Nutritional Status of Non-Institutionalized Adults Aged over 65. Study of Weight and Health in Older Adults (PYSMA)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects and Study Design
2.2. Experimental Procedure
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shrivastava, S.R.B.L.; Shrivastava, P.S.; Ramasamy, J. Health-care of Elderly: Determinants, Needs and Services. Int. J. Prev. Med. 2013, 4, 1224–1225. [Google Scholar]
- Camina-Martín, M.A.; de Mateo-Silleras, B.; Malafarina, V.; Lopez-Mongil, R.; Niño-Martín, V.; López-Trigo, J.A.; Redondo-Del-Río, M.P. Valoración del estado nutricional en Geriatría: Declaración de consenso del Grupo de Nutrición de la Sociedad Española de Geriatría y Gerontología. Rev. Esp. Geriatr. Gerontol. 2016, 51, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Cuervo, M.; García, A.; Ansorena, D.; Sánchez-Villegas, A.; Martínez-González, M.; Astiasarán, I.; Martínez, J. Nutritional assessment interpretation on 22 007 Spanish community-dwelling elders through the Mini Nutritional Assessment test. Public Health Nutr. 2009, 12, 82–90. [Google Scholar] [CrossRef] [Green Version]
- Kaiser, M.J.; Bauer, J.M.; Ms, R.P.S.A.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef]
- Soini, H.; Suominen, M.H.; Muurinen, S.; Strandberg, T.E.; Pitkala, K.H. Malnutrition According to the Mini Nutritional Assessment in Older Adults in Different Settings. J. Am. Geriatr. Soc. 2011, 59, 765–766. [Google Scholar] [CrossRef] [PubMed]
- Childers, D.K.; Allison, D.B. The ‘obesity paradox’: A parsimonious explanation for relations among obesity, mortality rate and aging? Int. J. Obes. 2010, 34, 1231–1238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorner, T.E.; Rieder, A. Obesity paradox in elderly patients with cardiovascular diseases. Int. J. Cardiol. 2012, 155, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Monteagudo-Sánchez, C.M.; Dijkstra, S.C.; Visser, M. Self-perception of body weight status in older Dutch adults. J. Nutr. Health. Aging 2015, 19, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvadó, J.; Rubio, M.A.; Barbany, M.; Moreno, B. Consenso SEEDO 2007 para la evaluación del sobrepeso y la obesidad y el establecimiento de criterios de intervención terapéutica. Med. Clín. 2007, 128, 184–196. [Google Scholar] [CrossRef]
- Varo, J.; Martínez-González, M.; Martínez, J. Obesity prevalence in Europe. An. Sist. Sanit. Navar. 2009, 25, 103–108. [Google Scholar] [CrossRef] [Green Version]
- Özkaya, I.; Gürbüz, M. Malnourishment in the overweight and obese elderly. Nutr. Hosp. 2019, 36, 39–42. [Google Scholar]
- Cruz-Jenfot, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Cederholm, T.; Landi, F.; Rolland, Y.; Sayer, A.A.; Schneider, S.M.; Sieber, C.C.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerri, A.P.; Bellelli, G.; Mazzone, A.; Pittella, F.; Landi, F.; Zambon, A.; Annoni, G. Sarcopenia and malnutrition in acutely ill hospitalized elderly: Prevalence and outcomes. Clin. Nutr. 2015, 34, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Fielding, R.A.; Vellas, B.; Evans, W.J.; Bhasin, S.; Morley, J.E.; Newman, A.B.; van Kan, G.A.; Andrieu, S.; Bauer, J.; Breuille, D.; et al. Sarcopenia: An Undiagnosed Condition in Older Adults. Current Consensus Definition: Prevalence, Etiology, and Consequences. International Working Group on Sarcopenia. J. Am. Med. Dir. Assoc. 2011, 12, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Cabello, A.; Pedrero-Chamizo, R.; Olivares, P.R.; Luzardo, L.; Juez-Bengoechea, A.; Mata, E.; Albers, U.; Aznar, S.; Villa, G.; Espino, L.; et al. Prevalence of overweight and obesity in non-institutionalized people aged 65 or over from Spain: The elderly EXERNET multicentre study. Obes. Rev. 2011, 12, 583–592. [Google Scholar] [CrossRef]
- Gómez-Cabello, A.; Rodríguez, G.V.; Vila-Maldonado, S.; Casajús, J.A.; Ara, I. Aging and body composition: The sarcopenic obesity in Spain. Nutr. Hosp. 2012, 27, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Arribas, A.; Mata, E.; Pedrero-Chamizo, R.; Espino, L.; Gusi, N.; Villa, G.; Gonzalez-Gross, M.; Casajús, J.A.; Ara, I.; Gómez-Cabello, A. Sarcopenic obesity and physical fitness in octogenarians: The multi-center EXERNET Project. Nutr. Hosp. 2013, 28, 1877–1883. [Google Scholar] [CrossRef] [PubMed]
- Lochs, H.; Allison, S.; Meier, R.; Pirlich, M.; Kondrup, J.; Schneider, S.; Berghe, G.V.D.; Pichard, C. Introductory to the ESPEN Guidelines on Enteral Nutrition: Terminology, Definitions and General Topics. Clin. Nutr. 2006, 25, 180–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Sagarra-Romero, L.; Gómez-Cabello, A.; Pedrero-Chamizo, R.; Vila-Maldonado, S.; Gusi-Fuertes, N.; Villa-Vicente, J.G.; Espino-Torón, L.; González-Gross, M.; Casajús-Mallén, J.A.; Vicente-Rodríguez, G.; et al. Relation between educational level and body composition in non-institutionalized elderly: The elderly EXERNET multi-center study. Rev. Esp. Salud. Publica 2017, 91, e1–e15. [Google Scholar]
- Cuesta Triana, F.M.; Matia Martin, P. Detección y evaluación del anciano con desnutrición o en riesgo. Nutr. Hosp. 2011, 4, 15–27. [Google Scholar]
- Gutiérrez-Valencia, M.; Herce, P.A.; Lacalle-Fabo, E.; Escámez, B.C.; Cedeno-Veloz, B.; Martínez-Velilla, N. Prevalencia de polifarmacia y factores asociados en adultos mayores en España: Datos de la Encuesta Nacional de Salud 2017. Med. Clín. 2019, 153, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Hita-Contreras, F.; Bueno-Notivol, J.; Martínez-Amat, A.; Cruz-Díaz, D.; Hernandez, A.V.; Pérez-López, F.R. Effect of exercise alone or combined with dietary supplements on anthropometric and physical performance measures in community-dwelling elderly people with sarcopenic obesity: A meta-analysis of randomized controlled trials. Maturitas 2018, 116, 24–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Cai, L.; Cui, W.-L.; Wang, X.-M.; Li, H.-F.; He, J.-H.; Golden, A.R. Association of socioeconomic and lifestyle factors with chronic non-communicable diseases and multimorbidity among the elderly in rural southwest China. J. Public Health 2019, 42, 239–246. [Google Scholar] [CrossRef]
- Brandão, M.P.; Cardoso, M.F. Misperception of Healthy Weight: Associations Among Weight, Body Size Satisfaction and Body Appreciation in Older Adults. J. Prim. Prev. 2019, 41, 1–14. [Google Scholar] [CrossRef]
- Villareal, D.T.; Chode, S.; Parimi, N.; Sinacore, D.R.; Hilton, T.; Armamento-Villareal, R.; Napoli, N.; Qualls, C.; Shah, K. Weight Loss, Exercise, or Both and Physical Function in Obese Older Adults. N. Engl. J. Med. 2011, 364, 1218–1229. [Google Scholar] [CrossRef] [Green Version]
- Ferrer, M.D.; Capó, X.; Martorell, M.; Busquets-Cortés, C.; Bouzas, C.; Carreres, S.; Mateos, D.; Sureda, A.; Tur, J.A.; Pons, A. Regular Practice of Moderate Physical Activity by Older Adults Ameliorates Their Anti-Inflammatory Status. Nutrition 2018, 10, 1780. [Google Scholar] [CrossRef] [Green Version]
- Campbell, A.J.; Spears, G.F.S.; Brown, J.S.; Busby, W.J.; Borrie, M.J. Anthropometric Measurements as Predictors of Mortality in a Community Population Aged 70 Years and Over. Age Ageing 1990, 19, 131–135. [Google Scholar] [CrossRef]
- Aranceta, J.; Blay, G.; Carrillo, L.; Fernández, J.M.; Garaulet, M.; Gil, A. Guía de Alimentación Saludable SENC (Sociedad Española de Nutrición Comunitaria); Planeta: Madrid, Spain, 2019; ISBN 840820193X. [Google Scholar]
- Crespo, J.J.; Delgado, J.L.; Blanco, O.; Aldecoa, S. Guía básica de detección de sedentarismo y recomendaciones de actividad física en Atención Primaria. Aten Primaria 2015, 47, 175–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodríguez-Rejón, A.I.; Ruiz-López, M.D.; Artacho, R. Dietary Intake and Associated Factors in Long-Term Care Homes in Southeast Spain. Nutition 2019, 11, 266. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Koukoulis, G.N.; Sakka, C.; Katsaros, F.; Goutou, M.; Tsirona, S.; Tsiapali, E.; Piterou, A.; Stefanidis, I.; Stathakis, N. High rates of obesity prevalence in adults living in central Greece: Data from the ARGOS study. Hormones 2010, 9, 253–262. [Google Scholar] [CrossRef] [Green Version]
- Cea-Calvo, L.; Moreno, B.; Monereo, S.; Gil-Guillén, V.; Lozano, J.V.; Martí-Canales, J.C.; Llisterri, J.L.; Aznar, J.; González-Esteban, J.; Redón, J.; et al. Prevalence and related factors of overweight and obesity in Spanish population aged 60 years-old or older. The PREV-ICTUS study. Med. Clin. 2008, 131, 205–210. [Google Scholar] [CrossRef] [PubMed]
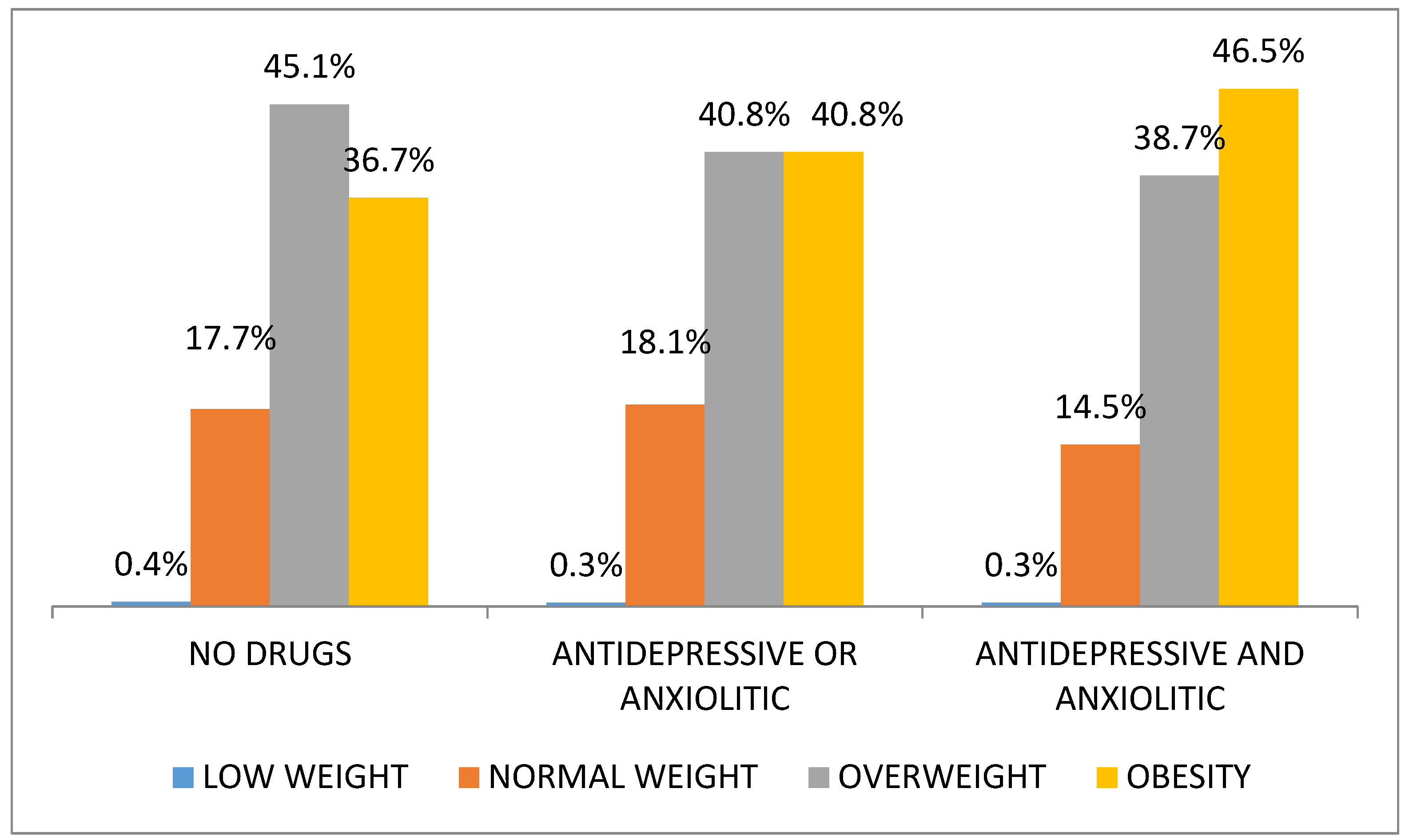
- Gafoor, R.; Booth, H.P.; Gulliford, M.C. Antidepressant utilisation and incidence of weight gain during 10 years’ follow-up: Population based cohort study. BMJ 2018, 361, k1951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, B.J.; Beasley, T.M.; Brown, A.W.; Dawson, J.; Dimova, R.; Divers, J.; Goldsby, T.U.; Heo, M.; Kaiser, K.A.; Keith, S.W.; et al. Common scientific and statistical errors in obesity research. Obesity 2016, 24, 781–790. [Google Scholar] [CrossRef]
| Men | Women | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | ||
| 1000 | 38.2% | 1621 | 61.8% | |||
| Age Group (years) | 65–69 | 251 | 25.1% | 486 | 30.0% | 0.006 * |
| 70–74 | 261 | 26.1% | 447 | 27.6% | ||
| 75–79 | 217 | 21.7% | 340 | 21.0% | ||
| 80–84 | 186 | 18.6% | 247 | 15.2% | ||
| ≥85 | 85 | 8.5% | 101 | 6.2% | ||
| Economic Allowance—Economic Contribution Pharmacy Expenses (Euros-%) | TSI01 < 18.000€—0% | 68 | 7.0% | 154 | 9.9% | 0.011 * |
| TSI02 < 18.000€—10% | 763 | 78.7% | 1239 | 79.3% | ||
| TSI02B 18–100.000€—10% | 71 | 7.3% | 85 | 5.4% | ||
| TSI06B Work Insurance—30% | 56 | 5.8% | 76 | 4.9% | ||
| TSI05 > 100.000€—60% | 12 | 1.2% | 9 | 0.6% | ||
| Variety Food Main Meals | Full breakfast | 92 | 10.2% | 189 | 12.7% | 0.166 * |
| Complete lunch | 733 | 79.0% | 1231 | 81.4% | 0.104 * | |
| Complete dinner | 403 | 43.8% | 630 | 42.1% | 0.421 ** | |
| Physical Activity | Sedentary lifestyle | 149 | 15.4% | 316 | 20.2% | 0.000 * |
| Light (walk) | 507 | 52.3% | 896 | 57.3% | ||
| Moderate (1–3 days/week) | 213 | 22.0% | 267 | 17.1% | ||
| Intense (>3 days/week) | 101 | 10.4% | 84 | 5.4% | ||
| Polypharmacy and Drug Consumption Frequency | 5 or more drugs | 531 | 54.7% | 868 | 55.5% | 0.712 ** |
| Anxiolytics | 223 | 23.0% | 617 | 39.5% | 0.000 ** | |
| Antidepressants | 113 | 11.6% | 363 | 23.2% | 0.000 ** | |
| Anxiolytics+antidepressants | 68 | 6.8% | 242 | 14.9% | 0.000 * | |
| Antiparkinsonians | 45 | 4.6% | 141 | 9.0% | 0.000 ** | |
| Percentiles | Men (n = 1000) | ||||
|---|---|---|---|---|---|
| 65–69 years | 70–74 years | 75–79 years | 80–84 years | ≥85 years | |
| P5 | 22.83 | 21.99 | 23.01 | 22.56 | 21.79 |
| P10 | 23.97 | 24.11 | 23.81 | 24.08 | 22.79 |
| P25 | 26.05 | 26.01 | 25.70 | 25.76 | 25.03 |
| P50 | 28.87 | 28.31 | 28.04 | 28.28 | 28.27 |
| P75 | 31.93 | 31.12 | 30.10 | 30.85 | 31.07 |
| P90 | 34.77 | 33.45 | 33.23 | 33.41 | 33.68 |
| P95 | 37.05 | 35.26 | 34.99 | 34.97 | 35.47 |
| Women (n = 1621) | |||||
| 65–69 years | 70–74 years | 75–79 years | 80–84 years | ≥85 years | |
| P5 | 21.57 | 22.31 | 22.05 | 22.27 | 19.48 |
| P10 | 22.83 | 23.93 | 23.48 | 23.71 | 21.83 |
| P25 | 25.80 | 26.28 | 26.05 | 25.63 | 25.14 |
| P50 | 29.02 | 29.38 | 29.77 | 28.93 | 28.03 |
| P75 | 32.58 | 32.64 | 32.38 | 32.31 | 30.19 |
| P90 | 36.69 | 36.29 | 35.47 | 35.20 | 34.52 |
| P95 | 38.82 | 39.26 | 37.86 | 37.20 | 35.81 |
| BMI | |||||
|---|---|---|---|---|---|
| Age Group | <18.5 | 18.5–24.9 | 25–29.9 | ≥30 | |
| Underweight | Normalweight | Overweight | Obesity | ||
| MEN | 65–69 | 16.7% | 40.2% | 43.0% | |
| 70–74 | 0.8% | 13.8% | 52.5% | 33.0% | |
| 75–79 | 0.5% | 18.4% | 55.8% | 25.3% | |
| 80–84 | 0.5% | 16.1% | 49.5% | 33.9% | |
| ≥85 | 24.7% | 47.1% | 28.2% | ||
| All groups | 0.4% | 16.9% | 49.1% | 33.6% | |
| WOMEN | 65–69 | 0.2% | 18.9% | 40.5% | 40.3% |
| 70–74 | 0.4% | 14.5% | 40.7% | 44.3% | |
| 75–79 | 0.3% | 16.5% | 35.3% | 47.9% | |
| 80–84 | 21.1% | 38.1% | 40.9% | ||
| ≥85 | 2.0% | 22.8% | 48.5% | 26.7% | |
| All groups | 0.4% | 17.8% | 39.6% | 42.3% | |
| Types of Cities | ||||
|---|---|---|---|---|
| Rural | Semi-Urban | Urban | Total | |
| Level of physical activity | ||||
| Sedentary lifestyle | 13.4% * | 23.80% | 17.80% | 18.50% |
| Light physical activity (walk) | 55.10% | 53.50% | 55.90% | 55.40% |
| Moderate physical activity (1–3 days/week) | 21.8% * | 16.70% | 19.00% | 18.80% |
| Intense physical activity (>3 days/week) | 9.70% | 6.00% | 7.30% | 7.30% |
| Variety of food groups main meals | ||||
| Full breakfast | 8.00% | 11.40% | 12.20% | 11.70% |
| Complete lunch | 79.20% | 78.80% | 81.10% | 80.60% |
| Complete dinner | 45.00% | 44.20% | 42.10% | 42.70% |
| Polypharmacy | 63.0% φ | 55.80% | 54.40% | 55.40% |
| (5 or more drugs) | ||||
| 95% C.I. EXP(B) | ||||||
|---|---|---|---|---|---|---|
| B | Standard Error | p-Value. | Exp(B) | Low | High | |
| SEX | 0.114 | 0.114 | 0.316 | 1.121 | 0.897 | 1.400 |
| AGE GROUPS | 0.001 | |||||
| 65–69 years | 0.719 | 0.206 | 0.000 | 2.053 | 1.372 | 3.071 |
| 70–74 years | 0.846 | 0.208 | 0.000 | 2.331 | 1.550 | 3.506 |
| 75–79 years | 0.544 | 0.210 | 0.009 | 1.722 | 1.142 | 2.597 |
| 80–84 years | 0.457 | 0.217 | 0.035 | 1.579 | 1.032 | 2.416 |
| ECONOMIC CONTRIBUTION PHARMACY EXPENSES (TS) | −0.175 | 0.080 | 0.028 | 0.839 | 0.717 | 0.982 |
| PHYSICAL ACTIVITY LEVEL | 0.026 | |||||
| Sedentary lifestyle | 0.475 | 0.236 | 0.044 | 1.608 | 1.012 | 2.553 |
| Light physical activity (walk) | 0.321 | 0.201 | 0.109 | 1.379 | 0.931 | 2.043 |
| Moderate physical activity (1–3 days/week) | 0.007 | 0.217 | 0.974 | 1.007 | 0.659 | 1.540 |
| FOOD VARIETY IN DINNER | 0.248 | 0.109 | 0.023 | 1.281 | 1.034 | 1.586 |
| POLIPHARMACY | 0.285 | 0.112 | 0.011 | 1.330 | 1.068 | 1.657 |
| Constant | 1.005 | 0.324 | 0.002 | 2.733 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mozo-Alonso, F.; Novalbos-Ruiz, J.P.; Duran-Alonso, J.C.; Rodríguez-Martin, A. Nutritional Status of Non-Institutionalized Adults Aged over 65. Study of Weight and Health in Older Adults (PYSMA). Nutrients 2021, 13, 1561. https://doi.org/10.3390/nu13051561
Mozo-Alonso F, Novalbos-Ruiz JP, Duran-Alonso JC, Rodríguez-Martin A. Nutritional Status of Non-Institutionalized Adults Aged over 65. Study of Weight and Health in Older Adults (PYSMA). Nutrients. 2021; 13(5):1561. https://doi.org/10.3390/nu13051561
Chicago/Turabian StyleMozo-Alonso, Felipe, José P. Novalbos-Ruiz, Juan C. Duran-Alonso, and Amelia Rodríguez-Martin. 2021. "Nutritional Status of Non-Institutionalized Adults Aged over 65. Study of Weight and Health in Older Adults (PYSMA)" Nutrients 13, no. 5: 1561. https://doi.org/10.3390/nu13051561
APA StyleMozo-Alonso, F., Novalbos-Ruiz, J. P., Duran-Alonso, J. C., & Rodríguez-Martin, A. (2021). Nutritional Status of Non-Institutionalized Adults Aged over 65. Study of Weight and Health in Older Adults (PYSMA). Nutrients, 13(5), 1561. https://doi.org/10.3390/nu13051561








