Point-of-Care Diagnostics for Improving Maternal Health in South Africa
Abstract
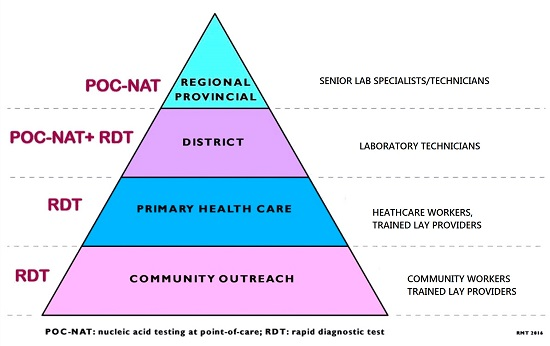
:1. Introduction
2. Recommended of Diagnostics for Antenatal Patients at in South Africa
3. Current and Emerging POC Diagnostics for Maternal Health
3.1. Pregnancy Test
3.2. Blood Glucose Test
3.3. HIV Testing
3.4. CD4 Cell Count Test for HIV Monitoring
3.5. HIV Viral Load Test
3.6. Syphilis Testing
3.7. Chlamydia, Gonorrhoea
3.8. Hepatitis B Virus
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Maternal Health. Available online: http://www.who.int/topics/maternal_health/en/ (accesssed on 29 July 2015).
- Saving Mothers 2011–2013: Sixth report on the Confidential Enquiries into Maternal Deaths in South Africa. Available online: http://www.kznhealth.gov.za/mcwh/Maternal/Saving-Mothers-2011-2013-short-report.pdf (accessed on 31 July 2016).
- Barron, P.; Pillay, Y.; Doherty, T.; Sherman, G.; Jackson, D.; Bhardwaj, S.; Robinson, P.; Goga, A. Eliminating mother-to-child HIV transmission in South Africa. Bull. World Health Organ. 2013, 91, 70–74. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. 90–90–90: An Ambitious Treatment Target to Help End the Aids Epidemic; UNAIDS: Geneva, Switzerland, 2014. [Google Scholar]
- Griggs, D.; Stafford-Smith, M.; Gaffney, O.; Rockström, J.; Öhman, M.C.; Shyamsundar, P.; Steffen, W.; Glaser, G.; Kanie, N.; Noble, I. Policy: Sustainable development goals for people and planet. Nature 2013, 495, 305–307. [Google Scholar] [CrossRef] [PubMed]
- International Amnesty. South Africa: Struggle for Maternal Health: Barriers to Antenatal Care in South Africa; International Amnesty: London, UK, 2014. [Google Scholar]
- Strasser, R. Rural health around the world: Challenges and solutions. Fam. Pract. 2003, 20, 457–463. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. UNAIDS and partners launch initiative to improve HIV diagnostics. Available online: http://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2014/july/20140723dai/ (accessed on 30 July 2016).
- Cheung, G.; Sahai, A.; Billia, M.; Dasgupta, P.; Khan, M.S. Recent advances in the diagnosis and treatment of bladder cancer. BMC Med. 2013, 11. [Google Scholar] [CrossRef] [PubMed]
- Warren, A.D.; Kwong, G.A.; Wood, D.K.; Lin, K.Y.; Bhatia, S.N. Bhatiaa Sangeeta N. Point-of-care diagnostics for noncommunicable diseases using synthetic urinary biomarkers and paper microfluidics. Proc. Natl. Acad. Sci. USA 2014, 10, 3671–3676. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Isikman, S.O.; Mudanyali, O.; Greenbaum, A.; Ozcan, A. Optical imaging techniques for point-of-care diagnostics. Lab Chip 2013, 13, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Drain, P.K.; Garrett, N.J. The arrival of a true point-of-care molecular assay—Ready for global implementation? Lancet Glob. Health 2015, 3, e663–e664. [Google Scholar] [CrossRef]
- Dinnes, J.; Deeks, J.; Kunst, H.; Gibson, A.; Cummins, E.; Waugh, N.; Drobniewski, F.; Lalvani, A. A systematic review of rapid diagnostic tests for the detection of tuberculosis infection. Health Technol. Assess. 2007, 11, 1–196. [Google Scholar] [CrossRef] [PubMed]
- Drain, P.K.; Hyle, E.P.; Noubary, F.; Freedberg, K.A.; Wilson, D.; Bishai, W.R.; Rodriguez, W.; Bassett, I.V. Diagnostic point-of-care tests in resource-limited settings. Lancet Infect. Dis. 2014, 14, 239–249. [Google Scholar] [CrossRef]
- Pai, N.P.; Vadnais, C.; Denkinger, C.; Engel, N.; Pai, M. Point-of-care testing for infectious diseases: Diversity, complexity, and barriers in low- and middle-income countries. PLoS Med. 2012, 9, e1001306. [Google Scholar] [CrossRef] [PubMed]
- Nichols, J.H. Point of care testing. Clin. Lab. Med. 2007, 27, 893–908. [Google Scholar] [CrossRef] [PubMed]
- Option B and B+: Key Considerations for Countries to Implement and Equity-Focused Approach. 2012. Available online: http://www.unicef.org/aids/files/hiv_Key_considerations_options_B.pdf (accessed on 31 July 2016).
- WHO. Consolidated Guidelines on HIV Testing Services; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Kharsany, A.B.; Frohlich, J.A.; Yende-Zuma, N.; Mahlase, G.; Samsunder, N.; Dellar, R.C.; Zuma-Mkhonza, M.; Karim, S.S.A.; Karim, Q.A. Trends in HIV prevalence in pregnant women in rural South Africa. J. Acquir. Immune Defic. Syndr. 2015, 70, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Lincetto, O.; Mothebesoane-Anoh, S.; Gomez, P.; Munjanja, S. Antenatal Care. Opportunities for Africa’s Newborns: Practical Data, Policy and Programmatic Support for Newborn Care in Africa; World Health Organiation: Geneva, Switzerland, 2010. [Google Scholar]
- Butsashvili, M.; Preble, E.; Kamkamidze, G.; Robinson, J.; Chubinishvili, O.; Sukhiashvili, R. Uptake of an HIV voluntary counseling and testing program for pregnant women in Georgia. AIDS Care 2008, 20, 1125–1127. [Google Scholar] [CrossRef] [PubMed]
- Dennis, R.L.; Negron, T.J.; Lindsay, M.; Nesheim, S.R.; Lee, F.K.; Jamieson, D.J. Rapid human immunodeficiency virus testing in labor and delivery: A comparison of implementation models between 2 hospitals. J. Perinat. Neonatal Nurs. 2007, 21, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Faal, M.; Naidoo, N.; Glencross, D.K.; Venter, W.D.; Osih, R. Providing immediate CD4 count results at HIV testing improves ART initiation. JAIDS J. Acquir. Immune Defic. Syndr. 2011, 58, e54–e59. [Google Scholar] [CrossRef] [PubMed]
- Garcia, P.J.; Carcamo, C.P.; Chiappe, M.; Valderrama, M.; La Rosa, S.; Holmes, K.K.; Mabey, D.C.; Peeling, R.W. Rapid syphilis tests as catalysts for health systems strengthening: A case study from Peru. PLoS ONE 2013, 8, e66905. [Google Scholar] [CrossRef] [PubMed]
- WHO; UNICEF. Trends in Maternal Mortality: 1990 to 2013: Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division: Executive Summary; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Peeling, R.W.; Mabey, D.; Herring, A.; Hook, E.W. Why do we need quality-assured diagnostic tests for sexually transmitted infections? Nat. Rev. Microbiol. 2006, 4, 909–921. [Google Scholar] [CrossRef] [PubMed]
- WHO. Rapid HIV Tests: Guidelines for Use in HIV Testing and Counselling Services in Resource-Constrained Settings; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Mast, E.E.; Margolis, H.S.; Fiore, A.E.; Brink, E.W.; Goldstein, S.T.; Wang, S.A.; Moyer, L.A.; Bell, B.P.; Alter, M.J. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States. MMWR 2005, 54, 1–32. [Google Scholar] [PubMed]
- Routine Tests During Pregnancy. 2016. Available online: http://www.acog.org/~/media/For%20Patients/faq133.pdf (accessed on 10 May 2016).
- Pillay-van Wyk, V.; Msemburi, W.; Laubscher, R.; Dorrington, RE.; Groenewald, P.; Matzopoulos, R.; Prinsloo, M.; Nojilana, B.; Nannan, N.; Gwebushe, N.; et al. Second national burden of disease study South Africa: National and subnational mortality trends, 1997–2009. Lancet 2013, 381, S113. [Google Scholar]
- Olasagasti, F.; de Gordoa, J.C.R. Miniaturized technology for protein and nucleic acid point-of-care testing. Transl. Res. 2012, 160, 332–345. [Google Scholar] [CrossRef] [PubMed]
- Dominique, J.K.; Ortiz-Osorno, A.A.; Fitzgibbon, J.; Gnanashanmugam, D.; Gilpin, C.; Tucker, T.; Peel, S.; Peter, T.; Kim, P.; Smith, S. Implementation of HIV and tuberculosis diagnostics: The importance of context. Clin. Infect. Dis. 2015, 61, S119–S125. [Google Scholar] [CrossRef] [PubMed]
- St John, A.; Price, C.P. Existing and emerging technologies for point-of-care testing. Clin. Biochem. Rev. 2014, 35, 155–167. [Google Scholar] [PubMed]
- Farrance, I. Reviw: Policies, Procedures and Guidelines for Point of Care Testing; Australian Government Department of Health and Ageing: Phillip, Australia, 2012.
- Johnson, L.F.; Davies, M.A.; Moultrie, H.; Sherman, G.G.; Bland, R.M.; Rehle, T.M.; Dorrington, R.E.; Newell, M.L. The effect of early initiation of antiretroviral treatment in infants on pediatric AIDS mortality in South Africa: A model-based analysis. Pediatr. Infect. Dis. J. 2012, 31, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Min, J.; Buckel, C.; Secura, G.M.; Peipert, J.F.; Madden, T. Performance of a checklist to exclude pregnancy at the time of contraceptive initiation among women with a negative urine pregnancy test. Contraception 2015, 91, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Division of Reproductive Health NC. US selected practice recommendations for contraceptive use, 2013: Adapted from the World Health Organization selected practice recommendations for contraceptive use. MMWR 2013, 62, 1. [Google Scholar]
- Comfort, A.B.; Chankova, S.; Juras, R.; Hsi, C.N.; Peterson, L.A.; Hathi, P. Providing free pregnancy test kits to community health workers increases distribution of contraceptives: Results from an impact evaluation in Madagascar. Contraception 2016, 93, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Bastian, L.A.; Nanda, K.; Hasselblad, V.; Simel, D.L. Diagnostic efficiency of home pregnancy test kits: A meta-analysis. Arch. Fam. Med. 1998, 7, 465–469. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Expert Committee on Diabetes Mellitus, Second Report; World Health Organization: Geneva, Switzerland, 1980. [Google Scholar]
- Wendland, E.M.; Torloni, M.R.; Falavigna, M.; Trujillo, J.; Dode, M.A.; Campos, M.A.; Duncan, B.B.; Schmidt, M.I. Gestational diabetes and pregnancy outcomes-a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childbirth 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Boney, C.M.; Verma, A.; Tucker, R.; Vohr, B.R. Metabolic syndrome in childhood: Association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 2005, 115, e290–e296. [Google Scholar] [CrossRef] [PubMed]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global multimorbidity patterns: A cross-sectional, population-based, multi-country study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 71, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Mackillop, L.H.; Bartlett, K.; Birks, J.; Farmer, A.J.; Gibson, O.J.; Kevat, D.A.; Kenworthy, Y.; Levy, J.C.; Loerup, L.; Tarassenko, L.; et al. Trial protocol to compare the efficacy of a smartphone-based blood glucose management system with standard clinic care in the gestational diabetic population. BMJ Open 2016, 6, e009702. [Google Scholar] [CrossRef] [PubMed]
- Mackillop, L.; Loerup, L.; Bartlett, K.; Farmer, A.; Gibson, O.J.; Hirst, J.E.; Kenworthy, Y.; Kevat, D.A.; Levy, J.C.; Tarassenko, L. Development of a real-time smartphone solution for the management of women with or at high risk of gestational diabetes. J. Diabetes Sci. Technol. 2014, 8, 1105–1114. [Google Scholar] [CrossRef] [PubMed]
- Stevens, W.S.; Marshall, T.M. Challenges in implenting HIV load testing in South Africa. J. Infect. Dis. 2010, 201, S78–S84. [Google Scholar] [CrossRef] [PubMed]
- National Strategic Plan on HIV, STIs and TB 2012–2016; Department of Health: Pretoria, South Africa, 2012.
- Heller, T.; Kunthea, S.; Bunthoeun, E.; Sok, K.; Seuth, C.; Killam, W.P.; Sovanna, T.; Sathiarany, V.; Kanal, K. Point-of-care HIV testing at antenatal care and maternity sites: Experience in Battambang Province, Cambodia. Int. J. STD AIDS 2011, 22, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Kissin, D.M.; Akatova, N.; Rakhmanova, A.G.; Vinogradova, E.N.; Voronin, E.E.; Jamieson, D.J.; Glynn, M.K.; Yakovlev, A.; Robinson, J.; Miller, W.C.; et al. Rapid HIV testing and prevention of perinatal HIV transmission in high-risk maternity hospitals in St. Petersburg, Russia. Am. J. Obstet. Gynecol. 2008, 198, 183.e1–183.e17. [Google Scholar] [CrossRef] [PubMed]
- Kizito, D.; Woodburn, P.W.; Kesande, B.; Ameke, C.; Nabulime, J.; Muwanga, M.; Grosskurth, H.; Elliott, A.M. Uptake of HIV and syphilis testing of pregnant women and their male partners in a programme for prevention of mother-to-child HIV transmission in Uganda. Trop. Med. Int. Health 2008, 13, 680–682. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, S.A.; Lambert, J.S.; Albuquerque, A.L.; Rodrigues, R.; Reis, S.; Bornia, R.; Dias, M.; Barbosa, R.; Sztanjbock, D.; Santos, A.L.; et al. Assessment of a rapid HIV test strategy during labor: A pilot study from Rio de Janeiro, Brazil. J. Hum. Virol. 2000, 4, 278–282. [Google Scholar]
- Smith, A.; Sabido, M.; Camey, E.; Batres, A.; Casabona, J. Lessons learned from integrating simultaneous triple point-of-care screening for syphilis, hepatitis B, and HIV in prenatal services through rural outreach teams in Guatemala. Int. J. Gynaecol. Obstet. 2015, 130, S70–S72. [Google Scholar] [CrossRef] [PubMed]
- Aluisio, A.; Richardson, B.A.; Bosire, R.; John-Stewart, G.; Mbori-Ngacha, D.; Farquhar, C. Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV free survival. J. Acquir. Immune Defic. Syndr. 2011, 56, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Msuya, S.; Mbizvo, E.; Hussain, A.; Uriyo, J.; Sam, N.; Stray-Pedersen, B. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: Implications for preventive programs. AIDS Care 2008, 20, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Estem, K.S.; Catania, J.; Klausner, J.D. HIV Self-Testing: A review of current implementation and fidelity. Curr. HIV/AIDS Rep. 2016, 13, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Peck, R.B.; Lim, J.M.; van Rooyen, H.; Mukoma, W.; Chepuka, L.; Bansil, P.; Knight, L.C.; Muturi, N.; Chirwa, E.; Lee, A.M.; et al. What should the ideal HIV self-test look like? A usability study of test prototypes in unsupervised HIV self-testing in Kenya, Malawi, and South Africa. AIDS Behav. 2014, 18, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Pai, N.P.; Balram, B.; Shivkumar, S.; Martinez-Cajas, J.L.; Claessens, C.; Lambert, G.; Peeling, R.W.; Joseph, L. Head-to-head comparison of accuracy of a rapid point-of-care HIV test with oral versus whole-blood specimens: A systematic review and meta-analysis. Lancet Infect. Dis. 2012, 12, 373–380. [Google Scholar] [CrossRef]
- Pavie, J.; Rachline, A.; Loze, B.; Niedbalski, L.; Delaugerre, C.; Laforgerie, E.; Plantier, J.C.; Rozenbaum, W.; Chevret, S.; Molina, J.M.; et al. Sensitivity of five rapid HIV tests on oral fluid or finger-stick whole blood: A real-time comparison in a healthcare setting. PLoS ONE 2010, 5, e11581. [Google Scholar] [CrossRef] [PubMed]
- WHOC DEFINITIONS. HIV/AIDS Programme; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults. 2014. Available online: http://www.kznhealth.gov.za/family/HIV-Guidelines-Jan2015.pdf (accessed on 31 July 2016).
- Ciaranello, A.L.; Myer, L.; Kelly, K.; Christensen, S.; Daskilewicz, K.; Doherty, K.; Bekker, L.G.; Hou, T.; Wood, R.; Francke, J.A.; et al. Point-of-care CD4 testing to inform selection of antiretroviral medications in south african antenatal clinics: A cost-effectiveness analysis. PLoS ONE 2015, 10, e0117751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manasa, J.; Danaviah, S.; Lessells, R.; Elshareef, M.; Tanser, F.; Wilkinson, E.; Pillay, S.; Mthiyane, H.; Mwambi, H.; Pillay, D.; et al. Increasing HIV-1 drug resistance between 2010 and 2012 in adults participating in population-based HIV surveillance in rural KwaZulu-Natal, South Africa. AIDS Res. Hum. Retrovir. 2016, 32, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Panpradist, N.; Beck, I.A.; Chung, M.H.; Kiarie, J.N.; Frenkel, L.M.; Lutz, B.R. Simplified paper format for detecting HIV drug resistance in clinical specimens by oligonucleotide ligation. PLoS ONE 2016, 11, e0145962. [Google Scholar] [CrossRef] [PubMed]
- Jani, I.V.; Sitoe, N.E.; Alfai, E.R.; Chongo, P.L.; Quevedo, J.I.; Rocha, B.M.; Lehe, J.D.; Peter, T.F. Effect of point-of-care CD4 cell count tests on retention of patients and rates of antiretroviral therapy initiation in primary health clinics: An observational cohort study. Lancet 2011, 378, 1572–1579. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.E.; Campbell, J.; Westerman, L.; Kestens, L.; Vojnov, L.; Kohastsu, L.; Nkengasong, J.; Peter, T.; Stevens, W. A meta-analysis of the performance of the Pima TM CD4 for point of care testing. BMC Med. 2015, 13. [Google Scholar] [CrossRef] [PubMed]
- Aliyu, M.H.; Blevins, M.; Audet, C.; Shepherd, B.E.; Hassan, A.; Onwujekwe, O.; Gebi, U.I.; Kalish, M.; Lindegren, M.L.; Vermund, S.H.; et al. Optimizing PMTCT service delivery in rural North-Central Nigeria: Protocol and design for a cluster randomized study. Contemp. Clin. Trials 2013, 36, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Glencross, D.K.; Coetzee, L.M.; Faal, M.; Masango, M.; Stevens, W.S.; Venter, W.F.; Osih, R. Performance evaluation of the Pima™ point-of-care CD4 analyser using capillary blood sampling in field tests in South Africa. J. Int. AIDS Soc. 2012, 15. [Google Scholar] [CrossRef] [PubMed]
- Peter, T.; Badrichani, A.; Wu, E.; Freeman, R.; Ncube, B.; Ariki, F.; Daily, J.; Shimada, Y.; Murtagh, M. Challenges in implementing CD4 testing in resource-limited settings. Cytom. B Clin. Cytom. 2008, 74, S123–S130. [Google Scholar] [CrossRef] [PubMed]
- Library TWRH. Available online: http://wwwwhoint/mediacentre/factsheets/fs348/en/ (accessed on 11 September 2014).
- De Deus, N.; Moraleda, C.; Serna-Bolea, C.; Renom, M.; Menendez, C.; Naniche, D. Impact of elevated maternal HIV viral load at delivery on T-cell populations in HIV exposed uninfected infants in Mozambique. BMC Infect. Dis. 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Solutions, C. Xpert® HIV-1 Viral Load. Available online: http://www.cepheid.com/en/cepheid-solutions-uk/clinical-ivd-tests/virology/xpert-hiv-1-viral-load (accessed on 16 August 2016).
- Garrett, N.J.; Drain, P.K.; Werner, L.; Samsunder, N.; Karim, S.S.A. Diagnostic accuracy of the point-of-care Xpert HIV-1 viral load assay in a South African HIV clinic. J. Acquir. Immune Defic. Syndr. 2016, 72, e45–e48. [Google Scholar] [CrossRef] [PubMed]
- WHO. Standards for Maternal and Neonatal Care; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Mullick, S.; Beksinksa, M.; Msomi, S. Treatment for syphilis in antenatal care: Compliance with the three dose standard treatment regimen. Sex. Transm. Infect. 2005, 81, 220–222. [Google Scholar] [CrossRef] [PubMed]
- WHO; HIV/AIDS JUNPo; UNICEF. Global HIV/AIDS Response: Epidemic Update and Health Sector Progress Towards Universal Access: Progress Report 2011; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Sabidó, M.; Benzaken, A.S.; de Andrade Rodrigues, E.J.; Mayaud, P. Rapid point-of-care diagnostic test for syphilis in high-risk populations, Manaus, Brazil. Emerg. Infect. Dis. 2009, 15, 647–649. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.R.; Esfandiari, J.; Kumar, S.; Ashton, M.; Kikkert, S.E.; Park, M.M.; Ballard, R.C. Novel point-of-care test for simultaneous detection of nontreponemal and treponemal antibodies in patients with syphilis. J. Clin. Microbiol. 2010, 48, 4615–4619. [Google Scholar] [CrossRef] [PubMed]
- Omoding, D.; Katawera, V.; Siedner, M.; Boum, Y. Evaluation of the SD Bioline HIV/Syphilis Duo assay at a rural health center in Southwestern Uganda. BMC Res. Notes 2014, 7, 746. [Google Scholar] [CrossRef] [PubMed]
- Ghope, P.; Sonkar, S.C.; Wasnik, K.; Mittal, P.; Saluja, D. Prevalence of Chlamydia trachomatis, Neisseria gonorrhoeae and Trichomonas vaginalis infection in pregnant adolescent women and its association with pregnancy outcomes. BMC Infect. Dis. 2014, 14, E33. [Google Scholar] [CrossRef]
- Adachi, K.; Klausner, J.D.; Xu, J.; Ank, B.; Bristow, C.C.; Morgado, M.G.; Watts, D.H.; Weir, F.; Persing, D.; Mofenson, L.M.; et al. Chlamydia trachomatis and Neisseria gonorrhoeae in HIV-infected Pregnant women and adverse infant outcomes. Pediatr. Infect. Dis. J. 2016, 35, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Gaydos, C.A. Review of use of a new rapid real-time PCR, the Cepheid GeneXpert®(Xpert) CT/NG assay, for Chlamydia trachomatis and Neisseria gonorrhoeae: Results for patients while in a clinical setting. Expert Rev. Mol. Diagn. 2014, 14, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Gaydos, C.A.; van der Pol, B.; Jett-Goheen, M.; Barnes, M.; Quinn, N.; Clark, C.; Daniel, G.E.; Dixon, P.B.; Hook, E.W. Performance of the Cepheid CT/NG Xpert rapid PCR test for the detection of Chlamydia trachomatis and Neisseria gonorrhoeae. J. Clin. Microbiol. 2013. [Google Scholar] [CrossRef] [PubMed]
- Natoli, L.; Maher, L.; Shephard, M.; Hengel, B.; Tangey, A.; Badman, S.G.; Ward, J.; Guy, R.J. Point-of-care testing for chlamydia and gonorrhoea: Implications for clinical practice. PLoS ONE 2014, 9, e100518. [Google Scholar] [CrossRef] [PubMed]
- Whiley, D.M.; Goire, N.; Lahra, M.M.; Donovan, B.; Limnios, A.E.; Nissen, M.D.; Sloots, T.P. The ticking time bomb: Escalating antibiotic resistance in Neisseria gonorrhoeae is a public health disaster in waiting. J. Antimicrob. Chemother. 2012, 67, 2059–2061. [Google Scholar] [CrossRef] [PubMed]
- Ott, J.J.; Stevens, G.A.; Wiersma, S.T. The risk of perinatal Hepatitis B virus transmission: Hepatitis B e antigen (HBeAg) prevalence estimates for all world regions. BMC Infect. Dis. 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Thio, C.L.; Seaberg, E.C.; Skolasky, R.; Phair, J.; Visscher, B.; Muñoz, A.; Thomas, D.L. HIV-1, Hepatitis B virus, and risk of liver-related mortality in the Multicenter Cohort Study (MACS). Lancet 2002, 360, 1921–1926. [Google Scholar] [CrossRef]
- Njai, H.F.; Shimakawa, Y.; Sanneh, B.; Ferguson, L.; Ndow, G.; Mendy, M.; Sow, A.; Lo, G.; Toure-Kane, C.; Tanaka, J.; et al. Validation of rapid point-of-care (POC) tests for detection of hepatitis B surface antigen in field and laboratory settings in the Gambia, Western Africa. J. Clin. Microbiol. 2015, 53, 1156–1163. [Google Scholar] [CrossRef] [PubMed]
- Toliman, P.; Badman, S.; Gabuzzi, J.; Silim, S.; Forereme, L.; Kumbia, A.; Kombuk, B.; Kombati, Z.; Allan, J.; Munnull, G.; et al. Field evaluation of the Xpert® HPV Point of Care Test for the detection of human papillomavirus infection using self-collected vaginal and clinician-collected cervical specimens. J. Clin. Microbiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Kirmse, B.; Baumgart, S.; Rakhmanina, N. Metabolic and mitochondrial effects of antiretroviral drug exposure in pregnancy and postpartum: Implications for fetal and future health. Semin. Fetal Neonatal Med. 2013, 18, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Chang, I.; Lee, J.C.; Kim, D.K.; Noh, S.; Ahn, H.; Cho, J.H.; Kwak, Y.H.; Kim, S.; Kim, H.C. Smartphone-based urine reagent strip test in the emergency department. Telemed. E-Health 2016, 22, 534–540. [Google Scholar] [CrossRef] [PubMed]
- WHO. Short, Medium and Long Term Product Development Priorities in HIV-Related Diagnostics; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Banoo, S.; Bell, D.; Bossuyt, P.; Herring, A.; Mabey, D.; Poole, F.; Smith, P.G.; Sriram, N.; Wongsrichanalai, C.; Linke, R.; et al. Evaluation of diagnostic tests for infectious diseases: General principles. Nat. Rev. Microbiol. 2008, 8, S16–S28. [Google Scholar] [CrossRef] [PubMed]
- Kettler, H.; White, K.; Hawkes, S. Mapping the Landscape of Diagnostics for Sexually Transmitted Infections; WHO: Geneva, Switzerland, 2004. [Google Scholar]



| Criteria | Characteristic |
|---|---|
| Affordable | Purchasable price for settings comprised of population at risk of infection |
| Sensitive | Results contain minimal false negatives (99%) |
| Specific | Results contain minimal false positives (99%) |
| User-friendly | Required minimal steps to carry test |
| Rapid and robust | Short turnaround time and no need for refrigerated storage |
| Equipment free | No need for no complex equipment |
| Delivered | Made accessible to end users |
| Routine Tests | |||
| South Africa | USA | ||
| Test | Communicable (Yes/No) | Test | Communicable (Yes/No) |
| Pregnancy test | No | Pregnancy test | No |
| Syphilis serology | Yes | Blood type and Rh factor | No |
| Rhesus (D) blood group | No | Anemia | No |
| Hemoglobin (Hb) level | No | Hepatitis B and C | Yes |
| HIV serology | Yes | Syphilis | Yes |
| Urine protein | No | HIV serology | Yes |
| Urine glucose | No | Chlamydia | Yes |
| Chicken pox | Yes | ||
| Rubella | Yes | ||
| Gestational diabetes | Yes | ||
| Toxoplasmosis | Yes | ||
| Ultrasound scan | No | ||
| Group B Streptococci | Yes | ||
| TOTAL | 2 | 9 | |
| Non-Routine Tests | |||
| South Africa | USA | ||
| Test | Communicable (Yes/No) | Test | Communicable (Yes/No) |
| ABO blood group | No | Down’s syndrome screening | No |
| Down’s syndrome screening | No | Viral load | Yes |
| Rubella serology (German measles) | Yes | CD4 count | No |
| Blood glucose screening | No | TB | Yes |
| CD4 count | No | ||
| TB | Yes | ||
| Creatinine | No | ||
| HIV Viral load | No | ||
| Ultrasound scan | No | ||
| Urine culture | Yes | ||
| Cervical (Papanicolaou) smear | Yes | ||
| TOTAL | 4 | 2 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mashamba-Thompson, T.P.; Sartorius, B.; Drain, P.K. Point-of-Care Diagnostics for Improving Maternal Health in South Africa. Diagnostics 2016, 6, 31. https://doi.org/10.3390/diagnostics6030031
Mashamba-Thompson TP, Sartorius B, Drain PK. Point-of-Care Diagnostics for Improving Maternal Health in South Africa. Diagnostics. 2016; 6(3):31. https://doi.org/10.3390/diagnostics6030031
Chicago/Turabian StyleMashamba-Thompson, Tivani P., Benn Sartorius, and Paul K. Drain. 2016. "Point-of-Care Diagnostics for Improving Maternal Health in South Africa" Diagnostics 6, no. 3: 31. https://doi.org/10.3390/diagnostics6030031