Chronic Inflammation, Oxidative Stress and Adult Stem Cells
A topical collection in Cells (ISSN 2073-4409). This collection belongs to the section "Stem Cells".
Viewed by 22925Editor
Interests: dentistry; regenerative medicine; stem cells; tissue engineering
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
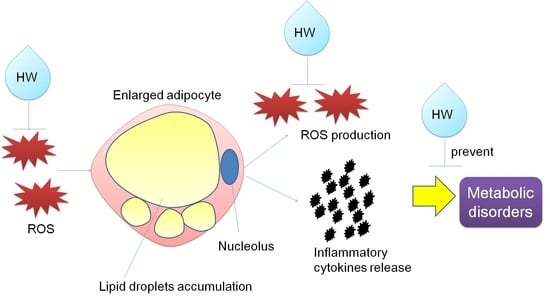
Chronic inflammation plays crucial roles in various kinds of diseases, including autoimmune diseases, cancer, arteriosclerosis, obesity, and Alzheimer's disease. Chronic inflammation is usually accompanied by reactive oxygen species (ROS), which are overproduced by activated immune cells and local fibroblasts in the tissue. When ROS overwhelm the antioxidant system, oxidative stress occurs. Oxidative stress injures cellular compounds (including DNA, proteins, and lipids), resulting in apoptotic and necrotic cell death. This process induces the secretion of proinflammatory cytokines in cells and consequently worsens the inflammation. As a result, cells and tissues eventually become functionally depleted.
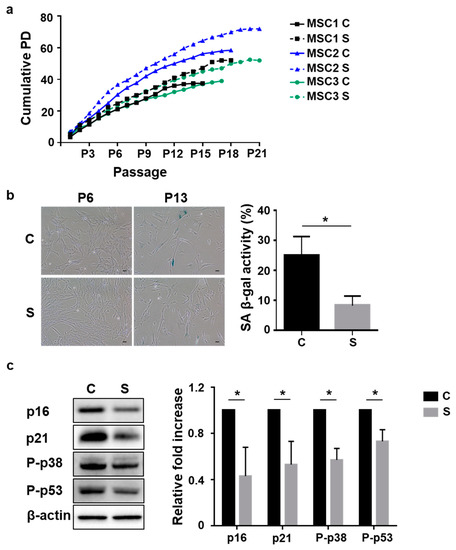
Adult stem cells (also known as somatic stem cells or tissue stem cells) are undifferentiated cells (that replace damaged functional cells) in the tissue. During chronic inflammation, adult stem cells repair oxidative-stress-induced injuries to the tissue to maintain tissue homeostasis. However, oxidative stress and inflammatory stimuli can also cause stem cell senescence or mutation that leads to the abovementioned diseases.
This Topical Collection welcomes manuscripts (including original research articles and comprehensive reviews) providing insight into aspects of the relationship between chronic inflammation, oxidative stress, and adult stem cells. We are interested in a wide range of work, including experimental, preclinical, and clinical studies.
We look forward to your contributions.
Dr. Li Xiao
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- chronic inflammation
- adult stem cells
- oxidative stress
- reactive oxygen species (ROS)
- regenerative medicine
- tissue engineering
- cell culture
- DNA damage
- aging-associated disease
- SASP (senescence-associated secretory phenotype)