Coronavirus Disease 2019: Clinical Presentation, Pathogenesis and Treatment
A topical collection in Journal of Clinical Medicine (ISSN 2077-0383). This collection belongs to the section "Infectious Diseases".
Viewed by 133832Editor
Interests: clinical immunology; tumor immunology; emergency medicine; pharmacotherapy
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
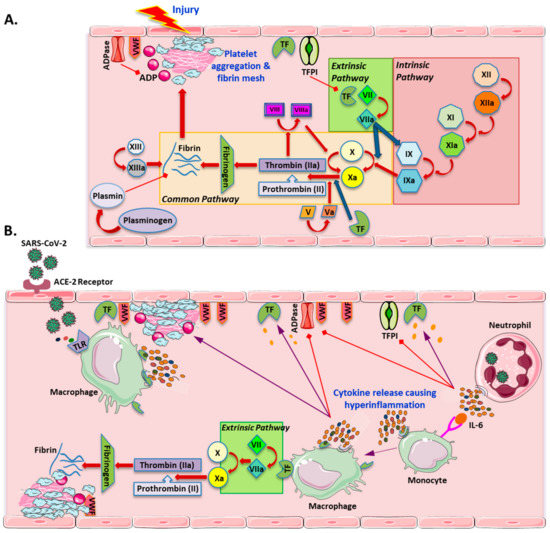
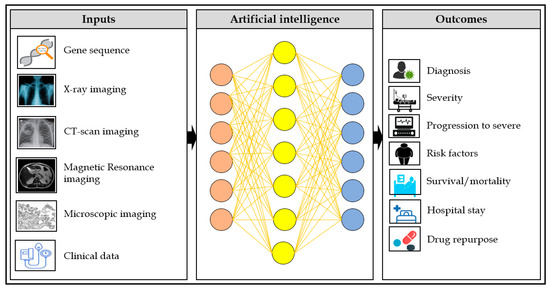
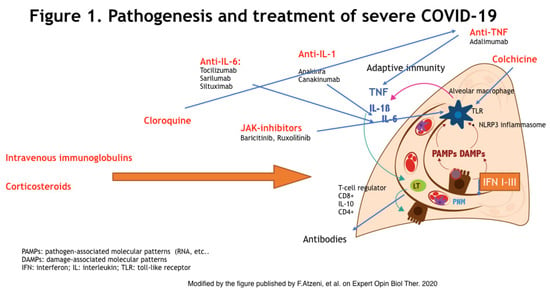
The pandemic of coronavirus disease 2019 (COVID-19) caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) represents an extraordinary challenge to world’s scientists. High infectivity of the virus, lack of effective antivirals and vaccines, and large asymptomatic populations make the disease hard to conquer. The clinical spectrum of COVID-19 appears to be abnormally wide, and its pathogenesis is yet to be decoded. Patients can experience a range of clinical manifestations, from no symptoms to critical illness. Accurate prediction of clinical outcomes for patients across this spectrum is often difficult. Advanced age and comorbidities are associated with more severe disease and poorer outcomes. In severe cases, it seems that most organ damage is done through an immune-mediated mechanism, although SARS-CoV-2 is the necessary initiator. Treatment for COVID‐19 is currently only supportive, focused on appropriate management of the associated respiratory dysfunction. The synergistic role that viral and host-dependent mechanisms play in the disease pathogenesis suggests that new therapeutic strategies must combine antiviral drugs and immune-modulating agents.
This Special Issue is aimed at offering a place to present the state of the art in basic, translational, and clinical research on COVID-19 pathogenesis, diagnosis, and management. Original and review articles dealing with the following issues are welcome:
- identification of biological and clinical markers that could optimize patient care and resource consumption;
- immunological profiling of patients;
- diagnostic value of laboratory tests and imaging techniques;
- prediction of disease severity and mortality and identification of contributing factors;
- definition and timing of optimal therapeutic approaches;
- efficacy, tolerability, and safety of specific therapies.
Prof. Dr. Vito Racanelli
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- SARS-CoV-2
- COVID-19
- pathogenesis
- clinical presentation
- diagnosis
- prognosis
- therapy