Factors Influencing the Total Functional Capacity Score as a Critical Endpoint in Huntington’s Disease Research
Abstract
:1. Introduction
2. Methods
2.1. ENROLL-HD Database with Regard to Functional Classification
2.2. Statistical Analysis
3. Results
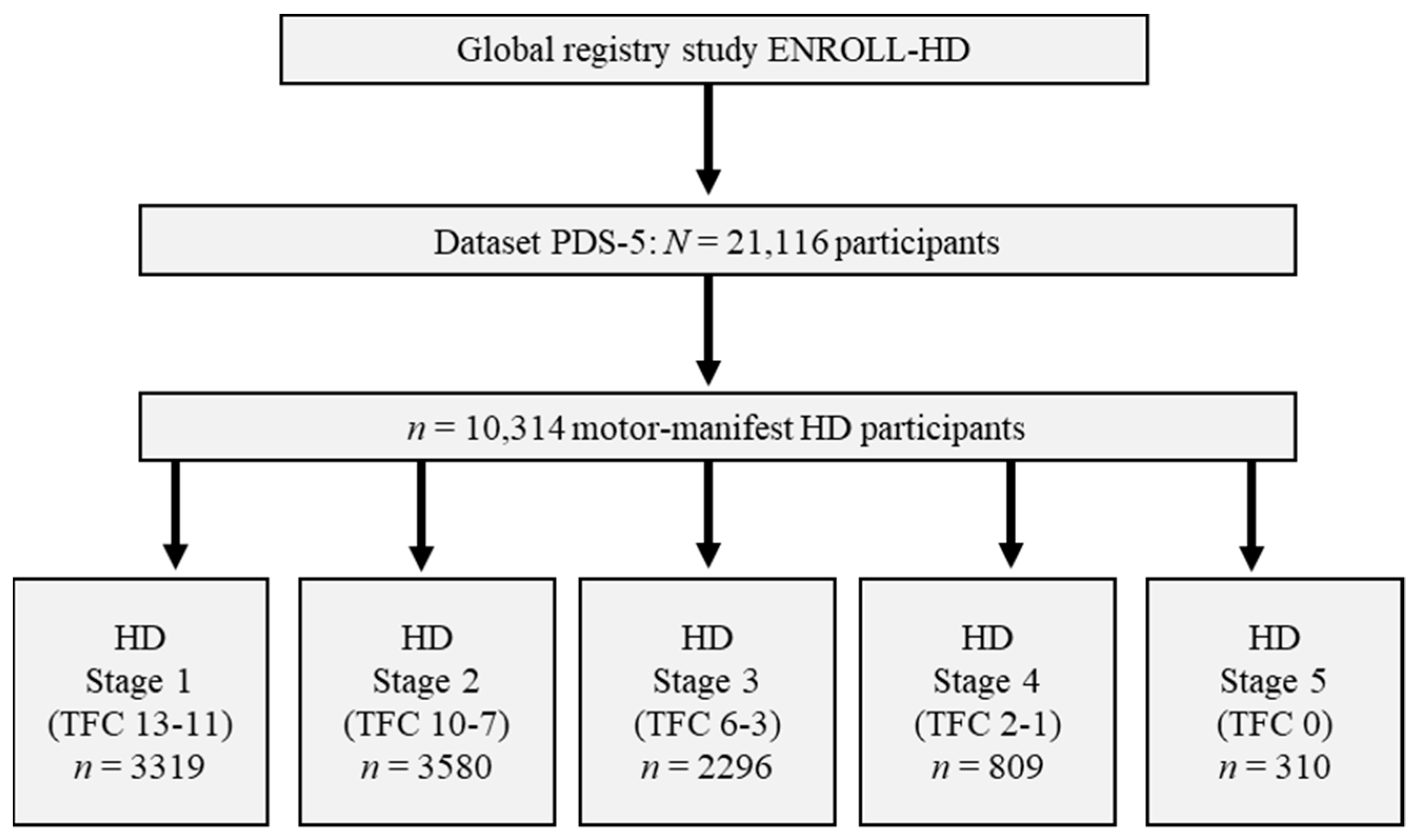
3.1. Motor-Manifest Participants from ENROLL-HD According to Individual Disease Stages
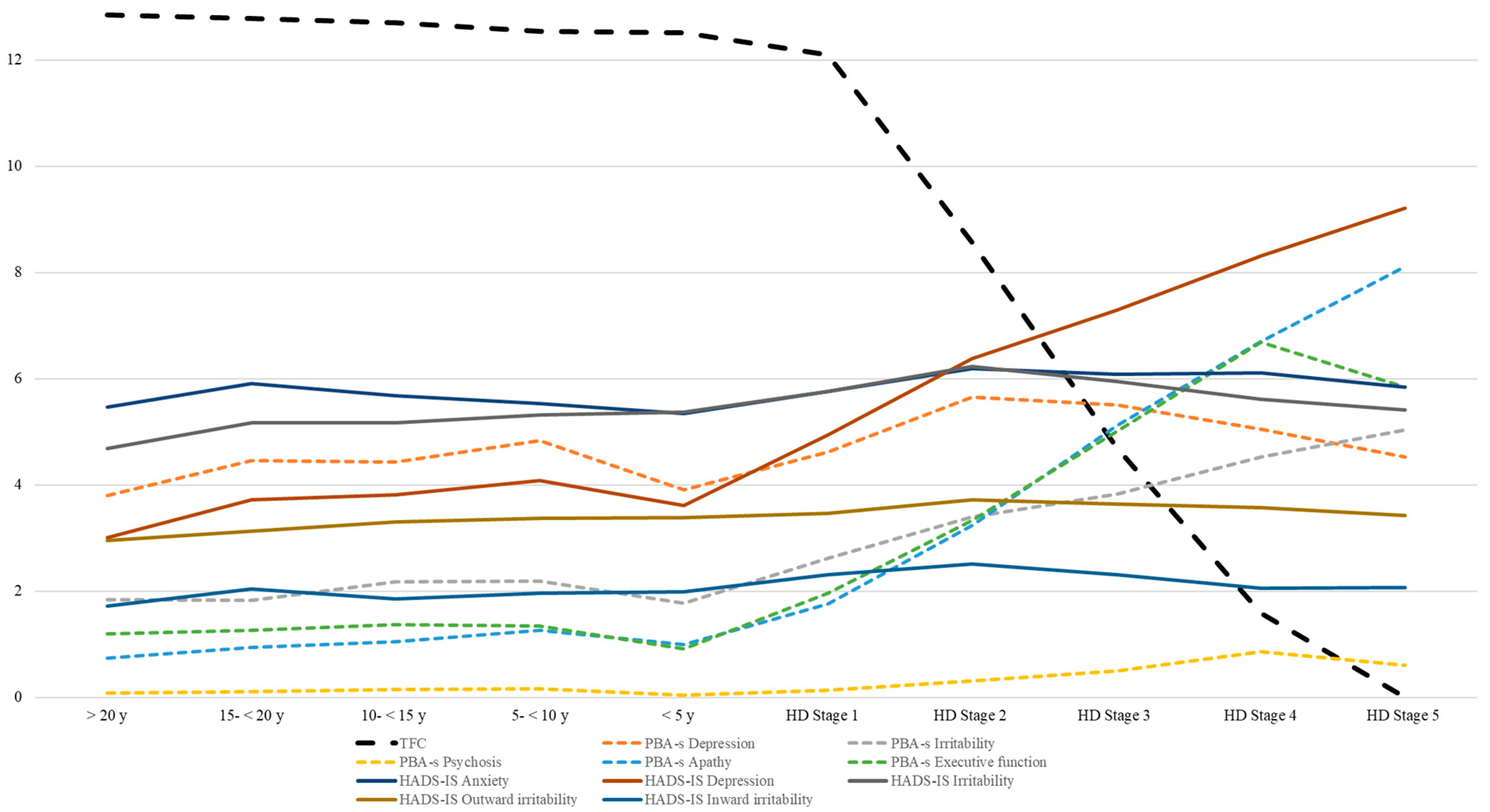
3.2. Neuropsychiatric Symptoms According to Different Disease Stages
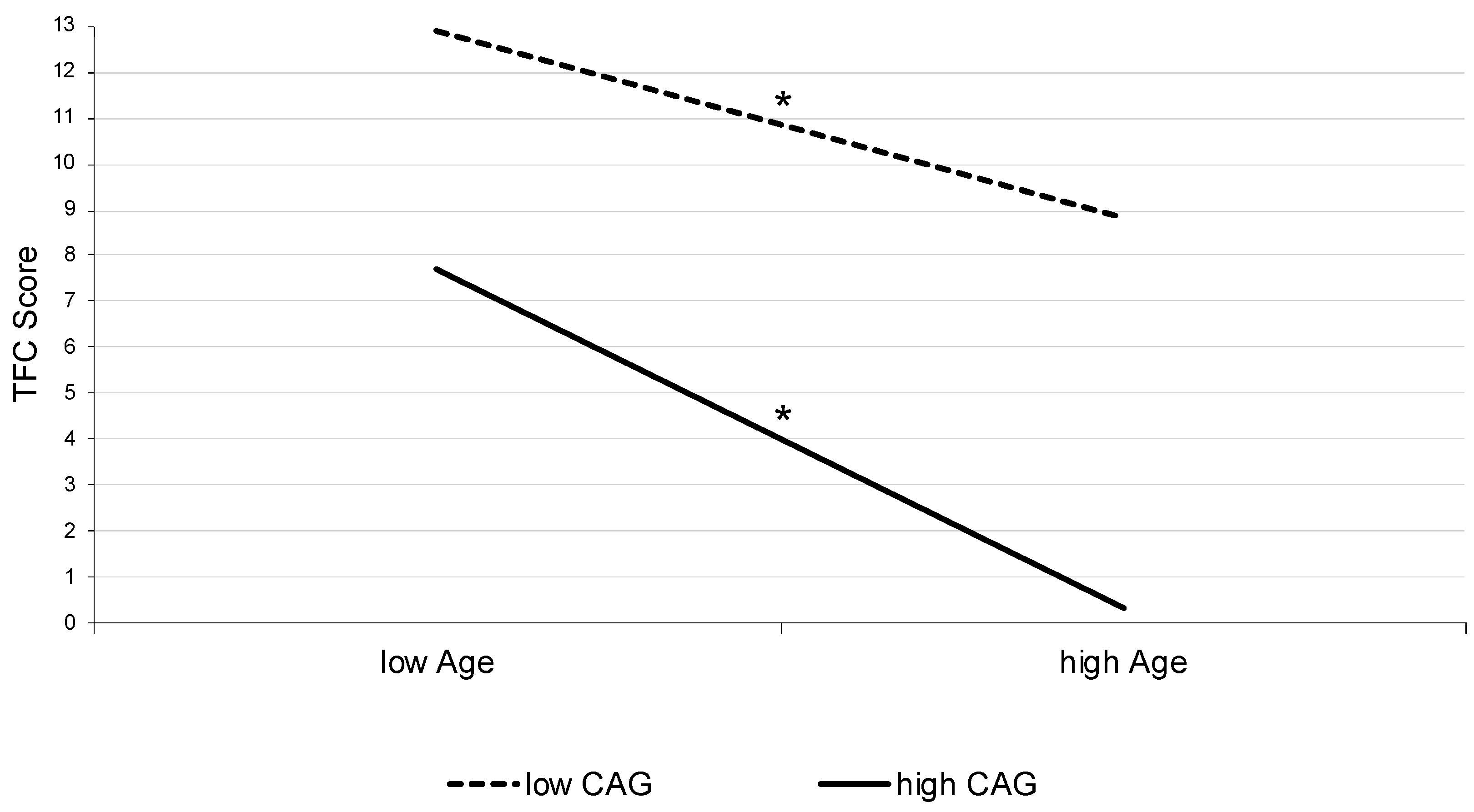
3.3. Interaction Effect between Age and CAG-Repeat Length in Motor-Manifest HD
3.4. Neuropsychiatric Symptoms in Pre-Manifest HD According to Calculated Years to Onset
4. Discussion
4.1. TFC as a Robust Criterion in Manifest HD: Quantifying Neurobiological Effects
4.2. Psychiatric and Cognitive Manifestation in Manifest HD and Its Influence on TFC-Based Stages
4.3. Analyzing Different “Pre-Manifesting Aspects” in Pre-Manifest HD
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roos, R.A.C. Huntington’s disease: A clinical review. Orphanet. J. Rare Dis. 2010, 5, 40. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, J.; von Hein, S.M.; Saft, C. Functional and cognitive capacity differ in dystonic motor subtypes when compared to choreatic and hypokinetic-rigid motor subtypes in Huntington’s disease. Brain Behav. 2020, 10, e01704. [Google Scholar] [CrossRef] [PubMed]
- Walker, F.O. Huntington’s disease. Lancet 2007, 369, 218–228. [Google Scholar] [CrossRef] [PubMed]
- Mestre, T.A.; van Duijn, E.; Davis, A.M.; Bachoud-Lévi, A.-C.; Busse, M.; Anderson, K.E.; Ferreira, J.J.; Mahlknecht, P.; Tumas, V.; Sampaio, C.; et al. Rating scales for behavioral symptoms in Huntington’s disease: Critique and recommendations. Mov. Disord. 2016, 31, 1466–1478. [Google Scholar] [CrossRef]
- Ellis, N.; Tee, A.; McAllister, B.; Massey, T.; McLauchlan, D.; Stone, T.; Correia, K.; Loupe, J.; Kim, K.-H.; Barker, D.; et al. Genetic Risk Underlying Psychiatric and Cognitive Symptoms in Huntington’s Disease. Biol. Psychiatry 2020, 87, 857–865. [Google Scholar] [CrossRef]
- Paulsen, J.S.; Ready, R.E.; Hamilton, J.M.; Mega, M.S.; Cummings, J.L. Neuropsychiatric aspects of Huntington’s disease. J. Neurol. Neurosurg. Psychiatry 2001, 71, 310–314. [Google Scholar] [CrossRef]
- Goh, A.M.; Wibawa, P.; Loi, S.M.; Walterfang, M.; Velakoulis, D.; Looi, J.C. Huntington’s disease: Neuropsychiatric manifestations of Huntington’s disease. Australas. Psychiatry 2018, 26, 366–375. [Google Scholar] [CrossRef]
- Gregory, S.; Scahill, R.I.; Seunarine, K.K.; Stopford, C.; Zhang, H.; Zhang, J.; Orth, M.; Durr, A.; Roos, R.A.C.; Langbehn, D.R.; et al. Neuropsychiatry and White Matter Microstructure in Huntington’s Disease. J. Huntingt. Dis. 2015, 4, 239–249. [Google Scholar] [CrossRef]
- Bordelon, Y.M. Clinical neurogenetics: Huntington disease. Neurol. Clin. 2013, 31, 1085–1094. [Google Scholar] [CrossRef]
- Vassos, E.; Panas, M.; Kladi, A.; Vassilopoulos, D. Effect of CAG repeat length on psychiatric disorders in Huntington’s disease. J. Psychiatr. Res. 2008, 42, 544–549. [Google Scholar] [CrossRef]
- McAllister, B.; Gusella, J.F.; Landwehrmeyer, G.B.; Lee, J.-M.; MacDonald, M.E.; Orth, M.; Rosser, A.E.; Williams, N.M.; Holmans, P.; Jones, L.; et al. Timing and Impact of Psychiatric, Cognitive, and Motor Abnormalities in Huntington Disease. Neurology 2021, 96, e2395–e2406. [Google Scholar] [CrossRef] [PubMed]
- Goold, R.; Flower, M.; Moss, D.H.; Medway, C.; Wood-Kaczmar, A.; Andre, R.; Farshim, P.; Bates, G.P.; Holmans, P.; Jones, L.; et al. FAN1 modifies Huntington’s disease progression by stabilizing the expanded HTT CAG repeat. Hum. Mol. Genet. 2019, 28, 650–661. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.-M.; Zhang, Y.-B.; Wu, Z.-Y. Huntington’s Disease: Relationship Between Phenotype and Genotype. Mol. Neurobiol. 2017, 54, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Wexler, N.S.; Lorimer, J.; Porter, J.; Gomez, F.; Moskowitz, C.; Shackell, E.; Marder, K.; Penchaszadeh, G.; Roberts, S.A.; Gayán, J.; et al. Venezuelan kindreds reveal that genetic and environmental factors modulate Huntington’s disease age of onset. Proc. Natl. Acad. Sci. USA 2004, 101, 3498–3503. [Google Scholar] [PubMed]
- Langbehn, D.R.; Hayden, M.R.; Paulsen, J.S. CAG-repeat length and the age of onset in Huntington disease (HD): A review and validation study of statistical approaches. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2010, 153, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Langbehn, D.R.; Paulsen, J.S. Predictors of diagnosis in Huntington disease. Neurology 2007, 68, 1710–1717. [Google Scholar] [CrossRef]
- Furtado, S.; Suchowersky, O.; Rewcastle, B.; Graham, L.; Klimek, M.L.; Garber, A. Relationship between trinucleotide repeats and neuropathological changes in Huntington’s disease. Ann. Neurol. 1996, 39, 132–136. [Google Scholar] [CrossRef]
- Vojvodić, N.; Culjković, B.; Romac, S.; Stojković, O.; Sternić, N.; Sokić, D.; Kostić, V.S. Znacaj povećanja broja trinukleotidnih ponovaka za klinicka ispoljavanja Hantigtonove horeje. Srp. Arh. Celok. Lek. 1998, 126, 77–82. [Google Scholar]
- Sieradzan, K.; Mann, D.M.; Dodge, A. Clinical presentation and patterns of regional cerebral atrophy related to the length of trinucleotide repeat expansion in patients with adult onset Huntington’s disease. Neurosci. Lett. 1997, 225, 45–48. [Google Scholar] [CrossRef]
- Andrew, S.E.; Goldberg, Y.P.; Kremer, B.; Telenius, H.; Theilmann, J.; Adam, S.; Starr, E.; Squitieri, F.; Lin, B.; Kalchman, M.A. The relationship between trinucleotide (CAG) repeat length and clinical features of Huntington’s disease. Nat. Genet. 1993, 4, 398–403. [Google Scholar] [CrossRef]
- Penney, J.B.; Vonsattel, J.P.; MacDonald, M.E.; Gusella, J.F.; Myers, R.H. CAG repeat number governs the development rate of pathology in Huntington’s disease. Ann. Neurol. 1997, 41, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Long, J.D.; Mills, J.A.; Warner, J.H.; Lu, W.; Paulsen, J.S. Indexing disease progression at study entry with individuals at-risk for Huntington disease. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2011, 156B, 751–763. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.A.; Pantelyat, A.; Kogan, J.; Brandt, J. Determinants of functional disability in Huntington’s disease: Role of cognitive and motor dysfunction. Mov. Disord. 2014, 29, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, J.S.; Nehl, C.; Hoth, K.F.; Kanz, J.E.; Benjamin, M.; Conybeare, R.; McDowell, B.; Turner, B. Depression and stages of Huntington’s disease. J. Neuropsychiatry Clin. Neurosci. 2005, 17, 496–502. [Google Scholar] [CrossRef] [PubMed]
- de Souza, J.; Jones, L.A.; Rickards, H. Validation of self-report depression rating scales in Huntington’s disease. Mov. Disord. 2010, 25, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Horta-Barba, A.; Martínez-Horta, S.; Pérez-Pérez, J.; Sampedro, F.; Puig-Davi, A.; Pagonabarraga, J.; Kulisevsky, J. Measuring the functional impact of cognitive impairment in Huntington’s disease. J. Neurol. 2022, 269, 3541–3549. [Google Scholar] [CrossRef] [PubMed]
- Carlozzi, N.E.; Schilling, S.G.; Boileau, N.R.; Chou, K.L.; Perlmutter, J.S.; Frank, S.; McCormack, M.K.; Stout, J.C.; Paulsen, J.S.; Lai, J.-S.; et al. How different aspects of motor dysfunction influence day-to-day function in huntington’s disease. Mov. Disord. 2019, 34, 1910–1914. [Google Scholar] [CrossRef]
- Marder, K.; Zhao, H.; Myers, R.H.; Cudkowicz, M.; Kayson, E.; Kieburtz, K.; Orme, C.; Paulsen, J.; Penney, J.B.; Siemers, E.; et al. Rate of functional decline in Huntington’s disease. Huntington Study Group. Neurology 2000, 54, 452–458. [Google Scholar] [CrossRef]
- Sellers, J.; Ridner, S.H.; Claassen, D.O. A Systematic Review of Neuropsychiatric Symptoms and Functional Capacity in Huntington’s Disease. J. Neuropsychiatry Clin. Neurosci. 2020, 32, 109–124. [Google Scholar] [CrossRef]
- Gibson, J.S.; Ridner, S.H.; Dietrich, M.S.; Sohn, M.B.; Rhoten, B.A.; Claassen, D.O. Measuring Functional Status in Huntington’s Disease. Mov. Disord. 2021, 36, 757–761. [Google Scholar] [CrossRef]
- Podvin, S.; Reardon, H.T.; Yin, K.; Mosier, C.; Hook, V. Multiple clinical features of Huntington’s disease correlate with mutant HTT gene CAG repeat lengths and neurodegeneration. J. Neurol. 2019, 266, 551–564. [Google Scholar] [CrossRef] [PubMed]
- van Duijn, E.; Kingma, E.M.; van der Mast, R.C. Psychopathology in verified Huntington’s disease gene carriers. J. Neuropsychiatry Clin. Neurosci. 2007, 19, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.C.; Harris, J.; Sollom, A.C.; Stopford, C.L.; Howard, E.; Snowden, J.S.; Craufurd, D. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J. Neuropsychiatry Clin. Neurosci. 2012, 24, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Landwehrmeyer, G.B.; Fitzer-Attas, C.J.; Giuliano, J.D.; Gonçalves, N.; Anderson, K.E.; Cardoso, F.; Ferreira, J.J.; Mestre, T.A.; Stout, J.C.; Sampaio, C. Data Analytics from Enroll-HD, a Global Clinical Research Platform for Huntington’s Disease. Mov. Disord. Clin. Pract. 2017, 4, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, J.; Saft, C.; Faissner, S. Longitudinal Evaluation of the Effect of Tricyclic Antidepressants and Neuroleptics on the Course of Huntington’s Disease—Data from a Real World Cohort. Brain Sci. 2021, 11, 413. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, J.; Saft, C. Data from ENROLL-HD: Is the prevalence of juvenile and pediatric Huntington’s disease overestimated? Park. Relat. Disord. 2021, 88, 1–2. [Google Scholar] [CrossRef]
- Huntington Study Group. Unified Huntington’s Disease Rating Scale: Reliability and consistency. Mov. Disord. 1996, 11, 136–142. [Google Scholar] [CrossRef]
- Shoulson, I.; Fahn, S. Huntington disease: Clinical care and evaluation. Neurology 1979, 29, 1–3. [Google Scholar] [CrossRef]
- Rosenblatt, A.; Kumar, B.V.; Mo, A.; Welsh, C.S.; Margolis, R.L.; Ross, C.A. Age, CAG repeat length, and clinical progression in Huntington’s disease. Mov. Disord. 2012, 27, 272–276. [Google Scholar] [CrossRef]
- Swami, M.; Hendricks, A.E.; Gillis, T.; Massood, T.; Mysore, J.; Myers, R.H.; Wheeler, V.C. Somatic expansion of the Huntington’s disease CAG repeat in the brain is associated with an earlier age of disease onset. Hum. Mol. Genet. 2009, 18, 3039–3047. [Google Scholar] [CrossRef]
- Bassi, S.; Tripathi, T.; Monziani, A.; Di Leva, F.; Biagioli, M. Epigenetics of Huntington’s Disease. Adv. Exp. Med. Biol. 2017, 978, 277–299. [Google Scholar] [PubMed]
- Lee, J.; Hwang, Y.J.; Kim, K.Y.; Kowall, N.W.; Ryu, H. Epigenetic mechanisms of neurodegeneration in Huntington’s disease. Neurotherapeutics 2013, 10, 664–676. [Google Scholar] [CrossRef] [PubMed]
- Alcalá-Vida, R.; Seguin, J.; Lotz, C.; Molitor, A.M.; Irastorza-Azcarate, I.; Awada, A.; Karasu, N.; Bombardier, A.; Cosquer, B.; Skarmeta, J.L.G.; et al. Age-related and disease locus-specific mechanisms contribute to early remodelling of chromatin structure in Huntington’s disease mice. Nat. Commun. 2021, 12, 364. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.A.; van der Burg, J.M.M.; Tabrizi, S.J.; Landwehrmeyer, G.B. Overlap between age-at-onset and disease-progression determinants in Huntington disease. Neurology 2018, 90, e2099–e2106. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.; Houlden, H.; Tabrizi, S.J. DNA repair in the trinucleotide repeat disorders. Lancet Neurol. 2017, 16, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Jonson, I.; Ougland, R.; Larsen, E. DNA Repair Mechanisms in Huntington’s Disease. Mol. Neurobiol. 2013, 47, 1093–1102. [Google Scholar] [CrossRef] [PubMed]
- Pinto, R.M.; Arning, L.; Giordano, J.V.; Razghandi, P.; Andrew, M.A.; Gillis, T.; Correia, K.; Mysore, J.S.; Urtubey, D.-M.G.; Parwez, C.R.; et al. Patterns of CAG repeat instability in the central nervous system and periphery in Huntington’s disease and in spinocerebellar ataxia type 1. Hum. Mol. Genet. 2020, 29, 2551–2567. [Google Scholar] [CrossRef]
- Fusilli, C.; Migliore, S.; Mazza, T.; Consoli, F.; de Luca, A.; Barbagallo, G.; Ciammola, A.; Gatto, E.M.; Cesarini, M.; Etcheverry, J.L.; et al. Biological and clinical manifestations of juvenile Huntington’s disease: A retrospective analysis. Lancet Neurol. 2018, 17, 986–993. [Google Scholar] [CrossRef]
- Epping, E.A.; Kim, J.-I.; Craufurd, D.; Brashers-Krug, T.M.; Anderson, K.E.; McCusker, E.; Luther, J.; Long, J.D.; Paulsen, J.S. Longitudinal Psychiatric Symptoms in Prodromal Huntington’s Disease: A Decade of Data. Am. J. Psychiatry 2016, 173, 184–192. [Google Scholar] [CrossRef]
- Achenbach, J.; Saft, C. Another Perspective on Huntington’s Disease: Disease Burden in Family Members and Pre-Manifest HD When Compared to Genotype-Negative Participants from ENROLL-HD. Brain Sci. 2021, 11, 1621. [Google Scholar] [CrossRef]
- Tabrizi, S.J.; Schobel, S.; Gantman, E.C.; Mansbach, A.; Borowsky, B.; Konstantinova, P.; Mestre, T.A.; Panagoulias, J.; Ross, C.A.; Zauderer, M.; et al. A biological classification of Huntington’s disease: The Integrated Staging System. Lancet Neurol. 2022, 21, 632–644. [Google Scholar] [CrossRef] [PubMed]

| HD Stage 1 n = 3319 | HD Stage 2 n = 3580 | HD Stage 3 n = 2296 | HD Stage 4 n = 809 | HD Stage 5 n = 310 | F | p | Part. Eta2 | |
|---|---|---|---|---|---|---|---|---|
| Age (y); M (SD) | 50.30 (11.95) | 52.86 (12.49) | 54.48 (12.82) | 56.53 (12.85) | 58.17 (13.95) | 68.93 | <0.001 | 0.026 |
| CAG; M(SD) | 43.73 (3.43) | 43.92 (3.87) | 44.40 (4.31) | 44.69 (4.37) | 45.63 (4.55) | 33.27 | <0.001 | 0.013 |
| Sex (f/m) (%f) | 1513/1806 (45.6) | 1891/1689 (52.8) | 1249/1047 (54.4) | 465/344 (57.5) | 183/127 (59.0) | 75.27 | <0.001 | 0.004 |
| ISCED; M (SD) | 3.67 (1.19) | 3.43 (1.20) | 3.21 (1.25) | 2.97 (1.24) | 2.84 (1.29) | 93.97 | <0.001 | 0.035 |
| CAP-Score; M (SD) | 475.53 (78.31) | 507.03 (87.63) | 548.37 (92.99) | 587.65 (98.79) | 632.34 (128.66) | 523.96 | <0.001 | 0.169 |
| Disease duration (y); M (SD) | 4.90 (6.33) | 6.75 (5.62) | 9.18 (6.69) | 12.87 (8.76) | 19.19 (14.45) | 522.51 | <0.001 | 0.169 |
| HD Diagnosis (y); M (SD) | 48.68 (12.09) | 49.63 (12.75) | 49.41 (13.22) | 48.39 (13.77) | 46.14 (13.17) | 6.97 | <0.001 | 0.003 |
| Motor Onset (y); M (SD) | 46.29 (11.79) | 46.77 (12.27) | 46.31 (12.78) | 45.15 (13.43) | 42.10 (12.94) | 10.91 | <0.001 | 0.004 |
| TMS; M (SD) # | 23.84 (11.31) | 35.62 (14.00) | 50.51 (17.10) | 69.54 (17.33) | 85.82 (16.24) | 3056.04 | <0.001 | 0.544 |
| SDMT + | 30.49 (11.01) (n = 3278) | 22.19 (9.5) (n = 3470) | 14.32 (8.91) (n = 1959) | 5.45 (6.60) (n = 510) | 0.97 (3.16) (n = 156) | 1458.27 | <0.001 | 0.384 |
| VFc + | 15.29 (5.20) (n = 3286) | 12.12 (4.66) (n = 3537) | 8.73 (4.31) (n = 2225) | 5.32 (3.57) (n = 680) | 1.77 (2.65) (n = 189) | 124.97 | <0.001 | 0.334 |
| SCNT + | 51.93 (14.10) (n = 3272) | 42.02 (13.67) (n = 3512) | 30.96 (13.37) (n = 2172) | 18.82 (12.85) (n = 638) | 5.94 (9.92) (n = 184) | 1549.98 | <0.001 | 0.388 |
| SWRT + | 69.91 (18.30) (n = 3281) | 55.51 (17.61) (n = 3497) | 41.27 (17.92) (n = 2140) | 24.39 (17.44) (n = 626) | 6.79 (12.31) (n = 181) | 1682.56 | <0.001 | 0.409 |
| SIT + | 28.92 (10.04) (n = 3038) | 22.82 (9.70) (n = 3128) | 15.96 (9.10) (n = 1721) | 9.29 (7.76) (n = 423) | 4.07 (6.65) (n = 74) | 808.67 | <0.001 | 0.279 |
| HD Stage 1 n = 3319 | HD Stage 2 n = 3580 | HD Stage 3 n = 2296 | HD Stage 4 n = 809 | HD Stage 5 n = 310 | F | p | Part. Eta2 | |
|---|---|---|---|---|---|---|---|---|
| Clinical rater (PBA-s) | ||||||||
| Depression; M (SD) # | 4.63 (5.81) (n = 3315) | 5.66 (6.65) (n = 3571) | 5.51 (6.90) (n = 2278) | 5.05 (6.30) (n = 775) | 4.53 (5.77) (n = 205) | 13.241 | <0.001 | 0.005 |
| Irritability; M (SD) # | 2.62 (3.99) | 3.40 (4.82) | 3.83 (5.63) | 4.53 (6.42) | 5.04 (6.65) | 42.44 | <0.001 | 0.016 |
| Psychosis; M (SD) # | 0.14 (1.10) | 0.31 (1.61) | 0.50 (2.22) | 0.86 (3.21) | 0.61 (2.03) | 31.74 | <0.001 | 0.012 |
| Apathy; M (SD) # | 1.76 (3.03) | 3.24 (3.93) | 5.12 (4.96) | 6.71 (5.86) | 8.11 (6.47) | 411.00 | <0.001 | 0.139 |
| Executive function; M (SD) # | 1.97 (3.76) | 3.33 (5.04) | 5.01 (6.25) | 6.69 (7.41) | 5.84 (7.04) | 199.82 | <0.001 | 0.073 |
| Self-report (HADS-IS) | ||||||||
| Anxiety; M (SD) # | 5.76 (4.08) (n = 2055) | 6.20 (4.31) (n = 2116) | 6.09 (4.31) (n = 1093) | 6.12 (4.34) (n = 269) | 5.84 (4.54) (n = 46) | 3.00 | 0.018 | 0.002 |
| Depression; M (SD) # | 4.95 (3.78) | 6.38 (4.05) | 7.30 (4.39) | 8.32 (4.92) | 9.22 (4.75) | 93.28 | <0.001 | 0.063 |
| Irritability; M (SD) # | 5.77 (4.39) | 6.24 (4.76) | 5.95 (4.73) | 5.62 (4.62) | 5.42 (4.01) | 3.31 | <0.001 | 0.002 |
| Outward irritability; M (SD) # | 3.47 (2.64) | 3.73 (2.88) | 3.65 (2.94) | 3.58 (3.08) | 3.43 (2.60) | 2.45 | 0.044 | 0.002 |
| Inward irritability; M (SD) # | 2.31 (2.35) | 2.51 (2.54) | 2.31 (2.58) | 2.06 (2.39) | 2.07 (2.24) | 3.30 | 0.011 | 0.002 |
| Post Hoc Tukey-HSD | HD Stage Comparison | p | |
|---|---|---|---|
| PBA-Depression # | Stage 1 | Stage 2 | <0.001 |
| Stage 3 | <0.001 | ||
| PBA-Irritability # | Stage 1 | Stage 2 | <0.001 |
| Stage 3 | <0.001 | ||
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 2 | Stage 3 | 0.009 | |
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 3 | Stage 4 | <0.001 | |
| Stage 5 | <0.005 | ||
| PBA-Psychosis # | Stage 1 | Stage 2 | <0.005 |
| Stage 3 | <0.001 | ||
| Stage 4 | <0.001 | ||
| Stage 5 | <0.005 | ||
| Stage 2 | Stage 3 | <0.005 | |
| Stage 4 | <0.001 | ||
| Stage 3 | Stage 4 | <0.001 | |
| PBA-Apathy # | Stage 1 | Stage 2 | <0.001 |
| Stage 3 | <0.001 | ||
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 2 | Stage 3 | <0.001 | |
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 3 | Stage 4 | <0.001 | |
| Stage 5 | <0.001 | ||
| Stage 4 | Stage 5 | <0.001 | |
| PBA-Executive function # | Stage 1 | Stage 2 | <0.001 |
| Stage 3 | <0.001 | ||
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 2 | Stage 3 | <0.001 | |
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 3 | Stage 4 | <0.001 | |
| HADS-Anxiety # | Stage 1 | Stage 2 | <0.050 |
| HADS-Depression # | Stage 1 | Stage 2 | <0.001 |
| Stage 3 | <0.001 | ||
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 2 | Stage 3 | <0.001 | |
| Stage 4 | <0.001 | ||
| Stage 5 | <0.001 | ||
| Stage 3 | Stage 4 | <0.005 | |
| Stage 5 | <0.050 | ||
| HADS-Irritability # | Stage 1 | Stage 2 | <0.050 |
| HADS-Outward irritability # | Stage 1 | Stage 2 | <0.050 |
| Stage 4 | <0.050 | ||
| Years to Calculated Onset | <5 y n = 138 | 5–<10 y n = 1242 | 10–<15 y n = 1215 | 15–<20 y n = 920 | >20 y n = 1634 | F | p | Part. Eta2 |
|---|---|---|---|---|---|---|---|---|
| Years to onset M (SD) | 4.43 (0.47) | 7.71 (1.40) | 12.44 (1.43) | 17.33 (1.43) | 29.00 (8.60) | 3938.84 | <0.001 | 0.754 |
| TFC; M (SD) + | 12.51 (0.97) | 12.54 (1.01) | 12.70 (0.97) | 12.78 (0.90) | 12.85 (0.74) | 22.01 | <0.001 | 0.017 |
| Age (y); M (SD) | 44.61 (9.35) | 46.78 (12.17) | 41.54 (11.98) | 32.22 (10.30) | 33.76 (9.73) | 267.16 | <0.001 | 0.172 |
| CAG; M(SD) | 46.38 (2.94) | 43.55 (2.95) | 42.96 (2.73) | 42.24 (2.11) | 40.76 (1.94) | 256.36 | <0.001 | 0.217 |
| Sex (f/m) (%f) | 70/68 (50.7) | 177/509 (59.0) | 705/510 (58.0) | 591/329 (64.2) | 987/647 (60.4) | 14.40 | <0.010 | 0.006 |
| ISCED | 3.93 (1.16) | 3.83 (1.16) | 3.91 (1.13) | 4.01 (1.09) | 4.06 (1.08) | 8.68 | <0.001 | 0.007 |
| CAP-Score; M (SD) | 544.19 (55.02) | 430.22 (32.56) | 355.67 (18.36) | 306.94 (16.73) | 226.57 (46.43) | 8164.42 | <0.001 | 0.864 |
| TMS; M (SD) # | 8.52 (8.14) | 5.19 (5.72) | 3.12 (3.83) | 1.92 (3.33) | 1.53 (2.65) | 212.15 | <0.001 | 0.142 |
| SDMT + | 38.67 (11.40) (n = 135) | 43.03 (11.79) (n = 1232) | 48.08 (11.07) (n = 1204) | 51.86 (10.96) (n = 917) | 54.36 (10.83) (n = 1627) | 226.91 | <0.001 | 0.151 |
| VFc + | 17.86 (5.39) (n = 134) | 19.44 (5.69) (n = 1235) | 21.00 (5.51) (n = 1201) | 22.08 (5.64) (n = 914) | 22.38 (5.65) (n = 1625) | 66.045 | <0.001 | 0.049 |
| SCNT + | 60.49 (15.00) (n = 136) | 66.50 (14.52) (n = 1230) | 71.84 (14.21) (n = 1199) | 74.29 (14.02) (n = 912) | 77.09 (13.96) (n = 1625) | 125.97 | <0.001 | 0.090 |
| SWRT + | 77.78 (16.96) (n = 135) | 85.84 (19.05) (n = 1232) | 92.44 (17.14) (n = 1200) | 95.59 (17.67) (n = 913) | 97.76 (17.16) (n = 1626) | 108.47 | <0.001 | 0.078 |
| SIT + | 35.88 (11.18) (n = 128) | 38.26 (10.92) (n = 1161) | 42.64 (10.88) (n = 1133) | 44.84 (10.65) (n = 856) | 46.32 (10.68) (n = 1547) | 113.06 | <0.001 | 0.086 |
| Clinical rater (PBA-s) | ||||||||
| Depression; M (SD) # | 3.91 (5.90) (n = 137) | 4.84 (6.40) (n = 1238) | 4.44 (5.87) (n = 1213) | 4.46 (5.85) (n = 917) | 3.80 (5.27) (n = 1627) | 6.148 | <0.001 | 0.005 |
| Irritability; M (SD) # | 1.78 (3.65) | 2.20 (4.03) | 2.18 (3.75) | 1.83 (3.25) | 1.84 (3.25) | 3.18 | <0.050 | 0.002 |
| Psychosis; M (SD) # | 0.04 (0.38) | 0.17 (1.51) | 0.15 (1.05) | 0.11 (0.88) | 0.09 (0.78) | 1.58 | 0.177 | 0.001 |
| Apathy; M (SD) # | 1.00 (2.28) | 1.27 (2.74) | 1.05 (2.47) | 0.94 (2.39) | 0.74 (1.96) | 9.05 | <0.001 | 0.007 |
| Executive function; M (SD) # | 0.92 (2.46) | 1.35 (3.28) | 1.37 3.18) | 1.27 (3.25) | 1.20 (3.00) | 1.11 | 0.350 | 0.001 |
| Self-report (HADS-IS) | ||||||||
| Anxiety; M (SD) # | 5.35 (3.90) (n = 82) | 5.54 (3.94) (n = 804) | 5.68 (4.00) (n = 837) | 5.91 (4.22) (n = 641) | 5.47 (3.94) (n = 1179) | 1.47 | 0.208 | 0.002 |
| Depression; M (SD) # | 3.61 (3.65) | 4.09 (3.66) | 3.82 (3.60) | 3.72 (3.71) | 3.01 (3.12) | 13.48 | <0.001 | 0.015 |
| Irritability; M (SD) # | 5.38 (4.11) | 5.32 (4.15) | 5.18 (4.02) | 5.17 (4.10) | 4.69 (3.88) | 3.74 | <0.010 | 0.004 |
| Outward irritability; M (SD) # | 3.39 (2.69) | 3.37 (2.52) | 3.31 (2.56) | 3.13 (2.43) | 2.96 (2.43) | 4.17 | <0.010 | 0.005 |
| Inward irritability; M (SD) # | 1.99 (2.02) | 1.96 (2.20) | 1.86 (2.06) | 2.05 (2.35) | 1.73 (2.05) | 2.80 | <0.050 | 0.003 |
| Post Hoc Tukey-HSD | Pre-Manifest HD Comparisons | p | |
|---|---|---|---|
| <5 y | 15–<20 y | <0.050 | |
| >20 y | <0.001 | ||
| 5–<10 y | 10–<15 y | <0.001 | |
| 15–<20 y | <0.001 | ||
| >20 y | <0.001 | ||
| 10–<15 y | >20 y | <0.001 | |
| PBA-Depression # | 5–<10 y | >20 y | <0.001 |
| 10–<15 y | >20 y | <0.050 | |
| 15–<20 y | >20 y | <0.050 | |
| PBA-Apathy # | 5–<10 y | 15–<20 y | <0.050 |
| >20 y | <0.001 | ||
| 10–<15 y | >20 y | <0.010 | |
| HADS-Depression # | 5–<10 y | >20 y | <0.001 |
| 10–<15 y | >20 y | <0.001 | |
| 15–<20 y | >20 y | <0.001 | |
| HADS-Irritability # | 5–<10 y | >20 y | <0.010 |
| HADS-Outward irritability # | 5–<10 y | >20 y | <0.005 |
| 10–<15 y | >20 y | <0.050 | |
| HADS-Inward irritability # | 15–<20 y | >20 y | <0.050 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Achenbach, J.; Stodt, B.; Saft, C. Factors Influencing the Total Functional Capacity Score as a Critical Endpoint in Huntington’s Disease Research. Biomedicines 2023, 11, 3336. https://doi.org/10.3390/biomedicines11123336
Achenbach J, Stodt B, Saft C. Factors Influencing the Total Functional Capacity Score as a Critical Endpoint in Huntington’s Disease Research. Biomedicines. 2023; 11(12):3336. https://doi.org/10.3390/biomedicines11123336
Chicago/Turabian StyleAchenbach, Jannis, Benjamin Stodt, and Carsten Saft. 2023. "Factors Influencing the Total Functional Capacity Score as a Critical Endpoint in Huntington’s Disease Research" Biomedicines 11, no. 12: 3336. https://doi.org/10.3390/biomedicines11123336







