Sestrin2 as a Potential Target in Hypertension
Abstract
:1. Introduction
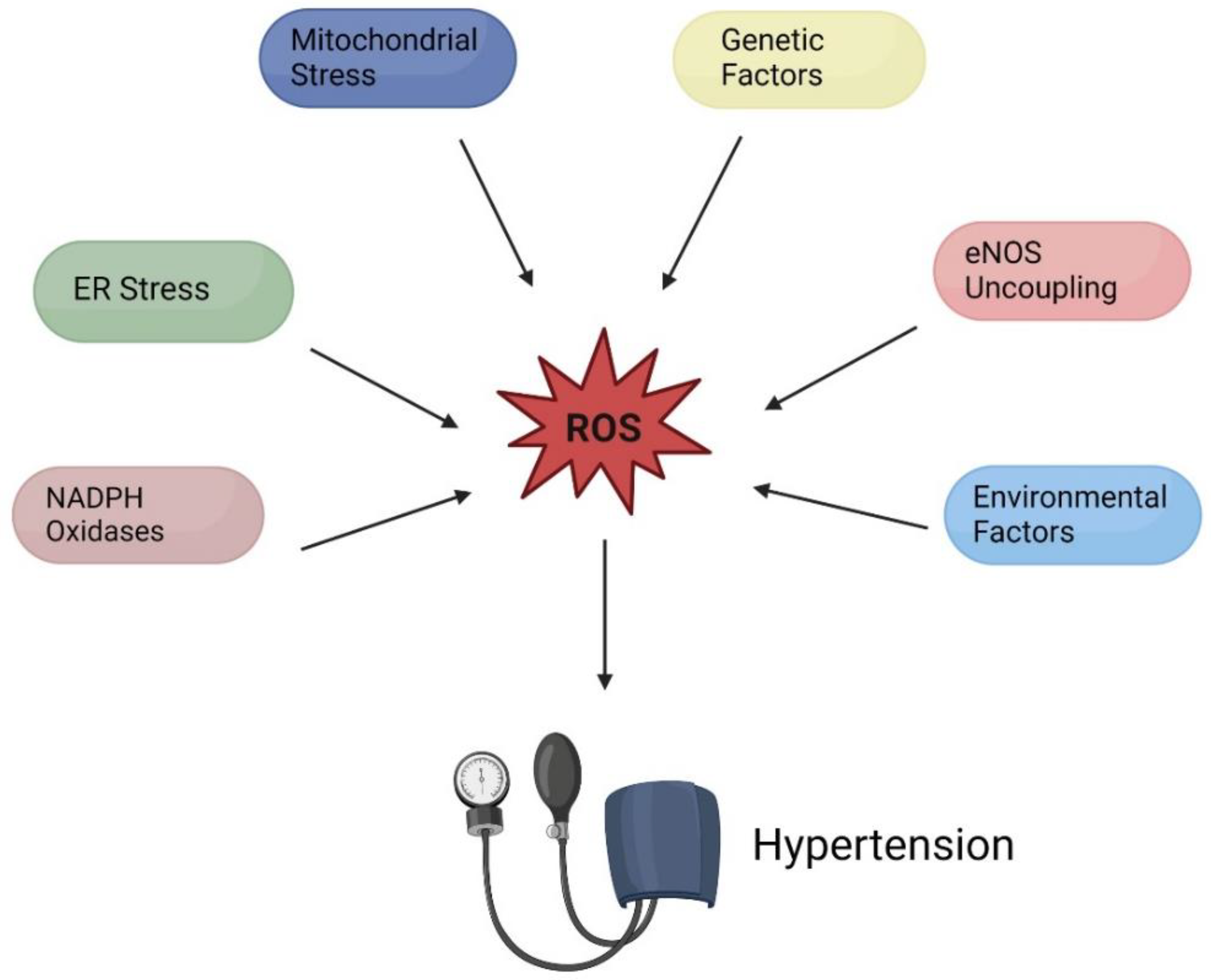
2. Hypertension Etiology
2.1. The Oxidative Stress Approaches
2.2. Mitochondrial Stress Contributing to Hypertension
2.3. Endoplasmic Reticulum (ER) Stress Contributing to Hypertension
2.4. NADPH Oxidase (NOX) Hyperactivity Contributing to Hypertension
2.5. NOS Uncoupling Contributing to Hypertension
2.6. Genetic and Environmental Factors in Hypertension
3. Sestrin2
3.1. Background and Function
3.2. Structure
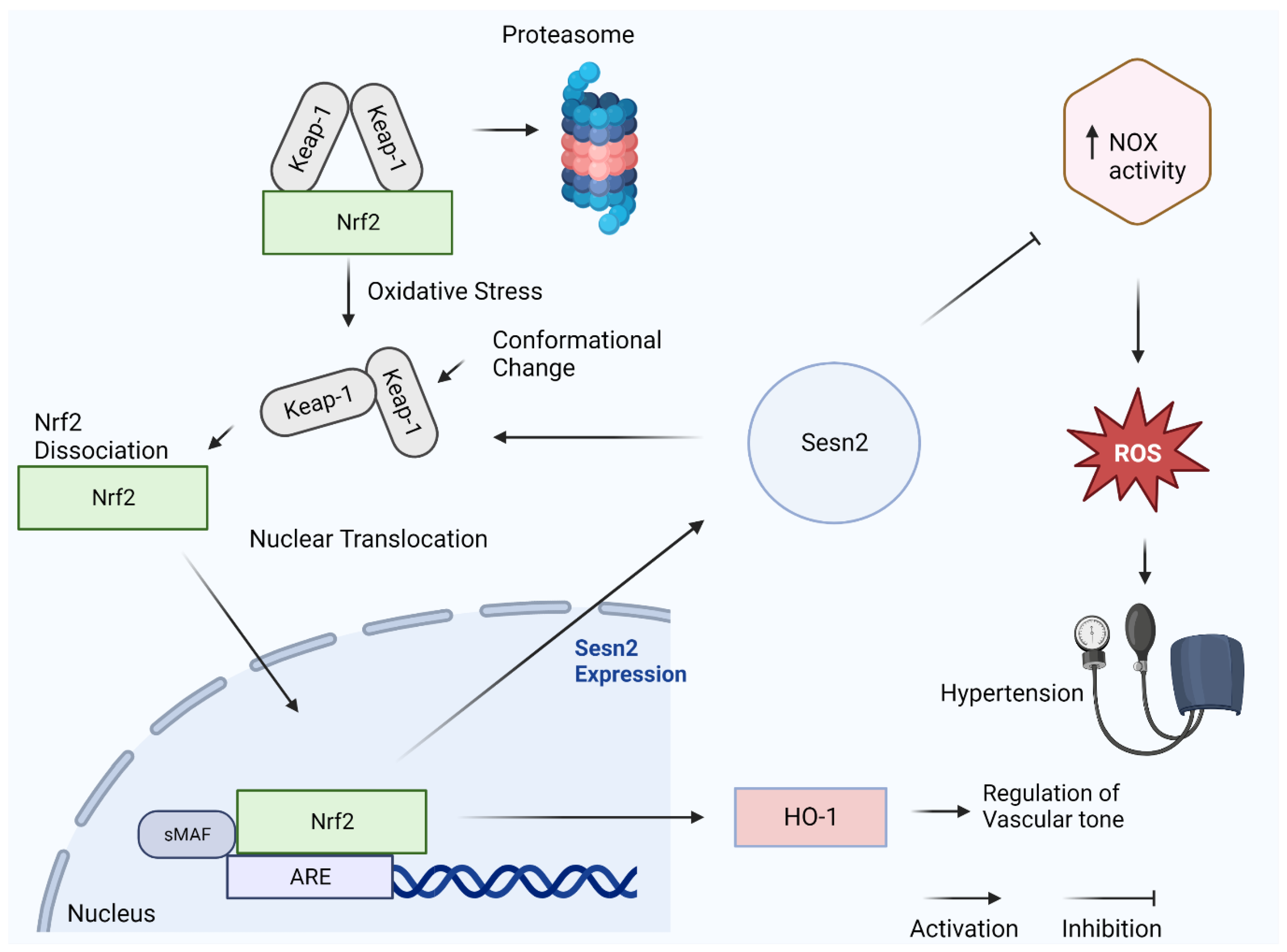
3.3. Sesn2 and Nrf2
3.4. Sesn2 and Angiotensin II
3.5. Sesn2, AMPK, and mTOR
3.6. Sesn2 Protein as a Therapeutic Modality for the Treatment of Hypertension
3.7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAR | Area at risk |
| AAV | Adeno-associated virus |
| AMPK | Adenosine monophosphate-activated protein kinase |
| ANG II | Angiotensin 2 |
| BH4 | Tetrahydrobiopterin |
| EDRF | Endothelial-derived relaxing factor |
| eNOS | Endothelial nitric oxide synthase |
| ER | Endoplasmic Reticulum |
| ET-1 | Endothelin 1 |
| mTOR | Mammalian target of rapamycin |
| NADPH | Nicotinamide adenine dinucleotide phosphate |
| NO | Nitric oxide |
| NOS | Nitric oxide synthase |
| NOX | NADPH oxidase |
| Nrf2 | Nuclear factor erythroid 2 |
| RAS | Renin–angiotensin system |
| ROS | Reactive oxygen species |
| Sesn2 | Sestrin2 |
| TNF | Tumor necrosis factor |
References
- Oparil, S.; Acelajado, M.C.; Bakris, G.L.; Berlowitz, D.R.; Cífková, R.; Dominiczak, A.F.; Grassi, G.; Jordan, J.; Poulter, N.R.; Rodgers, A.; et al. Hypertension (Primer). Nat. Rev. Dis. Prim. 2018, 4, 18014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giles, T.D.; Berk, B.C.; Black, H.R.; Cohn, J.N.; Kostis, J.B.; Izzo, J.L.; Weber, M.A. Expanding the definition and classification of hypertension. J. Clin. Hypertens. 2005, 7, 505–512. [Google Scholar] [CrossRef]
- MacLeod, K.E.; Ye, Z.; Donald, B.; Wang, G. A Literature Review of Productivity Loss Associated with Hypertension in the United States. Popul. Health Manag. 2022, 25, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Dosh, S.A. The diagnosis of essential and secondary hypertension in adults. J. Fam. Pract. 2001, 50, 707–712. [Google Scholar]
- Chiong, J.R.; Aronow, W.S.; Khan, I.A.; Nair, C.K.; Vijayaraghavan, K.; Dart, R.A.; Behrenbeck, T.R.; Geraci, S.A. Secondary hypertension: Current diagnosis and treatment. Int. J. Cardiol. 2008, 124, 6–21. [Google Scholar] [CrossRef] [PubMed]
- Griendling, K.K.; Camargo, L.L.; Rios, F.J.; Alves-Lopes, R.; Montezano, A.C.; Touyz, R.M. Oxidative Stress and Hypertension. Circ. Res. 2021, 128, 993–1020. [Google Scholar] [CrossRef] [PubMed]
- Paravicini, T.M.; Touyz, R.M. NADPH oxidases, reactive oxygen species, and hypertension: Clinical implications and therapeutic possibilities. Diabetes Care 2008, 31 (Suppl. 2), S170–S180. [Google Scholar] [CrossRef] [Green Version]
- Masi, S.; Uliana, M.; Virdis, A. Angiotensin II and vascular damage in hypertension: Role of oxidative stress and sympathetic activation. Vascul. Pharmacol. 2019, 115, 13–17. [Google Scholar] [CrossRef]
- Dikalov, S.I.; Ungvari, Z. Role of mitochondrial oxidative stress in hypertension. Am. J. Physiol. Heart Circ. Physiol. 2013, 305, H1417–H1427. [Google Scholar] [CrossRef] [Green Version]
- Widlansky, M.E.; Gutterman, D.D. Regulation of endothelial function by mitochondrial reactive oxygen species. Antioxid. Redox Signal. 2011, 15, 1517–1530. [Google Scholar] [CrossRef] [Green Version]
- Halperin, L.; Jung, J.; Michalak, M. The many functions of the endoplasmic reticulum chaperones and folding enzymes. IUBMB Life 2014, 66, 318–326. [Google Scholar] [CrossRef]
- Young, C.N. Endoplasmic reticulum stress in the pathogenesis of hypertension. Exp. Physiol. 2017, 102, 869–884. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Zhao, L.; Zhang, Z.; Lu, X. Protective Effect of Enalapril against Methionine-Enriched Diet-Induced Hypertension: Role of Endoplasmic Reticulum and Oxidative Stress. Biomed. Res. Int. 2015, 2015, 724876. [Google Scholar] [CrossRef] [Green Version]
- Konior, A.; Schramm, A.; Czesnikiewicz-Guzik, M.; Guzik, T.J.; Urner, S.; Ho, F.; Jha, J.C.; Ziegler, D.; Jandeleit-Dahm, K.; Karki, P.; et al. NADPH oxidases in vascular pathology. Antioxid. Redox Signal. 2014, 20, 2794–2814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, H.C.; Griendling, K.K. NADPH oxidase inhibitors: New antihypertensive agents? J. Cardiovasc. Pharmacol. 2007, 50, 9–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, R.C.; Loscalzo, J. Vascular Nitric Oxide: Formation and Function. J. Blood Med. 2010, 2010, 147–162. [Google Scholar]
- Bigazzi, R.; Zagato, L.; Lanzani, C.; Fontana, S.; Messaggio, E.; Carpini, S.D.; Citterio, L.; Simonini, M.; Brioni, E.; Magnaghi, C.; et al. Hypertension in High School Students: Genetic and Environmental Factors. Hypertension 2020, 75, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Kunes, J.; Zicha, J. The interaction of genetic and environmental factors in the etiology of hypertension. Physiol. Res. 2009, 58 (Suppl. 2), S33–S42. [Google Scholar] [CrossRef]
- Bruno, R.M.; Di Pilla, M.; Ancona, C.; Sørensen, M.; Gesi, M.; Taddei, S.; Munzel, T.; Virdis, A. Environmental Factors and Hypertension. Curr. Pharm. Des. 2017, 23, 3239–3246. [Google Scholar] [CrossRef] [PubMed]
- Savica, V.; Bellinghieri, G.; Kopple, J.D. The effect of nutrition on blood pressure. Annu. Rev. Nutr. 2010, 30, 365–401. [Google Scholar] [CrossRef] [Green Version]
- Juul, F.; Vaidean, G.; Parekh, N. Ultra-processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action. Adv. Nutr. 2021, 12, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Du, X.; Huang, Z.; Zheng, Y.; Quan, N. Sestrin 2 controls the cardiovascular aging process via an integrated network of signaling pathways. Ageing Res. Rev. 2020, 62, 101096. [Google Scholar] [CrossRef]
- Liu, Y.; Li, M.; Du, X.; Huang, Z.; Quan, N. Sestrin 2, a potential star of antioxidant stress in cardiovascular diseases. Free Radic. Biol. Med. 2021, 163, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Pasha, M.; Eid, A.H.; Eid, A.A.; Gorin, Y.; Munusamy, S. Sestrin2 as a Novel Biomarker and Therapeutic Target for Various Diseases. Oxidative Med. Cell. Longev. 2017, 2017, 3296294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, A.; Li, F.; Zhou, Q.; Chen, L. Sestrin2 as a potential therapeutic target for cardiovascular diseases. Pharmacol. Res. 2020, 159, 104990. [Google Scholar] [CrossRef]
- Shin, B.Y.; Jin, S.H.; Cho, I.J.; Ki, S.H. Nrf2-ARE pathway regulates induction of Sestrin-2 expression. Free Radic. Biol. Med. 2012, 53, 834–841. [Google Scholar] [CrossRef]
- Bhakkiyalakshmi, E.; Sireesh, D.; Ramkumar, K.M. Redox Sensitive Transcription via Nrf2-Keap1 in Suppression of Inflammation. Immun. Inflamm. Health Dis. 2018, 149–161. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Yet, S.-F.; Perrella, M.A. Role of Heme Oxygenase-1 in the Regulation of Blood Pressure and Cardiac Function. Exp. Biol. Med. 2003, 228, 447–453. [Google Scholar] [CrossRef]
- Fountain, J.H.; Kaur, J.; Lappin, S.L. Physiology, Renin Angiotensin System; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Touyz, R.M. Molecular and cellular mechanisms in vascular injury in hypertension: Role of angiotensin II—Editorial review. Curr. Opin. Nephrol. Hypertens. 2005, 14, 125–131. [Google Scholar] [CrossRef]
- Kumar, V.; Evans, L.C.; Kurth, T.; Yang, C.; Wollner, C.; Nasci, V.; Zheleznova, N.N.; Bukowy, J.; Dayton, A.; Cowley, A.W.C., Jr. Therapeutic Suppression of mTOR (Mammalian Target of Rapamycin) Signaling Prevents and Reverses Salt-Induced Hypertension and Kidney Injury in Dahl Salt-Sensitive Rats. Hypertension 2019, 73, 630–639. [Google Scholar] [CrossRef]
- Guimaraes, D.A.; Passos, M.A.D.; Rizzi, E.; Pinheiro, L.C.; Amaral, J.H.; Gerlach, R.F.; Castro, M.M.; Tanus-Santos, J.E. Nitrite exerts antioxidant effects, inhibits the mTOR pathway and reverses hypertension-induced cardiac hypertrophy. Free Radic. Biol. Med. 2018, 120, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Tai, P.W.L.; Gao, G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat. Rev. Drug Discov. 2019, 18, 358–378. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Didik, S.; Wang, H.; James, A.S.; Slotabec, L.; Li, J. Sestrin2 as a Potential Target in Hypertension. Diagnostics 2023, 13, 2374. https://doi.org/10.3390/diagnostics13142374
Didik S, Wang H, James AS, Slotabec L, Li J. Sestrin2 as a Potential Target in Hypertension. Diagnostics. 2023; 13(14):2374. https://doi.org/10.3390/diagnostics13142374
Chicago/Turabian StyleDidik, Steven, Hao Wang, Adewale Segun James, Lily Slotabec, and Ji Li. 2023. "Sestrin2 as a Potential Target in Hypertension" Diagnostics 13, no. 14: 2374. https://doi.org/10.3390/diagnostics13142374





