A Conceptual Modeling Approach to Health-Related Urban Well-Being
Abstract
:1. Introduction
2. Health-Related Urban Well-Being-Conceptual Considerations
2.1. Conceptions of Urban Health
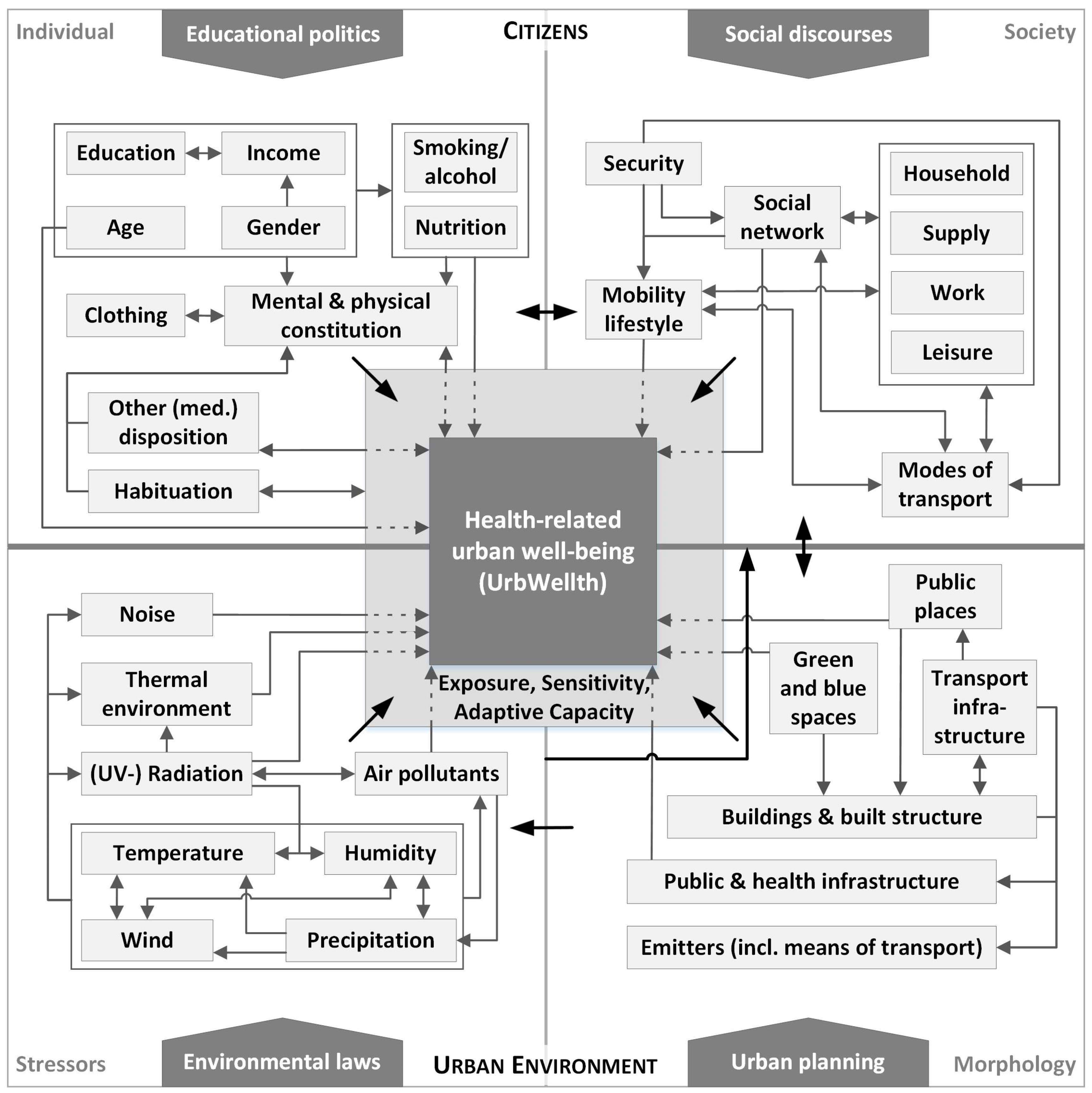
2.2. Basic Architecture of the Conceptual Model
2.3. Variables and Interrelations in the Conceptual Model
3. Health-Related Relations
3.1. Urban Impacts on Environmental Variables
3.2. Impacts on UrbWellth
3.3. Influences on Health-Related Behavior and Society
4. Discussion and Outlook
Acknowledgments
Author Contributions
Conflicts of Interest
References
- UN Habitat. The State of the World's Cities 2012: Prosperity of Cities; Routledge: London, UK, 2013. [Google Scholar]
- UN DESA. World Urbanization Prospects. The 2014 Revision: Highlights; United Nations: New York, NY, USA, 2014. [Google Scholar]
- Harlan, S.; Brazel, A.; Prashad, L.; Stefanov, W.; Larsen, L. Neighborhood microclimates and vulnerability to heat stress. Soc. Sci. Med. 2006, 63, 2847–2863. [Google Scholar] [CrossRef] [PubMed]
- Vlahov, D.; Freudenberg, N.; Proietti, F.; Ompad, D.; Quinn, A.; Nandi, V.; Galea, S. Urban as a determinant of health. J. Urban Health 2007, 3, 16–26. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 1998. Life in the 21st Century: A Vision for All; Report of the Director-General; WHO: Geneva, Switzerland, 1998. [Google Scholar]
- World Health Organization. Regional Office for Europe. In Health 2020: A European Policy Framework and Strategy for the 21st Century; WHO: Copenhagen, Denmark, 2013. [Google Scholar]
- International Council for Science. Health and Wellbeing in the Changing Urban Environment: A Systems Analysis Approach. An Interdisciplinary Science Plan; International Council for Science: Paris, France, 2011; Available online: http://www.icsu.org/publications/reports-and-reviews/health-and-wellbeing/health-and-wellbeing-in-the-changing-urban-environment (accessed on 20 September 2016).
- Kenzer, M. Healthy cities: A guide to the literature. Environ. Urban. 1999, 1, 201–220. [Google Scholar] [CrossRef]
- World Health Organization. Types of Healthy Settings. Available online: http://www.who.int/healthy_settings/types/cities/en/ (accessed on 20 September 2016).
- Bai, X.; Nath, I.; Capon, A.; Hasan, N.; Jaron, D. Health and wellbeing in the changing urban environment. Complex challenges, scientific responses, and the way forward. Curr. Opin. Environ. Sustain 2012, 4, 465–472. [Google Scholar] [CrossRef]
- Shanahan, D.F.; Lin, B.B.; Bush, R.; Gaston, K.J.; Dean, J.H.; Barber, E.; Fuller, R.A. Toward improved public health outcomes from urban nature. Am. J. Public Health 2015, 3, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Van Kamp, I.; Leidelmeijer, K.; Marsman, G.; de Hollander, A. Urban environmental quality and human well-being. Landsc. Urban Plan 2003, 1–2, 5–18. [Google Scholar] [CrossRef]
- Hancock, T. Lalonde and beyond. Looking back at “A New Perspective on the Health of Canadians”. Health Promot. Int. 1986, 1, 93–100. [Google Scholar] [CrossRef]
- Coutts, C. Green Infrastructure and Public Health; Routledge: Abingdon, UK; New York, NY, USA, 2016. [Google Scholar]
- Hancock, T. The mandala of health. A model of the human ecosystem. Fam. Community Health 1985, 3, 1–10. [Google Scholar]
- Evans, R.G.; Stoddart, G.L. Producing health, consuming health care. Soc. Sci. Med. 1990, 12, 1347–1363. [Google Scholar] [CrossRef]
- Northridge, M.E.; Sclar, E.D.; Biswas, M.P. Sorting out the connections between the built environment and health: A conceptual framework for navigating pathways and planning healthy cities. J. Urban Health 2003, 4, 556–568. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Freudenberg, N.; Vlahov, D. Cities and population health. Soc. Sci. Med. 2005, 5, 1017–1033. [Google Scholar] [CrossRef] [PubMed]
- Barton, H.; Grant, M. A health map for the local human habitat. J. R. Soc. Promot. Health 2006, 6, 252–253. [Google Scholar] [CrossRef]
- Coutts, C. Public health ecology. J. Environ. Health 2010, 72, 53–55. [Google Scholar] [PubMed]
- Mendis, S.; Banerjee, A. Cardiovascular disease: Equity and social determinants. In Equity, Social Determinants and Public Health Programmes; Blas, E., Kurup, A.S., Eds.; WHO: Geneva, Switzerland, 2010; pp. 32–48. [Google Scholar]
- Honold, J.; Beyer, R.; Lakes, T.; van der Meer, E. Multiple environmental burdens and neighborhood-related health of city residents. J. Environ. Psychol. 2012, 4, 305–317. [Google Scholar] [CrossRef]
- De Leeuw, E. Evidence for Healthy Cities: Reflections on practice, method and theory. Health Promot. Int. 2009, 24, i19–i36. [Google Scholar] [CrossRef] [PubMed]
- Rydin, Y.; Bleahu, A.; Davies, M.; Dávila, J.D.; Friel, S.; de Grandis, G.; Groce, N.; Hallal, P.C.; Hamilton, I.; Howden-Chapman, P.; et al. Shaping cities for health. Complexity and the planning of urban environments in the 21st century. Lancet 2012, 9831, 2079–2108. [Google Scholar] [CrossRef]
- Kickbush, I. The move towards a new public health. Promot. Educ. 2007, 14, 9. [Google Scholar]
- Millennium Ecosystem Assessment. Ecosystems and Human Well-Being: Synthesis; Island Press: Washington, DC, USA, 2005. [Google Scholar]
- Ballas, D. What makes a ‘happy city’? Cities 2013, 32, S39–S50. [Google Scholar] [CrossRef]
- Spiro, A.; Bossé, R. Relations between health-related quality of life and well-being: The gerontologist’s new clothes? Int. J. Aging Hum. Dev. 2000, 4, 297–318. [Google Scholar] [CrossRef] [PubMed]
- Bolund, P.; Hunhammar, S. Ecosystem services in urban areas. Ecol. Econ. 1999, 2, 293–301. [Google Scholar] [CrossRef]
- Haase, D.; Larondelle, N.; Andersson, E.; Artmann, M.; Borgstrom, S.; Breuste, J.; Gomez-Baggethun, E.; Gren, A.; Hamstead, Z.; Hansen, R.; et al. A quantitative review of urban ecosystem service assessments: concepts, models, and implementation. Ambio 2014, 4, 413–433. [Google Scholar] [CrossRef] [PubMed]
- Thomson, H.; Thomas, S. Developing empirically supported theories of change for housing investment and health. Soc. Sci. Med. 2015, 124, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.L.; Bailey, S. Third World Political Ecology: An Introduction; Routledge: London, UK, 1997. [Google Scholar]
- Bryant, R.L. Political ecology: An emerging research agenda in Third-World studies. Political Geogr. 1992, 1, 12–36. [Google Scholar] [CrossRef]
- Bourdieu, P. Die Feinen Unterschiede. Kritik Der Gesellschaftlichen Urteilskraft, 5th ed.; Suhrkamp: Frankfurt, Germany, 1992. [Google Scholar]
- Grusky, D.B. Theories of Stratification and Inequality. In The Concise Encyclopedia of Sociology; Ritzer, G., Ryan, J.M., Eds.; Wiley-Blackwell: Chichester, UK, 2011; pp. 622–624. [Google Scholar]
- Walker, G.; Bulkeley, H. Geographies of environmental justice. Geoforum 2006, 5, 655–659. [Google Scholar] [CrossRef]
- Brulle, R.J.; Pellow, D.N. Environmental justice: Human health and environmental inequalities. Annu. Rev. Public Health 2006, 27, 103–124. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W. The built environment and mental health. J. Urban Health 2003, 4, 536–555. [Google Scholar] [CrossRef] [PubMed]
- Lee, C. Environmental justice: Building a unified vision of health and the environment. Environ. Health Perspect. 2002, 2, 141–144. [Google Scholar] [CrossRef]
- Taylor, W.C.; Floyd, M.F.; Whitt-Glover, M.C.; Brooks, J. Environmental justice: A framework for collaboration between the public health and parks and recreation fields to study disparities in physical activity. J. Phys. Act. Health 2007, 4, S50–S63. [Google Scholar] [CrossRef] [PubMed]
- Bolte, G. Umweltgerechtigkeit. In Chancengleichheit bei Umwelt und Gesundheit: Konzepte, Datenlage und Handlungsperspektiven, 1 ed.; Huber: Bern, Switzerland, 2012. [Google Scholar]
- Maschewsky, W. Umweltgerechtigkeit, Public Health und Soziale Stadt; Verlag für Akademische Schriften (VAS): Frankfurt (Main), Germany, 2001. [Google Scholar]
- Sen, A. The Idea of Justice; Belknap Press of Harvard University Press: Cambridge, MA, USA, 2009. [Google Scholar]
- De Leeuw, E.; Tsouros, A.D.; Dyakova, M.; Green, G. Healthy cities. Promoting health and equity–evidence for local policy and practice. In Summary Evaluation of Phase V of the WHO European Healthy Cities Network; WHO Regional Office for Europe: Copenhagen, Denmark, 2014. [Google Scholar]
- Backman, G.; Hunt, P.; Khosla, R.; Jaramillo-Strouss, C.; Fikre, B.M.; Rumble, C.; Pevalin, D.; Páez, D.A.; Pineda, M.A.; Frisancho, A.; et al. Health systems and the right to health. An assessment of 194 countries. Lancet 2008, 9655, 2047–2085. [Google Scholar] [CrossRef]
- UN. International Covenant on Economic, Social and Cultural Rights 1966. Available online: http://www.ohchr.org/EN/ProfessionalInterest/Pages/CESCR.aspx (accessed on 20 September 2016).
- Turner, B.L.; Kasperson, R.E.; Matson, P.A.; McCarthy, J.J.; Corell, R.W.; Christensen, L.; Eckley, N.; Kasperson, J.X.; Luers, A.; Martello, M.L.; et al. A framework for vulnerability analysis in sustainability science. Proc. Natl. Acad. Sci. USA 2003, 14, 8074–8079. [Google Scholar] [CrossRef] [PubMed]
- Beck, U. Risikogesellschaft. In Auf dem Weg in eine Andere Moderne, 1st ed.; Suhrkamp: Frankfurt, Germany, 1986. (In German) [Google Scholar]
- Cutter, S.L. Hazards Vulnerability and Environmental Justice; Earthscan Publications: London, UK, 2006. [Google Scholar]
- Füssel, H.-M. Vulnerability in Climate Change Research: A Comprehensive Conceptual Framework. Breslauer, Potsdam Institute for Climate Impact Research & Stockholm Environment Institute. Working Paper. Available online: https://www.pik-potsdam.de/research/projects/projects-archive/favaia/pubs/fuessel_2005.pdf (accessed on 20 September 2016).
- Green, C. The evaluation of vulnerability to flooding. Disaster Prev. Manag. 2004, 4, 323–329. [Google Scholar] [CrossRef]
- Thornes, J.E. IPCC, 2001. Climate change 2001: Impacts, adaptation and vulnerability. Contribution of Working Group II to the Third Assessment Report of the Intergovernmental Panel on Climate Change. Int. J. Climatol. 2002, 10, 1285–1286. [Google Scholar] [CrossRef]
- European Environment Agency. Regional Climate Change and Adaptation: The Alps Facing the Challenge of Changing Water Resources; Office for Official Publ. of the Europ. Communities: Luxembourg, 2009; Available online: http://www.riob.org/IMG/pdf/EEA_Report_8-2009_Alps.pdf (accessed on 20 September 2016).
- Brooks, N. Vulnerability, risk and adaptation: A conceptual framework. Working Paper. 2003. Available online: http://www.tyndall.ac.uk/sites/default/files/wp38.pdf (accessed on 20 September 2016).
- Scheffran, J. The Security Risks of Climate Change: Vulnerabilities, Threats, Conflicts and Strategies. In Coping with Global Environmental Change, Disasters and Security: Threats, Challenges, Vulnerabilities and Risks; Brauch, H.G., Spring, U.O., Mesjasz, C., Grin, J., Kameri-Mbote, P., Chourou, B., Dunay, P., Birkmann, J., Eds.; Springer: Berlin, Germany, 2011; pp. 735–756. [Google Scholar]
- Lopez, A.D. Global Burden of Disease and Risk Factors; Oxford University Press: New York, NY, USA; World Bank: Washington, DC, USA, 2006. [Google Scholar]
- World Health Organization. Quantification of the Disease Burden Attributable to Environmental Risk Factors; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Lakes, T.; Brückner, M.; Krämer, A. Development of an environmental justice index to determine socio-economic disparities of noise pollution and green space in residential areas in Berlin. J. Environ. Plan. Manag. 2013, 4, 538–556. [Google Scholar] [CrossRef]
- Mills, G.; Cleugh, H.; Emmanuel, R.; Endlicher, W.; Erell, E.; McGranahan, G.; Ng, E.; Nickson, A.; Rosenthal, J.; Steemer, K. Climate Information for Improved Planning and Management of Mega Cities (Needs Perspective). Procedia Environ. Sci. 2010, 1, 228–246. [Google Scholar] [CrossRef]
- US EPA. EJSCREEN: Environmental Justice Screening and Mapping Tool. Available online: http://www.epa.gov/ejscreen (accessed on 20 September 2016).
- Gregory, D.; Urry, J. Social Relations and Spatial Structures; Macmillan: New York, NY, USA, 1985. [Google Scholar]
- Pohl, T. Entgrenzte Stadt. Räumliche Fragmentierung und Zeitliche Flexibilisierung in der Spätmoderne; Transcript: Bielefeld, Germany, 2009. (In German) [Google Scholar]
- Storper, M. Keys to the City. In How Economics, Institutions, Social Interactions, and Politics Shape Development; Princeton University Press: Princeton, NJ, USA, 2013. [Google Scholar]
- De Freitas, C.R.; Grigorieva, E.A. The impact of acclimatization on thermophysiological strain for contrasting regional climates. Int. J. Biometeorol. 2014, 10, 2129–2137. [Google Scholar] [CrossRef] [PubMed]
- Koppe, C.; Jendritzky, G. Inclusion of short-term adaptation to thermal stresses in a heat load warning procedure. Meteorol. Z. 2005, 2, 271–278. [Google Scholar] [CrossRef]
- Lin, T.-P. Thermal perception, adaptation and attendance in a public square in hot and humid regions. Build. Environ. 2009, 10, 2017–2026. [Google Scholar] [CrossRef]
- Froehle, A.W. Climate variables as predictors of basal metabolic rate: New equations. Am. J. Hum. Boil. 2008, 5, 510–529. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, B.; Paunovic, K.; Belojevic, G. Road-traffic noise and factors influencing noise annoyance in an urban population. Environ. Int. 2009, 3, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Jürgens, C.; Kasper, B. Alltagsmobilität, Raum und Lebensstile. In StadtLeben-Wohnen, Mobilität und Lebensstil: Neue Perspektiven für Raum- und Verkehrsentwicklung, 1st ed.; Beckmann, K.J., Ed.; VS, Verl. für Sozialwiss: Wiesbaden, Germany, 2006; pp. 125–141. (In German) [Google Scholar]
- Oßenbrügge, J.; Pohl, T.; Vogelpohl, A. Entgrenzte Zeitregime und wirtschaftsräumliche Konzentrationen. Z. Wirtsch. 2009, 53, 249–263. [Google Scholar] [CrossRef]
- Gehl, J. Leben Zwischen Häusern; Jovis Verlag: Berlin, Germany, 2012. (In German) [Google Scholar]
- Hägerstrand, T. The Impact of Transport on the Quality of Life; Lunds Universitets Kulturgeografiska Institution: Lund, Sweden, 1974. [Google Scholar]
- Hägerstrand, T. What about people in Regional Science? Pap. Reg. Sci. Assoc. 1970, 1, 6–21. [Google Scholar] [CrossRef]
- Oke, T.R. Boundary Layer Climates, 2nd ed.; Routledge: London, UK, 1987. [Google Scholar]
- Arnfield, A.J. Two decades of urban climate research: A review of turbulence, exchanges of energy and water, and the urban heat island. Int. J. Climatol. 2003, 1, 1–26. [Google Scholar] [CrossRef]
- Bechtel, B.; Schmidt, K. Floristic mapping data as a proxy for the mean Urban heat Island. Clim. Res. 2011, 1, 45–58. [Google Scholar] [CrossRef]
- Hoffmann, P.; Krueger, O.; Schlünzen, K.H. A statistical model for the urban heat island and its application to a climate change scenario. Int. J. Climatol. 2012, 8, 1238–1248. [Google Scholar] [CrossRef]
- Han, J.-Y.; Baik, J.-J.; Lee, H. Urban impacts on precipitation. Asia-Pac. J. Atmos. Sci. 2014, 1, 17–30. [Google Scholar] [CrossRef]
- Schlünzen, K.H.; Hoffmann, P.; Rosenhagen, G.; Riecke, W. Long-term changes and regional differences in temperature and precipitation in the metropolitan area of Hamburg. Int. J. Climatol. 2010, 8, 1121–1136. [Google Scholar] [CrossRef]
- Shepherd, J.M. A Review of Current Investigations of Urban-Induced Rainfall and Recommendations for the Future. Earth Interact. 2005, 12, 1–27. [Google Scholar] [CrossRef]
- Moussiopoulos, N. (Ed.) Air Quality in Cities; Springer: Berlin, Germany, 2003; p. 297. [Google Scholar]
- Mage, D.; Ozolins, G.; Peterson, P.; Webster, A.; Orthofer, R.; Vandeweerd, V.; Gwynne, M. Urban air pollution in megacities of the world. Atmos. Environ. 1996, 5, 681–686. [Google Scholar] [CrossRef]
- Ross, B.M.; Wolde, T. Ten Noise from traffic as a worldwide policy problem. Noise Control Eng. J. 2001, 4, 159. [Google Scholar] [CrossRef]
- Kheirbek, I.; Ito, K.; Neitzel, R.; Kim, J.; Johnson, S.; Ross, Z.; Eisl, H.; Matte, T. Spatial variation in environmental noise and air pollution in New York City. J. Urban Health 2014, 3, 415–431. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Burden of Disease from Environmental Noise. Quantification of Healthy Life Years Lost in Europe; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Heimann, D. Schallausbreitung Unter Meteorologischen und Topografischen Gegebenheiten. PhD thesis, Deutsches Zentrum für Luft-und Raumfahrt, Cologne, Germany, 2003. [Google Scholar]
- Kohoutek, S. Quantifizierung der Wirkungen des Straßenverkehrs auf Partikel- und Stickoxid-Immissionen. PhD thesis, Technische Universität Darmstadt, Darmstadt, Germany, 2010. [Google Scholar]
- Mayer, H. Air pollution in cities. Atmos. Environ. 1999, 24–25, 4029–4037. [Google Scholar] [CrossRef]
- Fischer, G.; Ziemann, A. Untersuchung des Einflusses der Variierenden Urbanen Grenzschicht auf die Schallausbreitung. Available online: https://www.researchgate.net/profile/Astrid_Ziemann/publication/261637274_Untersuchung_des_Einflusses_der_variierenden_urbanen_Grenzschicht_auf_die_Schallausbreitung/links/02e7e534e4f661c129000000.pdf (accessed on 20 September 2016).
- Stewart, I.D.; Oke, T.R. Local Climate Zones for Urban Temperature Studies. Bull. Am. Meteorol. Soc. 2012, 12, 1879–1900. [Google Scholar] [CrossRef]
- Schlünzen, K.H.; Grawe, D.; Bohnenstengel, S.I.; Schlüter, I.; Koppmann, R. Joint modelling of obstacle induced and mesoscale changes—Current limits and challenges. J. Wind Eng. Ind. Aerodyn. 2011, 99, 217–225. [Google Scholar] [CrossRef]
- Yang, W.; Kang, J. Acoustic comfort evaluation in urban open public spaces. Appl. Acoust. 2005, 2, 211–229. [Google Scholar] [CrossRef]
- Yang, W.; Kang, J. Soundscape and Sound Preferences in Urban Squares. A Case Study in Sheffield. J. Urban Des. 2005, 1, 61–80. [Google Scholar] [CrossRef]
- Bowler, D.E.; Buyung-Ali, L.; Knight, T.M.; Pullin, A.S. Urban greening to cool towns and cities. A systematic review of the empirical evidence. Landsc. Urban Plan. 2010, 3, 147–155. [Google Scholar] [CrossRef]
- Chen, L.; Ng, E. Simulation of the effect of downtown greenery on thermal comfort in subtropical climate using PET index. A case study in Hong Kong. Archit. Sci. Rev. 2013, 4, 297–305. [Google Scholar] [CrossRef]
- Umweltbundesamt. Umweltbewusstsein in Deutschland 2014. Ergebnisse Einer Repräsentativen Bevölkerungsumfrage; Umweltbundesamt (UBA): Dessau-Roßlau, Germany, 2015. [Google Scholar]
- Gaffron, P. Urban transport, environmental justice and human daily activity patterns. Transp. Policy 2012, 20, 114–127. [Google Scholar] [CrossRef]
- Babisch, W.; Wolf, K.; Petz, M.; Heinrich, J.; Cyrys, J.; Peters, A. Associations between traffic noise, particulate air pollution, hypertension, and isolated systolic hypertension in adults: The KORA study. Environ. Health Perspect. 2014, 5, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Babisch, W.; Wölke, G.; Heinrich, J.; Straff, W. Road traffic noise and hypertension-accounting for the location of rooms. Environ. Res. 2014, 133, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Jarup, L.; Babisch, W.; Houthuijs, D.; Pershagen, G.; Katsouyanni, K.; Cadum, E.; Dudley, M.-L.; Savigny, P.; Seiffert, I.; Swart, W.; et al. Hypertension and exposure to noise near airports: The HYENA study. Environ. Health Perspect. 2008, 3, 329–333. [Google Scholar]
- Duhme, H.; Weiland, S.K.; Keil, U.; Kraemer, B.; Schmid, M.; Stender, M.; Chambless, L. The association between self-reported symptoms of asthma and allergic rhinitis and self-reported traffic density on street of residence in adolescents. Epidemiology 1996, 6, 578–582. [Google Scholar] [CrossRef]
- Ising, H.; Lange-Asschenfeldt, H.; Lieber, G.F.; Weinhold, H.; Eilts, M. Respiratory and dermatological diseases in children with long-term exposure to road traffic immissions. Noise Health 2003, 19, 41–50. [Google Scholar]
- Hiramatsu, K.; Yamamoto, T.; Taira, K.; Ito, A.; Nakasone, T. A survey on health effects due to aircraft noise on residents living around kadena air base in the ryukyus. J. Sound Vib. 1997, 4, 451–460. [Google Scholar] [CrossRef]
- Yoshida, T.; Osada, Y.; Kawaguchi, T.; Hoshiyama, Y.; Yoshida, K.; Yamamoto, K. Effects of road traffic noise on inhabitants of tokyo. J. Sound Vib. 1997, 4, 517–522. [Google Scholar] [CrossRef]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 9341, 1233–1242. [Google Scholar] [CrossRef]
- Orru, K.; Orru, H.; Maasikmets, M.; Hendrikson, R.; Ainsaar, M. Well-being and environmental quality: Does pollution affect life satisfaction? Qual. Life Res. 2015, 25, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Faustini, A.; Stafoggia, M.; Berti, G.; Bisanti, L.; Chiusolo, M.; Cernigliaro, A.; Mallone, S.; Primerano, R.; Scarnato, C.; Simonato, L.; et al. The relationship between ambient particulate matter and respiratory mortality: A multi-city study in Italy. Eur. Respir. J. 2011, 3, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Gehring, U.; Heinrich, J.; Krämer, U.; Grote, V.; Hochadel, M.; Sugiri, D.; Kraft, M.; Rauchfuss, K.; Eberwein, H.G.; Wichmann, H.-E. Long-term exposure to ambient air pollution and cardiopulmonary mortality in women. Epidemiology 2006, 5, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Naess, O.; Nafstad, P.; Aamodt, G.; Claussen, B.; Rosland, P. Relation between concentration of air pollution and cause-specific mortality: Four-year exposures to nitrogen dioxide and particulate matter pollutants in 470 neighborhoods in Oslo, Norway. Am. J. Epidemiol. 2007, 4, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.; Burnett, R.T.; Thurston, G.D.; Thun, M.J.; Calle, E.E.; Krewski, D.; Godleski, J.J. Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004, 1, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Ziello, C.; Sparks, T.H.; Estrella, N.; Belmonte, J.; Bergmann, K.C.; Bucher, E.; Brighetti, M.A.; Damialis, A.; Detandt, M.; Galán, C.; et al. Changes to airborne pollen counts across Europe. PLoS ONE 2012, 4, e34076. [Google Scholar] [CrossRef] [PubMed]
- D’Amato, G.; Holgate, S.T.; Pawankar, R.; Ledford, D.K.; Cecchi, L.; Al-Ahmad, M.; Al-Enezi, F.; Al-Muhsen, S.; Ansotegui, I.; Baena-Cagnani, C.E.; et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ. J. 2015, 1, 407. [Google Scholar]
- Lim, Y.-H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.-C. Air pollution and symptoms of depression in elderly adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Tzivian, L.; Winkler, A.; Dlugaj, M.; Schikowski, T.; Vossoughi, M.; Fuks, K.; Hoffmann, B. Effect of long-term outdoor air pollution and noise on cognitive and psychological functions in adults. Int. J. Hyg. Environ. Health 2015, 218, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Oishi, S.; Lucas, R.E. Personality, culture, and subjective well-being: Emotional and Cognitive Evaluations of Life. Annu. Rev. Psychol. 2003, 54, 403–425. [Google Scholar] [CrossRef] [PubMed]
- Diener, E. Subjective well-being. Psychol. Bull. 1984, 95, 542–575. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.B.; Tay, L.; Diener, E. Leisure and Subjective Well-Being: A Model of Psychological Mechanisms as Mediating Factors. J. Happiness Stud. 2014, 15, 555–578. [Google Scholar] [CrossRef]
- Błażejczyk, K.; Epstein, Y.; Jendritzky, G.; Staiger, H.; Tinz, B. Comparison of UTCI to selected thermal indices. Int. J. Biometeorol. 2012, 3, 515–535. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, C.R.; Grigorieva, E.A. A comprehensive catalogue and classification of human thermal climate indices. Int. J. Biometeorol. 2015, 1, 109–120. [Google Scholar] [CrossRef] [PubMed]
- McGregor, G. Human biometeorology. Prog. Phys. Geogr. 2011, 1, 93–109. [Google Scholar] [CrossRef]
- Ali-Toudert, F.; Mayer, H. Numerical study on the effects of aspect ratio and orientation of an urban street canyon on outdoor thermal comfort in hot and dry climate. Build. Environ. 2006, 2, 94–108. [Google Scholar] [CrossRef]
- Holst, J.; Mayer, H. Impacts of street design parameters on human-biometeorological variables. Meteorol. Z. 2011, 5, 541–552. [Google Scholar] [CrossRef]
- Ketterer, C.; Matzarakis, A. Human-biometeorological assessment of heat stress reduction by replanning measures in Stuttgart, Germany. Landsc. Urban Plan. 2014, 122, 78–88. [Google Scholar] [CrossRef]
- Thorsson, S.; Rocklöv, J.; Konarska, J.; Lindberg, F.; Holmer, B.; Dousset, B.; Rayner, D. Mean radiant temperature—A predictor of heat related mortality. Urban Clim. 2014, 10, 332–345. [Google Scholar] [CrossRef]
- Theeuwes, N.E.; Solcerová, A.; Steeneveld, G.J. Modeling the influence of open water surfaces on the summertime temperature and thermal comfort in the city. J. Geophys. Res. Atmos. 2013, 16, 8881–8896. [Google Scholar] [CrossRef]
- McMichael, A.J.; Wilkinson, P.; Kovats, R.S.; Pattenden, S.; Hajat, S.; Armstrong, B.; Vajanapoom, N.; Niciu, E.M.; Mahomed, H.; Kingkeow, C.; et al. International study of temperature, heat and urban mortality: The ‘ISOTHURM’ project. Int. J. Epidemiol. 2008, 5, 1121–1131. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Xiao, Y.; Li, G.; Zeng, W.; Lin, H.; Rutherford, S.; Xu, Y.; Luo, Y.; Xu, X.; Chu, C.; et al. Temperature-mortality relationship in four subtropical Chinese cities: A time-series study using a distributed lag non-linear model. Sci. Total Environ. 2013, 449, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Wolff, R.; Yu, W.; Vaneckova, P.; Pan, X.; Tong, S. Ambient temperature and morbidity: A review of epidemiological evidence. Environ. Health Perspect. 2012, 1, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Analitis, A.; Becker, P.; Biggeri, A.; zak Bouchama, A.; De’Donato, F.; D’Ippoliti, D.; Hajat, S.; Hales, S.; Katsouyanni, K.; Kirchmayer, U.; et al. Improving Public Health Responses to Extreme Weather/heat-Waves-EuroHEAT; World Health Organization: Copenhagen, Denmark, 2009. [Google Scholar]
- Burkart, K.; Canário, P.; Breitner, S.; Schneider, A.; Scherber, K.; Andrade, H.; Alcoforado, M.J.; Endlicher, W. Interactive short-term effects of equivalent temperature and air pollution on human mortality in Berlin and Lisbon. Environ. Pollut. 2013, 183, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Babisch, W.; Swart, W.; Houthuijs, D.; Selander, J.; Bluhm, G.; Pershagen, G.; Dimakopoulou, K.; Haralabidis, A.S.; Katsouyanni, K.; Davou, E.; et al. Exposure modifiers of the relationships of transportation noise with high blood pressure and noise annoyance. J. Acoust. Soc. Am. 2012, 6, 3788–3808. [Google Scholar] [CrossRef] [PubMed]
- Bodin, T.; Albin, M.; Ardö, J.; Stroh, E.; Ostergren, P.-O.; Björk, J. Road traffic noise and hypertension: Results from a cross-sectional public health survey in southern Sweden. Environ. Health 2009, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Gusmano, M.K.; Weisz, D.; Rodwin, V.G.; Lang, J.; Qian, M.; Bocquier, A.; Moysan, V.; Verger, P. Disparities in access to health care in three French regions. Health Policy 2014, 1, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Sørgaard, K.W.; Sandlund, M.; Heikkilä, J.; Hansson, L.; Vinding, H.R.; Bjarnason, O.; Bengtsson-Tops, A.; Merinder, L.; Nilsson, L.-L.; Middelboe, T. Schizophrenia and contact with health and social services: A Nordic multi-centre study. Nord. J. Psychiatry 2003, 4, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Thorsson, S.; Tsuyoshi, H.; Lindberg, F.; Eliasson, I.; Lim, E.-M. Thermal Comfort and Outdoor Activity in Japanese Urban Public Places. Environ. Behav. 2007, 5, 660–684. [Google Scholar] [CrossRef]
- De Montigny, L.; Ling, R.; Zacharias, J. The Effects of Weather and Walking Rates in Nine Cities. Environ. Behav. 2012, 6, 821–840. [Google Scholar] [CrossRef]
- Böcker, L.; Thorsson, S. Integrated weather effects on cycling shares, frequencies, and durations in Rotterdam, the Netherlands. Weather Clim. Soc. 2014, 6, 468–481. [Google Scholar] [CrossRef]
- Eisinga, R.; Franses, P.; Vergeer, M. Weather conditions and daily television use in the Netherlands, 1996–2005. Int. J. Biometeorol. 2011, 4, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Spinney, J.E.L; Millward, H. Weather impacts on leisure activities in Halifax, Nova Scotia. Int. J. Biometeorol. 2010, 2, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, I.; Knez, I.; Westerberg, U.; Thorsson, S.; Lindberg, F. Climate and behaviour in a Nordic city. Landsc. Urban Plan 2007, 1–2, 72–84. [Google Scholar] [CrossRef]
- Knez, I.; Thorsson, S.; Eliasson, I.; Lindberg, F. Psychological mechanisms in outdoor place and weather assessment: Towards a conceptual model. Int. J. Biometeorol. 2009, 1, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Thorsson, S.; Lindqvist, M.; Lindqvist, S. Thermal bioclimatic conditions and patterns of behaviour in an urban park in Göteborg, Sweden. Int. J. Biometeorol. 2004, 48, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Zacharias, J.; Stathopoulos, T.; Wu, H. Microclimate and Downtown Open Space Activity. Environ. Behav. 2001, 2, 296–315. [Google Scholar] [CrossRef]
- Chan, C.B.; Ryan, D.A. Assessing the Effects of Weather Conditions on Physical Activity Participation Using Objective Measures. Int. J. Environ. Res. Public Health 2009, 10, 2639–2654. [Google Scholar] [CrossRef] [PubMed]
- Togo, F.; Watanabe, E.; Park, H.; Shephard, J.R.; Aoyagi, Y. Meteorology and the physical activity of the elderly: The Nakanojo Study. Int. J. Biometeorol. 2005, 2, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Sumukadas, D.; Witham, M.; Struthers, A.; McMurdo, M. Day length and weather conditions profoundly affect physical activity levels in older functionally impaired people. J. Epidemiol. Community Health 2009, 4, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Bresnahan, B.W.; Dickie, M.; Gerking, S. Averting Behavior and Urban Air Pollution. Land Econ. 1997, 3, 340–357. [Google Scholar] [CrossRef]
- Skov, T.; Cordtz, T.; Jensen, L.K.; Saugman, P.; Schmidt, K.; Theilade, P. Modifications of health behaviour in response to air pollution notifications in Copenhagen. Soc. Sci. Med. 1991, 5, 621–626. [Google Scholar] [CrossRef]
- Semenza, J.C.; Wilson, D.J.; Parra, J.; Bontempo, B.D.; Hart, M.; Sailor, D.J.; George, L.A. Public perception and behavior change in relationship to hot weather and air pollution. Environ. Res. 2008, 3, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Lercher, P.; Rudi Schmitzberger, R.; Walter Kofler, W. Perceived traffic air pollution, associated behavior and health in an alpine area. Sci. Total Environ. 1995, 1–3, 71–74. [Google Scholar] [CrossRef]
- Rotko, T.; Oglesby, L.; Künzli, N.; Carrer, P.; Nieuwenhuijsen, M.J.; Jantunen, M. Determinants of perceived air pollution annoyance and association between annoyance scores and air pollution (PM2.5, NO2) concentrations in the European EXPOLIS study. Atmos. Environ. 2002, 29, 4593–4602. [Google Scholar] [CrossRef]
- Hino, A.A.F.; Reis, R.S.; Sarmiento, O.L.; Parra, D.C.; Brownson, R.C. Built environment and physical activity for transportation in adults from Curitiba, Brazil. J. Urban Health 2014, 3, 446–462. [Google Scholar] [CrossRef] [PubMed]
- Gehl, J. Cities for People; Island Press: Washington, DC, USA, 2010. [Google Scholar]
- Bühler, R.; Kunert, U. Trends und Determinanten des Verkehrsverhaltens in den USA und in Deutschland. Forschungsprojekt im Auftrag des Bundesministeriums für Verkehr, Bau und Stadtentwicklung; Deutsches Institut für Wirtschaftsforschung and VirginiaTech: Berlin, Germany, 2008. (In German) [Google Scholar]
- Litmann, T.A. Land Use Impacts on Transport. How Land Use Factors Affect Travel Behavior; Victoria Transport Policy Institute: Victoria, Australia, 2015. [Google Scholar]
- Pucher, J. Urban Travel Behavior as the Outcome of Public Policy. The Example of Modal-Split in Western Europe and North America. J. Am. Plan. Assoc. 1988, 4, 509–520. [Google Scholar] [CrossRef]
- Yang, F.; Chen, L.; Cheng, Y.; Yao, Z.; Zhang, X. Urban public transport choice behavior analysis and service improvement policy-making. A case study from the metropolitan city, Chengdu, China. J. Appl. Stat. 2014, 4, 806–816. [Google Scholar] [CrossRef]
- Köckler, H. Umweltbezogene Gerechtigkeit und Immissionsbelastungen am Beispiel der Stadt Kassel; Kassel Univ. Press: Kassel, Germany, 2008. (In German) [Google Scholar]
- Umweltbundesamt. Umweltbedingte Krankheitslasten: Methodische Grundlagen des Environment Burden of Disease (EBD)-Ansatzes der WHO zur quantitativen Bewertung von Umweltbedingten Krankheitslasten. Chancen, Risiken und Grenzen der Methodik aus Naturwissenschaftlicher, Rechtlicher und Ethischer Perspektive (EBDreview). Available online: http://www.umweltbundesamt.de/sites/default/files/medien/378/publikationen/umwelt_und_gesundheit_05_2015_methodische_grundlagen_des_environment_burden_disease-ansatzes.pdf (accessed on 20 September 2016).
- World Health Organization. Disease and Injury Country Estimates. Available online: http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/ (accessed on 20 September 2016).
- Salim, M.M.H.; Schlünzen, K.H.; Grawe, D. Including trees in the numerical simulations of the wind flow in urban areas: Should we care? J. Wind Eng. Ind. Aerod. 2015, 144, 84–95. [Google Scholar] [CrossRef]
- Mills, G. Progress toward sustainable settlements: A role for urban climatology. Theor. Appl. Clim. 2006, 1–3, 69–76. [Google Scholar]


© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Von Szombathely, M.; Albrecht, M.; Antanaskovic, D.; Augustin, J.; Augustin, M.; Bechtel, B.; Bürk, T.; Fischereit, J.; Grawe, D.; Hoffmann, P.; et al. A Conceptual Modeling Approach to Health-Related Urban Well-Being. Urban Sci. 2017, 1, 17. https://doi.org/10.3390/urbansci1020017
Von Szombathely M, Albrecht M, Antanaskovic D, Augustin J, Augustin M, Bechtel B, Bürk T, Fischereit J, Grawe D, Hoffmann P, et al. A Conceptual Modeling Approach to Health-Related Urban Well-Being. Urban Science. 2017; 1(2):17. https://doi.org/10.3390/urbansci1020017
Chicago/Turabian StyleVon Szombathely, Malte, Myriam Albrecht, Dejan Antanaskovic, Jobst Augustin, Matthias Augustin, Benjamin Bechtel, Thomas Bürk, Jana Fischereit, David Grawe, Peter Hoffmann, and et al. 2017. "A Conceptual Modeling Approach to Health-Related Urban Well-Being" Urban Science 1, no. 2: 17. https://doi.org/10.3390/urbansci1020017
APA StyleVon Szombathely, M., Albrecht, M., Antanaskovic, D., Augustin, J., Augustin, M., Bechtel, B., Bürk, T., Fischereit, J., Grawe, D., Hoffmann, P., Kaveckis, G., Krefis, A. C., Oßenbrügge, J., Scheffran, J., & Schlünzen, K. H. (2017). A Conceptual Modeling Approach to Health-Related Urban Well-Being. Urban Science, 1(2), 17. https://doi.org/10.3390/urbansci1020017







