Molecular Targets of Cannabidiol in Experimental Models of Neurological Disease
Abstract
:1. Introduction
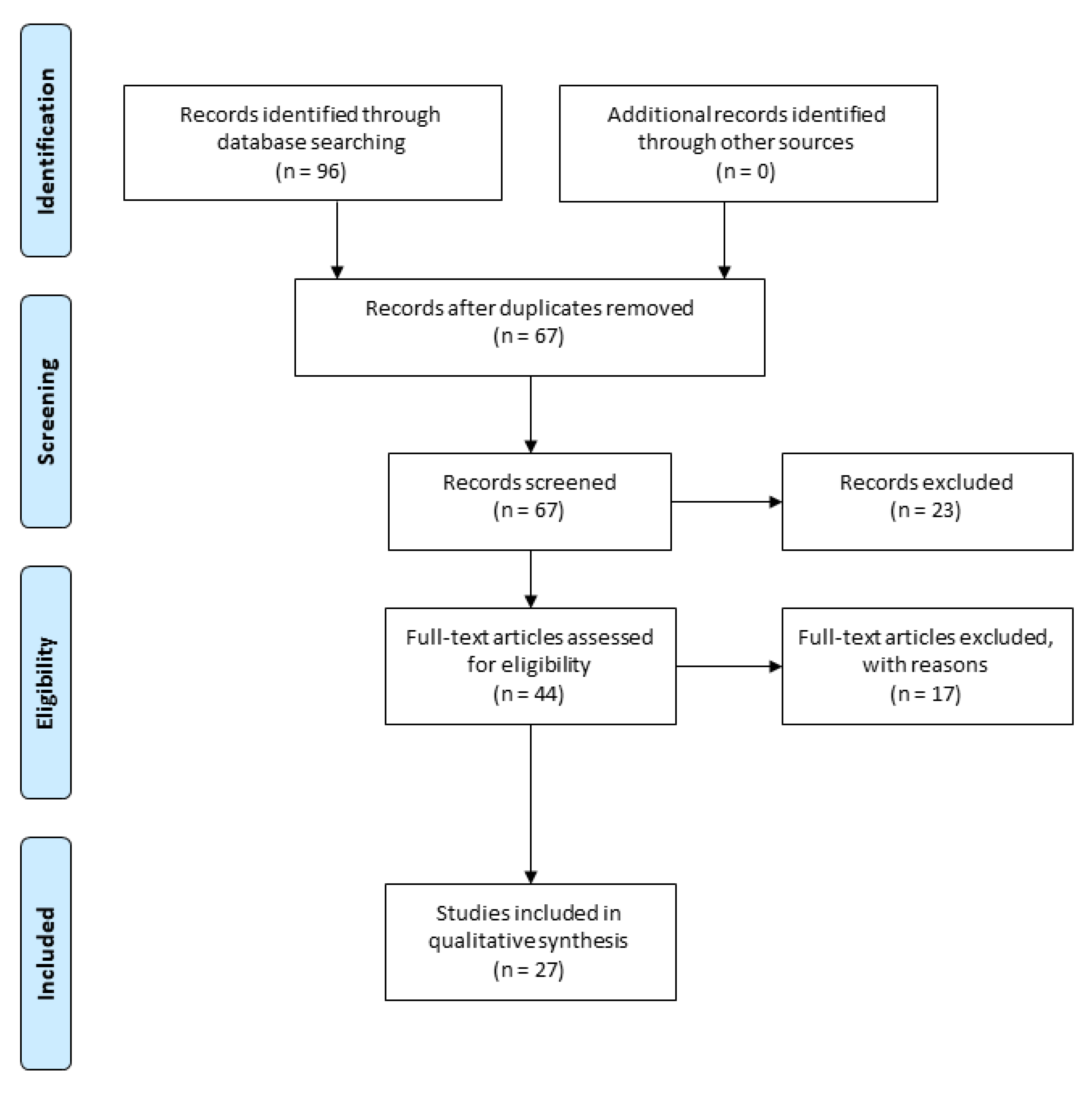
2. Methodology
3. Chemical Properties of Cannabidiol
4. Cannabidiol Mechanism of Action
5. Pharmacokinetic Properties of Cannabidiol
6. Molecular Targets of CBD for Application in Neurodegenerative Diseases
6.1. GPCRs
6.1.1. Adenosine Receptors
6.1.2. 5-HT Receptors
6.1.3. GPR55
6.2. TRP
6.3. PPARγ Receptors
6.4. GABA Receptors
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CBD | cannabidiol |
| Δ9-THC | Δ9-tetrahydro-cannabinol |
| Nrf2 | nuclear factor erythroid 2 – related factor 2 |
| SOD | superoxide dismutase |
| GSH | glutathione |
| ROS | reactive oxygen species |
| iNOS | inducible nitric oxide synthase |
| IL-6 | interleukin-6 |
| IL-1β | interleukin-1β |
| TNF-α | tumor necrosis factor α |
| NF-κB | nuclear factor κB |
| PPARγ | peroxisome proliferator-activated receptor γ |
| TRP | transient receptor potential |
| TRPV | transient receptor potential vanilloid |
| CB1 | cannabinoid receptor type 1 |
| CB2 | cannabinoid receptor type 2 |
| 2-AG | 2-arachidonoyl glycerol |
| AEA | arachidonoylethanolamide |
| ECS | endocannabinoid system |
| Ca2+ | calcium |
| FAAH | fatty acid amide hydrolase |
| GABA | γ-aminobutyric acid |
| 5-HT | Serotonin |
| GPCRs | G protein-coupled receptors |
| ARs | adenosine receptors |
| BBB | blood–brain barrier |
| CYPs | cytochrome P450 enzymes |
| 7-OH-CBD | 7-hydroxycannabidiol |
| Gi/o | inhibiting G |
| cAMP | cyclic adenosine monophosphate |
| PI3K/Akt | phosphoinositide 3-kinases/protein kinase B |
| CNS | central nervous system |
| TMEV | Theiler’s murine encephalomyelitis virus |
| i.p. | intraperitoneal |
| VCAM-1 | vascular cell adhesion molecule-1 |
| CCL2 | chemokine 2 |
| CCL5 | chemokine 5 |
| COX-2 | cyclooxygenase-2 |
| Aβ | amyloid-β |
| BDNF | brain-derived neurotrophic factor |
| K+ | potassium |
| MCA | middle cerebral artery occlusion |
| PTZ | pentylenetetrazole |
| i.v. | intravenous |
| GPR55 | G protein-coupled receptors 55 |
| ERK | extracellular receptor-activated kinases |
| DS | Dravet syndrome |
| MPTP | 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine |
| EAE | experimental autoimmune encephalomyelitis |
| TRPA1 | transient receptor potential ankyrin 1 |
| TRPM8 | transient receptor potential cation channel subfamily M member 8 |
| hPBMECs | human Primary Brain Microvascular Endothelial Cells |
| GSK-3β | glycogen synthase kinase 3β |
| SH-SY5YAPP+ | SH-SY5Y cells transfected with the amyloid precursor protein |
| l-DOPA | l-3,4-Dihydroxyphenylalanine |
| 6-OHDA | 6-hydroxydopamine |
| AA-5-HT | arachidonoyl-serotonin |
| IFN-γ | interferon-γ |
| IL-17 | interleukin-17 |
| TSC | tuberous sclerosis complex |
| CLB | clobazam |
| N-CLB | N-desmethylclobazam |
| Scn1a+/− | heterozygous loss of function SCN1A |
References
- WHO. WHO Methods and Data Sources for Global Burden of Disease Estimates 2000–2011; Department of Health Statistics and Information Systems: Geneva, Switzerland, 2013; Available online: http://www.who.int/healthinfo/statistics/GlobalDALYmethods_2000_2011.pdf?ua=1 (accessed on 6 November 2020).
- Roy, M.; Tapadia, M.G.; Joshi, S.; Koch, B. Molecular and genetic basis of depression. J. Genet. 2014, 93, 879–892. [Google Scholar] [CrossRef] [PubMed]
- Lopizzo, N.; Bocchio Chiavetto, L.; Cattane, N.; Plazzotta, G.; Tarazi, F.I.; Pariante, C.M.; Riva, M.A.; Cattaneo, A. Gene–environment interaction in major depression: Focus on experience-dependent biological systems. Front. Psychiatry 2015, 6, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nowicka, N.; Juranek, J.; Juranek, J.K.; Wojtkiewicz, J. Risk factors and emerging therapies in amyotrophic lateral sclerosis. Int. J. Mol. Sci. 2019, 20, 2616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ascherio, A.; Munger, K. Epidemiology of multiple sclerosis: From risk factors to prevention, Semin. Neurol. 2016, 36, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ruiz, J.; Sagredo, O.; Pazos, M.R.; García, C.; Pertwee, R.; Mechoulam, R.; Martínez-Orgado, J. Cannabidiol for neurodegenerative disorders: Important new clinical applications for this phytocannabinoid? Br. J. Clin. Pharm. 2013, 75, 323–333. [Google Scholar] [CrossRef]
- Campos, A.C.; Moreira, F.A.; Gomes, F.V.; Del Bel, E.A.; Guimaraes, F.S. Multiple mechanisms involved in the large-spectrum therapeutic potential of cannabidiol in psychiatric disorders. Philos. Trans. R. Soc. B Biol. Sci. 2012, 367, 3364–3378. [Google Scholar] [CrossRef]
- Mechoulam, R.; Gaoni, Y. Hashish—IV: The isolation and structure of cannabinolic cannabidiolic and cannabigerolic acids. Tetrahedron 1965, 21, 1223–1229. [Google Scholar] [CrossRef]
- Pertwee, R.G. Pharmacological actions of cannabinoids. In Cannabinoids; Springer: Heidelberg, Germany, 2005; pp. 1–51. [Google Scholar]
- Fiani, B.; Sarhadi, K.J.; Soula, M.; Zafar, A.; Quadri, S.A. Current application of cannabidiol (CBD) in the management and treatment of neurological disorders. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2020, 41, 3085–3098. [Google Scholar] [CrossRef] [PubMed]
- Zuardi, A.W.; Cosme, R.; Graeff, F.; Guimarães, F. Effects of ipsapirone and cannabidiol on human experimental anxiety. J. Psychopharmacol. 1993, 7, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Campos, A.; Brant, F.; Miranda, A.; Machado, F.; Teixeira, A. Cannabidiol increases survival and promotes rescue of cognitive function in a murine model of cerebral malaria. Neuroscience 2015, 289, 166–180. [Google Scholar] [CrossRef]
- Silveira, J.W.; Issy, A.C.; Castania, V.A.; Salmon, C.E.; Nogueira-Barbosa, M.H.; Guimarães, F.S.; Defino, H.L.; Del Bel, E. Protective effects of cannabidiol on lesion-induced intervertebral disc degeneration. PLoS ONE 2014, 9, e113161. [Google Scholar] [CrossRef] [PubMed]
- Schiavon, A.P.; Soares, L.M.; Bonato, J.M.; Milani, H.; Guimaraes, F.S.; de Oliveira, R.M.W. Protective effects of cannabidiol against hippocampal cell death and cognitive impairment induced by bilateral common carotid artery occlusion in mice. Neurotox. Res. 2014, 26, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Kwiatkoski, M.; Guimaraes, F.S.; Del-Bel, E. Cannabidiol-treated rats exhibited higher motor score after cryogenic spinal cord injury. Neurotox. Res. 2012, 21, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Linge, R.; Jiménez-Sánchez, L.; Campa, L.; Pilar-Cuéllar, F.; Vidal, R.; Pazos, A.; Adell, A.; Díaz, Á. Cannabidiol induces rapid-acting antidepressant-like effects and enhances cortical 5-HT/glutamate neurotransmission: Role of 5-HT1A receptors. Neuropharmacology 2016, 103, 16–26. [Google Scholar] [CrossRef] [Green Version]
- Esposito, G.; Scuderi, C.; Valenza, M.; Togna, G.I.; Latina, V.; De Filippis, D.; Cipriano, M.; Carratù, M.R.; Iuvone, T.; Steardo, L. Cannabidiol reduces Aβ-induced neuroinflammation and promotes hippocampal neurogenesis through PPARγ involvement. PLoS ONE 2011, 6, e28668. [Google Scholar] [CrossRef] [PubMed]
- Mecha, M.; Feliú, A.; Iñigo, P.; Mestre, L.; Carrillo-Salinas, F.; Guaza, C. Cannabidiol provides long-lasting protection against the deleterious effects of inflammation in a viral model of multiple sclerosis: A role for A2A receptors. Neurobiol. Dis. 2013, 59, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Napimoga, M.H.; Benatti, B.B.; Lima, F.O.; Alves, P.M.; Campos, A.C.; Pena-dos-Santos, D.R.; Severino, F.P.; Cunha, F.Q.; Guimarães, F.S. Cannabidiol decreases bone resorption by inhibiting RANK/RANKL expression and pro-inflammatory cytokines during experimental periodontitis in rats. Int. Immunopharmacol. 2009, 9, 216–222. [Google Scholar] [CrossRef]
- Malfait, A.; Gallily, R.; Sumariwalla, P.; Malik, A.; Andreakos, E.; Mechoulam, R.; Feldmann, M. The nonpsychoactive cannabis constituent cannabidiol is an oral anti-arthritic therapeutic in murine collagen-induced arthritis. Proc. Natl. Acad. Sci. USA 2000, 97, 9561–9566. [Google Scholar] [CrossRef] [Green Version]
- Kozela, E.; Pietr, M.; Juknat, A.; Rimmerman, N.; Levy, R.; Vogel, Z. Cannabinoids Δ9-tetrahydrocannabinol and cannabidiol differentially inhibit the lipopolysaccharide-activated NF-κB and interferon-β/STAT proinflammatory pathways in BV-2 microglial cells. J. Biol. Chem. 2010, 285, 1616–1626. [Google Scholar] [CrossRef] [Green Version]
- Mannucci, C.; Navarra, M.; Calapai, F.; Spagnolo, E.V.; Busardo, F.P.; Cas, R.D.; Ippolito, F.M.; Calapai, G. Neurological Aspects of Medical Use of Cannabidiol. Cns. Neurol. Disord. Drug Targets 2017, 16, 541–553. [Google Scholar] [CrossRef] [Green Version]
- Peres, F.F.; Lima, A.C.; Hallak, J.E.C.; Crippa, J.A.; Silva, R.H.; Abilio, V.C. Cannabidiol as a Promising Strategy to Treat and Prevent Movement Disorders? Front Pharm. 2018, 9, 482. [Google Scholar] [CrossRef] [Green Version]
- Atalay, S.; Jarocka-Karpowicz, I.; Skrzydlewska, E. Antioxidative and Anti-Inflammatory Properties of Cannabidiol. Antioxidants 2019, 9, 21. [Google Scholar] [CrossRef] [Green Version]
- Costa, B.; Trovato, A.E.; Comelli, F.; Giagnoni, G.; Colleoni, M. The non-psychoactive cannabis constituent cannabidiol is an orally effective therapeutic agent in rat chronic inflammatory and neuropathic pain. Eur. J. Pharm. 2007, 556, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.; Mukhopadhyay, P.; Rajesh, M.; Patel, V.; Mukhopadhyay, B.; Gao, B.; Hasko, G.; Pacher, P. Cannabidiol Attenuates Cisplatin-Induced Nephrotoxicity by Decreasing Oxidative/Nitrosative Stress, Inflammation, and Cell Death. J. Pharm. Exp. 2009, 328, 708–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esposito, G.; De Filippis, D.; Maiuri, M.C.; De Stefano, D.; Carnuccio, R.; Iuvone, T. Cannabidiol inhibits inducible nitric oxide synthase protein expression and nitric oxide production in β-amyloid stimulated PC12 neurons through p38 MAP kinase and NF-κB involvement. Neurosci. Lett. 2006, 399, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Castillo, A.; Tolon, M.R.; Fernandez-Ruiz, J.; Romero, J.; Martinez-Orgado, J. The neuroprotective effect of cannabidiol in an in vitro model of newborn hypoxic-ischemic brain damage in mice is mediated by CB2 and adenosine receptors. Neurobiol. Dis. 2010, 37, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Jean-Gilles, L.; Gran, B.; Constantinescu, C.S. Interaction between cytokines, cannabinoids and the nervous system. Immunobiology 2010, 215, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Jastrzab, A.; Gegotek, A.; Skrzydlewska, E. Cannabidiol Regulates the Expression of Keratinocyte Proteins Involved in the Inflammation Process through Transcriptional Regulation. Cells-Basel 2019, 8, 827. [Google Scholar] [CrossRef] [Green Version]
- Costa, B.; Giagnoni, G.; Franke, C.; Trovato, A.E.; Colleoni, M. Vanilloid TRPV1 receptor mediates the antihyperalgesic effect of the nonpsychoactive cannabinoid, cannabidiol, in a rat model of acute inflammation. Br. J. Pharm. 2004, 143, 247–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajan, T.S.; Giacoppo, S.; Iori, R.; De Nicola, G.R.; Grassi, G.; Pollastro, F.; Bramanti, P.; Mazzon, E. Anti-inflammatory and antioxidant effects of a combination of cannabidiol and moringin in LPS-stimulated macrophages. Fitoterapia 2016, 112, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Santos, N.A.G.; Martins, N.M.; Sisti, F.M.; Fernandes, L.S.; Ferreira, R.S.; Queiroz, R.H.C.; Santos, A.C. The neuroprotection of cannabidiol against MPP+-induced toxicity in PC12 cells involves trkA receptors, upregulation of axonal and synaptic proteins, neuritogenesis, and might be relevant to Parkinson’s disease. Toxicol. In Vitro 2015, 30, 231–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chagas, M.H.N.; Zuardi, A.W.; Tumas, V.; Pena-Pereira, M.A.; Sobreira, E.T.; Bergamaschi, M.M.; dos Santos, A.C.; Teixeira, A.L.; Hallak, J.E.; Crippa, J.A.S. Effects of cannabidiol in the treatment of patients with Parkinson’s disease: An exploratory double-blind trial. J. Psychopharmacol. 2014, 28, 1088–1098. [Google Scholar] [CrossRef] [PubMed]
- Vallée, A.; Lecarpentier, Y.; Guillevin, R.; Vallée, J.-N. Effects of cannabidiol interactions with Wnt/β-catenin pathway and PPARγ on oxidative stress and neuroinflammation in Alzheimer’s disease. Acta Biochim. Et Biophys. Sin. 2017, 49, 853–866. [Google Scholar] [CrossRef] [Green Version]
- Watt, G.; Karl, T. In vivo evidence for therapeutic properties of cannabidiol (CBD) for Alzheimer’s disease. Front Pharm. 2017, 8, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Libro, R.; Diomede, F.; Scionti, D.; Piattelli, A.; Grassi, G.; Pollastro, F.; Bramanti, P.; Mazzon, E.; Trubiani, O. Cannabidiol Modulates the Expression of Alzheimer’s Disease-Related Genes in Mesenchymal Stem Cells. Int. J. Mol. Sci. 2017, 18, 26. [Google Scholar] [CrossRef] [Green Version]
- Hussain, S.A.; Zhou, R.; Jacobson, C.; Weng, J.; Cheng, E.; Lay, J.; Hung, P.; Lerner, J.T.; Sankar, R. Perceived efficacy of cannabidiol-enriched cannabis extracts for treatment of pediatric epilepsy: A potential role for infantile spasms and Lennox–Gastaut syndrome. Epilepsy Behav. 2015, 47, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Devinsky, O.; Cilio, M.R.; Cross, H.; Fernandez-Ruiz, J.; French, J.; Hill, C.; Katz, R.; Di Marzo, V.; Jutras-Aswad, D.; Notcutt, W.G. Cannabidiol: Pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia 2014, 55, 791–802. [Google Scholar] [CrossRef] [Green Version]
- Bergamaschi, M.M.; Queiroz, R.H.C.; Chagas, M.H.N.; De Oliveira, D.C.G.; De Martinis, B.S.; Kapczinski, F.; Quevedo, J.; Roesler, R.; Schröder, N.; Nardi, A.E. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology 2011, 36, 1219–1226. [Google Scholar] [CrossRef]
- Zhornitsky, S.; Potvin, S. Cannabidiol in humans-the quest for therapeutic targets. Pharmaceuticals 2012, 5, 529–552. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Adams, R. Marihuana: Harvey lecture, February 19, 1942. Bull. New York Acad. Med. 1942, 18, 705. [Google Scholar]
- Todd, A. The chemistry of hashish. Sci. J. R. Coll. Sci. 1942, 12, 37. [Google Scholar]
- Jones, P.G.; Falvello, L.; Kennard, O.; Sheldrick, G.; Mechoulam, R. Cannabidiol. Acta Cryst. Sect. B Struct. Cryst. Cryst. Chem. 1977, 33, 3211–3214. [Google Scholar] [CrossRef] [Green Version]
- Morales, P.; Reggio, P.H.; Jagerovic, N. An Overview on Medicinal Chemistry of Synthetic and Natural Derivatives of Cannabidiol. Front Pharm. 2017, 8, 422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elmes, M.W.; Kaczocha, M.; Berger, W.T.; Leung, K.; Ralph, B.P.; Wang, L.Q.; Sweeney, J.M.; Miyauchi, J.T.; Tsirka, S.E.; Ojima, I.; et al. Fatty Acid-binding Proteins (FABPs) Are Intracellular Carriers for Delta (9)-Tetrahydrocannabinol (THC) and Cannabidiol (CBD). J. Biol. Chem. 2015, 290, 8711–8721. [Google Scholar] [CrossRef] [Green Version]
- Borges, R.S.; Batista, J.; Viana, R.B.; Baetas, A.C.; Orestes, E.; Andrade, M.A.; Honorio, K.M.; da Silva, A.B.F. Understanding the Molecular Aspects of Tetrahydrocannabinol and Cannabidiol as Antioxidants. Molecules 2013, 18, 12663–12674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laprairie, R.B.; Bagher, A.M.; Kelly, M.E.M.; Denovan-Wright, E.M. Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br. J. Pharm. 2015, 172, 4790–4805. [Google Scholar] [CrossRef] [Green Version]
- Morales, P.; Goya, P.; Jagerovic, N.; Hernandez-Folgado, L. Allosteric modulators of the CB1 cannabinoid receptor: A structural update review. Cannabis Cannabinoid Res. 2016, 1, 22–30. [Google Scholar] [CrossRef] [Green Version]
- Leweke, F.; Piomelli, D.; Pahlisch, F.; Muhl, D.; Gerth, C.; Hoyer, C.; Klosterkötter, J.; Hellmich, M.; Koethe, D. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl. Psychiatry 2012, 2, e94. [Google Scholar] [CrossRef] [Green Version]
- Campos, A.C.; Fogaca, M.V.; Sonego, A.B.; Guimaraes, F.S. Cannabidiol, neuroprotection and neuropsychiatric disorders. Pharm. Res. 2016, 112, 119–127. [Google Scholar] [CrossRef]
- Ibeas Bih, C.; Chen, T.; Nunn, A.V.; Bazelot, M.; Dallas, M.; Whalley, B.J. Molecular Targets of Cannabidiol in Neurological Disorders. Neurotherapeutics 2015, 12, 699–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassano, T.; Villani, R.; Pace, L.; Carbone, A.; Bukke, V.N.; Orkisz, S.; Avolio, C.; Serviddio, G. From Cannabis sativa to Cannabidiol: Promising Therapeutic Candidate for the Treatment of Neurodegenerative Diseases. Front Pharm. 2020, 11, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kano, M.; Ohno-Shosaku, T.; Maejima, T. Retrograde signaling at central synapses via endogenous cannabinoids. Mol. Psychiatr. 2002, 7, 234–235. [Google Scholar] [CrossRef] [PubMed]
- Freund, T.F.; Katona, I.; Piomelli, D. Role of endogenous cannabinoids in synaptic signaling. Physiol. Rev. 2003, 83, 1017–1066. [Google Scholar] [CrossRef]
- Pertwee, R.G.; Ross, R.A. Cannabinoid receptors and their ligands. Prostaglandins Leukot. Essent. Fat. Acids 2002, 66, 101–121. [Google Scholar] [CrossRef] [PubMed]
- Szabo, B.; Schlicker, E. Effects of cannabinoids on neurotransmission. Handb. Exp. Pharm. 2005, 327–365. [Google Scholar]
- Russo, E.B.; Burnett, A.; Hall, B.; Parker, K.K. Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem. Res. 2005, 30, 1037–1043. [Google Scholar] [CrossRef]
- Yang, K.-H.; Galadari, S.; Isaev, D.; Petroianu, G.; Shippenberg, T.S.; Oz, M. The nonpsychoactive cannabinoid cannabidiol inhibits 5-hydroxytryptamine3A receptor-mediated currents in Xenopus laevis oocytes. J. Pharm. Exp. 2010, 333, 547–554. [Google Scholar] [CrossRef] [Green Version]
- Rock, E.; Bolognini, D.; Limebeer, C.; Cascio, M.; Anavi-Goffer, S.; Fletcher, P.; Mechoulam, R.; Pertwee, R.G.; Parker, L.A. Cannabidiol, a non-psychotropic component of cannabis, attenuates vomiting and nausea-like behaviour via indirect agonism of 5-HT1A somatodendritic autoreceptors in the dorsal raphe nucleus. Br. J. Pharm. 2012, 165, 2620–2634. [Google Scholar] [CrossRef] [Green Version]
- Gonca, E.; Darıcı, F. The effect of cannabidiol on ischemia/reperfusion-induced ventricular arrhythmias: The role of adenosine A1 receptors. J. Cardiovasc. Pharm. 2015, 20, 76–83. [Google Scholar] [CrossRef]
- Izzo, A.A.; Borrelli, F.; Capasso, R.; Di Marzo, V.; Mechoulam, R. Non-psychotropic plant cannabinoids: New therapeutic opportunities from an ancient herb. Trends Pharm. Sci. 2009, 30, 515–527. [Google Scholar] [CrossRef] [PubMed]
- Scuderi, C.; Steardo, L.; Esposito, G. Cannabidiol promotes amyloid precursor protein ubiquitination and reduction of β amyloid expression in SHSY5YAPP+ cells through PPARγ involvement. Phytother. Res. 2014, 28, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Bakas, T.; van Nieuwenhuijzen, P.S.; Devenish, S.O.; McGregor, I.S.; Arnold, J.C.; Chebib, M. The direct actions of cannabidiol and 2-arachidonoyl glycerol at GABAA receptors. Pharm. Res. 2017, 119, 358–370. [Google Scholar] [CrossRef] [PubMed]
- Newmeyer, M.N.; Swortwood, M.J.; Barnes, A.J.; Abulseoud, O.A.; Scheidweiler, K.B.; Huestis, M.A. Free and Glucuronide Whole Blood Cannabinoids’ Pharmacokinetics after Controlled Smoked, Vaporized, and Oral Cannabis Administration in Frequent and Occasional Cannabis Users: Identification of Recent Cannabis Intake. Clin. Chem. 2016, 62, 1579–1592. [Google Scholar] [CrossRef] [Green Version]
- Mechoulam, R.; Parker, L.A.; Gallily, R. Cannabidiol: An overview of some pharmacological aspects. J. Clin. Pharm. 2002, 42, 11s–19s. [Google Scholar] [CrossRef]
- Grotenhermen, F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin. Pharm. 2003, 42, 327–360. [Google Scholar] [CrossRef] [PubMed]
- Fasinu, P.S.; Phillips, S.; ElSohly, M.A.; Walker, L.A. Current Status and Prospects for Cannabidiol Preparations as New Therapeutic Agents. Pharmacotherapy 2016, 36, 781–796. [Google Scholar] [CrossRef] [PubMed]
- Huestis, M.A. Pharmacokinetics and metabolism of the plant cannabinoids, delta9-tetrahydrocannabinol, cannabidiol and cannabinol. Handb. Exp. Pharm. 2005, 657–690. [Google Scholar] [CrossRef]
- Gaston, T.E.; Friedman, D. Pharmacology of cannabinoids in the treatment of epilepsy. Epilepsy Behav. 2017, 70, 313–318. [Google Scholar] [CrossRef]
- Bergamaschi, M.M.; Queiroz, R.H.; Zuardi, A.W.; Crippa, J.A. Safety and side effects of cannabidiol, a Cannabis sativa constituent. Curr. Drug Saf. 2011, 6, 237–249. [Google Scholar] [CrossRef]
- Zendulka, O.; Dovrtelova, G.; Noskova, K.; Turjap, M.; Sulcova, A.; Hanus, L.; Jurica, J. Cannabinoids and Cytochrome P450 Interactions. Curr. Drug Metab. 2016, 17, 206–226. [Google Scholar] [CrossRef]
- Jiang, R.R.; Yamaori, S.; Okamoto, Y.; Yamamoto, I.; Watanabe, K. Cannabidiol Is a Potent Inhibitor of the Catalytic Activity of Cytochrome P450 2C19. Drug Metab. Pharm. 2013, 28, 332–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Premoli, M.; Aria, F.; Bonini, S.A.; Maccarinelli, G.; Gianoncelli, A.; Pina, S.D.; Tambaro, S.; Memo, M.; Mastinu, A. Cannabidiol: Recent advances and new insights for neuropsychiatric disorders treatment. Life Sci. 2019, 224, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Dal Ben, D.; Lambertucci, C.; Buccioni, M.; Marti Navia, A.; Marucci, G.; Spinaci, A.; Volpini, R. Non-Nucleoside Agonists of the Adenosine Receptors: An Overview. Pharmaceuticals 2019, 12, 150. [Google Scholar] [CrossRef] [Green Version]
- Kamp, T.J.; Hell, J.W. Regulation of cardiac l-type calcium channels by protein kinase A and protein kinase C. Circ. Res. 2000, 87, 1095–1102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borea, P.A.; Gessi, S.; Merighi, S.; Vincenzi, F.; Varani, K. Pharmacology of Adenosine Receptors: The State of the Art. Physiol. Rev. 2018, 98, 1591–1625. [Google Scholar] [CrossRef]
- Jacobson, K.A.; Gao, Z.G. Adenosine receptors as therapeutic targets. Nat. Rev. Drug Discov. 2006, 5, 247–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.F.; Eltzschig, H.K.; Fredholm, B.B. Adenosine receptors as drug targets-what are the challenges? Nat. Rev. Drug Discov. 2013, 12, 265–286. [Google Scholar] [CrossRef] [Green Version]
- Carrier, E.J.; Auchampach, J.A.; Hillard, C.J. Inhibition of an equilibrative nucleoside transporter by cannabidiol: A mechanism of cannabinoid immunosuppression. Proc. Natl. Acad. Sci. USA 2006, 103, 7895–7900. [Google Scholar] [CrossRef] [Green Version]
- Magen, I.; Avraham, Y.; Ackerman, Z.; Vorobiev, L.; Mechoulam, R.; Berry, E.M. Cannabidiol ameliorates cognitive and motor impairments in mice with bile duct ligation. J. Hepatol. 2009, 51, 528–534. [Google Scholar] [CrossRef] [PubMed]
- Magen, I.; Avraham, Y.; Ackerman, Z.; Vorobiev, L.; Mechoulam, R.; Berry, E.M. Cannabidiol ameliorates cognitive and motor impairments in bile-duct ligated mice via 5-HT1A receptor activation. Br. J. Pharm. 2010, 159, 950–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin-Moreno, A.M.; Reigada, D.; Ramirez, B.G.; Mechoulam, R.; Innamorato, N.; Cuadrado, A.; de Ceballos, M.L. Cannabidiol and other cannabinoids reduce microglial activation in vitro and in vivo: Relevance to Alzheimer’s disease. Mol. Pharm. 2011, 79, 964–973. [Google Scholar] [CrossRef] [Green Version]
- Raymond, J.R.; Mukhin, Y.V.; Gettys, T.W.; Garnovskaya, M.N. The recombinant 5-HT1A receptor: G protein coupling and signalling pathways. Br. J. Pharm. 1999, 127, 1751–1764. [Google Scholar] [CrossRef] [Green Version]
- Bevilaqua, L.; Ardenghi, P.; Schroder, N.; Bromberg, E.; Schmitz, P.K.; Schaeffer, E.; Quevedo, J.; Bianchin, M.; Walz, R.; Medina, J.H.; et al. Drugs acting upon the cyclic adenosine monophosphate protein kinase A signalling pathway modulate memory consolidation when given late after training into rat hippocampus but not amygdala. Behav. Pharm. 1997, 8, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Mishima, K.; Hayakawa, K.; Abe, K.; Ikeda, T.; Egashira, N.; Iwasaki, K.; Fujiwara, M. Cannabidiol prevents cerebral infarction via a serotonergic 5-hydroxytryptamine1A receptor-dependent mechanism. Stroke 2005, 36, 1077–1082. [Google Scholar] [CrossRef] [Green Version]
- Gomes, F.V.; Del Bel, E.A.; Guimaraes, F.S. Cannabidiol attenuates catalepsy induced by distinct pharmacological mechanisms via 5-HT1A receptor activation in mice. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 46, 43–47. [Google Scholar] [CrossRef] [Green Version]
- Sonego, A.B.; Gomes, F.V.; Del Bel, E.A.; Guimaraes, F.S. Cannabidiol attenuates haloperidol-induced catalepsy and c-Fos protein expression in the dorsolateral striatum via 5-HT1A receptors in mice. Behav. Brain Res. 2016, 309, 22–28. [Google Scholar] [CrossRef]
- Pelz, M.C.; Schoolcraft, K.D.; Larson, C.; Spring, M.G.; Lopez, H.H. Assessing the role of serotonergic receptors in cannabidiol’s anticonvulsant efficacy. Epilepsy Behav. 2017, 73, 111–118. [Google Scholar] [CrossRef] [PubMed]
- De Gregorio, D.; McLaughlin, R.J.; Posa, L.; Ochoa-Sanchez, R.; Enns, J.; Lopez-Canul, M.; Aboud, M.; Maione, S.; Comai, S.; Gobbi, G. Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain. Pain 2019, 160, 136–150. [Google Scholar] [CrossRef] [PubMed]
- Avraham, Y.; Grigoriadis, N.; Poutahidis, T.; Vorobiev, L.; Magen, I.; Ilan, Y.; Mechoulam, R.; Berry, E. Cannabidiol improves brain and liver function in a fulminant hepatic failure-induced model of hepatic encephalopathy in mice. Br. J. Pharm. 2011, 162, 1650–1658. [Google Scholar] [CrossRef] [Green Version]
- Marichal-Cancino, B.A.; Fajardo-Valdez, A.; Ruiz-Contreras, A.E.; Mendez-Diaz, M.; Prospero-Garcia, O. Advances in the Physiology of GPR55 in the Central Nervous System. Curr. Neuropharmacol. 2017, 15, 771–778. [Google Scholar] [CrossRef] [Green Version]
- Kremshofer, J.; Siwetz, M.; Berghold, V.M.; Lang, I.; Huppertz, B.; Gauster, M. A role for GPR55 in human placental venous endothelial cells. Histochem. Cell Biol. 2015, 144, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Sylantyev, S.; Jensen, T.P.; Ross, R.A.; Rusakov, D.A. Cannabinoid- and lysophosphatidylinositol-sensitive receptor GPR55 boosts neurotransmitter release at central synapses. Proc. Natl. Acad. Sci. USA 2013, 110, 5193–5198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryberg, E.; Larsson, N.; Sjögren, S.; Hjorth, S.; Hermansson, N.O.; Leonova, J.; Elebring, T.; Nilsson, K.; Drmota, T.; Greasley, P. The orphan receptor GPR55 is a novel cannabinoid receptor. Br. J. Pharm. 2007, 152, 1092–1101. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.A.; Hill, A.J.; Smith, I.; Bevan, S.A.; Williams, C.M.; Whalley, B.J.; Stephens, G.J. Cannabidiol displays antiepileptiform and antiseizure properties in vitro and in vivo. J. Pharm. Exp. 2010, 332, 569–577. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, J.S.; Stella, N.; Catterall, W.A.; Westenbroek, R.E. Cannabidiol attenuates seizures and social deficits in a mouse model of Dravet syndrome. Proc. Natl. Acad. Sci. USA 2017, 114, 11229–11234. [Google Scholar] [CrossRef] [Green Version]
- Celorrio, M.; Rojo-Bustamante, E.; Fernandez-Suarez, D.; Saez, E.; Estella-Hermoso de Mendoza, A.; Muller, C.E.; Ramirez, M.J.; Oyarzabal, J.; Franco, R.; Aymerich, M.S. GPR55: A therapeutic target for Parkinson’s disease? Neuropharmacology 2017, 125, 319–332. [Google Scholar] [CrossRef]
- Gonzalez-Garcia, C.; Torres, I.M.; Garcia-Hernandez, R.; Campos-Ruiz, L.; Esparragoza, L.R.; Coronado, M.J.; Grande, A.G.; Garcia-Merino, A.; Sanchez Lopez, A.J. Mechanisms of action of cannabidiol in adoptively transferred experimental autoimmune encephalomyelitis. Exp. Neurol. 2017, 298, 57–67. [Google Scholar] [CrossRef]
- De Petrocellis, L.; Ligresti, A.; Moriello, A.S.; Allara, M.; Bisogno, T.; Petrosino, S.; Stott, C.G.; Di Marzo, V. Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br. J. Pharm. 2011, 163, 1479–1494. [Google Scholar] [CrossRef] [Green Version]
- Ross, R.A. Anandamide and vanilloid TRPV1 receptors. Br J. Pharm. 2003, 140, 790–801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vyklicky, L.; Novakova-Tousova, K.; Benedikt, J.; Samad, A.; Touska, F.; Vlachova, V. Calcium-dependent desensitization of vanilloid receptor TRPV1: A mechanism possibly involved in analgesia induced by topical application of capsaicin. Physiol. Res. 2008, 57, 59–68. [Google Scholar]
- Jara-Oseguera, A.; Simon, S.A.; Rosenbaum, T. TRPV1: On the road to pain relief. Curr. Mol. Pharm. 2008, 1, 255–269. [Google Scholar] [CrossRef]
- Novakova-Tousova, K.; Vyklicky, L.; Susankova, K.; Benedikt, J.; Samad, A.; Teisinger, J.; Vlachova, V. Functional changes in the vanilloid receptor subtype 1 channel during and after acute desensitization. Neuroscience 2007, 149, 144–154. [Google Scholar] [CrossRef]
- Planells-Cases, R.; Garcia-Sanz, N.; Morenilla-Palao, C.; Ferrer-Montiel, A. Functional aspects and mechanisms of TRPV1 involvement in neurogenic inflammation that leads to thermal hyperalgesia. Pflug. Arch. Eur. J. Phys. 2005, 451, 151–159. [Google Scholar] [CrossRef]
- Srivastava, M.D.; Srivastava, B.I.; Brouhard, B. Delta9 tetrahydrocannabinol and cannabidiol alter cytokine production by human immune cells. Immunopharmacology 1998, 40, 179–185. [Google Scholar] [CrossRef]
- Bisogno, T.; Hanus, L.; De Petrocellis, L.; Tchilibon, S.; Ponde, D.E.; Brandi, I.; Moriello, A.S.; Davis, J.B.; Mechoulam, R.; Di Marzo, V. Molecular targets for cannabidiol and its synthetic analogues: Effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br. J. Pharm. 2001, 134, 845–852. [Google Scholar] [CrossRef]
- Luo, H.L.; Rossi, E.; Saubamea, B.; Chasseigneaux, S.; Cochois, V.; Choublier, N.; Smirnova, M.; Glacial, F.; Perriere, N.; Bourdoulous, S.; et al. Cannabidiol Increases Proliferation, Migration, Tubulogenesis, and Integrity of Human Brain Endothelial Cells through TRPV2 Activation. Mol. Pharm. 2019, 16, 1312–1326. [Google Scholar] [CrossRef] [PubMed]
- Nabissi, M.; Morelli, M.B.; Santoni, M.; Santoni, G. Triggering of the TRPV2 channel by cannabidiol sensitizes glioblastoma cells to cytotoxic chemotherapeutic agents. Carcinogenesis 2013, 34, 48–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esposito, G.; De Filippis, D.; Carnuccio, R.; Izzo, A.A.; Iuvone, T. The marijuana component cannabidiol inhibits β-amyloid-induced tau protein hyperphosphorylation through Wnt/β-catenin pathway rescue in PC12 cells. J. Mol. Med. 2006, 84, 253–258. [Google Scholar] [CrossRef]
- Cheng, D.; Low, J.K.; Logge, W.; Garner, B.; Karl, T. Chronic cannabidiol treatment improves social and object recognition in double transgenic APP. (swe)/PS1a Delta E9 mice. Psychopharmacology 2014, 231, 3009–3017. [Google Scholar] [CrossRef] [PubMed]
- Cai, W.; Yang, T.; Liu, H.; Han, L.J.; Zhang, K.; Hu, X.M.; Zhang, X.J.; Yin, K.J.; Gao, Y.Q.; Bennett, M.V.L.; et al. Peroxisome proliferator-activated receptor γ (PPARγ): A master gatekeeper in CNS injury and repair. Prog. Neurobiol. 2018, 163, 27–58. [Google Scholar] [CrossRef]
- Surgucheva, I.; Surguchov, A. Γ-synuclein: Cell-type-specific promoter activity and binding to transcription factors. J. Mol. Neurosci. Mn 2008, 35, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.Z.; Moreau, F.; Chadee, K. PPAR γ is an E3 ligase that induces the degradation of NF-κB/p65. Nat. Commun. 2012, 3, 1–11. [Google Scholar] [CrossRef] [Green Version]
- O’Sullivan, S.E. An update on PPAR activation by cannabinoids. Br J. Pharm. 2016, 173, 1899–1910. [Google Scholar] [CrossRef] [Green Version]
- Hughes, B.; Herron, C.E. Cannabidiol Reverses Deficits in Hippocampal LTP in a Model of Alzheimer’s Disease. Neurochem. Res. 2019, 44, 703–713. [Google Scholar] [CrossRef]
- Aia, P.G.; Revuelta, G.J.; Cloud, L.J.; Factor, S.A. Tardive dyskinesia. Curr. Treat. Options Neurol. 2011, 13, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Sonego, A.B.; Prado, D.S.; Vale, G.T.; Sepulveda-Diaz, J.E.; Cunha, T.M.; Tirapelli, C.R.; Del Bel, E.A.; Raisman-Vozari, R.; Guimaraes, F.S. Cannabidiol prevents haloperidol-induced vacuos chewing movements and inflammatory changes in mice via PPARγ receptors. Brain Behav. Immun. 2018, 74, 241–251. [Google Scholar] [CrossRef]
- Dos-Santos-Pereira, M.; da-Silva, C.A.; Guimaraes, F.S.; Del-Bel, E. Co-administration of cannabidiol and capsazepine reduces l-DOPA-induced dyskinesia in mice: Possible mechanism of action. Neurobiol. Dis. 2016, 94, 179–195. [Google Scholar] [CrossRef]
- Hind, W.H.; England, T.J.; O’Sullivan, S.E. Cannabidiol protects an in vitro model of the blood-brain barrier from oxygen-glucose deprivation via PPARγ and 5-HT1A receptors. Br J. Pharm. 2016, 173, 815–825. [Google Scholar] [CrossRef] [Green Version]
- Giacoppo, S.; Pollastro, F.; Grassi, G.; Bramanti, P.; Mazzon, E. Target regulation of PI3K/Akt/mTOR pathway by cannabidiol in treatment of experimental multiple sclerosis. Fitoterapia 2017, 116, 77–84. [Google Scholar] [CrossRef]
- Sigel, E.; Steinmann, M.E. Structure, function, and modulation of GABA(A) receptors. J. Biol. Chem. 2012, 287, 40224–40231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabow, L.E.; Russek, S.J.; Farb, D.H. From ion currents to genomic analysis: Recent advances in GABAA receptor research. Synapse 1995, 21, 189–274. [Google Scholar] [CrossRef]
- Cifelli, P.; Ruffolo, G.; De Felice, E.; Alfano, V.; van Vliet, E.A.; Aronica, E.; Palma, E. Phytocannabinoids in Neurological Diseases: Could They Restore a Physiological GABAergic Transmission? Int. J. Mol. Sci. 2020, 21, 723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holley, S.M.; Galvan, L.; Kamdjou, T.; Dong, A.; Levine, M.S.; Cepeda, C. Major Contribution of Somatostatin-Expressing Interneurons and Cannabinoid Receptors to Increased GABA Synaptic Activity in the Striatum of Huntington’s Disease Mice. Front. Synaptic Neurosci. 2019, 11, 14. [Google Scholar] [CrossRef] [Green Version]
- Palma, E.; Ruffolo, G.; Cifelli, P.; Roseti, C.; Vliet, E.A.V.; Aronica, E. Modulation of GABAA Receptors in the Treatment of Epilepsy. Curr. Pharm. Des. 2017, 23, 5563–5568. [Google Scholar] [CrossRef]
- Olsen, R.W.; Liang, J. Role of GABAA receptors in alcohol use disorders suggested by chronic intermittent ethanol (CIE) rodent model. Mol. Brain 2017, 10, 45. [Google Scholar] [CrossRef] [PubMed]
- Bambico, F.R.; Li, Z.; Oliveira, C.; McNeill, S.; Diwan, M.; Raymond, R.; Nobrega, J.N. Rostrocaudal subregions of the ventral tegmental area are differentially impacted by chronic stress. Psychopharmacol. (Berl.) 2019, 236, 1917–1929. [Google Scholar] [CrossRef]
- Gugliandolo, A.; Silvestro, S.; Chiricosta, L.; Pollastro, F.; Bramanti, P.; Mazzon, E. The Transcriptomic Analysis of NSC-34 Motor Neuron-Like Cells Reveals That Cannabigerol Influences Synaptic Pathways: A Comparative Study with Cannabidiol. Life 2020, 10, 227. [Google Scholar] [CrossRef]
- Perucca, E. Cannabinoids in the Treatment of Epilepsy: Hard Evidence at Last? J. Epilepsy Res. 2017, 7, 61–76. [Google Scholar] [CrossRef]
- Tang, R.R.; Fang, F. Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N. Engl. J. Med. 2017, 377, 699. [Google Scholar]
- Devinsky, O.; Cross, J.H.; Laux, L.; Marsh, E.; Miller, I.; Nabbout, R.; Scheffer, I.E.; Thiele, E.A.; Wright, S.; Cannabidiol in Dravet Syndrome Study, G. Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N. Engl. J. Med. 2017, 376, 2011–2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruffolo, G.; Cifelli, P.; Roseti, C.; Thom, M.; van Vliet, E.A.; Limatola, C.; Aronica, E.; Palma, E. A novel GABAergic dysfunction in human Dravet syndrome. Epilepsia 2018, 59, 2106–2117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FDA, U.S. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. Silver Spring: Us Food Drug Adm. 2018. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-drug-comprised-active-ingredient-derived-marijuana-treat-rare-severe-forms (accessed on 16 December 2019).
- Geffrey, A.L.; Pollack, S.F.; Bruno, P.L.; Thiele, E.A. Drug-drug interaction between clobazam and cannabidiol in children with refractory epilepsy. Epilepsia 2015, 56, 1246–1251. [Google Scholar] [CrossRef]
- Hess, E.J.; Moody, K.A.; Geffrey, A.L.; Pollack, S.F.; Skirvin, L.A.; Bruno, P.L.; Paolini, J.L.; Thiele, E.A. Cannabidiol as a new treatment for drug-resistant epilepsy in tuberous sclerosis complex. Epilepsia 2016, 57, 1617–1624. [Google Scholar] [CrossRef]
- Gaston, T.E.; Bebin, E.M.; Cutter, G.R.; Liu, Y.; Szaflarski, J.P.; Program, U.C. Interactions between cannabidiol and commonly used antiepileptic drugs. Epilepsia 2017, 58, 1586–1592. [Google Scholar] [CrossRef] [Green Version]
- Nakajima, H. A pharmacological profile of clobazam (Mystan), a new antiepileptic drug. Nihon Yakurigaku Zasshi. Folia Pharm. Jpn. 2001, 118, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Sankar, R. GABA A receptor physiology and its relationship to the mechanism of action of the 1,5-benzodiazepine clobazam. Cns. Drugs 2012, 26, 229–244. [Google Scholar] [CrossRef] [PubMed]
- Jensen, H.S.; Nichol, K.; Lee, D.; Ebert, B. Clobazam and its active metabolite N-desmethylclobazam display significantly greater affinities for α 2-versus α 1-GABA A–receptor complexes. PLoS ONE 2014, 9, e88456. [Google Scholar] [CrossRef]
- Anderson, L.L.; Absalom, N.L.; Abelev, S.V.; Low, I.K.; Doohan, P.T.; Martin, L.J.; Chebib, M.; McGregor, I.S.; Arnold, J.C. Coadministered cannabidiol and clobazam: Preclinical evidence for both pharmacodynamic and pharmacokinetic interactions. Epilepsia 2019, 60, 2224–2234. [Google Scholar] [CrossRef] [Green Version]
- Aso, E.; Andres-Benito, P.; Ferrer, I. Delineating the Efficacy of a Cannabis-Based Medicine at Advanced Stages of Dementia in a Murine Model. J. Alzheimers Dis. 2016, 54, 903–912. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| In Vitro and in Vivo Models | CBD Dose | Treatments | Biological/Pharmacological Effect | Neurological Diseases | Ref. |
|---|---|---|---|---|---|
| Female SJL/J mice | 5 mg/kg | Once-daily during Days 1–7 post-infection | CBD attenuated the activation of microglia downregulating the expression of VCAM-1, CCL2 and CCL5 and the proinflammatory cytokine IL-1β. Moreover, CBD improved motor deficits in the chronic phase of the disease | multiple sclerosis | [18] |
| Newborn C57BL6 mice | 0.1–1000 µM | 15 min. pre-incubation | CBD reduced acute brain damage and apoptosis. Moreover, it induced a reduction concentration of glutamate and IL-6 and decreased the expression of TNF-α, COX-2 and iNOS. | hypoxic-ischemic brain damage | [28] |
| Primary Rat Microglial and N13 Microglial Cells and C57Bl/6 mice | 20 mg/kg | Once-daily during the first week, then 3 days/week for 2 weeks | CBD inhibited ATP-induced intracellular Ca2 + increase in cultured N13 and primary microglial cells and A2A receptors may be involved in this mechanism. In vivo, CBD reduced the gene expression of proinflammatory cytokine IL-6 and prevented cognitive impairment induced by Aβ. | Alzheimer’s disease | [84] |
| Female Sabra mice | 5 mg/kg | Every day for 4 weeks | CBD reduced the expression of the TNF-α-receptor 1 gene in the hippocampus. Conversely, enhanced the expression of the BDNF gene. Moreover, CBD, through the indirect activation of the A2AR, improved the cognitive and motor function of the rats with Hepatic Encephalopathy. | hepatic encephalopathy | [82] |
| In Vivo Models | CBD Dose | Treatments | Biological/Pharmacological Effect | Neurological Diseases | Ref. |
|---|---|---|---|---|---|
| MCA occlusion male mice | 3 or 10 mg/kg | Before and 3 h after damage | CBD, at dose of 3 mg/kg, significantly reduced the infarct volume induced by MCA occlusion, at least in part, through the 5-HT1A receptor. | cerebral ischemia | [87] |
| Male Swiss mice | 5, 15, 30 or 60 mg/kg | 30 min before receiving the drugs that induce catalepsy | Pretreatment with CBD reduced the cataleptic effects, in a dose-dependent manner, through the 5-HT1A receptor. | striatal disorders | [88] |
| Male Swiss mice | 15–60 mg/kg or 60 nmol | 30 min before or 2.5 h after receiving the drugs that induce catalepsy | Pretreatment with CBD reduced the cataleptic effects, in a dose-dependent manner, through the 5-HT1A receptor. | striatal disorders | [89] |
| Male Wistar Kyoto rats | 100 mg/kg | 60 min before induction of seizures | CBD significantly mitigated PTZ-induced seizure. | seizure disorders | [90] |
| Adult male Wistar rats | 0.1–1.0 mg/kg and 5 mg/kg | Acute treatment with cumulative injections of CBD every 5 min and repeated treatment with 5 mg/kg/day for 7 days | CBD (5 mg/kg) protects nerve injury-induced deficits in dorsal raphe nucleus 5-HT neuronal activity. Moreover, CBD exerts antiallodynic effects through the activation of TRPV1 and anxiolytic properties through the activation of 5-HT1A receptors. | allodynia and anxiety-like behavior | [91] |
| Female Sabra mice | 5 mg/kg | 28 days | CBD, through the 5-HT1A receptor activation, improved cognition and motor function, which were impaired by bile-duct ligation. Moreover, in the animal model of hepatic encephalopathy, CBD also reduced neuroinflammation, increasing expression of the BDNF genes and reducing TNF-α receptor 1 gene expression. | hepatic encephalopathy | [83] |
| Female Sabra mice | 5 mg/kg | Single dose | CBD ameliorated cognitive impairments and locomotor activity. Moreover, CBD restored the 5-HT levels in the brain and improved the liver function. | hepatic encephalopathy | [92] |
| In Vitro and in Vivo Models | CBD Dose | Treatments | Biological/Pharmacological Effect | Neurological Diseases | Ref. |
|---|---|---|---|---|---|
| Scn1a mutant mice | 10, 20, 100 or 200 mg/kg | Twice daily for 1 week | Acute treatment of CBD decreased thermally-induced seizures and reduced the rate of spontaneous seizures. Moreover, the low doses of CBD ameliorated the autism-type social interaction deficits in the mouse model of genetically-induced DS. CBD also increased the GABA inhibitory transmission which was impaired in DS. These therapeutic effects of CBD are mediated through GPR55. | DS | [98] |
| Adult male C57BL/6 mice | 5 mg/kg | 5 days a week for 5 weeks | Abnormal-CBD, but not CBD, ameliorated MPTP-induced motor damage. Instead, both compounds significantly reduced the density of microglial cells in the cell body. In the haloperidol-induced catalepsy mouse model, abnormal-CBD also showed anti-cataleptic effects, through the GPR55-activation. | Parkinson’s disease | [99] |
| Male and female C57BL/6 mice | 5–10 and 50 mg/kg | Increasing doses from 5 to 10 mg/kg three times per week, or daily, at a dose of 50 mg/kg, for 23 days | CBD, both at low and high doses, ameliorated the EAE disease. Moreover, CBD treatment reduced the vitality of encephalitogenic cells, levels of IL-6, production of ROS with consequent decrease of the apoptosis process. Additionally, it decreased the levels of GPR55 receptors in the CNS. | EAE disease | [100] |
| In Vitro and in Vivo Models | CBD Dose | Treatments | Biological/Pharmacological Effect | Neurological Diseases | Ref. |
|---|---|---|---|---|---|
| Male Wistar rats | 10 mg/kg | 2 h after the induction of model | CBD inhibited the carrageenan-induced hyperalgesia through the desensitization of the TRPV1 receptor | Hyperalgesia | [31] |
| hPBMECs and hCMEC/D3 Cells | 0.1, 0.3, 1, 3, 10 and 15 μM | 7 or 24 h of incubation | CBD, in a dose-dependent manner, led a last-lasting increase in intracellular Ca2+ level, through activation of TRPV2. In this way, CBD, enhanced cell proliferation, cell migration and tubulogenesis in human brain endothelial cells. | - | [109] |
| U87MG glioma cell line | 10 µM | Cells were treated with different doses of CBD for 1 day or co-treated with CBD 10 µM and chemotherapeutic drugs for 6 h. | CBD, through activation of TRPV2 and the consequent entry of Ca2+, improved the action of chemotherapy drugs enhancing drug absorption and ameliorated cytotoxic activity in human glioma cells. | - | [110] |
| human Gingival Mesenchymal Stem Cells | 5 μM | 24 h of incubation | CBD, through TRPV1 desensitization, promoted the PI3K/Akt pathway signaling, which can reduce Alzheimer’s hallmarks. | Alzheimer’s disease | [37] |
| In Vitro and in Vivo Models | CBD Dose | Treatments | Biological/Pharmacological Effect | Neurological Diseases | Ref. |
|---|---|---|---|---|---|
| SH-SY5YAPP+ | 10−9–10−6 M | 24 h | CBD reduced the expression of the APP protein, as well as its ubiquitination, thus leading to the reduction of Aβ and neuronal apoptosis. These CBD’s effects were mediated by PPARγ activation. | Alzheimer’s disease | [64] |
| Cultures primary of astrocytes rat and male Sprague-Dawley rats | 10−9–10−7 M for in vitro study; 10 mg/kg, for in vivo study. | Daily for 15 days | In the in vitro study, CBD in a concentration-dependent manner reduced the effect of Aβ mediated through the inhibition of NF-κB. In addition, in vivo, CBD ameliorated neuronal damage induced by Aβ and led to a reduction of gliosis and glial fibrillary acidic protein. CBD exerts these effects through PPARγ activation. | Alzheimer’s disease | [17] |
| Hippocampal slices from C57Bl/6 mice | 10 µM | 30 min before to the addition of Aβ | The treatment with CBD improved the synaptic transmission and the potentiation long-term in the hippocampus slice of C57/black 6 mice, thereby preserving it from cognitive deficits induced by Aβ1–42. CBD exerts these effects, at least in part, through interaction with PPARγ. | Alzheimer’s disease | [117] |
| Primary microglial cultures from brain of male and female newborn C57/BL6 mice and Swiss mice | 60 mg/kg; for in vivo study; 10 µM for in vitro study | Two daily injections 30 min before received haloperidol for 21 days | In mice, CBD treatment prevented dyskinesia induced by haloperidol. Moreover, in the corpus striatum, CBD reduced oxidative stress, activation of microglial, inflammatory cytokine (such as IL-1β and TNF-α) and increased anti-inflammatory cytokine IL-10. It was demonstrated that PPARγ is a molecular target of CBD. In the same way, it was also confirmed the effect of CBD through PPARγ on lipopolysaccharide-stimulated microglial cells. | Tardive dyskinesia | [119] |
| Male adult C57 ⁄ BL6 mice | 15, 30 and 60 mg/kg | 15 min before the l-DOPA administration for three days | CBD alone was not able to prevent the l-DOPA-induced dyskinesia. The co-treatment with CBD and capsazepine, through the interaction with CB1 and PPARγ receptors, ameliorate dyskinesia. | Parkinson’s disease | [120] |
| Human brain microvascular endothelial cell and human astrocyte co-cultures modeled | 100 nM, 1 and 10 μM | Either before or immediately after the induction of ischemic damage | CBD (10 μM) prevented the enhance of BBB permeability following the ischemic damage induced by oxygen-glucose deprivation, through the activation of PPARγ and 5-HT1A receptors. | Ischemic stroke | [121] |
| Male C57BL/6 mice | 10 mg/kg | Daily treated, approximately 14 days after disease induction, for 14 days | CBD treatment ameliorated the clinical evidence of disease in EAE mice. CBD restored the PI3K/Akt/mTOR pathway that was downregulated after EAE induction. Moreover, CBD reduced inflammatory cytokines IFN-γ and IL-17 significantly and increased the levels of PPARγ. Probably, the anti-inflammatory effects of CBD are linked to the increased of PPARγ. | EAE disease | [122] |
| In Vitro and in Vivo Models | CBD Dose | Treatments | Biological/Pharmacological Effect | Neurological Diseases | Ref. |
|---|---|---|---|---|---|
| Surgical human DS and TSC cortical tissue in Xenopus oocytes | 5 μM | Pre-incubation of cells of 10 s before the co-application of GABA and CBD | CBD, through positive modulation of GABAA receptors, enhanced the amplitude of the GABA-evoked current, in brain tissues of patients with DS and TSC. | DS and TSC | [134] |
| Male and female Scn1a+/− mice and Xenopus oocytes expressing GABAA receptors | 12 mg/kg or 100 mg/kg for in vivo study; 10 µM for in vitro study | In in vivo study, CBD was administrated i.p. 45 min before CLB; in in vitro study CBD (10 µM) was co-applied with GABA, for 60 s | CBD significantly increased the concentrations of CLB and its active metabolite N-CLB, both in the plasma and in the brain. Co-administration of both compounds significantly increased the anticonvulsant effect. CBD and CLB exert their anticonvulsant action by enhancing the activity of the GABAA receptor. | DS | [142] |
Sample Availability: Not available. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silvestro, S.; Schepici, G.; Bramanti, P.; Mazzon, E. Molecular Targets of Cannabidiol in Experimental Models of Neurological Disease. Molecules 2020, 25, 5186. https://doi.org/10.3390/molecules25215186
Silvestro S, Schepici G, Bramanti P, Mazzon E. Molecular Targets of Cannabidiol in Experimental Models of Neurological Disease. Molecules. 2020; 25(21):5186. https://doi.org/10.3390/molecules25215186
Chicago/Turabian StyleSilvestro, Serena, Giovanni Schepici, Placido Bramanti, and Emanuela Mazzon. 2020. "Molecular Targets of Cannabidiol in Experimental Models of Neurological Disease" Molecules 25, no. 21: 5186. https://doi.org/10.3390/molecules25215186
APA StyleSilvestro, S., Schepici, G., Bramanti, P., & Mazzon, E. (2020). Molecular Targets of Cannabidiol in Experimental Models of Neurological Disease. Molecules, 25(21), 5186. https://doi.org/10.3390/molecules25215186






