Biodegradable Implantation Material: Mechanical Properties and Surface Corrosion Mechanism of Mg-1Ca-0.5Zr Alloy
Abstract
:1. Introduction
2. Material and Methods
3. Results and Discussion
3.1. Metallographic Analysis
3.2. Tensile Properties and Fracture Morphology
3.3. Fracture Toughness
3.4. Erosion Properties and Surface Roughness
3.5. Potentiodynamic Polarization Test
3.6. Immersion Test
4. Conclusions
- (1)
- The brittle Mg2Ca phase of the XK105 solid dissolved into the matrix after heat treatment. This made the texture uniform and increased both elongation and fracture toughness. The Young’s modulus of XK105 increased after heat treatment because of the solid solution of Ca atoms.
- (2)
- The TD plane of XK105 had higher strength but lower elongation than those of the ED plane because of the texture effects in which the grain slip was hard to start up on the ED plane. The fracture toughness along ED was better than that along TD because the crack-spreading direction was parallel to the arrangement direction of the secondary phase.
- (3)
- The heat treatment of XK105 reduced galvanic corrosion due to the solid solution, and further improved anti-corrosion ability. The surface-roughened XK105 had a larger surface area, which enhanced the corrosion reaction.
- (4)
- A calcium phosphate layer formed during corrosion on the XK105-H surface, significantly reducing the corrosion rate. The surface-roughened XK105 formed magnesium hydroxide instead because of its faster corrosion rate. The magnesium hydroxide did not provide a protective effect.
- (5)
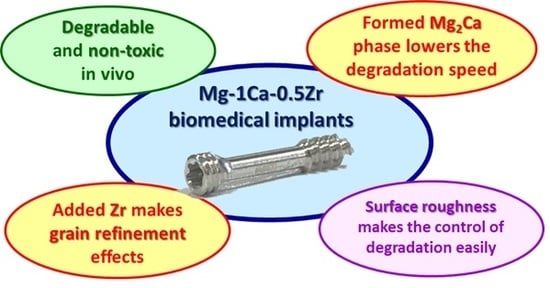
- This study developed a biomedical implant material, Mg-1Ca-0.5Zr alloy. The results can be used as a reference for the biomedical material industry.
Author Contributions
Funding
Conflicts of Interest
References
- Staiger, M.P.; Pietak, A.M.; Huadmai, J.; Dias, G. Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 2006, 27, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Dikici, B.; Topuz, M. Production of annealed cold-Sprayed 316L stainless steel coatings for biomedical applications and their in-vitro corrosion response. Prot. Met. Phys. Chem. Surf. 2018, 54, 333–339. [Google Scholar] [CrossRef]
- Yadroitsev, I.; Karkhmalev, P.; Yadroitsava, I.; Du Plessis, A. Qualification of Ti6Al4V ELI alloy produced by laser powder bed fusion for biomedical applications. JOM 2018, 70, 372–377. [Google Scholar] [CrossRef]
- Chen, Q.Z.; Thouas, G.A. Metallic implant biomaterials. Mater. Sci. Eng. R Rep. 2015, 87, 1–57. [Google Scholar] [CrossRef]
- Chien, C.; Liao, T.Y.; Hong, T.F.; Kuo, T.Y.; Chang, C.H.; Yeh, M.L.; Lee, T.M. Surface microstructure and bioactivity of hydroxyapatite and fluorapatite coatings deposited on Ti-6Al-4V substrates using Nd-YAG Laser. J. Med. Biol. Eng. 2014, 34, 109–115. [Google Scholar] [CrossRef]
- Hench, L.L.; Polak, J.M. Third-generation biomedical materials. Science 2002, 295, 1014–1017. [Google Scholar] [CrossRef] [PubMed]
- Kojima, Y. Platform science and technology for advanced magnesium alloys. Mater. Sci. Forum 2000, 350, 3–18. [Google Scholar] [CrossRef]
- Musso, C.G. Magnesium metabolism in health and disease. Int. Urol. Nephrol. 2009, 41, 357–362. [Google Scholar] [CrossRef]
- Nagels, J.; Stokdijk, M.; Rozing, P.M. Stress shielding and bone resorption in shoulder. J. Shoulder Elb. Surg. 2003, 12, 35–39. [Google Scholar] [CrossRef]
- Jurgen, V. Magnesium: Nutrition and metabolism. Mol. Asp. Med. 2003, 24, 27–37. [Google Scholar] [CrossRef]
- Lin, D.J.; Hung, F.Y.; Jakfar, S.; Yeh, M.L. Tailored coating chemistry and interfacial properties for construction of bioactive ceramic coatings on magnesium biomaterial. Mater. Des. 2016, 89, 235–244. [Google Scholar] [CrossRef]
- Witte, F.; Kaese, V.; Haferkamp, H.; Switzer, E.; Meyer-Lindenberg, A.; Wirth, C.J.; Windhagen, H. In vivo corrosion of four magnesium alloys and the associated bone response. Biomaterials 2005, 26, 3557–3563. [Google Scholar] [CrossRef] [PubMed]
- Pietak, A.; Mahoney, P.; Dias, G.J.; Staiger, M.P. Bone-like matrix formation on magnesium and magnesium alloys. J. Mater. Sci. Mater. Med. 2008, 19, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Witte, F.; Hort, N.; Vogt, C.; Cohen, S.; Kainer, K.U.; Willumeit, R.; Feyerabend, F. Degradable biomaterials based on magnesium corrosion. Curr. Opin. Solid State Mater. Sci. 2008, 12, 63–72. [Google Scholar] [CrossRef] [Green Version]
- Hong, Y.S.; Yang, K.; Zhang, G.D.; Huang, J.J.; Hao, Y.Q.; Ai, H.J. The role of Bone induction of a biodegradable magnesium alloy. Acta Metall. Sin. 2008, 44, 1035–1041. [Google Scholar]
- Radha, R.; Sreekanth, D. Insight of magnesium alloys and composites for orthopedic implant applications—A review. J. Magnes. Alloy. 2017, 5, 286–312. [Google Scholar] [CrossRef]
- Harandi, S.E.; Idris, M.H.; Jafari, H. Effect of forging process on microstructure, mechanical and corrosion properties of biodegradable Mg–1Ca alloy. Mater. Des. 2011, 32, 2596–2603. [Google Scholar] [CrossRef]
- Du, H.; Wei, Z.J.; Liu, X.W.; Zhang, E.L. Effects of Zn on the microstructure, mechanical property and bio-corrosion property of Mg–3Ca alloys for biomedical application. Mater. Chem. Phys. 2011, 125, 568–575. [Google Scholar] [CrossRef]
- Kannan, M.B.; Raman, R.K.S. In vitro degradation and mechanical integrity of calcium-containing magnesium alloys in modified-simulated body fluid. Biomaterials 2008, 29, 2306–2314. [Google Scholar] [CrossRef]
- Lin, D.J.; Hung, F.Y.; Lui, T.S.; Yeh, M.L. Heat treatment mechanism and biodegradable characteristics of ZAX1330 Mg alloy. Mater. Sci. Eng. C 2015, 51, 300–308. [Google Scholar] [CrossRef]
- Jeong, Y.S.; Kim, W.J. Enhancement of mechanical properties and corrosion resistance of Mg–Ca alloys through microstructural refinement by indirect extrusion. Corros. Sci. 2014, 82, 392–403. [Google Scholar] [CrossRef]
- Kim, W.C.; Kim, J.G.; Lee, J.Y.; Seok, H.K. Influence of Ca on the corrosion properties of magnesium for biomaterials. Mater. Lett. 2008, 62, 4146–4148. [Google Scholar] [CrossRef]
- Zheng, Y.F.; Gu, X.N.; Xi, Y.L.; Chai, D.L. In vitro degradation and cytotoxicity of Mg/Ca composites produced by powder metallurgy. Acta Biomater. 2010, 6, 1783–1791. [Google Scholar] [CrossRef] [PubMed]
- Qian, M.; StJohn, D.H.; Frost, M.T. Heterogeneous nuclei size in magnesium–zirconium alloys. Scr. Mater. 2004, 50, 1115–1119. [Google Scholar] [CrossRef]
- Liu, G.L. The electronic structure of the microstructure of Mg-Zr alloys. Acta Phys. Sin. 2008, 57, 1043–1047. [Google Scholar]
- Zhou, Y.L.; Li, Y.; Luo, D.M.; Wen, C.; Hodgson, P. Microstructures, mechanical properties and in vitro corrosion behaviour of biodegradable Mg–Zr–Ca alloys. J. Mater. Sci. 2012, 48, 1632–1639. [Google Scholar] [CrossRef]
- Tamura, Y.; Sugimoto, Y.; Soda, H. Structure and mechanical properties of Mg–Ca and Mg–Ca–Zr alloys. J. Jpn. Inst. Light Met. 2013, 63, 279–285. [Google Scholar] [CrossRef]
- Zhong, C.; Liu, F.; Wu, Y.T.; Le, J.J.; Liu, L.; He, M.F.; Zhu, J.C.; Hu, W.B. Protective diffusion coatings on magnesium alloys: A review of recent developments. J. Alloys Compd. 2012, 520, 11–21. [Google Scholar] [CrossRef]
- Ali, Y.H.; Qiu, D.; Jiang, B.; Pan, F.S.; Zhang, M.X. Current research progress in grain refinement of cast magnesium alloys: A review article. J. Alloys Compd. 2015, 619, 639–651. [Google Scholar] [CrossRef]
- Oyane, A.; Kim, H.M.; Furuya, T.; Kokubo, T.; Miyazaki, T.; Nakamura, T. Preparation and assessment of revised simulated body fluids. J. Biomed. Mater. Res. Part A 2003, 65, 188–195. [Google Scholar] [CrossRef]
- Zeng, R.C.; Qi, W.C.; Cui, H.Z.; Zhang, F.; Li, S.Q.; Han, E.H. In vitro corrosion of as-extruded Mg–Ca alloys—The influence of Ca concentration. Corros. Sci. 2015, 96, 23–31. [Google Scholar] [CrossRef]
- Wang, C.Q.; Sun, M.; Zheng, F.Y.; Peng, L.M.; Ding, W.J. Improvement in grain refinement efficiency of Mg–Zr master alloy for magnesium alloy by friction stir processing. J. Magnes. Alloys 2014, 2, 239–244. [Google Scholar] [CrossRef]
- Zeng, Z.R.; Bian, M.Z.; Xu, S.W.; Davies, C.H.J.; Birbilis, N.; Nie, J.F. Effects of dilute additions of Zn and Ca on ductility of magnesium alloy sheet. Mater. Sci. Eng. A 2016, 674, 459–471. [Google Scholar] [CrossRef]
- Gu, X.N.; Li, S.S.; Li, X.M.; Fan, Y.B. Magnesium based degradable biomaterials: A review. Front. Mater. Sci. 2014, 8, 200–218. [Google Scholar] [CrossRef]
- Yang, G.L.; He, F.M.; Yang, X.F.; Wang, X.X.; Zhao, S.F. Bone responses to titanium implants surface-roughened by sandblasted and double etched treatments in a rabbit model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 106, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Hagihara, K.; Fujii, K.; Matsugaki, A.; Nakano, T. Possibility of Mg-and Ca-based intermetallic compounds as new biodegradable implant materials. Mater. Sci. Eng. C 2013, 33, 4101–4111. [Google Scholar] [CrossRef] [PubMed]
- Von Der Hoh, N.; Bormann, D.; Lucas, A.; Denkena, B.; Hackenbroich, C.; Meyer-Lindenberg, A. Influence of different surface machining treatments of magnesium-based resorbable implants on the degradation behavior in rabbits. Adv. Eng. Mater. 2009, 11, 47–54. [Google Scholar] [CrossRef]
- Song, Y.W.; Shan, D.Y.; Han, E.H. Electrodeposition of hydroxyapatite coating on AZ91D magnesium alloy for biomaterial application. Mater. Lett. 2008, 62, 3276–3279. [Google Scholar] [CrossRef]
- Zhang, C.Y.; Gao, J.C.; Zeng, R.C.; Liu, C.L.; Wu, X.; Wu, D. Corrosion behavior of magnesium alloy AZ31 with calcium phosphate coating in hank’s solition. J. Chin. Ceram. Soc. 2010, 38, 885–891. [Google Scholar]


















| Sample | Pure Mg | XK105-F | XK105-H |
|---|---|---|---|
| Ecorr (V) | −1.601 | −1.971 | −1.786 |
| Icorr (A) | 3.69 × 10−5 | 1.13 × 10−4 | 3.85 × 10−6 |
| Sample | XK105-H | SiO2-90° |
|---|---|---|
| Ecorr (V) | −1.786 | −1.485 |
| Icorr (A) | 3.85 × 10−6 | 5.85 × 10−4 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-T.; Hung, F.-Y.; Syu, J.-C. Biodegradable Implantation Material: Mechanical Properties and Surface Corrosion Mechanism of Mg-1Ca-0.5Zr Alloy. Metals 2019, 9, 857. https://doi.org/10.3390/met9080857
Chen Y-T, Hung F-Y, Syu J-C. Biodegradable Implantation Material: Mechanical Properties and Surface Corrosion Mechanism of Mg-1Ca-0.5Zr Alloy. Metals. 2019; 9(8):857. https://doi.org/10.3390/met9080857
Chicago/Turabian StyleChen, Yen-Ting, Fei-Yi Hung, and Jie-Cheng Syu. 2019. "Biodegradable Implantation Material: Mechanical Properties and Surface Corrosion Mechanism of Mg-1Ca-0.5Zr Alloy" Metals 9, no. 8: 857. https://doi.org/10.3390/met9080857