Comparison of Recurrent Laryngeal Nerve Identification Time in the Lower Central Triangle during Thyroid Surgery Using Neurophysiological Mapping and Monitoring
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
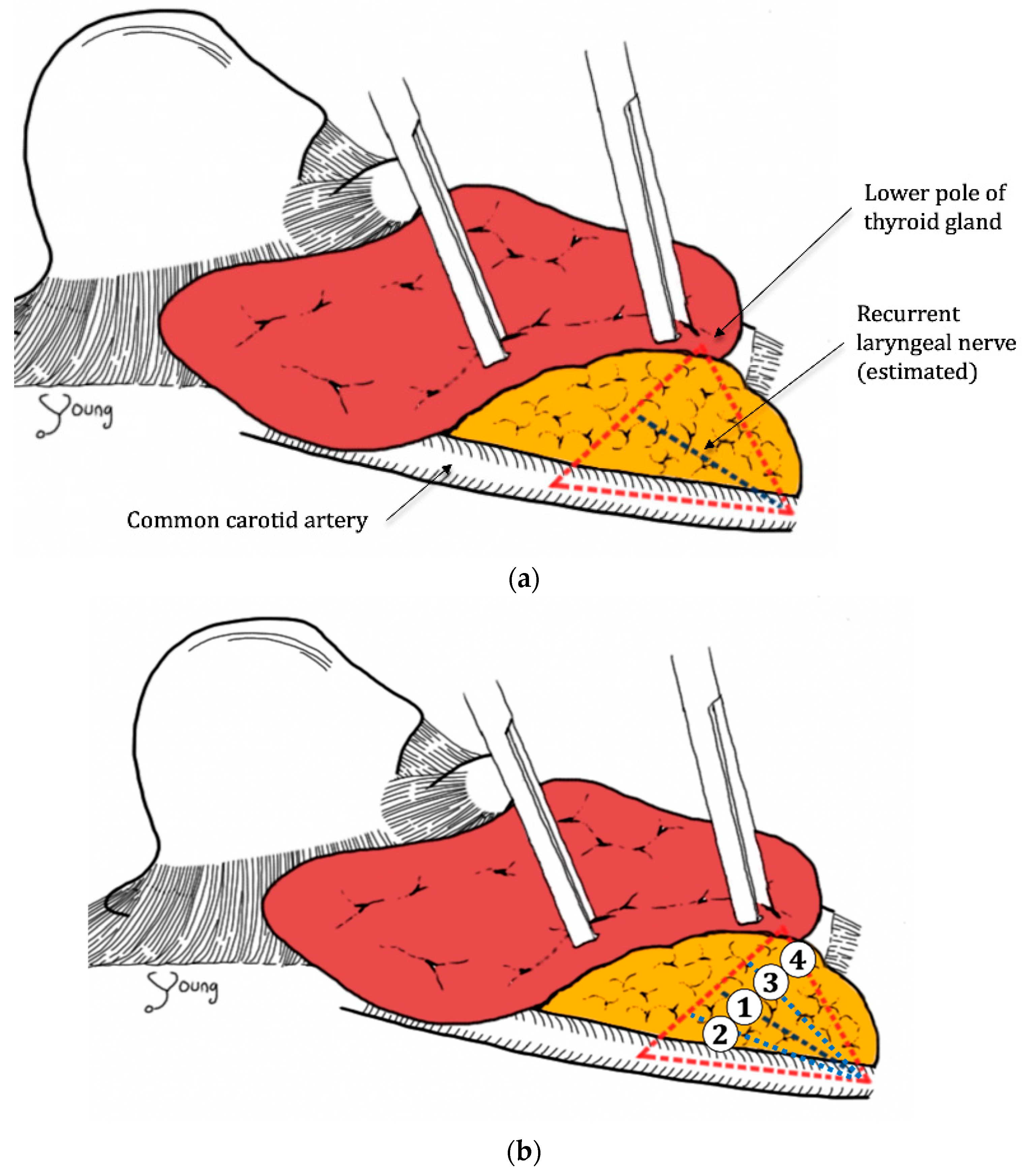
2.2. Procedure
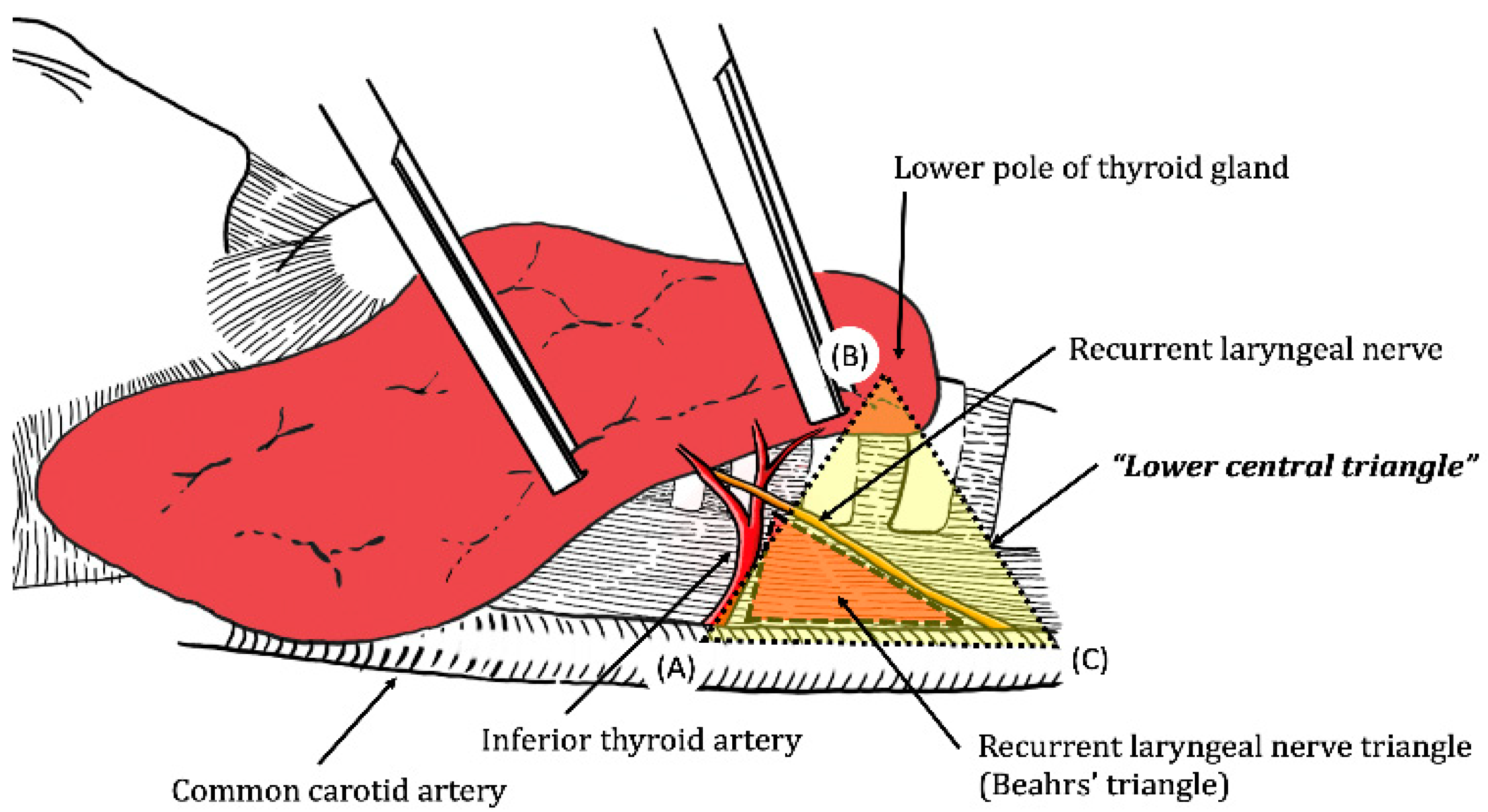
2.3. Anatomical Definition of the Lower Central Triangle (LCT)
2.4. Statistics
3. Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hayward, N.J.; Grodski, S.; Yeung, M.; Johnson, W.R.; Serpell, J. Recurrent laryngeal nerve injury in thyroid surgery: A review. ANZ J. Surg. 2013, 83, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Jeannon, J.P.; Orabi, A.A.; Bruch, G.A.; Abdalsalam, H.A.; Simo, R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: A systematic review. Int. J. Clin. Pract. 2009, 63, 624–629. [Google Scholar] [CrossRef]
- Stojadinovic, A.; Shaha, A.R.; Orlikoff, R.F.; Nissan, A.; Komak, M.; Singh, B.; Boyle, J.O.; Shah, J.P.; Brennan, M.F.; Kraus, D.H. Prospective functional voice assessment in patients undergoing thyroid surgery. Ann. Surg. 2002, 236, 823–832. [Google Scholar] [CrossRef]
- Lo, C.Y.; Kwok, K.F.; Yuen, P.W. A prospective evaluation of recurrent laryngeal nerve paralysis during thyroidectomy. Arch. Surg. 2000, 135, 204–207. [Google Scholar] [CrossRef]
- Beldi, G.; Kinsbergen, T.; Schlumpf, R. Evaluation of intraoperative recurrent nerve monitoring in thyroid surgery. World J. Surg. 2004, 28, 589–591. [Google Scholar] [CrossRef] [PubMed]
- Chiang, F.Y.; Wang, L.F.; Huang, Y.F.; Lee, K.W.; Kuo, W.R. Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery 2005, 137, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Randolph, G.W.; Dralle, H. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: International standards guideline statement. Laryngoscope 2011, 121, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.E.; Seiler, C. Recurrent laryngeal nerve palsy after thyroid gland surgery. Br. J. Surg. 1994, 81, 226–228. [Google Scholar] [CrossRef] [PubMed]
- Barczyński, M.; Konturek, A.; Pragacz, K.; Papier, A.; Stopa, M.; Nowak, W. Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: Results of a retrospective cohort study. World J. Surg. 2014, 38, 599–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barczyński, M.; Konturek, A.; Cichoń, S. Randomized clinical trial of visualization wersus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br. J. Surg. 2009, 96, 240–246. [Google Scholar] [CrossRef]
- Brennan, J.; Moore, E.J.; Shuler, K.J. Prospective analysis of the efficacy of continuous intraoperative nerve monitoring during thyroidectomy parathyroidectomy and parotidectomy. Otolaryngol. Head Neck Surg. 2001, 124, 537–543. [Google Scholar] [CrossRef]
- Chan, W.F.; Lang, B.H.H.; Lo, C.Y. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: A comparative study on 1000 nerves at risk. Surgery 2006, 140, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Dralle, H.; Sekulla, C.; Haerting, J.; Timmermann, W.; Neumann, H.J.; Kruse, E.; Grond, S.; Mühlig, H.P.; Richter, C.; Voss, J.; et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 2004, 136, 1310–1322. [Google Scholar] [CrossRef]
- Barczyński, M.; Randolph, G.W.; Cernea, C. International survey on the identification and neural monitoring of the EBSLN during thyroidectomy. Laryngoscope 2016, 126, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Horne, S.K.; Gal, T.J.; Brennan, J.A. Prevalence and patterns of intraoperative nerve monitoring for thyroidectomy. Otolaryngol. Head Neck Surg. 2007, 136, 952–956. [Google Scholar] [CrossRef] [PubMed]
- Dralle, H.; Sekulla, C.; Lorenz, K.; Brauckhoff, M.; Machens, A. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J. Surg. 2008, 32, 1358–1366. [Google Scholar] [CrossRef] [PubMed]
- Sturniolo, G.; D’Alia, C.; Tonante, A.; Gagliano, E.; Taranto, F.; Lo Schiavo, M.G. The recurrent laryngeal nerve related to thyroid surgery. Am. J. Surg. 1999, 177, 485–488. [Google Scholar] [CrossRef]
- Snyder, S.K.; Lairmore, T.C.; Hendricks, J.C.; Roberts, J.W. Elucidating Mechanisms of Recurrent Laryngeal Nerve Injury During Thyroidectomy and Parathyroidectomy. J. Am. Coll. Surg. 2008, 206, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Miyauchi, A.; Masuoka, H.; Yabuta, T.; Fukushima, M.; Kihara, M.; Higashiyama, T.; Takamura, Y.; Ito, Y.; Kobayashi, K.; Miya, A. The ima approach for the quick identification of the right recurrent laryngeal nerve in thyroid cancer surgery. Surg. Today 2013, 43, 225–228. [Google Scholar] [CrossRef]
- Page, C.; Peltier, J.; Charlet, L.; Laude, M.; Strunski, V. Superior approach to the inferior laryngeal nerve in thyroid surgery: Anatomy, surgical technique and indications. Surg. Radiol. Anat. 2006, 28, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Sebag, F.; Palazzo, F.F.; Harding, J.; Sierra, M.; Ippolito, G.; Henry, J.F. Endoscopic lateral approach thyroid lobectomy: Safe evolution from endoscopic parathyroidectomy. World J. Surg. 2006, 30, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Poveda, M.C.D.; Dionigi, G.; Sitges-Serra, A.; Barczynski, M.; Angelos, P.; Dralle, H.; Phelan, E.; Randolph, G. Intraoperative monitoring of the recurrent laryngeal nerve during thyroidectomy: A standardized approach (Part 1). World J. Endocr. Surg. 2011, 3, 144–150. [Google Scholar] [CrossRef]
- Delbridge, L.; Reeve, T.S.; Khadra, M.; Poole, A.G. Total Thyroidectomy: The Technique of Capsular Dissection. Aust. N. Z. J. Surg. 1992, 62, 96–99. [Google Scholar] [CrossRef]
- Lee, K.E.; Rao, J.; Youn, Y.K. Endoscopic thyroidectomy with the da vinci robot system using the bilateral axillary breast approach (BABA) technique: Our initial experience. Surg. Laparosc. Endosc. Percutaneous Tech. 2009, 19, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Yun, J.H.; Nam, K.H.; Choi, U.J.; Chung, W.Y.; Soh, E. Perioperative clinical outcomes after robotic thyroidectomy for thyroid carcinoma: A multicenter study. Surg. Endosc. 2011, 25, 906–912. [Google Scholar] [CrossRef]
- Kang, S.W.; Jeong, J.J.; Nam, K.H.; Chang, H.S.; Chung, W.Y.; Park, C.S. Robot-Assisted Endoscopic Thyroidectomy for Thyroid Malignancies Using a Gasless Transaxillary Approach. J. Am. Coll. Surg. 2009, 209, e1–e7. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Non-IONM * (n = 18, 45%) | IONM * (n = 22, 55%) | p Value |
|---|---|---|---|
| Age (year) | 51.78 ± 13.42 | 51.73 ± 12.37 | 0.990 |
| Gender, Male | 4 (22.2%) | 5 (22.7%) | <0.001 |
| Cancer | 17 (94.4%) | 19 (86.4%) | 0.421 |
| Nodule size (cm) | 1.21 ± 0.98 | 2.22 ± 1.56 | 0.037 |
| Thyroiditis on pathology | 7 (38.9%) | 10 (45.5%) | 0.676 |
| Mapping/Detection (s) | Identification (s) | p | |
|---|---|---|---|
| IONM | 3.3936 ± 1.55 | 14.8932 ± 7.33 | <0.001 |
| non-IONM | 13.8189 ± 8.60 | 25.5589 ± 14.12 | 0.009 |
| Right Lobes (n = 20) | non-IONM * | IONM * | Total |
| 1 | 3 (37.5%) | 8 (72.7%) | 11 (55.0%) |
| 2 | 3 (37.5%) | 3 (27.3%) | 6 (30.0%) |
| 3 | 2 (25.0%) | 0 (0.0%) | 2 (10.0%) |
| 4 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Left Lobes (n = 20) | non-IONM * | IONM * | Total |
| 1 | 9 (90.0%) | 9 (81.8%) | 18 (85.7%) |
| 2 | 0 (0.0%) | 2 (18.2%) | 2 (9.5%) |
| 3 | 1 (10.0%) | 0 (0.0%) | 1 (4.8%) |
| 4 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.; Lee, K.; Yu, H.W.; Kim, S.-j.; Chai, Y.J.; Choi, J.Y.; Lee, K.E. Comparison of Recurrent Laryngeal Nerve Identification Time in the Lower Central Triangle during Thyroid Surgery Using Neurophysiological Mapping and Monitoring. Medicina 2021, 57, 748. https://doi.org/10.3390/medicina57080748
Lee E, Lee K, Yu HW, Kim S-j, Chai YJ, Choi JY, Lee KE. Comparison of Recurrent Laryngeal Nerve Identification Time in the Lower Central Triangle during Thyroid Surgery Using Neurophysiological Mapping and Monitoring. Medicina. 2021; 57(8):748. https://doi.org/10.3390/medicina57080748
Chicago/Turabian StyleLee, Eunhye, Keunchul Lee, Hyeong Won Yu, Su-jin Kim, Young Jun Chai, June Young Choi, and Kyu Eun Lee. 2021. "Comparison of Recurrent Laryngeal Nerve Identification Time in the Lower Central Triangle during Thyroid Surgery Using Neurophysiological Mapping and Monitoring" Medicina 57, no. 8: 748. https://doi.org/10.3390/medicina57080748






