Factors Affecting the Acceptance of Pandemic Influenza A H1N1 Vaccine amongst Essential Service Providers: A Cross Sectional Study
Abstract
:1. Introduction
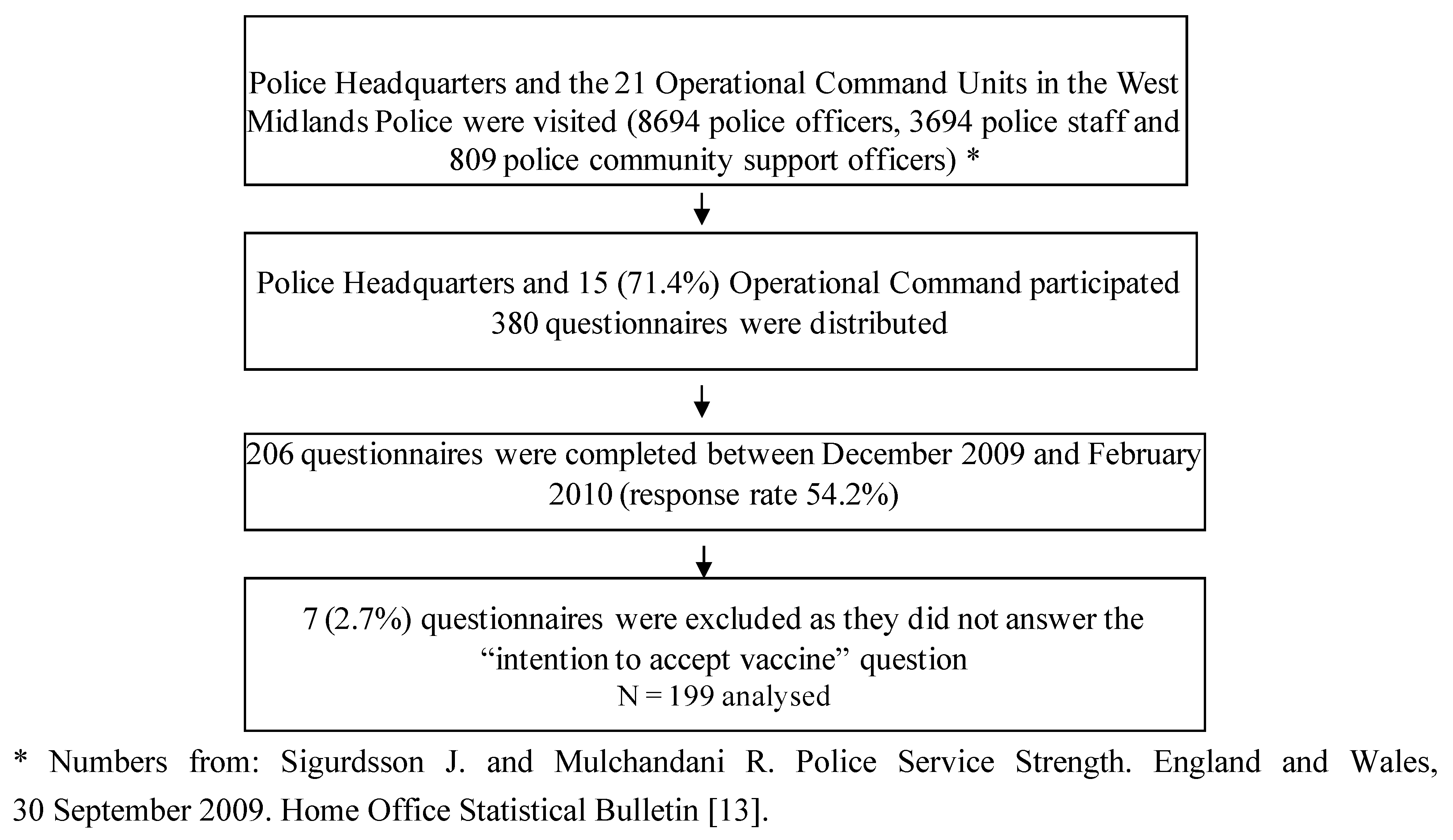
2. Experimental Section
2.1. Study Design and Setting
2.2. Questionnaire Distribution and Sample
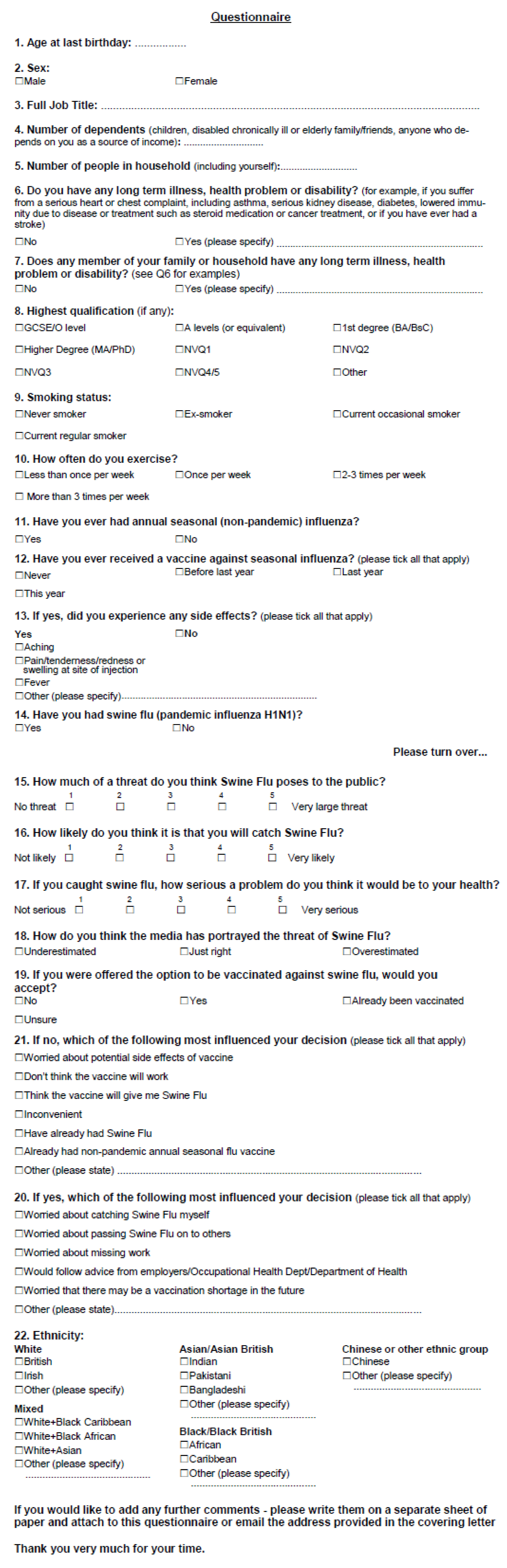
2.3. Questionnaire Content
2.4. Statistical Analysis
3. Results
3.1. Response Rates
3.2. Baseline Characteristics and Descriptive Data
| Variable | Total (%) | |
|---|---|---|
| Age (years): | ||
| <30 | 44 (22.1) | |
| 30–39 | 64 (32.2) | |
| 40–49 | 58 (29.2) | |
| 50–59 | 23 (11.6) | |
| >60 | 7 (3.5) | |
| Missing | 3 (1.5) | |
| Sex: | ||
| Men | 94 (47.2) | |
| Women | 105 (52.8) | |
| Ethnicity: | ||
| White | 176 (88.4) | |
| Mixed | 5 (2.5) | |
| Asian | 10 (5.0) | |
| Black | 3 (1.5) | |
| Chinese | 1 (0.5) | |
| Other | 1 (0.5) | |
| Missing | 3 (1.5) | |
| Job: | ||
| Office Based | 46 (23.1) | |
| Non Office-Based | 149 (74.9) | |
| Missing | 4(2.0) | |
| Presence of a Long Term Illness in Respondent: | ||
| Yes | 32 (16.1) | |
| No | 165 (82.9) | |
| Missing | 2 (1.0) | |
| Presence of a Long Term Illness in a Family Member of Responder: | ||
| Yes | 44 (22.1) | |
| No | 153 (76.9) | |
| Missing | 2 (1.0) | |
| Highest Qualification: | ||
| GCSE/O Level/NVQ1+2 | 64 (32.1) | |
| A Level/NVQ3 | 59 (29.6) | |
| Degree/NVQ4+5/Higher degree | 56 (28.1) | |
| Other | 16 (8.0) | |
| Missing | 4 (2.0) | |
| Smoking Status: | ||
| Never-Smoker | 124 (62.3) | |
| Ex-Smoker | 52 (26.1) | |
| Current Smoker | 22 (11.0) | |
| Missing | 1 (0.5) | |
| Exercise Level: | ||
| Less than once per week | 57 (28.6) | |
| once a week | 33 (16.6) | |
| 2-3 times per week | 77 (38.7) | |
| More than 3 times a week | 32 (16.1) | |
| Ever had Seasonal Flu: | ||
| Yes | 86 (43.2) | |
| No | 110 (55.3) | |
| Missing | 3 (1.5) | |
| Ever received Seasonal influenza vaccination: | ||
| Yes | 90 (45.3) | |
| No | 107 (53.8) | |
| Missing | 2(1.5) | |
| Seasonal Vaccine Side Effects: | ||
| Yes | 39 (43.3) | |
| No | 51 (56.7) | |
| Have had pandemic influenza A (H1N1) virus : | ||
| Yes | 28 (14.1) | |
| No | 169 (84.9) | |
| Missing | 2 (1.0) | |
3.3. Knowledge and Attitudes of Respondents to Pandemic Influenza A (H1N1) Virus
| Variable | Total n(%) |
|---|---|
| Threat of “Swine Flu” to public: | |
| Low | 81 (40.7) |
| Medium | 90 (45.2) |
| High | 28 (14.1) |
| Likelihood of catching “Swine Flu”: | |
| Low | 99 (49.7) |
| Medium | 75 (37.7) |
| High | 24 (12.1) |
| Missing | 1 (0.5) |
| Seriousness of “Swine Flu” to Health: | |
| Low | 93 (46.7) |
| Medium | 56 (28.1) |
| High | 47 (23.6) |
| Missing | 3 (1.5) |
| Media portrayal of threat of “Swine Flu”: | |
| Underestimated | 4 (2.0) |
| Just Right | 55 (27.6) |
| Overestimated | 139 (69.8) |
| Missing | 1 (0.5) |
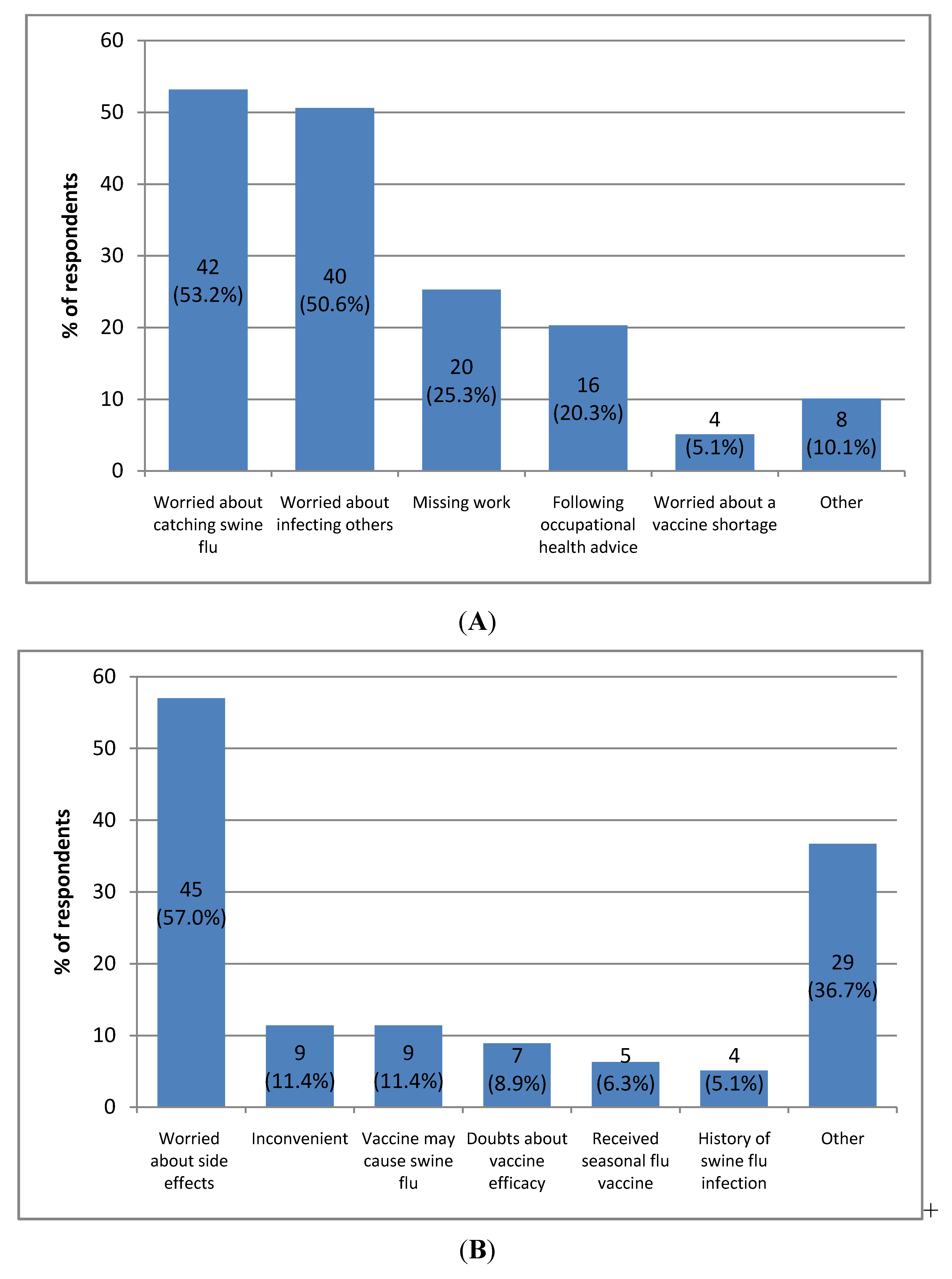
3.4. Acceptance or Declination of the Pandemic Influenza A (H1N1) Vaccine
3.5. Determinants Associated with Intention to Accept the Vaccine
| Variable | Number accepting (%) | OR (95%CI) | Model 1 * | Model 2 * | |
|---|---|---|---|---|---|
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | ||||
| Age: | |||||
| <40 | 42 (52.5%) | 1 | 1 | 1 | |
| ≥40 | 35 (46.1%) | 0.77 (0.41–1.45) | 0.36 (0.16–0.82) | 0.36 (0.15–0.85) | |
| Sex: | |||||
| Men | 43 (56.6%) | 1 | 1 | 1 | |
| Women | 36 (43.4%) | 0.59 (0.31–1.10) | 0.47 (0.23–0.99) | 0.53 (0.25–1.12) | |
| Job: | |||||
| Office Based | 14 (35.1%) | 1 | - | 1 | |
| Non Office-Based | 64 (54.7%) | 2.24 (1.06–4.72) | - | 2.05 (0.87–4.86) | |
| Presence of Long Term Illness: | |||||
| No | 60 (46.9%) | 1 | - | - | |
| Yes | 17 (58.6%) | 1.61 (0.71–3.63) | - | - | |
| Presence of a Long Term Illness in a Family Member: | |||||
| No | 59 (48.0%) | 1 | - | - | |
| Yes | 19 (55.9%) | 1.37 (0.64–2.95) | - | - | |
| Highest Qualification: | |||||
| Below A’level | 24 (45.3%) | 1 | - | - | |
| A Level equivalent or higher | 47 (53.4%) | 1.39 (0.70, 2.75) | - | - | |
| Smoking Status: | |||||
| Non-Smoker | 52 (50.5%) | 1 | 1 | 1 | |
| Ex-Smoker | 17 (40.5%) | 0.67 (0.32–1.38) | 0.69 (0.30, 1.61) | 0.73 (0.31, 1.71) | |
| Current smoker | 10 (71.4%) | 2.45(0.72–8.32) | 4.89 (1.05, 22.72) | 4.37 (0.89, 21.35) | |
| Exercise Level: | |||||
| Less than once a week | 22 (45.8%) | 1 | - | - | |
| Once a week | 14 (53.9%) | 1.37(0.53–3.59) | - | - | |
| 2-3 times a week | 30 (51.7%) | 1.27(0.59–2.73) | - | - | |
| More than 3 times a week | 13 (48.2%) | 1.10(0.43–2.82) | - | - | |
| Ethnicity: | |||||
| White | 65 (46.8%) | 1 | - | 1 | |
| Non-White | 12 (70.6%) | 2.66 (0.96–7.31) | - | 2.47 (0.73, 8.42) | |
| Ever received seasonal influenza vaccine | |||||
| No | 27 (33.3%) | 1 | 1 | 1 | |
| Yes | 51 (67.1%) | 4.08 (2.1, 7.93) | 7.92 (3.38, 18.53) | 8.59 (3.55, 20.79) | |
| Had pandemic influenza A (H1N1) infection: | |||||
| No | 64 (47.1%) | 1 | - | - | |
| Yes | 15 (71.4%) | 2.81 (1.03–7.68) | - | - | |
| Variable | Number accepting (%) | OR (95% CI) | Adjusted OR* 95% CI) | |
|---|---|---|---|---|
| Threat of “Swine Flu” to public: | ||||
| Low | 28 (40.6%) | 1 | 1 | |
| Medium | 32 (49.2%) | 1.42 (0.72–2.81) | 1.86 (0.83, 4.18) | |
| High | 19 (76.0%) | 4.64 (1.65–13.07) | 4.44 (1.34, 14.70) | |
| Likelihood of catching “Swine Flu”: | ||||
| Low | 33 (42.9%) | 1 | 1 | |
| Medium | 29 (48.3%) | 1.24 (0.63–2.46) | 1.38 (0.64–3.00) | |
| High | 16 (76.2%) | 4.27 (1.42–12.83) | 5.08 (1.44, 17.93) | |
| Seriousness of “Swine Flu” to Health: | ||||
| Low | 29 (38.2%) | 1 | 1 | |
| Medium | 23 (54.8%) | 1.96 (0.91–4.21) | 1.43 (0.57–3.56) | |
| High | 26 (65.0%) | 3.01 (1.36–6.68) | 2.86 (1.14, 7.15) | |
| Media portrayal of threat of “Swine Flu”: | ||||
| Underestimated | 3 (75.0%) | 1 | 1 | |
| Just right | 29 (65.9%) | 0.64 (0.06–6.74) | 1.70 (0.12, 24.21) | |
| Overestimated | 47 (42.7%) | 0.25 (0.03–2.47) | 0.54 (0.04–7.24) | |
4. Discussion
4.1. Main Findings
4.1.1. Acceptance of Pandemic and Seasonal Influenza Vaccinations
4.1.2. Attitudes and Perceptions
- The existence of sufficient health concern or motivation;
- Belief of susceptibility to a serious health problem or its complications;
- Belief that the benefit of an action outweighs its possible disadvantages.
4.2. Strengths and Limitations of This Study
4.3. Implications
5. Conclusions
Appendix
| Variable | Study sample (%) | WM Police (%) | |
|---|---|---|---|
| Age: | |||
| ≤30 | 30.6 | 28.4 | |
| >30 | 69.4 | 71.6 | |
| Sex: | |||
| Male | 47.1 | 73.9 | |
| Female | 52.9 | 26.1 | |
| Ethnicity: | |||
| White | 89.9 | 92.7 | |
| Non-white | 10.1 | 7.3 | |
| Smoking Status *: | |||
| Never Smoked | 62.9 | 52.0 | |
| Ex-Smokers | 25.9 | 28.0 | |
| Current Smokers | 11.2 | 20.0 | |
Conflict of Interest
Acknowledgments
References
- Centres for Disease Control. Outbreak of Swine-Origin Influenza A (H1N1) Virus Infection—Mexico, March–April 2009. Available online: http://www.webcitation.org/5jhPR679t/ (accessed on 3 December 2012).
- World Health Organisation. Statement to the press by WHO Director-General Dr. Margaret Chan.11 June 2009. Available online: http://www.who.int/mediacentre/news/statements/2009/h1n1_pandemic_phase6_20090611/en/index.html/ (accessed on 3 December 2012).
- UK Health Departments. UK Influenza Pandemic Contingency Plan [Online]. 2005 March [cited 2009 Nov 21]. Available online: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4104437.pdf (accessed on 3 December 2012).
- The H1N1 swine flu program for October 2009. Available online: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_107190.pdf (accessed on 3 December 2012).
- Health Protection Agency. Epidemiological report of pandemic H1N1 (2009) in the UK. Available online: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1284475321350/ (accessed on 3 December 2012).
- Monto, A.S. Seasonal influenza and vaccination coverage. Vaccine 2010, 285, D33–D44. [Google Scholar] [CrossRef]
- Burls, A.; Jordan, R.; Barton, P.; Olowokure, B.; Wake, B.; Albon, E.; Hawker, J.I. Vaccinating healthcare workers against influenza to protect the vulnerable—is it a good use of healthcare resources? A systematic review of the evidence and an economic evaluation. Vaccine 2006, 24, 4212–4221. [Google Scholar] [CrossRef]
- Hollmeyer, H.G.; Hayden, F.; Poland, G.; Buchholz, U. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine 2009, 27, 3935–3944. [Google Scholar] [CrossRef]
- Stokes, S.; Ismail, K.M. Uptake of the H1N1 vaccine by maternity staff at a university hospital in the UK. Int. J. Gynecol. Obstet. 2011, 12, 247. [Google Scholar] [CrossRef]
- Chor, J.S.Y.; Ngai, K.L.K.; Goggins, W.B.; Wong, M.C.S.; Wong, S.Y.S.; Lee, N.; Leung, T.F.; Rainer, T.H.; Griffiths, S.; Chan, P.K.S. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ 2009, 339, b3391. [Google Scholar]
- Bish, A.; Yardley, L.; Nicoll, A.; Michie, S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine 2011, 29, 6472–6484. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Dedoukou, X.; Patrinos, S.; Maragos, A.; Poufta, S.; Gargalianos, P.; Lazanas, M. Determinants of intention to get vaccinated against novel (pandemic) influenza A H1N1 among health-care workers in a nationwide survey. J. Infect. 2010, 61, 252–258. [Google Scholar] [CrossRef]
- Sigurdsson, J.; Mulchandani, R. Police Service Strength, England and Wales, 30 September 2009; London, UK, 2010; Home Office Statistical Bulletin 03/10 Research Development and Statistics Directorate. [Google Scholar]
- Robinson, S. Bugler C for the Office for National Statistics. General lifestyle survey 2008. Smoking and drinking among adults, 2008. Available online: http://www.ons.gov.uk/ons/search/index.html?pageSize=50&newquery=General+Lifestyle+Survey+Smoking+and+drinking+among+adults/ (accessed on 3 December 2012).
- Department of Health and Health Protection Agency. Influenza vaccine uptake for HCW in England. Winter 2008-9. Available online: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_116625.pdf (accessed on 3 December 2012).
- Pareek, M.; Clark, T.; Dillon, H.; Kumar, R.; Stephenson, I. Willingness of healthcare workers to accept voluntary stockpiled H5N1 vaccine in advance of pandemic activity. Vaccine 2009, 27, 1242–1247. [Google Scholar] [CrossRef]
- Virseda, S.; Restrepo, M.A.; Arranz, E.; Magan-Tapia, P.; Fernandez-Riuz, M.; Gomez de la Camara, A.; Aguado, J.M.; Lopez-Medrano, F. Seasonal and pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish University Hospital. Vaccine 2010, 28, 4751–4757. [Google Scholar]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social Learning and the health Belief Model. Health Educ. Behav. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Esteves-Jaramillo, A.; Omer, S.B.; Gonzalez-Diaz, E.; Salmon, D.A.; Hixson, B.; Navarro, F.; Kawa-Karasik, S.; Frew, P.; Morfin-Otero, R.; Rodriguez-Noriega, E.; et al. Acceptance of a vaccine against novel influenza A (H1N1) virus among health care workers in two major cities in Mexico. Arch. Med. Res. 2009, 40, 705–711. [Google Scholar] [CrossRef]
- Al-Tawfiq, J.A.; Antony, A.; Abed, M.S. Attitudes towards influenza vaccination of multi-nationality health-care workers in Saudi Arabia. Vaccine 2009, 27, 5538–5541. [Google Scholar] [CrossRef]
- Clark, S.J.; Cowan, A.E.; Wortley, P.M.; Arbor, A. Influenza vaccination attitudes and practices among US registered nurses. Am. J. Infect. Control 2009, 37, 551–556. [Google Scholar]
- Rachiotis, G.; Mouchtouri, V.A.; Kremastinou, J.; Gourgoulianis, K.; Hadjichristodolou, C. Low acceptance of vaccination against the 2009 pandemic influenza A(H1N1) among healthcare workers in Greece. Euro. Surveill. 2010, 15, 19486. [Google Scholar]
- Sartor, C.; Tissot-Dupont, H.; Zandotti, C.; Martin, F.; Roques, P.; Drancourt, M. Use of a Mobile Cart Influenza Program for Vaccination of Hospital Employees. Infect. Control Hosp. Epidemiol. 2004, 25, 918–922. [Google Scholar]
- Trick, W.E.; Das, K.; Gerard, M.N.; Charles-Damte, M.; Murphy, G.; Benson, I.; Morita, J.Y. Clinical trial of standing-orders strategies to increase the inpatient influenza vaccination rate. Infect. Control Hosp. Epidemiol. 2009, 30, 86–88. [Google Scholar] [CrossRef]
- Szilagyi, P.; Vann, J.; Bordley, C.; Chelminski, A.; Kraus, R.; Margolis, P.; Rodewald, L. Interventions aimed at improving immunization rates. Cochrane Database Syst Rev. Available online: http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD003941/frame.html/ (accessed on 3 December 2012). [serial online] 2002 [cited 16 April 2010] (4):CD003941..
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Beattie, A.; Palmer, K.; Rees, E.; Riddell, Z.; Roberts, C.; Jordan, R. Factors Affecting the Acceptance of Pandemic Influenza A H1N1 Vaccine amongst Essential Service Providers: A Cross Sectional Study. Vaccines 2013, 1, 17-33. https://doi.org/10.3390/vaccines1010017
Beattie A, Palmer K, Rees E, Riddell Z, Roberts C, Jordan R. Factors Affecting the Acceptance of Pandemic Influenza A H1N1 Vaccine amongst Essential Service Providers: A Cross Sectional Study. Vaccines. 2013; 1(1):17-33. https://doi.org/10.3390/vaccines1010017
Chicago/Turabian StyleBeattie, Alice, Katie Palmer, Emily Rees, Zoe Riddell, Charlotte Roberts, and Rachel Jordan. 2013. "Factors Affecting the Acceptance of Pandemic Influenza A H1N1 Vaccine amongst Essential Service Providers: A Cross Sectional Study" Vaccines 1, no. 1: 17-33. https://doi.org/10.3390/vaccines1010017
APA StyleBeattie, A., Palmer, K., Rees, E., Riddell, Z., Roberts, C., & Jordan, R. (2013). Factors Affecting the Acceptance of Pandemic Influenza A H1N1 Vaccine amongst Essential Service Providers: A Cross Sectional Study. Vaccines, 1(1), 17-33. https://doi.org/10.3390/vaccines1010017




