; Gabreëls, F.J.; Hulst, K.V.; Rotteveel, J.J. Effect of botulinum toxin in the treatment of drooling: A controlled clinical trial. Pediatrics 2004, 114, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Egevad, G.; Petkova, V.Y.; Vilholm, O.J. Sialorrhea in patients with Parkinson’s disease: Safety and administration of botulinum neurotoxin. J. Park. Dis. 2014, 4, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Jost, W.H.; Bäumer, T.; Laskawi, R.; Slawek, J.; Spittau, B.; Steffen, A.; Winterholler, M.; Bavikatte, G. Therapy of sialorrhea with botulinum neurotoxin. Neurol. Ther. 2019, 8, 273–288. [Google Scholar] [CrossRef] [PubMed]
- Heikel, T.; Patel, S.; Ziai, K.; Shah, S.J.; Lighthall, J.G. Botulinum Toxin A in the Management of Pediatric Sialorrhea: A Systematic Review. Ann. Otol. Rhinol. Laryngol. 2023, 132, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.C.; Chung, C.C.; Tu, Y.K.; Hong, C.T.; Chen, K.H.; Tam, K.W.; Kuan, Y.C. Efficacy and safety of botulinum toxin for treating sialorrhea: A systematic review and meta-analysis. Eur. J. Neurol. 2022, 29, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Montoya, F.J.; Riddell, C.E.; Caesar, R.; Hague, S. Treatment of gustatory hyperlacrimation (crocodile tears) with injection of botulinum toxin into the lacrimal gland. Eye 2002, 16, 705–709. [Google Scholar] [CrossRef]
- Pattanayak, S.; Sharma, P.K.; Samikhya, S.; Khuntia, I.; Patra, K. Transconjunctival botulinum toxin injection into the lacrimal gland in crocodile tears syndrome. Indian J. Ophthalmol. 2022, 70, 1339–1342. [Google Scholar] [CrossRef]
- Girard, B.; Piaton, J.-M.; Keller, P.; Nguyen, T.H. Botulinum neurotoxin A injection for the treatment of epiphora with patent lacrymal ducts. J. Français D’ophtalmologie 2018, 41, 343–349. [Google Scholar] [CrossRef]
- Girard, B.; Piaton, J.-M.; Keller, P.; Abadie, C.; Nguyen, T.H. Botulinum neurotoxin injection for the treatment of epiphora in nasolacrimal duct obstruction. J. Français d’Ophtalmologie 2017, 40, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Min, P.; Xi, W.; Grassetti, L.; Trisliana Perdanasari, A.; Torresetti, M.; Feng, S.; Su, W.; Pu, Z.; Zhang, Y.; Han, S.; et al. Sebum production alteration after botulinum toxin type A injections for the treatment of forehead rhytides: A prospective randomized double-blind dose-comparative clinical investigation. Aesthetic Surg. J. 2015, 35, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Shirshakova, M.; Morozova, E.; Sokolova, D.; Pervykh, S.; Smirnova, L. The effectiveness of botulinum toxin type A (BTX-A) in the treatment of facial skin oily seborrhea, enlarged pores, and symptom complex of post-acne. Int. J. Dermatol. 2021, 60, 1232–1241. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, P.F.; Chiu, H.C.; Chen, K.C.; Chang, C.H.; Chou, E.C.L. Botulinum toxin A for the treatment of overactive bladder. Toxins 2016, 8, 59. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.C.; Hsu, L.N.; Lee, W.C.; Chuang, Y.C.; Wang, H.J. Role of Urological Botulinum Toxin-A Injection for Overactive Bladder and Voiding Dysfunction in Patients with Parkinson’s Disease or Post-Stroke. Toxins 2023, 15, 166. [Google Scholar] [CrossRef] [PubMed]
- Chughtai, B.; Ricker, C.N.; Boldt, R.J.; Elterman, D. Real-world onabotulinumtoxinA treatment patterns in patients with overactive bladder. Neurourol. Urodyn. 2024, 43, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Karakeci, A.; Keles, A.; Onur, R. Comparison of the efficacy and safety of onabotulinum toxin A and mirabegron for overactive bladder in elderly patients. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 350–356. [Google Scholar] [CrossRef] [PubMed]
- MacDiarmid, S.; Glazier, D.B.; McCrery, R.J.; Kennelly, M.J.; Nelson, M.; Ifantides, K.B.; McCammon, K.A. Efficacy and safety of an alternative onabotulinumtoxinA injection paradigm for refractory overactive bladder. Neurourol. Urodyn. 2024, 43, 31–43. [Google Scholar] [CrossRef]
- Cui, Y.; Zhou, X.; Zong, H.; Yan, H.; Zhang, Y. The efficacy and safety of onabotulinumtoxinA in treating idiopathic OAB: A systematic review and meta-analysis. Neurourol. Urodyn. 2015, 34, 413–419. [Google Scholar] [CrossRef]
- Zhou, X.; Yan, H.L.; Cui, Y.S.; Zong, H.T.; Zhang, Y. Efficacy and safety of onabotulinumtoxinA in treating neurogenic detrusor overactivity: A systematic review and meta-analysis. Chin. Med. J. 2015, 128, 963–968. [Google Scholar] [CrossRef]
- Reynolds, W.S.; Suskind, A.M.; Anger, J.T.; Brucker, B.M.; Cameron, A.P.; Chung, D.E.; Daignault-Newton, S.; Lane, G.I.; Lucioni, A.; Mourtzinos, A.P.; et al. Incomplete bladder emptying and urinary tract infections after botulinum toxin injection for overactive bladder: Multi-institutional collaboration from the SUFU research network. Neurourol. Urodyn. 2022, 41, 662–671. [Google Scholar] [CrossRef]
- Safarpour, Y.; Jabbari, B. Botulinum toxin treatment of pain syndromes–an evidence based review. Toxicon 2018, 147, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A. Use of botulinum toxin in musculoskeletal pain. F1000Research 2013, 2, 52. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, A.; Smith, H.S. Botulinum toxins: Mechanisms of action, antinociception and clinical applications. Toxicology 2013, 306, 124–146. [Google Scholar] [CrossRef]
- Dodick, D.W.; Turkel, C.C.; DeGryse, R.E.; Aurora, S.K.; Silberstein, S.D.; Lipton, R.B.; Diener, H.C.; Brin, M.F. OnabotulinumtoxinA for treatment of chronic migraine: Pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache J. Head Face Pain 2010, 50, 921–936. [Google Scholar] [CrossRef] [PubMed]
- Aurora, S.K.; Dodick, D.W.; Diener, H.C.; DeGryse, R.E.; Turkel, C.C.; Lipton, R.B.; Silberstein, S.D. OnabotulinumtoxinA for chronic migraine: Efficacy, safety, and tolerability in patients who received all five treatment cycles in the PREEMPT clinical program. Acta Neurol. Scand. 2014, 129, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Lipton, R.B.; Varon, S.F.; Grosberg, B.; McAllister, P.J.; Freitag, F.; Aurora, S.K.; Dodick, D.W.; Silberstein, S.D.; Diener, H.C.; DeGryse, R.E.; et al. OnabotulinumtoxinA improves quality of life and reduces impact of chronic migraine. Neurology 2011, 77, 1465–1472. [Google Scholar] [CrossRef] [PubMed]
- Khalil, M.; Zafar, H.W.; Quarshie, V.; Ahmed, F. Prospective analysis of the use of OnabotulinumtoxinA (BOTOX) in the treatment of chronic migraine; real-life data in 254 patients from Hull, UK. J. Headache Pain 2014, 15, 54. [Google Scholar] [CrossRef]
- Klein, A.W. Complications and adverse reactions with the use of botulinum toxin. Dis. Mon. 2002, 48, 336–356. [Google Scholar] [CrossRef]
- Herd, C.P.; Tomlinson, C.L.; Rick, C.; Scotton, W.J.; Edwards, J.; Ives, N.; Clarke, C.E.; Sinclair, A. Botulinum toxins for the prevention of migraine in adults. Cochrane Database Syst. Rev. 2018, 6, CD011616. [Google Scholar] [CrossRef]
- Wu, S.; Lian, Y.; Zhang, H.; Chen, Y.; Wu, C.; Li, S.; Zheng, Y.; Wang, Y.; Cheng, W.; Huang, Z. Botulinum Toxin Type A for refractory trigeminal neuralgia in older patients: A better therapeutic effect. J. Pain Res. 2019, 12, 2177–2186. [Google Scholar] [CrossRef] [PubMed]
- Tereshko, Y.; Valente, M.; Belgrado, E.; Dalla Torre, C.; Dal Bello, S.; Merlino, G.; Gigli, G.L.; Lettieri, C. The Therapeutic Effect of Botulinum Toxin Type A on Trigeminal Neuralgia: Are There Any Differences between Type 1 versus Type 2 Trigeminal Neuralgia? Toxins 2023, 15, 654. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K. Effects of botulinum toxin type A on pain among trigeminal neuralgia, myofascial temporomandibular disorders, and oromandibular dystonia. Toxins 2021, 13, 605. [Google Scholar] [CrossRef] [PubMed]
- Stuart, M.E.; Strite, S.A.; Gillard, K.K. A systematic evidence-based review of treatments for primary hyperhidrosis. J. Drug Assess. 2021, 10, 35–50. [Google Scholar] [CrossRef] [PubMed]
- Orasanu, B.; Mahajan, S.T. The use of botulinum toxin for the treatment of overactive bladder syndrome. Indian J. Urol. 2013, 29, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Rubis, A.; Juodzbalys, G. The use of botulinum toxin A in the management of trigeminal neuralgia: A systematic literature review. J. Oral Maxillofac. Res. 2020, 11, e2. [Google Scholar] [CrossRef] [PubMed]
- Lacy, D.B.; Tepp, W.; Cohen, A.C.; DasGupta, B.R.; Stevens, R.C. Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat. Struct. Biol. 1998, 5, 898–902. [Google Scholar] [CrossRef] [PubMed]
- Mueller, G.A.; Ankney, J.A.; Glesner, J.; Khurana, T.; Edwards, L.L.; Pedersen, L.C.; Perera, L.; Slater, J.E.; Pomés, A.; London, R.E. Characterization of an anti-Bla g 1 scFv: Epitope mapping and cross-reactivity. Mol. Immunol. 2014, 59, 200–207. [Google Scholar] [CrossRef][Green Version]
- Masuyer, G.; Davies, J.R.; Moore, K.; Chaddock, J.A.; Ravi Acharya, K. Structural analysis of Clostridium botulinum neurotoxin type D as a platform for the development of targeted secretion inhibitors. Sci. Rep. 2015, 5, 13397. [Google Scholar] [CrossRef]
- Camacho, N.P.; Smith, D.R.; Goldman, A.; Schneider, B.; Green, D.; Young, P.R.; Berman, H.M. Structure of an interleukin-1 beta mutant with reduced bioactivity shows multiple subtle changes in conformation that affect protein-protein recognition. Biochemistry 1993, 32, 8749–8757. [Google Scholar] [CrossRef]
- Cao, J.; Belousoff, M.J.; Liang, Y.L.; Johnson, R.M.; Josephs, T.M.; Fletcher, M.M.; Christopoulos, A.; Hay, D.L.; Danev, R.; Wootten, D.; et al. A structural basis for amylin receptor phenotype. Science 2022, 375, eabm9609. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.B.; Fasshauer, D.; Jahn, R.; Brunger, A.T. Crystal structure of a SNARE complex involved in synaptic exocytosis at 2.4 A resolution. Nature 1998, 395, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Lerman, J.C.; Robblee, J.; Fairman, R.; Hughson, F.M. Structural analysis of the neuronal SNARE protein syntaxin-1A. Biochemistry 2000, 39, 8470–8479. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Fierer, J.O.; Rapoport, T.A.; Howarth, M. Structural analysis and optimization of the covalent association between SpyCatcher and a peptide Tag. J. Mol. Biol. 2014, 426, 309–317. [Google Scholar] [CrossRef]
- Harris, J.A.; Faust, B.; Gondin, A.B.; Dämgen, M.A.; Suomivuori, C.M.; Veldhuis, N.A.; Cheng, Y.; Dror, R.O.; Thal, D.M.; Manglik, A. Selective G protein signaling driven by substance P-neurokinin receptor dynamics. Nat. Chem. Biol. 2022, 18, 109–115. [Google Scholar] [CrossRef]
- Ma, H.; Meng, J.; Wang, J.; Hearty, S.; Dolly, J.O.; O’Kennedy, R. Targeted delivery of a SNARE protease to sensory neurons using a single chain antibody (scFv) against the extracellular domain of P2X3 inhibits the release of a pain mediator. Biochem. J. 2014, 462, 247–256. [Google Scholar] [CrossRef]
- Mustafa, G.; Anderson, E.M.; Bokrand-Donatelli, Y.; Neubert, J.K.; Caudle, R.M. Anti-nociceptive effect of a conjugate of substance P and light chain of botulinum neurotoxin type A. Pain 2013, 154, 2547–2553. [Google Scholar] [CrossRef]
- Tang, M.; Meng, J.; Wang, J. New engineered-botulinum toxins inhibit the release of pain-related mediators. Int. J. Mol. Sci. 2019, 21, 262. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, E.; Maywood, E.S.; Restani, L.; Caleo, M.; Pirazzini, M.; Rossetto, O.; Hastings, M.H.; Niranjan, D.; Schiavo, G.; Davletov, B. Re-assembled botulinum neurotoxin inhibits CNS functions without systemic toxicity. Toxins 2011, 3, 345–355. [Google Scholar] [CrossRef]
- Darios, F.; Niranjan, D.; Ferrari, E.; Zhang, F.; Soloviev, M.; Rummel, A.; Bigalke, H.; Suckling, J.; Ushkaryov, Y.; Naumenko, N.; et al. SNARE tagging allows stepwise assembly of a multimodular medicinal toxin. Proc. Natl. Acad. Sci. USA 2010, 107, 18197–18201. [Google Scholar] [CrossRef]
- Mangione, A.S.; Obara, I.; Maiarú, M.; Geranton, S.M.; Tassorelli, C.; Ferrari, E.; Leese, C.; Davletov, B.; Hunt, S.P. Nonparalytic botulinum molecules for the control of pain. Pain 2016, 157, 1045. [Google Scholar] [CrossRef] [PubMed]
- Andreou, A.P.; Leese, C.; Greco, R.; Demartini, C.; Corrie, E.; Simsek, D.; Zanaboni, A.; Koroleva, K.; Lloyd, J.O.; Lambru, G.; et al. Double-binding botulinum molecule with reduced muscle paralysis: Evaluation in in vitro and in vivo models of migraine. Neurotherapeutics 2021, 18, 556–568. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, E.; Gu, C.; Niranjan, D.; Restani, L.; Rasetti-Escargueil, C.; Obara, I.; Geranton, S.M.; Arsenault, J.; Goetze, T.A.; Harper, C.B.; et al. Synthetic self-assembling clostridial chimera for modulation of sensory functions. Bioconjugate Chem. 2013, 24, 1750–1759. [Google Scholar] [CrossRef] [PubMed]
- Maiarù, M.; Leese, C.; Certo, M.; Echeverria-Altuna, I.; Mangione, A.S.; Arsenault, J.; Davletov, B.; Hunt, S.P. Selective neuronal silencing using synthetic botulinum molecules alleviates chronic pain in mice. Sci. Transl. Med. 2018, 10, eaar7384. [Google Scholar] [CrossRef] [PubMed]
- Veggiani, G.; Zakeri, B.; Howarth, M. Superglue from bacteria: Unbreakable bridges for protein nanotechnology. Trends Biotechnol. 2014, 32, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Leese, C.; Christmas, C.; Mészáros, J.; Ward, S.; Maiaru, M.; Hunt, S.P.; Davletov, B. New botulinum neurotoxin constructs for treatment of chronic pain. Life Sci. Alliance 2023, 6, e202201631. [Google Scholar] [CrossRef] [PubMed]
- Bellows, S.; Jankovic, J. Immunogenicity associated with botulinum toxin treatment. Toxins 2019, 11, 491. [Google Scholar] [CrossRef] [PubMed]
- Carr, W.; Jain, N.; Sublett, J. Immunogenicity of botulinum toxin formulations: Potential therapeutic implications. Adv. Ther. 2021, 38, 5046–5064. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, M.; Harrison, A. Profile of Xeomin® (incobotulinumtoxinA) for the treatment of blepharospasm. Clin. Ophthalmol. 2011, 5, 725–732. [Google Scholar] [CrossRef]
- Park, J.; Corduff, N.; Frevert, J.; Wanitphakdeedecha, R.; Chao, Y. Immunogenicity associated with aesthetic botulinumtoxin a: A survey of asia-pacific physicians’ experiences and recommendations. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4217. [Google Scholar] [CrossRef]
- Rummel, A.; Mahrhold, S.; Bigalke, H.; Binz, T. Exchange of the hcc domain mediating double receptor recognition improves the pharmacodynamic properties of botulinum neurotoxin. FEBS J. 2011, 278, 4506–4515. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, K.; Münchau, A.; Thompson, P.; Houser, M.; Chauhan, V.; Hutchinson, M.; Shapira, A.H.; Marsden, C.D. Generalised muscular weakness after botulinum toxin injections for dystonia: A report of three cases. J. Neurol. Neurosurg. Psychiatry 1999, 67, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Yiannakopoulou, E. Serious and long-term adverse events associated with the therapeutic and cosmetic use of botulinum toxin. Pharmacology 2015, 95, 65–69. [Google Scholar] [CrossRef] [PubMed]

| Indication | Adverse Effects Not Related to Myorelaxant Action | Adverse Effects Related to Myorelaxant Action |
|---|---|---|
| Hyperhidrosis [56] | Anhidrosis Pain Bruising | Muscle weakness Facial asymmetry (facial hyperhidrosis) Handgrip weakness (palmar hyperhidrosis) |
| Sialorrhea [27] | Pain Dry mouth Viscous saliva | Tongue control Chewing weakness |
| Overactive bladder [57] | Pain Procedure-related urinary tract infections Mild hematuria | Urinary retention or intermittent self-catheterization |
| Chronic migraine [52] | Pain | Blepharoptosis Muscle weakness |
| Trigeminal neuralgia [58] | Hematoma Itching Pain Transient edema | Facial asymmetry |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhantleuova, A.; Leese, C.; Andreou, A.P.; Karimova, A.; Carpenter, G.; Davletov, B. Recent Developments in Engineering Non-Paralytic Botulinum Molecules for Therapeutic Applications. Toxins 2024, 16, 175. https://doi.org/10.3390/toxins16040175
Zhantleuova A, Leese C, Andreou AP, Karimova A, Carpenter G, Davletov B. Recent Developments in Engineering Non-Paralytic Botulinum Molecules for Therapeutic Applications. Toxins. 2024; 16(4):175. https://doi.org/10.3390/toxins16040175
Chicago/Turabian StyleZhantleuova, Aisha, Charlotte Leese, Anna P. Andreou, Altynay Karimova, Guy Carpenter, and Bazbek Davletov. 2024. "Recent Developments in Engineering Non-Paralytic Botulinum Molecules for Therapeutic Applications" Toxins 16, no. 4: 175. https://doi.org/10.3390/toxins16040175
APA StyleZhantleuova, A., Leese, C., Andreou, A. P., Karimova, A., Carpenter, G., & Davletov, B. (2024). Recent Developments in Engineering Non-Paralytic Botulinum Molecules for Therapeutic Applications. Toxins, 16(4), 175. https://doi.org/10.3390/toxins16040175





