Osteonecrosis of the Jaw (ONJ) in Osteoporosis Patients: Report of Delayed Diagnosis of a Multisite Case and Commentary about Risks Coming from a Restricted ONJ Definition
Abstract
:1. Introduction
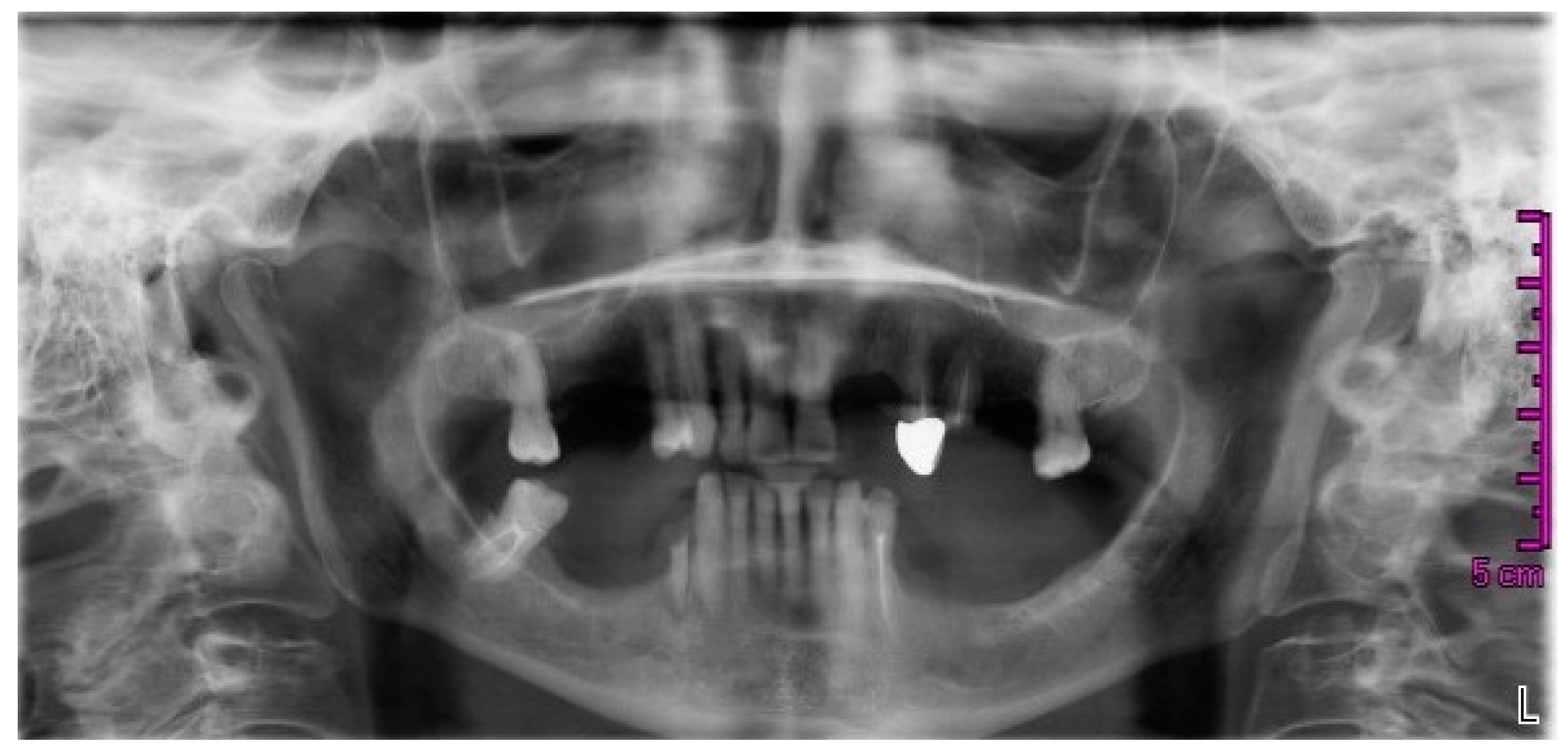
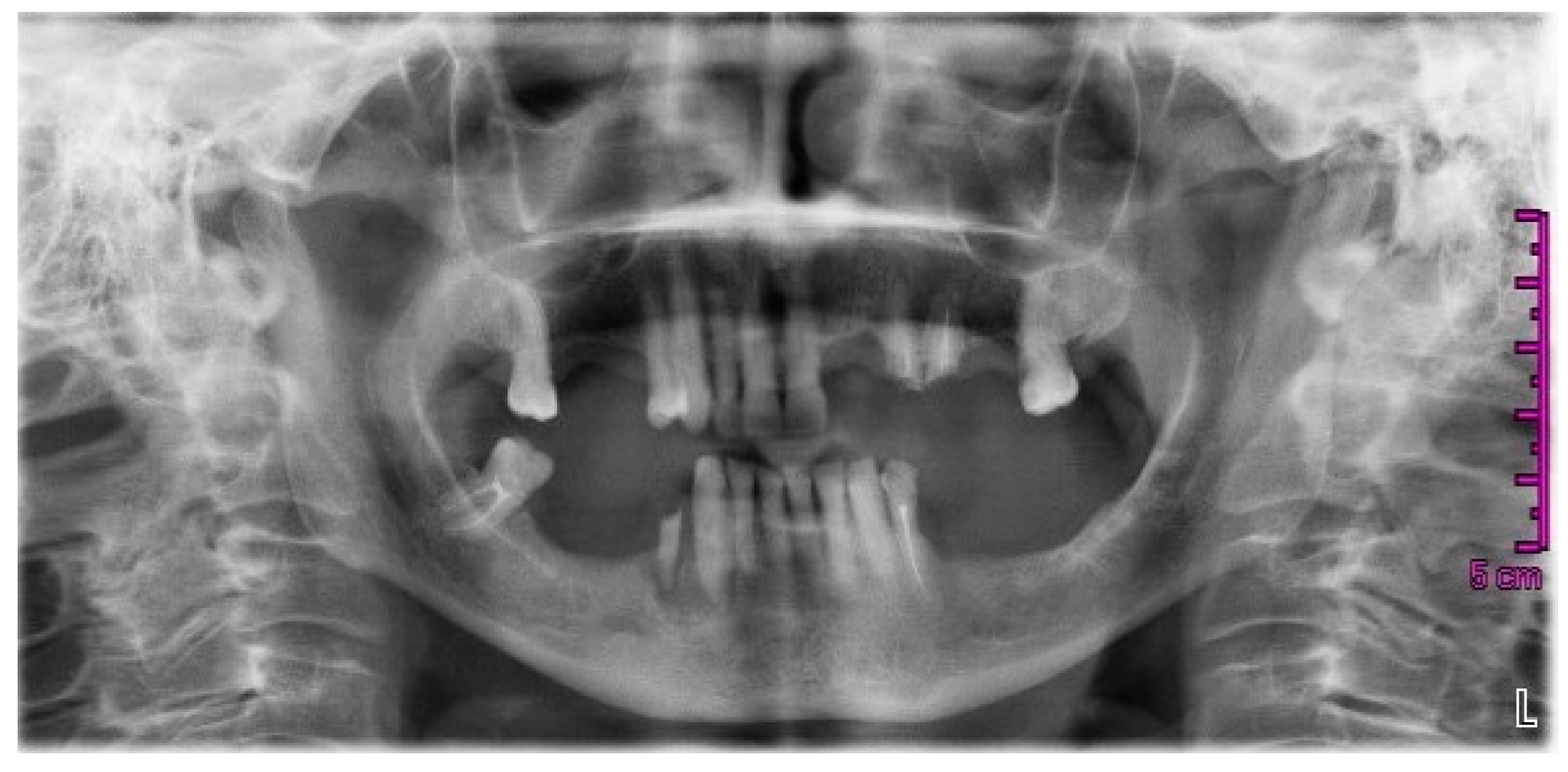
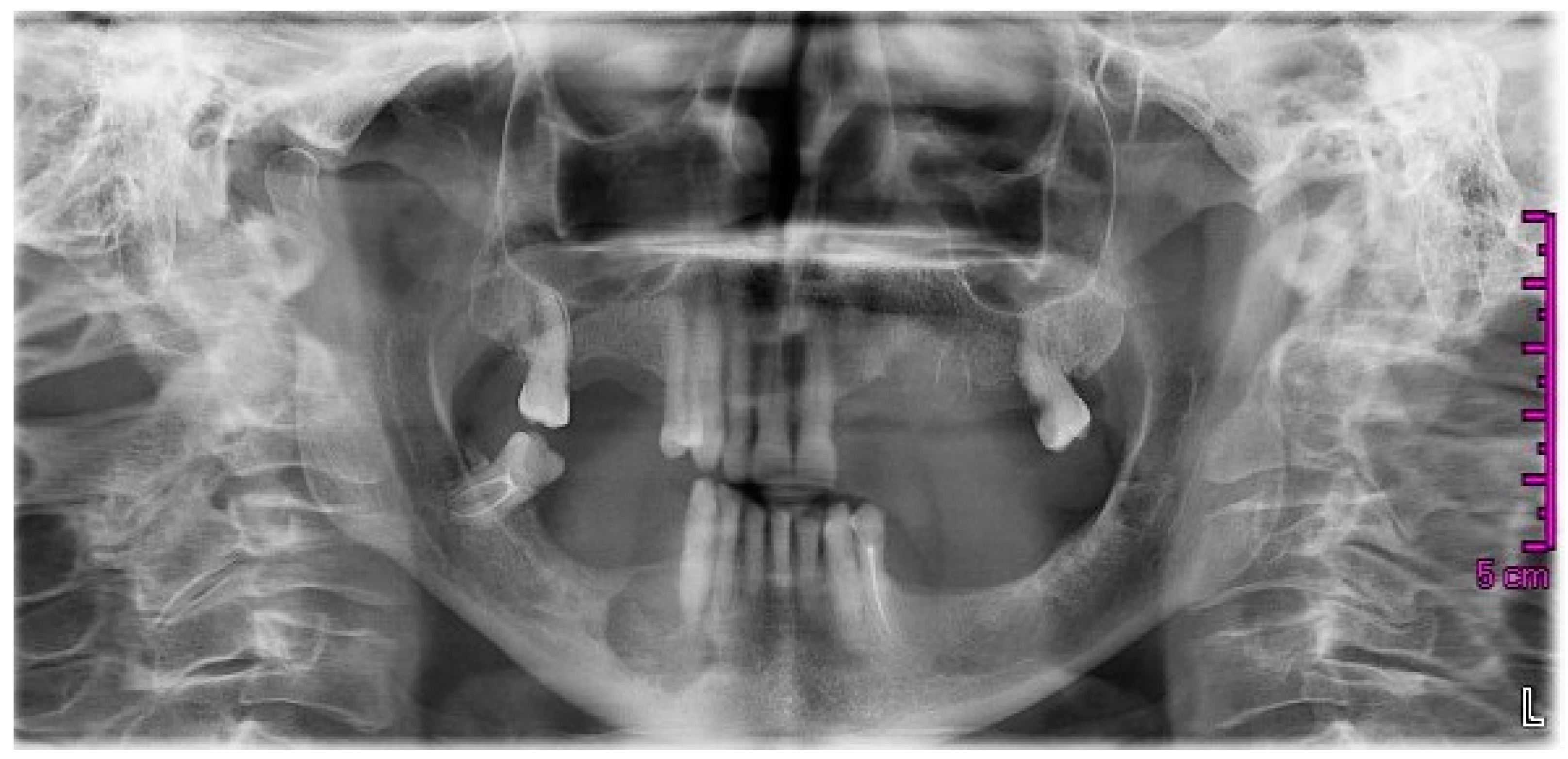
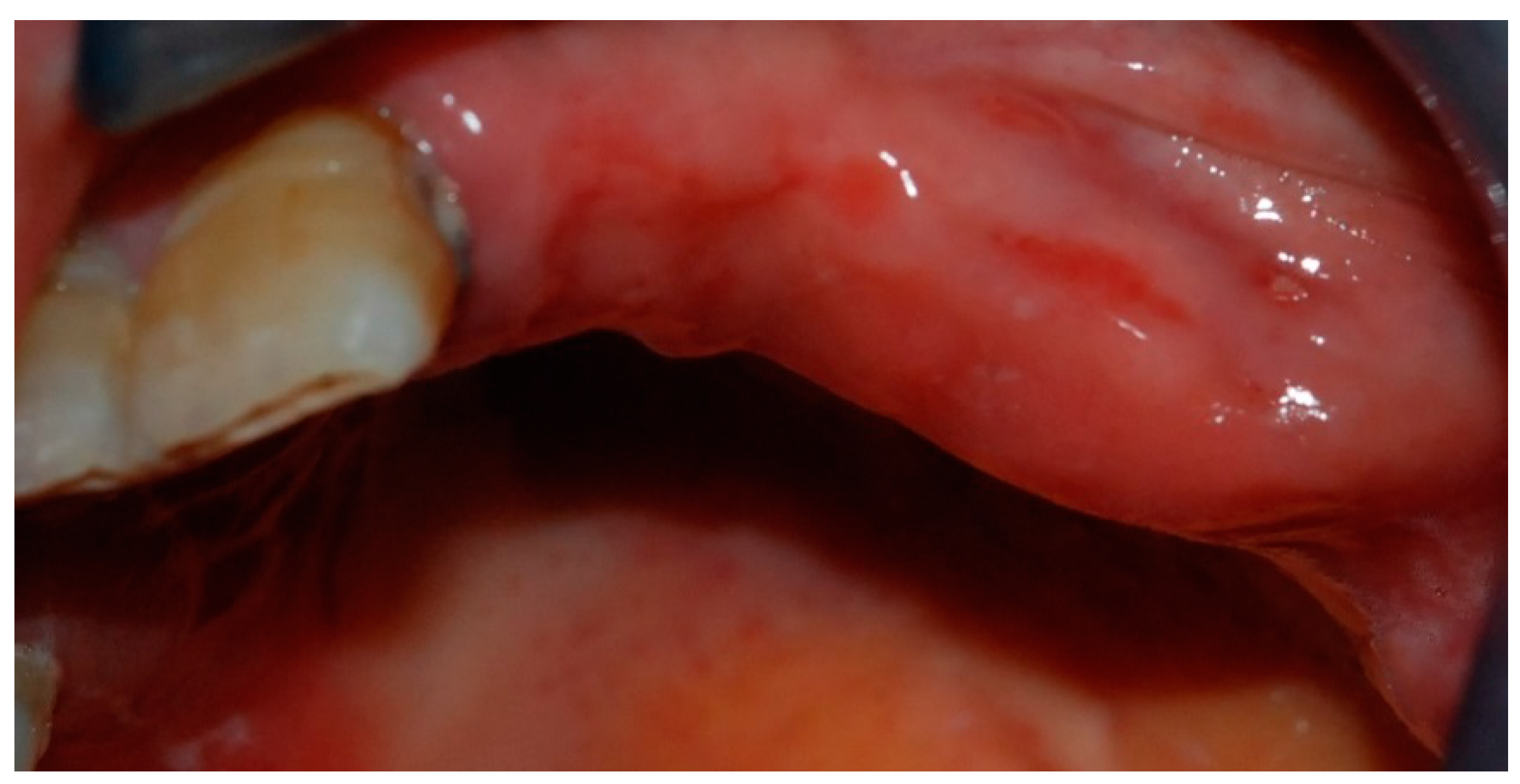
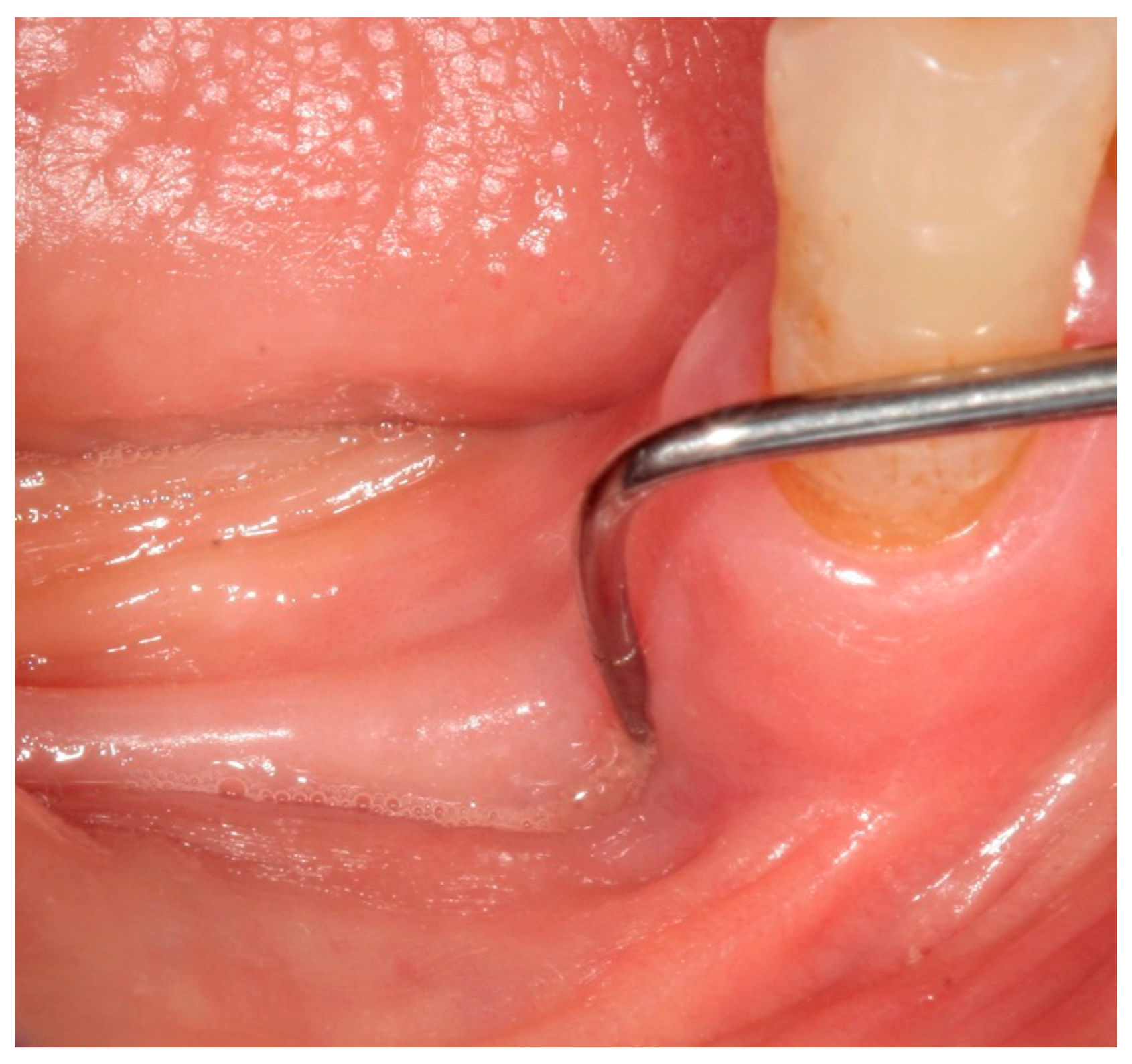
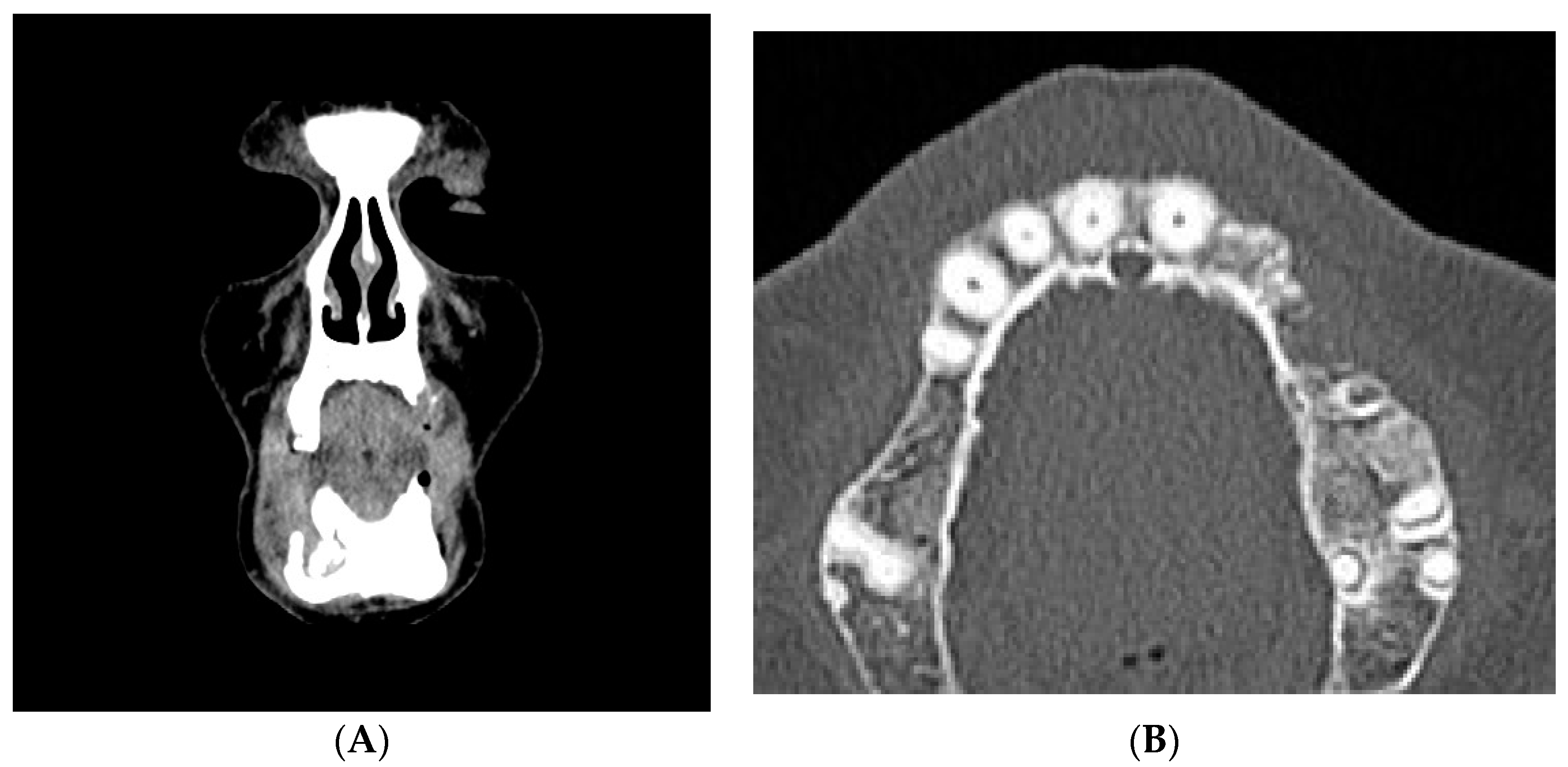
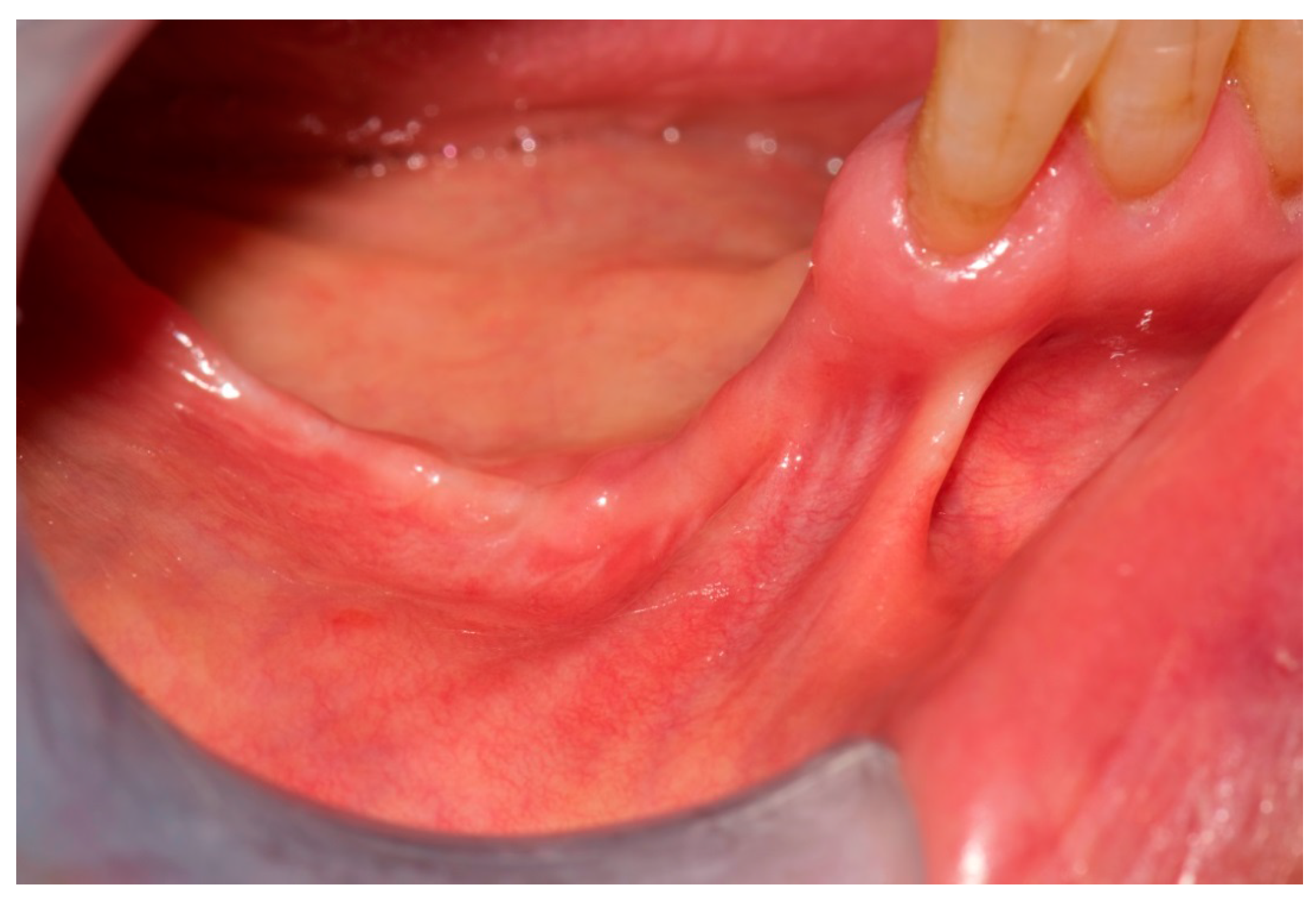
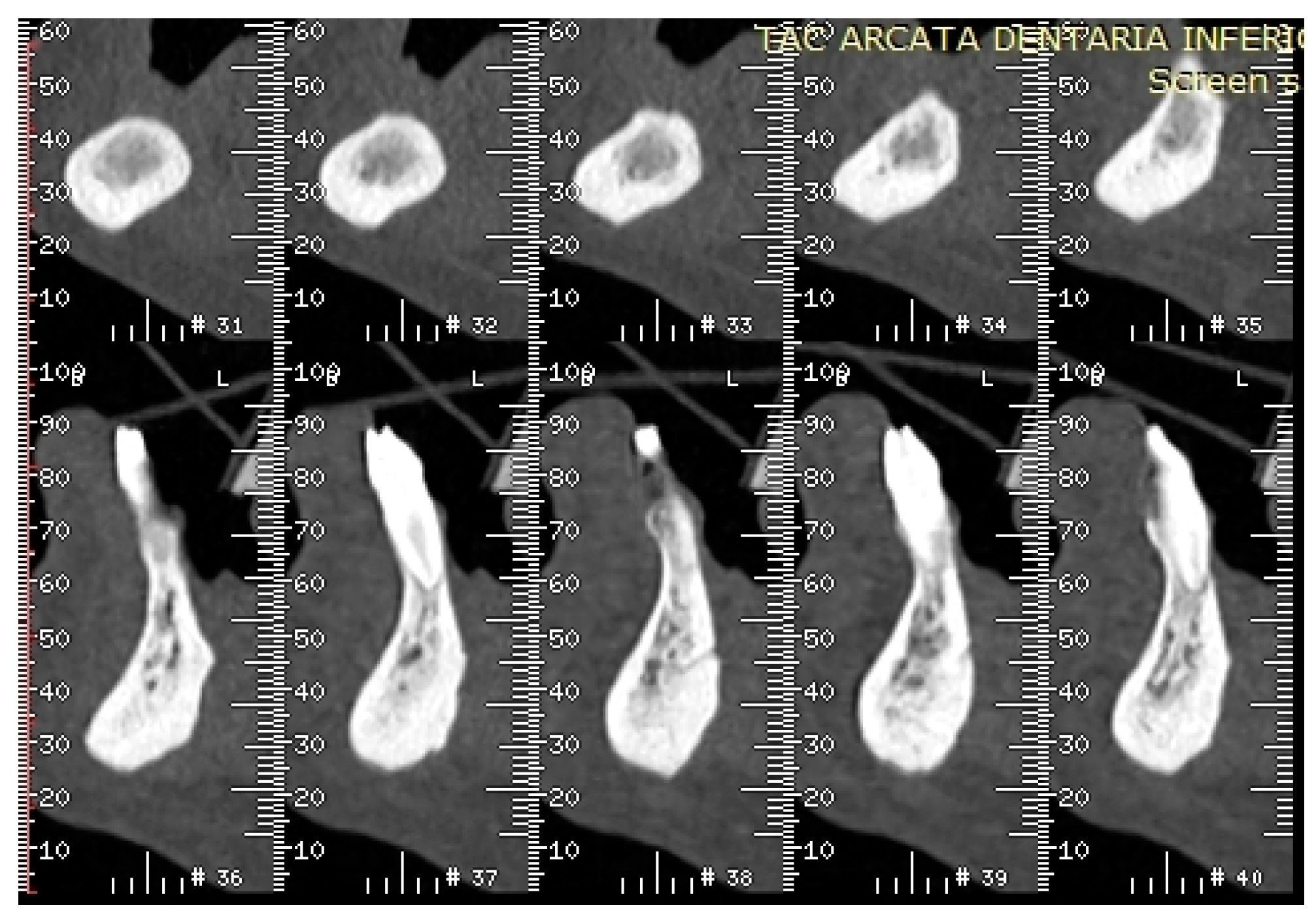
2. Case Report
3. Discussion
3.1. Origin of ONJ
3.2. ONJ Related to Alendronate and Other Drugs Administered for Osteoporosis
3.3. Learning from the Case
3.4. Frequency of ONJ in Osteoporosis Patients after Bisphosphonates or Denosumab: Possible Underestimation and Late Diagnosis
4. Conclusive Remarks
Author Contributions
Conflicts of Interest
References
- Ruggiero, S.L. Bisphosphonate-related osteonecrosis of the jaw (BRONJ): Initial discovery and subsequent development. J. Oral Maxillofac. Surg. 2009, 67, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons Position Paper on Bisphosphonate-Related Osteonecrosis of the Jaws. J. Oral Maxillofac. Surg. 2007, 65, 369–376. [Google Scholar]
- Khosla, S.; Burr, D.; Cauley, J.; Dempster, D.W.; Ebeling, P.R.; Felsenberg, D.; Gagel, R.F.; Gilsanz, V.; Guise, T.; Koka, S.; et al. Bisphosphonate-associated osteonecrosis of the jaw: Report of a task force of the American Society for Bone and Mineral Research. J. Bone Miner. Res. 2007, 22, 1479–1491. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, S.L.; Dodson, T.B.; Assael, L.A.; Landesberg, R.; Marx, R.E.; Mehrotra, B.; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons Position Paper on Bisphosphonate-Related Osteonecrosis of the Jaw—2009 Update. J. Oral Maxillofac. Surg. 2009, 67, 2–12. [Google Scholar] [PubMed]
- Junquera, L.; Gallego, L. Non exposed bisphosphonate-related osteonecrosis of the jaws: Another clinical variant? J. Oral Maxillofac. Surg. 2008, 66, 1516–1517. [Google Scholar] [CrossRef] [PubMed]
- Mawardi, H.; Treister, N.; Richardson, P. Sinus tracts—An early sign of bisphosphonate-associated osteonecrosis of the jaws? J. Oral Maxillofac. Surg. 2009, 67, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Fedele, S.; Porter, S.R.; D’Aiuto, F.; Aljohani, S.; Vescovi, P.; Manfredi, M.; Arduino, P.G.; Broccoletti, R.; Musciotto, A.; Di Fede, O.; et al. Nonexposed variant of bisphosphonate-associated osteonecrosis of the jaw: A case series. Am. J. Med. 2010, 123, 1060–1064. [Google Scholar] [CrossRef] [PubMed]
- Colella, G.; Campisi, G.; Fusco, V. American Association of Oral and Maxillofacial Surgeons position paper: Bisphosphonate-Related Osteonecrosis of the Jaws—2009 update: The need to refine the BRONJ definition. J. Oral Maxillofac. Surg. 2009, 67, 2698–2699. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, A.; Fusco, V.; Agrillo, A.; Campisi, G. Learning from experience. Proposal of a refined definition and staging system for bisphosphonate-related osteonecrosis of the jaw (BRONJ). Oral Dis. 2012, 18, 621–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schiodt, M.; Reibel, J.; Oturai, P.; Kofod, T. Comparison of non-exposed and exposed bisphosphonate-induced osteonecrosis of the jaws: A retrospective analysis from the Copenhagen cohort and a proposal for an updated classification system. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Otto, S.; Marx, R.E.; Tröltzsch, M.; Ristow, O.; Ziebart, T.; Al-Nawas, B.; Groetz, K.A.; Ehrenfeld, M.; Mercadante, V.; Porter, S.; et al. Comments on “diagnosis and management of osteonecrosis of the jaw: A systematic review and international consensus. J. Bone Miner.Res. 2015, 30, 1113–1115. [Google Scholar] [CrossRef] [PubMed]
- Fusco, V.; Bedogni, A.; Addeo, A.; Campisi, G. Definition and estimation of osteonecrosis of jaw (ONJ), and optimal duration of antiresorptive treatment in bone metastatic cancer patients: supplementary data from the denosumab extension study? Support. Care Cancer 2016, 25, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, S.L.; Dodson, T.B.; Fantasia, J.; Goodday, R.; Aghaloo, T.; Mehrotra, B.; O’Ryan, F. American Association of Oral and Maxillofacial Surgeons, American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J. Oral Maxillofac. Surg. 2014, 72, 1938–1956. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Morrison, A.; Hanley, D.A.; Felsenberg, D.; McCauley, L.K.; O’Ryan, F.; Reid, I.R.; Ruggiero, S.L.; Taguchi, A.; Tetradis, S.; et al. International Task Force on Osteonecrosis of the Jaw, Diagnosis and management of osteonecrosis of the jaw: A systematic review and international consensus. J. Bone Miner. Res. 2015, 30, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.R.; Burr, D.B. The pathogenesis of bisphosphonate-related osteonecrosis of the jaw: So many hypotheses, so few data. J. Oral Maxillofac. Surg. 2009, 67, 61–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kühl, S.; Walter, C.; Acham, S.; Pfeffer, R.; Lambrecht, J.T. Bisphosphonate-related osteonecrosis of the jaws—A review. Oral Oncol. 2012, 48, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Campisi, G.; Fedele, S.; Fusco, V.; Pizzo, G.; Di Fede, O.; Bedogni, A. Epidemiology, clinical manifestations, risk reduction and treatment strategies of jaw osteonecrosis in cancer patients exposed to antiresorptive agents. Future Oncol. 2014, 10, 257–275. [Google Scholar] [CrossRef] [PubMed]
- Vermeer, J.A.; Renders, G.A.; Everts, V. Osteonecrosis of the Jaw—A Bone Site-Specific Effect of Bisphosphonates. Curr. Osteoporos. Rep. 2016, 14, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Edwards, B.J.; Gounder, M.; McKoy, J.M.; Boyd, I.; Farrugia, M.; Migliorati, C.; Marx, R.; Ruggiero, S.; Dimopoulos, M.; Raisch, D.W.; et al. Pharmacovigilance and reporting oversight in US FDA fast-track process: bisphosphonates and osteonecrosis of the jaw. Lancet Oncol. 2009, 9, 1166–1172. [Google Scholar] [CrossRef]
- Lee, J.K.; Kim, K.W.; Choi, J.Y.; Moon, S.Y.; Kim, S.G.; Kim, C.H.; Kim, H.M.; Kwon, Y.D.; Kim, Y.D.; Lee, D.K.; et al. Bisphosphonates-related osteonecrosis of the jaw in Korea: A preliminary report. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 9–13. [Google Scholar] [CrossRef] [PubMed]
- De Boissieu, P.; Kanagaratnam, L.; AbouTaam, M.; Roux, M.P.; Dramé, M.; Trenque, T. Notoriety bias in a database of spontaneous reports: The example of osteonecrosis of the jaw under bisphosphonate therapy in the French national pharmacovigilance database. Pharmacoepidemiol. Drug. Saf. 2014, 23, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Parretta, E.; Sottosanti, L.; Sportiello, L.; Rafaniello, C.; Potenza, S.; D’Amato, S.; González-González, R.; Rossi, F.; Colella, G.; Capuano, A. Bisphosphonate-related osteonecrosis of the jaw: An Italian post-marketing surveillance analysis. Expert Opin. Drug Saf. 2014, 13, S31–S40. [Google Scholar] [CrossRef] [PubMed]
- Schiodt, M.; Larsson Wexell, C.; Herlofson, B.B.; Giltvedt, K.M.; Norholt, S.E.; Ehrenstein, V. Existing data sources for clinical epidemiology: Scandinavian Cohort for osteonecrosis of the jaw—Work in progress and challenges. Clin. Epidemiol. 2015, 7, 7–16. [Google Scholar] [CrossRef] [PubMed]
- De Boissieu, P.; Gaboriau, L.; Morel, A.; Trenque, T. Bisphosphonate-related osteonecrosis of the jaw: Data from the French national pharmacovigilance database. Fundam. Clin. Pharmacol. 2016, 30, 450–458. [Google Scholar] [CrossRef] [PubMed]
- López-Jornet, P.; Camacho-Alonso, F.; Molina-Miñano, F.; Gomez-Garcia, F. Bisphosphonate-associated osteonecrosis of the jaw. Knowledge and attitudes of dentists and dental students: A preliminary study. J. Eval. Clin. Pract. 2010, 16, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.Y.; Park, Y.D.; Kwon, Y.D.; Kim, D.Y.; Ohe, J.Y. Survey of Korean dentists on the awareness on bisphosphonate-related osteonecrosis of the jaws. J. Investig. Clin. Dent. 2010, 1, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Osta, L.E.; Osta, B.E.; Lakiss, S.; Hennequin, M.; Osta, N.E. Bisphosphonate-related osteonecrosis of the jaw: Awareness and level of knowledge of Lebanese physicians. Support. Care Cancer. 2015, 23, 2825–2831. [Google Scholar] [CrossRef] [PubMed]
- De Lima, P.B.; Brasil, V.L.; de Castro, J.F.; de Moraes Ramos-Perez, F.M.; Alves, F.A.; dos AnjosPontual, M.L.; da Cruz Perez, D.E. Knowledge and attitudes of Brazilian dental students and dentists regarding bisphosphonate-related osteonecrosis of the jaw. Support. Care Cancer. 2015, 23, 3421–3426. [Google Scholar] [CrossRef] [PubMed]
- Alhussain, A.; Peel, S.; Dempster, L.; Clokie, C.; Azarpazhooh, A. Knowledge, practices, and opinions of Ontario dentists when treating patients receiving bisphosphonates. J. Oral Maxillofac. Surg. 2015, 73, 1095–1105. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, A.; Fedele, S.; Bedogni, G.; Scoletta, M.; Favia, G.; Colella, G.; Agrillo, A.; Bettini, G.; Di Fede, O.; Oteri, G.; et al. Staging of osteonecrosis of the jaw requires computed tomography for accurate definition of the extent of bony disease. Br. J. Oral Maxillofac. Surg. 2014, 52, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Fedele, S.; Bedogni, G.; Scoletta, M.; Favia, G.; Colella, G.; Agrillo, A.; Bettini, G.; Di Fede, O.; Oteri, G.; Fusco, V.; et al. Up to a quarter of patients with osteonecrosis of the jaw associated with antiresorptive agents remain undiagnosed. Br. J. Oral Maxillofac. Surg. 2015, 53, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Wilde, F.; Heufelder, M.; Lorenz, K.; Liese, S.; Liese, J.; Helmrich, J.; Schramm, A.; Hemprich, A.; Hirsch, E.; Winter, K. Prevalence of cone beam computed tomography imaging findings according to the clinical stage of bisphosphonate-related osteonecrosis of the jaw. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Setabutr, D.; Hales, N.W.; Krempl, G.A. Necrotizing fasciitis secondary to bisphosphonate-induced osteonecrosis of the jaw. Am. J. Otolaryngol. 2010, 31, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Randi, L.; De Martino, I.; Fasciolo, A.; Gambino, A.; Fusco, V. Osteonecrosis of jaw (ONJ): Sometimes a life-threatening event. Literature review and two cases. Ann. Stomatol. (Roma) 2014, 5, 33–34. [Google Scholar]
- Mondello, P.; Pitini, V.; Arrigo, C.; Mondello, S.; Mian, M.; Altavilla, G. Necrotizing fasciitis as a rare complication of osteonecrosis of the jaw in a patient with multiple myeloma treated with lenalidomide: Case report and review of the literature. SpringerPlus 2014, 5, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.H.; Shen, S.H.; Li, W.Y.; Chu, Y.K. Bisphosphonate-related osteonecrosis of the jaw complicated by Ludwig’s angina. J. Chin. Med. Assoc. 2015, 78, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Mehanna, P.; Goddard, R. Bisphosphonate associated osteonecrosis: An unusual case. Aust. Dent. J. 2010, 55, 311–333. [Google Scholar] [CrossRef] [PubMed]
- Ebker, T.; Rech, J.; von Wilmowsky, C.; Neukam, F.W.; Stockmann, P. Fulminant course of osteonecrosis of the jaw in a rheumatoid arthritis patient following oral bisphosphonate intake and biologic therapy. Rheumatology (Oxf.) 2013, 52, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Kaehling, C.H.; Streckbein, P.; Schmermund, D.; Henrich, M.; Burchert, D.; Gattenloehner, S.; Howaldt, H.P.; Wilbrand, J.F. Lethal cervical abscess following bisphosphonate related osteonecrosis of the jaw. J. Craniomaxillofac. Surg. 2014, 42, 1203–1206. [Google Scholar] [CrossRef] [PubMed]
- Qaisi, M.; Hargett, J.; Loeb, M.; Brown, J.; Caloss, R. Denosumab Related Osteonecrosis of the Jaw with Spontaneous Necrosis of the Soft Palate: Report of a Life Threatening Case. Case Rep. Dent. 2016, 2016, 5070187. [Google Scholar] [CrossRef] [PubMed]
- Otto, S.; Schreyer, C.; Hafner, S.; Mast, G.; Ehrenfeld, M.; Stürzenbaum, S.; Pautke, C. Bisphosphonate-related osteonecrosis of the jaws—Characteristics, risk factors, clinical features, localization and impact on oncological treatment. J. Craniomaxillofac. Surg. 2012, 40, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Di Fede, O.; Bedogni, A.; Giancola, F.; Saia, G.; Bettini, G.; Toia, F.; D’Alessandro, N.; Firenze, A.; Matranga, D.; Fedele, S.; et al. BRONJ in patients with rheumatoid arthritis: A multicenter case series. Oral Dis. 2016, 22, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Vescovi, P. Bisphosphonates and osteonecrosis: An open matter. Clin. Cases Miner. Bone Metab. 2012, 9, 142–144. [Google Scholar] [PubMed]
- Walter, C.; Sagheb, K.; Bitzer, J.; Rahimi-Nedjat, R.; Taylor, K.J. Analysis of reasons for osteonecrosis of the jaws. Clin. Oral Investig. 2014, 18, 2221–2226. [Google Scholar] [CrossRef] [PubMed]
- Papapoulos, S.; Lippuner, K.; Roux, C.; Lin, C.J.; Kendler, D.L.; Lewiecki, E.M.; Brandi, M.L.; Czerwiński, E.; Franek, E.; Lakatos, P.; et al. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: Results from the FREEDOM Extension study. Osteoporos. Int. 2015, 26, 2773–2783. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.; Blanco, R. Osteonecrosis of the jaw (ONJ) and atypical femoral fracture (AFF) in an osteoporotic patient chronically treated with bisphosphonates. Osteoporos. Int. 2017, 28, 1145–1147. [Google Scholar] [CrossRef] [PubMed]
- Bagan, J.; Peydró, A.; Calvo, J.; Leopoldo, M.; Jiménez, Y.; Bagan, L. Medication-related osteonecrosis of the jaw associated with bisphosphonates and denosumab in osteoporosis. Oral Dis. 2016, 22, 324–329. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency (EMA). PSUR/PSUSA Submission and Expected PRAC Outcome Dates for Bisphosphonates and Denosumab. March 2015. Available online: http://www.ema.europa.eu/docs/en_GB/document_library/Other/2015/03/WC500184239.pdf (accessed on 13 March 2017).





© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Migliario, M.; Mergoni, G.; Vescovi, P.; Martino, I.D.; Alessio, M.; Benzi, L.; Renò, F.; Fusco, V. Osteonecrosis of the Jaw (ONJ) in Osteoporosis Patients: Report of Delayed Diagnosis of a Multisite Case and Commentary about Risks Coming from a Restricted ONJ Definition. Dent. J. 2017, 5, 13. https://doi.org/10.3390/dj5010013
Migliario M, Mergoni G, Vescovi P, Martino ID, Alessio M, Benzi L, Renò F, Fusco V. Osteonecrosis of the Jaw (ONJ) in Osteoporosis Patients: Report of Delayed Diagnosis of a Multisite Case and Commentary about Risks Coming from a Restricted ONJ Definition. Dentistry Journal. 2017; 5(1):13. https://doi.org/10.3390/dj5010013
Chicago/Turabian StyleMigliario, Mario, Giovanni Mergoni, Paolo Vescovi, Iolanda De Martino, Manuela Alessio, Luca Benzi, Filippo Renò, and Vittorio Fusco. 2017. "Osteonecrosis of the Jaw (ONJ) in Osteoporosis Patients: Report of Delayed Diagnosis of a Multisite Case and Commentary about Risks Coming from a Restricted ONJ Definition" Dentistry Journal 5, no. 1: 13. https://doi.org/10.3390/dj5010013




