A Machine Learning Approach for Chronic Heart Failure Diagnosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Dataset
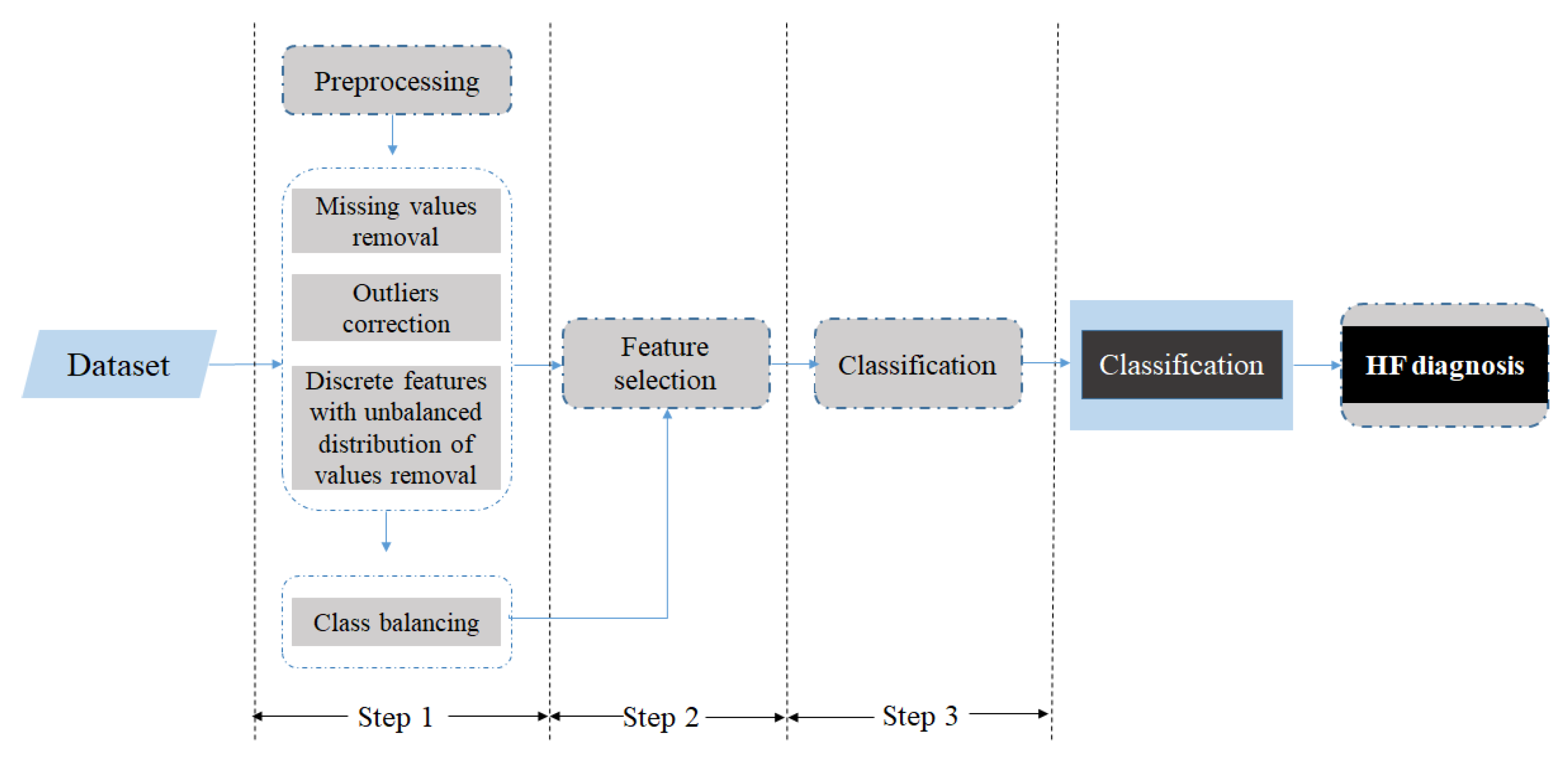
2.2. The Proposed Methodology
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
HF Diagnosis Classification Results without CAD and Arr-Afib Features
| Features Type | Classifier | Accuracy % | Sensitivity % | Specificity % |
|---|---|---|---|---|
| Clinical features | NB | 75.36 | 80.70 | 67.30 |
| Clinical features and BNP | ROT | 86.02 | 92.80 | 77.50 |
| Clinical and echocardiographic features | ROT | 88.39 | 92.70 | 82.30 |
| All features | ROT | 90.28 | 94.00 | 85.00 |
Appendix B
Contribution of Each Individual Feature to the Predicted Outcome
| Ranking | Feature | Information Gain |
|---|---|---|
| 1 | BNP | 0.4202 |
| 2 | Arr_Afib | 0.3076 |
| 3 | LAVI | 0.302 |
| 4 | EF | 0.2813 |
| 5 | DBP | 0.131 |
| 6 | LVMI | 0.1181 |
| 7 | CAD | 0.1143 |
| 8 | SBP | 0.1129 |
| 9 | Hypertension | 0.0905 |
| 10 | Peak_E_Value | 0.066 |
| 11 | Age | 0.0544 |
| 12 | Gender | 0.0489 |
| 13 | Ee | 0.0405 |
| 14 | MI | 0.0393 |
| 15 | LVIDd | 0.0312 |
| 16 | E Deceleration Time | 0.02 |
| 17 | HR | 0 |
| 18 | BMI | 0 |
| 19 | Ee | 0 |
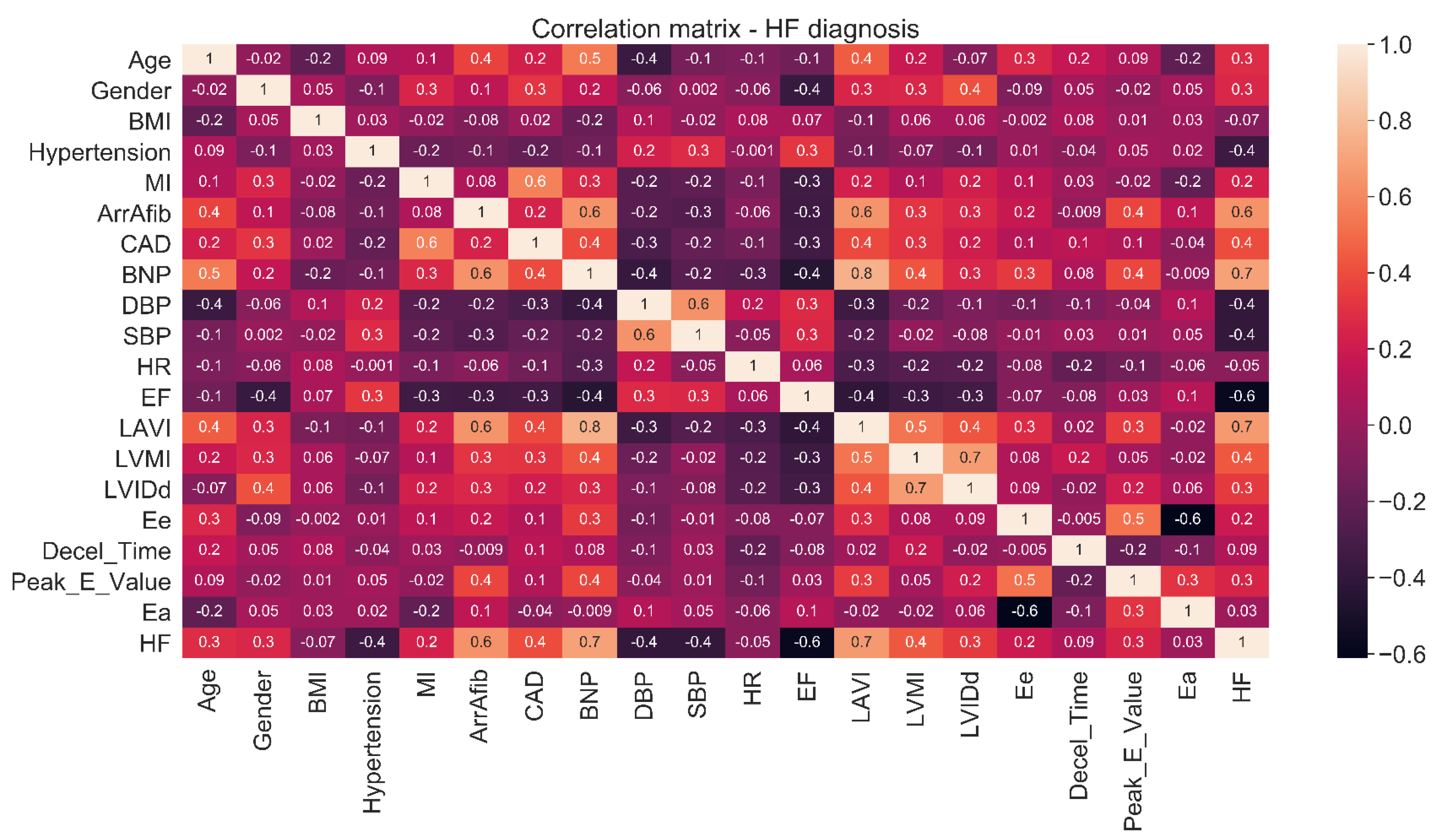
| Feature | Correlation with Class |
|---|---|
| Age | 0.3 |
| Gender | 0.3 |
| BMI | –0.07 |
| Hypertension | –0.4 |
| MI | 0.2 |
| Arr-Afib | 0.6 |
| CAD | 0.4 |
| BNP | 0.7 |
| SBP | –0.4 |
| DBP | –0.4 |
| HR | –0.05 |
| EF | –0.6 |
| LAVI | 0.7 |
| LVMI | 0.4 |
| LVIDd | 0.3 |
| Ee | 0.2 |
| E Deceleration time | 0.09 |
| Peak_E_Value | 0.3 |
| EA | 0.03 |
| Chi-Square Test | p-Value | |
|---|---|---|
| LAVI | 12.791 | <0.001 |
| LVMI | 8.467 | <0.001 |
| SBP | –7.987 | <0.001 |
| BNP | 14.2434 | <0.001 |
| EF | –11.659 | <0.001 |
| HyperT | 53.74 | <0.001 |
| Arr-Afib | 172.51 | <0.001 |
| CAD | 67.11 | <0.001 |
Appendix C
Results from the Logistic Regression for Clinical Features
| Accuracy % | Sensitivity % | Specificity % | |
|---|---|---|---|
| Logistic regression | 84.12 | 88.10 | 78.10 |
| LMT | 84.12 | 82.10 | 85.38 |
References
- Braunwald, E.; Zipes, D.P.; Libby, P.; Bonow, R.O. Heart Disease: A Textbook of Cardiovascular Medicine, 7th ed.; Elsevier Science: Philadelphia, PA, USA, 2004. [Google Scholar]
- Sabate, E. Adherence to Long-Term Therapies, Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Franzén, K.; Saveman, B.-I.; Blomqvist, K. Predictors for Health Related Quality of Life in Persons 65 Years or Older with Chronic Heart Failure. Eur. J. Cardiovasc. Nurs. 2007, 6, 112–120. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J.; Howard, V.J.; et al. Heart Disease and Stroke Statistics—2015 Update. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef] [Green Version]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Ali, L.; Niamat, A.; Khan, J.A.; Golilarz, N.A.; Xingzhong, X.; Noor, A.; Nour, R.; Bukhari, S.A.C. An Optimized Stacked Support Vector Machines Based Expert System for the Effective Prediction of Heart Failure. IEEE Access 2019, 7, 54007–54014. [Google Scholar] [CrossRef]
- Javeed, A.; Zhou, S.; Yongjian, L.; Qasim, I.; Noor, A.; Nour, R. An Intelligent Learning System Based on Random Search Algorithm and Optimized Random Forest Model for Improved Heart Disease Detection. IEEE Access 2019, 7, 180235–180243. [Google Scholar] [CrossRef]
- Samuel, O.W.; Asogbon, G.M.; Sangaiah, A.K.; Fang, P.; Li, G. An integrated decision support system based on ANN and Fuzzy_AHP for heart failure risk prediction. Expert Syst. Appl. 2017, 68, 163–172. [Google Scholar] [CrossRef]
- Mohan, S.; Thirumalai, C.; Srivastava, G. Effective Heart Disease Prediction Using Hybrid Machine Learning Techniques. IEEE Access 2019, 7, 81542–81554. [Google Scholar] [CrossRef]
- Potter, E.L.; Rodrigues, C.; Ascher, D.; Marwick, T.H. Machine Learning Applied to Energy Waveform Ecg for Prediction of Stage B Heart Failure in the Community. J. Am. Coll. Cardiol. 2020, 75, 1894. [Google Scholar] [CrossRef]
- Choi, E.; Schuetz, A.; Stewart, W.F.; Sun, J. Using recurrent neural network models for early detection of heart failure onset. J. Am. Med. Inform. Assoc. 2017, 24, 361–370. [Google Scholar] [CrossRef]
- Son, C.-S.; Kim, Y.-N.; Kim, H.-S.; Park, H.-S.; Kim, M.-S. Decision-making model for early diagnosis of congestive heart failure using rough set and decision tree approaches. J. Biomed. Inform. 2012, 45, 999–1008. [Google Scholar] [CrossRef] [Green Version]
- Reddy, Y.N.V.; Carter, R.E.; Obokata, M.; Redfield, M.M.; Borlaug, B.A. A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure With Preserved Ejection Fraction. Circulation 2018, 138, 861–870. [Google Scholar] [CrossRef]
- Masetic, Z.; Subasi, A. Congestive heart failure detection using random forest classifier. Comput. Methods Programs Biomed. 2016, 130, 54–64. [Google Scholar] [CrossRef]
- Acharya, U.R.; Fujita, H.; Oh, S.L.; Hagiwara, Y.; Tan, J.H.; Adam, M.; Tan, R.S. Deep convolutional neural network for the automated diagnosis of congestive heart failure using ECG signals. Appl. Intell. 2019, 49, 16–27. [Google Scholar] [CrossRef]
- Ning, W.; Li, S.; Wei, D.; Guo, L.Z.; Chen, H. Automatic Detection of Congestive Heart Failure Based on a Hybrid Deep Learning Algorithm in the Internet of Medical Things. IEEE Internet Things J. 2021, 8, 12550–12558. [Google Scholar] [CrossRef]
- Lal, H.; Wajid, A.; Ishtiaq, K.; Monagi, A.; Jalal, A. Detecting Congestive Heart Failure by Extracting Multimodal Features and Employing Machine Learning Techniques. BioMed Res. Int. 2020, 6, 1–19. [Google Scholar]
- Wang, L.; Zhou, X. Detection of Congestive Heart Failure Based on LSTM-Based Deep Network via Short-Term RR Intervals. Sensors 2019, 19, 1502. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Liu, G.; Su, S.; Jiang, Q.; Nguyen, H. A CHF detection method based on deep learning with RR intervals. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Korea, 11–15 July 2017; pp. 3369–3372. [Google Scholar]
- Gladence, L.M.; Ravi, T.; Karthi, M. An enhanced method for detecting congestive heart failure—Automatic Classifier. In Proceedings of the 2014 IEEE International Conference on Advanced Communications, Control and Computing Technologies, Ramanathapuram, India, 8–10 May 2014; pp. 586–590. [Google Scholar]
- Zheng, Y.; Guo, X.; Qin, J.; Xiao, S. Computer-assisted diagnosis for chronic heart failure by the analysis of their cardiac reserve and heart sound characteristics. Comput. Methods Programs Biomed. 2015, 122, 372–383. [Google Scholar] [CrossRef]
- Gjoreski, M.; Gradisek, A.; Budna, B.; Gams, M.; Poglajen, G. Machine Learning and End-to-End Deep Learning for the Detection of Chronic Heart Failure From Heart Sounds. IEEE Access 2020, 8, 20313–20324. [Google Scholar] [CrossRef]
- From, A.M.; Lam, C.S.P.; Pitta, S.R.; Kumar, P.V.; Balbissi, K.A.; Booker, J.D.; Singh, I.M.; Sorajja, P.; Reeder, G.S.; Borlaug, B.A. Bedside Assessment of Cardiac Hemodynamics: The Impact of Noninvasive Testing and Examiner Experience. Am. J. Med. 2011, 124, 1051–1057. [Google Scholar] [CrossRef] [PubMed]
- Thibodeau, J.; Drazner, M.H. The Role of the Clinical Examination in Patients With Heart Failure. JACC Heart Fail. 2018, 6, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Luengo, J.; Fernández, A.; García, S.; Herrera, F. Addressing data complexity for imbalanced data sets: Analysis of SMOTE-based oversampling and evolutionary undersampling. Soft Comput. 2010, 15, 1909–1936. [Google Scholar] [CrossRef]
- Quinlan, J.R. Induction of Decision Trees. Mach. Learn. 1986, 1, 81–106. [Google Scholar] [CrossRef] [Green Version]
- Hall, M. Correlation-Based Feature Selection for Machine Learning; University of Waikato: Hamilton, New Zealand, 1998. [Google Scholar]
- Marcot, B.G.; Hanea, A.M. What is an optimal value of k in k-fold cross-validation in discrete Bayesian network analysis? Comput. Stat. 2021, 36, 2009–2031. [Google Scholar] [CrossRef]
- Zaphiriou, A.; Robb, S.; Murray-Thomas, T.; Mendez, G.; Fox, K.; McDonagh, T.; Hardman, S.M.; Dargie, H.J.; Cowie, M.R. The diagnostic accuracy of plasma BNP and NTproBNP in patients referred from primary care with suspected heart failure: Results of the UK natriuretic peptide study. Eur. J. Heart Fail. 2005, 7, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Duchnowski, P.; Hryniewiecki, T.; Małgorzata, K.; Kuśmierczyk, M.; Szymański, P. High-sensitivity troponin T is a prognostic marker of hemodynamic instability in patients undergoing valve surgery. Biomark. Med. 2018, 12, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- Duchnowski, P.; Hryniewiecki, T.; Kuśmierczyk, M.; Szymański, P. High-Sensitivity Troponin T Predicts Postoperative Cardiogenic Shock Requiring Mechanical Circulatory Support in Patients With Valve Disease. Shock 2020, 53, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Eggers, K.M.; Lindahl, B. Application of Cardiac Troponin in Cardiovascular Diseases Other Than Acute Coronary Syndrome. Clin. Chem. 2017, 63, 223–235. [Google Scholar] [CrossRef] [PubMed]

| Study | Target | Method | Features | Dataset | Measures |
|---|---|---|---|---|---|
| Zheng et al. [21] (2015) | Chronic HF diagnosis Healthy vs. chronic HF | Least square-Stacked Support Vector Machine (SVM) model | Cardiac reserve and heart sound characteristics | 152 subjects 88 controls 64 chronic with HF | Acc 95.39% Sens 96.59% Spec 93.75% |
| Masetic et al. [14] (2016) | Congestive HF diagnosis Healthy vs. congestive HF | Decision tree, K-Nearest Neighbors (K-NN), SVM, Neural Network (NN), and Random Forest (RF) | ECG signals | 31 subjects 18 with congestive HF 13 controls | RF acc 100% |
| Choi et al. [11] (2017) | HF diagnosis Healthy vs. HF | Recurrent Neural Network (RNN) models, Logistic Regression (LR), SVM, Multilayer Perceptron (MLP), K-NN | Demographics, habits, clinical and laboratory values, ICD-9 codes, CPT codes, and medications | 3884 with HF 28.903 controls | RNN model AUC 77.70% |
| Chen et al. [19] (2017) | Congestive HF diagnosis Healthy vs. congestive HF | Deep Neural Network (DNN) | HRV measures based on the RR interval | 116 subjects 44 with congestive HF 72 controls | Acc 72.44% Sens 50.39% Spec 84.93% |
| Samuel et al. [8] (2017) | HF diagnosis Healthy vs. HF | Hybrid decision support method based on artificial neural networks and fuzzy analytic hierarchy process (Fuzzy_AHP) techniques | Demographics, symptoms, clinical and laboratory values, and electrocardiographic results | Cleveland heart disease database 297 subjects 137 with HF 160 controls | Acc 91.10% |
| Reddy et al. [13] (2018) | HFpEF identification | LR | Medications, demographics, comorbidities, and echocardiographic and ECG features | 414 subjects 267 with HFpEF 147 controls | AUC 88.60% |
| Wang et al. [18] (2019) | Congestive HF diagnosis Healthy vs. congestive HF | Combination of the Long Short-Term Memory (LSTM) network and convolution net architecture | HRV measures based on the RR interval | 156 subjects 44 with congestive HF 112 controls | Acc 99.22% |
| Acharya et al. [15] (2019) | Congestive HF diagnosis Healthy vs. congestive HF | Convolutional neural network (CNN) | ECG signals | 73 subjects 15 with congestive HF 58 controls | Acc 98.97% Spec 99.01% Sens 98.87% |
| Ali et al. [6] (2019) | HF diagnosis Healthy vs. HF | SVM | Demographics, symptoms, clinical and laboratory values, and electrocardiographic results | Cleveland heart disease database 297 subjects 137 with HF 160 controls | Acc 92.22% Sens 100.00% Spec 82.92% |
| Javeed et al. [7] (2019) | HF diagnosis Healthy vs. HF | Random Search Algorithm (RSA) for feature selection and RF for classification | Demographics, symptoms, clinical and laboratory values, and electrocardiographic results | Cleveland heart disease database 297 subjects 137 with HF 160 controls | Acc 93.33% |
| Mohan et al. [9] (2019) | HF diagnosis Healthy vs. HF | Hybrid RF | Demographics, symptoms, clinical and laboratory values, and electrocardiographic results | Cleveland heart disease database 297 subjects 137 with HF 160 controls | Acc 88.40% Sens 92.80% Spec 82.60% |
| Lal et al. [17] (2020) | Congestive HF diagnosis Healthy vs. congestive HF | SVM Gaussian, K-NN, decision tree, SVM RBF, and SVM polynomial | HRV measures | 116 subjects 44 with congestive HF 72 controls | SVM Gaussian Acc 88.79% Sens 93.06% Spec 81.82% AUC 95.00% |
| Gjoreski et al. [22] (2020) | Chronic HF diagnosis Healthy vs. chronic HF | Combination of classic ML and end-to-end Deep Learning (DL) | Heart sound characteristics | 947 subjects | Acc 92.90% Sens 82.30% Spec 96.20% |
| Potter et al. [10] (2020) | Stage B HF detection | RF | Demographics, symptoms, clinical and laboratory values, and electrocardiographic results | Cleveland Heart Disease Database 254 subjects as train set (135 with HF, 119 controls) 65 subjects as test set (27 with HF, 38 controls) | AUC 76.00% Sens 93.00% Spec 61.00% |
| Ning et al. [16] (2020) | Congestive HF diagnosis Healthy vs. congestive HF | Hybrid DL algorithm that is composed of a CNN and a recursive NN | ECG signals | 33 subjects 15 chronic HF subjects 18 controls | Acc 99.93% Sens 99.85% Spec 100% |
| Category | Description |
|---|---|
| General demographic data | Age and gender |
| Classical cardiovascular risk factors | Hypertension and diabetes mellitus |
| Personal history of cardiovascular disease | Device, myocardial infarction (MI), coronary artery disease (CAD), angina, peripheral vascular disease, any arrhythmia (Arr), paroxysmal atrial fibrillation (Afib), and stroke |
| Other diseases | Arthritis, chronic obstructive pulmonary disease, cancer, asthma, gout |
| Lifestyle/habits | smoking, and physical activity |
| Medications | Mineralocorticoid receptor antagonists (MRAs), diuretics (loop or thiazide diuretic), calcium channel blocker (CCB), statin, antiplatelet, renin angiotensin aldosterone system (RAAS), beta blocker (BB), oral anticoagulant (OAC), other lipid-lowering drugs (LipD), alpha blocker, digoxin, insulin, warfarin, nitrate, diabetes drugs, and ivabradine |
| Symptoms | Dyspnea, orthopnea, NYHA classes I–IV, and paroxysmal nocturnal dyspnea |
| Physical examination | Weight, height, body mass index (BMI), murmurs, systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), pulse, crackles, oedemas, JVP distension, and body surface area |
| Laboratory findings | BNP, Na, K, Ca, Cl, urea, creatinine, eGFR, full blood count including WBC, full blood count including Hb, platelet count, total cholesterol, HDL, LDL, triglycerides, and glucose (non-fasting) |
| Echocardiographic parameters | Interventricular septal thickness at end-diastole (IVS), posterior wall thickness at end diastole (PW), left ventricular internal dimension in diastole (LVIDd), LV mass, left ventricular mass index (LVMI), left atrial volume (average 4ch and 2ch) (LAVI), left atrial (LA) dimension (mm), peak E-value, peak A-value, early filling (E wave)/late diastolic filling (A wave) ratio (E/A), mitral annular velocity (E’), early filling (E wave)/mitral annular velocity(E/E’), Ε deceleration time, ejection fraction (EF), diastolic biventricular inner dimension, estimation of any valvular disease, right ventricular systolic pressure, and pulmonary artery systolic pressure; classification of HF phenotype into: HFrEF, HFmrEF, and HFpEF |
| Category | Description |
|---|---|
| General demographic data | Age and gender |
| Classical cardiovascular risk factors | Hypertension and diabetes mellitus |
| Personal history of cardiovascular disease | MI, CAD, angina, peripheral vascular disease, Arr, Afib, and stroke |
| Other diseases | Arthritis, chronic obstructive pulmonary disease, cancer, asthma, and gout |
| Lifestyle/habits | Smoking and physical activity |
| Symptoms | Orthopnea, Paroxysmal Nocturnal Dyspnea |
| Physical examination | Weight, height, BMI, murmurs, SBP, DBP, HR, pulse, crackles, edemas, JVP distension, and body surface area |
| Laboratory findings | BNP, Na, K, Ca, Cl, urea, creatinine, eGFR, full blood count including WBC, full blood count including Hb, platelet count, total cholesterol, HDL, LDL, triglycerides, and glucose (non-fasting) |
| Echocardiographic parameters | LVIDd, LV mass, LVMI, LAVI, left atrial dimension (mm), peak E-value, peak A-value, EA, mitral annular velocity, Ee, Ε deceleration time, EF, diastolic biventricular inner dimension, estimation of any valvular disease, right ventricular systolic pressure, and pulmonary artery systolic pressure |
| Category | Description |
|---|---|
| General demographic data | Age and gender |
| Classical cardiovascular risk factors | Hypertension |
| Personal history of cardiovascular disease | MI, CAD, and any arrhythmia (Arr) or paroxysmal atrial fibrillation (Afib) combined as Arr-Afib |
| Physical examination | BMI, SBP, DBP, and HR |
| Laboratory findings | BNP |
| Echocardiographic parameters | LVIDd, LVMI, LAVI, EA, E deceleration time, Ee, EF, and peak E-value |
| Features Type | Classifier | Accuracy % | Sensitivity % | Specificity % |
|---|---|---|---|---|
| Clinical features | LMT | 84.12 | 82.10 | 85.38 |
| Clinical features and BNP | LMT | 88.15 | 85.80 | 89.62 |
| Clinical and echocardiographic features | ROT | 90.76 | 93.21 | 89.23 |
| Echocardiographic features | ROT | 87.91 | 90.74 | 86.15 |
| All features | ROT | 91.23 | 93.83 | 89.62 |
| Feature Set | Retained Features |
|---|---|
| Clinical features | Hypertension, Arr-Afib, CAD, and SBP |
| Clinical features and BNP | Hypertension, Arr-Afib, CAD, SBP, and BNP |
| Clinical and echocardiogram features | Hypertension, Arr-Afib, CAD, SBP, EF, LAVI, LVMI, E/E’, and E deceleration time |
| Echocardiogram features | EF, LAVI, LVMI, and E deceleration time |
| All features | Hypertension, Arr-Afib, LAVI, LVMI, CAD, BNP, SBP, and EF |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plati, D.K.; Tripoliti, E.E.; Bechlioulis, A.; Rammos, A.; Dimou, I.; Lakkas, L.; Watson, C.; McDonald, K.; Ledwidge, M.; Pharithi, R.; et al. A Machine Learning Approach for Chronic Heart Failure Diagnosis. Diagnostics 2021, 11, 1863. https://doi.org/10.3390/diagnostics11101863
Plati DK, Tripoliti EE, Bechlioulis A, Rammos A, Dimou I, Lakkas L, Watson C, McDonald K, Ledwidge M, Pharithi R, et al. A Machine Learning Approach for Chronic Heart Failure Diagnosis. Diagnostics. 2021; 11(10):1863. https://doi.org/10.3390/diagnostics11101863
Chicago/Turabian StylePlati, Dafni K., Evanthia E. Tripoliti, Aris Bechlioulis, Aidonis Rammos, Iliada Dimou, Lampros Lakkas, Chris Watson, Ken McDonald, Mark Ledwidge, Rebabonye Pharithi, and et al. 2021. "A Machine Learning Approach for Chronic Heart Failure Diagnosis" Diagnostics 11, no. 10: 1863. https://doi.org/10.3390/diagnostics11101863






