Evaluation of microRNA Expression Features in Patients with Various Types of Arterial Damage: Thoracic Aortic Aneurysm and Coronary Atherosclerosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of the Study
2.2. Inclusion Criteria
- A written informed consent of the patient to participate in the study.
- Age 18–80;
- Availability of blood plasma samples suitable for analysis from the first and second cohorts of patients.
2.3. Exclusion Criteria
- Any previous heart surgery or coronary interventions (only for first cohort);
- Severe heart failure (III-IV classes according to the classification of the New York Heart Association NYHA);
- History of myocardial infarction (only for first cohort);
- Body mass index 35 or more;
- The presence of any other severe pathology at the time of the study (including active cancer, impaired liver and kidney function, systemic diseases, inflammatory processes).
- Refusal of the patient from participation in the study;
- Psychiatric disorders, including claustrophobia.
2.4. Study Duration
2.5. Description of the Intervention
2.6. Statistical Data Analysis Methods
3. Results
3.1. Study Participants
3.2. Associations of microRNA Levels with Vascular Damage
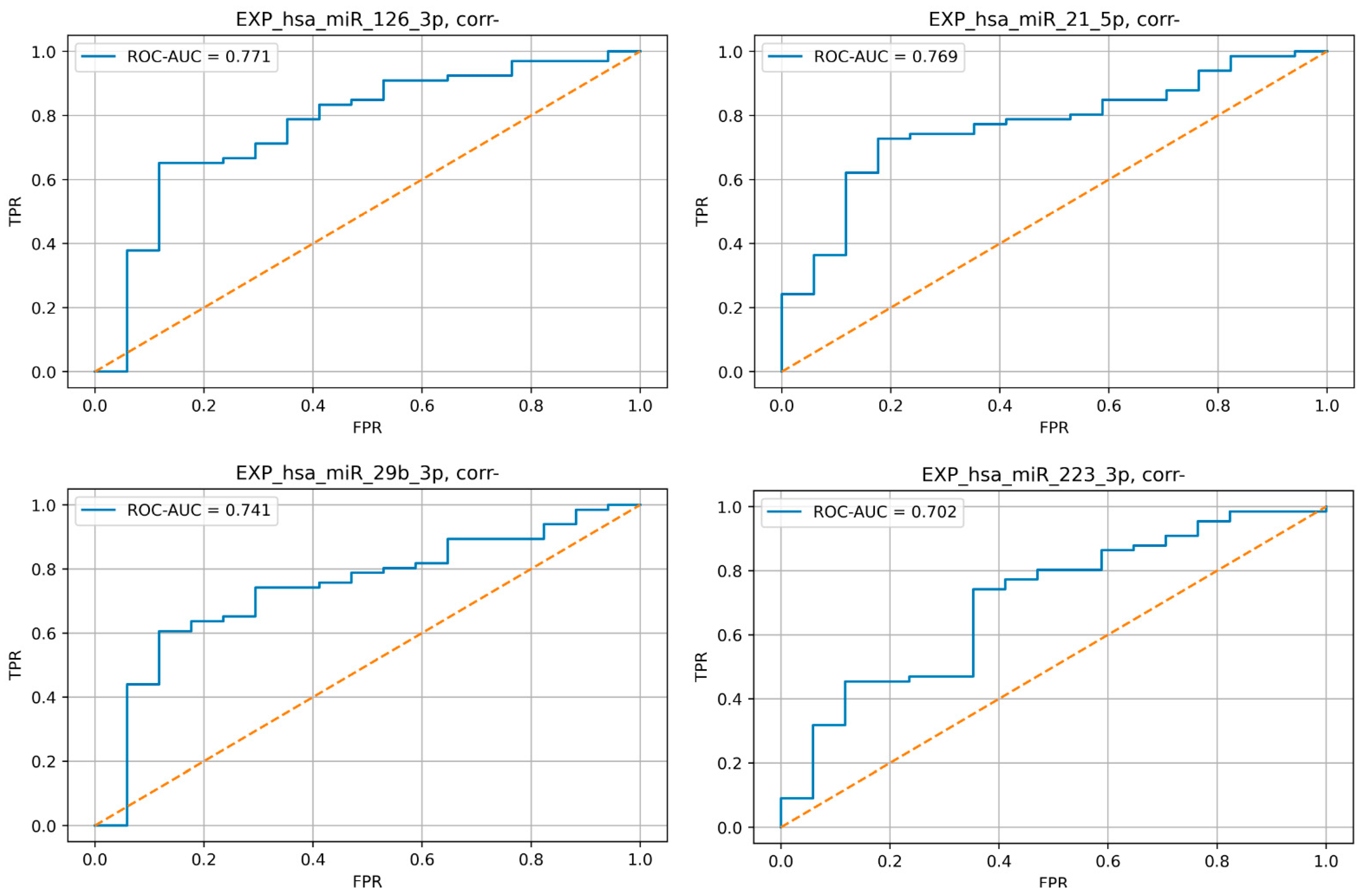
3.3. Evaluation of microRNA Expression Profiles in Patients with and without TAA
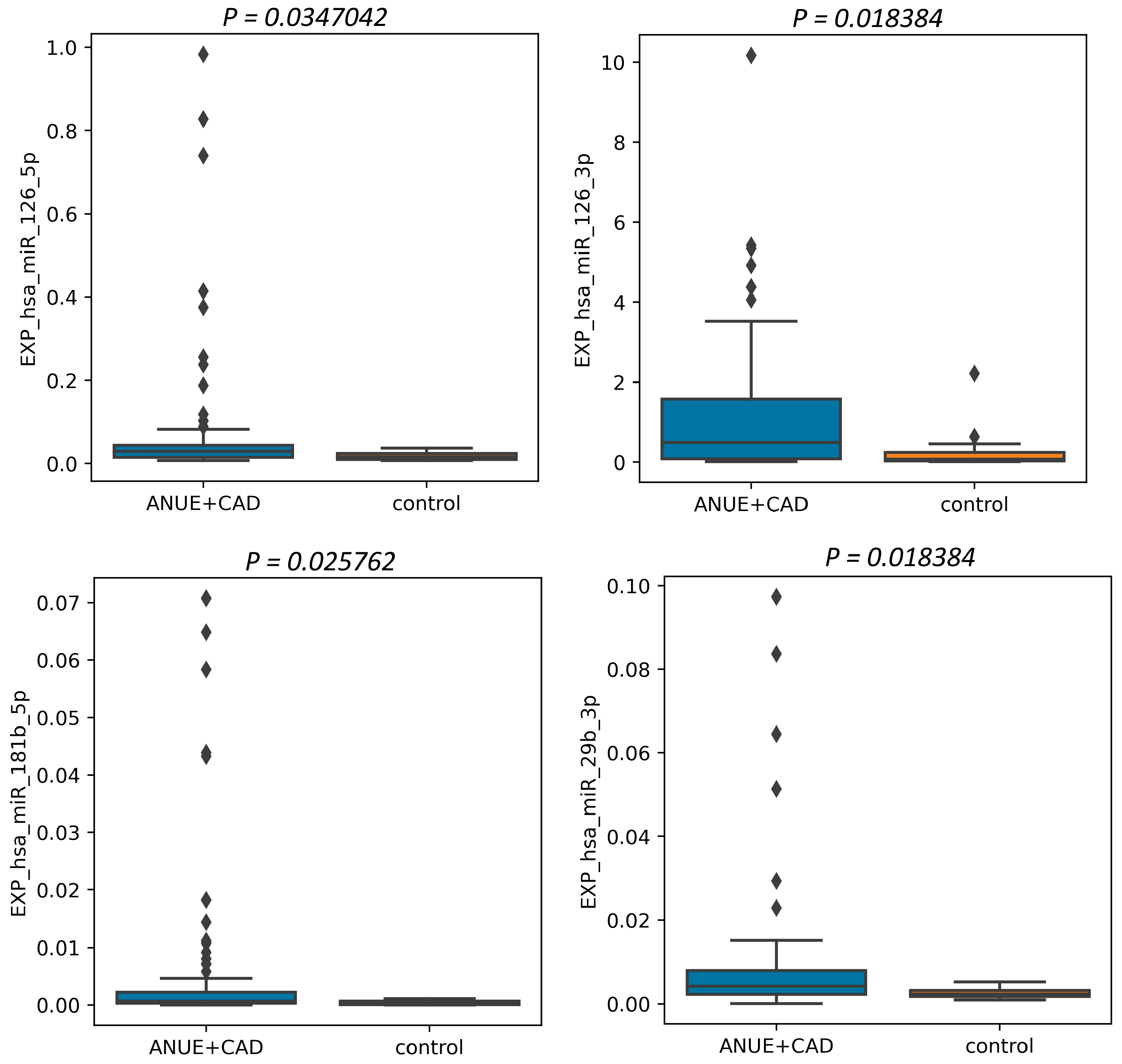
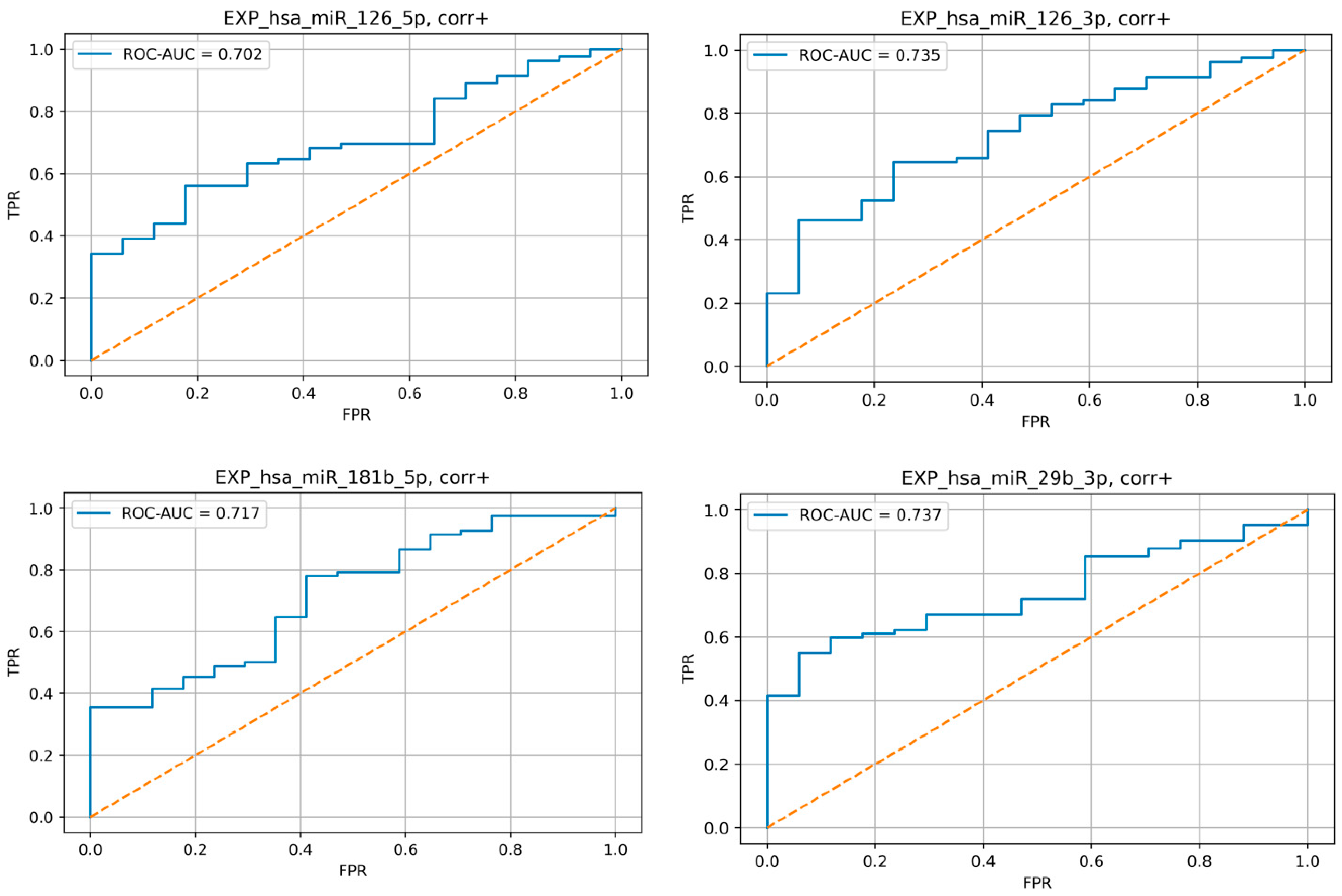
3.4. Evaluation of microRNA Expression Profiles in Patients with and without Coronary Atherosclerosis
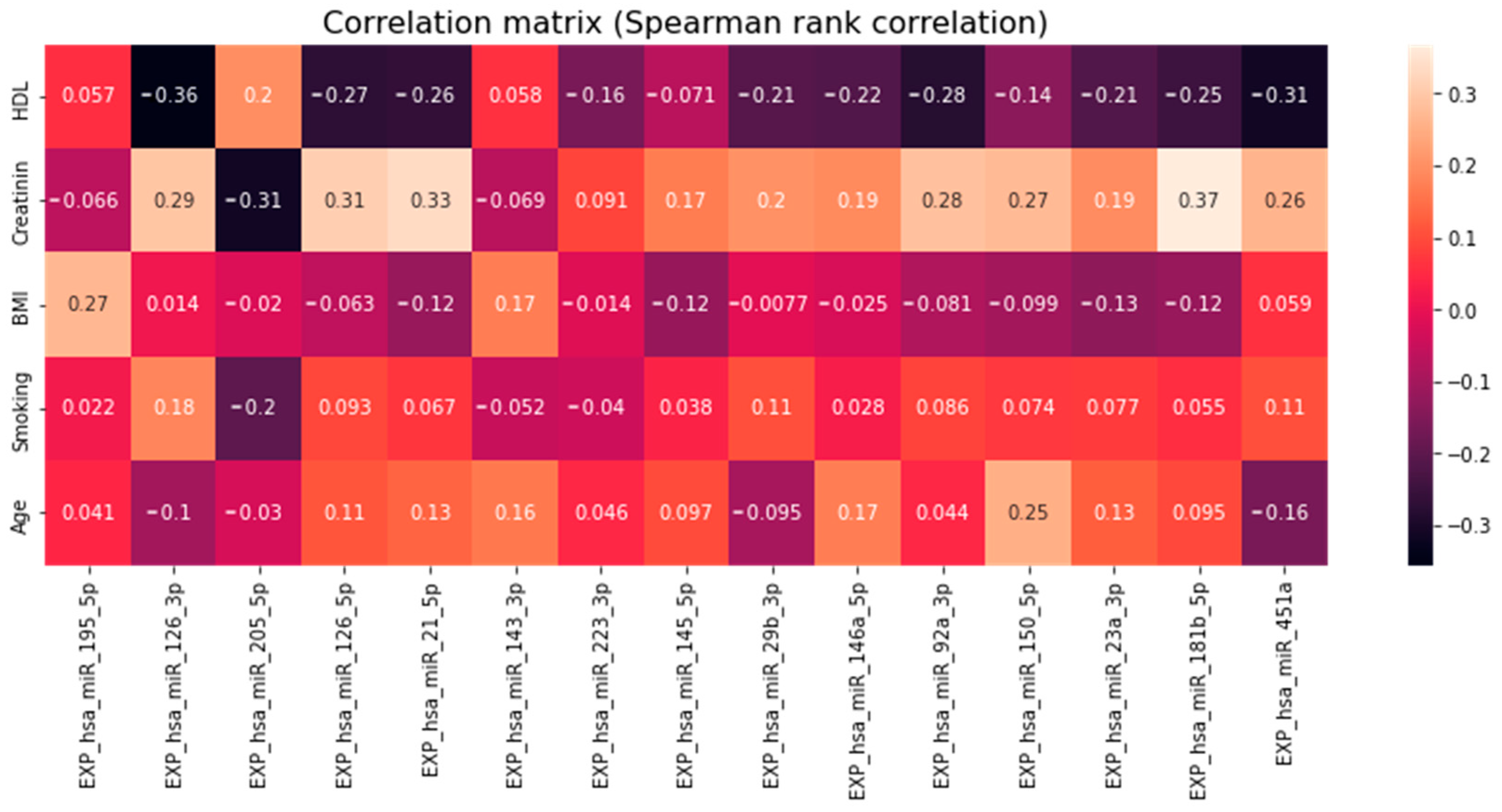
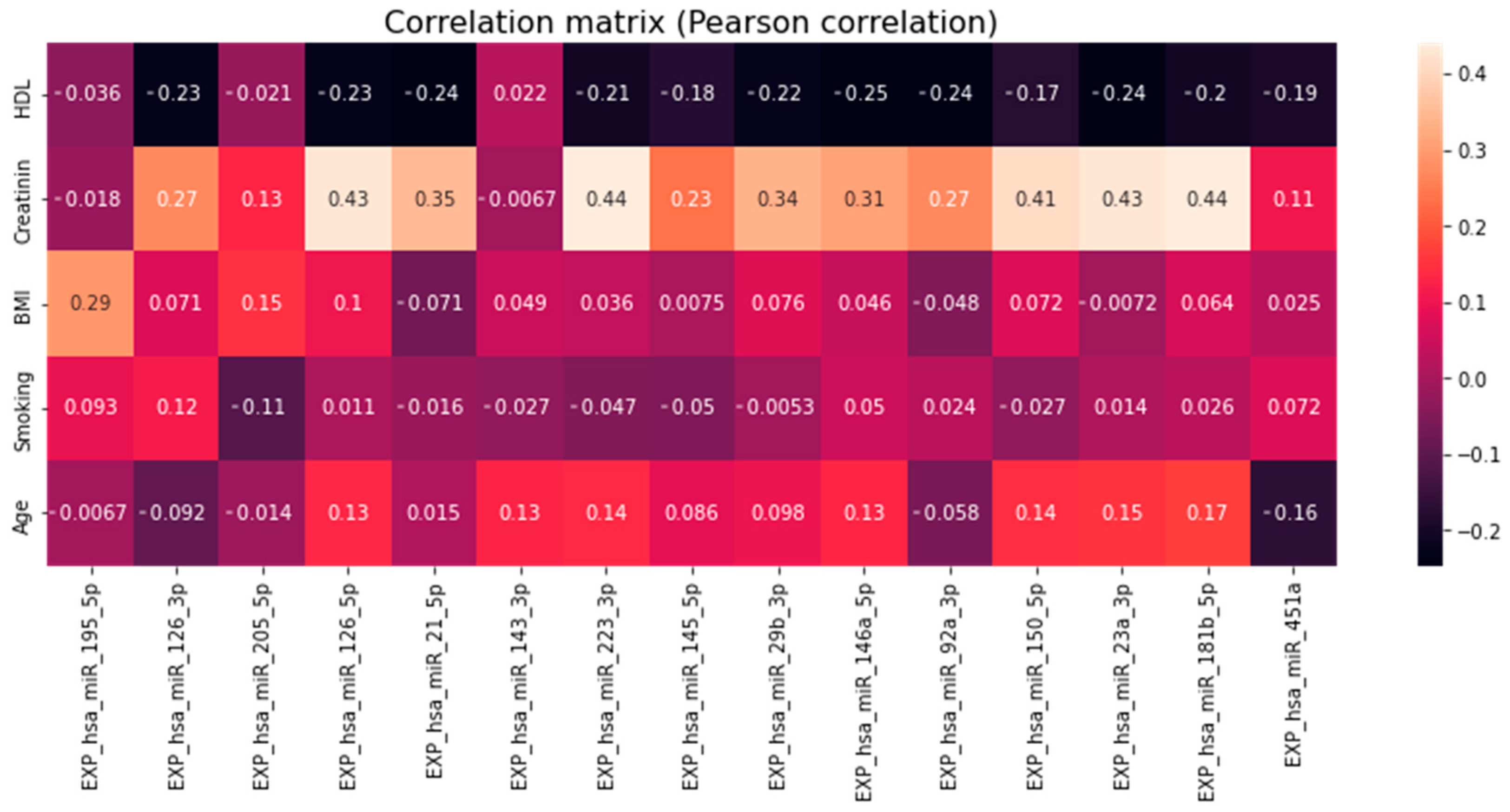
3.5. Association of miRNA Levels with Clinical and Demographical Characteristics of Patients and Cardiovascular Risks
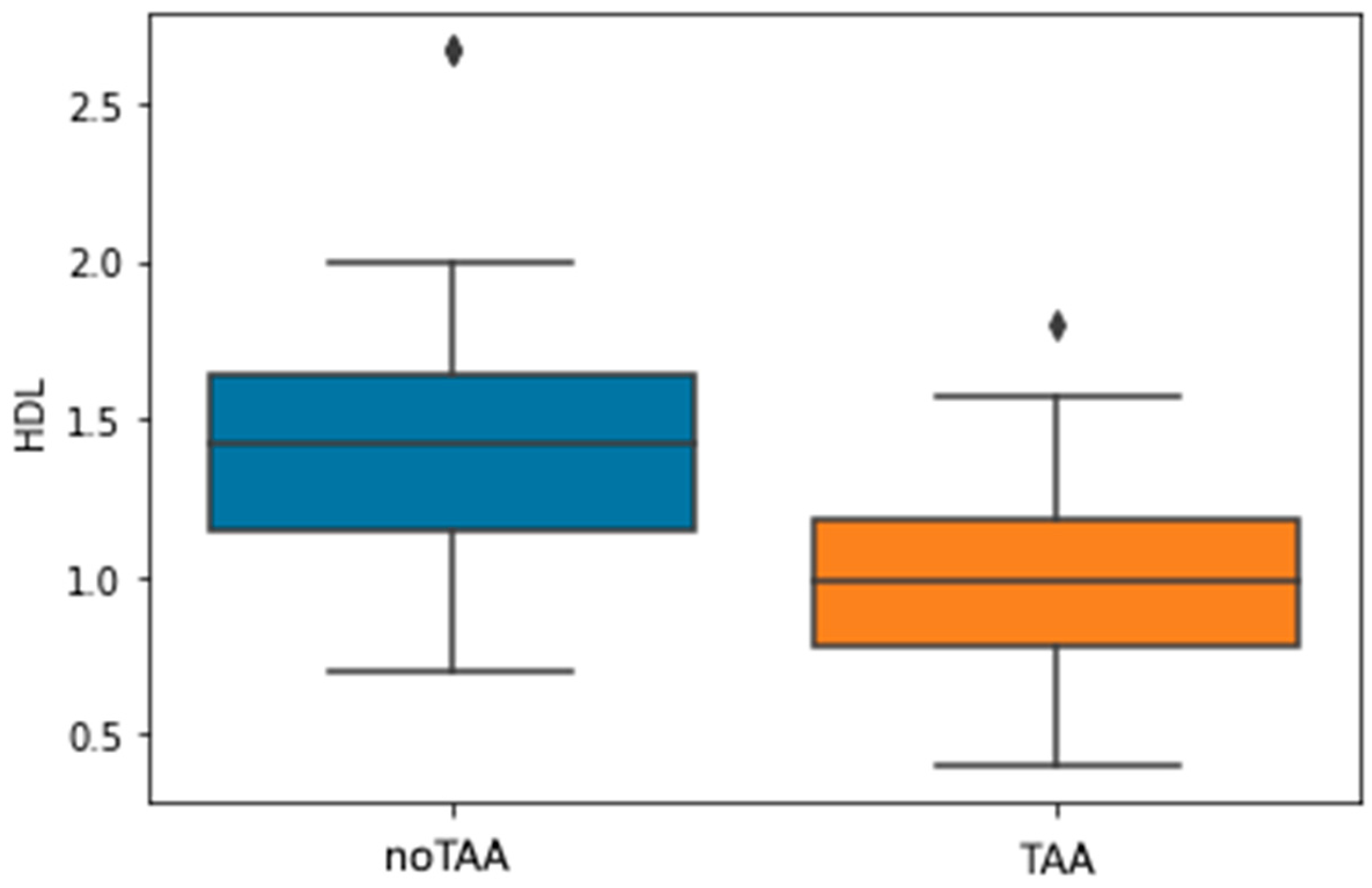
3.6. Association of HDL Levels with the Presence of TAA
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, E.; Wilson, L.; Wickramasinghe, K.; Bhatnagar, P.; Leal, J.; Luengo-Fernandez, R.; Burns, R.; Rayner, M.; Townsend, N. European Cardiovascular Disease Statistics; European Heart Network: Brussels, Belgium, 2017; Available online: https://www.ehnheart.org/images/CVD-statistics-report-August-2017.pdf (accessed on 3 May 2023).
- Oladokun, D.; Patterson, B.O.; Sobocinski, J.; Karthikesalingam, A.; Loftus, I.; Thompson, M.M.; Holt, P.J. Systematic Review of the Growth Rates and Influencing Factors in Thoracic Aortic Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 674–681. [Google Scholar] [CrossRef] [Green Version]
- Isselbacher, E.M. Thoracic and abdominal aortic aneurysms. Circulation 2005, 111, 816–828. [Google Scholar] [CrossRef] [Green Version]
- Romaine, S.P.R.; Tomaszewski, M.; Condorelli, G.; Samani, N.J. MicroRNAs in cardiovascular disease: An introduction for clinicians. Heart 2015, 101, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Navickas, R.; Gal, D.; Laucevičius, A.; Taparauskaitė, A.; Zdanytė, M.; Holvoet, P. Identifying circulating microRNAs as biomarkers of cardiovascular disease: A systematic review. Cardiovasc. Res. 2016, 111, 322–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, J.; Zhao, J.; Evan, G.; Xiao, C.; Cheng, Y.; Xiao, J. Circulating microRNAs: Novel biomarkers for cardiovascular diseases. J. Mol. Med. 2012, 90, 865–875. [Google Scholar] [CrossRef]
- Zhou, S.-S.; Jin, J.-P.; Wang, J.-Q.; Zhang, Z.-G.; Freedman, J.H.; Zheng, Y.; Cai, L. miRNAS in cardiovascular diseases: Potential biomarkers, therapeutic targets and challenges. Acta Pharmacol. Sin. 2018, 39, 1073–1084. [Google Scholar] [CrossRef] [Green Version]
- Jia, H.; Le, K.; Ma, Z.; Lu, S.; Huang, B.; Wang, C.; Zou, Y.; Sun, Y. MicroRNAs involve in bicuspid aortic aneurysm: Pathogenesis and biomarkers. J. Cardiothorac. Surg. 2021, 16, 230. [Google Scholar] [CrossRef]
- Moushi, A.; Pillar, N.; Keravnou, A.; Soteriou, M.; Shomron, N.; Cariolou, M.A.; Bashiardes, E. MicroRNAs in ascending thoracic aortic aneurysms. Biosci. Rep. 2020, 40, BSR20200218. [Google Scholar] [CrossRef]
- Rozhkov, A.N.; Shchekochikhin, D.Y.; Ashikhmin, Y.I.; Mitina, Y.O.; Evgrafova, V.V.; Zhelankin, A.V.; Gognieva, D.G.; Akselrod, A.S.; Kopylov, P.Y. The Profile of Circulating Blood microRNAs in Outpatients with Vulnerable and Stable Atherosclerotic Plaques: Associations with Cardiovascular Risks. Noncoding RNA 2022, 8, 47. [Google Scholar] [CrossRef]
- Ngo Bilong, E.; Rozhkov, A.N.; Mitina, Y.; Vasiliev, S.V.; Zhelankin, A.V.; Generozov, E.V.; Shchekochikhin, D.; Ternovoy, S.K.; Akselrod, A.S. Upregulation of miRNA 23A-3P, 146A-5P AND 150A-5P as a possible diagnostic marker of unstable angina in patients with thoracic aortic aneurysm. Cardiol. Cardiovasc. Surg. 2022, 15, 385. [Google Scholar] [CrossRef]
- Isselbacher, E.M.; Preventza, O.; Hamilton Black, J.; Augoustides, J.G.; Beck, A.W.; Bolen, M.A.; Braverman, A.C.; Bray, B.E.; Brown-Zimmerman, M.M.; Chen, E.P.; et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2022, 146, e334–e482. [Google Scholar] [CrossRef]
- Mondadori dos Santos, A.; Metzinger, L.; Haddad, O.; M’baya-Moutoula, E.; Taïbi, F.; Charnaux, N.; Massy, Z.A.; Hlawaty, H.; Metzinger-Le Meuth, V. miR-126 Is Involved in Vascular Remodeling under Laminar Shear Stress. BioMed Res. Int. 2015, 2015, 497280. [Google Scholar] [CrossRef] [Green Version]
- Pan, J.; Qu, M.; Li, Y.; Wang, L.; Zhang, L.; Wang, Y.; Tang, Y.; Tian, H.-L.; Zhang, Z.; Yang, G.-Y. MicroRNA-126-3p/-5p Overexpression Attenuates Blood-Brain Barrier Disruption in a Mouse Model of Middle Cerebral Artery Occlusion. Stroke 2020, 51, 619–627. [Google Scholar] [CrossRef]
- Yu, B.; Jiang, Y.; Wang, X.; Wang, S. An integrated hypothesis for miR-126 in vascular disease. Med. Res. Arch. 2020, 8, 2133. [Google Scholar] [CrossRef]
- Sun, L.-L.; Li, W.-D.; Lei, F.-R.; Li, X.-Q. The regulatory role of microRNAs in angiogenesis-related diseases. J. Cell. Mol. Med. 2018, 22, 4568–4587. [Google Scholar] [CrossRef] [Green Version]
- Li, H.-Y.; Zhao, X.; Liu, Y.-Z.; Meng, Z.; Wang, D.; Yang, F.; Shi, Q.-W. Plasma MicroRNA-126-5p is Associated with the Complexity and Severity of Coronary Artery Disease in Patients with Stable Angina Pectoris. Cell. Physiol. Biochem. 2016, 39, 837–846. [Google Scholar] [CrossRef]
- Raskurazhev, A.A.; Shabalina, A.A.; Kuznetsova, P.I.; Tanashyan, M.M. MicroRNA as significant biomarkers of cerebrovascular atherosclerosis. Ann. Clin. Exp. Neurol. 2022, 16, 5–13. [Google Scholar] [CrossRef]
- Abu-Halima, M.; Oberhoffer, F.S.; Wagner, V.; Abd El Rahman, M.; Jung, A.-M.; Zemlin, M.; Rohrer, T.R.; Meese, E.; Abdul-Khaliq, H. MicroRNA-126-3p/5p and Aortic Stiffness in Patients with Turner Syndrome. Children 2022, 9, 1109. [Google Scholar] [CrossRef]
- Venkatesh, P.; Phillippi, J.; Chukkapalli, S.; Rivera-Kweh, M.; Velsko, I.; Gleason, T.; VanRyzin, P.; Aalaei-Andabili, S.H.; Ghanta, R.K.; Beaver, T.; et al. Aneurysm-Specific miR-221 and miR-146a Participates in Human Thoracic and Abdominal Aortic Aneurysms. Int. J. Mol. Sci. 2017, 18, 875. [Google Scholar] [CrossRef] [Green Version]
- Gasiulė, S.; Stankevičius, V.; Patamsytė, V.; Ražanskas, R.; Žukovas, G.; Kapustina, Ž.; Žaliaduonytė, D.; Benetis, R.; Lesauskaitė, V.; Vilkaitis, G. Tissue-Specific miRNAs Regulate the Development of Thoracic Aortic Aneurysm: The Emerging Role of KLF4 Network. J. Clin. Med. 2019, 8, 1609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schober, A.; Nazari-Jahantigh, M.; Wei, Y.; Bidzhekov, K.; Gremse, F.; Grommes, J.; Megens, R.T.A.; Heyll, K.; Noels, H.; Hristov, M.; et al. MicroRNA-126-5p promotes endothelial proliferation and limits atherosclerosis by suppressing Dlk1. Nat. Med. 2014, 20, 368–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hao, X.-Z.; Fan, H.-M. Identification of miRNAs as atherosclerosis biomarkers and functional role of miR-126 in atherosclerosis progression through MAPK signalling pathway. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 2725–2733. [Google Scholar] [PubMed]
- Churov, A.; Summerhill, V.; Grechko, A.; Orekhova, V.; Orekhov, A. MicroRNAs as Potential Biomarkers in Atherosclerosis. Int. J. Mol. Sci. 2019, 20, 5547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, D.; Kassiri, Z. Biology of Tissue Inhibitor of Metalloproteinase 3 (TIMP3), and Its Therapeutic Implications in Cardiovascular Pathology. Front. Physiol. 2020, 11, 661. [Google Scholar] [CrossRef]
- Jiang, Q.; Li, Y.; Wu, Q.; Huang, L.; Xu, J.; Zeng, Q. Pathogenic role of microRNAs in atherosclerotic ischemic stroke: Implications for diagnosis and therapy. Genes Dis. 2022, 9, 682–696. [Google Scholar] [CrossRef]
- Di Gregoli, K.; Mohamad Anuar, N.N.; Bianco, R.; White, S.J.; Newby, A.C.; George, S.J.; Johnson, J.L. MicroRNA-181b Controls Atherosclerosis and Aneurysms through Regulation of TIMP-3 and Elastin. Circ. Res. 2017, 120, 49–65. [Google Scholar] [CrossRef]
- Singh, S.; de Ronde, M.W.J.; Kok, M.G.M.; Beijk, M.A.; de Winter, R.J.; van der Wal, A.C.; Sondermeijer, B.M.; Meijers, J.C.M.; Creemers, E.E.; Pinto-Sietsma, S.-J. MiR-223-3p and miR-122-5p as circulating biomarkers for plaque instability. Open Heart 2020, 7, e001223. [Google Scholar] [CrossRef]
- Yang, N.; Song, Y.; Dong, B.; Yang, J.; Li, Y.; Qin, Q.; Guo, Z. Analysis of miRNA Associated with Coronary Artery Calcification. Comput. Math. Methods Med. 2022, 2022, 3708547. [Google Scholar] [CrossRef]
- Deng, X.; Chu, X.; Wang, P.; Ma, X.; Wei, C.; Sun, C.; Yang, J.; Li, Y. MicroRNA-29a-3p Reduces TNFα-Induced Endothelial Dysfunction by Targeting Tumor Necrosis Factor Receptor 1. Mol. Ther. Nucleic Acids 2019, 18, 903–915. [Google Scholar] [CrossRef] [Green Version]
- Lu, Z.; Wang, F.; Yu, P.; Wang, X.; Wang, Y.; Tang, S.-T.; Zhu, H.-Q. Inhibition of miR-29b suppresses MAPK signaling pathway through targeting SPRY1 in atherosclerosis. Vascul. Pharmacol. 2018, 102, 29–36. [Google Scholar] [CrossRef]
- Widlansky, M.E.; Jensen, D.M.; Wang, J.; Liu, Y.; Geurts, A.M.; Kriegel, A.J.; Liu, P.; Ying, R.; Zhang, G.; Casati, M.; et al. miR-29 contributes to normal endothelial function and can restore it in cardiometabolic disorders. EMBO Mol. Med. 2018, 10, e8046. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.-N.; Luo, G.; Gao, W.-J.; Yang, S.-J.; Zhou, H. miR-29 family: A potential therapeutic target for cardiovascular disease. Pharmacol. Res. 2021, 166, 105510. [Google Scholar] [CrossRef]
- Boon, R.A.; Seeger, T.; Heydt, S.; Fischer, A.; Hergenreider, E.; Horrevoets, A.J.G.; Vinciguerra, M.; Rosenthal, N.; Sciacca, S.; Pilato, M.; et al. MicroRNA-29 in aortic dilation: Implications for aneurysm formation. Circ. Res. 2011, 109, 1115–1119. [Google Scholar] [CrossRef]
- Liang, K.; Cui, M.; Fu, X.; Ma, J.; Zhang, K.; Zhang, D.; Zhai, S. LncRNA Xist induces arterial smooth muscle cell apoptosis in thoracic aortic aneurysm through miR-29b-3p/Eln pathway. Biomed. Pharmacother. 2021, 137, 111163. [Google Scholar] [CrossRef]
- Maegdefessel, L.; Azuma, J.; Toh, R.; Merk, D.R.; Deng, A.; Chin, J.T.; Raaz, U.; Schoelmerich, A.M.; Raiesdana, A.; Leeper, N.J.; et al. Inhibition of microRNA-29b reduces murine abdominal aortic aneurysm development. J. Clin. Investig. 2012, 122, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Raitoharju, E.; Lyytikäinen, L.-P.; Levula, M.; Oksala, N.; Mennander, A.; Tarkka, M.; Klopp, N.; Illig, T.; Kähönen, M.; Karhunen, P.J.; et al. miR-21, miR-210, miR-34a, and miR-146a/b are up-regulated in human atherosclerotic plaques in the Tampere Vascular Study. Atherosclerosis 2011, 219, 211–217. [Google Scholar] [CrossRef]
- Zhelankin, A.V.; Stonogina, D.A.; Vasiliev, S.V.; Babalyan, K.A.; Sharova, E.I.; Doludin, Y.V.; Shchekochikhin, D.Y.; Generozov, E.V.; Akselrod, A.S. Circulating Extracellular miRNA Analysis in Patients with Stable CAD and Acute Coronary Syndromes. Biomolecules 2021, 11, 962. [Google Scholar] [CrossRef]
- Sheikh, M.A. Clinical impact of circulating microRNA-21-5p on the severity of coronary artery disease. Atherosclerosis 2022, 355, 257–258. [Google Scholar] [CrossRef]
- Dai, B.; Wang, F.; Nie, X.; Du, H.; Zhao, Y.; Yin, Z.; Li, H.; Fan, J.; Wen, Z.; Wang, D.W.; et al. The Cell Type-Specific Functions of miR-21 in Cardiovascular Diseases. Front. Genet. 2020, 11, 563166. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Li, D.Y.; Chernogubova, E.; Sun, C.; Busch, A.; Eken, S.M.; Saliba-Gustafsson, P.; Winter, H.; Winski, G.; Raaz, U.; et al. Local Delivery of miR-21 Stabilizes Fibrous Caps in Vulnerable Atherosclerotic Lesions. Mol. Ther. 2018, 26, 1040–1055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canfrán-Duque, A.; Rotllan, N.; Zhang, X.; Fernández-Fuertes, M.; Ramírez-Hidalgo, C.; Araldi, E.; Daimiel, L.; Busto, R.; Fernández-Hernando, C.; Suárez, Y. Macrophage deficiency of miR-21 promotes apoptosis, plaque necrosis, and vascular inflammation during atherogenesis. EMBO Mol. Med. 2017, 9, 1244–1262. [Google Scholar] [CrossRef] [PubMed]
- Maegdefessel, L.; Azuma, J.; Toh, R.; Deng, A.; Merk, D.R.; Raiesdana, A.; Leeper, N.J.; Raaz, U.; Schoelmerich, A.M.; McConnell, M.V.; et al. MicroRNA-21 blocks abdominal aortic aneurysm development and nicotine-augmented expansion. Sci. Transl. Med. 2012, 4, 122ra22. [Google Scholar] [CrossRef] [Green Version]
- Li, K.; Cui, M.-Z.; Zhang, K.-W.; Wang, G.-Q.; Zhai, S.-T. Effect of miR-21 on rat thoracic aortic aneurysm model by regulating the expressions of MMP-2 and MMP-9. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 878–884. [Google Scholar] [CrossRef]
- Olivieri, F.; Prattichizzo, F.; Giuliani, A.; Matacchione, G.; Rippo, M.R.; Sabbatinelli, J.; Bonafè, M. miR-21 and miR-146a: The microRNAs of inflammaging and age-related diseases. Ageing Res. Rev. 2021, 70, 101374. [Google Scholar] [CrossRef]
- Li, Y.; Maegdefessel, L. Non-coding RNA Contribution to Thoracic and Abdominal Aortic Aneurysm Disease Development and Progression. Front. Physiol. 2017, 8, 429. [Google Scholar] [CrossRef] [Green Version]
- Parahuleva, M.S.; Lipps, C.; Parviz, B.; Hölschermann, H.; Schieffer, B.; Schulz, R.; Euler, G. MicroRNA expression profile of human advanced coronary atherosclerotic plaques. Sci. Rep. 2018, 8, 7823. [Google Scholar] [CrossRef] [Green Version]
- Ren, J.; Zhang, J.; Xu, N.; Han, G.; Geng, Q.; Song, J.; Li, S.; Zhao, J.; Chen, H. Signature of circulating microRNAs as potential biomarkers in vulnerable coronary artery disease. PLoS ONE 2013, 8, e80738. [Google Scholar] [CrossRef] [Green Version]
- Kin, K.; Miyagawa, S.; Fukushima, S.; Shirakawa, Y.; Torikai, K.; Shimamura, K.; Daimon, T.; Kawahara, Y.; Kuratani, T.; Sawa, Y. Tissue- and plasma-specific MicroRNA signatures for atherosclerotic abdominal aortic aneurysm. J. Am. Heart Assoc. 2012, 1, e000745. [Google Scholar] [CrossRef] [Green Version]
- Portelli, S.S.; Robertson, E.N.; Malecki, C.; Liddy, K.A.; Hambly, B.D.; Jeremy, R.W. Epigenetic influences on genetically triggered thoracic aortic aneurysm. Biophys. Rev. 2018, 10, 1241–1256. [Google Scholar] [CrossRef]
- Koba, A.; Yamagishi, K.; Sairenchi, T.; Noda, H.; Irie, F.; Takizawa, N.; Tomizawa, T.; Iso, H.; Ota, H. Risk Factors for Mortality from Aortic Aneurysm and Dissection: Results from a 26-Year Follow-Up of a Community-Based Population. J. Am. Heart Assoc. 2023, 12, e027045. [Google Scholar] [CrossRef] [PubMed]



| Parameter 1 | Control, n = 17 | TAA, n = 38 | CAD, n = 67 | adj. p-Value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age, years | 65.0 | 10.88 | 63.0 | 11.93 | 63.0 | 9.23 | 1.0 |
| BMI, kg/m2 | 29.14 | 04.03 | 26.79 | 4.75 | 27.74 | 4.3 | 1.0 |
| Glucose, mmol/L | 5.1 | 0.68 | 5.45 | 0.8 | 5.46 | 0.83 | 1.0 |
| Cholesterol, mmol/L | 5.68 | 1.44 | 4.7 | 1.14 | 5.5 | 1.23 | 0.112375 |
| Triglycerides, mmol/L | 1.43 | 0.49 | 1.31 | 0.94 | 1.42 | 0.85 | 1.0 |
| LDL, mmol/L | 3.72 | 1.38 | 2.7 | 01.01 | 3.24 | 1.08 | 0.216216 |
| HDL, mmol/L | 1.62 | 0.26 | 0.99 | 0.3 | 1.21 | 0.41 | 5.8 × 10−5 |
| VLDL, mmol/L | 0.64 | 0.22 | n/a | n/a | 0.58 | 0.43 | n/a |
| Creatinine, µmol/L | 84.95 | 13.37 | 109.7 | 20.62 | 90.1 | 20.9 | 0.005963 |
| eGFRCKD-EPI, mL/min/1.73 m2 | 66.29 | 14.6 | 60.95 | 18.05 | 63.0 | 16.55 | 1.0 |
| Parameter | Control | TAA | CAD | adj.p-value | |||
| % | % | % | |||||
| Female Sex | 22.2 | 68.4 | 45.5 | 1.0 | |||
| Smoking | 5.6 | 36.8 | 25.8 | 1.0 | |||
| Type 2 Diabetes mellitus | 0.0 | 15.8 | 7.6 | 1.0 | |||
| Myocardial infarction or PCI | 0.0 | 18.8 | 9.7 | 1.0 | |||
| Stroke | 0.0 | 25.0 | 8.1 | 0.949574 | |||
| Hypertension | 88.9 | 86.8 | 90.9 | 1.0 | |||
| Atrial fibrillation | 44.4 | 28.9 | 18.2 | 1.0 | |||
| Acetylsalicylic acid | 44.4 | 42.1 | 53.0 | 1.0 | |||
| Anticoagulation | 33.3 | 36.8 | 42.4 | 1.0 | |||
| Angiotensin-converting enzyme inhibitors | 38.9 | 21.1 | 9.1 | 0.748319 | |||
| Angiotensin receptor blockers | 22.2 | 39.5 | 34.8 | 1.0 | |||
| Beta-blockers | 33.3 | 18.4 | 34.8 | 1.0 | |||
| Calcium channels blockers | 44.4 | 89.5 | 72.7 | 1.0 | |||
| Hypertension | 16.7 | 39.5 | 37.9 | 1.0 | |||
| MicroRNA | p-Level |
|---|---|
| (↓) miR-195-5p | 0.000661 |
| (↑) miR-126-5p | 0.000001 |
| (↑) miR-223-3p | 0.001696 |
| (↑) miR-146a-5p | 0.000026 |
| (↑) miR-23a-3p | 0.00015 |
| (↑) miR-126-3p | <0.000001 |
| (↑) miR-21-5p | <0.000001 |
| (↑) miR-145-5p | 0.001432 |
| (↑) miR-181b-5p | 0.000001 |
| (↑) miR-92a-3p | 0.000002 |
| (↑) miR-205-5p | 0.002194 |
| (↑) miR-143-3p | 0.258977 |
| (↑) miR-29b-5p | 0.000005 |
| (↑) miR-150-5p | 0.009458 |
| (↑) miR-451a | 0.00002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ekedi, A.V.N.B.; Rozhkov, A.N.; Shchekochikhin, D.Y.; Novikova, N.A.; Kopylov, P.Y.; Bestavashvili, A.A.; Ivanova, T.V.; Zhelankin, A.V.; Generozov, E.V.; Konanov, D.N.; et al. Evaluation of microRNA Expression Features in Patients with Various Types of Arterial Damage: Thoracic Aortic Aneurysm and Coronary Atherosclerosis. J. Pers. Med. 2023, 13, 1161. https://doi.org/10.3390/jpm13071161
Ekedi AVNB, Rozhkov AN, Shchekochikhin DY, Novikova NA, Kopylov PY, Bestavashvili AA, Ivanova TV, Zhelankin AV, Generozov EV, Konanov DN, et al. Evaluation of microRNA Expression Features in Patients with Various Types of Arterial Damage: Thoracic Aortic Aneurysm and Coronary Atherosclerosis. Journal of Personalized Medicine. 2023; 13(7):1161. https://doi.org/10.3390/jpm13071161
Chicago/Turabian StyleEkedi, Ange Veroniqe Ngo Bilong, Andrey N. Rozhkov, Dmitry Yu. Shchekochikhin, Nina A. Novikova, Philippe Yu. Kopylov, Afina A. Bestavashvili, Tatiana V. Ivanova, Andrey V. Zhelankin, Eduard V. Generozov, Dmitry N. Konanov, and et al. 2023. "Evaluation of microRNA Expression Features in Patients with Various Types of Arterial Damage: Thoracic Aortic Aneurysm and Coronary Atherosclerosis" Journal of Personalized Medicine 13, no. 7: 1161. https://doi.org/10.3390/jpm13071161







