Formulation and In-Vitro Characterization of pH-Responsive Semi-Interpenetrating Polymer Network Hydrogels for Controlled Release of Ketorolac Tromethamine
Abstract
:1. Introduction
2. Results and Discussion
2.1. Fourier Transform Infrared (FTIR) Spectroscopy
2.2. Sol-Gel Analysis
2.3. Polymer Volume Fraction
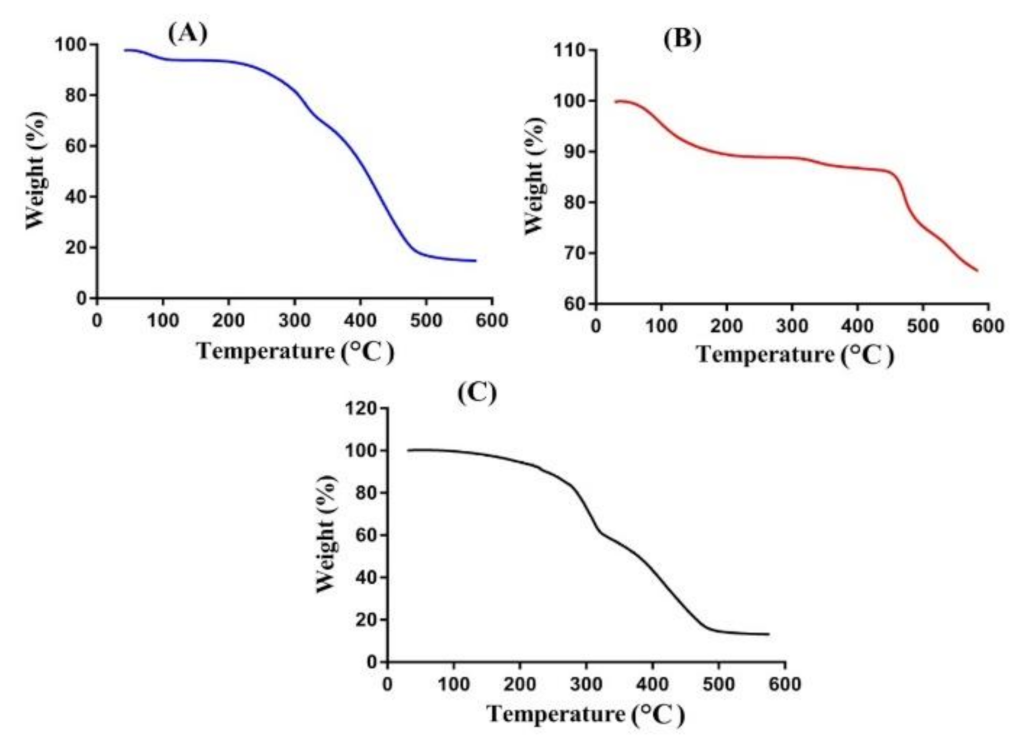
2.4. Thermogravimetric Analysis (TGA)
2.5. Differential Scanning Calorimetry (DSC)
2.6. Swelling Studies
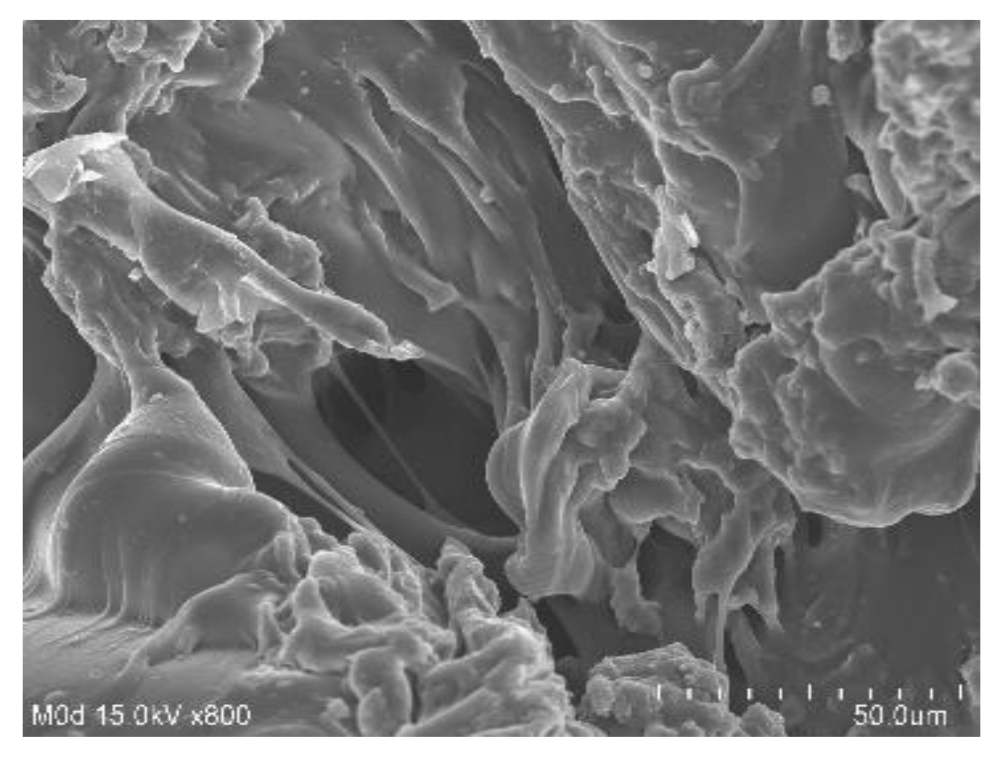
2.7. Scanning Electron Microscopy (SEM)
2.8. Drug Loading of Hydrogel Samples
2.9. In-Vitro Drug Release Studies
2.10. Drug Release Kinetics
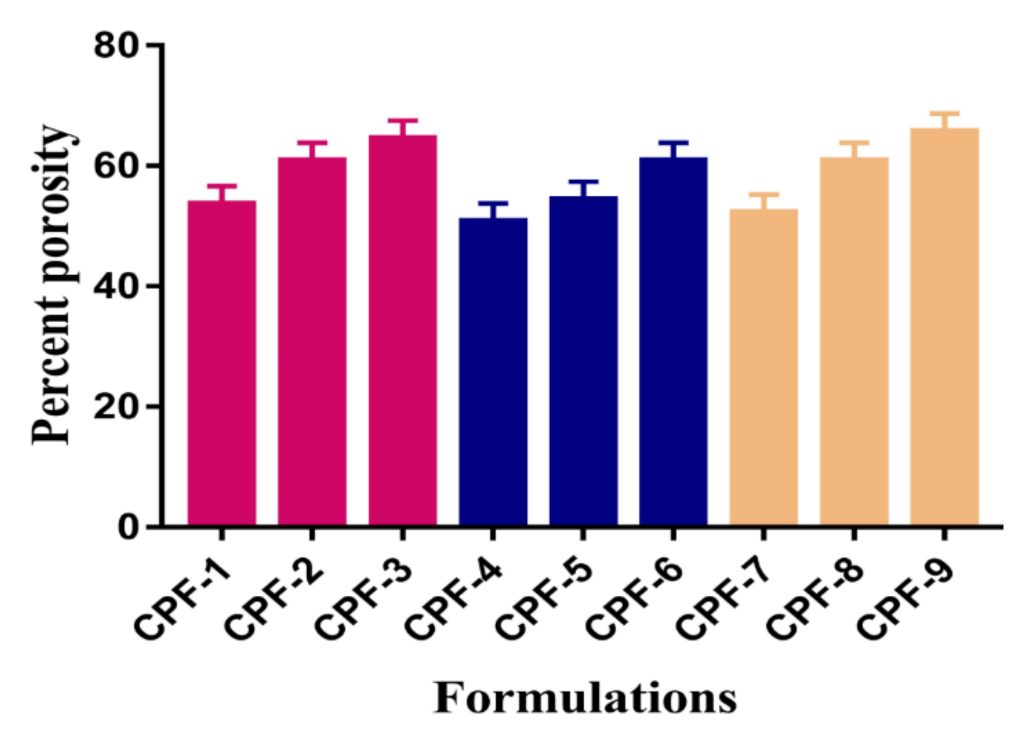
2.11. Percent Porosity
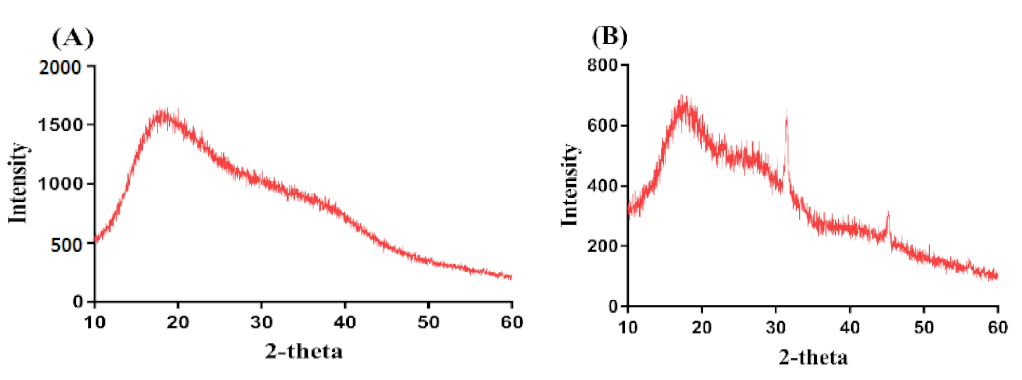
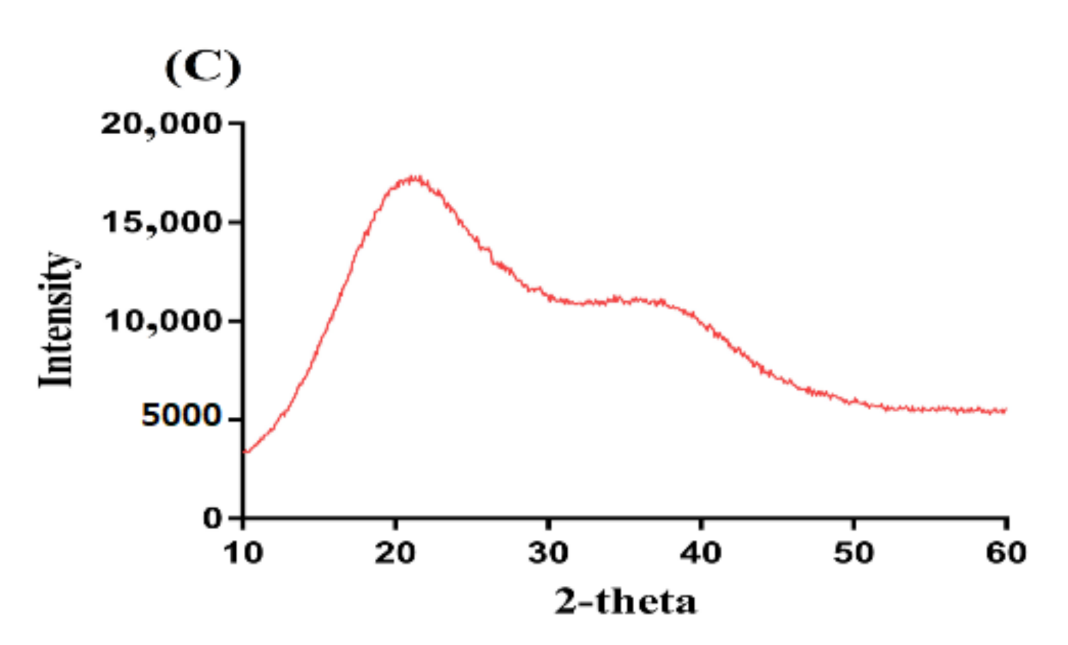
2.12. Powder X-ray Diffraction (PXRD)
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Development of CP/SpScPAA Hydrogels
4.3. Fourier Transform Infrared (FTIR) Spectroscopy
4.4. Sol-Gel Analysis
4.5. Polymer Volume Fraction
4.6. Thermogravimetric Analysis (TGA)
4.7. Differential Scanning Calorimetry (DSC)
4.8. Swelling Studies
4.9. Scanning Electron Microscopy (SEM)
4.10. Drug Loading of Hydrogel
4.11. In Vitro Drug Release Studies
4.12. Drug Release Kinetics
4.13. Percent Porosity
4.14. Powder X-ray Diffraction (PXRD) Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jeganath, S.; Asha, D.; Kumar, S.S.; Nair, K.S.; Kumaran, K.S. Oral Controlled Drug Delivery System—A Review. Res. J. Pharm. Technol. 2018, 11, 797–804. [Google Scholar] [CrossRef]
- Szycher, M. Controlled drug delivery: A critical review. J. Biomater. Appl. 1986, 1, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Park, K. Environment-sensitive hydrogels for drug delivery. Adv. Drug Deliv. Rev. 2001, 53, 321–339. [Google Scholar] [CrossRef]
- Suhail, M.; Rosenholm, J.M.; Minhas, M.U.; Badshah, S.F.; Naeem, A.; Khan, K.U.; Fahad, M. Nanogels as drug-delivery systems: A comprehensive overview. Ther. Deliv. 2019, 10, 697–717. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Minhas, M.U.; Ahmad, M.; Sohail, M. Self-assembled supramolecular thermoreversible beta-cyclodextrin/ethylene glycol injectable hydrogels with difunctional Pluronic((R))127 as controlled delivery depot of curcumin. Development, characterization and in vitro evaluation. J. Biomater. Sci. Polym. Ed. 2018, 29, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ranjha, N.M. Effect of degree of cross-linking on swelling and on drug release of low viscous chitosan/poly(vinyl alcohol) hydrogels. Polym. Bull. 2014, 71, 2133–2158. [Google Scholar] [CrossRef]
- Bukhari, S.M.H.; Khan, S.; Rehanullah, M.; Ranjha, N.M. Synthesis and Characterization of Chemically Cross-Linked Acrylic Acid/Gelatin Hydrogels: Effect of pH and Composition on Swelling and Drug Release. Int. J. Polym. Sci. 2015, 2015, 187961. [Google Scholar] [CrossRef]
- Ahmed, E.M. Hydrogel: Preparation, characterization, and applications: A review. J. Adv. Res. 2015, 6, 105–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bettini, R.; Colombo, P.; Peppas, N.A. Solubility Effects on Drug Transport through Ph-Sensitive, Swelling-Controlled Release Systems—Transport of Theophylline and Metoclopramide Monohydrochloride. J. Control. Release 1995, 37, 105–111. [Google Scholar] [CrossRef]
- Rizwan, M.; Yahya, R.; Hassan, A.; Yar, M.; Azzahari, A.D.; Selvanathan, V.; Sonsudin, F.; Abouloula, C.N. pH Sensitive Hydrogels in Drug Delivery: Brief History, Properties, Swelling, and Release Mechanism, Material Selection and Applications. Polymers 2017, 9, 137. [Google Scholar] [CrossRef]
- Wang, K.; Fu, Q.; Chen, X.; Gao, Y.; Dong, K. Preparation and characterization of pH-sensitive hydrogel for drug delivery system. RSC Adv. 2012, 2, 7772–7780. [Google Scholar] [CrossRef]
- Khalid, I.; Ahmad, M.; Minhas, M.U.; Barkat, K. Preparation and characterization of alginate-PVA-based semi-IPN: Controlled release pH-responsive composites. Polym. Bull. 2018, 75, 1075–1099. [Google Scholar] [CrossRef]
- Al-Tabakha, M.M.; Khan, S.A.; Ashames, A.; Ullah, H.; Ullah, K.; Murtaza, G.; Hassan, N. Synthesis, Characterization and Safety Evaluation of Sericin-Based Hydrogels for Controlled Delivery of Acyclovir. Pharmaceuticals 2021, 14, 234. [Google Scholar] [CrossRef] [PubMed]
- Ullah, K.; Khan, S.A.; Murtaza, G.; Sohail, M.; Manan, A.; Afzal, A. Gelatin-based hydrogels as potential biomaterials for colonic delivery of oxaliplatin. Int. J. Pharm. 2019, 556, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Ron, E.S.; Bromberg, L.E. Temperature-responsive gels and thermogelling polymer matrices for protein and peptide delivery. Adv. Drug Deliv. Rev. 1998, 31, 197–221. [Google Scholar] [CrossRef] [PubMed]
- Fogueri, L.R.; Singh, S. Smart polymers for controlled delivery of proteins and peptides: A review of patents. Recent Pat. Drug Deliv. Formul. 2009, 3, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Galaev, I.Y.; Mattiasson, B. ‘Smart’ polymers and what they could do in biotechnology and medicine. Trends Biotechnol. 1999, 17, 335–340. [Google Scholar] [CrossRef]
- Sarfraz, R.M.; Khan, M.U.; Mahmood, A.; Akram, M.R.; Minhas, M.U.; Qaisar, M.N.; Ali, M.R.; Ahmad, H.; Zaman, M. Synthesis of co-polymeric network of carbopol-g-methacrylic acid nanogels drug carrier system for gastro-protective delivery of ketoprofen and its evaluation. Polym.-Plast. Technol. Mater. 2020, 59, 1109–1123. [Google Scholar] [CrossRef]
- Taylor, N.W.; Bagley, E.B. Tailoring closely packed gel–particle systems for use as thickening agents. J. Appl. Polym. Sci. 1977, 21, 113–122. [Google Scholar] [CrossRef]
- Garg, S.; Vermani, K.; Garg, A.; Anderson, R.A.; Rencher, W.B.; Zaneveld, L.J. Development and characterization of bioadhesive vaginal films of sodium polystyrene sulfonate (PSS), a novel contraceptive antimicrobial agent. Pharm. Res. 2005, 22, 584–595. [Google Scholar] [CrossRef]
- Suhail, M.; Fang, C.W.; Minhas, M.U.; Wu, P.C. Preparation, Characterization, Swelling Potential, and In-Vitro Evaluation of Sodium Poly(Styrene Sulfonate)-Based Hydrogels for Controlled Delivery of Ketorolac Tromethamine. Pharmaceuticals 2021, 14, 350. [Google Scholar] [CrossRef]
- EFSA Panel on Food Contact Materials, Enzymes, Flavourings and Processing Aids (CEF). Safety assessment of the active substance polyacrylic acid, sodium salt, cross-linked, for use in active food contact materials. EFSA J. 2018, 16, e05448. [Google Scholar] [CrossRef]
- Mahmood, S.; Buabeid, M.A.; Ullah, K.; Murtaza, G.; Mannan, A.; Khan, S.A. Synthesis, characterization and safety profiling of eudragit-based pH-responsive hydrogels: A promising platform for colonic delivery of losartan potassium. Curr. Drug Deliv. 2019, 16, 548–564. [Google Scholar] [CrossRef]
- Mun, E.A.; Hannell, C.; Rogers, S.E.; Hole, P.; Williams, A.C.; Khutoryanskiy, V.V. On the role of specific interactions in the diffusion of nanoparticles in aqueous polymer solutions. Langmuir 2014, 30, 308–317. [Google Scholar] [CrossRef]
- Puglia, C.; Filosa, R.; Peduto, A.; de Caprariis, P.; Rizza, L.; Bonina, F.; Blasi, P. Evaluation of alternative strategies to optimize ketorolac transdermal delivery. AAPS PharmSciTech 2006, 7, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagh, P.; Mujumdar, A.; Naik, J.B. Preparation and characterization of ketorolac tromethamine-loaded ethyl cellulose micro-/nanospheres using different techniques. Part. Sci. Technol. 2019, 37, 347–357. [Google Scholar] [CrossRef]
- Alsarra, I.A.; Bosela, A.A.; Ahmed, S.M.; Mahrous, G.M. Proniosomes as a drug carrier for transdermal delivery of ketorolac. Eur. J. Pharm. Biopharm. 2005, 59, 485–490. [Google Scholar] [CrossRef]
- Mathew, S.T.; Devi, S.G.; Kv, S. Formulation and evaluation of ketorolac tromethamine-loaded albumin microspheres for potential intramuscular administration. AAPS PharmSciTech 2007, 8, 14. [Google Scholar] [CrossRef] [Green Version]
- Sahoo, S.; Chakraborti, C.K.; Mishra, S.C. Qualitative analysis of controlled release ciprofloxacin/carbopol 934 mucoadhesive suspension. J. Adv. Pharm. Technol. Res. 2011, 2, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, S.; Chakraborti, C.K.; Behera, P.K.; Mishra, S.C. Characterization of mucoadhesive ciprofloxacin suspensions by Fourier transform infrared spectroscopy. Int. J. Pharm. Sci. Rev. Res. 2011, 11, 122–128. [Google Scholar]
- Patel, R.P.; Dadhani, B.; Ladani, R.; Baria, A.H.; Patel, J. Formulation, evaluation and optimization of stomach specific in situ gel of clarithromycin and metronidazole benzoate. Int. J. Drug Deliv. 2010, 2, 141–153. [Google Scholar] [CrossRef] [Green Version]
- De, R.; Lee, H.; Das, B. Exploring the interactions in binary mixtures of polyelectrolytes: Influence of mixture composition, concentration, and temperature on counterion condensation. J. Mol. Liq. 2018, 251, 94–99. [Google Scholar] [CrossRef]
- Moharram, M.A.; Khafagi, M.G. Application of FTIR spectroscopy for structural characterization of ternary poly(acrylic acid)-metal-poly(vinyl pyrrolidone) complexes. J. Appl. Polym. Sci. 2007, 105, 1888–1893. [Google Scholar] [CrossRef]
- Begum, M.Y.; Shaik, M.R.; Abbulu, K.; Sudhakar, M.; Reddy, M. Ketorolac tromethamine loaded liposomes of long alkyl chain lipids: Development, characterization and in vitro performance. Int. J. Pharm. Tech. Res. 2012, 4, 218–225. [Google Scholar]
- Waghulde, M.; Mujumdar, A.; Naik, J. Preparation and characterization of miglitol-loaded Poly (d, l-lactide-co-glycolide) microparticles using high pressure homogenization-solvent evaporation method. Int. J. Polym. Mater. 2019, 68, 198–207. [Google Scholar] [CrossRef]
- Aşık, M.D.; Uğurlu, N.; Yülek, F.; Tuncer, S.; Türk, M.; Denkbaş, E.B. Ketorolac tromethamine loaded chitosan nanoparticles as a nanotherapeutic system for ocular diseases. Hacet. J. Biol. Chem. 2013, 41, 81–86. [Google Scholar]
- Patil, J.S.; Yadava, S.K.; Mokale, V.J.; Naik, J.B. Preparation and Characterization of Single Pulse Sustained Release Ketorolac Nanoparticles to Reduce their Side-Effects at Gastrointestinal Tract. In Proceedings of the International Conference on Advances in Engineering and Technology 2014, Kollam, India, 30–31 December 2014; pp. 59–62. [Google Scholar]
- Khalid, I.; Ahmad, M.; Minhas, M.U.; Barkat, K. Synthesis and evaluation of chondroitin sulfate based hydrogels of loxoprofen with adjustable properties as controlled release carriers. Carbohydr. Polym. 2018, 181, 1169–1179. [Google Scholar] [CrossRef]
- Harish, N.M.; Prabhu, P.; Charyulu, R.N.; Gulzar, M.A.; Subrahmanyam, E.V. Formulation and Evaluation of in situ Gels Containing Clotrimazole for Oral Candidiasis. Indian J. Pharm. Sci. 2009, 71, 421–427. [Google Scholar] [CrossRef] [Green Version]
- Hussain, T.; Ranjha, N.M.; Shahzad, Y. Swelling and Controlled Release of Tramadol Hydrochloride from a pH-Sensitive Hydrogel. Des. Monomers Polym. 2011, 14, 233–249. [Google Scholar] [CrossRef]
- Dergunov, S.A.; Nam, I.K.; Mun, G.A.; Nurkeeva, Z.S.; Shaikhutdinov, E.M. Radiation synthesis and characterization of stimuli-sensitive chitosan-polyvinyl pyrrolidone hydrogels. Radiat. Phys. Chem. 2005, 72, 619–623. [Google Scholar] [CrossRef]
- Badshah, S.F.; Akhtar, N.; Minhas, M.U.; Khan, K.U.; Khan, S.; Abdullah, O.; Naeem, A. Porous and highly responsive cross-linked β-cyclodextrin based nanomatrices for improvement in drug dissolution and absorption. Life Sci. 2021, 267, 118931. [Google Scholar] [CrossRef]
- Suhail, M.; Wu, P.C.; Minhas, M.U. Using Carbomer-Based Hydrogels for Control the Release Rate of Diclofenac Sodium: Preparation and In Vitro Evaluation. Pharmaceuticals 2020, 13, 399. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.C.; Gong, B.L.; Zhou, Y.Q.; Sun, Z.A.; Wang, X.X.; Zhao, S.W. Preparation of high-capacity magnetic polystyrene sulfonate sodium material based on SI-ATRP method and its adsorption property research for sulfonamide antibiotics. BMC Chem. 2020, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barkat, K.; Ahmad, M.; Minhas, M.U.; Khalid, I.; Nasir, B. Development and characterization of pH-responsive polyethylene glycol-co-poly (methacrylic acid) polymeric network system for colon target delivery of oxaliplatin: Its acute oral toxicity study. Adv. Polym. Technol. 2018, 37, 1806–1822. [Google Scholar] [CrossRef]
- Shen, X.; Yu, D.; Zhu, L.; Branford-White, C.; White, K.; Chatterton, N.P. Electrospun diclofenac sodium loaded Eudragit(R) L 100-55 nanofibers for colon-targeted drug delivery. Int. J. Pharm. 2011, 408, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Barkat, K.; Ahmad, M.; Minhas, M.U.; Khalid, I. Oxaliplatin-loaded crosslinked polymeric network of chondroitin sulfate-co-poly(methacrylic acid) for colorectal cancer: Its toxicological evaluation. J. Appl. Polym. Sci. 2017, 134. [Google Scholar] [CrossRef]
- Atta, A.M. Swelling behaviors of polyelectrolyte hydrogels containing sulfonate groups. Polym. Adv. Technol. 2002, 13, 567–576. [Google Scholar] [CrossRef]
- Ali, A.E.H. Removal of Heavy Metals from Model Wastewater by Using Carboxymehyl Cellulose/2-Acrylamido-2-methyl Propane Sulfonic Acid Hydrogels. J. Appl. Polym. Sci. 2012, 123, 763–769. [Google Scholar] [CrossRef]
- Ju, Y.H.; Huynh, L.H.; Kasim, N.S.; Guo, T.J.; Wang, J.H.; Fazary, A.E. Analysis of soluble and insoluble fractions of alkali and subcritical water treated sugarcane bagasse. Carbohydr. Polym. 2011, 83, 591–599. [Google Scholar] [CrossRef]
- Sohail, M.; Ahmad, M.; Minhas, M.U.; Ali, L.; Munir, A.; Khalid, I. Synthesis and Characterization of Graft PVA Composites for Controlled Delivery of Valsartan. Lat. Am. J. Pharm. 2014, 33, 1237–1244. [Google Scholar]
- Sharmin, N.; Al-Mamun, M.; Jalil, R.U. A novel method to study the effect of pH and excipients on water uptake and swelling behaviour of Carbopol polymers. Bangl. Pharm. J. 2010, 3, 1–7. [Google Scholar]
- Qudah, Y.H.; Raafat, A.I.; Ali, A. Removal of some heavy metals from their aqueous solutions using 2-acrylamido-2-methyl-1-propane sulfonic acid/polyvinyl alcohol copolymer hydrogels prepared by gamma irradiation. Arab. J. Nucl. Sci. Appl. 2013, 46, 80–91. [Google Scholar]
- Sanli, O.; Ay, N.; Isiklan, N. Release characteristics of diclofenac sodium from poly(vinyl alcohol)/sodium alginate and poly(vinyl alcohol)-grafted-poly(acrylamide)/sodium alginate blend beads. Eur. J. Pharm. Biopharm. 2007, 65, 204–214. [Google Scholar] [CrossRef]
- Khanum, H.; Ullah, K.; Murtaza, G.; Khan, S.A. Fabrication and in vitro characterization of HPMC-g-poly(AMPS) hydrogels loaded with loxoprofen sodium. Int. J. Biol. Macromol. 2018, 120, 1624–1631. [Google Scholar] [CrossRef] [PubMed]
- Murthy, P.S.K.; Mohan, Y.M.; Sreeramulu, J.; Raju, K.M. Semi-IPNs of starch and poly(acrylamide-co-sodium methacrylate): Preparation, swelling and diffusion characteristics evaluation. React. Funct. Polym. 2006, 66, 1482–1493. [Google Scholar] [CrossRef]
- Sullad, A.G.; Manjeshwar, L.S.; Aminabhavi, T.M. Novel pH-Sensitive Hydrogels Prepared from the Blends of Poly(vinyl alcohol) with Acrylic Acid-graft-Guar Gum Matrixes for Isoniazid Delivery. Ind. Eng. Chem. Res. 2010, 49, 7323–7329. [Google Scholar] [CrossRef]
- Rashid, H.; Ahmad, M.; Minhas, M.U.; Sohail, M.; Aamir, M.F. Synthesis and Characterization of Poly(hydroxyethyl methacrylate-co-methacrylic acid) Cross Linked Polymeric Network for the Delivery of Analgesic Agent. J. Chem. Soc. Pak. 2015, 37, 999–1007. [Google Scholar]
- Khan, G.M.; Jiabi, Z. Formulation and in vitro evaluation of ibuprofen-Carbopol 974P-NF controlled release matrix tablets. III: Influence of co-excipients on release rate of the drug. J. Control. Release 1998, 54, 185–190. [Google Scholar] [CrossRef]
- Khan, G.M.; Zhu, J.B. Studies on drug release kinetics from ibuprofen-carbomer hydrophilic matrix tablets: Influence of co-excipients on release rate of the drug. J. Control. Release 1999, 57, 197–203. [Google Scholar] [CrossRef]
- Liu, C.H.; Chen, Y.Q.; Chen, J.G. Synthesis and characteristics of pH-sensitive semi-interpenetrating polymer network hydrogels based on konjac glucomannan and poly(aspartic acid) for in vitro drug delivery. Carbohydr. Polym. 2010, 79, 500–506. [Google Scholar] [CrossRef]
- Korsmeyer, R.W.; Gurny, R.; Doelker, E.; Buri, P.; Peppas, N.A. Mechanisms of potassium chloride release from compressed, hydrophilic, polymeric matrices: Effect of entrapped air. J. Pharm. Sci. 1983, 72, 1189–1191. [Google Scholar] [CrossRef] [PubMed]
- Sarika, P.; James, N.R.; Raj, D.K. Preparation, characterization and biological evaluation of curcumin loaded alginate aldehyde–gelatin nanogels. Mater. Sci. Eng. C 2016, 68, 251–257. [Google Scholar]
- Chang, C.; Duan, B.; Zhang, L. Fabrication and characterization of novel macroporous cellulose–alginate hydrogels. Polymer 2009, 50, 5467–5473. [Google Scholar] [CrossRef]
- Abdullah, O.; Minhas, M.U.; Ahmad, M.; Ahmad, S.; Ahmad, A. Synthesis of hydrogels for combinatorial delivery of 5-fluorouracil and leucovorin calcium in colon cancer: Optimization, in vitro characterization and its toxicological evaluation. Polym. Bull. 2019, 76, 3017–3037. [Google Scholar] [CrossRef]
- Lee, C.T.; Huang, C.P.; Lee, Y.D. Synthesis and characterizations of amphiphilic poly(L-lactide)-grafted chondroitin sulfate copolymer and its application as drug carrier. Biomol. Eng. 2007, 24, 131–139. [Google Scholar] [CrossRef]
- Suhail, M.; Wu, P.C.; Minhas, M.U. Development and characterization of pH-sensitive chondroitin sulfate-co-poly(acrylic acid) hydrogels for controlled release of diclofenac sodium. J. Saudi Chem. Soc. 2021, 25. [Google Scholar] [CrossRef]
- Zahra, Q.; Minhas, M.U.; Khan, S.; Wu, P.C.; Suhail, M.; Iqbal, R.; Bashir, M. Fabrication of polyethylene glycol hydrogels with enhanced swelling; loading capacity and release kinetics. Polym. Bull. 2021. [Google Scholar] [CrossRef]
- Suhail, M.; Khan, A.; Rosenholm, J.M.; Minhas, M.U.; Wu, P.C. Fabrication and Characterization of Diclofenac Sodium Loaded Hydrogels of Sodium Alginate as Sustained Release Carrier. Gels 2021, 7, 10. [Google Scholar] [CrossRef]
- Suhail, M.; Hsieh, Y.H.; Khan, A.; Minhas, M.U.; Wu, P.C. Preparation and In Vitro Evaluation of Aspartic/Alginic Acid Based Semi-Interpenetrating Network Hydrogels for Controlled Release of Ibuprofen. Gels 2021, 7, 68. [Google Scholar] [CrossRef]
- Abdullah, O.; Minhas, M.U.; Mahmood Ahmad, M.; Ahmad, S.; Barkat, K.; Ahmad, A. Synthesis, optimization, and evaluation of polyvinyl alcohol-based hydrogels as controlled combinatorial drug delivery system for colon cancer. Adv. Polym. Technol. 2018, 37, 8. [Google Scholar] [CrossRef]
- Sarfraz, R.M.; Khan, H.U.; Mahmood, A.; Ahmad, M.; Maheen, S.; Sher, M. Formulation and evaluation of mouth disintegrating tablets of atenolol and atorvastatin. Indian J. Pharm. Sci. 2015, 77, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Kheradmandnia, S.; Vasheghani-Farahani, E.; Nosrati, M.; Atyabi, F. Preparation and characterization of ketoprofen-loaded solid lipid nanoparticles made from beeswax and carnauba wax. Nanomed. Nanotechnol. Biol. Med. 2010, 6, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Khalid, S.H.; Qadir, M.I.; Massud, A.; Ali, M.; Khan, I.U.; Saleem, M.; Iqbal, M.S.; Asghar, S.; Gul, H. Water uptake and drug release behaviour of methyl methacrylate-co-itaconic acid [P(MMA/IA)] hydrogels cross-linked with methylene bis-acrylamide. J. Drug Deliv. Sci. Technol. 2011, 21, 249–255. [Google Scholar] [CrossRef]
- Ullah, K.; Sohail, M.; Murtaza, G.; Khan, S.A. Natural and synthetic materials based cmch/PVA hydrogels for oxaliplatin delivery: Fabrication, characterization, in-vitro and in-vivo safety profiling. Int. J. Biol. Macromol. 2019, 122, 538–548. [Google Scholar] [CrossRef] [PubMed]
- Zia, M.A.; Sohail, M.; Minhas, M.U.; Sarfraz, R.M.; Khan, S.; de Matas, M.; Hussain, Z.; Abbasi, M.; Shah, S.A.; Kousar, M. HEMA based pH-sensitive semi IPN microgels for oral delivery; A rationale approach for ketoprofen. Drug Dev. Ind. Pharm. 2020, 46, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.U.; Minhas, M.U.; Sohail, M.; Badshah, S.F.; Abdullah, O.; Khan, S.; Munir, A.; Suhail, M. Synthesis of PEG-4000-co-poly (AMPS) nanogels by cross-linking polymerization as highly responsive networks for enhancement in meloxicam solubility. Drug Dev. Ind. Pharm. 2021, 47, 465–476. [Google Scholar] [CrossRef]



| F. Code | Sol Fraction % | Gel Fration % | Drug Loaded (mg) /400 mg of Dry Gel | Polymer Volume Fration | |
|---|---|---|---|---|---|
| pH 1.2 | pH 7.4 | ||||
| CPF-1 | 10.12 ± 0.08 | 89.88 ± 0.13 | 204.96 ± 1.08 | 0.229 | 0.053 |
| CPF-2 | 08.67 ± 0.10 | 91.93 ± 0.09 | 232.30 ± 0.98 | 0.217 | 0.043 |
| CPF-3 | 06.32 ± 0.07 | 93.68 ± 0.11 | 245.43 ± 1.13 | 0.207 | 0.040 |
| CPF-4 | 11.03 ± 0.11 | 88.97 ± 0.08 | 180.64 ± 1.18 | 0.232 | 0.057 |
| CPF-5 | 09.21 ± 0.13 | 90.79 ± 0.05 | 199.31 ± 1.14 | 0.225 | 0.049 |
| CPF-6 | 08.67 ± 0.10 | 91.93 ± 0.09 | 232.30 ± 0.98 | 0.217 | 0.043 |
| CPF-7 | 09.92 ± 0.08 | 90.08± 0.12 | 196.85 ± 1.21 | 0.229 | 0.050 |
| CPF-8 | 08.67 ± 0.10 | 91.93 ± 0.09 | 232.30 ± 0.98 | 0.217 | 0.043 |
| CPF-9 | 06.89 ± 0.08 | 93.11 ± 0.13 | 248.81 ± 1.20 | 0.204 | 0.041 |
| F. Code | Dynamic Swelling Up to 36 h | Percent Drug Release Up to 36 h | ||
|---|---|---|---|---|
| pH 1.2 | pH 7.4 | pH 1.2 | pH 7.4 | |
| CPF-1 | 4.35 ± 0.24 | 18.73 ± 0.31 | 30.03 ± 0.74 | 96.35 ± 0.91 |
| CPF-2 | 4.60 ± 0.12 | 22.82 ± 0.26 | 28.62 ± 0.98 | 94.80 ± 0.78 |
| CPF-3 | 4.82 ± 0.08 | 24.70 ± 0.33 | 27.12 ± 1.20 | 91.48 ± 1.28 |
| CPF-4 | 4.31 ± 0.13 | 17.51 ± 0.28 | 23.25 ± 1.53 | 88.61 ± 1.23 |
| CPF-5 | 4.43 ± 0.10 | 20.40 ± 0.13 | 26.37 ± 1.29 | 91.90 ± 1.40 |
| CPF-6 | 4.60 ± 0.12 | 22.82 ± 0.26 | 28.62 ± 0.98 | 94.80 ± 0.78 |
| CPF-7 | 4.35 ± 0.11 | 19.63 ± 0.31 | 25.90 ± 1.39 | 90.48 ± 1.21 |
| CPF-8 | 4.60 ± 0.12 | 22.82 ± 0.26 | 28.62 ± 0.98 | 94.80 ± 0.78 |
| CPF-9 | 4.90 ± 0.19 | 24.60 ± 0.19 | 30.73 ± 1.27 | 97.22 ± 1.61 |
| F. Code | Zero Order r2 | First Order r2 | Higuchi r2 | Korsmeyer-Peppas | |
|---|---|---|---|---|---|
| r2 | n | ||||
| CPF-1 | 0.9555 | 0.9925 | 0.9919 | 0.9897 | 0.6284 |
| CPF-2 | 0.9903 | 0.9910 | 0.9639 | 0.9909 | 0.6219 |
| CPF-3 | 0.9915 | 0.9932 | 0.9796 | 0.9901 | 0.6220 |
| CPF-4 | 0.9646 | 0.9762 | 0.9812 | 0.9840 | 0.6626 |
| CPF-5 | 0.9804 | 0.9869 | 0.9829 | 0.9880 | 0.6542 |
| CPF-6 | 0.9903 | 0.9910 | 0.9639 | 0.9909 | 0.6219 |
| CPF-7 | 0.9930 | 0.9965 | 0.9794 | 0.9962 | 0.8522 |
| CPF-8 | 0.9903 | 0.9910 | 0.9639 | 0.9909 | 0.6219 |
| CPF-9 | 0.9219 | 0.9870 | 0.9880 | 0.9752 | 0.5017 |
| F. Code | Polymer (CP) g/100 g | Polymer (SpS) g/100 g | Monomer (AA) g/100 g | Initiator (APS) g/100 g | Cross-Linker (MBA) g/100 g |
|---|---|---|---|---|---|
| CPF-1 | 0.25 | 1.00 | 25 | 0.5 | 0.5 |
| CPF-2 | 0.50 | 1.00 | 25 | 0.5 | 0.5 |
| CPF-3 | 0.75 | 1.00 | 25 | 0.5 | 0.5 |
| CPF-4 | 0.50 | 0.50 | 25 | 0.5 | 0.5 |
| CPF-5 | 0.50 | 0.75 | 25 | 0.5 | 0.5 |
| CPF-6 | 0.50 | 1.00 | 25 | 0.5 | 0.5 |
| CPF-7 | 0.50 | 1.00 | 20 | 0.5 | 0.5 |
| CPF-8 | 0.50 | 1.00 | 25 | 0.5 | 0.5 |
| CPF-9 | 0.50 | 1.00 | 30 | 0.5 | 0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suhail, M.; Hsieh, Y.-H.; Shao, Y.-F.; Minhas, M.U.; Wu, P.-C. Formulation and In-Vitro Characterization of pH-Responsive Semi-Interpenetrating Polymer Network Hydrogels for Controlled Release of Ketorolac Tromethamine. Gels 2021, 7, 167. https://doi.org/10.3390/gels7040167
Suhail M, Hsieh Y-H, Shao Y-F, Minhas MU, Wu P-C. Formulation and In-Vitro Characterization of pH-Responsive Semi-Interpenetrating Polymer Network Hydrogels for Controlled Release of Ketorolac Tromethamine. Gels. 2021; 7(4):167. https://doi.org/10.3390/gels7040167
Chicago/Turabian StyleSuhail, Muhammad, Yi-Han Hsieh, Yu-Fang Shao, Muhammad Usman Minhas, and Pao-Chu Wu. 2021. "Formulation and In-Vitro Characterization of pH-Responsive Semi-Interpenetrating Polymer Network Hydrogels for Controlled Release of Ketorolac Tromethamine" Gels 7, no. 4: 167. https://doi.org/10.3390/gels7040167






