Use of Ultra-Translucent Monolithic Zirconia as Esthetic Dental Restorative Material: A Narrative Review
Abstract
:1. Introduction
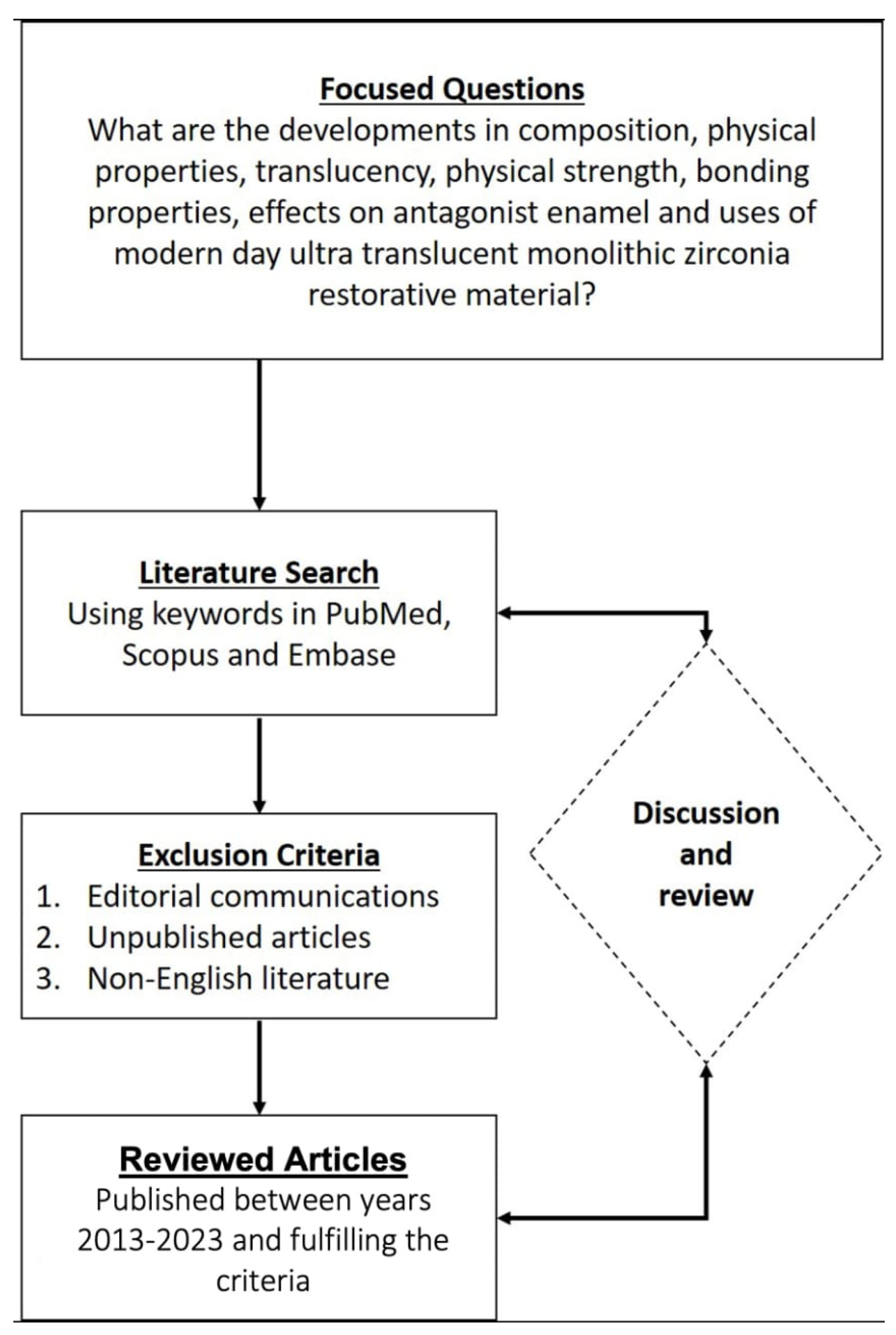
2. Search Strategy
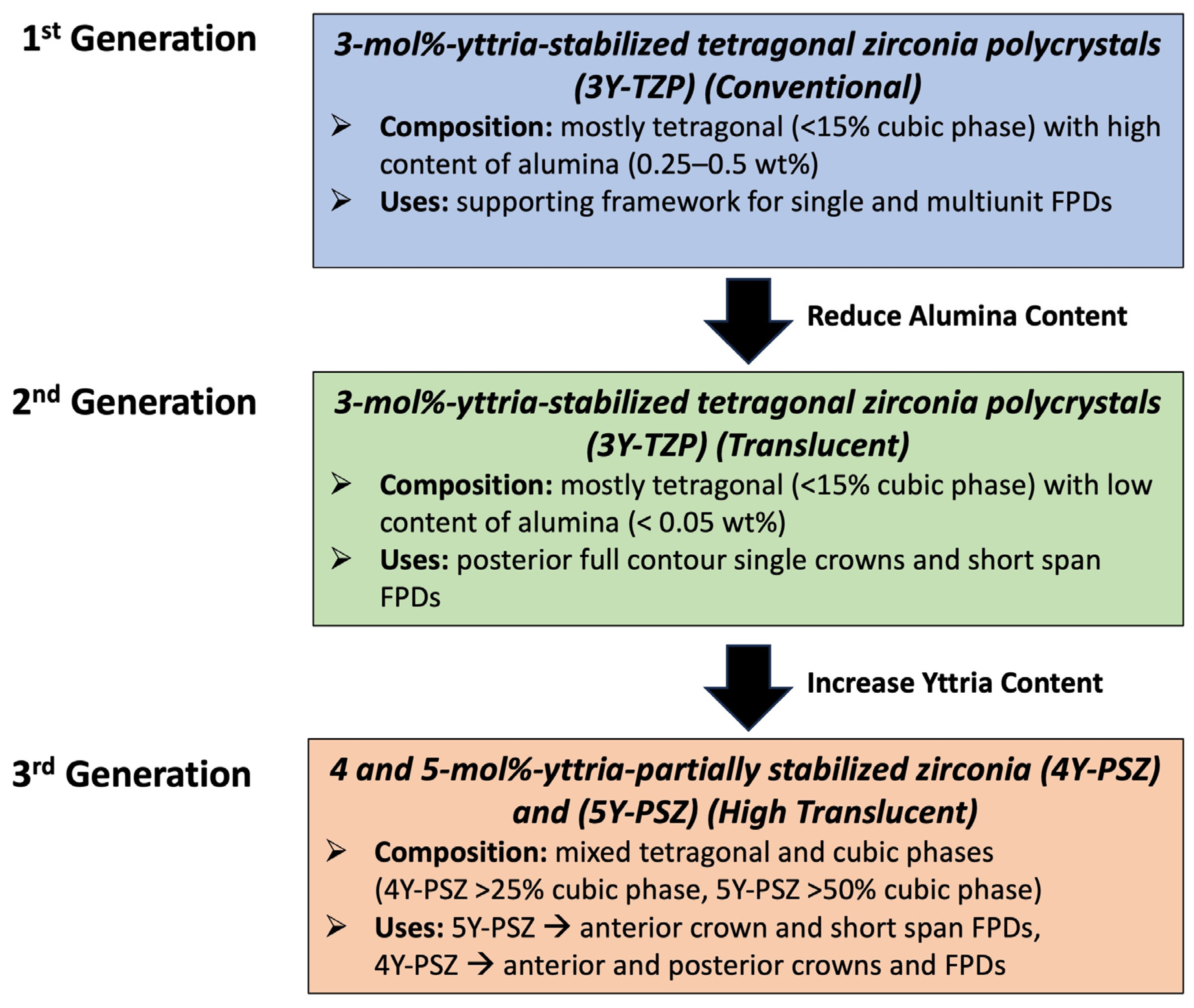
3. Development and Associated Physical Properties
4. Progress in Color Properties and Enhanced Translucency
5. Veneer Preparation Design, Marginal Fit, and Adaptation
6. Bonding Properties with Adhesive Cements
7. Effect on Antagonist Teeth
8. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Hjerppe, J.; Özcan, M. Zirconia: More and more translucent. Curr. Oral Health Rep. 2023, 10, 203–211. [Google Scholar] [CrossRef]
- Prithviraj, D.R.; Bhalla, H.K.; Vashisht, R.; Sounderraj, K.; Prithvi, S. Revolutionizing restorative dentistry: An overview. J. Indian Prosthodont. Soc. 2014, 14, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Kongkiatkamon, S.; Rokaya, D.; Kengtanyakich, S.; Peampring, C. Current classification of zirconia in dentistry: An updated review. PeerJ 2023, 11, e15669. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Reveron, H.; Spies, B.C.; Van Meerbeek, B.; Chevalier, J. Trade-off between fracture resistance and translucency of zirconia and lithium-disilicate glass ceramics for monolithic restorations. Acta Biomater. 2019, 91, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Subash, M.; Vijitha, D.; Deb, S.; Satish, A.; Mahendirakumar, N. Evaluation of shear bond strength between zirconia core and ceramic veneers fabricated by pressing and layering techniques: In vitro study. J. Pharm. Bioallied Sci. 2015, 7 (Suppl. S2), S612–S615. [Google Scholar] [PubMed]
- Zhang, Y.; Lawn, B.R. Novel zirconia materials in dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Khattar, A.; Alsaif, M.H.; Alghafli, J.A.; Alshaikh, A.A.; Alsalem, A.M.; Almindil, I.A.; Alsalman, A.M.; Alboori, A.J.; Al-Ajwad, A.M.; Almuhanna, H.M.; et al. Influence of ZrO2 nanoparticle addition on the optical properties of denture base materials fabricated using additive technologies. Nanomaterials 2022, 12, 4190. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Ghulam, O.; Krsoum, M.; Binmahmoud, S.; Taher, H.; Elmalky, W.; Zafar, M.S. Revolution of current dental zirconia: A comprehensive review. Molecules 2022, 27, 1699. [Google Scholar] [CrossRef]
- Bajraktarova-Valjakova, E.; Korunoska-Stevkovska, V.; Kapusevska, B.; Gigovski, N.; Bajraktarova-Misevska, C.; Grozdanov, A. Contemporary dental ceramic materials, A review: Chemical composition, physical and mechanical properties, indications for use. Maced. J. Med. Sci. 2018, 6, 1742–1755. [Google Scholar] [CrossRef]
- Song, X.; Ding, Y.; Zhang, J.; Jiang, C.; Liu, Z.; Lin, C.; Zheng, W.; Zeng, Y. Thermophysical and mechanical properties of cubic, tetragonal and monoclinic ZrO2. J. Mater. Res. Technol. 2023, 23, 648–655. [Google Scholar] [CrossRef]
- Zhang, Y. Making yttria-stabilized tetragonal zirconia translucent. Dent. Mater. 2014, 30, 1195–1203. [Google Scholar] [CrossRef]
- Arellano Moncayo, A.M.; Peñate, L.; Arregui, M.; Giner-Tarrida, L.; Cedeño, R. State of the art of different zirconia materials and their indications according to evidence-based clinical performance: A narrative review. Dent. J. 2023, 11, 18. [Google Scholar] [CrossRef]
- Camposilvan, E.; Leone, R.; Gremillard, L.; Sorrentino, R.; Zarone, F.; Ferrari, M.; Chevalier, J. Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications. Dent. Mater. 2018, 34, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int. 2017, 48, 369–380. [Google Scholar]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three generations of zirconia: From veneered to monolithic. Part II. Quintessence Int. 2017, 48, 441–450. [Google Scholar] [PubMed]
- Ban, S. Classification and properties of dental zirconia as implant fixtures and superstructures. Materials 2021, 14, 4879. [Google Scholar] [CrossRef]
- Leitão, C.I.; de Oliveira Fernandes, G.V.; Azevedo, L.P.; Araújo, F.M.; Donato, H.; Correia, A.R. Clinical performance of monolithic CAD/CAM tooth-supported zirconia restorations: Systematic review and meta-analysis. J. Prosthod. Res. 2022, 66, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Health 2019, 19, 134. [Google Scholar] [CrossRef]
- Kontonasaki, E.; Rigos, A.E.; Ilia, C.; Istantsos, T. Monolithic zirconia: An update to current knowledge. optical properties, wear, and clinical performance. Dent. J. 2019, 7, 90. [Google Scholar] [CrossRef]
- Kaur, D.P.; Raj, S.; Bhandari, M. Chapter 2—Recent advances in structural ceramics. In Advanced Ceramics for Versatile Interdisciplinary Applications; Singh, S., Kumar, P., Mondal, D.P., Eds.; Elsevier Series on Advanced Ceramic Materials; Elsevier: Amsterdam, The Netherlands, 2022; pp. 15–39. [Google Scholar]
- Harada, K.; Raigrodski, A.J.; Chung, K.H.; Flinn, B.D.; Dogan, S.; Mancl, L.A. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J. Prosthet. Dent. 2016, 116, 257–263. [Google Scholar] [CrossRef]
- Singh, S.P.; Sontakke, A.D. Transparent glass ceramics. Crystals 2021, 11, 156. [Google Scholar] [CrossRef]
- Kim, H.K. Optical and mechanical properties of highly translucent dental zirconia. Materials 2020, 13, 3395. [Google Scholar] [CrossRef] [PubMed]
- Kontonasaki, E.; Giasimakopoulos, P.; Rigos, A.E. Strength and aging resistance of monolithic zirconia: An update to current knowledge. Jpn. Dent. Sci. Rev. 2020, 56, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Kui, A.; Manziuc, M.; Petruțiu, A.; Buduru, S.; Labuneț, A.; Negucioiu, M.; Chisnoiu, A. translucent zirconia in fixed prosthodontics—An integrative overview. Biomedicines 2023, 11, 3116. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Paladines, Á.; Ulloa, A.L.; Paltán, C.A.; Fajardo, J.I. Comparative fracture resistance analysis of translucent monolithic zirconia dioxide milled in a cad/cam system. Ceramics 2023, 6, 1179–1190. [Google Scholar] [CrossRef]
- de Araújo-Júnior, E.N.; Bergamo, E.T.; Bastos, T.M.; Jalkh, E.B.; Lopes, A.C.; Monteiro, K.N.; Cesar, P.F.; Tognolo, F.C.; Migliati, R.; Tanaka, R.; et al. Ultra-translucent zirconia processing and aging effect on microstructural, optical, and mechanical properties. Dent. Mater. 2022, 38, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Pereira, G.K.; Venturini, A.B.; Silvestri, T.; Dapieve, K.S.; Montagner, A.F.; Soares, F.Z.; Valandro, L.F. Low-temperature degradation of Y-TZP ceramics: A systematic review and meta-analysis. J. Mech. Behav. Biomed. Mater. 2016, 55, 151–163. [Google Scholar] [CrossRef]
- Ramesh, S.; Lee, K.S.; Tan, C.Y. A review on the hydrothermal ageing behaviour of Y-TZP ceramics. Ceram. Int. 2018, 44, 20620–20634. [Google Scholar] [CrossRef]
- Zhang, F.; Vanmeensel, K.; Inokoshi, M.; Batuk, M.; Hadermann, J.; Van Meerbeek, B.; Naert, I.; Vleugels, J. Critical influence of alumina content on the low temperature degradation of 2–3 mol% yttria-stabilized TZP for dental restorations. J. Eur. Ceram. Soc. 2015, 35, 741–750. [Google Scholar] [CrossRef]
- Jia-Mahasap, W.; Jitwirachot, K.; Holloway, J.A.; Rangsri, W.; Rungsiyakull, P. Wear of various restorative materials against 5Y-ZP zirconia. J Prosthet. Dent. 2022, 128, 814.e1–814.e10. [Google Scholar] [CrossRef]
- Arya, N.R.; Gupta, R.; Weber, D.D.S.; Kurt, K. Zirconia Biomaterials. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK493144/ (accessed on 14 August 2023).
- El-Ghany, O.; Sherief, A. Zirconia based ceramics, some clinical and biological aspects: Review. Future Dent. J. 2016, 2, 55–64. [Google Scholar] [CrossRef]
- Elsayed, A.; Meyer, G.; Wille, S.; Kern, M. Influence of the yttrium content on the fracture strength of monolithic zirconia crowns after artificial aging. Quintessence Int. 2019, 50, 344–348. [Google Scholar] [PubMed]
- Almohammed, S.N.; Alshorman, B.; Abu-Naba’a, L.A. Mechanical properties of five esthetic ceramic materials used for monolithic restorations: A comparative in vitro study. Ceramics 2023, 6, 1031–1049. [Google Scholar] [CrossRef]
- Bergamo, E.T.; da Silva, W.J.; Cesar, P.F.; Del Bel Cury, A.A. Fracture load and phase transformation of monolithic zirconia crowns submitted to different aging protocols. Oper. Dent. 2016, 41, E118–E130. [Google Scholar] [CrossRef] [PubMed]
- Ban, S. Chemical durability of high translucent dental zirconia. Dent. Mater. J. 2020, 39, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Kolakarnprasert, N.; Kaizer, M.R.; Kim, D.K.; Zhang, Y. New multi-layered zirconias: Composition, microstructure and translucency. Dent. Mater. 2019, 35, 797–806. [Google Scholar] [CrossRef] [PubMed]
- Toma, F.R.; Porojan, S.D.; Vasiliu, R.D.; Porojan, L. The effect of polishing, glazing, and aging on optical characteristics of multi-layered dental zirconia with different degrees of translucency. J. Funct. Biomater. 2023, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Oshina, I.; Spigulis, J. Beer-Lambert law for optical tissue diagnostics: Current state of the art and the main limitations. J. Biomed. Opt. 2021, 26, 100901. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.Y.; Agingu, C.; Tsoi, J.K.H.; Yu, H. Effects of aging on the color and translucency of monolithic translucent y-tzp ceramics: A systematic review and meta-analysis of in vitro studies. BioMed Res. Int. 2021, 2021, 8875023. [Google Scholar] [CrossRef]
- Mekled, S.; Elwazeer, S.; Jurado, C.A.; White, J.; Faddoul, F.; Afrashtehfar, K.I.; Fischer, N.G. Ultra-translucent zirconia laminate veneers: The influence of restoration thickness and stump tooth-shade. Materials 2023, 16, 3030. [Google Scholar] [CrossRef]
- Souza, R.; Barbosa, F.; Araújo, G.; Miyashita, E.; Bottino, M.A.; Melo, R.; Zhang, Y. ultrathin monolithic zirconia veneers: Reality or future? Report of a clinical case and one-year follow-up. Oper. Dent. 2018, 43, 3–11. [Google Scholar] [CrossRef]
- Alrabeah, G.; Alamro, N.; Alghamdi, A.; Almslam, A.; Azaaqi, M. Influences of luting cement shade on the color of various translucent monolithic zirconia and lithium disilicate ceramics for veneer restorations. J. Adv. Prosthodont. 2023, 15, 238–247. [Google Scholar] [CrossRef]
- Subaşı, M.G.; Alp, G.; Johnston, W.M.; Yilmaz, B. Effects of fabrication and shading technique on the color and translucency of new-generation translucent zirconia after coffee thermocycling. J. Prosthet. Dent. 2018, 120, 603–608. [Google Scholar] [CrossRef]
- Kim, H.K.; Kim, S.H. Effect of hydrothermal aging on the optical properties of precolored dental monolithic zirconia ceramics. J. Prosthet. Dent. 2019, 121, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Bang, H.J.; Choi, N.H.; Park, E.J. Translucency and masking ability of translucent zirconia; comparison with conventional zirconia and lithium disilicate. J. Adv. Prosthodont. 2022, 14, 324–333. [Google Scholar] [CrossRef]
- Alshali, S.A.; Kazim, S.A.; Nageeb, R.; Almarshoud, H.S. Comparative evaluation of the translucency of monolithic zirconia. J. Contemp. Dent. Pract. 2020, 21, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Mohaghegh, M.; Firouzmandi, M.; Ansarifard, E.; Ramazani, L. Marginal fit of full contour monolithic zirconia in different thicknesses and layered zirconia crowns. J. Int. Soc. Prev. Community Dent. 2020, 10, 652–658. [Google Scholar] [PubMed]
- Lepe, X.; Streiff, K.R.; Johnson, G.H. Long-term retention of zirconia crowns cemented with current automixed cements. J. Prosthet. Dent. 2021, 125, 788–794. [Google Scholar] [CrossRef]
- Shokry, M.; Al-Zordk, W.; Ghazy, M. Retention strength of monolithic zirconia crowns cemented with different primer-cement systems. BMC Oral Health 2022, 22, 187. [Google Scholar] [CrossRef]
- Emerson, J.S.; Johnson, G.H.; Kronström, M.H. Comparison of retention of monolithic zirconia crowns with alumina airborne-particle abraded and nonabraded intaglio using three different cements: A clinical simulation. J. Prosthet. Dent. 2023, 131, 100.e1–100.e5. [Google Scholar] [CrossRef]
- Kusaba, K.; Komine, F.; Honda, J.; Kubochi, K.; Matsumura, H. Effect of preparation design on marginal and internal adaptation of translucent zirconia laminate veneers. Eur. J. Oral Sci. 2018, 126, 507–511. [Google Scholar] [CrossRef]
- Abdulazeez, M.I.; Majeed, M.A. Fracture strength of monolithic zirconia crowns with modified vertical preparation: A comparative in vitro study. Eur. J. Dent. 2022, 16, 209–214. [Google Scholar] [CrossRef]
- Kim, S.H.; Yeo, M.Y.; Choi, S.Y.; Park, E.J. Fracture resistance of monolithic zirconia crowns depending on different marginal thicknesses. Materials 2022, 15, 4861. [Google Scholar] [CrossRef] [PubMed]
- Tekin, Y.H.; Hayran, Y. Fracture resistance and marginal fit of the zirconia crowns with varied occlusal thickness. J. Adv. Prosthodont. 2020, 12, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.R.; Al Ajmi, M.G.; Al Dhafyan, M.; Jomah, A.; Abualsaud, H.; Almashali, M. Effect of margin designs on the marginal adaptation of zirconia copings. Acta Stomatol. Croat. 2017, 51, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Abushanan, A.; Sharanesha, R.B.; Aljuaid, B.; Alfaifi, T.; Aldurayhim, A. Fracture resistance of primary zirconia crowns: An in vitro study. Children 2022, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Saker, S.; Özcan, M. Marginal discrepancy and load to fracture of monolithic zirconia laminate veneers: The effect of preparation design and sintering protocol. Dent. Mater. J. 2021, 40, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Catramby, M.F.; do Vale, A.L.; Dos Santos, H.E.S.; Elias, C.N. Effect of sintering process on microstructure, 4-point flexural strength, and grain size of yttria-stabilized tetragonal zirconia polycrystal for use in monolithic dental restorations. J. Prosthet. Dent. 2021, 125, e1–e824. [Google Scholar] [CrossRef]
- Jurado, C.A.; Sadid-Zadeh, R.; Watanabe, H.; Robbins, C.E.; Afrashtehfar, K.I.; Fischer, N.G.; Lee, D.J. Effect of incisal preparation design on the fracture strength of monolithic zirconia-reinforced lithium silicate laminate veneers. J. Prosthodont. 2023. [Google Scholar] [CrossRef]
- Chai, S.; Bennani, V.; Aarts, J.; Lyons, K. Incisal preparation design for ceramic veneers. J. Am. Dent. Assoc. 2018, 149, 25–37. [Google Scholar] [CrossRef]
- Baig, M.R.; Qasim, S.S.; Baskaradoss, J.K. Marginal and internal fit of porcelain laminate veneers: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 131, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Paul, N.; Raghavendra Swamy, K.N.; Dhakshaini, M.R.; Sowmya, S.; Ravi, M.B. Marginal and internal fit evaluation of conventional metal-ceramic versus zirconia CAD/CAM crowns. J. Clin. Exp. Dent. 2020, 12, e31–e37. [Google Scholar] [CrossRef] [PubMed]
- Alrabeah, G.; Binhassan, F.; Al Khaldi, S.; Al Saleh, A.; Al Habeeb, K.; Anwar, S.; Habib, S.R. Effect of self-adhesive resin cement film thickness on the shear bond strength of lithium disilicate ceramic–cement–tooth triplex. Inorganics 2023, 12, 14. [Google Scholar] [CrossRef]
- Çin, V.; İzgi, A.D.; Kale, E.; Yilmaz, B. Marginal and internal fit of monolithic zirconia crowns fabricated by using two different cad-cam workflows: An in vitro study. Prosthesis 2023, 5, 35–47. [Google Scholar] [CrossRef]
- Vág, J.; Nagy, Z.; Bocklet, C.; Kiss, T.; Nagy, Á.; Simon, B.; Mikolicz, Á.; Renne, W. Marginal and internal fit of full ceramic crowns milled using CADCAM systems on cadaver full arch scans. BMC Oral Health 2020, 20, 189. [Google Scholar] [CrossRef]
- Aldakheel, M.; Aldosary, K.; Alnafissah, S.; Alaamer, R.; Alqahtani, A.; Almuhtab, N. Deep margin elevation: Current concepts and clinical considerations: A review. Medicina 2022, 58, 1482. [Google Scholar] [CrossRef]
- Heboyan, A.; Vardanyan, A.; Karobari, M.I.; Marya, A.; Avagyan, T.; Tebyaniyan, H.; Mustafa, M.; Rokaya, D.; Avetisyan, A. Dental luting cements: An updated comprehensive review. Molecules 2023, 28, 1619. [Google Scholar] [CrossRef]
- Homsy, F. Self-adhesive cements and all ceramic crowns: A review. Int. J. Dent. 2014, 2, 65–73. [Google Scholar] [CrossRef]
- Colombo, M.; Gallo, S.; Padovan, S.; Chiesa, M.; Poggio, C.; Scribante, A. Influence of different surface pretreatments on shear bond strength of an adhesive resin cement to various zirconia ceramics. Materials 2020, 13, 652. [Google Scholar] [CrossRef]
- Gołasz, P.; Kołkowska, A.; Zieliński, R.; Simka, W. Zirconium surface treatment via chemical etching. Materials 2023, 16, 7404. [Google Scholar] [CrossRef]
- Scaminaci Russo, D.; Cinelli, F.; Sarti, C.; Giachetti, L. Adhesion to zirconia: A systematic review of current conditioning methods and bonding materials. Dent. J. 2019, 7, 74. [Google Scholar] [CrossRef]
- Comino-Garayoa, R.; Peláez, J.; Tobar, C.; Rodríguez, V.; Suárez, M.J. Adhesion to zirconia: A systematic review of surface pretreatments and resin cements. Materials 2021, 14, 2751. [Google Scholar] [CrossRef]
- Alrabeah, G.; Alomar, S.; Almutairi, A.; Alali, H.; ArRejaie, A. Analysis of the effect of thermocycling on bonding cements to zirconia. Saudi Dent. J. 2023, 35, 734–740. [Google Scholar] [CrossRef]
- Blatz, M.B.; Conejo, J. cementation and bonding of zirconia restorations. Compend. Contin. Educ. Dent. 2018, 39 (Suppl. S4), 9–13. [Google Scholar]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Clinical performance of resin-matrix ceramic partial coverage restorations: A systematic review. Clin. Oral Investig. 2022, 26, 3807–3822. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.R.; Araújo, G.D.; Moura, D.M.; Araújo, L.D.; Gurgel, B.D.; Melo, R.M.; Bottino, M.A.; Özcan, M.; Zhang, Y.; Souza, R.O. Clinical Performance of Minimally Invasive Monolithic Ultratranslucent Zirconia Veneers: A Case Series up to Five Years of Follow-up. Oper. Dent. 2023, 48, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.Y.; Pang, R.; Yang, J.; Fan, D.; Cai, H.; Jiang, H.B.; Han, J.; Lee, E.S.; Sun, Y. Overview of several typical ceramic materials for restorative dentistry. BioMed Res. Int. 2022, 2022, 8451445. [Google Scholar] [CrossRef]
- Daou, E.E. The zirconia ceramic: Strengths and weaknesses. Open Dent. J. 2014, 8, 33–42. [Google Scholar] [CrossRef]
- Dikicier, S.; Korkmaz, C.; Atay, A. Surface roughness and characteristics of CAD/CAM zirconia and glass ceramics after combined treatment procedures. BMC Oral Health 2022, 22, 524. [Google Scholar] [CrossRef] [PubMed]
- Jitwirachot, K.; Rungsiyakull, P.; Holloway, J.A.; Jia-Mahasap, W. Wear Behavior of Different Generations of Zirconia: Present Literature. Int. J. Dent. 2022, 2022, 9341616. [Google Scholar] [CrossRef]
- Preis, V.; Weiser, F.; Handel, G.; Rosentritt, M. Wear performance of monolithic dental ceramics with different surface treatments. Quintessence Int. 2013, 44, 393–405. [Google Scholar] [PubMed]
- Rosentritt, M.; Preis, V.; Behr, M.; Strasser, T. Fatigue and wear behaviour of zirconia materials. J. Mech. Behav. Biomed. Mater. 2020, 110, 103970. [Google Scholar] [CrossRef] [PubMed]
- Preis, V.; Grumser, K.; Schneider-Feyrer, S.; Behr, M.; Rosentritt, M. Cycle-dependent in vitro wear performance of dental ceramics after clinical surface treatments. J. Mech. Behav. Biomed. Mater. 2016, 53, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Amer, J.Y.; Rayyan, M.M. Effect of different surface treatments and bonding modalities on the shear bond strength between metallic orthodontic brackets andglazed monolithic zirconia crowns. J. Orthod. Sci. 2018, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Esquivel-Upshaw, J.F.; Kim, M.J.; Hsu, S.M.; Abdulhameed, N.; Jenkins, R.; Neal, D.; Ren, F.; Clark, A.E. Randomized clinical study of wear of enamel antagonists against polished monolithic zirconia crowns. J. Dent. 2018, 68, 19–27. [Google Scholar] [CrossRef]
- Soleimani, F.; Jalali, H.; Mostafavi, A.S.; Zeighami, S.; Memarian, M. Retention, and clinical performance of zirconia crowns: A comprehensive review. Int. J. Dent. 2020, 2020, 8846534. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Choi, J.W.; Jeong, C.M.; Huh, J.B.; Lee, S.H.; Lee, H.; Yun, M.J. Evaluating the wear of resin teeth by different opposing restorative materials. Materials 2019, 12, 3684. [Google Scholar] [CrossRef]
- Solá-Ruíz, M.F.; Baima-Moscardó, A.; Selva-Otaolaurruchi, E.; Montiel-Company, J.M.; Agustín-Panadero, R.; Fons-Badal, C.; Fernández-Estevan, L. Wear in antagonist teeth produced by monolithic zirconia crowns: A systematic review and meta-analysis. J. Clin. Med. 2020, 9, 997. [Google Scholar] [CrossRef]
- Mundhe, K.; Jain, V.; Pruthi, G.; Shah, N. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns. J. Prosthet. Dent. 2015, 114, 358–363. [Google Scholar] [CrossRef]
- Pathan, M.S.; Kheur, M.G.; Patankar, A.H.; Kheur, S.M. Assessment of antagonist enamel wear and clinical performance of full-contour monolithic zirconia crowns: One-year results of a prospective study. J. Prosthodont. 2019, 28, e411–e416. [Google Scholar] [CrossRef]
| First Generation Lava Frame * (3M ESPE) | Second Generation Cercon ht * Dentsply Sirona | Third Generation Cercon xt * Dentsply Sirona | Lithium Disilicate IPS Emax CAD (LT) * Ivoclar Vivadent | |
|---|---|---|---|---|
| Flexural Strength (MPa) | >1100 | 1200 | 750 | 400 |
| Coefficient of Thermal Expansion (CTE) | 10.5 μm/m·K (25–500 °C) | 10.5 μm/m·K (25–500 °C) | 10.1 μm/m·K (25–500 °C) | 10.5 μm/m·K (100–500 °C) |
| Modulus of Elasticity (GPa) | 210 | 210 | 210 | 95 |
| Fracture Toughness (Mpa.m0.5) | 3.5–4.5 | 3.5–4.5 | 2.7–3.5 | 2.75 |
| Translucency ** | --- | 41% | 49% | 40.32% *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alrabeah, G.; Al-Sowygh, A.H.; Almarshedy, S. Use of Ultra-Translucent Monolithic Zirconia as Esthetic Dental Restorative Material: A Narrative Review. Ceramics 2024, 7, 264-275. https://doi.org/10.3390/ceramics7010017
Alrabeah G, Al-Sowygh AH, Almarshedy S. Use of Ultra-Translucent Monolithic Zirconia as Esthetic Dental Restorative Material: A Narrative Review. Ceramics. 2024; 7(1):264-275. https://doi.org/10.3390/ceramics7010017
Chicago/Turabian StyleAlrabeah, Ghada, Abdulrahman H. Al-Sowygh, and Samaher Almarshedy. 2024. "Use of Ultra-Translucent Monolithic Zirconia as Esthetic Dental Restorative Material: A Narrative Review" Ceramics 7, no. 1: 264-275. https://doi.org/10.3390/ceramics7010017





