Integrative Medicine and Helmet Constructions—A Feature Article about Milestones and Perspectives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Database Search
3. Results and Discussion
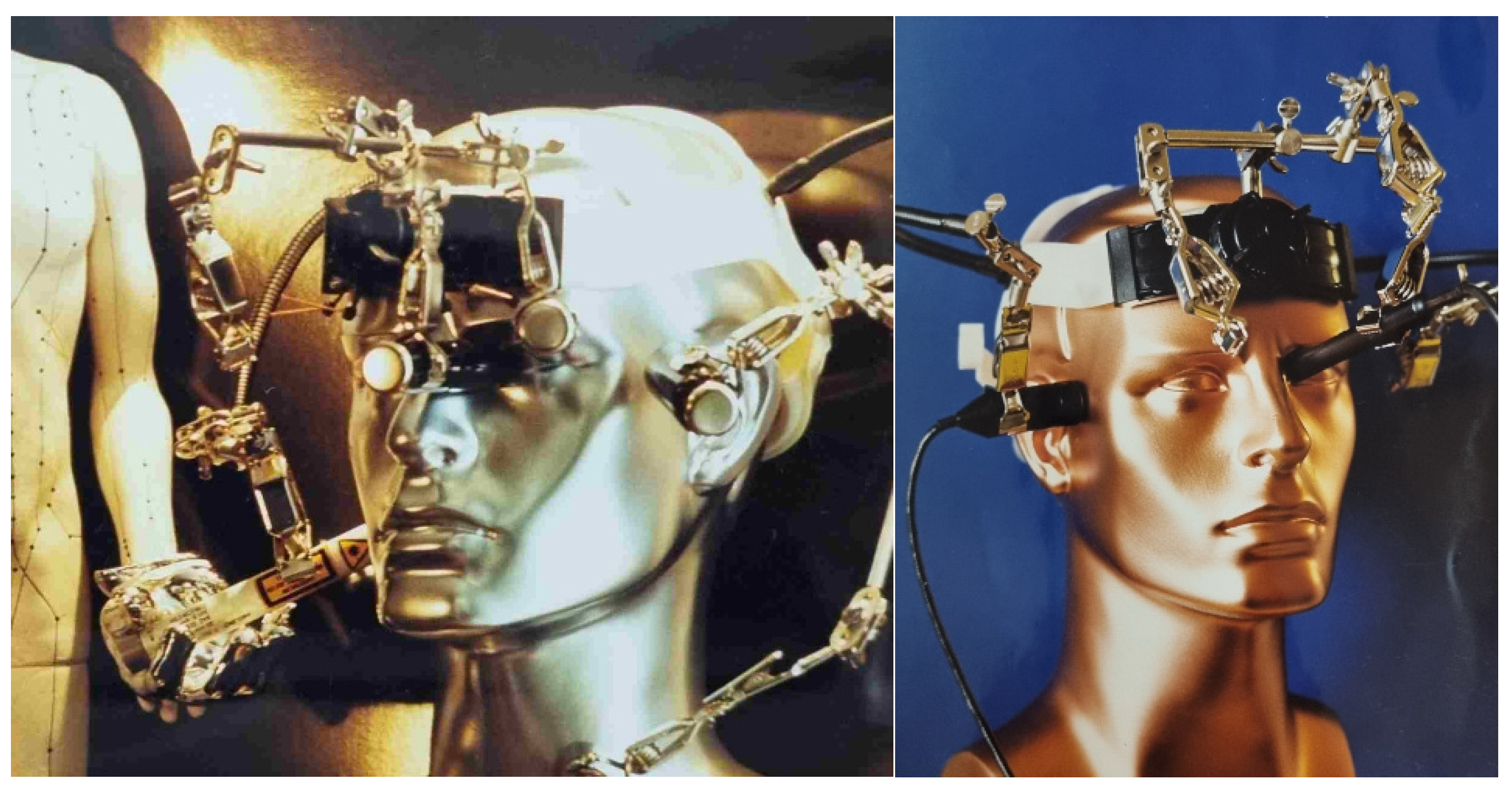
3.1. The Multifunctional Helmet as a Multimodal Sensor System in Acupuncture Research
3.2. Scientific Investigations with PBM Stimulation Helmets
4. Perspectives
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Litscher, G. Helmet constructions for acupuncture research and photobiomodulation—Including highlights from own research and development areas. Akupunkt. Aurikulomedizin. 2022; 3, in press. (In German) [Google Scholar]
- Litscher, G.; Schwarz, G.; Sandner-Kiesling, A.; Hadolt, I.; Eger, E. Effects of acupuncture on the oxygenation of cerebral tissue. Neurol. Res. 1998, 20 (Suppl. S1), S28–S32. [Google Scholar] [CrossRef] [PubMed]
- Litscher, G.; Cho, Z.H. Computer-Controlled Acupuncture; Pabst Science Publishers: Lengerich, Germany, 2000; 238p. [Google Scholar]
- Litscher, G.; Schwarz, G.; Sandner-Kiesling, A.; Hadolt, I. Transcranial Doppler sonography robotic-controlled sensors for quantification of the effects of acupuncture. Dtsch. Z. Akupunkt. (DZA) 1998, 41, 63–70. [Google Scholar]
- Litscher, G.; Wang, L.; Wiesner-Zechmeister, M. Specific effects of laserpuncture on the cerebral circulation. Lasers Med. Sci. 2000, 15, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Litscher, G. From basic science to robot-assisted acupuncture. Med. Acupunct. 2019, 31, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Lan, K.C.; Litscher, G. Robot-controlled acupuncture—An innovative step towards modernization of the ancient traditional medical treatment method. Medicines 2019, 6, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanzafame, R.J.; Blanche, R.R.; Bodian, A.B.; Chiacchierini, R.P.; Fernandez-Obregon, A.; Kazmirek, E.R. The growth of human scalp hair mediated by visible red light laser and LED sources in males. Lasers Surg. Med. 2013, 45, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Lanzafame, R.J.; Blanche, R.R.; Chiacchierini, R.P.; Kazmirek, E.R.; Sklar, J.A. The growth of human scalp hair in females using visible red light laser and LED sources. Lasers Surg. Med. 2014, 46, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Suchonwanit, P.; Chalermroj, N.; Khunkhet, S. Low-level laser therapy for the treatment of androgenetic alopecia in Thai men and women: A 24-week, randomized, double-blind, sham device-controlled trial. Lasers Med. Sci. 2019, 34, 1107–1114. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.K.; Carviel, J.L. Meta-analysis of photobiomodulation for the treatment of androgenetic alopecia. J. Dermatol. Treat. 2021, 32, 643–647. [Google Scholar] [CrossRef]
- Torres, A.E.; Lim, H.W. Photobiomodulation for the management of hair loss. Photodermatol. Photoimmunol. Photomed. 2021, 37, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Amer, M.; Nassar, A.; Attallah, H.; Amer, A. Results of low-level laser therapy in the treatment of hair growth: An Egyptian experience. Dermatol. Ther. 2021, 34, e14940. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R. Shining light on the head: Photobiomodulation for brain disorders. BBA Clin. 2016, 6, 113–124. [Google Scholar] [CrossRef] [Green Version]
- Berman, M.H.; Halper, J.P.; Nichols, T.W.; Jarrett, H.; Lundy, A.; Huang, J.H. Photobiomodulation with near infrared light helmet in a pilot, placebo controlled clinical trial in dementia patients testing memory and cognition. J. Neurol. Neurosci. 2017, 8, 176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, J.; Zaninotto, A.; Zângaro, R.A.; Carneiro, A.; Neville, I.S.; de Andrade, A.F.; Teixeira, M.J.; Paiva, W.S. Effects of transcranial LED therapy on the cognitive rehabilitation for diffuse axonal injury due to severe acute traumatic brain injury: Study protocol for a randomized controlled trial. Trials 2018, 19, 249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litscher, G. Brain photobiomodulation—Preliminary results from regional cerebral oximetry and thermal imaging. Medicines 2019, 6, 11. [Google Scholar] [CrossRef] [Green Version]
- Gefver, B. Phototherapy: Brain photomodulation makes initial steps. Laser Focus World 2020, 56, 1–4. [Google Scholar]
- Zomorrodi, R.; Loheswaran, G.; Pushparaj, A.; Lim, L. Pulsed near infrared transcranial and intranasal photobiomodulation significantly modulates neural oscillations: A pilot exploratory study. Sci. Rep. 2019, 9, 6309. [Google Scholar] [CrossRef] [Green Version]
- Salehpour, F.; Hamblin, M.R.; DiDuro, J.O. Rapid reversal of cognitive decline, olfactory dysfunction, and quality of life using multi-modality photobiomodulation therapy: Case report. Photobiomodulation Photomed. Laser Surg. 2019, 37, 159–167. [Google Scholar] [CrossRef]
- Hamilton, C.L.; El Khoury, H.; Hamilton, D.; Nicklason, F.; Mitrofanis, J. “Buckets”: Early observations on the use of red and infrared light helmets in Parkinson’s disease patients. Photobiomodulation Photomed. Laser Surg. 2019, 37, 615–622. [Google Scholar] [CrossRef]
- Berman, M.H.; Nichols, T.W. Treatment of neurodegeneration: Integrating photobiomodulation and neurofeedback in Alzheimer’s dementia and Parkinson’s: A review. Photobiomodulation Photomed. Laser Surg. 2019, 37, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, D.M.; Hamilton, C.; Gordon, L.C.; Moro, C.; Torres, N.; Nicklason, F.; Stone, J.; Benabid, A.L.; Mitrofanis, J. Exploring the use of intracranial and extracranial (remote) photobiomodulation devices in Parkinson’s disease: A comparison of direct and indirect systemic stimulations. J. Alzheimer’s Dis. (JAD) 2021, 83, 1399–1413. [Google Scholar] [CrossRef] [PubMed]
- Dougal, G.; Ennaceur, A.; Chazot, P.L. Effect of transcranial near-infrared light 1068 nm upon memory performance in aging healthy individuals: A pilot study. Photobiomodulation Photomed. Laser Surg. 2021, 39, 654–660. [Google Scholar] [CrossRef]
- Lan, K.C.; Lee, C.Y.; Wu, X.Y.; Litscher, G. An initial study on multi-point laser acupuncture based on 2D galvo mirror. Med. Acupunct. 2022, 34, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Litscher, G. A multifunctional helmet for noninvasive neuromonitoring. J. Neurosurg. Anesthesiol. 1998, 10, 116–119. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Litscher, G. Integrative Medicine and Helmet Constructions—A Feature Article about Milestones and Perspectives. Sci 2022, 4, 38. https://doi.org/10.3390/sci4040038
Litscher G. Integrative Medicine and Helmet Constructions—A Feature Article about Milestones and Perspectives. Sci. 2022; 4(4):38. https://doi.org/10.3390/sci4040038
Chicago/Turabian StyleLitscher, Gerhard. 2022. "Integrative Medicine and Helmet Constructions—A Feature Article about Milestones and Perspectives" Sci 4, no. 4: 38. https://doi.org/10.3390/sci4040038





