A Bio-Inspired Arched Foot with Individual Toe Joints and Plantar Fascia
Abstract
:1. Introduction
1.1. Background
1.2. Relevant Foot Anatomy
1.3. Main Joints and Movements of the Human Foot
1.4. Design Goals
2. Materials and Methods
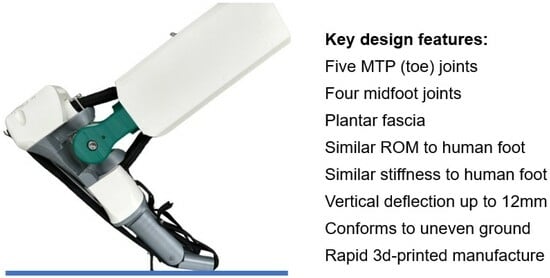
3. Design Solution
4. Modeling
4.1. Modeling Arch Stiffness
4.2. Modeling Ankle Stiffness
4.3. Modeling Windlass Mechanism
5. Results
5.1. Stiffness and Loading Tests
5.2. Range of Movement Tests
5.3. Ground Contact Test
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Angin, S.; Şimşek, I.E. Chapter 23—Ankle and foot complex Salih Angin İlkşan Demirbüken. In Comparative Kinesiology of the Human Body: Normal and Pathological Conditions; Academic Press: Cambridge, MA, USA, 2020; pp. 411–439. [Google Scholar]
- Salathé, E.P., Jr.; Arangio, G.A.; Salathe, E.P. The foot as a shock absorber. J. Biomech. 1990, 23, 655–659. [Google Scholar] [CrossRef] [PubMed]
- Kelly, L.A.; Cresswell, A.G.; Farris, D.J. The energetic behaviour of the human foot across a range of running speeds. Sci. Rep. 2018, 8, 10576. [Google Scholar] [CrossRef] [PubMed]
- Versluys, R.; Beyl, P.; Van Damme, M.; Desomer, A.; Van Ham, R.; Lefeber, D. Prosthetic feet: State-of-the-art review and the importance of mimicking human ankle–foot biomechanics. Disabil. Rehabil. Assist. Technol. 2009, 4, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Grimmer, M.; Seyfarth, A. Mimicking Human-Like Leg Function in Prosthetic Limbs. In Neuro-Robotics; Springer: Dordrecht, The Netherlands, 2014; pp. 105–155. ISBN 9789401789325. [Google Scholar]
- Bojsen-Møller, F.; Lamoreux, L. Significance of Free Dorsiflexion of the Toes in Walking. Acta Orthop. Scand. 1979, 50, 471–479. [Google Scholar] [CrossRef] [PubMed]
- McDonald, K.A.; Stearne, S.M.; Alderson, J.A.; North, I.; Pires, N.J.; Rubenson, J. The role of arch compression and metatarsophalangeal joint dynamics in modulating plantar fascia strain in running. PLoS ONE 2016, 11, e0152602. [Google Scholar] [CrossRef]
- Honert, E.C.; Bastas, G.; Zelik, K.E. Effect of toe joint stiffness and toe shape on walking biomechanics. Bioinspir. Biomim. 2018, 13, 066007. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.A.; Hagy, J.L. The Function of the Toes in Walking, Jogging and Running. Clin. Orthop. Relat. Res. 1979, 142, 24–29. [Google Scholar] [CrossRef]
- Waters, R.L.; Mulroy, S. The energy expenditure of normal and pathologic gait. Gait Posture 1999, 9, 207–231. [Google Scholar] [CrossRef]
- McDonald, K.A.; Teater, R.H.; Cruz, J.P.; Kerr, J.T.; Bastas, G.; Zelik, K.E. Adding a toe joint to a prosthesis: Walking biomechanics, energetics, and preference of individuals with unilateral below-knee limb loss. Sci. Rep. 2021, 11, 1924. [Google Scholar] [CrossRef]
- Geyer, H.; Seyfarth, A.; Blickhan, R. Compliant leg behaviour explains basic dynamics of walking and running. Proc. R. Soc. B Biol. Sci. 2006, 273, 2861–2867. [Google Scholar] [CrossRef]
- Fogelberg, D.J.; Allyn, K.J.; Smersh, M.; Maitland, M.E. What People Want in a Prosthetic Foot: A Focus Group Study. J. Prosthetics Orthot. 2016, 28, 145–151. [Google Scholar] [CrossRef]
- Sacino, A.; Cocchella, F.; De Vita, G.; Bracco, F.; Rea, F.; Sciutti, A.; Andrighetto, L. Human- or object-like? Cognitive anthropomorphism of humanoid robots. PLoS ONE 2022, 17, e0270787. [Google Scholar] [CrossRef]
- Kojima, K.; Nozawa, S.; Okada, K.; Inaba, M. Shuffle motion for humanoid robot by sole load distribution and foot force control. In Proceedings of the 2015 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Hamburg, Germany, 28 September–2 October 2015; pp. 2187–2194. [Google Scholar] [CrossRef]
- Reher, J.P.; Hereid, A.; Kolathaya, S.; Hubicki, C.M. Algorithmic Foundations of Realizing Multi-Contact Locomotion on the Humanoid Robot DURUS. In Algorithmic Foundations of Robotics XII; Springer: Cham, Switzerland, 2020; pp. 400–415. [Google Scholar]
- Reher, J.; Cousineau, E.A.; Hereid, A.; Hubicki, C.M.; Ames, A.D. Realizing dynamic and efficient bipedal locomotion on the humanoid robot DURUS. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016; pp. 1794–1801. [Google Scholar] [CrossRef]
- Kwon, S.; Park, J. Kinesiology-Based Robot Foot Design for Human-Like Walking. Int. J. Adv. Robot. Syst. 2012, 9, 259. [Google Scholar] [CrossRef]
- Chen, T.-Y.; Shigaki, S.; Hosoda, K. Bevel-geared mechanical foot: A bioinspired robotic foot compensating yaw moment of bipedal walking. Adv. Robot. 2022, 36, 631–640. [Google Scholar] [CrossRef]
- Lathrop, E.; Adibnazari, I.; Gravish, N.; Tolley, M.T. Shear Strengthened Granular Jamming Feet for Improved Performance over Natural Terrain. In Proceedings of the 2020 3rd IEEE International Conference on Soft Robotics (RoboSoft), New Haven, CT, USA, 15 May–15 July 2020. [Google Scholar]
- Windrich, M.; Grimmer, M.; Christ, O.; Rinderknecht, S.; Beckerle, P. Active lower limb prosthetics: A systematic review of design issues and solutions. BioMed. Eng. OnLine 2016, 15, 140. [Google Scholar] [CrossRef] [PubMed]
- Sanghamitra, D.; Kaushik, K. Biomedical Design of Powered Ankle- Foot Prosthesis—A Review. Mater. Today Proc. 2018, 5, 3273–3282. [Google Scholar]
- Sun, J.; Song, G.; Chu, J.; Ren, L. An Adaptive Bioinspired Foot Mechanism Based on Tensegrity Structures. Soft Robot. 2019, 6, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.; Chaparro-Rico, B.D.M.; Pavone, L.; Pasqua, G.; Cafolla, D. A Bioinspired Humanoid Foot Mechanism. Appl. Sci. 2021, 11, 1686. [Google Scholar] [CrossRef]
- Qaisera, Z.; Kanga, L.; Johnson, S. Design of a bioinspired tuneable stiffness robotic foot. Mech. Mach. Theory 2017, 110, 1–15. [Google Scholar] [CrossRef]
- Grabowski, A.M.; Rifkin, J.M.; Kram, R. K3 Promoter™ Prosthetic Foot Reduces the Metabolic Cost of Walking for Unilateral Transtibial Amputees. JPO J. Prosthet. Orthot. 2010, 22, 113–120. [Google Scholar] [CrossRef]
- Boonpratatong, A.; Ren, L. The Human Ankle-Foot Complex as a Multi-Configurable Mechanism during the Stance Phase of Walking. J. Bionic Eng. 2010, 7, 211–218. [Google Scholar] [CrossRef]
- Farris, D.J.; Birch, J.; Kelly, L. Foot stiffening during the push-off phase of human walking is linked to active muscle contraction, and not the windlass mechanism. J. R. Soc. Interface 2020, 17, 20200208. [Google Scholar] [CrossRef] [PubMed]
- Asghar, A.; Naaz, S. The transverse arch in the human feet: A narrative review of its evolution, anatomy, biomechanics and clinical implications. Morphologie 2022, 106, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Venkadesan, M.; Yawar, A.; Eng, C.M.; Dias, M.A.; Singh, D.K.; Tommasini, S.M.; Haims, A.H.; Bandi, M.M.; Mandre, S. Stiffness of the human foot and evolution of the transverse arch. Nature 2020, 579, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Welte, L.; Kelly, L.A.; Kessler, S.E.; Lieberman, D.E.; D’Andrea, S.E.; Lichtwark, G.A.; Rainbow, M.J. The extensibility of the plantar fascia influences the windlass mechanism during human running. Proc. R. Soc. B Biol. Sci. 2021, 288, 20202095. [Google Scholar] [CrossRef] [PubMed]
- Voller, T. Surgical anatomy and biomechanics of the foot. Orthop. Trauma 2022, 36, 239–243. [Google Scholar] [CrossRef]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef]
- Nicoloso, L.G.D.V.; Pelz, J.; Barrack, H.; Kuester, F. Towards 3D printing of a monocoque transtibial prosthesis using a bio-inspired design workflow. Rapid Prototyp. J. 2021, 27, 67–80. [Google Scholar] [CrossRef]
- Vujaklija, I.; Farina, D. 3D printed upper limb prosthetics. Expert Rev. Med. Devices 2018, 15, 505–512. [Google Scholar] [CrossRef]
- O’Brien, L.; Cho, E.; Khara, A.; Lavranos, J.; Lommerse, L.; Chen, C. 3D-printed custom-designed prostheses for partial hand amputation: Mechanical challenges still exist. J. Hand Ther. 2021, 34, 539–542. [Google Scholar] [CrossRef]
- Cowley, E.S.; Olenick, A.A.; McNulty, K.L.; Ross, E.Z. “Invisible Sportswomen”: The Sex Data Gap in Sport and Exercise Science Research. Women Sport Phys. Act. J. 2021, 29, 146–151. [Google Scholar] [CrossRef]
- Holdcroft, A. Gender bias in research: How does it affect evidence based medicine? J. R. Soc. Med. 2007, 100, 2–3. [Google Scholar] [CrossRef] [PubMed]
- ISO 10328:2016; Prosthetics—Structural Testing of Lower-Limb Prostheses—Requirements and Test Methods. International Organization for Standardization: Geneva, Switzerland, 2016; Edition 2.
- Lan, W.; Huang, X.; Huang, D.; Wei, X.; Chen, W. Progress in 3D printing for bone tissue engineering: A review. J. Mater. Sci. 2022, 57, 12685–12709. [Google Scholar] [CrossRef]
- Pheasant, S.; Haslegrave, C.M. Bodyspace, Anthropometry, Ergonomics and the Design of Work, 3rd ed.; CRC Press: Boca Raton, FL, USA, 1986. [Google Scholar]
- Holowka, N.B.; Wallace, I.J.; Lieberman, D.E. Foot strength and stiffness are related to footwear use in a comparison of minimally- vs. conventionally-shod populations. Sci. Rep. 2018, 8, 3679. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-W.; Hung, W.; Wu, H.-W.; Chiu, Y.-C.; Hsu, H.-C. Measurements of Foot Arch in Standing, Level Walking, Vertical Jump and Sprint Start. Int. J. Sport Exerc. Sci. 2010, 2, 31–38. [Google Scholar]
- Cheung, J.T.-M.; Zhang, M.; An, K.-N. Effects of plantar fascia stiffness on the biomechanical responses of the ankle–foot complex. Clin. Biomech. 2004, 19, 839–846. [Google Scholar] [CrossRef]
- Shepherd, M.K.; Rouse, E.J. Comparing preference of ankle–foot stiffness in below-knee amputees and prosthetists. Sci. Rep. 2020, 10, 16067. [Google Scholar] [CrossRef]
- Clites, T.R.; Shepherd, M.K.; Ingraham, K.A.; Wontorcik, L.; Rouse, E.J. Understanding patient preference in prosthetic ankle stiffness. J. NeuroEngineering Rehabil. 2021, 18, 128. [Google Scholar] [CrossRef]
- Etoundi, A.C.; Burgess, S.C.; Vaidyanathan, R. A Bio-Inspired Condylar Hinge for Robotic Limbs. J. Mech. Robot. 2013, 5, 031011. [Google Scholar] [CrossRef]
- Çaykara, T.; Sande, M.G.; Azoia, N.; Rodrigues, L.R.; Silva, C.J. Exploring the potential of polyethylene terephthalate in the design of antibacterial surfaces. Med. Microbiol. Immunol. 2020, 209, 363–372. [Google Scholar] [CrossRef]
- Ashby, M.F. Materials Selection in Mechanical Design, 2nd ed.; Elsevier Science & Technology Books: Amsterdam, The Netherlands, 1999. [Google Scholar]
- Oberg, E.; Jones, F.D.; Horton, H.; Ryffel, H.; McCauley, C. Machinery’s Handbook, 31st ed.; Industrial Press: New York, NY, USA, 2020. [Google Scholar]
- Sichting, F.; Ebrecht, F. The rise of the longitudinal arch when sitting, standing, and walking: Contributions of the windlass mechanism. PLoS ONE 2021, 16, e0249965. [Google Scholar] [CrossRef] [PubMed]
- Alazzawi, S.; Sukeik, M.; King, D.; Vemulapalli, K. Foot and ankle history and clinical examination: A guide to everyday practice. World J. Orthop. 2017, 8, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Fisher, V.; Allinger, T.L.; Ronsky, J.R.; Engsberg, J.R. Range of motion of the foot as a function of age. Foot Ankle 1992, 13, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Buldt, A.K.; Forghany, S.; Landorf, K.B.; Murley, G.S.; Levinger, P.; Menz, H.B. Centre of pressure characteristics in normal, planus and cavus feet. J. Foot Ankle Res. 2018, 11, 3. [Google Scholar] [CrossRef] [PubMed]













| Movement | Joints Involved | Key Functions |
|---|---|---|
| Dorsiflexion Plantarflexion | Ankle (talocrural or talus-tibia) joint | Walking, running |
| Eversion Inversion | Subtalar (calcaneus-talus) joint and transverse tarsal joints | Cope with uneven ground |
| Pronation | Eversion, ankle dorsiflexion, and forefoot abduction | Shock absorption in running |
| Arch deflection | Rearfoot joints, midfoot joints, and metatarsal joints | Shock absorption |
| Toe dorsiflexion | MTP joints | Running |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burgess, S.; Beeston, A.; Carr, J.; Siempou, K.; Simmonds, M.; Zanker, Y. A Bio-Inspired Arched Foot with Individual Toe Joints and Plantar Fascia. Biomimetics 2023, 8, 455. https://doi.org/10.3390/biomimetics8060455
Burgess S, Beeston A, Carr J, Siempou K, Simmonds M, Zanker Y. A Bio-Inspired Arched Foot with Individual Toe Joints and Plantar Fascia. Biomimetics. 2023; 8(6):455. https://doi.org/10.3390/biomimetics8060455
Chicago/Turabian StyleBurgess, Stuart, Alex Beeston, Joshua Carr, Kallia Siempou, Maya Simmonds, and Yasmin Zanker. 2023. "A Bio-Inspired Arched Foot with Individual Toe Joints and Plantar Fascia" Biomimetics 8, no. 6: 455. https://doi.org/10.3390/biomimetics8060455