New Insights in the Cytogenetic Practice: Karyotypic Chaos, Non-Clonal Chromosomal Alterations and Chromosomal Instability in Human Cancer and Therapy Response
Abstract
:1. Introduction
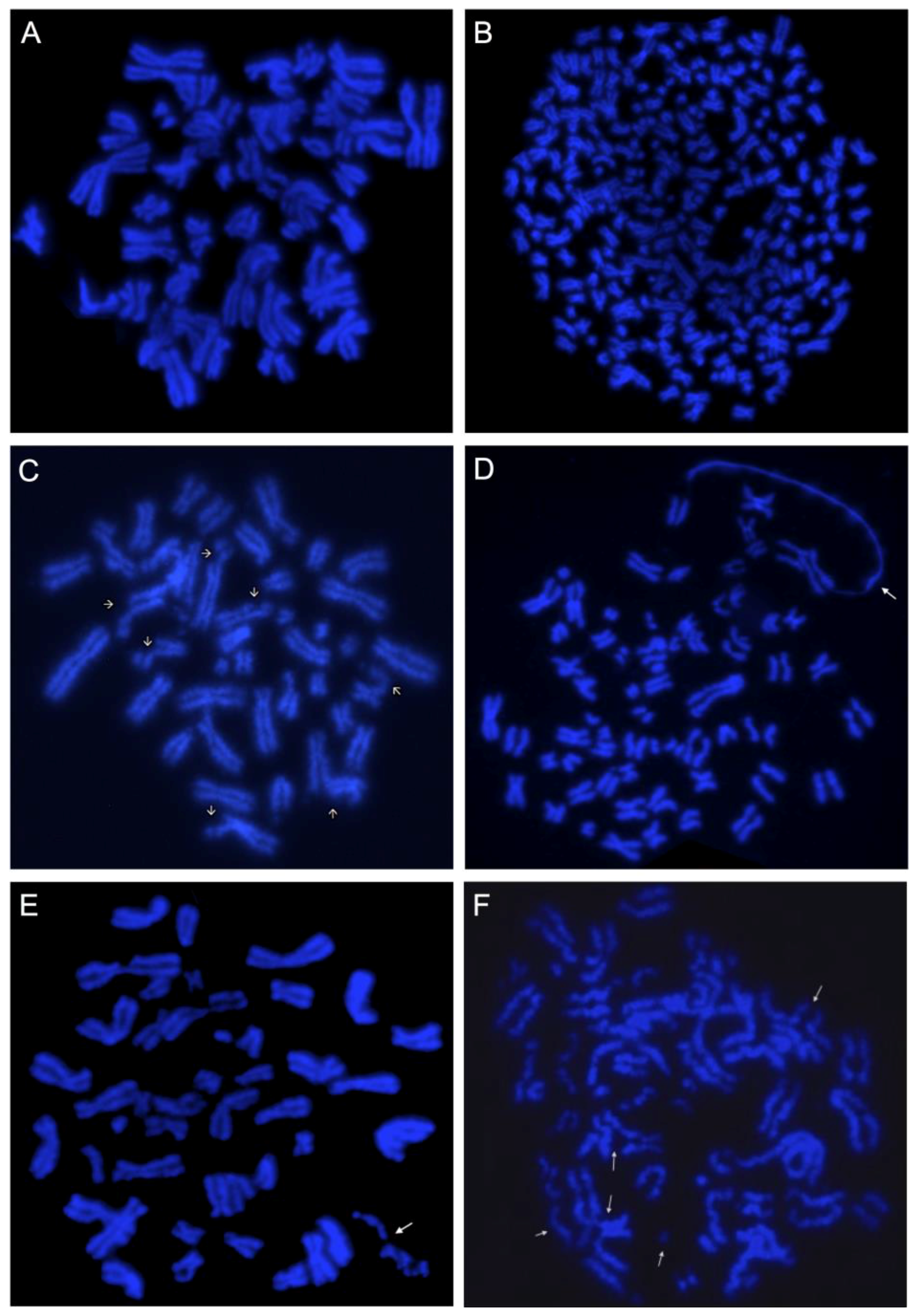
2. Clonal and Non-Clonal Chromosome Alterations (NCCAs)
2.1. Clonal Chromosome Alterations—CCAs
2.2. Non-Clonal Chromosome Alterations (NCCAs)
2.2.1. Chromosomal Breakage
2.2.2. Defective Mitotic Figures
2.2.3. Chromosome Fragmentation (C-Frag)
2.2.4. Large Scale Chromosome Fusion
2.2.5. Chromoplexy
2.2.6. Chromothripsis
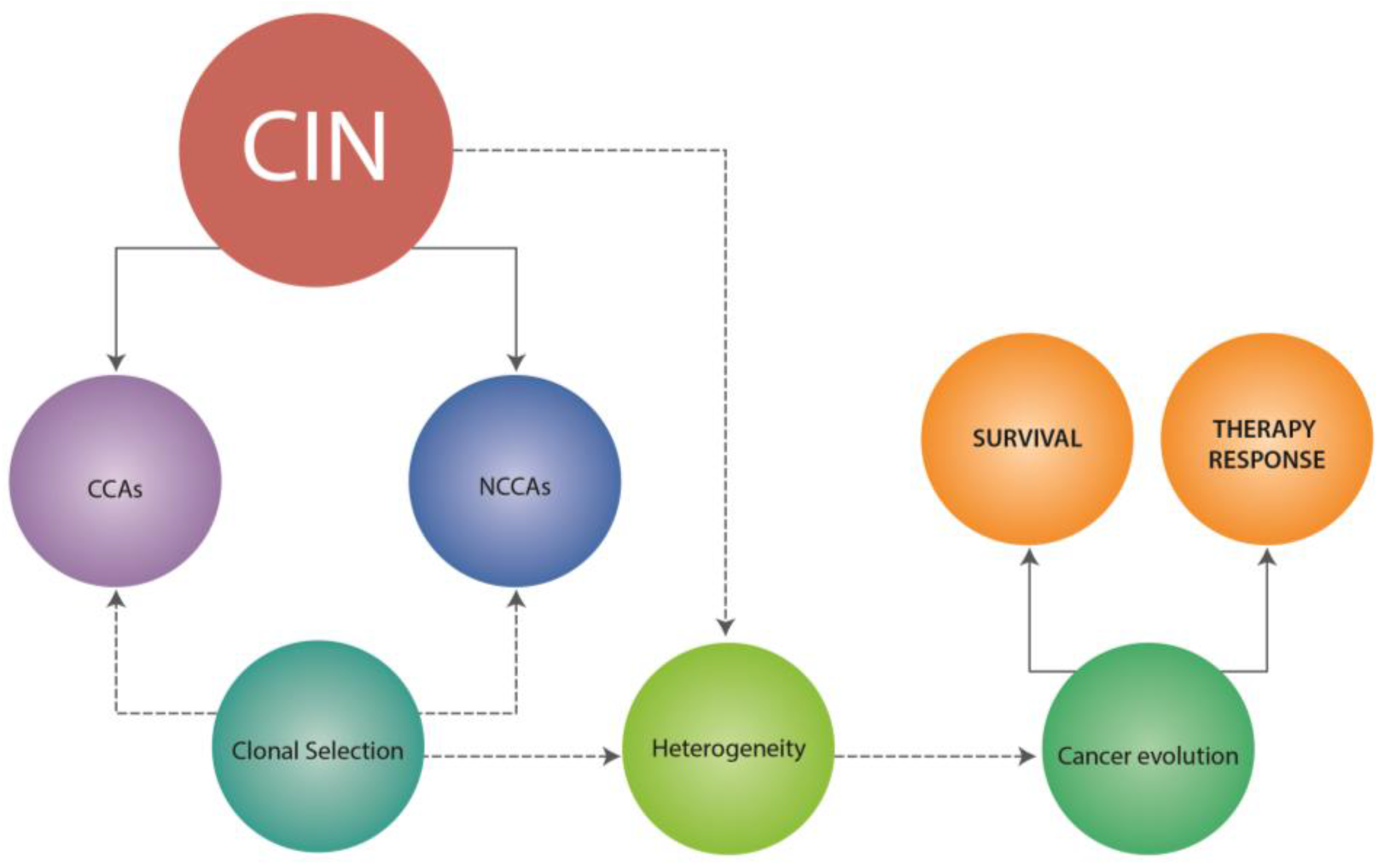
3. CCAs, NCCAs and Cancer Evolution
4. Chromosomal Instability
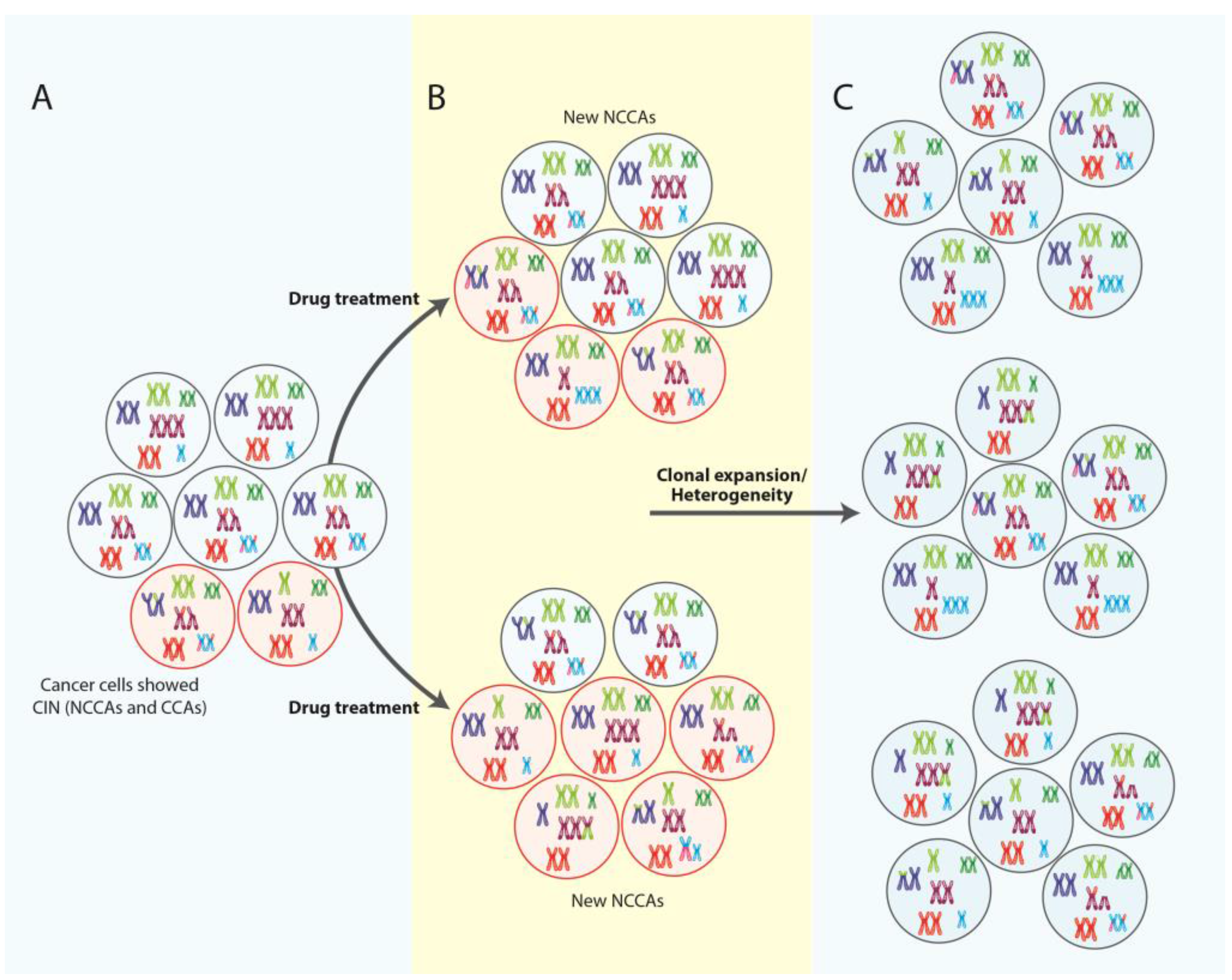
5. NCCAS, CIN and Therapy Response
5.1. Solid Tumors
5.2. Lymphoid Malignancies
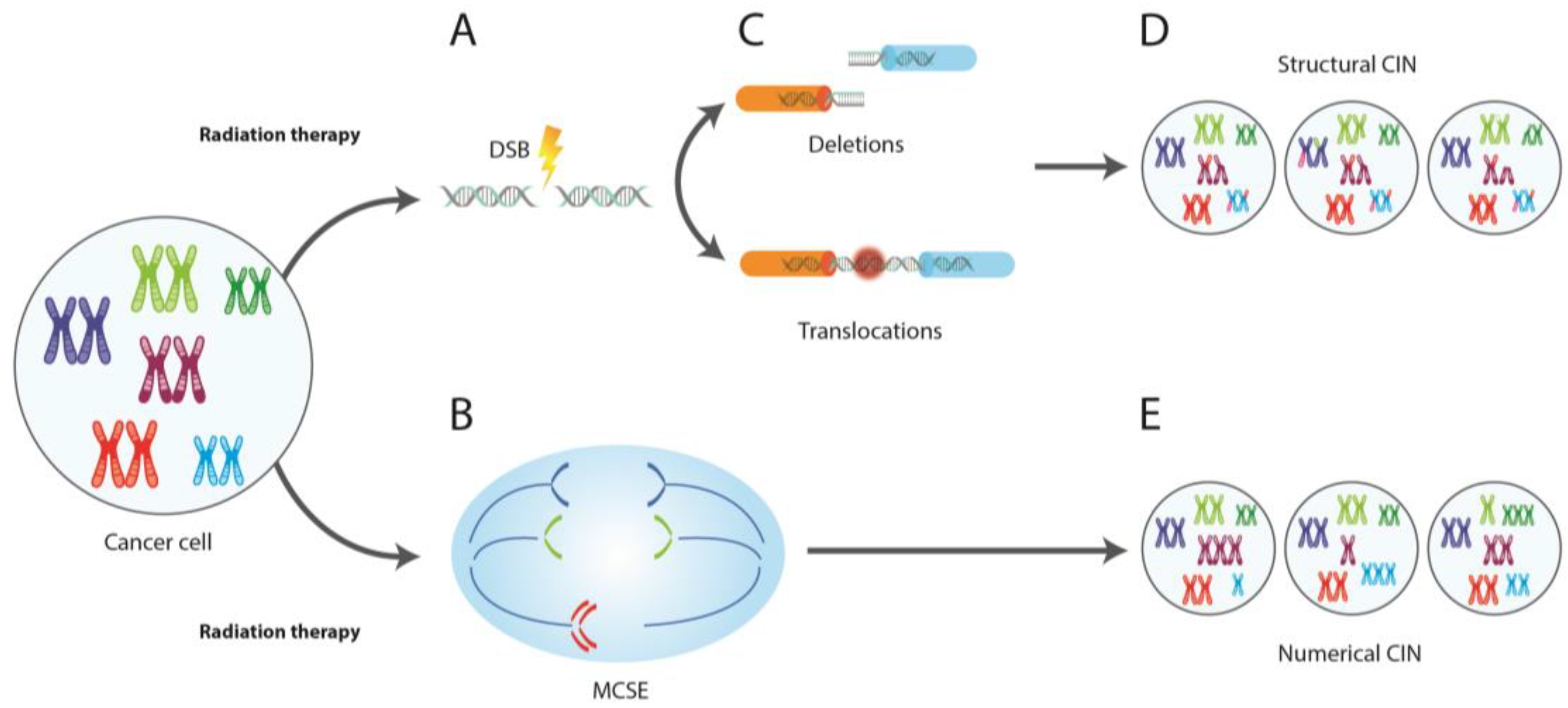
6. CIN and Radiotherapy
7. Conclusions
Acknowledgments
Conflicts of Interest
References
- Liu, G.; Stevens, J.B.; Horne, S.D.; Abdallah, B.Y.; Ye, K.J.; Bremer, S.W.; Ye, C.J.; Chen, D.J.; Heng, H.H. Genome chaos: Survival strategy during crisis. Cell Cycle 2014, 13, 528–537. [Google Scholar] [CrossRef] [PubMed]
- Duesberg, P. Chromosomal chaos and cancer. Sci. Am. 2007, 296, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Stevens, J.B.; Liu, G.; Bremer, S.W.; Ye, K.J.; Reddy, P.V.; Wu, G.S.; Wang, Y.A.; Tainsky, M.A.; Ye, C.J. Stochastic cancer progression driven by non-clonal chromosome aberrations. J. Cell. Physiol. 2006, 208, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Liu, G.; Stevens, J.B.; Abdallah, B.Y.; Horne, S.D.; Ye, K.J.; Bremer, S.W.; Chowdhury, S.K.; Ye, C.J. Karyotype heterogeneity and unclassified chromosomal abnormalities. Cytogenet. Genome Res. 2013, 139, 144–157. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Liu, G.; Stevens, J.B.; Bremer, S.W.; Ye, K.J.; Abdallah, B.Y.; Horne, S.D.; Ye, C.J. Decoding the genome beyond sequencing: The new phase of genomic research. Genomics 2011, 98, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Wahab, M.A.; Nickless, E.M.; Najar-M’kacher, R.; Parmentier, C.; Podd, J.V.; Rowland, R.E. Elevated chromosome translocation frequencies in new zealand nuclear test veterans. Cytogenet. Genome Res. 2008, 121, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Bremer, S.W.; Stevens, J.B.; Horne, S.D.; Liu, G.; Abdallah, B.Y.; Ye, K.J.; Ye, C.J. Chromosomal instability (CIN): What it is and why it is crucial to cancer evolution. Cancer Metastasis Rev. 2013, 32, 325–340. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.M.; Murnane, J.P. Telomeres, chromosome instability and cancer. Nucleic Acids Res. 2006, 34, 2408–2417. [Google Scholar] [CrossRef] [PubMed]
- Burrell, R.A.; McClelland, S.E.; Endesfelder, D.; Groth, P.; Weller, M.C.; Shaikh, N.; Domingo, E.; Kanu, N.; Dewhurst, S.M.; Gronroos, E.; et al. Replication stress links structural and numerical cancer chromosomal instability. Nature 2013, 494, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Dereli-Oz, A.; Versini, G.; Halazonetis, T.D. Studies of genomic copy number changes in human cancers reveal signatures of DNA replication stress. Mol. Oncol. 2011, 5, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Regan, S.M.; Liu, G.; Ye, C.J. Why it is crucial to analyze non clonal chromosome aberrations or NCCAS? Mol. Cytogenet. 2016, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Barbie, T.U.; Alexe, G.; Aref, A.R.; Li, S.; Zhu, Z.; Zhang, X.; Imamura, Y.; Thai, T.C.; Huang, Y.; Bowden, M.; et al. Targeting an IKBKE cytokine network impairs triple-negative breast cancer growth. J. Clin. Investig. 2014, 124, 5411–5423. [Google Scholar] [CrossRef] [PubMed]
- Yagyu, S.; Iehara, T.; Tanaka, S.; Gotoh, T.; Misawa-Furihata, A.; Sugimoto, T.; London, W.B.; Hogarty, M.D.; Teramukai, S.; Nakagawara, A.; et al. Serum-based quantification of MYCN gene amplification in young patients with neuroblastoma: Potential utility as a surrogate biomarker for neuroblastoma. PLoS ONE 2016, 11, e0161039. [Google Scholar] [CrossRef] [PubMed]
- Garraway, L.A.; Widlund, H.R.; Rubin, M.A.; Getz, G.; Berger, A.J.; Ramaswamy, S.; Beroukhim, R.; Milner, D.A.; Granter, S.R.; Du, J.; et al. Integrative genomic analyses identify mitf as a lineage survival oncogene amplified in malignant melanoma. Nature 2005, 436, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Gans, J.D.; Nogueira, C.; Wang, A.; Paik, J.H.; Feng, B.; Brennan, C.; Hahn, W.C.; Cordon-Cardo, C.; Wagner, S.N.; et al. Comparative oncogenomics identifies NEDD9 as a melanoma metastasis gene. Cell 2006, 125, 1269–1281. [Google Scholar] [CrossRef] [PubMed]
- Holst, F.; Stahl, P.R.; Ruiz, C.; Hellwinkel, O.; Jehan, Z.; Wendland, M.; Lebeau, A.; Terracciano, L.; Al-Kuraya, K.; Janicke, F.; et al. Estrogen receptor alpha (ESR1) gene amplification is frequent in breast cancer. Nat. Genet. 2007, 39, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Albertson, D.G. Conflicting evidence on the frequency of esr1 amplification in breast cancer. Nat. Genet. 2008, 40, 821–822. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.V.; Bell, D.W.; Settleman, J.; Haber, D.A. Epidermal growth factor receptor mutations in lung cancer. Nat. Rev. Cancer 2007, 7, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Hudis, C.A. Trastuzumab—Mechanism of action and use in clinical practice. N. Engl. J. Med. 2007, 357, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Cools, J.; Stover, E.H.; Gilliland, D.G. Detection of the FIP1L1-PDGFRA fusion in idiopathic hypereosinophilic syndrome and chronic eosinophilic leukemia. Methods Mol. Med. 2006, 125, 177–187. [Google Scholar] [PubMed]
- Ebert, B.L.; Pretz, J.; Bosco, J.; Chang, C.Y.; Tamayo, P.; Galili, N.; Raza, A.; Root, D.E.; Attar, E.; Ellis, S.R.; et al. Identification of RPS14 as a 5q- syndrome gene by RNA interference screen. Nature 2008, 451, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Sansal, I.; Sellers, W.R. The biology and clinical relevance of the PTEN tumor suppressor pathway. J. Clin. Oncol. 2004, 22, 2954–2963. [Google Scholar] [CrossRef] [PubMed]
- Herrero, A.B.; Rojas, E.A.; Misiewicz-Krzeminska, I.; Krzeminski, P.; Gutierrez, N.C. Molecular mechanisms of p53 deregulation in cancer: An overview in multiple myeloma. Int. J. Mol. Sci. 2016, 17, 2003. [Google Scholar] [CrossRef] [PubMed]
- Tomlins, S.A.; Rhodes, D.R.; Perner, S.; Dhanasekaran, S.M.; Mehra, R.; Sun, X.W.; Varambally, S.; Cao, X.; Tchinda, J.; Kuefer, R.; et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 2005, 310, 644–648. [Google Scholar] [CrossRef] [PubMed]
- Mets, E.; Van der Meulen, J.; Van Peer, G.; Boice, M.; Mestdagh, P.; Van de Walle, I.; Lammens, T.; Goossens, S.; De Moerloose, B.; Benoit, Y.; et al. MicroRNA-193b-3p acts as a tumor suppressor by targeting the MYB oncogene in T-cell acute lymphoblastic leukemia. Leukemia 2015, 29, 798–806. [Google Scholar] [CrossRef] [PubMed]
- Soda, M.; Choi, Y.L.; Enomoto, M.; Takada, S.; Yamashita, Y.; Ishikawa, S.; Fujiwara, S.; Watanabe, H.; Kurashina, K.; Hatanaka, H.; et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007, 448, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Dillon, L.W.; Lehman, C.E.; Wang, Y.H. The role of fragile sites in sporadic papillary thyroid carcinoma. J. Thyroid. Res. 2012, 2012, 927683. [Google Scholar] [CrossRef] [PubMed]
- Licht, J.D.; Sternberg, D.W. The molecular pathology of acute myeloid leukemia. Hematol. Am. Soc. Hematol. Educ. Program 2005, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Morris, S.W.; Valentine, V.; Li, M.; Herbrick, J.A.; Cui, X.; Bouman, D.; Li, Y.; Mehta, P.K.; Nizetic, D.; et al. Fusion of two novel genes, RBM15 and MKL1, in the t(1;22)(p13;q13) of acute megakaryoblastic leukemia. Nat. Genet. 2001, 28, 220–221. [Google Scholar] [CrossRef] [PubMed]
- McIver, B.; Grebe, S.K.; Eberhardt, N.L. The PAX8/PPAR gamma fusion oncogene as a potential therapeutic target in follicular thyroid carcinoma. Curr. Drug Targets Immune Endocr. Metabol. Disord. 2004, 4, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Mathas, S.; Kreher, S.; Meaburn, K.J.; Johrens, K.; Lamprecht, B.; Assaf, C.; Sterry, W.; Kadin, M.E.; Daibata, M.; Joos, S.; et al. Gene deregulation and spatial genome reorganization near breakpoints prior to formation of translocations in anaplastic large cell lymphoma. Proc. Natl. Acad. Sci. USA 2009, 106, 5831–5836. [Google Scholar] [CrossRef] [PubMed]
- Bernheim, A. Cytogenomics of cancers: From chromosome to sequence. Mol. Oncol. 2010, 4, 309–322. [Google Scholar] [CrossRef] [PubMed]
- Bain, B.J. Myeloid and lymphoid neoplasms with eosinophilia and abnormalities of PDGFRA, PDGFRB or FGFR1. Haematologica 2010, 95, 696–698. [Google Scholar] [CrossRef] [PubMed]
- Zech, L.; Haglund, U.; Nilsson, K.; Klein, G. Characteristic chromosomal abnormalities in biopsies and lymphoid-cell lines from patients with Burkitt and non-Burkitt lymphomas. Int. J. Cancer 1976, 17, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Taub, R.; Kirsch, I.; Morton, C.; Lenoir, G.; Swan, D.; Tronick, S.; Aaronson, S.; Leder, P. Translocation of the c-myc gene into the immunoglobulin heavy chain locus in human burkitt lymphoma and murine plasmacytoma cells. Proc. Natl. Acad. Sci. USA 1982, 79, 7837–7841. [Google Scholar] [CrossRef] [PubMed]
- Nowell, P.C. Discovery of the philadelphia chromosome: A personal perspective. J. Clin. Investig. 2007, 117, 2033–2035. [Google Scholar] [CrossRef] [PubMed]
- Soler, G.; Radford, I.; Meyer, C.; Marschalek, R.; Brouzes, C.; Ghez, D.; Romana, S.; Berger, R. MLL insertion with MLL-MLLT3 gene fusion in acute leukemia: Case report and review of the literature. Cancer Genet. Cytogenet. 2008, 183, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Turc-Carel, C.; Philip, I.; Berger, M.P.; Philip, T.; Lenoir, G. [chromosomal translocation (11; 22) in cell lines of ewing’s sarcoma]. C. R. Seances Acad. Sci. III 1983, 296, 1101–1103. [Google Scholar] [PubMed]
- Al-Kawaaz, M.; Mathew, S.; Liu, Y.; Gomez, M.L.; Chaviano, F.; Knowles, D.M.; Orazi, A.; Tam, W. Cyclin D1-positive diffuse large B-cell lymphoma with IGH-CCND1 translocation and BCL6 rearrangement: A report of two cases. Am. J. Clin. Pathol. 2015, 143, 288–299. [Google Scholar] [CrossRef] [PubMed]
- Seethala, R.R.; Chiosea, S.I.; Liu, C.Z.; Nikiforova, M.; Nikiforov, Y.E. Clinical and morphologic features of ETV6-NTRK3 translocated papillary thyroid carcinoma in an adult population without radiation exposure. Am. J. Surg. Pathol. 2017, 41, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Uphoff, C.C.; MacLeod, R.A.; Denkmann, S.A.; Golub, T.R.; Borkhardt, A.; Janssen, J.W.; Drexler, H.G. Occurrence of TEL-AML1 fusion resulting from (12;21) translocation in human early b-lineage leukemia cell lines. Leukemia 1997, 11, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Chase, A.; Reiter, A.; Burci, L.; Cazzaniga, G.; Biondi, A.; Pickard, J.; Roberts, I.A.; Goldman, J.M.; Cross, N.C. Fusion of ETV6 to the caudal-related homeobox gene CDX2 in acute myeloid leukemia with the t(12;13)(p13;q12). Blood 1999, 93, 1025–1031. [Google Scholar] [PubMed]
- Bakhshi, A.; Wright, J.J.; Graninger, W.; Seto, M.; Owens, J.; Cossman, J.; Jensen, J.P.; Goldman, P.; Korsmeyer, S.J. Mechanism of the t(14;18) chromosomal translocation: Structural analysis of both derivative 14 and 18 reciprocal partners. Proc. Natl. Acad. Sci. USA 1987, 84, 2396–2400. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, P.H.; Lessnick, S.L.; Lopez-Terrada, D.; Liu, X.F.; Triche, T.J.; Denny, C.T. A second Ewing’s sarcoma translocation, t(21;22), fuses the EWS gene to another ETS-family transcription factor, ERG. Nat. Genet. 1994, 6, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Liu, G.; Bremer, S.; Ye, K.J.; Stevens, J.; Ye, C.J. Clonal and non-clonal chromosome aberrations and genome variation and aberration. Genome 2006, 49, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.J.; Stevens, J.B.; Liu, G.; Bremer, S.W.; Jaiswal, A.S.; Ye, K.J.; Lin, M.F.; Lawrenson, L.; Lancaster, W.D.; Kurkinen, M.; et al. Genome based cell population heterogeneity promotes tumorigenicity: The evolutionary mechanism of cancer. J. Cell. Physiol. 2009, 219, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Hecht, F.; Sutherland, G.R. Detection of fragile sites on human chromosomes. Clin. Genet. 1985, 28, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Stevens, J.B.; Liu, G.; Bremer, S.W.; Ye, C.J. Imaging genome abnormalities in cancer research. Cell Chromosome 2004, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Lopez de Mesa, R.; Sierrasesumaga, L.; Calasanz, M.J.; Lopez de Cerain, A.L.; Patino-Garcia, A. Nonclonal chromosomal aberrations induced by anti-tumoral regimens in childhood cancer: Relationship with cancer-related genes and fragile sites. Cancer Genet. Cytogenet. 2000, 121, 78–85. [Google Scholar] [CrossRef]
- Vincent-Salomon, A.; Benhamo, V.; Gravier, E.; Rigaill, G.; Gruel, N.; Robin, S.; de Rycke, Y.; Mariani, O.; Pierron, G.; Gentien, D.; et al. Genomic instability: A stronger prognostic marker than proliferation for early stage luminal breast carcinomas. PLoS ONE 2013, 8, e76496. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.Q.; Chen, W.Y.; Wang, Y.C. Effects of pingyanymycin on chromosomes: A possible structural basis for chromosome aberration. Mutat. Res. 1988, 199, 199–205. [Google Scholar] [CrossRef]
- Smith, L.; Plug, A.; Thayer, M. Delayed replication timing leads to delayed mitotic chromosome condensation and chromosomal instability of chromosome translocations. Proc. Natl. Acad. Sci. USA 2001, 98, 13300–13305. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.B.; Liu, G.; Bremer, S.W.; Ye, K.J.; Xu, W.; Xu, J.; Sun, Y.; Wu, G.S.; Savasan, S.; Krawetz, S.A.; et al. Mitotic cell death by chromosome fragmentation. Cancer Res. 2007, 67, 7686–7694. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.B.; Abdallah, B.Y.; Liu, G.; Ye, C.J.; Horne, S.D.; Wang, G.; Savasan, S.; Shekhar, M.; Krawetz, S.A.; Huttemann, M.; et al. Diverse system stresses: Common mechanisms of chromosome fragmentation. Cell Death Dis. 2011, 2, e178. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H.; Bremer, S.W.; Stevens, J.; Ye, K.J.; Miller, F.; Liu, G.; Ye, C.J. Cancer progression by non-clonal chromosome aberrations. J. Cell. Biochem. 2006, 98, 1424–1435. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.B.; Abdallah, B.Y.; Regan, S.M.; Liu, G.; Bremer, S.W.; Ye, C.J.; Heng, H.H. Comparison of mitotic cell death by chromosome fragmentation to premature chromosome condensation. Mol. Cytogenet. 2010, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- Baca, S.C.; Prandi, D.; Lawrence, M.S.; Mosquera, J.M.; Romanel, A.; Drier, Y.; Park, K.; Kitabayashi, N.; MacDonald, T.Y.; Ghandi, M.; et al. Punctuated evolution of prostate cancer genomes. Cell 2013, 153, 666–677. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.M. Chromoplexy: A new category of complex rearrangements in the cancer genome. Cancer Cell 2013, 23, 567–569. [Google Scholar] [CrossRef] [PubMed]
- Forment, J.V.; Kaidi, A.; Jackson, S.P. Chromothripsis and cancer: Causes and consequences of chromosome shattering. Nat. Rev. Cancer 2012, 12, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.J.; Jallepalli, P.V. Chromothripsis: Chromosomes in crisis. Dev. Cell 2012, 23, 908–917. [Google Scholar] [CrossRef] [PubMed]
- Hatch, E.M.; Hetzer, M.W. Chromothripsis. Curr. Biol. 2015, 25, R397–R399. [Google Scholar] [CrossRef] [PubMed]
- Nijhawan, D.; Zack, T.I.; Ren, Y.; Strickland, M.R.; Lamothe, R.; Schumacher, S.E.; Tsherniak, A.; Besche, H.C.; Rosenbluh, J.; Shehata, S.; et al. Cancer vulnerabilities unveiled by genomic loss. Cell 2012, 150, 842–854. [Google Scholar] [CrossRef] [PubMed]
- Kloosterman, W.P.; Koster, J.; Molenaar, J.J. Prevalence and clinical implications of chromothripsis in cancer genomes. Curr. Opin. Oncol. 2014, 26, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Kumar, N.; Bagheri, H.C.; von Mering, C.; Robinson, M.D.; Baudis, M. Chromothripsis-like patterns are recurring but heterogeneously distributed features in a survey of 22,347 cancer genome screens. BMC Genom. 2014, 15, 82. [Google Scholar] [CrossRef] [PubMed]
- Przybytkowski, E.; Lenkiewicz, E.; Barrett, M.T.; Klein, K.; Nabavi, S.; Greenwood, C.M.; Basik, M. Chromosome-breakage genomic instability and chromothripsis in breast cancer. BMC Genom. 2014, 15, 579. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, D.; Kemmerling, R.; Davis, S.; Camps, J.; Meltzer, P.S.; Ried, T.; Gaiser, T. Chromothripsis and focal copy number alterations determine poor outcome in malignant melanoma. Cancer Res. 2013, 73, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Magrangeas, F.; Avet-Loiseau, H.; Munshi, N.C.; Minvielle, S. Chromothripsis identifies a rare and aggressive entity among newly diagnosed multiple myeloma patients. Blood 2011, 118, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Molenaar, J.J.; Koster, J.; Zwijnenburg, D.A.; van Sluis, P.; Valentijn, L.J.; van der Ploeg, I.; Hamdi, M.; van Nes, J.; Westerman, B.A.; van Arkel, J.; et al. Sequencing of neuroblastoma identifies chromothripsis and defects in neuritogenesis genes. Nature 2012, 483, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Rausch, T.; Jones, D.T.; Zapatka, M.; Stutz, A.M.; Zichner, T.; Weischenfeldt, J.; Jager, N.; Remke, M.; Shih, D.; Northcott, P.A.; et al. Genome sequencing of pediatric medulloblastoma links catastrophic DNA rearrangements with TP53 mutations. Cell 2012, 148, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Tubio, J.M.; Estivill, X. Cancer: When catastrophe strikes a cell. Nature 2011, 470, 476–477. [Google Scholar] [CrossRef] [PubMed]
- Meyerson, M.; Pellman, D. Cancer genomes evolve by pulverizing single chromosomes. Cell 2011, 144, 9–10. [Google Scholar] [CrossRef] [PubMed]
- Crasta, K.; Ganem, N.J.; Dagher, R.; Lantermann, A.B.; Ivanova, E.V.; Pan, Y.; Nezi, L.; Protopopov, A.; Chowdhury, D.; Pellman, D. DNA breaks and chromosome pulverization from errors in mitosis. Nature 2012, 482, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.Z.; Spektor, A.; Cornils, H.; Francis, J.M.; Jackson, E.K.; Liu, S.; Meyerson, M.; Pellman, D. Chromothripsis from DNA damage in micronuclei. Nature 2015, 522, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Terradas, M.; Martin, M.; Tusell, L.; Genesca, A. Genetic activities in micronuclei: Is the DNA entrapped in micronuclei lost for the cell? Mutat. Res. 2010, 705, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Bakhoum, S.F.; Kabeche, L.; Wood, M.D.; Laucius, C.D.; Qu, D.; Laughney, A.M.; Reynolds, G.E.; Louie, R.J.; Phillips, J.; Chan, D.A.; et al. Numerical chromosomal instability mediates susceptibility to radiation treatment. Nat. Commun. 2015, 6, 5990. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.M.; Xi, R.; Luquette, L.J.; Park, R.W.; Johnson, M.D.; Park, P.J. Functional genomic analysis of chromosomal aberrations in a compendium of 8000 cancer genomes. Genome Res. 2013, 23, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Forero-Castro, M.; Robledo, C.; Benito, R.; Abaigar, M.; Africa Martin, A.; Arefi, M.; Fuster, J.L.; de Las Heras, N.; Rodriguez, J.N.; Quintero, J.; et al. Genome-wide DNA copy number analysis of acute lymphoblastic leukemia identifies new genetic markers associated with clinical outcome. PLoS ONE 2016, 11, e0148972. [Google Scholar] [CrossRef] [PubMed]
- Abaigar, M.; Robledo, C.; Benito, R.; Ramos, F.; Diez-Campelo, M.; Hermosin, L.; Sanchez-Del-Real, J.; Alonso, J.M.; Cuello, R.; Megido, M.; et al. Chromothripsis is a recurrent genomic abnormality in high-risk myelodysplastic syndromes. PLoS ONE 2016, 11, e0164370. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, A.; Lindberg, M.; Faust, G.G.; Leibowitz, M.L.; Clark, R.A.; Layer, R.M.; Quinlan, A.R.; Hall, I.M. Breakpoint profiling of 64 cancer genomes reveals numerous complex rearrangements spawned by homology-independent mechanisms. Genome Res. 2013, 23, 762–776. [Google Scholar] [CrossRef] [PubMed]
- Stephens, P.J.; Greenman, C.D.; Fu, B.; Yang, F.; Bignell, G.R.; Mudie, L.J.; Pleasance, E.D.; Lau, K.W.; Beare, D.; Stebbings, L.A.; et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell 2011, 144, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Niederwieser, C.; Nicolet, D.; Carroll, A.J.; Kolitz, J.E.; Powell, B.L.; Kohlschmidt, J.; Stone, R.M.; Byrd, J.C.; Mrozek, K.; Bloomfield, C.D. Chromosome abnormalities at onset of complete remission are associated with worse outcome in patients with acute myeloid leukemia and an abnormal karyotype at diagnosis: CALGB 8461 (alliance). Haematologica 2016, 101, 1516–1523. [Google Scholar] [CrossRef] [PubMed]
- Navin, N.; Kendall, J.; Troge, J.; Andrews, P.; Rodgers, L.; McIndoo, J.; Cook, K.; Stepansky, A.; Levy, D.; Esposito, D.; et al. Tumour evolution inferred by single-cell sequencing. Nature 2011, 472, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Waters, J.; Leung, M.L.; Unruh, A.; Roh, W.; Shi, X.; Chen, K.; Scheet, P.; Vattathil, S.; Liang, H.; et al. Clonal evolution in breast cancer revealed by single nucleus genome sequencing. Nature 2014, 512, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Hoffelder, D.R.; Luo, L.; Burke, N.A.; Watkins, S.C.; Gollin, S.M.; Saunders, W.S. Resolution of anaphase bridges in cancer cells. Chromosoma 2004, 112, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Pikor, L.; Thu, K.; Vucic, E.; Lam, W. The detection and implication of genome instability in cancer. Cancer Metastasis Rev. 2013, 32, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Castro-Gamero, A.M.; Borges, K.S.; Lira, R.C.; Andrade, A.F.; Fedatto, P.F.; Cruzeiro, G.A.; Silva, R.B.; Fontes, A.M.; Valera, E.T.; Bobola, M.; et al. Chromosomal heterogeneity and instability characterize pediatric medulloblastoma cell lines and affect neoplastic phenotype. Cytotechnology 2013, 65, 871–885. [Google Scholar] [CrossRef] [PubMed]
- McCormack, A.; Fan, J.L.; Duesberg, M.; Bloomfield, M.; Fiala, C.; Duesberg, P. Individual karyotypes at the origins of cervical carcinomas. Mol. Cytogenet. 2013, 6, 44. [Google Scholar] [CrossRef] [PubMed]
- Stepanenko, A.A.; Vassetzky, Y.S.; Kavsan, V.M. Antagonistic functional duality of cancer genes. Gene 2013, 529, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Valind, A.; Gisselsson, D. Reply to duesberg: Stability of peritriploid and triploid states in neoplastic and nonneoplastic cells. Proc. Natl. Acad. Sci. USA 2014, 111, E975. [Google Scholar] [CrossRef] [PubMed]
- Heng, H.H. Debating Cancer: The Paradox in Cancer Research; World Scientific Publishing Co Pte Ltd: Singapore, 2016; p. 400. [Google Scholar]
- Gagos, S.; Irminger-Finger, I. Chromosome instability in neoplasia: Chaotic roots to continuous growth. Int. J. Biochem. Cell Biol. 2005, 37, 1014–1033. [Google Scholar] [CrossRef] [PubMed]
- Bayani, J.; Selvarajah, S.; Maire, G.; Vukovic, B.; Al-Romaih, K.; Zielenska, M.; Squire, J.A. Genomic mechanisms and measurement of structural and numerical instability in cancer cells. Semin. Cancer Biol. 2007, 17, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Hirota, T. Chromosomal instability: A common feature and a therapeutic target of cancer. Biochim. Biophys. Acta 2016, 1866, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Geigl, J.B.; Obenauf, A.C.; Schwarzbraun, T.; Speicher, M.R. Defining ‘chromosomal instability’. Trends Genet. 2008, 24, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Chandrakasan, S.; Ye, C.J.; Chitlur, M.; Mohamed, A.N.; Rabah, R.; Konski, A.; Heng, H.H.; Savasan, S. Malignant fibrous histiocytoma two years after autologous stem cell transplant for hodgkin lymphoma: Evidence for genomic instability. Pediatr. Blood Cancer 2011, 56, 1143–1145. [Google Scholar] [CrossRef] [PubMed]
- Bakhoum, S.F.; Danilova, O.V.; Kaur, P.; Levy, N.B.; Compton, D.A. Chromosomal instability substantiates poor prognosis in patients with diffuse large B-cell lymphoma. Clin. Cancer Res. 2011, 17, 7704–7711. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.L.; Compton, D.A. Chromosomes and cancer cells. Chromosome Res. 2011, 19, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Dayal, J.; Albergant, L.; Newman, T.; South, A. Quantitation of multiclonality in control and drug-treated tumour populations using high-throughput analysis of karyotypic heterogeneity. Converg. Sci. Phys. Oncol. 2015, 1, 2. [Google Scholar] [CrossRef]
- Fedorenko, I.V.; Wargo, J.A.; Flaherty, K.T.; Messina, J.L.; Smalley, K.S. Braf inhibition generates a host-tumor niche that mediates therapeutic escape. J. Investig. Dermatol. 2015, 135, 3115–3124. [Google Scholar] [CrossRef] [PubMed]
- Horne, S.; Wexler, M.; Stevens, J.; Heng, H.H. Insights on processes of evolutionary tumor growth. Atlas Genet. Cytogenet. Oncol. Haematol. Available online: http://AtlasGeneticsOncology.org/Deep/EvolTumorGrowthID20142.htm (accessed on 1 April 2017).
- Rondón-Lagos, M.; Villegas, V.E.; Rangel, N.; Sanchez, M.C.; Zaphiropoulos, P.G. Tamoxifen resistance: Emerging molecular targets. Int. J. Mol. Sci. 2016, 17, 1357. [Google Scholar] [CrossRef] [PubMed]
- Gao, C.; Furge, K.; Koeman, J.; Dykema, K.; Su, Y.; Cutler, M.L.; Werts, A.; Haak, P.; Vande Woude, G.F. Chromosome instability, chromosome transcriptome, and clonal evolution of tumor cell populations. Proc. Natl. Acad. Sci. USA 2007, 104, 8995–9000. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.J.; Endesfelder, D.; Rowan, A.J.; Walther, A.; Birkbak, N.J.; Futreal, P.A.; Downward, J.; Szallasi, Z.; Tomlinson, I.P.; Howell, M.; et al. Chromosomal instability confers intrinsic multidrug resistance. Cancer Res. 2011, 71, 1858–1870. [Google Scholar] [CrossRef] [PubMed]
- Davoli, T.; Uno, H.; Wooten, E.C.; Elledge, S.J. Tumor aneuploidy correlates with markers of immune evasion and with reduced response to immunotherapy. Science 2017, 355, eaaf8399. [Google Scholar] [CrossRef] [PubMed]
- Hiley, C.T.; Swanton, C. Spatial and temporal cancer evolution: Causes and consequences of tumour diversity. Clin. Med. (Lond.) 2014, 14 (Suppl. 6), s33–s37. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.L.; Eklund, A.C.; Kohane, I.S.; Harris, L.N.; Szallasi, Z. A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat. Genet. 2006, 38, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- Bakhoum, S.F.; Compton, D.A. Chromosomal instability and cancer: A complex relationship with therapeutic potential. J. Clin. Investig. 2012, 122, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Salas, C.; Niembro, A.; Lozano, V.; Gallardo, E.; Molina, B.; Sanchez, S.; Ramos, S.; Carnevale, A.; Perez-Vera, P.; Rivera Luna, R.; et al. Persistent genomic instability in peripheral blood lymphocytes from Hodgkin lymphoma survivors. Environ. Mol. Mutagen. 2012, 53, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Walther, A.; Houlston, R.; Tomlinson, I. Association between chromosomal instability and prognosis in colorectal cancer: A meta-analysis. Gut 2008, 57, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Jamal-Hanjani, M.; A’Hern, R.; Birkbak, N.J.; Gorman, P.; Gronroos, E.; Ngang, S.; Nicola, P.; Rahman, L.; Thanopoulou, E.; Kelly, G.; et al. Extreme chromosomal instability forecasts improved outcome in er-negative breast cancer: A prospective validation cohort study from the tact trial. Ann. Oncol. 2015, 26, 1340–1346. [Google Scholar] [CrossRef] [PubMed]
- Roylance, R.; Endesfelder, D.; Gorman, P.; Burrell, R.A.; Sander, J.; Tomlinson, I.; Hanby, A.M.; Speirs, V.; Richardson, A.L.; Birkbak, N.J.; et al. Relationship of extreme chromosomal instability with long-term survival in a retrospective analysis of primary breast cancer. Cancer Epidemiol. Biomark. Prev. 2011, 20, 2183–2194. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Mao, J.H.; Zhu, W.; Jain, A.K.; Liu, K.; Brown, J.B.; Karpen, G.H. Centromere and kinetochore gene misexpression predicts cancer patient survival and response to radiotherapy and chemotherapy. Nat. Commun. 2016, 7, 12619. [Google Scholar] [CrossRef] [PubMed]
- Janssen, A.; Kops, G.J.; Medema, R.H. Elevating the frequency of chromosome mis-segregation as a strategy to kill tumor cells. Proc. Natl. Acad. Sci. USA 2009, 106, 19108–19113. [Google Scholar] [CrossRef] [PubMed]
- Galimberti, F.; Thompson, S.L.; Ravi, S.; Compton, D.A.; Dmitrovsky, E. Anaphase catastrophe is a target for cancer therapy. Clin. Cancer Res. 2011, 17, 1218–1222. [Google Scholar] [CrossRef] [PubMed]
- Orticello, M.; Fiore, M.; Totta, P.; Desideri, M.; Barisic, M.; Passeri, D.; Lenzi, J.; Rosa, A.; Orlandi, A.; Maiato, H.; et al. N-terminus-modified HEC1 suppresses tumour growth by interfering with kinetochore-microtubule dynamics. Oncogene 2015, 34, 3325–3335. [Google Scholar] [CrossRef] [PubMed]
- Bakhoum, S.F.; Thompson, S.L.; Manning, A.L.; Compton, D.A. Genome stability is ensured by temporal control of kinetochore-microtubule dynamics. Nat. Cell Biol. 2009, 11, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Rondón-Lagos, M.; Verdun Di Cantogno, L.; Rangel, N.; Mele, T.; Ramirez-Clavijo, S.R.; Scagliotti, G.; Marchio, C.; Sapino, A. Unraveling the chromosome 17 patterns of FISH in interphase nuclei: An in-depth analysis of the HER2 amplicon and chromosome 17 centromere by karyotyping, FISH and M-FISH in breast cancer cells. BMC Cancer 2014, 14, 922. [Google Scholar] [CrossRef] [PubMed]
- Smid, M.; Hoes, M.; Sieuwerts, A.M.; Sleijfer, S.; Zhang, Y.; Wang, Y.; Foekens, J.A.; Martens, J.W. Patterns and incidence of chromosomal instability and their prognostic relevance in breast cancer subtypes. Breast Cancer Res. Treat 2011, 128, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Burrell, R.A.; Juul, N.; Johnston, S.R.; Reis-Filho, J.S.; Szallasi, Z.; Swanton, C. Targeting chromosomal instability and tumour heterogeneity in HER2-positive breast cancer. J. Cell Biochem. 2010, 111, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Ott, K.; Vogelsang, H.; Mueller, J.; Becker, K.; Muller, M.; Fink, U.; Siewert, J.R.; Hofler, H.; Keller, G. Chromosomal instability rather than p53 mutation is associated with response to neoadjuvant cisplatin-based chemotherapy in gastric carcinoma. Clin. Cancer Res. 2003, 9, 2307–2315. [Google Scholar] [PubMed]
- Juul, N.; Wang, Y.A.; Kim, J.; Eklund, A.; Li, Q.; Carlton, V.; Gerlinger, M.; Swanton, C.; Garber, J.; Silver, D.; et al. A genomic-profile derived summary measure of chromosomal breakpoints predicts response to treatment with the DNA-damaging agent cisplatin. Cancer Res. 2009, 69. [Google Scholar] [CrossRef]
- Swanton, C.; Nicke, B.; Schuett, M.; Eklund, A.C.; Ng, C.; Li, Q.; Hardcastle, T.; Lee, A.; Roy, R.; East, P.; et al. Chromosomal instability determines taxane response. Proc. Natl. Acad. Sci. USA 2009, 106, 8671–8676. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, K.I.; Shepherd, L.E.; O’Malley, F.P.; Andrulis, I.L.; Tu, D.; Bramwell, V.H.; Levine, M.N. National Cancer Institute of Canada Clinical Trials, G. HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N. Engl. J. Med. 2006, 354, 2103–2111. [Google Scholar] [CrossRef] [PubMed]
- Sikov, W.M.; Dizon, D.S.; Strenger, R.; Legare, R.D.; Theall, K.P.; Graves, T.A.; Gass, J.S.; Kennedy, T.A.; Fenton, M.A. Frequent pathologic complete responses in aggressive stages II to III breast cancers with every-4-week carboplatin and weekly paclitaxel with or without trastuzumab: A brown university oncology group study. J. Clin. Oncol. 2009, 27, 4693–4700. [Google Scholar] [CrossRef] [PubMed]
- Kuppers, R. Mechanisms of b-cell lymphoma pathogenesis. Nat. Rev. Cancer 2005, 5, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Nussenzweig, A.; Nussenzweig, M.C. Origin of chromosomal translocations in lymphoid cancer. Cell 2010, 141, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Greisman, H.A.; Lu, Z.; Tsai, A.G.; Greiner, T.C.; Yi, H.S.; Lieber, M.R. IgH partner breakpoint sequences provide evidence that aid initiates t(11;14) and t(8;14) chromosomal breaks in mantle cell and burkitt lymphomas. Blood 2012, 120, 2864–2867. [Google Scholar] [CrossRef] [PubMed]
- Nanjangud, G.; Rao, P.H.; Hegde, A.; Teruya-Feldstein, J.; Donnelly, G.; Qin, J.; Jhanwar, S.C.; Zelenetz, A.D.; Chaganti, R.S. Spectral karyotyping identifies new rearrangements, translocations, and clinical associations in diffuse large B-cell lymphoma. Blood 2002, 99, 2554–2561. [Google Scholar] [CrossRef] [PubMed]
- Diehl, V.; Stein, H.; Hummel, M.; Zollinger, R.; Connors, J.M. Hodgkin’s lymphoma: Biology and treatment strategies for primary, refractory, and relapsed disease. Hematol. Am. Soc. Hematol. Educ. Program 2003, 225–247. [Google Scholar] [CrossRef]
- Thomson, A.B.; Wallace, W.H. Treatment of paediatric Hodgkin’s disease. A balance of risks. Eur. J. Cancer 2002, 38, 468–477. [Google Scholar] [CrossRef]
- Constine, L.S.; Tarbell, N.; Hudson, M.M.; Schwartz, C.; Fisher, S.G.; Muhs, A.G.; Basu, S.K.; Kun, L.E.; Ng, A.; Mauch, P.; et al. Subsequent malignancies in children treated for hodgkin’s disease: Associations with gender and radiation dose. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Sieniawski, M.; Franklin, J.; Nogova, L.; Glossmann, J.P.; Schober, T.; Nisters-Backes, H.; Diehl, V.; Josting, A. Outcome of patients experiencing progression or relapse after primary treatment with two cycles of chemotherapy and radiotherapy for early-stage favorable hodgkin’s lymphoma. J. Clin. Oncol. 2007, 25, 2000–2005. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.L.; Whitton, J.; Leisenring, W.; Mertens, A.C.; Hammond, S.; Stovall, M.; Donaldson, S.S.; Meadows, A.T.; Robison, L.L.; Neglia, J.P. Subsequent neoplasms in 5-year survivors of childhood cancer: The childhood cancer survivor study. J. Natl. Cancer Inst. 2010, 102, 1083–1095. [Google Scholar] [CrossRef] [PubMed]
- Linch, D.C.; Gosden, R.G.; Tulandi, T.; Tan, S.L.; Hancock, S.L. Hodgkin’s lymphoma: Choice of therapy and late complications. Hematol. Am. Soc. Hematol. Educ. Program 2000, 205–221. [Google Scholar] [CrossRef]
- Foss Abrahamsen, A.; Andersen, A.; Nome, O.; Jacobsen, A.B.; Holte, H.; Foss Abrahamsen, J.; Kvaloy, S. Long-term risk of second malignancy after treatment of Hodgkin’s disease: The influence of treatment, age and follow-up time. Ann. Oncol. 2002, 13, 1786–1791. [Google Scholar] [CrossRef] [PubMed]
- Sarli, V.; Giannis, A. Targeting the kinesin spindle protein: Basic principles and clinical implications. Clin. Cancer Res. 2008, 14, 7583–7587. [Google Scholar] [CrossRef] [PubMed]
- Krem, M.M.; Press, O.W.; Horwitz, M.S.; Tidwell, T. Mechanisms and clinical applications of chromosomal instability in lymphoid malignancy. Br. J. Haematol. 2015, 171, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Shah, J.J.; Orlowski, R.Z. Novel approaches to treatment of double-refractory multiple myeloma. Am. Soc. Clin. Oncol. Educ. Book 2013. [Google Scholar] [CrossRef] [PubMed]
- Gerecitano, J.F.; Stephenson, J.J.; Lewis, N.L.; Osmukhina, A.; Li, J.; Wu, K.; You, Z.; Huszar, D.; Skolnik, J.M.; Schwartz, G.K. A phase I trial of the kinesin spindle protein (Eg5) inhibitor AZD4877 in patients with solid and lymphoid malignancies. Investig. New Drugs 2013, 31, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Baskar, R.; Lee, K.A.; Yeo, R.; Yeoh, K.W. Cancer and radiation therapy: Current advances and future directions. Int. J. Med. Sci. 2012, 9, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, R.D.; D’Andrea, A.D. DNA repair pathways in clinical practice: Lessons from pediatric cancer susceptibility syndromes. J. Clin. Oncol. 2006, 24, 3799–3808. [Google Scholar] [CrossRef] [PubMed]
- Zaki, B.I.; Suriawinata, A.A.; Eastman, A.R.; Garner, K.M.; Bakhoum, S.F. Chromosomal instability portends superior response of rectal adenocarcinoma to chemoradiation therapy. Cancer 2014, 120, 1733–1742. [Google Scholar] [CrossRef] [PubMed]
| CCAs | Altered Genes | Disease | Target Therapy | References |
|---|---|---|---|---|
| amp(1)(q32.1) | IKBKE | Breast cancer | Inhibitor CYT387 | Barbie, et al., 2014 [12] |
| amp(2)(p24.1) | MYCN | Neuroblastoma | Yagyu, et al., 2016 [13] | |
| amp(3)(p14.2-p14.1) | MITF | Malignant melanoma | Garraway, et al., 2005 [14] | |
| Kim, et al., 2006 [15] | ||||
| amp(6)(q25.1) | ESR1 | Breast cancer | Tamoxifen | Holst, et al., 2007 [16] |
| Albertson, et al., 2008 [17] | ||||
| amp(7)(p12) | EGFR | Various cancers | Cetuximab, panitumumab, gefitinib | Sharma, et al., 2007 [18] |
| amp(17)(q21.1) | ERBB2 | Various cancers | Trastuzumab, lapatinib | Hudis, et al., 2007 [19] |
| del(4)(q12q12) | FIP1L1-PDGFRA | Myeloid neoplasm associated with eosinophilia | Imatinib | Cools, et al., 2006 [20] |
| del(5)(q32) | RPS14 | Myelodysplastic syndrome | Lenalidomide | Ebert, et al., 2008 [21] |
| del(10)(q23.3) | PTEN | Various cancers | Sirolimus | Sansal, et al., 2004 [22] |
| del(17)(p13.1) | TP53 | Various cancers | Herrero, et al., 2016 [23] | |
| del(21)(q22.3q22.3) | TMPRSS2-ERG | Prostate cancer | Tomlins, et al., 2005 [24] | |
| dup(6)(q22-q23) | MYB | Acute lymphoblastic leukemia | MicroRNA-193b-3p | Mets, et al., 2015 [25] |
| inv(2)(p21p23) | EML4-ALK | Non–small-cell lung cancer | Soda, et al., 2007 [26] | |
| inv(10)(q11.2q11.2) | RET-NCOA4 | Papillary thyroid cancer | Dillon, et al., 2012 [27] | |
| inv(10)(q11.2q21) | RET-CCDC6 | Papillary thyroid cancer | Dillon, et al., 2012 [27] | |
| inv(16)(p13.11q22.1) | CBFB-MYH11 | Acute myeloid leukemia | Licht, et al., 2005 [28] | |
| t(1;22)(p13;q13) | RBM15-MKL1 | Acute megakaryoblastic leukemia | Ma, et al., 2001 [29] | |
| t(2;3)(q12-q14;p25) | PAX8-PPARG | Follicular thyroid cancer | McIver, et al., 2004 [30] | |
| t(2;5)(p23;q35) | ALK-NPM1 | Anaplastic large-cell lymphoma | Mathas, et al., 2009 [31] | |
| t(4;14)(p16.3;q32.33) | WHSC1-IGHG1 | Multiple myeloma | Bernheim, et al., 2010 [32] | |
| t(5;12)(q31-q32;p13) | PDGFRB-ETV6 | Myeloid neoplasm associated with eosinophilia | Imatinib | Bain, et al., 2010 [33] |
| t(8;21)(q22;q22.3) | RUNX1-RUNX1T1 | Acute myeloid leukemia | Licht, et al., 2005 [28] | |
| t(8;14)(q24.21;q32.33) | MYC-IGHG1 | Burkitt’s lymphoma | Zech, et al., 1976 [34] | |
| Taub, et al., 1982 [35] | ||||
| t(9;22)(q34.1;q11.23) | BCR-ABL1 | Chronic myeloid leukemia, acute lymphoblastic leukemia, acute myeloid leukemia | Imatinib, dasatinib, nilotinib | Nowell, et al., 2007 [36] |
| t(9;11)(p22;q23) | MLL-MLLT3 | Acute myeloid leukemia | Soler, et al., 2008 [37] | |
| t(11;22)(q24.1;q12.2) | FLI1-EWSR1 | Ewing’s sarcoma | Turc-Carel, et al., 1983 [38] | |
| t(11;14)(q13;q32.33) | CCND1-IGHG1 | Mantle-cell lymphoma | Al-Kawaaz, et al., 2015 [39] | |
| t(12;15)(p13;q25) | ETV6-NTRK3 | Various cancers | Seethala, et al., 2017 [40] | |
| t(12;21)(p13;q22.3) | ETV6-RUNX1 | Acute lymphoblastic leukemia | Uphoff, et al., 1997 [41] | |
| t(12;13)(p13;q12.3) | ETV6-CDX2 | Acute myeloid leukemia | Chase, et al., 1999 [42] | |
| t(14;18)(q32.33;q21.3) | IGHG1-BCL2 | Follicular lymphoma | Bakhshi, et al., 1987 [43] | |
| t(15;17)(q22;q21) | PML-RARA | Acute promyelocytic leukemia | All-trans retinoic acid, arsenic trioxide | Licht, et al., 2005 [28] |
| t(21;22)(q22.3;q12.2) | ERG-EWSR1 | Ewing’s sarcoma | Sorensen, et al., 1994 [44] |
| Neoplasia | Type of NCCAs | Incidence | Correlated with | References |
|---|---|---|---|---|
| Primary breast tumors | Chromotripsis | 41.4% | Early recurrence, high risk tumors | Przybytkowski, et al., 2014 [65] |
| Multiple myeloma | Chromotripsis | 1.3% | Poor clinical outcome, rapid release | Magrangeas, et al., 2011 [67] |
| Neuroblastoma | Chromotripsis | 18% | Poor prognosis | Molenaar, et al., 2012 [68] |
| Pediatric cancer | NCCAs | 75% | Non indicated | Lopez de Mesa, et al., 2000 [49] |
| Acute Myeloid Leukemia | Structural NCCAs | 7% | Poor prognosis | Niederwieser, et al., 2016 [81] |
| Cervical, papillary and squamous cell carcinomas | DMFs | NI | NI | Smith, et al., 2001 [52] |
| Breast cancer, Lipoma | C-Frag | NI | Evolutionary potential | Stevens, et al., 2011 [54] |
| Brain and hematological malignancies, Leukocytosis. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rangel, N.; Forero-Castro, M.; Rondón-Lagos, M. New Insights in the Cytogenetic Practice: Karyotypic Chaos, Non-Clonal Chromosomal Alterations and Chromosomal Instability in Human Cancer and Therapy Response. Genes 2017, 8, 155. https://doi.org/10.3390/genes8060155
Rangel N, Forero-Castro M, Rondón-Lagos M. New Insights in the Cytogenetic Practice: Karyotypic Chaos, Non-Clonal Chromosomal Alterations and Chromosomal Instability in Human Cancer and Therapy Response. Genes. 2017; 8(6):155. https://doi.org/10.3390/genes8060155
Chicago/Turabian StyleRangel, Nelson, Maribel Forero-Castro, and Milena Rondón-Lagos. 2017. "New Insights in the Cytogenetic Practice: Karyotypic Chaos, Non-Clonal Chromosomal Alterations and Chromosomal Instability in Human Cancer and Therapy Response" Genes 8, no. 6: 155. https://doi.org/10.3390/genes8060155






