Stress Coping Strategies in Parents of Newborns and Infants with Congenital Cyanotic Heart Disease with Regard to Stress Levels and Negative Emotions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
- What is the relationship between parents’ stress levels and anxiety, depression, irritability, and selected sociodemographic and clinical variables (time of defect diagnosis and stage of cardiac surgery treatment)?
- What stress coping strategies do parents choose depending on their gender and age?
- What is the relationship between parents’ choice of coping strategies and the level of stress and other variables studied?
2.2. Sample, Setting, and Data Collection
2.3. Participants and Involvement
2.4. Description of Research Tools
- -
- Self-designed questionnaire, including sociodemographic data of parents and selected clinical variables relating to children [10].
- -
- -
- -
- Coping Orientation to Problems Experienced (COPE) [25,26]. The COPE questionnaire includes 60 statements related to 15 strategies for responding to/coping with stressful situations and is based on Lazarus and Folkmans’ transactional model of stress Carver et al. [26]. The scale can determine someone’s primary coping styles with scores on the following three subscales: I. Problem-Focused Coping; II. Emotion-Focused Coping; III. Avoidant Coping [27]. The tool makes it possible to assess, based on dispositional coping, which of the given strategies are most often used in a stressful situation. The analysis of the responses given by the participants of the survey followed the key developed by the authors of the scale [25,26] and the study by Dias et al. [27]. In summary, a score (ranging from 4 to 16) was calculated for each of the 15 strategies as the sum of the 4 component statements. Then, the coping strategies thus obtained were grouped into 3 main subscales consisting of 5, 6, and 4 of the 15 strategies, respectively, and score values were summed within these groups. In addition, for the purpose of data analysis, each of the 15 strategies and the 3 main subscales were divided into high-level and low-level categories, with a cutoff point in the second tertile of the distribution of each variable.
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Group
3.2. Parents’ Coping with Stress by Gender, Age and Stress Level
3.3. Coping with Stress and Selected Sociodemographic and Clinical Variables
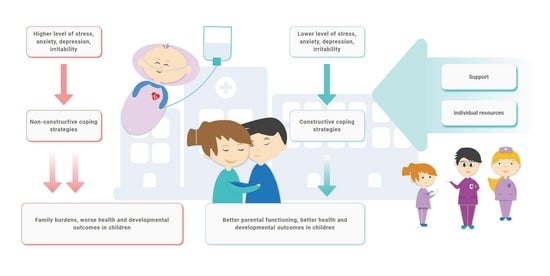
4. Discussion
4.1. Implications
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rozkrut, D. Statistical Yearbook of the Republic of Poland 2022; Statistics Poland: Warsaw, Poland, 2022; p. 221.
- Wu, W.; He, J.; Shao, X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990–2017. Medicine 2020, 99, e20593. [Google Scholar] [CrossRef] [PubMed]
- Varela-Chinchilla, C.D.; Sánchez-Mejía, D.E.; Trinidad-Calderón, P.A. Congenital heart disease: The State-of-the-Art on its pharmacological therapeutics. J. Cardiovasc. Dev. Dis. 2022, 26, 201. [Google Scholar] [CrossRef] [PubMed]
- Mandalenakis, Z.; Giang, K.W.; Eriksson, P.; Liden, H.; Synnergren, M.; Wåhlander, H.; Fedchenko, M.; Rosengren, A.; Dellborg, M. Survival in children with congenital heart disease: Have we reached a peak at 97%? J. Am. Heart Assoc. 2020, 9, e017704. [Google Scholar] [CrossRef] [PubMed]
- Cloete, E.; Bloomfield, F.H.; Sadler, L.; de Laat, M.W.M.; Finucane, A.K.; Gentles, T.L. Antenatal detection of treatable critical congenital heart disease is associated with lower morbidity and mortality. J. Pediatr. 2019, 204, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Ahn, J.A. Experiences of mothers facing the prognosis of their children with complex congenital heart disease. Int. J. Environ. Res. Public Health 2020, 17, 7134. [Google Scholar] [CrossRef] [PubMed]
- Dalir, Z.; Heydari, A.; Kareshki, H.; Manzari, Z.S. Coping with caregiving stress in families of children with congenital heart disease: A qualitative study. Int. J. Community Based Nurs. Midwifery 2020, 8, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Nayeri, N.D.; Roddehghan, Z.; Mahmoodi, F.; Mahmoodi, P. Being parent of a child with congenital heart disease, what does it mean? A qualitative research. BMC Psychol. 2021, 9, 33. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.D.; Kazazian, V.; Ford, M.K.; Marii, D.; Millera, S.P.; Chau, V.; Seed, M.; Ly, L.G.; Williams, T.S.; Sananes, R. The association between parent stress, coping and mental health, and neurodevelopmental outcomes of infants with congenital heart disease. Clin. Neuropsychol. 2021, 35, 948–972. [Google Scholar] [CrossRef] [PubMed]
- Cepuch, G.; Kruszecka-Krówka, A.; Lalik, A.; Micek, A. Toxic stress as a potential factor inducing negative emotions in parents of newborns and infants with cyanotic congenital heart disease. Children 2023, 10, 1893. [Google Scholar] [CrossRef]
- Bishop, M.; Cohen, L.L.; Robbertz, A.S. Illness-related parenting stress and maladjustment in congenital heart disease: Mindfulness as a moderator. J. Pediatr. Psychol. 2020, 45, 1208–1215. [Google Scholar] [CrossRef]
- Golfenshtein, N.; Hanlon, A.L.; Deatrick, J.A.; Medoff-Cooper, B. Parenting stress trajectories during infancy in infants with congenital heart disease: Comparison of single-ventricle and biventricular heart physiology. Congenit. Heart Dis. 2019, 14, 1113–1122. [Google Scholar] [CrossRef]
- Lumsden, M.R.; Smith, D.M.; Twigg, E.; Guerrero, R.; Wittkowski, A. Children with single ventricle congenital heart defects: An interpretative phenomenological analysis of the lived parent experience. Prog. Pediatr. Cardiol. 2020, 59, 101297. [Google Scholar] [CrossRef]
- McMahon, E.; Chang, Y.S. From surviving to thriving—Parental experiences of hospitalised infants with congenital heart disease undergoing cardiac surgery: A qualitative synthesis. J. Pediatr. Nurs. 2020, 51, 32–41. [Google Scholar] [CrossRef]
- Lazarus, R.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984; p. 30. [Google Scholar]
- Skalski, S. Choroba jako źródło stresu. Wybrane koncepcje stresu psychologicznego i radzenia sobie ze stresem. In Humanistyka i Nauki Społeczne. Doświadczenia, Konteksty, Wyzwania; Pujer, K., Ed.; Exante: Wrocław, Poland, 2018; pp. 11–22. [Google Scholar]
- Endler, N.S.; Parker, J.D.A. Assessment of multidimensional coping: Task, emotion and avoidance strategies. Psychol. Assess. 1994, 6, 50–60. [Google Scholar] [CrossRef]
- Endler, N.S.; Parker, J.D.A. Multidimensional assessment of coping: A critical evaluation. J. Person. Soc. Psychol. 1990, 58, 844–854. [Google Scholar] [CrossRef]
- Pietrzyk, A.; Pilarz, M.; Lizińczyk, S. Resilience and coping with stress and marital relationships of the parents of children with leukaemia. Psychoonkologia 2018, 22, 77–89. [Google Scholar] [CrossRef]
- Schaefer, J.A.; Moos, R.H. The context for posttraumatic growth: Life crises, individual and social resources, and coping. In Posttraumatic Growth: Positive Changes in the Aftermath of Crisis; Routledge: Abingdon, UK, 1998; p. 126. ISBN 9781410603401. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Majkowicz, M. Praktyczna ocena efektywności opieki paliatywnej—Wybrane techniki badawcze. In Ocena Jakości Opieki Paliatywnej Teorii i Praktyce; de Walden-Gałuszko, K., Majkowicz, M., Eds.; Akademia Medyczna Gdańsk, Zakład Medycyny Paliatywnej: Gdańsk, Poland, 2000; pp. 21–42. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Narzędzia Pomiaru Stresu i Radzenia Sobie ze Stresem; Pracownia Testów Psychologicznych: Warszawa, Poland, 2009; pp. 59–70. [Google Scholar]
- Carver, C.; Scheier, M.; Weintraub, J. Assessing coping strategies: A theoretically based approach. J. Pers. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Dias, C.; Cruz, J.F.; Fonseca, A.M. The relationship between multidimensional competitive anxiety, cognitive threat appraisal, and coping strategies: A multi-sport study. Int. J. Sport Exerc. Psychol. 2012, 10, 52–65. [Google Scholar] [CrossRef]
- Bratt, E.L.; Järvholm, S.; Ekman-Joelsson, B.M.; Johannsmeyer, A.; Carlsson, S.Å.; Mattsson, L.Å.; Mellander, M. Parental reactions, distress, and sense of coherence after prenatal versus postnatal diagnosis of complex congenital heart disease. Cardiol. Young 2019, 29, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Lisanti, A.J.; Allen, L.R.; Kelly, L.; Medoff-Cooper, B. Maternal stress and anxiety in the pediatric cardiac intensive care unit. Am. J. Crit. Care. 2017, 26, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Mussatto, K.A.; Van Rompay, M.I.; Trachtenberg, F.L.; Pemberton, V.; Young-Borkowski, L.; Uzark, K.; Hollenbeck-Pringle, D.; Dunbar-Masterson, C.; Infinger, P.; Walter, P.; et al. Family function, quality of life, and well-being in parents of infants with hypoplastic left heart syndrome. J. Fam. Nurs. 2021, 27, 222–234. [Google Scholar] [CrossRef] [PubMed]
- Joos, C.M.; McDonald, A.; Wadsworth, M.E. Extending the toxic stress model into adolescence: Profiles of cortisol reactivity. Psychoneuroendocrinology 2019, 107, 46–58. [Google Scholar] [CrossRef] [PubMed]
- McCrae, J.S.; Robinson, J.A.L.; Spain, A.K.; Byers, K.; Axelrod, J.L. The Mitigating Toxic Stress study design: Approaches to developmental evaluation of pediatric health care innovations addressing social determinants of health and toxic stress. BMC Health Serv. Res. 2021, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Condon, E.M.; Londono Tobon, A.; Jackson, B.; Holland, M.L.; Slade, A.; Mayes, L.; Sadler, L.S. Maternal experiences of racial discrimination, child indicators of toxic stress, and the minding the baby early home visiting intervention. Nurs. Res. 2021, 70, S43–S52. [Google Scholar] [CrossRef]
- Condon, E.M.; Sadler, L.S. Toxic stress and vulnerable mothers: A multilevel framework of stressors and strengths. West J. Nurs. Res. 2019, 41, 872–900. [Google Scholar] [CrossRef]
- Ribaudo, J.; Lawler, J.M.; Jester, J.M.; Riggs, J.; Erickson, N.L.; Stacks, A.M.; Brophy-Herb, H.; Muzik, M.; Rosenblum, K.L. Maternal history of adverse experiences and posttraumatic stress disorder symptoms impact toddlers’ early socioemotional wellbeing: The benefits of infant mental health-home visiting. Front. Psychol. 2022, 12, 792989. [Google Scholar] [CrossRef]
- Woolf-King, S.E.; Anger, A.; Arnold, E.A.; Weiss, S.J.; Teitel, D. Mental health among parents of children with critical congenital heart defects: A systematic review. J. Am. Heart Assoc. 2017, 6, e004862. [Google Scholar] [CrossRef]
- Wu, Y.; Kapse, K.; Jacobs, M.; Niforatos-Andescavage, N.; Donofrio, M.T.; Krishnan, A.; Vezina, G.; Wessel, D.; du Plessis, A.; Limperopoulos, C. Association of maternal psychological distress with in utero brain development in fetuses with congenital heart disease. JAMA Pediatr. 2020, 174, e195316. [Google Scholar] [CrossRef] [PubMed]
- Cantwell-Bartl, A.M.; Tibballs, J. Psychosocial responses of parents to their infant’s diagnosis of hypoplastic left heart syndrome. Cardiol. Young 2015, 25, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Kolaitis, A.; Meentken, M.G.; Utens, E.M.W.J. Mental health problems in parents of children with congenital heart disease gerasimos. Front. Pediatr. 2017, 5, 102. [Google Scholar] [CrossRef] [PubMed]
- Sood, E.; Karpyn, A.; Demianczyk, A.C.; Ryan, J.; Delaplane, E.A.; Neely, T.; Frazier, A.H.; Kazak, A.E. Mothers and fathers experience stress of congenital heart disease differently: Recommendations for pediatric critical care. Pediatr. Crit. Care Med. 2018, 19, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Biber, S.; Andonian, C.; Beckmann, J.; Ewert, P.; Freilinger, S.; Nagdyman, N.; Kaemmerer, H.; Oberhoffer, R.; Pieper, L.; Neidenbach, R.C. Current research status on the psychological situation of parents of children with congenital heart disease. Cardiovasc. Diagn. Ther. 2019, 9, S369–S376. [Google Scholar] [CrossRef] [PubMed]
- McKechnie, A.C.; Elgersma, K.M.; Ambrose, M.B.; Sanchez Mejia, A.; Shah, K.M.; Iwaszko Wagner, T.; Trebilcock, A.; Hallock, C. Nurse-guided mobile health care program to reduce emotional distress experienced by parents of infants prenatally diagnosed with critical congenital heart disease: A pilot study. Prog. Pediatr. Cardiol. 2024, 72, 101687. [Google Scholar] [CrossRef] [PubMed]
- Soulvie, M.A.; Desai, P.P.; White, C.P.; Sullivan, B.N. Psychological distress experienced by parents of young children with congenital heart defects: A comprehensive review of literature. J. Soc. Serv. Res. 2012, 38, 484–502. [Google Scholar] [CrossRef]
- Brosig, C.L.; Whitstone, B.N.; Frommelt, M.A.; Frisbee, S.J.; Leuthner, S.R. Psychological distress in parents of children with severe congenital heart disease: The impact of prenatal versus postnatal diagnosis. J. Perinatol. 2007, 27, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Lee, S. Coping self-efficacy and parenting stress in mothers of children with congenital heart disease. Heart Lung 2021, 50, 352–356. [Google Scholar] [CrossRef]
- Jackson, A.C.; Frydenberg, E.; Koey, X.M.; Fernandez, A.; Higgins, R.O.; Stanley, T.; Liang, R.P.-T.; Le Grande, M.R.; Murphy, B.M. Enhancing parental coping with a child’s heart condition: A co-production pilot study. Compr. Child Adolesc. Nurs. 2020, 43, 314–333. [Google Scholar] [CrossRef]
- Miller, V.A.; Newcombe, J.; Radovich, P.; Johnston, F.; Medina, E.; Nelson, A. The healing hearts at home© mobile application usability and influence on parental perceived stress: A pilot study. IJEHMC 2021, 12, 90–105. [Google Scholar] [CrossRef]
- Dardas, L.A.; Ahmad, M.M. Coping strategies as mediators and moderators between stress and quality of life among parents of children with autistic disorder. Stress Health 2015, 31, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Poh, P.-F.; Lee, J.H.; Loh, Y.J.; Tan, T.H.; Cheng, K.K.F. Readiness for hospital discharge, stress, and coping in mothers of children undergoing cardiac surgeries: A single-center prospective study. Pediatr. Crit. Care Med. 2020, 21, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Fairfax, A.; Brehaut, J.; Colman, I.; Sikora, L.; Kazakova, A.; Chakraborty, P.; Potter, B.K. Canadian inherited metabolic diseases research network. A systematic review of the association between coping strategies and quality of life among caregivers of children with chronic illness and/or disability. BMC Pediatr. 2019, 19, 215. [Google Scholar] [CrossRef] [PubMed]
- Eagleson, K.J.; McCombs, D.; Gerlich, T.M.; Justo, R.N.; Kasparian, N.A.; Bora, S. Systematic review of instruments assessing psychosocial adaptation and outcomes among families of children with congenital heart disease. J. Pediatr. Psychol. 2023, 48, 537–552. [Google Scholar] [CrossRef]
- Wie, H.; Roscigno, C.I.; Hanson, C.C.; Swanson, K.M. Families of children with congenital heart disease: A literature review. Heart Lung 2015, 44, 494–511. [Google Scholar] [CrossRef]
- Kasparian, N.A.; Kovacs, A.H. Quality of life and other patient-reported outcomes across the life span among people with Fontan palliation. Can. J. Cardiol. 2022, 38, 963–976. [Google Scholar] [CrossRef]
- Kasparian, N.A.; Winlaw, D.S.; Sholler, G.F. Congenital heart health: How psychological care can make a difference. Med. J. Aust. 2016, 205, 104–107. [Google Scholar] [CrossRef]

| Variable | PSS | p | |
|---|---|---|---|
| Low/Average (N = 37) | High (N = 117) | ||
| Child’s (clinical) characteristics | |||
| Correction, n (%) | |||
| Full | 5 (13.51) | 19 (16.24) | |
| Partial | 19 (51.35) | 63 (53.85) | 0.814 |
| No correction | 13 (35.14) | 35 (29.91) | |
| Time of defect diagnosis, n (%) | |||
| Prenatal | 27 (72.97) | 84 (71.79) | 1.000 |
| Postnatal | 10 (27.03) | 33 (28.21) | |
| Respondent’s (parent’s) characteristics | |||
| Sex, n (%) | |||
| Female | 30 (81.08) | 102 (87.18) | 0.513 |
| Male | 7 (18.92) | 15 (12.82) | |
| Age, mean (SD) | 32.84 (5.03) | 31.74 (4.87) | 0.246 |
| Age, n (%) | |||
| ≤29 | 8 (21.62) | 43 (36.75) | |
| 30–34 | 15 (40.54) | 38 (32.48) | 0.234 |
| ≥35 | 14 (37.84) | 36 (30.77) | |
| Residence, n (%) | |||
| Village | 9 (24.32) | 26 (22.22) | 0.967 |
| City/town | 28 (75.68) | 91 (77.78) | |
| Education, n (%) | |||
| Elementary/vocational/secondary | 23 (62.16) | 51 (43.59) | 0.075 |
| High | 14 (37.84) | 66 (56.41) | |
| HADS D score, mean (SD) | 6.32 (3.59) | 10.6 (2.92) | <0.001 |
| HADS A score, mean (SD) | 10.14 (4.14) | 12.69 (2.93) | 0.001 |
| HADS I score, mean (SD) | 2.7 (1.18) | 3.67 (1.33) | <0.001 |
| Strategies (COPE) | |||
| 1 | 11.81 (1.81) | 11.78 (1.97) | 0.925 |
| 2 | 11.49 (1.66) | 11.68 (2.6) | 0.589 |
| 3 | 11.49 (2.55) | 11.5 (2.88) | 0.985 |
| 4 | 10.76 (3.39) | 10.54 (3.23) | 0.731 |
| 5 | 10.76 (2.22) | 11.28 (1.94) | 0.201 |
| 6 | 11.65 (3.26) | 12.01 (3.46) | 0.566 |
| 7 | 12.08 (2.11) | 10.74 (1.92) | 0.001 |
| 8 | 8.89 (2.2) | 9.41 (1.71) | 0.194 |
| 9 | 11.43 (2.66) | 10.67 (3.05) | 0.146 |
| 10 | 10.03 (2.46) | 12.09 (1.93) | 0.000 |
| 11 | 5.78 (1.34) | 6.56 (1.82) | 0.007 |
| 12 | 8.14 (2.29) | 8.8 (2.54) | 0.137 |
| 13 | 5.57 (1.37) | 6.27 (1.66) | 0.011 |
| 14 | 4.49 (0.87) | 5.03 (1.18) | 0.003 |
| 15 | 6.27 (2.57) | 5.46 (1.5) | 0.076 |
| Subscales (COPE) | |||
| I. | 55.03 (6.13) | 54.9 (5.78) | 0.910 |
| II. | 41.68 (6.88) | 42.79 (5.27) | 0.368 |
| III. | 43.92 (8.4) | 46.13 (7.16) | 0.155 |
| Strategies (COPE) | Gender | p | Age | p | |||
|---|---|---|---|---|---|---|---|
| Female (N = 132) | Male (N = 22) | ≤29 (N = 51) | 30–34 (N = 53) | ≥35 (N = 50) | |||
| 1. | 11.78 (1.85) | 11.82 (2.34) | 0.943 | 11.78 (1.94) | 11.51 (2.12) | 12.08 (1.66) | 0.324 |
| 2. | 11.65 (2.49) | 11.55 (1.84) | 0.815 | 11.14 (2.65) | 11.51 (2.45) | 12.28 (1.94) | 0.050 |
| 3 | 11.79 (2.72) | 9.73 (2.66) | 0.002 | 11.12 (3.2) | 11.79 (2.48) | 11.56 (2.69) | 0.463 |
| 4 | 10.78 (3.25) | 9.45 (3.17) | 0.081 | 11.14 (3.16) | 10.38 (3.18) | 10.26 (3.43) | 0.340 |
| 5 | 11.26 (2.02) | 10.55 (1.92) | 0.121 | 11.04 (2.24) | 10.79 (1.85) | 11.66 (1.87) | 0.080 |
| 6 | 12.03 (3.44) | 11.27 (3.17) | 0.313 | 12.25 (3.01) | 11.92 (3.55) | 11.58 (3.65) | 0.611 |
| 7 | 11.12 (2.08) | 10.73 (1.8) | 0.361 | 10.43 (2.05) | 11.09 (2.12) | 11.68 (1.77) | 0.008 |
| 8 | 9.35 (1.87) | 8.91 (1.66) | 0.268 | 9.35 (1.82) | 9.19 (2.03) | 9.32 (1.68) | 0.892 |
| 9 | 10.91 (2.99) | 10.5 (2.87) | 0.544 | 10.47 (3.26) | 11.13 (2.93) | 10.94 (2.71) | 0.511 |
| 10 | 11.67 (2.21) | 11.14 (2.42) | 0.343 | 12.27 (1.99) | 11.51 (2.31) | 10.98 (2.26) | 0.013 |
| 11 | 6.45 (1.73) | 5.91 (1.8) | 0.202 | 6.53 (1.75) | 6.17 (1.58) | 6.42 (1.91) | 0.560 |
| 12 | 8.69 (2.52) | 8.36 (2.36) | 0.558 | 8.47 (2.63) | 8.64 (2.52) | 8.82 (2.35) | 0.783 |
| 13 | 6.15 (1.66) | 5.82 (1.33) | 0.303 | 6.16 (1.6) | 6.26 (1.56) | 5.88 (1.7) | 0.468 |
| 14 | 4.83 (1.03) | 5.36 (1.59) | 0.138 | 5 (1.08) | 4.91 (1.11) | 4.8 (1.23) | 0.679 |
| 15 | 5.77 (1.91) | 5 (1.2) | 0.016 | 5.33 (1.73) | 6.06 (2.13) | 5.56 (1.54) | 0.121 |
| Subscales (COPE) | |||||||
| I. | 55.16 (5.83) | 53.55 (5.82) | 0.239 | 53.75 (6.01) | 54.09 (6.2) | 57.02 (4.71) | 0.008 |
| II. | 42.79 (5.77) | 40.95 (5.01) | 0.130 | 41.96 (5.68) | 43.17 (5.98) | 42.42 (5.42) | 0.552 |
| III. | 46.27 (7.43) | 41.59 (6.84) | 0.006 | 46.78 (7.31) | 45.6 (7.67) | 44.38 (7.49) | 0.276 |
| COPE | PSS Score | Age |
|---|---|---|
| 1 | 0.109 | 0.071 |
| 2 | 0.052 | 0.157 |
| 3 | −0.036 | 0.078 |
| 4 | −0.110 | −0.108 |
| 5 | 0.062 | 0.141 |
| 6 | −0.020 | −0.022 |
| 7 | −0.199 * | 0.253 ** |
| 8 | −0.065 | 0.021 |
| 9 | −0.265 *** | 0.006 |
| 10 | 0.362 *** | −0.239 ** |
| 11 | 0.213 ** | −0.064 |
| 12 | 0.166 * | 0.038 |
| 13 | 0.033 | −0.120 |
| 14 | 0.263 *** | −0.122 |
| 15 | −0.099 | 0.075 |
| Subscales (COPE) | ||
| I. | −0.056 | 0.247 ** |
| II. | 0.017 | −0.025 |
| III. | −0.030 | −0.120 |
| COPE | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| 1 | 0.82 (0.38; 1.79) | 0.84 (0.39; 1.85) | 0.92 (0.41; 2.11) |
| 2 | 3.16 (1.35; 8.13) * | 3.17 (1.34; 8.25) * | 3.45 (1.43; 9.16) ** |
| 3 | 1.04 (0.48; 2.32) | 1.00 (0.44; 2.31) | 1.00 (0.44; 2.33) |
| 4 | 0.73 (0.34; 1.55) | 0.66 (0.30; 1.42) | 0.67 (0.30; 1.45) |
| 5 | 1.03 (0.49; 2.21) | 0.99 (0.45; 2.16) | 1.01 (0.46; 2.23) |
| 6 | 1.50 (0.69; 3.41) | 1.49 (0.67; 3.43) | 1.45 (0.64; 3.35) |
| 7 | 0.20 (0.08; 0.45) *** | 0.18 (0.07; 0.44) *** | 0.19 (0.07; 0.46) *** |
| 8 | 1.46 (0.69; 3.21) | 1.43 (0.66; 3.19) | 1.37 (0.62; 3.10) |
| 9 | 0.93 (0.44; 2.00) | 0.89 (0.41; 1.94) | 0.94 (0.43; 2.08) |
| 10 | 3.95 (1.59; 11.40) ** | 3.72 (1.48; 10.85) ** | 4.17 (1.61; 12.49) ** |
| 11 | 2.56 (1.14; 6.13) * | 2.49 (1.10; 6.03) * | 2.53 (1.11; 6.17) * |
| 12 | 1.61 (0.73; 3.72) | 1.62 (0.73; 3.77) | 1.59 (0.70; 3.74) |
| 13 | 2.77 (1.20; 7.06) * | 2.74 (1.17; 7.06) * | 2.72 (1.15; 7.09) * |
| 14 | 2.96 (1.35; 6.83) ** | 2.93 (1.31; 6.86) * | 3.36 (1.46; 8.18) ** |
| 15 | 0.89 (0.42; 1.92) | 0.95 (0.43; 2.10) | 1.00 (0.45; 2.27) |
| Subscales (COPE) | |||
| I. | 0.52 (0.24; 1.12) | 0.48 (0.21; 1.08) | 0.47 (0.20; 1.07) |
| II. | 1.41 (0.64; 3.31) | 1.39 (0.61; 3.31) | 1.39 (0.61; 3.33) |
| III. | 1.17 (0.54; 2.61) | 1.04 (0.46; 2.38) | 1.04 (0.46; 2.39) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kruszecka-Krówka, A.; Cepuch, G.; Micek, A. Stress Coping Strategies in Parents of Newborns and Infants with Congenital Cyanotic Heart Disease with Regard to Stress Levels and Negative Emotions. Children 2024, 11, 508. https://doi.org/10.3390/children11050508
Kruszecka-Krówka A, Cepuch G, Micek A. Stress Coping Strategies in Parents of Newborns and Infants with Congenital Cyanotic Heart Disease with Regard to Stress Levels and Negative Emotions. Children. 2024; 11(5):508. https://doi.org/10.3390/children11050508
Chicago/Turabian StyleKruszecka-Krówka, Agnieszka, Grażyna Cepuch, and Agnieszka Micek. 2024. "Stress Coping Strategies in Parents of Newborns and Infants with Congenital Cyanotic Heart Disease with Regard to Stress Levels and Negative Emotions" Children 11, no. 5: 508. https://doi.org/10.3390/children11050508