Analytical and Clinical Validation of Assays for Volumetric Absorptive Microsampling (VAMS) of Drugs in Different Blood Matrices: A Literature Review
Abstract
:1. Introduction
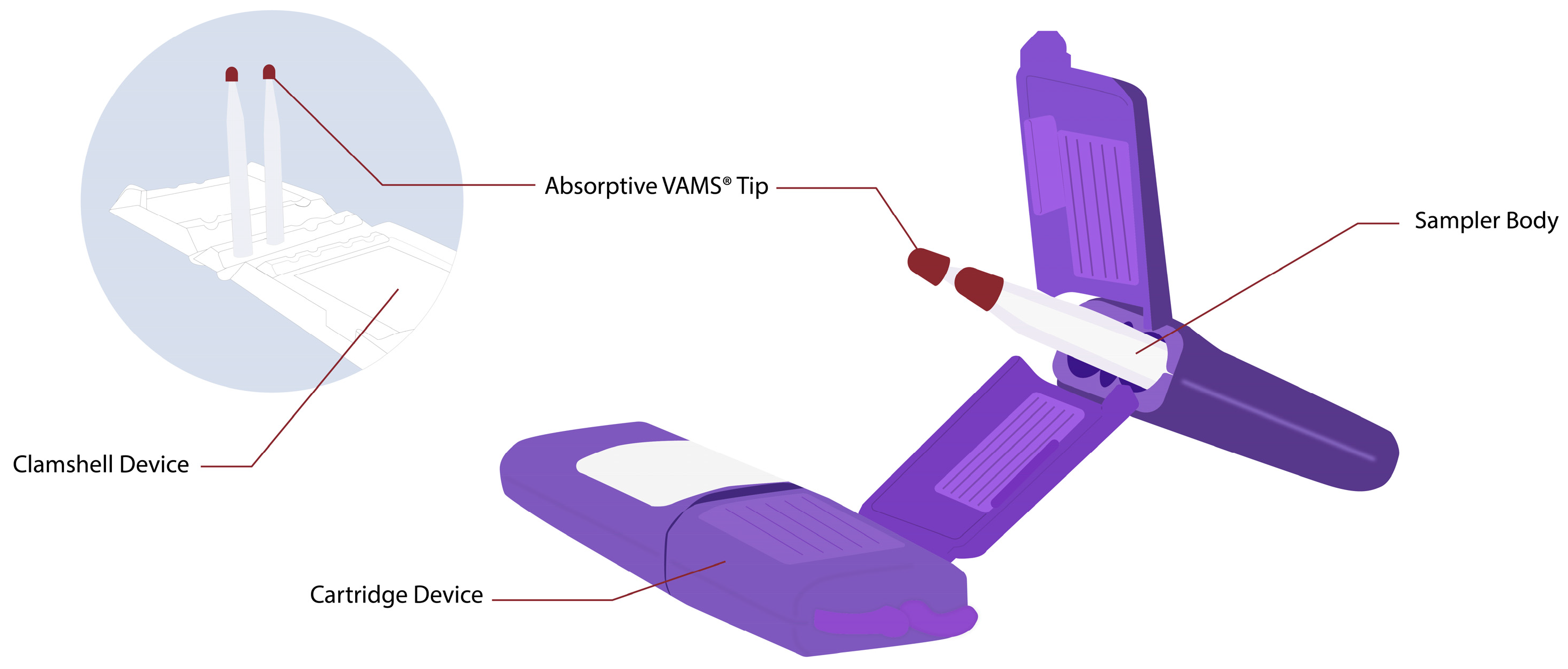
2. Volumetric Absorptive Microsampling (VAMS)
3. Analytical Validation of Volumetric Absorptive Microsampling (VAMS) Assays of Drugs
3.1. Optimization and Validation
3.1.1. Optimization and Validation of Assays for Acidic Drugs
3.1.2. Optimization and Validation of Assays for Basic Drugs
3.1.3. Optimization and Validation of Assays for Neutral Drugs
4. Clinical Validation of Volumetric Absorptive Microsampling (VAMS) of Drugs
5. Future Prospective of Volumetric Absorptive Microsampling (VAMS)
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Aronson, J.K. Concentration-effect and dose-response relations in clinical pharmacology. Br. J. Clin. Pharmacol. 2007, 63, 255–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holford, N.H.G.; Sheiner, L.B. Understanding the Dose-Effect Relationship. Clin. Pharmacokinet. 1981, 6, 429–453. [Google Scholar] [CrossRef] [PubMed]
- Aarnoutse, R.E.; Schapiro, J.M.; Boucher, C.A.B.; Hekster, Y.A.; Burger, D.M. Therapeutic drug monitoring: An aid to optimising response to antiretroviral drugs? Drugs 2003, 63, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Saleem, M.A.; Basharat, R.; Rana, N.A.; Akhtar Khan Khattak, S. Role of clinician in therapeutic drug monitoring practice. Clin. Pract. 2020, 17, 1429–1435. [Google Scholar]
- Ghiculesco, R. Abnormal laboratory results: Therapeutic drug monitoring: Which drugs, why, when and how to do it. Aust. Prescr. 2008, 31, 42–44. [Google Scholar] [CrossRef]
- Roberge, R.J. Venodilatation techniques to enhance venepuncture and intravenous cannulation. J. Emerg. Med. 2004, 27, 69–73. [Google Scholar] [CrossRef]
- Buowari, O.Y. Complications of venepuncture. Adv. Biosci. Biotechnol. 2013, 4, 126–128. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, R.; O’Sullivan, J.F.; O’Kennedy, R. Determination of serum and tissue levels of phenazines including clofazimine. J. Chromatogr. B Biomed. Appl. 1996, 681, 307–315. [Google Scholar] [CrossRef]
- Schaad-Lanyi, Z.; Dieterle, W.; Dubois, J.P.; Theobald, W.; Vischer, W. Pharmacokinetics of clofazimine in healthy volunteers. Int. J. Lepr. 1987, 55, 9–15. [Google Scholar]
- Katzung, B.G. Basic & Clinical Pharmacology, 14th ed.; McGraw Hill Medical: New York, NY, USA, 2018; ISBN 9781259641152. [Google Scholar]
- Lei, B.U.W.; Prow, T.W. A review of microsampling techniques and their social impact. Biomed. Microdevices 2019, 21, 81. [Google Scholar] [CrossRef] [Green Version]
- Parker, S.L.; Dorofaeff, T.; Lipman, J.; Ballot, D.E.; Bandini, R.M.; Wallis, S.C.; Roberts, J.A. Is there a role for microsampling in antibiotic pharmacokinetic studies? Expert Opin. Drug Metab. Toxicol. 2016, 12, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Gao, H. Evaluation of sample extraction methods for minimizing hematocrit effect on whole blood analysis with volumetric absorptive microsampling. Bioanalysis 2017, 9, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Barco, S.; Castagnola, E.; Moscatelli, A.; Rudge, J.; Tripodi, G.; Cangemi, G. Volumetric adsorptive microsampling-liquid chromatography tandem mass spectrometry assay for the simultaneous quantification of four antibiotics in human blood: Method development, validation and comparison with dried blood spot. J. Pharm. Biomed. Anal. 2017, 145, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Koponen, J.; Rudge, J.; Kushon, S.; Kiviranta, H. Novel volumetric adsorptive microsampling technique for determination of perfluorinated compounds in blood. Anal. Biochem. 2018, 545, 49–53. [Google Scholar] [CrossRef] [PubMed]
- D’Urso, A.; Rudge, J.; Patsalos, P.N.; De Grazia, U. Volumetric Absorptive Microsampling: A New Sampling Tool for Therapeutic Drug Monitoring of Antiepileptic Drugs. Ther. Drug Monit. 2019, 41, 681–692. [Google Scholar] [CrossRef]
- Lee, K.; Jun, S.H.; Choi, M.S.; Song, S.H.; Park, J.S.; Lee, J.H.; Park, K.U.; Song, J. Application of the isoniazid assay in dried blood spots using the ultra-performance liquid chromatography-tandem mass spectrometry. Clin. Biochem. 2017, 50, 882–885. [Google Scholar] [CrossRef]
- Denniff, P.; Spooner, N. Volumetric absorptive microsampling: A dried sample collection technique for quantitative bioanalysis. Anal. Chem. 2014, 86, 8489–8495. [Google Scholar] [CrossRef]
- Kok, M.G.M.M.; Fillet, M. Volumetric absorptive microsampling: Current advances and applications. J. Pharm. Biomed. Anal. 2018, 147, 288–296. [Google Scholar] [CrossRef]
- Marchand, A.; Roulland, I.; Semence, F.; Audran, M. Volumetric Absorptive Microsampling (VAMS) technology for IGF-1 quantification by automated chemiluminescent immunoassay in dried blood. Growth Horm. IGF Res. 2019, 50, 27–34. [Google Scholar] [CrossRef]
- Spooner, N.; Denniff, P.; Michielsen, L.; De Vries, R.; Ji, Q.C.; Arnold, M.E.; Woods, K.; Woolf, E.J.; Xu, Y.; Boutet, V.; et al. A device for dried blood microsampling in quantitative bioanalysis: Overcoming the issues associated blood hematocrit. Bioanalysis 2015, 7, 653–659. [Google Scholar] [CrossRef]
- Protti, M.; Mandrioli, R.; Mercolini, L. Tutorial: Volumetric absorptive microsampling (VAMS). Anal. Chim. Acta 2019, 1046, 32–47. [Google Scholar] [CrossRef]
- Imre, S.; Vlase, L.; Muntean, D.L. Bioanalytical method validation. Rev. Rom. Med. Lab. 2008, 10, 13–21. [Google Scholar] [CrossRef]
- Capiau, S.; Veenhof, H.; Koster, R.A.; Bergqvist, Y.; Boettcher, M.; Halmingh, O.; Keevil, B.G.; Koch, B.C.P.; Linden, R.; Pistos, C.; et al. Official International Association for Therapeutic Drug Monitoring and Clinical Toxicology Guideline: Development and Validation of Dried Blood Spot-Based Methods for Therapeutic Drug Monitoring. Ther. Drug Monit. 2019, 41, 409–430. [Google Scholar] [CrossRef] [PubMed]
- Kocur, A.; Pawiński, T. Volumetric Absorptive Microsampling in Therapeutic Drug Monitoring of Immunosuppressive Drugs—From Sampling and Analytical Issues to Clinical Application. Int. J. Mol. Sci. 2023, 24, 681. [Google Scholar] [CrossRef] [PubMed]
- Denniff, P.; Parry, S.; Dopson, W.; Spooner, N. Quantitative bioanalysis of paracetamol in rats using volumetric absorptive microsampling (VAMS). J. Pharm. Biomed. Anal. 2015, 108, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, G.S.; Vedar, C.; Downes, K.J.; Fitzgerald, J.C.; Scheetz, M.H.; Zuppa, A.F. Microsampling Assays for Pharmacokinetic Analysis and Therapeutic Drug Monitoring of Antimicrobial Drugs in Children: A Critical Review. Ther. Drug Monit. 2021, 43, 335–345. [Google Scholar] [CrossRef]
- De Kesel, P.M.M.; Lambert, W.E.; Stove, C.P. Does volumetric absorptive microsampling eliminate the hematocrit bias for caffeine and paraxanthine in dried blood samples? A comparative study. Anal. Chim. Acta 2015, 881, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Marahatta, A.; Megaraj, V.; McGann, P.T.; Ware, R.E.; Setchell, K.D.R. Stable-isotope dilution HPLC-electrospray ionization tandem mass spectrometry method for quantifying hydroxyurea in dried blood samples. Clin. Chem. 2016, 62, 1593–1601. [Google Scholar] [CrossRef] [Green Version]
- Anoshkina, Y.; Costas-Rodríguez, M.; Vanhaecke, F. Iron isotopic analysis of finger-prick and venous blood by multi-collector inductively coupled plasma-mass spectrometry after volumetric absorptive microsampling. J. Anal. At. Spectrom. 2017, 32, 314–321. [Google Scholar] [CrossRef]
- Kip, A.E.; Kiers, K.C.; Rosing, H.; Schellens, J.H.M.; Beijnen, J.H.; Dorlo, T.P.C. Volumetric absorptive microsampling (VAMS) as an alternative to conventional dried blood spots in the quantification of miltefosine in dried blood samples. J. Pharm. Biomed. Anal. 2017, 135, 160–166. [Google Scholar] [CrossRef]
- Protti, M.; Rudge, J.; Sberna, A.E.; Gerra, G.; Mercolini, L. Dried haematic microsamples and LC–MS/MS for the analysis of natural and synthetic cannabinoids. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1044–1045, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Nys, G.; Cobraiville, G.; Kok, M.G.M.; Wéra, O.; Servais, A.C.; Fillet, M. Comparison of nanofluidic and ultra-high performance liquid chromatography-tandem mass spectrometry for high sensitive pharmacokinetic studies of estrogens starting from whole blood microsampling. J. Chromatogr. A 2017, 1524, 160–168. [Google Scholar] [CrossRef]
- Kita, K.; Mano, Y. Application of volumetric absorptive microsampling device for quantification of tacrolimus in human blood as a model drug of high blood cell partition. J. Pharm. Biomed. Anal. 2017, 143, 168–175. [Google Scholar] [CrossRef]
- Youhnovski, N.; Mayrand-Provencher, L.; Bérubé, E.R.; Plomley, J.; Montpetit, H.; Furtado, M.; Keyhani, A. Volumetric absorptive microsampling combined with impact-assisted extraction for hematocrit effect free assays. Bioanalysis 2017, 9, 1761–1769. [Google Scholar] [CrossRef] [PubMed]
- Protti, M.; Catapano, M.C.; Samolsky Dekel, B.G.; Rudge, J.; Gerra, G.; Somaini, L.; Mandrioli, R.; Mercolini, L. Determination of oxycodone and its major metabolites in haematic and urinary matrices: Comparison of traditional and miniaturised sampling approaches. J. Pharm. Biomed. Anal. 2018, 152, 204–214. [Google Scholar] [CrossRef]
- Kovač, J.; Panic, G.; Neodo, A.; Meister, I.; Coulibaly, J.T.; Schulz, J.D.; Keiser, J. Evaluation of a novel micro-sampling device, MitraTM, in comparison to dried blood spots, for analysis of praziquantel in Schistosoma haematobium-infected children in rural Côte d’Ivoire. J. Pharm. Biomed. Anal. 2018, 151, 339–346. [Google Scholar] [CrossRef]
- Qu, Y.; Brady, K.; Apilado, R.; O’Malley, T.; Reddy, S.; Chitkara, P.; Ibarra, C.; Alexander, R.V.; Dervieux, T. Capillary blood collected on volumetric absorptive microsampling (VAMS) device for monitoring hydroxychloroquine in rheumatoid arthritis patients. J. Pharm. Biomed. Anal. 2017, 140, 334–341. [Google Scholar] [CrossRef]
- Parker, S.L.; Roberts, J.A.; Lipman, J.; Wallis, S.C. Quantitative bioanalytical validation of fosfomycin in human whole blood with volumetric absorptive microsampling. Bioanalysis 2015, 7, 2585–2595. [Google Scholar] [CrossRef]
- Houbart, V.; Cobraiville, G.; Servais, A.C.; Napp, A.; Merville, M.P.; Fillet, M. Hepcidin determination in dried blood by microfluidic LC-MS/MS: Comparison of DBS and volumetric absorptive microsampling for matrix effect and recovery. Bioanalysis 2015, 7, 2789–2799. [Google Scholar] [CrossRef] [PubMed]
- Bolea-Fernandez, E.; Phan, K.; Balcaen, L.; Resano, M.; Vanhaecke, F. Determination of ultra-trace amounts of prosthesis-related metals in whole blood using volumetric absorptive micro-sampling and tandem ICP-Mass spectrometry. Anal. Chim. Acta 2016, 941, 1–9. [Google Scholar] [CrossRef]
- Cañabate, Á.; García-Ruiz, E.; Resano, M.; Todolí, J.L. Analysis of whole blood by ICP-MS equipped with a high temperature total sample consumption system. J. Anal. At. Spectrom. 2017, 32, 78–87. [Google Scholar] [CrossRef] [Green Version]
- John, H.; Willoh, S.; Hörmann, P.; Siegert, M.; Vondran, A.; Thiermann, H. Procedures for Analysis of Dried Plasma Using Microsampling Devices to Detect Sulfur Mustard-Albumin Adducts for Verification of Poisoning. Anal. Chem. 2016, 88, 8787–8794. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Korfmacher, W.; Ho, S.; Shen, L.; Wang, J.; Wu, Z.; Guo, Y.; Snow, G.; O’shea, T. Evaluation of two blood microsampling approaches for drug discovery PK studies in rats. Bioanalysis 2015, 7, 2345–2359. [Google Scholar] [CrossRef] [PubMed]
- Mercolini, L.; Protti, M.; Catapano, M.C.; Rudge, J.; Sberna, A.E. LC-MS/MS and volumetric absorptive microsampling for quantitative bioanalysis of cathinone analogues in dried urine, plasma and oral fluid samples. J. Pharm. Biomed. Anal. 2016, 123, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Miao, Z.; Farnham, J.G.; Hanson, G.; Podoll, T.; Reid, M.J. Bioanalysis of emixustat (ACU-4429) in whole blood collected with volumetric absorptive microsampling by LC-MS/MS. Bioanalysis 2015, 7, 2071–2083. [Google Scholar] [CrossRef]
- Nys, G.; Gallez, A.; Kok, M.G.M.; Cobraiville, G.; Servais, A.C.; Piel, G.; Pequeux, C.; Fillet, M. Whole blood microsampling for the quantitation of estetrol without derivatization by liquid chromatography-tandem mass spectrometry. J. Pharm. Biomed. Anal. 2017, 140, 258–265. [Google Scholar] [CrossRef]
- Thiry, J.; Evrard, B.; Nys, G.; Fillet, M.; Kok, M.G.M. Sampling only ten microliters of whole blood for the quantification of poorly soluble drugs: Itraconazole as case study. J. Chromatogr. A 2017, 1479, 161–168. [Google Scholar] [CrossRef]
- Parker, S.L.; Guerra Valero, Y.C.; Lipman, J.; Roberts, J.A.; Wallis, S.C. Effect of time on recovery of plasma microsamples for the quantitative determination of vancomycin. Bioanalysis 2016, 8, 2235–2242. [Google Scholar] [CrossRef]
- Londhe, V.; Rajadhyaksha, M. Opportunities and obstacles for microsampling techniques in bioanalysis: Special focus on DBS and VAMS. J. Pharm. Biomed. Anal. 2020, 182, 113102. [Google Scholar] [CrossRef]
- Schulz, J.D.; Neodo, A.; Coulibaly, J.T.; Keiser, J. Pharmacokinetics of Albendazole, Albendazole Sulfoxide, and Albendazole Sulfone Determined from Plasma, Blood, Dried Blood Spots, and Mitra Samples of Hookworm-Infected Adolescents. Antimicrob. Agents Chemother. 2019, 63, e02489-18. [Google Scholar] [CrossRef] [Green Version]
- Canisius, T.P.I.J.M.; Soons, J.W.P.H.; Verschuure, P.; Wammes-Van Der Heijden, E.A.; Rouhl, R.P.W.; Majoie, H.J.M. Therapeutic drug monitoring of anti-epileptic drugs—A clinical verification of volumetric absorptive micro sampling. Clin. Chem. Lab. Med. 2020, 58, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Tron, C.; Ferrand-Sorre, M.J.; Querzerho-Raguideau, J.; Chemouny, J.M.; Houssel-Debry, P.; Verdier, M.C.; Bellissant, E.; Lemaitre, F. Volumetric absorptive microsampling for the quantification of tacrolimus in capillary blood by high performance liquid chromatography-tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2021, 1165, 122521. [Google Scholar] [CrossRef] [PubMed]
- Koster, R.A.; Niemeijer, P.; Veenhof, H.; van Hateren, K.; Alffenaar, J.-W.C.; Touw, D.J. A volumetric absorptive microsampling LC-MS/MS method for five immunosuppressants and their hematocrit effects. Bioanalysis 2019, 11, 495–508. [Google Scholar] [CrossRef] [PubMed]
- Gani, M.R.; Isnaeni; Prawita, A.; Hafid, A.F.; Widyawaruyanti, A. Bioanalytical method development and validation for quantification of morachalcone A in rabbit plasma using high performance liquid chromatography. Pak. J. Pharm. Sci. 2018, 31, 311–315. [Google Scholar]
- Arora, K.; Gangadharappa, H.V. An Approach to Bioanalytical Method Development and Validation: A Review. Int. J. Pharm. Sci. Res. 2016, 7, 2291–2301. [Google Scholar] [CrossRef]
- Moein, M.M.; El Beqqali, A.; Abdel-Rehim, M. Bioanalytical method development and validation: Critical concepts and strategies. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1043, 3–11. [Google Scholar] [CrossRef]
- Chanda Gupta, P. A View on Analytical Method Validation of Drugs. J. Cell Sci. Ther. 2016, 7, 1000235. [Google Scholar] [CrossRef] [Green Version]
- Ozkan, S.A. Analytical method validation: The importance for pharmaceutical analysis. Pharm. Sci. 2018, 24, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Ravichandran, V.; Shalini, S.; Sundram, K.M.; Rajak, H. Validation of analytical methods—Strategies & importance International Journal of Pharmacy and Pharmaceutical Sciences. Int. J. Pharm. Pharm. Sci. 2010, 2, 18–22. [Google Scholar]
- Paniagua-González, L.; Díaz-Louzao, C.; Lendoiro, E.; Otero-Antón, E.; Cadarso-Suárez, C.; López-Rivadulla, M.; Cruz, A.; de-Castro-Ríos, A. Volumetric Absorptive Microsampling (VAMS) for assaying immunosuppressants from venous whole blood by LC–MS/MS using a novel atmospheric pressure ionization probe (UniSprayTM). J. Pharm. Biomed. Anal. 2020, 189, 113422. [Google Scholar] [CrossRef]
- Delahaye, L.; Dhont, E.; De Cock, P.; De Paepe, P.; Stove, C.P. Volumetric absorptive microsampling as an alternative sampling strategy for the determination of paracetamol in blood and cerebrospinal fluid. Anal. Bioanal. Chem. 2019, 411, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Maggadani, B.P.; Harmita; Haryono, S.J.; Rinaldi, M.R.; Harahap, Y. Volumetric absorptive microsampling as a new biosampling tool for monitoring of tamoxifen, endoxifen, 4-oh tamoxifen and n-desmethyltamoxifen in breast cancer patients. Drug Des. Devel. Ther. 2021, 15, 2417–2430. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, G.S.; Vedar, C.; Zane, N.R.; Downes, K.J.; Prodell, J.L.; DiLiberto, M.A.; Zuppa, A.F. Development and validation of a volumetric absorptive microsampling- liquid chromatography mass spectrometry method for the analysis of cefepime in human whole blood: Application to pediatric pharmacokinetic study. J. Pharm. Biomed. Anal. 2020, 179, 113002. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, G.; Bustos, J.A.; Lescano, A.G.; Gonzales, I.; Saavedra, H.; Rodriguez, S.; Pretell, E.J.; Bonato, P.S.; Lanchote, V.L.; Takayanagui, O.M.; et al. Albendazole Sulfoxide Plasma Levels and Efficacy of Antiparasitic Treatment in Patients with Parenchymal Neurocysticercosis. Clin. Infect. Dis. 2019, 69, 1996–2002. [Google Scholar] [CrossRef]
- Wang, F.; Agnihotri, A.; Adabag, S.; Roukoz, H. Clinical Utility of Plasma Amiodarone Level Measurement: A Single Center Experience. Innov. Card. Rythm Manag. 2011, 2, 508–511. [Google Scholar]
- Lamoth, F.; Buclin, T.; Pascual, A.; Vora, S.; Bolay, S.; Decosterd, L.A.; Calandra, T.; Marchetti, O. High cefepime plasma concentrations and neurological toxicity in febrile neutropenic patients with mild impairment of renal function. Antimicrob. Agents Chemother. 2010, 54, 4360–4367. [Google Scholar] [CrossRef] [Green Version]
- Reid, M.J.; Eyre, R.; Podoll, T. Oxidative deamination of emixustat by human vascular adhesion protein-1/semicarbazide-sensitive amine oxidase. Drug Metab. Dispos. 2019, 47, 504–515. [Google Scholar] [CrossRef] [Green Version]
- Aubert, G.; Carricajo, A.; Coudrot, M.; Guyomarch, S.; Auboyer, C.; Zeni, F. Prospective determination of serum ceftazidime concentrations in intensive care units. Ther. Drug Monit. 2010, 32, 517–519. [Google Scholar] [CrossRef]
- Patsalos, P.N. Antiepileptic Drug Interactions; Springer: Berlin, Germany, 2014; ISBN 9781118456989. [Google Scholar]
- Wenzler, E.; Ellis-Grosse, E.J.; Rodvold, K.A. Pharmacokinetics, safety, and tolerability of single-dose intravenous (ZTI-01) and oral fosfomycin in healthy volunteers. Antimicrob. Agents Chemother. 2017, 61, e00775-17. [Google Scholar] [CrossRef] [Green Version]
- Thalhammer, F.; Schenk, P.; Burgmann, H.; El Menyawi, I.; Hollenstein, U.M.; Rosenkranz, A.R.; Sunder-Plassmann, G.; Breyer, S.; Ratheiser, K. Single-dose pharmacokinetics of meropenem during continuous venovenous hemofiltration. Antimicrob. Agents Chemother. 1998, 42, 2417–2420. [Google Scholar] [CrossRef] [Green Version]
- Lo Re, F.; Angelini, J.; Sponga, S.; Nalli, C.; Zucchetto, A.; Biasizzo, J.; Livi, U.; Baraldo, M. Therapeutic Drug Monitoring of Mycophenolic Acid as a Precision Medicine Tool for Heart Transplant Patients: Results of an Observational Pharmacokinetic Pilot Study. Pharmaceutics 2022, 14, 1304. [Google Scholar] [CrossRef]
- Brett, C.N.; Barnett, S.G.; Pearson, J. Postoperative plasma paracetamol levels following oral or intravenous paracetamol administration: A double-blind randomised controlled trial. Anaesth. Intensive Care 2012, 40, 166–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen-Wolkowiez, M.; Watt, K.M.; Zhou, C.; Bloom, B.T.; Poindexter, B.; Castro, L.; Gao, J.; Capparelli, E.V.; Smitha, P.B.; Benjamin, D.K. Developmental pharmacokinetics of piperacillin and tazobactam using plasma and dried blood spots from infants. Antimicrob. Agents Chemother. 2014, 58, 2856–2865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ximenez, J.P.B.; De Andrade, J.M.; Marques, M.P.; Coelho, E.B.; Suarez-Kurtz, G.; Lanchote, V.L. Hormonal status affects plasma exposure of tamoxifen and its main metabolites in tamoxifen-treated breast cancer patients. BMC Pharmacol. Toxicol. 2019, 20, 81. [Google Scholar] [CrossRef]
- Valera, H.R.; Ganguly, B. Study of plasma level of atorvastatin and its effect on lipid profile. Indian J. Physiol. Pharmacol. 2009, 53, 73–82. [Google Scholar] [PubMed]
- Cordell, R.L.; Valkenburg, T.S.E.; Pandya, H.C.; Hawcutt, D.B.; Semple, M.G.; Monks, P.S. Quantitation of salbutamol using micro-volume blood sampling–applications to exacerbations of pediatric asthma. J. Asthma 2018, 55, 1205–1213. [Google Scholar] [CrossRef]
- Abu-Rabie, P.; Neupane, B.; Spooner, N.; Rudge, J.; Denniff, P.; Mulla, H.; Pandya, H. Validation of methods for determining pediatric midazolam using wet whole blood and volumetric absorptive microsampling. Bioanalysis 2019, 11, 1737–1754. [Google Scholar] [CrossRef]
- Moorthy, G.S.; Vedar, C.; Zane, N.; Prodell, J.L.; Zuppa, A.F. Development and validation of a volumetric absorptive microsampling assay for analysis of voriconazole and voriconazole N-oxide in human whole blood. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2019, 1105, 67–75. [Google Scholar] [CrossRef]
- Sciberras, D.; Otoul, C.; Lurquin, F.; Smeraglia, J.; Lappert, A.; De Bruyn, S.; Jaap van Lier, J. A pharmacokinetic study of radiprodil oral suspension in healthy adults comparing conventional venous blood sampling with two microsampling techniques. Pharmacol. Res. Perspect. 2019, 7, e00459. [Google Scholar] [CrossRef] [Green Version]
- Friedl, B.; Kurlbaum, M.; Kroiss, M.; Fassnacht, M.; Scherf-Clavel, O. A method for the minimally invasive drug monitoring of mitotane by means of volumetric absorptive microsampling for a home-based therapeutic drug monitoring. Anal. Bioanal. Chem. 2019, 411, 3951–3962. [Google Scholar] [CrossRef]
- Gal, P. Caffeine Therapeutic Drug Monitoring Is Necessary and Cost-effective. J. Pediatr. Pharmacol. Ther. 2007, 12, 212–215. [Google Scholar] [CrossRef]
- Karch, S. Cathinone Neurotoxicity (“The “3Ms”). Curr. Neuropharmacol. 2014, 13, 21–25. [Google Scholar] [CrossRef] [Green Version]
- Blanchet, B.; Jallouli, M.; Allard, M.; Ghillani-Dalbin, P.; Galicier, L.; Aumaître, O.; Chasset, F.; Le Guern, V.; Lioté, F.; Smail, A.; et al. Hydroxychloroquine levels in patients with systemic lupus erythematosus: Whole blood is preferable but serum levels also detect non-adherence. Arthritis Res. Ther. 2020, 22, 223. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Gil Hurlé, A.; Sánchez Navarro, A.; García Sánchez, M.J. Therapeutic drug monitoring of itraconazole and the relevance of pharmacokinetic interactions. Clin. Microbiol. Infect. 2006, 12, 97–106. [Google Scholar] [CrossRef] [Green Version]
- Douglas-Hall, P.; Dzahini, O.; Gaughran, F.; Bile, A.; Taylor, D. Variation in dose and plasma level of lamotrigine in patients discharged from a mental health trust. Ther. Adv. Psychopharmacol. 2017, 7, 17–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pea, F.; Furlanut, M.; Cojutti, P.; Cristini, F.; Zamparini, E.; Franceschi, L.; Viale, P. Therapeutic drug monitoring of linezolid: A retrospective monocentric analysis. Antimicrob. Agents Chemother. 2010, 54, 4605–4610. [Google Scholar] [CrossRef] [Green Version]
- Jawad, A.M. Rational use of Metoprolol: The Relationship of Its Blood Concentration to Patient Compliance, Poor Quality Medicines and Side Effects. Univ. Thi-Qar J. Med. 2019, 16, 132–141. [Google Scholar] [CrossRef]
- Persson, P.; Nilsson, A.; Hartvig, P.; Tamsen, A. Pharmacokinetics of midazolam in total I. V. Anaesthesia. Br. J. Anaesth. 1987, 59, 548–556. [Google Scholar] [CrossRef]
- Mbui, J.; Olobo, J.; Omollo, R.; Solomos, A.; Kip, A.E.; Kirigi, G.; Sagaki, P.; Kimutai, R.; Were, L.; Omollo, T.; et al. Pharmacokinetics, safety, and efficacy of an allometric miltefosine regimen for the treatment of visceral leishmaniasis in eastern African children: An open-label, phase II clinical trial. Clin. Infect. Dis. 2019, 68, 1530–1538. [Google Scholar] [CrossRef]
- Kerkhofs, T.M.A.; Derijks, L.J.J.; Ettaieb, M.H.T.; Eekhoff, E.M.W.; Neef, C.; Gelderblom, H.; Den Hartigh, J.; Guchelaar, H.J.; Haak, H.R. Short-term variation in plasma mitotane levels confirms the importance of trough level monitoring. Eur. J. Endocrinol. 2014, 171, 677–683. [Google Scholar] [CrossRef] [Green Version]
- Meister, I.; Kovac, J.; Duthaler, U.; Odermatt, P.; Huwyler, J.; Vanobberghen, F.; Sayasone, S.; Keiser, J. Pharmacokinetic Study of Praziquantel Enantiomers and Its Main Metabolite R-trans-4-OH-PZQ in Plasma, Blood and Dried Blood Spots in Opisthorchis viverrini-Infected Patients. PLoS Negl. Trop. Dis. 2016, 10, e0004700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Auvin, S.; Dozières-Puyravel, B.; Avbersek, A.; Sciberras, D.; Collier, J.; Leclercq, K.; Mares, P.; Kaminski, R.M.; Muglia, P. Radiprodil, a NR2B negative allosteric modulator, from bench to bedside in infantile spasm syndrome. Ann. Clin. Transl. Neurol. 2020, 7, 343–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vet, N.J.; de Winter, B.C.M.; Koninckx, M.; Boeschoten, S.A.; Boehmer, A.L.M.; Verhallen, J.T.; Plötz, F.B.; Vaessen-Verberne, A.A.; van der Nagel, B.C.H.; Knibbe, C.A.J.; et al. Population Pharmacokinetics of Intravenous Salbutamol in Children with Refractory Status Asthmaticus. Clin. Pharmacokinet. 2020, 59, 257–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cojutti, P.; Candoni, A.; Forghieri, F.; Isola, M.; Zannier, M.E.; Bigliardi, S.; Luppi, M.; Fanin, R.; Pea, F. Variability of Voriconazole Trough Levels in Haematological Patients: Influence of Comedications with cytochrome P450(CYP) Inhibitors and/or with CYP Inhibitors plus CYP Inducers. Basic Clin. Pharmacol. Toxicol. 2016, 118, 474–479. [Google Scholar] [CrossRef] [Green Version]
- Vethe, N.T.; Gustavsen, M.T.; Midtvedt, K.; Lauritsen, M.E.; Andersen, A.M.; Asberg, A.; Bergan, S. Tacrolimus Can Be Reliably Measured with Volumetric Absorptive Capillary Microsampling Throughout the Dose Interval in Renal Transplant Recipients. Ther. Drug Monit. 2019, 41, 607–614. [Google Scholar] [CrossRef]
- Grześk, G.; Stolarek, W.; Kasprzak, M.; Grześk, E.; Rogowicz, D.; Wiciński, M.; Krzyżanowski, M. Therapeutic drug monitoring of carbamazepine: A 20-year observational study. J. Clin. Med. 2021, 10, 5396. [Google Scholar] [CrossRef]
- Narula, A.S.; Murthy, M.S.N.; Patrulu, K.S.K.; Saxena, V.K. Routine cyclosporine concentration—C2 level monitoring. Is it helpful during the early post transplant period? Med. J. Armed Forces India 2004, 60, 326–328. [Google Scholar] [CrossRef] [Green Version]
- Hirabatake, M.; Mizuno, T.; Kato, H.; Hashida, T. Everolimus pharmacokinetics and exposure-response relationship in Japanese patients with advanced breast cancer. Front. Pharmacol. 2022, 13, 984002. [Google Scholar] [CrossRef]
- May, T.W.; Brandt, C.; Helmer, R.; Bien, C.G.; Cawello, W. Comparison of lacosamide concentrations in cerebrospinal fluid and serum in patients with epilepsy. Epilepsia 2015, 56, 1134–1140. [Google Scholar] [CrossRef]
- Gupta, V.; Gupta, K.; Singh, G.; Kaushal, S. An analytical study to correlate serum levels of levetiracetam with clinical course in patients with epilepsy. J. Neurosci. Rural Pract. 2016, 7, S31–S36. [Google Scholar] [CrossRef]
- González-Esquivel, D.F.; Ortega-Gavilán, M.; Alcántara-López, G.; Jung-Cook, H. Plasma level monitoring of oxcarbazepine in epileptic patients. Arch. Med. Res. 2000, 31, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Steinhoff, B.J.; Hübers, E.; Kurth, C.; Jürges (Kehl-Kork), U. Plasma concentration and clinical effects of perampanel—The Kork experience. Seizure 2019, 67, 18–22. [Google Scholar] [CrossRef] [Green Version]
- Stenton, S.B.; Partovi, N.; Ensom, M.H.H. Sirolimus: The evidence for clinical pharmacokinetic monitoring. Clin. Pharmacokinet. 2005, 44, 769–786. [Google Scholar] [CrossRef]
- Alghanem, S.S.; Soliman, M.M.; Alibrahim, A.A.; Gheith, O.; Kenawy, A.S.; Awad, A. Monitoring Tacrolimus Trough Concentrations During the First Year After Kidney Transplantation: A National Retrospective Cohort Study. Front. Pharmacol. 2020, 11, 566638. [Google Scholar] [CrossRef] [PubMed]
- Martial, L.C.; Aarnoutse, R.E.; Mulder, M.; Schellekens, A.; Brüggemann, R.J.M.; Burger, D.M.; Schene, A.H.; Batalla, A. Dried Blood Spot sampling in psychiatry: Perspectives for improving therapeutic drug monitoring. Eur. Neuropsychopharmacol. 2017, 27, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Veenhof, H.; Koster, R.A.; Junier, L.A.T.; Berger, S.P.; Bakker, S.J.L.; Touw, D.J. Volumetric absorptive microsampling and dried blood spot microsampling vs. Conventional venous sampling for tacrolimus trough concentration monitoring. Clin. Chem. Lab. Med. 2020, 58, 1687–1695. [Google Scholar] [CrossRef]
- Zwart, T.C.; Metscher, E.; van der Boog, P.J.M.; Swen, J.J.; de Fijter, J.W.; Guchelaar, H.J.; de Vries, A.P.J.; Moes, D.J.A.R. Volumetric microsampling for simultaneous remote immunosuppressant and kidney function monitoring in outpatient kidney transplant recipients. Br. J. Clin. Pharmacol. 2022, 88, 4854–4869. [Google Scholar] [CrossRef]
| No | Drug | Extraction Solvent | Extraction Conditions | Additional Sample Preparation | Analytical Instrument | Validation Result | Ref. | |
|---|---|---|---|---|---|---|---|---|
| Available Parameter | Missing Parameter | |||||||
| 1 | Fosfomycin | Methanol + IS | On a lateral shaker for 30 min at 1200 rpm | - | LC-MS/MS | Calibration range of 5–2000 µg/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stability was only assessed for 500 µg/mL concentrations and was stable at RT for 10 days in an autosampler at 4 °C for 48 h | Stability for QC concentrations and dilution integrity was not assessed | [39] |
| 2 | Emixustat | Methanol containing 1% ammonium hydroxide + IS | Sonication for 15 min and vortex for 15 min | Evaporation at 40 °C with nitrogen, reconstitution in methanol–water (3:7, v/v) containing 0.1% formic acid | LC-MS/MS | Calibration range of 0.05–10 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 1 week; −4 °C for 1 months; −20 °C for 1 months | - | [46] |
| 3 | Atorvastatin | Methanol–acetonitrile (1:1, v/v) and 1% formic acid + IS | Vortex for 1 h | Centrifugation at 3000 rpm for 15 min | LC-MS/MS | Calibration range of 1–2000 ng/mL Linearity, accuracy and precision, and recovery were assessed and met the acceptance criteria | Sensitivity, selectivity, matrix effect, dilution integrity, carry-over, and stability were not assessed | [13] |
| 4 | Tamoxifen | Methanol–acetonitrile (1:1, v/v) and 1% formic acid + IS | Vortex for 1 h | Centrifugation at 3000 rpm for 15 min | LC-MS/MS | Calibration range of 1–2000 ng/mL Linearity, accuracy and precision, and recovery were assessed and met the acceptance criteria | Sensitivity, selectivity, matrix effect, dilution integrity, carry-over, and stability were not assessed | [13] |
| 5 | Amiodarone | Methanol–acetonitrile (1:1, v/v) and 1% formic acid + IS | Vortex for 1 h | Centrifugation at 3000 rpm for 15 min | LC-MS/MS | Calibration range of 1–2000 ng/mL Linearity, accuracy and precision, and recovery were assessed and met the acceptance criteria | Sensitivity, selectivity, matrix effect, dilution integrity, carry-over, and stability were not assessed | [13] |
| 6 | Piperacillin | Methanol | Sonication for 10 min | Rehydration using water and incubation for 10 min at 37 °C in the thermos block heater | LC-MS/MS | Calibration range of 3.125–200 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT and 4 °C for 72 h; −20 °C for 1 month | Dilution integrity was not assessed | [14] |
| 7 | Tazobactam | Methanol | Sonication for 10 min | Rehydration using water and incubation for 10 min at 37 °C in the thermos block heater | LC-MS/MS | Calibration range of 0.625–40 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT and 4 °C for 72 h; −20 °C for 1 month | Dilution integrity was not assessed | [14] |
| 8 | Meropenem | Methanol | Sonication for 10 min | Rehydration using water and incubation for 10 min at 37 °C in the thermos block heater | LC-MS/MS | Calibration range of 0.625–40 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT and 4 °C for 72 h; −20 °C for 1 month | Dilution integrity was not assessed | [14] |
| 9 | Ceftazidime | Methanol | Sonication for 10 min | Rehydration using water and incubation for 10 min at 37 °C in the thermos block heater | LC-MS/MS | Calibration range of 3.125–200 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at 4 °C for 72 h; −20 °C for 1 month | Dilution integrity was not assessed | [14] |
| 10 | Paracetamol | Methanol–water–formic acid (80:20:0.01, v/v/v) + IS | Shaking for 15 min in a thermomixer comfort | Centrifugation at RT for 10 min at 10,000× g, supernatant dilution with water with 0.01% formic acid | LC-MS/MS | Calibration range of 4.0–32.8 µg/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at 50 °C for 1 week; −80 °C, −20 °C, and 4 °C for 9 months; RT for at least 8 months | - | [62] |
| 11 | Albendazole | Acetonitrile-methanol (1:1, v/v) with 0.1% formic acid + IS | Sonication in an ultrasonic bath for 1 h and agitation for 1 h in RT at 1200 rpm | Centrifugation for 10 min at 3300× g, evaporation of supernatant, and reconstitution in methanol | LC-MS/MS | Calibration range of 1–200 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, and matrix effect were assessed and met the acceptance criteria Stable at RT for 2 months; in autosampler at 4 °C for 72 h; −80 °C for 2 months | Dilution integrity and carry-over were not assessed | [51] |
| 12 | Cefepime | Acetonitrile + IS | Sonication for 15 min, vortex at 700 rpm for 10 min, and centrifugation for 30 min at 3220× g at 4 °C | Rehydration using water, vortex for 2 min at 1000 rpm, and incubation for 10 min at 37 °C | LC-MS/MS | Calibration range of 0.100–100 µg/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at 4 °C for 1 week; −20 °C for 1 month (39 days); −78 °C for 3 months (91 days); in autosampler at 10 °C for 20 h | - | [64] |
| 13 | Ethosuximide | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 3.48–234 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 14 | Felbamate | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 9.55–428 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 15 | Phenobarbital | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.89–60 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 16 | Phenytoin | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.58–39 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 17 | Primidone | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.76–51 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 18 | Topiramate | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.67–45 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 19 | Zonisamide | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 1.07–72 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 20 | Mycophenolic acid | Water and methanol + IS | Sonication for 15 min | Centrifugation for 5 min at 14,500 rpm, evaporation of supernatant, and reconstitution using ammonium formate and 0.1% formic acid in water-acetonitrile (6:4, v/v) | LC-MS/MS | Calibration range of 75–7500 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable in autosampler at 6 °C for 72 h; 20 °C, 4 °C, and RT for 15 days; −20 °C for 8 months | Dilution integrity was not assessed | [61] |
| 21 | Tamoxifen | Methanol + IS | Vortex for 1 min, sonication for 25 min | Dry in a water bath at 55 °C under nitrogen steam, reconstitution using 0.1% formic acid and 0.1% formic acid in acetonitrile, vortex for 20 s | LC-MS/MS | Calibration range of 2.5–200 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 24 h; −20 °C for 1 month; in autosampler for 24 h | - | [63] |
| No | Drug | Extraction Solvent | Extraction Conditions | Additional Sample Preparation | Analytical Instrument | Validation Result | Ref. | |
|---|---|---|---|---|---|---|---|---|
| Available Parameter | Missing Parameter | |||||||
| 1 | Paraxanthine | Methanol–water (8:2, v/v) and 0.01% formic acid + IS | In a thermomixer at 1000 rpm and 22 °C | Centrifugation at RT (10 min, 10,000× g), supernatant diluted with 0.01% formic acid | LC-MS/MS | Calibration range of 0.025–5 µg/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT for 82 days; 60 °C for 4 days; −20 °C for 30 days; in autosampler at 4 °C for 4 days | Dilution integrity was not assessed | [28] |
| 2 | Caffeine | Methanol–water (8:2, v/v) and 0.01% formic acid + IS | In a thermomixer at 1000 rpm and 22 °C | Centrifugation at RT (10 min, 10,000× g), supernatant diluted with 0.01% formic acid | LC-MS/MS | Calibration range of 0.05–10 µg/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT for 82 days; 60 °C for 4 days; −20 °C for 30 days; in autosampler at 4 °C for 4 days | Dilution integrity was not assessed | [28] |
| 3 | Miltefosine | Methanol | Mixing for 15 min at 1250 rpm and vortex for 30 s | A 20-fold dilution of highly concentrated samples with methanol and the addition of IS | LC-MS/MS | Calibration range of 10–5000 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 1 month; 37 °C for 1 month; 2–8 °C for 5 days | - | [31] |
| 4 | Itraconazole | Acetonitrile-methanol (6:4, v/v) + IS | Incubation for 5 min, agitation for 5 min with a vortex mixer | Phospholipid removal with Ostroplate, evaporation under vacuum at 50 °C for 1 h, reconstitution in methanol–water (1:1, v/v) | LC-MS/MS | Calibration range of 10–1000 ng/mL Linearity, accuracy and precision, selectivity, recovery, and matrix effect were assessed and met the acceptance criteria Stable at RT for 24 h; −80 °C for 2 weeks; in autosampler at 6 °C for 24 h | Sensitivity, dilution integrity, and carry-over were not assessed | [48] |
| 5 | Cathinone analogs | Methanol | Ultrasound agitation for 15 min and vortex for 1 min | Evaporation under vacuum and reconstitution in acetonitrile-water (1:1, v/v) containing 0.1% formic acid | LC-MS/MS | Calibration range of 10–500 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, and matrix effect were assessed and met the acceptance criteria Stable at RT for 7 days only for one concentration of 250 ng/mL | Dilution integrity, carry-over, and stability for QC concentrations were not assessed | [45] |
| 6 | Metoprolol | Methanol–acetonitrile (1:1, v/v) and 1% formic acid + IS | Vortex for 1 h | Centrifugation at 3000 rpm for 15 min | LC-MS/MS | Calibration range of 1–2000 ng/mL Linearity, accuracy and precision, and recovery were assessed and met the acceptance criteria | Sensitivity, selectivity, matrix effect, dilution integrity, carry-over, and stability were not assessed | [13] |
| 7 | Midazolam | Methanol–acetonitrile (1:1, v/v) and 1% formic acid + IS | Vortex for 1 h | Centrifugation at 3000 rpm for 15 min | LC-MS/MS | Calibration range of 1–2000 ng/mL Linearity, accuracy and precision, and recovery were assessed and met the acceptance criteria | Sensitivity, selectivity, matrix effect, dilution integrity, carry-over, and stability were not assessed | [13] |
| 8 | Salbutamol | Methanol + IS | Sonication for 15 min | Evaporation for 60 min, resuspended in N, O-Bis(trimethylsilyl)trifluoroacetamide (BSTFA) with 1% trimethylchlorosilane (TMCS) by vortexing, and derivatization at 60 °C for 30 min | GC-MS | Calibration range of 3–100 ng/mL Linearity, accuracy and precision, and recovery were assessed and met the acceptance criteria Stable at −20 °C, RT, and 30 °C for 145 days; 4 °C for 75 days | Sensitivity, selectivity, matrix effect, dilution integrity, and carry-over were not assessed | [78] |
| 9 | Hydroxychloroquine | Water + IS | Vortex for 30 min | Protein precipitation with 70% perchloric acid, centrifugation for 5 min at 14,000 rpm | LC-MS/MS | Calibration range of 10–2000 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 10 days; 22 °C and 50 °C for 24 h | - | [38] |
| 10 | Linezolid | Methanol | Sonication for 10 min | Rehydration using water and incubation for 10 min at 37 °C in the thermos block heater | LC-MS/MS | Calibration range of 0.625–40 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT and 4 °C for 72 h; −20 °C for 1 month | Dilution integrity was not assessed | [14] |
| 11 | Praziquantel | Acetonitrile-water (4:1, v/v) + IS | Thermos-mixing for 5 min at 1400 rpm at RT and ultrasonication for 40 min | - | LC-MS/MS | Calibration range of 0.2–50 µg/mL Linearity, accuracy and precision, sensitivity, recovery, and matrix effect were assessed and met the acceptance criteria Stable at RT for 4 months; 4 °C for 72 h; −80 °C for 2 months | Carry-over, selectivity, and dilution integrity were not assessed | [37] |
| 12 | Radiprodil | Methanol–ethyl acetate (1:1, v/v) + IS | Sonication for 15 min, shaking for 1 h at 1200 rpm | Dry using nitrogen and reconstitution | LC-ESI-MS/MS | Calibration range of 1–1000 ng/mL Linearity, accuracy, and precision were assessed and met the acceptance criteria | Sensitivity, selectivity, recovery, matrix effect, dilution integrity, carry-over, and stability were not assessed | [81] |
| 13 | Voriconazole | Acetonitrile-methanol (1:1, v/v) + IS | Sonication for 15 min, vortex for 30 min at 350 rpm | Centrifugation for 30 min at 4000 rpm | LC-MS/MS | Calibration range of 10–10,000 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 19 h; −80 °C for 3 days; 4 °C, −20 °C, −80 °C for 1 month; in autosampler for 24 h | - | [80] |
| 14 | Voriconazole N-oxide | Acetonitrile-methanol (1:1, v/v) + IS | Sonication for 15 min, vortex for 30 min at 350 rpm | Centrifugation for 30 min at 4000 rpm | LC-MS/MS | Calibration range of 10–10,000 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 19 h; −80 °C for 3 days; in autosampler for 24 h | - | [80] |
| 15 | Midazolam | Methanol + IS | On a lateral shaker for 1 h | - | LC-MS/MS | Calibration range of 5–5000 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and dilution integrity were assessed and met the acceptance criteria Stable at RT for 131 days; 4 °C for 192 h; 37 °C for 4 h; 40 °C for 43 days; −20 °C for 43 days | Carry-over was not assessed | [79] |
| 16 | Lamotrigine | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.67–45 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 17 | Rufinamide | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.94–63 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 18 | Mitotane | Methanol–aqueous zinc sulfate heptahydrate solution 2% (4:1, v/v) | Ultrasonic bath for 15 min, shaking for 1 h at 1400 rpm | Centrifugation at 12,000× g for 5 min at 4 °C | LC-UV | Calibration range of 1–50 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, and carry-over were assessed and met the acceptance criteria Stable at RT for 1 week; 2–8 °C for 1 week; in autosampler for 24 h | Matrix effect and dilution integrity were not assessed | [82] |
| No | Drug | Extraction Solvent | Extraction Conditions | Additional Sample Preparation | Analytical Instrument | Validation Result | Ref. | |
|---|---|---|---|---|---|---|---|---|
| Available Parameter | Missing Parameter | |||||||
| 1 | Tacrolimus | Methanol–zinc sulfate 0.10 mol/L (2:1) + IS | Shaking on the orbital shaker at 1400 rpm for 6 min | Centrifugation at 2000× g for 10 min at 4 °C | LC-MS/MS | Calibration range of 0.7–6 µg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at RT for 2 months | - | [97] |
| 2 | Carbamazepine | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.45–30 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 3 | Lacosamide | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.45–30 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 4 | Oxcarbazepine | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.18–12 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 5 | Perampanel | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.03–1.86 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 6 | Levetiracetam | Acetonitrile + IS | Vortex mixing for 30 min at 600 rpm | Centrifugation for 10 min at 17,000× g, reconstitution of supernatant using water and 0.1% formic acid, and vortex for 30 s | LC-MS/MS | Calibration range of 0.94–63 mg/L Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, dilution integrity, and carry-over were assessed and met the acceptance criteria Stable at −20 °C, 4 °C, 37 °C, 10 °C (autosampler) for 10 days; −20 °C for 4 months | - | [16] |
| 7 | Tacrolimus | Water and methanol + IS | Sonication for 15 min | Centrifugation for 5 min at 14,500 rpm, evaporation of supernatant, and reconstitution using ammonium formate and 0.1% formic acid in water-acetonitrile (6:4, v/v) | LC-MS/MS | Calibration range of 0.5–50 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable in autosampler at 6 °C for 72 h; 20 °C, 4 °C, and RT for 15 days; −20 °C for 8 months | Dilution integrity was not assessed | [61] |
| 8 | Sirolimus | Water and methanol + IS | Sonication for 15 min | Centrifugation for 5 min at 14,500 rpm, evaporation of supernatant, and reconstitution using ammonium formate and 0.1% formic acid in water-acetonitrile (6:4, v/v) | LC-MS/MS | Calibration range of 0.5–50 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable in autosampler at 6 °C for 72 h; 20 °C, 4 °C, and RT for 15 days; −20 °C for 8 months | Dilution integrity was not assessed | [61] |
| 9 | Everolimus | Water and methanol + IS | Sonication for 15 min | Centrifugation for 5 min at 14,500 rpm, evaporation of supernatant, and reconstitution using ⁰ammonium formate and 0.1% formic acid in water-acetonitrile (6:4, v/v) | LC-MS/MS | Calibration range of 0.5–50 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable in autosampler at 6 °C for 72 h; 20 °C, 4 °C, and RT for 15 days; −20 °C for 8 months | Dilution integrity was not assessed | [61] |
| 10 | Cyclosporin A | Water and methanol + IS | Sonication for 15 min | Centrifugation for 5 min at 14,500 rpm, evaporation of supernatant, and reconstitution using ammonium formate and 0.1% formic acid in water-acetonitrile (6:4, v/v) | LC-MS/MS | Calibration range of 20–2000 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable in autosampler at 6 °C for 72 h; 20 °C, 4 °C, and RT for 15 days; −20 °C for 8 months | Dilution integrity was not assessed | [61] |
| 11 | Tacrolimus | Acetonitrile-zinc sulfate 0.05 M in water (1:1, v/v) + IS | Vortex for 1 min | Addition of ammonium sulfate 40% for salting out, vortex for 1 min, centrifugation at 16,260× g for 5 min at 8 °C | LC-MS/MS | Calibration range of 2.25–42.9 ng/mL Linearity, accuracy and precision, sensitivity, selectivity, recovery, matrix effect, and carry-over were assessed and met the acceptance criteria Stable at RT for 7 days; 4 °C and 60 °C for 48 h; −80 °C for 1 month | Dilution integrity was not assessed | [53] |
| No | Drug | Sample (n) | Patient (n) | Measures of Clinical Validation | Ref. | ||
|---|---|---|---|---|---|---|---|
| Passing–Bablock Analysis (Slope [95% CI]) | Bland–Altman Analysis | Predictive Performance | |||||
| 1 | Albendazole | 100 | 10 | NA | Good Agreement | NA | [51] |
| 2 | Tacrolimus | 88 | 72 | Linear (0.88 [0.81; 0.97]) a (1.00 [0.98; 1.02]) b | Good agreement (after correction) | Met the acceptance criteria | [108] |
| 679 | 27 | Linear (1.01 [NA]) | Good agreement | NA | [97] | ||
| 53 | 53 | Linear (1.26 [1.16; 1.4]) a (0.99 [0.91; 1.07]) b | Good agreement (after correction) | Met the acceptance criteria | [61] | ||
| 97 | 25 | Linear (1.05 [0.98; 1.14]) | Good agreement | NA | [109] | ||
| 3 | Radiprodil | 150 | 10 | NA | Good agreement | NA | [81] |
| 4 | Mycophenolic acid | 20 | 20 | Linear (0.98 [0.94; 1.05]) | Good agreement | Met the acceptance criteria | [61] |
| 64 | 25 | Linear (0.72 [0.66; 0.77]) a (1.07 [0.97; 1.13]) b | Good agreement (after correction) | NA | [109] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nugraha, R.V.; Yunivita, V.; Santoso, P.; Hasanah, A.N.; Aarnoutse, R.E.; Ruslami, R. Analytical and Clinical Validation of Assays for Volumetric Absorptive Microsampling (VAMS) of Drugs in Different Blood Matrices: A Literature Review. Molecules 2023, 28, 6046. https://doi.org/10.3390/molecules28166046
Nugraha RV, Yunivita V, Santoso P, Hasanah AN, Aarnoutse RE, Ruslami R. Analytical and Clinical Validation of Assays for Volumetric Absorptive Microsampling (VAMS) of Drugs in Different Blood Matrices: A Literature Review. Molecules. 2023; 28(16):6046. https://doi.org/10.3390/molecules28166046
Chicago/Turabian StyleNugraha, Rhea Veda, Vycke Yunivita, Prayudi Santoso, Aliya Nur Hasanah, Rob E. Aarnoutse, and Rovina Ruslami. 2023. "Analytical and Clinical Validation of Assays for Volumetric Absorptive Microsampling (VAMS) of Drugs in Different Blood Matrices: A Literature Review" Molecules 28, no. 16: 6046. https://doi.org/10.3390/molecules28166046
APA StyleNugraha, R. V., Yunivita, V., Santoso, P., Hasanah, A. N., Aarnoutse, R. E., & Ruslami, R. (2023). Analytical and Clinical Validation of Assays for Volumetric Absorptive Microsampling (VAMS) of Drugs in Different Blood Matrices: A Literature Review. Molecules, 28(16), 6046. https://doi.org/10.3390/molecules28166046








