Hypoxia Tolerant Species: The Wisdom of Nature Translated into Targets for Stroke Therapy
Abstract
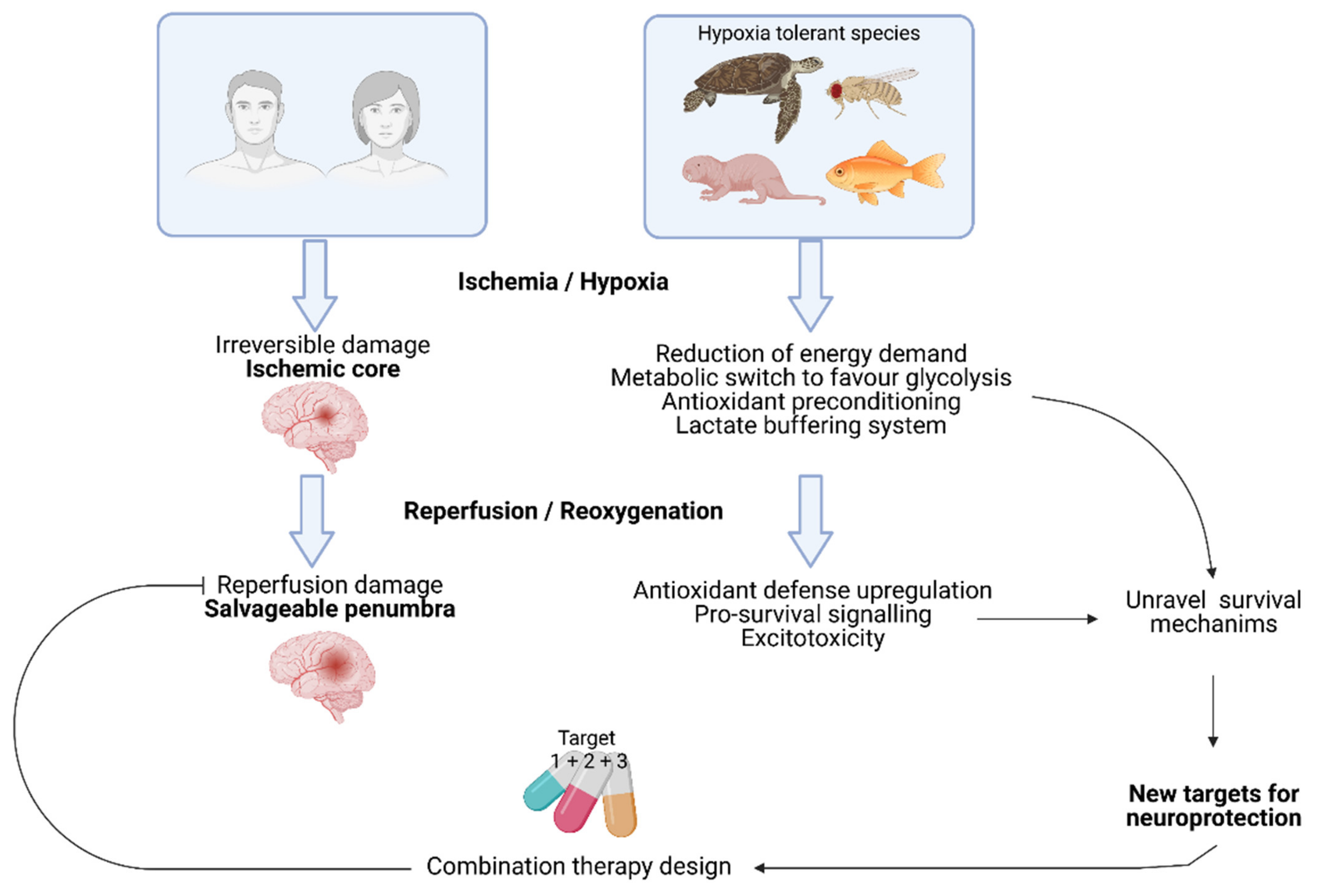
1. Introduction
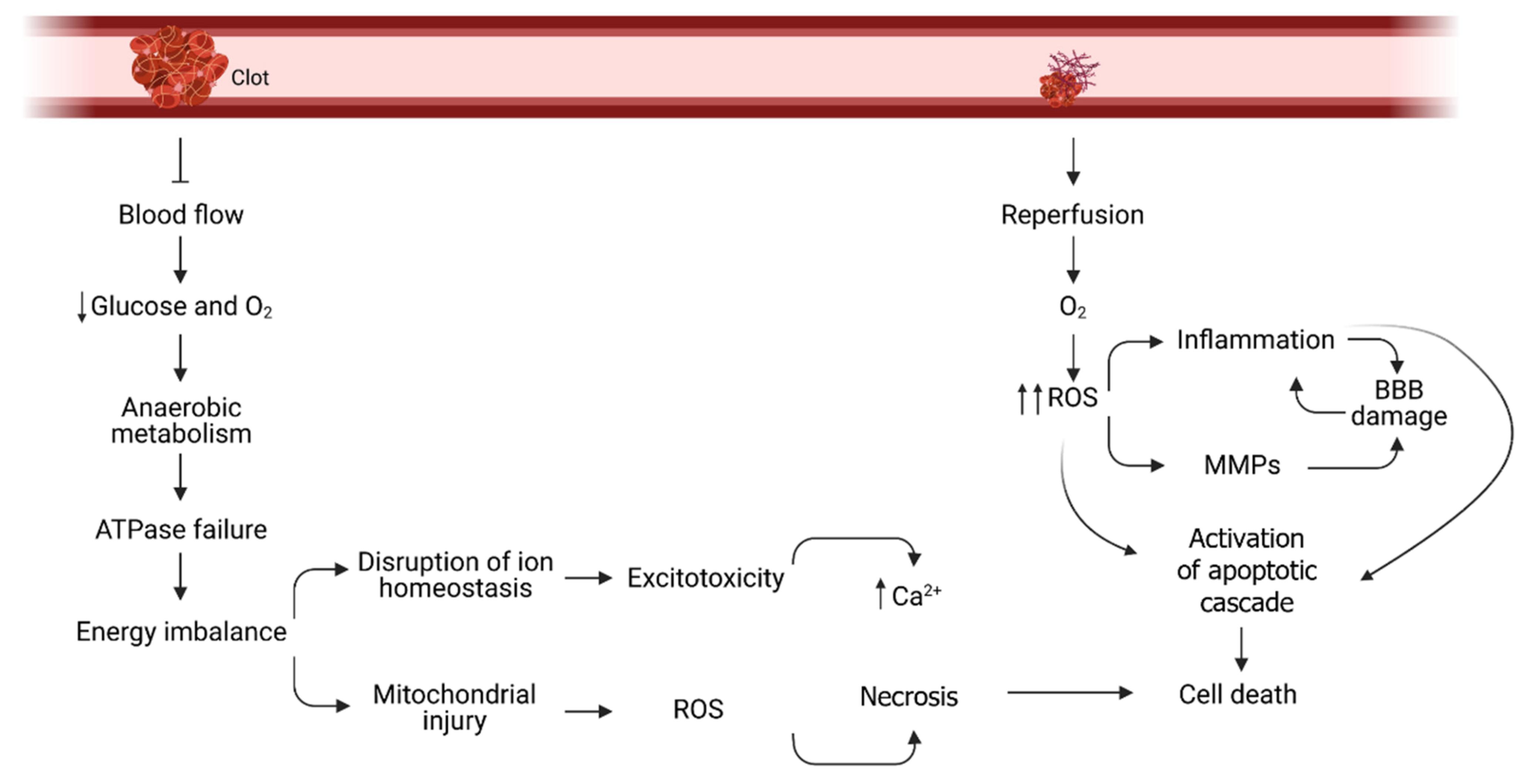
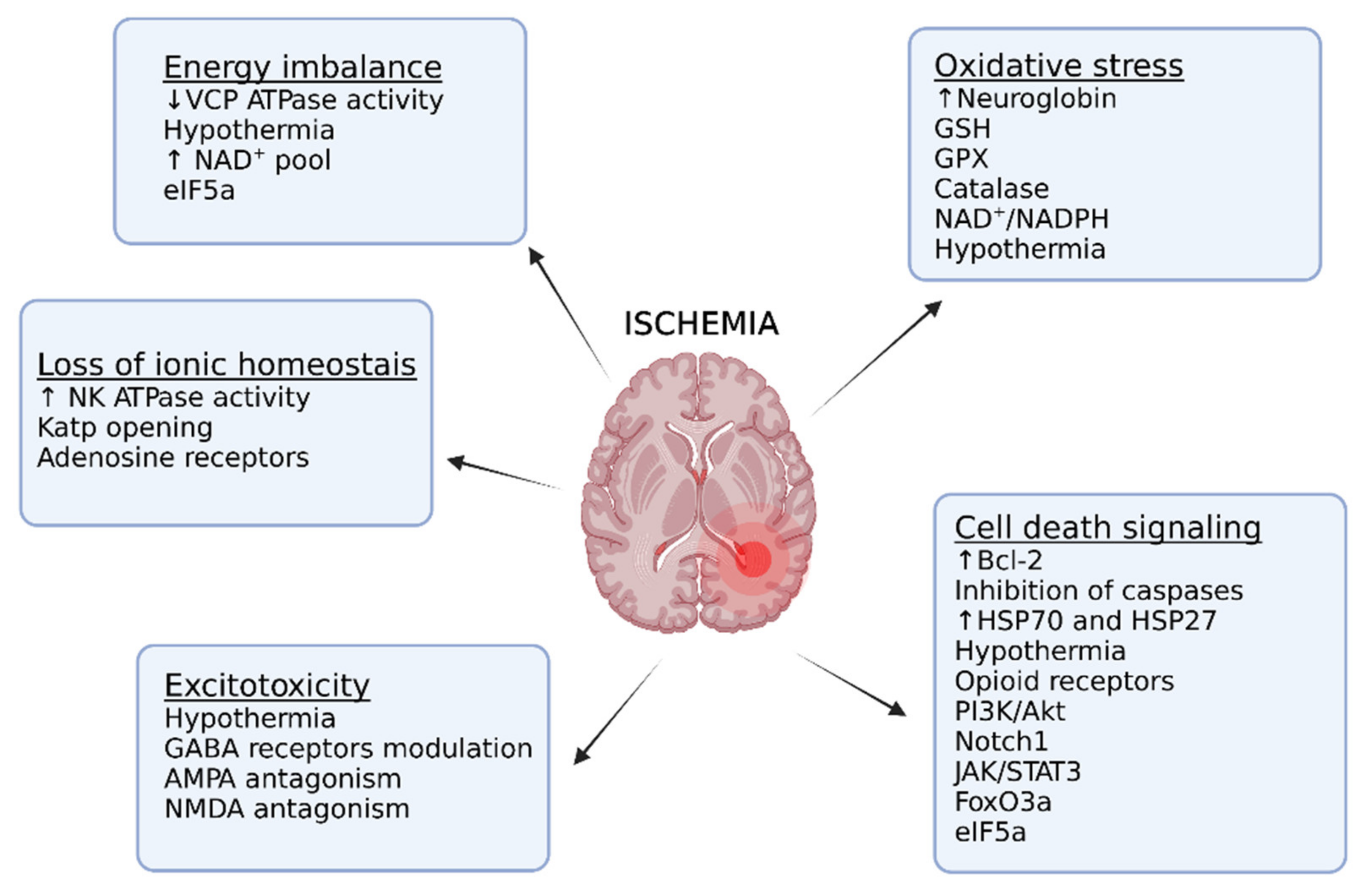
2. Stroke Pathophysiology: Molecular Consequences of Ischemia
3. The Failure of Treatment Translation
4. Tolerant Species: Mechanisms for Adaptation
4.1. Regulation of Cellular Energetics
4.2. Metabolic Acidosis Buffering Systems
4.3. Strategies to Control Excitotoxicity
4.4. Enhancement of the Antioxidant Defense
5. Preclinical Proof of Concept
5.1. Eukaryotic Initiation Factor 5A (eIF5A)
5.2. Forkhead Box O 3 (FoxO3)
5.3. Other Mechanisms Involved in Hypoxia Tolerance
6. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Doyle, K.P.; Simon, R.P.; Stenzel-Poore, M.P. Mechanisms of ischemic brain damage. Neuropharmacology 2008, 55, 310–318. [Google Scholar] [CrossRef]
- Eivind Berge, W.W.; Heinrich, A.; De Marchis, G.M.; Fonseca, A.C.; Padiglioni, C.; de la Ossa, N.P.; Strbian, D.; Tsivgoulis, G.; Turc, G. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur. Stroke J. 2021, 6, 1–62. [Google Scholar] [CrossRef]
- Urra, X.; Abilleira, S.; Dorado, L.; Ribo, M.; Cardona, P.; Millan, M.; Chamorro, A.; Molina, C.; Cobo, E.; Davalos, A.; et al. Mechanical Thrombectomy in and Outside the REVASCAT Trial: Insights From a Concurrent Population-Based Stroke Registry. Stroke 2015, 46, 3437–3442. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, G.E.; Lutz, P.L. Anoxia tolerant brains. J. Cereb. Blood Flow Metab. 2004, 24, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Larson, J.; Drew, K.L.; Folkow, L.P.; Milton, S.L.; Park, T.J. No oxygen? No problem! Intrinsic brain tolerance to hypoxia in vertebrates. J. Exp. Biol. 2014, 217, 1024–1039. [Google Scholar] [CrossRef]
- Wetterling, F.; Chatzikonstantinou, E.; Tritschler, L.; Meairs, S.; Fatar, M.; Schad, L.R.; Ansar, S. Investigating potentially salvageable penumbra tissue in an in vivo model of transient ischemic stroke using sodium, diffusion, and perfusion magnetic resonance imaging. BMC Neurosci. 2016, 17, 82. [Google Scholar] [CrossRef]
- Shi, L.; Rocha, M.; Leak, R.K.; Zhao, J.; Bhatia, T.N.; Mu, H.; Wei, Z.; Yu, F.; Weiner, S.L.; Ma, F.; et al. A new era for stroke therapy: Integrating neurovascular protection with optimal reperfusion. J. Cereb. Blood Flow Metab. 2018, 38, 2073–2091. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; De Silva, D.A.; Macleod, M.R.; Coutts, S.B.; Schwamm, L.H.; Davis, S.M.; Donnan, G.A. Ischaemic stroke. Nat. Rev. Dis. Primers 2019, 5, 70. [Google Scholar] [CrossRef] [PubMed]
- Belov Kirdajova, D.; Kriska, J.; Tureckova, J.; Anderova, M. Ischemia-Triggered Glutamate Excitotoxicity From the Perspective of Glial Cells. Front Cell Neurosci 2020, 14, 51. [Google Scholar] [CrossRef]
- Uzdensky, A.B. Apoptosis regulation in the penumbra after ischemic stroke: Expression of pro- and antiapoptotic proteins. Apoptosis 2019, 24, 687–702. [Google Scholar] [CrossRef]
- Li, W.; Yang, S. Targeting oxidative stress for the treatment of ischemic stroke: Upstream and downstream therapeutic strategies. Brain Circ 2016, 2, 153–163. [Google Scholar] [CrossRef]
- Savitz, S.I.; Baron, J.C.; Yenari, M.A.; Sanossian, N.; Fisher, M. Reconsidering Neuroprotection in the Reperfusion Era. Stroke 2017, 48, 3413–3419. [Google Scholar] [CrossRef] [PubMed]
- O'Collins, V.E.; Macleod, M.R.; Donnan, G.A.; Horky, L.L.; van der Worp, B.H.; Howells, D.W. 1,026 experimental treatments in acute stroke. Ann. Neurol. 2006, 59, 467–477. [Google Scholar] [CrossRef]
- Lapchak, P.A.; Zhang, J.H.; Noble-Haeusslein, L.J. RIGOR guidelines: Escalating STAIR and STEPS for effective translational research. Transl. Stroke Res. 2013, 4, 279–285. [Google Scholar] [CrossRef]
- Narayan, S.K.; Grace Cherian, S.; Babu Phaniti, P.; Babu Chidambaram, S.; Rachel Vasanthi, A.H.; Arumugam, M. Preclinical animal studies in ischemic stroke: Challenges and some solutions. Anim. Model Exp. Med. 2021, 4, 104–115. [Google Scholar] [CrossRef]
- Esposito, E.; Li, W.; E, T.M.; Park, J.H.; Sencan, I.; Guo, S.; Shi, J.; Lan, J.; Lee, J.; Hayakawa, K.; et al. Potential circadian effects on translational failure for neuroprotection. Nature 2020, 582, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.F. ESCAPE-NA1 Trial Brings Hope of Neuroprotective Drugs for Acute Ischemic Stroke: Highlights of the Phase 3 Clinical Trial on Nerinetide. Neurosci. Bull. 2021, 37, 579–581. [Google Scholar] [CrossRef]
- Lee, J.H.; Zhang, J.; Yu, S.P. Neuroprotective mechanisms and translational potential of therapeutic hypothermia in the treatment of ischemic stroke. Neural. Regen. Res. 2017, 12, 341–350. [Google Scholar] [CrossRef]
- Faggi, L.; Pignataro, G.; Parrella, E.; Porrini, V.; Vinciguerra, A.; Cepparulo, P.; Cuomo, O.; Lanzillotta, A.; Mota, M.; Benarese, M.; et al. Synergistic Association of Valproate and Resveratrol Reduces Brain Injury in Ischemic Stroke. Int. J. Mol. Sci. 2018, 19, 172. [Google Scholar] [CrossRef] [PubMed]
- Casas, A.I.; Hassan, A.A.; Larsen, S.J.; Gomez-Rangel, V.; Elbatreek, M.; Kleikers, P.W.M.; Guney, E.; Egea, J.; Lopez, M.G.; Baumbach, J.; et al. From single drug targets to synergistic network pharmacology in ischemic stroke. Proc. Natl. Acad. Sci. USA 2019, 116, 7129–7136. [Google Scholar] [CrossRef]
- Wu, M.H.; Huang, C.C.; Chio, C.C.; Tsai, K.J.; Chang, C.P.; Lin, N.K.; Lin, M.T. Inhibition of Peripheral TNF-alpha and Downregulation of Microglial Activation by Alpha-Lipoic Acid and Etanercept Protect Rat Brain Against Ischemic Stroke. Mol. Neurobiol. 2016, 53, 4961–4971. [Google Scholar] [CrossRef] [PubMed]
- Sukhum, K.V.; Freiler, M.K.; Wang, R.; Carlson, B.A. The costs of a big brain: Extreme encephalization results in higher energetic demand and reduced hypoxia tolerance in weakly electric African fishes. Proc. Biol. Sci. 2016, 283, 20162157. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.N.; Guo, W.T.; Liu, J.; Chang, J.; Ma, H.; Zhang, P.; Zhang, F.L.; Han, K.; Hu, H.H.; Jin, H.; et al. Changes in cerebral autoregulation and blood biomarkers after remote ischemic preconditioning. Neurology 2019, 93, e8–e19. [Google Scholar] [CrossRef] [PubMed]
- England, T.J.; Hedstrom, A.; O'Sullivan, S.; Donnelly, R.; Barrett, D.A.; Sarmad, S.; Sprigg, N.; Bath, P.M. RECAST (Remote Ischemic Conditioning After Stroke Trial): A Pilot Randomized Placebo Controlled Phase II Trial in Acute Ischemic Stroke. Stroke 2017, 48, 1412–1415. [Google Scholar] [CrossRef]
- Landman, T.R.J.; Schoon, Y.; Warle, M.C.; de Leeuw, F.E.; Thijssen, D.H.J. Remote Ischemic Conditioning as an Additional Treatment for Acute Ischemic Stroke. Stroke 2019, 50, 1934–1939. [Google Scholar] [CrossRef]
- Hess, D.C.; Blauenfeldt, R.A.; Andersen, G.; Hougaard, K.D.; Hoda, M.N.; Ding, Y.; Ji, X. Remote ischaemic conditioning-a new paradigm of self-protection in the brain. Nat. Rev. Neurol. 2015, 11, 698–710. [Google Scholar] [CrossRef]
- Ravn, M.V.; Campbell, J.B.; Gerber, L.; Harrison, J.F.; Overgaard, J. Effects of anoxia on ATP, water, ion and pH balance in an insect (Locusta migratoria). J. Exp. Biol. 2019, 222, jeb190850. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Liu, G.; Hou, L.; Gui, W.; Chen, B.; Kang, L. Genetic variation in PTPN1 contributes to metabolic adaptation to high-altitude hypoxia in Tibetan migratory locusts. Nat. Commun. 2018, 9, 4991. [Google Scholar] [CrossRef]
- Zhao, D.; Zhang, Z.; Cease, A.; Harrison, J.; Kang, L. Efficient utilization of aerobic metabolism helps Tibetan locusts conquer hypoxia. BMC Genom. 2013, 14, 631. [Google Scholar] [CrossRef]
- Campbell, J.B.; Andersen, M.K.; Overgaard, J.; Harrison, J.F. Paralytic hypo-energetic state facilitates anoxia tolerance despite ionic imbalance in adult Drosophila melanogaster. J. Exp. Biol. 2018, 221 (Pt 12). [Google Scholar] [CrossRef]
- Campbell, J.B.; Werkhoven, S.; Harrison, J.F. Metabolomics of anoxia tolerance in Drosophila melanogaster: Evidence against substrate limitation and for roles of protective metabolites and paralytic hypometabolism. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2019, 317, R442–R450. [Google Scholar] [CrossRef]
- Azad, P.; Zhou, D.; Russo, E.; Haddad, G.G. Distinct mechanisms underlying tolerance to intermittent and constant hypoxia in Drosophila melanogaster. PLoS ONE 2009, 4, e5371. [Google Scholar] [CrossRef]
- Hawkins, L.J.; Wang, M.; Zhang, B.; Xiao, Q.; Wang, H.; Storey, K.B. Glucose and urea metabolic enzymes are differentially phosphorylated during freezing, anoxia, and dehydration exposures in a freeze tolerant frog. Comp Biochem Physiol Part D Genom. Proteom. 2019, 30, 1–13. [Google Scholar] [CrossRef]
- Shekhovtsov, S.V.; Bulakhova, N.A.; Tsentalovich, Y.P.; Zelentsova, E.A.; Yanshole, L.V.; Meshcheryakova, E.N.; Berman, D.I. Metabolic response of the Siberian wood frog Rana amurensis to extreme hypoxia. Sci. Rep. 2020, 10, 14604. [Google Scholar] [CrossRef]
- Stenslokken, K.O.; Ellefsen, S.; Vasieva, O.; Fang, Y.; Farrell, A.P.; Olohan, L.; Vaage, J.; Nilsson, G.E.; Cossins, A.R. Life without oxygen: Gene regulatory responses of the crucian carp (Carassius carassius) heart subjected to chronic anoxia. PLoS ONE 2014, 9, e109978. [Google Scholar] [CrossRef]
- Sandvik, G.K.; Tomter, A.B.; Bergan, J.; Zoppellaro, G.; Barra, A.L.; Rohr, A.K.; Kolberg, M.; Ellefsen, S.; Andersson, K.K.; Nilsson, G.E. Studies of ribonucleotide reductase in crucian carp-an oxygen dependent enzyme in an anoxia tolerant vertebrate. PLoS ONE 2012, 7, e42784. [Google Scholar] [CrossRef]
- Vornanen, M.; Haverinen, J. Glycogen dynamics of crucian carp (Carassius carassius) in prolonged anoxia. J Comp Physiol B 2016, 186, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Lutz, P.L.; Milton, S.L. Negotiating brain anoxia survival in the turtle. J. Exp. Biol. 2004, 207, 3141–3147. [Google Scholar] [CrossRef]
- Bundgaard, A.; James, A.M.; Gruszczyk, A.V.; Martin, J.; Murphy, M.P.; Fago, A. Metabolic adaptations during extreme anoxia in the turtle heart and their implications for ischemia-reperfusion injury. Sci. Rep. 2019, 9, 2850. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.W.; Cash, P.; Hogg, D.W.; Buck, L.T. Proteomic changes in the brain of the western painted turtle (Chrysemys picta bellii) during exposure to anoxia. Proteomics 2015, 15, 1587–1597. [Google Scholar] [CrossRef] [PubMed]
- Hylland, P.; Nilsson, G.E.; Lutz, P.L. Time course of anoxia-induced increase in cerebral blood flow rate in turtles: Evidence for a role of adenosine. J. Cereb. Blood Flow Metab. 1994, 14, 877–881. [Google Scholar] [CrossRef]
- Bansal, S.; Biggar, K.K.; Krivoruchko, A.; Storey, K.B. Response of the JAK-STAT signaling pathway to oxygen deprivation in the red eared slider turtle, Trachemys scripta elegans. Gene 2016, 593, 34–40. [Google Scholar] [CrossRef]
- Dave, K.R.; Anthony Defazio, R.; Raval, A.P.; Dashkin, O.; Saul, I.; Iceman, K.E.; Perez-Pinzon, M.A.; Drew, K.L. Protein kinase C epsilon activation delays neuronal depolarization during cardiac arrest in the euthermic arctic ground squirrel. J. Neurochem. 2009, 110, 1170–1179. [Google Scholar] [CrossRef]
- Ma, Y.L.; Zhu, X.; Rivera, P.M.; Toien, O.; Barnes, B.M.; LaManna, J.C.; Smith, M.A.; Drew, K.L. Absence of cellular stress in brain after hypoxia induced by arousal from hibernation in Arctic ground squirrels. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005, 289, R1297-306. [Google Scholar] [CrossRef]
- MacDonald, J.A.; Storey, K.B. Regulation of ground squirrel Na+K+-ATPase activity by reversible phosphorylation during hibernation. Biochem. Biophys. Res. Commun. 1999, 254, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Pamenter, M.E.; Dzal, Y.A.; Thompson, W.A.; Milsom, W.K. Do naked mole rats accumulate a metabolic acidosis or an oxygen debt in severe hypoxia? J. Exp. Biol. 2019, 222 (Pt 3). [Google Scholar] [CrossRef] [PubMed]
- Park, T.J.; Reznick, J.; Peterson, B.L.; Blass, G.; Omerbasic, D.; Bennett, N.C.; Kuich, P.; Zasada, C.; Browe, B.M.; Hamann, W.; et al. Fructose-driven glycolysis supports anoxia resistance in the naked mole-rat. Science 2017, 356, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Peterson, B.L.; Larson, J.; Buffenstein, R.; Park, T.J.; Fall, C.P. Blunted neuronal calcium response to hypoxia in naked mole-rat hippocampus. PLoS ONE 2012, 7, e31568. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.N.; Vazquez-Medina, J.P. Natural Tolerance to Ischemia and Hypoxemia in Diving Mammals: A Review. Front Physiol. 2019, 10, 1199. [Google Scholar] [CrossRef]
- Tian, R.; Yin, D.; Liu, Y.; Seim, I.; Xu, S.; Yang, G. Adaptive Evolution of Energy Metabolism-Related Genes in Hypoxia-Tolerant Mammals. Front Genet 2017, 8, 205. [Google Scholar] [CrossRef]
- Folkow, L.P.; Ramirez, J.M.; Ludvigsen, S.; Ramirez, N.; Blix, A.S. Remarkable neuronal hypoxia tolerance in the deep-diving adult hooded seal (Cystophora cristata). Neurosci. Lett. 2008, 446, 147–150. [Google Scholar] [CrossRef]
- Dempsey, J.A.; Morgan, B.J. Humans In Hypoxia: A Conspiracy Of Maladaptation?! Physiology (Bethesda) 2015, 30, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Ge, R.L.; Simonson, T.S.; Gordeuk, V.; Prchal, J.T.; McClain, D.A. Metabolic aspects of high-altitude adaptation in Tibetans. Exp Physiol 2015, 100, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, R.; Okumiya, K.; Wang, H.; Dai, Q.; Fujisawa, M.; Wada, T.; Imai, H.; Kimura, Y.; Ishimoto, Y.; Fukutomi, E.; et al. Oxidized Low Density Lipoprotein Among the Elderly in Qinghai-Tibet Plateau. Wilderness Environ. Med. 2015, 26, 343–349. [Google Scholar] [CrossRef]
- Cheng, H.; Pamenter, M.E. Naked mole-rat brain mitochondria tolerate in vitro ischemia. J. Physiol. 2021, 0.0, 1–15. [Google Scholar] [CrossRef]
- Zhou, D.; Udpa, N.; Gersten, M.; Visk, D.W.; Bashir, A.; Xue, J.; Frazer, K.A.; Posakony, J.W.; Subramaniam, S.; Bafna, V.; et al. Experimental selection of hypoxia-tolerant Drosophila melanogaster. Proc. Natl. Acad. Sci. USA 2011, 108, 2349–2354. [Google Scholar] [CrossRef]
- Imbrogno, S.; Aiello, D.; Filice, M.; Leo, S.; Mazza, R.; Cerra, M.C.; Napoli, A. MS-based proteomic analysis of cardiac response to hypoxia in the goldfish (Carassius auratus). Sci. Rep. 2019, 9, 18953. [Google Scholar] [CrossRef] [PubMed]
- Fagernes, C.E.; Stenslokken, K.O.; Rohr, A.K.; Berenbrink, M.; Ellefsen, S.; Nilsson, G.E. Extreme anoxia tolerance in crucian carp and goldfish through neofunctionalization of duplicated genes creating a new ethanol-producing pyruvate decarboxylase pathway. Sci. Rep. 2017, 7, 7884. [Google Scholar] [CrossRef]
- Buscemi, L.B.C.; Price, M.; Magistretti, P.J.; Lei, H.; Hirt, L. Extended preclinical investigation of lactate for neuroprotection after ischemic stroke. Clin.Transl. Neurosci. 2020, 1–9. [Google Scholar] [CrossRef][Green Version]
- Buck, L.T.; Pamenter, M.E. The hypoxia-tolerant vertebrate brain: Arresting synaptic activity. Comp Biochem Physiol B Biochem Mol Biol 2018, 224, 61–70. [Google Scholar] [CrossRef]
- Keenan, S.W.; Hill, C.A.; Kandoth, C.; Buck, L.T.; Warren, D.E. Transcriptomic Responses of the Heart and Brain to Anoxia in the Western Painted Turtle. PLoS ONE 2015, 10, e0131669. [Google Scholar] [CrossRef] [PubMed]
- Pamenter, M.E.; Buck, L.T. delta-Opioid receptor antagonism induces NMDA receptor-dependent excitotoxicity in anoxic turtle cortex. J. Exp. Biol. 2008, 211, 3512–3517. [Google Scholar] [CrossRef]
- Milton, S.L.; Nayak, G.; Lutz, P.L.; Prentice, H.M. Gene transcription of neuroglobin is upregulated by hypoxia and anoxia in the brain of the anoxia-tolerant turtle Trachemys scripta. J. Biomed. Sci. 2006, 13, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Garbarino, V.R.; Orr, M.E.; Rodriguez, K.A.; Buffenstein, R. Mechanisms of oxidative stress resistance in the brain: Lessons learned from hypoxia tolerant extremophilic vertebrates. Arch. Biochem. Biophys. 2015, 576, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.H.; Eaton, L.; Pamenter, M.E. Nitric oxide homeostasis is maintained during acute in vitro hypoxia and following reoxygenation in naked mole-rat but not mouse cortical neurons. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2020, 250, 110792. [Google Scholar] [CrossRef]
- Nakajima, M.; Suda, S.; Sowa, K.; Sakamoto, Y.; Nito, C.; Nishiyama, Y.; Aoki, J.; Ueda, M.; Yokobori, S.; Yamada, M.; et al. AMPA Receptor Antagonist Perampanel Ameliorates Post-Stroke Functional and Cognitive Impairments. Neuroscience 2018, 386, 256–264. [Google Scholar] [CrossRef]
- Bourourou, M.; Gouix, E.; Melis, N.; Friard, J.; Heurteaux, C.; Tauc, M.; Blondeau, N. Inhibition of eIF5A hypusination pathway as a new pharmacological target for stroke therapy. J. Cereb. Blood Flow Metab. 2021, 41, 1080–1090. [Google Scholar] [CrossRef]
- Zhou, H.; Wang, X.; Ma, L.; Deng, A.; Wang, S.; Chen, X. FoxO3 transcription factor promotes autophagy after transient cerebral ischemia/reperfusion. Int. J. Neurosci. 2019, 129, 738–745. [Google Scholar] [CrossRef]
- Li, L.; Saliba, P.; Reischl, S.; Marti, H.H.; Kunze, R. Neuronal deficiency of HIF prolyl 4-hydroxylase 2 in mice improves ischemic stroke recovery in an HIF dependent manner. Neurobiol. Dis. 2016, 91, 221–235. [Google Scholar] [CrossRef]
- Hanson, L.R.; Roeytenberg, A.; Martinez, P.M.; Coppes, V.G.; Sweet, D.C.; Rao, R.J.; Marti, D.L.; Hoekman, J.D.; Matthews, R.B.; Frey, W.H., 2nd; et al. Intranasal deferoxamine provides increased brain exposure and significant protection in rat ischemic stroke. J. Pharm. Exp. 2009, 330, 679–686. [Google Scholar] [CrossRef]
- Zhou, J.; Li, J.; Rosenbaum, D.M.; Zhuang, J.; Poon, C.; Qin, P.; Rivera, K.; Lepore, J.; Willette, R.N.; Hu, E.; et al. The prolyl 4-hydroxylase inhibitor GSK360A decreases post-stroke brain injury and sensory, motor, and cognitive behavioral deficits. PLoS ONE 2017, 12, e0184049. [Google Scholar] [CrossRef]
- Kinoshita, H.; Maki, T.; Yasuda, K.; Kishida, N.; Sasaoka, N.; Takagi, Y.; Kakizuka, A.; Takahashi, R. KUS121, a valosin-containing protein modulator, attenuates ischemic stroke via preventing ATP depletion. Sci. Rep. 2019, 9, 11519. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Yenari, M.A.; Cheng, D.; Sapolsky, R.M.; Steinberg, G.K. Bcl-2 overexpression protects against neuron loss within the ischemic margin following experimental stroke and inhibits cytochrome c translocation and caspase-3 activity. J. Neurochem. 2003, 85, 1026–1036. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Samal, B.; Hamelink, C.R.; Xiang, C.C.; Chen, Y.; Chen, M.; Vaudry, D.; Brownstein, M.J.; Hallenbeck, J.M.; Eiden, L.E. Neuroprotection by endogenous and exogenous PACAP following stroke. Regul. Pept. 2006, 137, 4–19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Matsumoto, M.; Nakamachi, T.; Watanabe, J.; Sugiyama, K.; Ohtaki, H.; Murai, N.; Sasaki, S.; Xu, Z.; Hashimoto, H.; Seki, T.; et al. Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP) Is Involved in Adult Mouse Hippocampal Neurogenesis After Stroke. J. Mol. Neurosci. 2016, 59, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Kilic, U.; Caglayan, A.B.; Beker, M.C.; Gunal, M.Y.; Caglayan, B.; Yalcin, E.; Kelestemur, T.; Gundogdu, R.Z.; Yulug, B.; Yilmaz, B.; et al. Particular phosphorylation of PI3K/Akt on Thr308 via PDK-1 and PTEN mediates melatonin's neuroprotective activity after focal cerebral ischemia in mice. Redox. Biol. 2017, 12, 657–665. [Google Scholar] [CrossRef]
- Wang, M.M.; Zhang, M.; Feng, Y.S.; Xing, Y.; Tan, Z.X.; Li, W.B.; Dong, F.; Zhang, F. Electroacupuncture Inhibits Neuronal Autophagy and Apoptosis via the PI3K/AKT Pathway Following Ischemic Stroke. Front Cell Neurosci 2020, 14, 134. [Google Scholar] [CrossRef]
- Li, Y.H.; Fu, H.L.; Tian, M.L.; Wang, Y.Q.; Chen, W.; Cai, L.L.; Zhou, X.H.; Yuan, H.B. Neuron-derived FGF10 ameliorates cerebral ischemia injury via inhibiting NF-kappaB-dependent neuroinflammation and activating PI3K/Akt survival signaling pathway in mice. Sci. Rep. 2016, 6, 19869. [Google Scholar] [CrossRef] [PubMed]
- Shabanzadeh, A.P.; D'Onofrio, P.M.; Monnier, P.P.; Koeberle, P.D. Targeting caspase-6 and caspase-8 to promote neuronal survival following ischemic stroke. Cell Death Dis. 2015, 6, e1967. [Google Scholar] [CrossRef]
- Sun, Y.; Xu, Y.; Geng, L. Caspase-3 inhibitor prevents the apoptosis of brain tissue in rats with acute cerebral infarction. Exp. Med. 2015, 10, 133–138. [Google Scholar] [CrossRef]
- Lee, J.H.; Wei, Z.Z.; Cao, W.; Won, S.; Gu, X.; Winter, M.; Dix, T.A.; Wei, L.; Yu, S.P. Regulation of therapeutic hypothermia on inflammatory cytokines, microglia polarization, migration and functional recovery after ischemic stroke in mice. Neurobiol. Dis. 2016, 96, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, T.V.; Chan, S.L.; Jo, D.G.; Yilmaz, G.; Tang, S.C.; Cheng, A.; Gleichmann, M.; Okun, E.; Dixit, V.D.; Chigurupati, S.; et al. Gamma secretase-mediated Notch signaling worsens brain damage and functional outcome in ischemic stroke. Nat. Med. 2006, 12, 621–623. [Google Scholar] [CrossRef] [PubMed]
- Zacharek, A.; Chen, J.; Cui, X.; Yang, Y.; Chopp, M. Simvastatin increases notch signaling activity and promotes arteriogenesis after stroke. Stroke 2009, 40, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Satriotomo, I.; Bowen, K.K.; Vemuganti, R. JAK2 and STAT3 activation contributes to neuronal damage following transient focal cerebral ischemia. J. Neurochem. 2006, 98, 1353–1368. [Google Scholar] [CrossRef]
- Zhu, H.; Zou, L.; Tian, J.; Du, G.; Gao, Y. SMND-309, a novel derivative of salvianolic acid B, protects rat brains ischemia and reperfusion injury by targeting the JAK2/STAT3 pathway. Eur. J. Pharm. 2013, 714, 23–31. [Google Scholar] [CrossRef]
- Shi, M.; Cao, L.; Cao, X.; Zhu, M.; Zhang, X.; Wu, Z.; Xiong, S.; Xie, Z.; Yang, Y.; Chen, J.; et al. DR-region of Na(+)/K(+) ATPase is a target to treat excitotoxicity and stroke. Cell Death Dis. 2018, 10, 6. [Google Scholar] [CrossRef]
- Shevtsov, M.A.; Nikolaev, B.P.; Yakovleva, L.Y.; Dobrodumov, A.V.; Dayneko, A.S.; Shmonin, A.A.; Vlasov, T.D.; Melnikova, E.V.; Vilisov, A.D.; Guzhova, I.V.; et al. Neurotherapeutic activity of the recombinant heat shock protein Hsp70 in a model of focal cerebral ischemia in rats. Drug. Des. Devel. 2014, 8, 639–650. [Google Scholar] [CrossRef]
- Qi, J.; Han, X.; Liu, H.T.; Chen, T.; Zhang, J.L.; Yang, P.; Bo, S.H.; Lu, X.T.; Zhang, J. 17-Dimethylaminoethylamino-17-demethoxygeldanamycin attenuates inflammatory responses in experimental stroke. Biol. Pharm. Bull. 2014, 37, 1713–1718. [Google Scholar] [CrossRef]
- Hoehn, B.; Ringer, T.M.; Xu, L.; Giffard, R.G.; Sapolsky, R.M.; Steinberg, G.K.; Yenari, M.A. Overexpression of HSP72 after induction of experimental stroke protects neurons from ischemic damage. J. Cereb. Blood Flow Metab. 2001, 21, 1303–1309. [Google Scholar] [CrossRef]
- Teramoto, S.; Shimura, H.; Tanaka, R.; Shimada, Y.; Miyamoto, N.; Arai, H.; Urabe, T.; Hattori, N. Human-derived physiological heat shock protein 27 complex protects brain after focal cerebral ischemia in mice. PLoS ONE 2013, 8, e66001. [Google Scholar] [CrossRef]
- Shimada, Y.; Shimura, H.; Tanaka, R.; Yamashiro, K.; Koike, M.; Uchiyama, Y.; Urabe, T.; Hattori, N. Phosphorylated recombinant HSP27 protects the brain and attenuates blood-brain barrier disruption following stroke in mice receiving intravenous tissue-plasminogen activator. PLoS ONE 2018, 13, e0198039. [Google Scholar] [CrossRef] [PubMed]
- Leak, R.K.; Zhang, L.; Stetler, R.A.; Weng, Z.; Li, P.; Atkins, G.B.; Gao, Y.; Chen, J. HSP27 protects the blood-brain barrier against ischemia-induced loss of integrity. CNS Neurol. Disord. Drug Targets 2013, 12, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Lake, E.M.; Chaudhuri, J.; Thomason, L.; Janik, R.; Ganguly, M.; Brown, M.; McLaurin, J.; Corbett, D.; Stanisz, G.J.; Stefanovic, B. The effects of delayed reduction of tonic inhibition on ischemic lesion and sensorimotor function. J. Cereb. Blood Flow Metab. 2015, 35, 1601–1609. [Google Scholar] [CrossRef]
- Clarkson, A.N.; Huang, B.S.; Macisaac, S.E.; Mody, I.; Carmichael, S.T. Reducing excessive GABA-mediated tonic inhibition promotes functional recovery after stroke. Nature 2010, 468, 305–309. [Google Scholar] [CrossRef]
- Olsson, T.; Cronberg, T.; Rytter, A.; Asztely, F.; Fredholm, B.B.; Smith, M.L.; Wieloch, T. Deletion of the adenosine A1 receptor gene does not alter neuronal damage following ischaemia in vivo or in vitro. Eur. J. Neurosci. 2004, 20, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Gui, L.; Duan, W.; Tian, H.; Li, C.; Zhu, J.; Chen, J.F.; Zheng, J. Adenosine A 2A receptor deficiency reduces striatal glutamate outflow and attenuates brain injury induced by transient focal cerebral ischemia in mice. Brain Res. 2009, 1297, 185–193. [Google Scholar] [CrossRef]
- Kawasaki-Yatsugi, S.; Ichiki, C.; Yatsugi, S.; Takahashi, M.; Shimizu-Sasamata, M.; Yamaguchi, T.; Minematsu, K. Neuroprotective effects of an AMPA receptor antagonist YM872 in a rat transient middle cerebral artery occlusion model. Neuropharmacology 2000, 39, 211–217. [Google Scholar] [CrossRef]
- Aarts, M.; Liu, Y.; Liu, L.; Besshoh, S.; Arundine, M.; Gurd, J.W.; Wang, Y.T.; Salter, M.W.; Tymianski, M. Treatment of ischemic brain damage by perturbing NMDA receptor- PSD-95 protein interactions. Science 2002, 298, 846–850. [Google Scholar] [CrossRef]
- Zhang, S.; Taghibiglou, C.; Girling, K.; Dong, Z.; Lin, S.Z.; Lee, W.; Shyu, W.C.; Wang, Y.T. Critical role of increased PTEN nuclear translocation in excitotoxic and ischemic neuronal injuries. J. Neurosci. 2013, 33, 7997–8008. [Google Scholar] [CrossRef]
- Weilinger, N.L.; Lohman, A.W.; Rakai, B.D.; Ma, E.M.; Bialecki, J.; Maslieieva, V.; Rilea, T.; Bandet, M.V.; Ikuta, N.T.; Scott, L.; et al. Metabotropic NMDA receptor signaling couples Src family kinases to pannexin-1 during excitotoxicity. Nat. Neurosci. 2016, 19, 432–442. [Google Scholar] [CrossRef]
- Zhao, P.; Huang, Y.; Zuo, Z. Opioid preconditioning induces opioid receptor-dependent delayed neuroprotection against ischemia in rats. J. Neuropathol. Exp. Neurol. 2006, 65, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Mayanagi, K.; Gaspar, T.; Katakam, P.V.; Busija, D.W. Systemic administration of diazoxide induces delayed preconditioning against transient focal cerebral ischemia in rats. Brain Res. 2007, 1168, 106–111. [Google Scholar] [CrossRef]
- Mayanagi, K.; Gaspar, T.; Katakam, P.V.; Kis, B.; Busija, D.W. The mitochondrial K(ATP) channel opener BMS-191095 reduces neuronal damage after transient focal cerebral ischemia in rats. J. Cereb. Blood Flow Metab. 2007, 27, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Heron-Milhavet, L.; Xue-Jun, Y.; Vannucci, S.J.; Wood, T.L.; Willing, L.B.; Stannard, B.; Hernandez-Sanchez, C.; Mobbs, C.; Virsolvy, A.; LeRoith, D. Protection against hypoxic-ischemic injury in transgenic mice overexpressing Kir6.2 channel pore in forebrain. Mol. Cell Neurosci. 2004, 25, 585–593. [Google Scholar] [CrossRef]
- Dong, Y.F.; Wang, L.X.; Huang, X.; Cao, W.J.; Lu, M.; Ding, J.H.; Sun, X.L.; Hu, G. Kir6.1 knockdown aggravates cerebral ischemia/reperfusion-induced neural injury in mice. CNS Neurosci. 2013, 19, 617–624. [Google Scholar] [CrossRef]
- Raida, Z.; Hundahl, C.A.; Nyengaard, J.R.; Hay-Schmidt, A. Neuroglobin over expressing mice: Expression pattern and effect on brain ischemic infarct size. PLoS ONE 2013, 8, e76565. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.; Liu, L.; Zhan, L.; Liang, D.; Li, L.; Liu, D.; Sun, W.; Xu, E. Neuroglobin mediates neuroprotection of hypoxic postconditioning against transient global cerebral ischemia in rats through preserving the activity of Na(+)/K(+) ATPases. Cell Death Dis. 2018, 9, 635. [Google Scholar] [CrossRef]
- Cai, B.; Lin, Y.; Xue, X.H.; Fang, L.; Wang, N.; Wu, Z.Y. TAT-mediated delivery of neuroglobin protects against focal cerebral ischemia in mice. Exp. Neurol. 2011, 227, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Park, J.; Oh, Y.; Lee, J.E. Glutathione suppresses cerebral infarct volume and cell death after ischemic injury: Involvement of FOXO3 inactivation and Bcl2 expression. Oxid. Med. Cell Longev. 2015, 2015, 426069. [Google Scholar] [CrossRef]
- Hoehn, B.; Yenari, M.A.; Sapolsky, R.M.; Steinberg, G.K. Glutathione peroxidase overexpression inhibits cytochrome C release and proapoptotic mediators to protect neurons from experimental stroke. Stroke 2003, 34, 2489–2494. [Google Scholar] [CrossRef]
- Armogida, M.; Spalloni, A.; Amantea, D.; Nutini, M.; Petrelli, F.; Longone, P.; Bagetta, G.; Nistico, R.; Mercuri, N.B. The protective role of catalase against cerebral ischemia in vitro and in vivo. Int. J. Immunopathol. Pharm. 2011, 24, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Sun, M.; Li, M.; Zhang, D.; Han, F.; Wu, J.C.; Fukunaga, K.; Chen, Z.; Qin, Z.H. Combination of NAD(+) and NADPH Offers Greater Neuroprotection in Ischemic Stroke Models by Relieving Metabolic Stress. Mol. Neurobiol. 2018, 55, 6063–6075. [Google Scholar] [CrossRef] [PubMed]
- Vigne, P.; Frelin, C. The role of polyamines in protein-dependent hypoxic tolerance of Drosophila. BMC Physiol. 2008, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Park, M.H.; Nishimura, K.; Zanelli, C.F.; Valentini, S.R. Functional significance of eIF5A and its hypusine modification in eukaryotes. Amino Acids 2010, 38, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Puleston, D.J.; Buck, M.D.; Klein Geltink, R.I.; Kyle, R.L.; Caputa, G.; O'Sullivan, D.; Cameron, A.M.; Castoldi, A.; Musa, Y.; Kabat, A.M.; et al. Polyamines and eIF5A Hypusination Modulate Mitochondrial Respiration and Macrophage Activation. Cell Metab. 2019, 30, 352–363.e8. [Google Scholar] [CrossRef] [PubMed]
- Melis, N.; Rubera, I.; Cougnon, M.; Giraud, S.; Mograbi, B.; Belaid, A.; Pisani, D.F.; Huber, S.M.; Lacas-Gervais, S.; Fragaki, K.; et al. Targeting eIF5A Hypusination Prevents Anoxic Cell Death through Mitochondrial Silencing and Improves Kidney Transplant Outcome. J. Am. Soc. Nephrol. 2017, 28, 811–822. [Google Scholar] [CrossRef]
- Turpaev, K.T. Translation Factor eIF5A, Modification with Hypusine and Role in Regulation of Gene Expression. eIF5A as a Target for Pharmacological Interventions. Biochemistry (Moscow) 2018, 83, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Atkins, M.B.; Redman, B.; Mier, J.; Gollob, J.; Weber, J.; Sosman, J.; MacPherson, B.L.; Plasse, T. A phase I study of CNI-1493, an inhibitor of cytokine release, in combination with high-dose interleukin-2 in patients with renal cancer and melanoma. Clin. Cancer Res. 2001, 7, 486–492. [Google Scholar]
- Wang, J.; Grishin, A.V.; Ford, H.R. Experimental Anti-Inflammatory Drug Semapimod Inhibits TLR Signaling by Targeting the TLR Chaperone gp96. J. Immunol. 2016, 196, 5130–5137. [Google Scholar] [CrossRef]
- Lorenz, H.M.; Schmitt, W.H.; Tesar, V.; Muller-Ladner, U.; Tarner, I.; Hauser, I.A.; Hiepe, F.; Alexander, T.; Woehling, H.; Nemoto, K.; et al. Treatment of active lupus nephritis with the novel immunosuppressant 15-deoxyspergualin: An open-label dose escalation study. Arthritis Res. 2011, 13, R36. [Google Scholar] [CrossRef]
- Priotto, G.; Pinoges, L.; Fursa, I.B.; Burke, B.; Nicolay, N.; Grillet, G.; Hewison, C.; Balasegaram, M. Safety and effectiveness of first line eflornithine for Trypanosoma brucei gambiense sleeping sickness in Sudan: Cohort study. BMJ 2008, 336, 705–708. [Google Scholar] [CrossRef]
- Nho, R.S.; Hergert, P. FoxO3a and disease progression. World J. Biol. Chem. 2014, 5, 346–354. [Google Scholar] [CrossRef]
- Mendenhall, A.R.; LaRue, B.; Padilla, P.A. Glyceraldehyde-3-phosphate dehydrogenase mediates anoxia response and survival in Caenorhabditis elegans. Genetics 2006, 174, 1173–1187. [Google Scholar] [CrossRef]
- Malik, A.I.; Storey, K.B. Transcriptional regulation of antioxidant enzymes by FoxO1 under dehydration stress. Gene 2011, 485, 114–119. [Google Scholar] [CrossRef]
- Barretto, E.C.; Polan, D.M.; Beevor-Potts, A.N.; Lee, B.; Grewal, S.S. Tolerance to Hypoxia Is Promoted by FOXO Regulation of the Innate Immunity Transcription Factor NF-kappaB/Relish in Drosophila. Genetics 2020, 215, 1013–1025. [Google Scholar] [CrossRef]
- Reiterer, M.; Milton, S.L. Induction of foxo3a protects turtle neurons against oxidative stress. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2020, 243, 110671. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Zhu, C.; Wang, B.; Zheng, H.; McAlister, V.; Lacefield, J.C.; Quan, D.; Mele, T.; Greasley, A.; Liu, K.; et al. Circular RNA Foxo3 in cardiac ischemia-reperfusion injury in heart transplantation: A new regulator and target. Am. J. Transpl. 2020, 2992–3004. [Google Scholar] [CrossRef]
- Zhang, J.C.; Xu, H.; Yuan, Y.; Chen, J.Y.; Zhang, Y.J.; Lin, Y.; Yuan, S.Y. Delayed Treatment with Green Tea Polyphenol EGCG Promotes Neurogenesis After Ischemic Stroke in Adult Mice. Mol. Neurobiol. 2017, 54, 3652–3664. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Zhang, W.; Wang, J.; Yang, H.; Zhou, Q.; Wang, H.; Li, L.; Du, G. Inhibition of FOXO3a/BIM signaling pathway contributes to the protective effect of salvianolic acid A against cerebral ischemia/reperfusion injury. Acta Pharm. Sin. B 2019, 9, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.K.; Jain, S.A.; Bae, O.N.; Majid, A.; Rajanikant, G.K. Hypoxia Mimetic Agents for Ischemic Stroke. Front Cell Dev. Biol. 2018, 6, 175. [Google Scholar] [CrossRef] [PubMed]
- Sharp, F.R.; Bernaudin, M. HIF1 and oxygen sensing in the brain. Nat. Rev. Neurosci. 2004, 5, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Yeh, S.H.; Ou, L.C.; Gean, P.W.; Hung, J.J.; Chang, W.C. Selective inhibition of early--but not late--expressed HIF-1alpha is neuroprotective in rats after focal ischemic brain damage. Brain Pathol. 2011, 21, 249–262. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, H.O.; Sasaoka, N.; Koike, M.; Nakano, N.; Muraoka, Y.; Toda, Y.; Fuchigami, T.; Shudo, T.; Iwata, A.; Hori, S.; et al. Novel VCP modulators mitigate major pathologies of rd10, a mouse model of retinitis pigmentosa. Sci. Rep. 2014, 4, 5970. [Google Scholar] [CrossRef]
- Ikeda, H.O.; Muraoka, Y.; Hata, M.; Sumi, E.; Ikeda, T.; Nakagawa, T.; Abe, H.; Tada, H.; Morita, S.; Kakizuka, A.; et al. Safety and effectiveness of a novel neuroprotectant, KUS121, in patients with non-arteritic central retinal artery occlusion: An open-label, non-randomized, first-in-humans, phase 1/2 trial. PLoS ONE 2020, 15, e0229068. [Google Scholar] [CrossRef] [PubMed]
- Oorschot, D.E.; Sizemore, R.J.; Amer, A.R. Treatment of Neonatal Hypoxic-Ischemic Encephalopathy with Erythropoietin Alone, and Erythropoietin Combined with Hypothermia: History, Current Status, and Future Research. Int. J. Mol. Sci. 2020, 21, 1487. [Google Scholar] [CrossRef]
- van der Worp, H.B.; Sena, E.S.; Donnan, G.A.; Howells, D.W.; Macleod, M.R. Hypothermia in animal models of acute ischaemic stroke: A systematic review and meta-analysis. Brain 2007, 130 Pt 12, 3063–3074. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Steinberg, G.K.; Sapolsky, R.M. General versus specific actions of mild-moderate hypothermia in attenuating cerebral ischemic damage. J. Cereb. Blood Flow Metab. 2007, 27, 1879–1894. [Google Scholar] [CrossRef] [PubMed]
- Hua, C.; Ju, W.N.; Jin, H.; Sun, X.; Zhao, G. Molecular chaperones and hypoxic-ischemic encephalopathy. Neural. Regen. Res. 2017, 12, 153–160. [Google Scholar] [CrossRef]
- Currie, R.W.; Ellison, J.A.; White, R.F.; Feuerstein, G.Z.; Wang, X.; Barone, F.C. Benign focal ischemic preconditioning induces neuronal Hsp70 and prolonged astrogliosis with expression of Hsp27. Brain Res. 2000, 863, 169–181. [Google Scholar] [CrossRef]
- Stetler, R.A.; Gao, Y.; Zhang, L.; Weng, Z.; Zhang, F.; Hu, X.; Wang, S.; Vosler, P.; Cao, G.; Sun, D.; et al. Phosphorylation of HSP27 by protein kinase D is essential for mediating neuroprotection against ischemic neuronal injury. J. Neurosci. 2012, 32, 2667–2682. [Google Scholar] [CrossRef]
- Zuo, Y.; Wang, J.; Liao, F.; Yan, X.; Li, J.; Huang, L.; Liu, F. Inhibition of Heat Shock Protein 90 by 17-AAG Reduces Inflammation via P2X7 Receptor/NLRP3 Inflammasome Pathway and Increases Neurogenesis After Subarachnoid Hemorrhage in Mice. Front Mol. Neurosci. 2018, 11, 401. [Google Scholar] [CrossRef]
- Shi, Y.; Jiang, X.; Zhang, L.; Pu, H.; Hu, X.; Zhang, W.; Cai, W.; Gao, Y.; Leak, R.K.; Keep, R.F.; et al. Endothelium-targeted overexpression of heat shock protein 27 ameliorates blood-brain barrier disruption after ischemic brain injury. Proc. Natl. Acad. Sci. USA 2017, 114, E1243–E1252. [Google Scholar] [CrossRef]
- Lee, H.J.; Yoon, Y.S.; Lee, S.J. Mechanism of neuroprotection by trehalose: Controversy surrounding autophagy induction. Cell Death Dis. 2018, 9, 712. [Google Scholar] [CrossRef]
- Rodriguez-Navarro, J.A.; Rodriguez, L.; Casarejos, M.J.; Solano, R.M.; Gomez, A.; Perucho, J.; Cuervo, A.M.; Garcia de Yebenes, J.; Mena, M.A. Trehalose ameliorates dopaminergic and tau pathology in parkin deleted/tau overexpressing mice through autophagy activation. Neurobiol. Dis. 2010, 39, 423–438. [Google Scholar] [CrossRef]
- Chen, Q.; Haddad, G.G. Role of trehalose phosphate synthase and trehalose during hypoxia: From flies to mammals. J. Exp. Biol. 2004, 207 (Pt 18), 3125–3129. [Google Scholar] [CrossRef]
- Sciarretta, S.; Yee, D.; Nagarajan, N.; Bianchi, F.; Saito, T.; Valenti, V.; Tong, M.; Del Re, D.P.; Vecchione, C.; Schirone, L.; et al. Trehalose-Induced Activation of Autophagy Improves Cardiac Remodeling After Myocardial Infarction. J. Am. Coll Cardiol. 2018, 71, 1999–2010. [Google Scholar] [CrossRef]
- Schwartz-Bloom, R.D.; Sah, R. gamma-Aminobutyric acid(A) neurotransmission and cerebral ischemia. J. Neurochem. 2001, 77, 353–371. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhang, J.; Wang, L.N. Gamma aminobutyric acid (GABA) receptor agonists for acute stroke. Cochrane Database Syst. Rev. 2018, 10, CD009622. [Google Scholar] [CrossRef] [PubMed]
- Hiu, T.; Farzampour, Z.; Paz, J.T.; Wang, E.H.; Badgely, C.; Olson, A.; Micheva, K.D.; Wang, G.; Lemmens, R.; Tran, K.V.; et al. Enhanced phasic GABA inhibition during the repair phase of stroke: A novel therapeutic target. Brain 2016, 139, 468–480. [Google Scholar] [CrossRef]
- Wu, Q.J.; Tymianski, M. Targeting NMDA receptors in stroke: New hope in neuroprotection. Mol Brain 2018, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- McQueen, J.; Ryan, T.J.; McKay, S.; Marwick, K.; Baxter, P.; Carpanini, S.M.; Wishart, T.M.; Gillingwater, T.H.; Manson, J.C.; Wyllie, D.J.A.; et al. Pro-death NMDA receptor signaling is promoted by the GluN2B C-terminus independently of Dapk1. Elife 2017, 6, e17161. [Google Scholar] [CrossRef]
- Weilinger, N.L.; Tang, P.L.; Thompson, R.J. Anoxia-induced NMDA receptor activation opens pannexin channels via Src family kinases. J. Neurosci. 2012, 32, 12579–12588. [Google Scholar] [CrossRef]
- Fan, X.; Jin, W.Y.; Wang, Y.T. The NMDA receptor complex: A multifunctional machine at the glutamatergic synapse. Front Cell Neurosci. 2014, 8, 160. [Google Scholar] [CrossRef]
- Cook, D.J.; Teves, L.; Tymianski, M. Treatment of stroke with a PSD-95 inhibitor in the gyrencephalic primate brain. Nature 2012, 483, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.D.; Goyal, M.; Menon, B.K.; Nogueira, R.G.; McTaggart, R.A.; Demchuk, A.M.; Poppe, A.Y.; Buck, B.H.; Field, T.S.; Dowlatshahi, D.; et al. Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): A multicentre, double-blind, randomised controlled trial. Lancet 2020, 395, 878–887. [Google Scholar] [CrossRef]
- Davis, S.M.; Lees, K.R.; Albers, G.W.; Diener, H.C.; Markabi, S.; Karlsson, G.; Norris, J. Selfotel in acute ischemic stroke: Possible neurotoxic effects of an NMDA antagonist. Stroke 2000, 31, 347–354. [Google Scholar] [CrossRef]
- Melani, A.; Pugliese, A.M.; Pedata, F. Adenosine receptors in cerebral ischemia. Int. Rev. Neurobiol. 2014, 119, 309–348. [Google Scholar] [CrossRef]
- Kitagawa, H.; Mori, A.; Shimada, J.; Mitsumoto, Y.; Kikuchi, T. Intracerebral adenosine infusion improves neurological outcome after transient focal ischemia in rats. Neurol. Res. 2002, 24, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Coelho, J.E.; Rebola, N.; Fragata, I.; Ribeiro, J.A.; de Mendonca, A.; Cunha, R.A. Hypoxia-induced desensitization and internalization of adenosine A1 receptors in the rat hippocampus. Neuroscience 2006, 138, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Birben, E.; Sahiner, U.M.; Sackesen, C.; Erzurum, S.; Kalayci, O. Oxidative stress and antioxidant defense. World Allergy Organ J. 2012, 5, 9–19. [Google Scholar] [CrossRef]
- Liu, L.; Locascio, L.M.; Dore, S. Critical Role of Nrf2 in Experimental Ischemic Stroke. Front Pharm. 2019, 10, 153. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, B.A.; Minnerup, J.; Balami, J.S.; Arba, F.; Buchan, A.M.; Kleinschnitz, C. Neuroprotection for ischaemic stroke: Translation from the bench to the bedside. Int. J. Stroke 2012, 7, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Shankaran, S.; Laptook, A.R.; Ehrenkranz, R.A.; Tyson, J.E.; McDonald, S.A.; Donovan, E.F.; Fanaroff, A.A.; Poole, W.K.; Wright, L.L.; Higgins, R.D.; et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl. J. Med. 2005, 353, 1574–1584. [Google Scholar] [CrossRef] [PubMed]
- Milton, S.L.; Dawson-Scully, K. Alleviating brain stress: What alternative animal models have revealed about therapeutic targets for hypoxia and anoxia. Future Neurol. 2013, 8, 287–301. [Google Scholar] [CrossRef]
| Specie | Type of Resistance | Metabolism | Source of Energy | Neurotransmission | Molecular Mechanisms of Neuroprotection | pH Buffering | ||
|---|---|---|---|---|---|---|---|---|
| Invertebrates | Locust L. migratoria Ref: [27,28,29] | Natural: environmental O2 depletion Experimental anoxia: 4 h at 30 °C | Reversible coma ↓ ATP muscle ↑ K ↓ Na haemolymph ↓ haemolymph volume | Glycogen ↓ ATP | PTPN1 and PDHE1β variants in Tibetan locust and increased PDHE1β expresion : enhanced aerobic metabolism | ↓ hemolymph pH | ||
| Fruit fly D. melanogaster Ref: [30,31,32] | Natural: environmental O2 depletion Experimental anoxia: LT50 = 8 h Selected resistant flies: live under constant 4 % O2 | Reversible coma ↓ metabolism ↓ ATP ↑ K Hypoxia resistant flies: ↓ Glycolytic, TCA and β-oxidation enzymes and respiratory complexes | Glycogen Trehalose | Editing of ion channels by adenosine deaminase improves hypoxia survival | Threalose, tsp1 Polyols, β-alanine, taurine ↑ HIF1α ↑ FOXO Acute: ↑ Hsp70, Hsc73 Chronic: ↑ Notch, Toll, hairy | ↓ haemolymph pH ↑ lactate, alanine, succinate and acetate | ||
| Vertebrates | Frog R. sylvatica and amurensis Ref: [33,34] | Natural: Freeze during the winter (−2.5 °C) Experimental anoxia: 24 h at 5 °C | ↓ ATP ↑ glycogenolysis: ↑ glucose but ↓ lower products | Glycogen | Changes in phosphoproteins to use glucose and urea as cryoprotectant ↑ Glycerol Low succinate/fumarate ratio | ↑ lactate, alanine, succinate | ||
| Crucian carp C. carassius Ref: [4,35,36,37] | Natural: 4–5 months’ anoxia under frozen lakes Experimental anoxia: 7 days at 8 and 13 °C. 6 weeks at 2 °C | ↓ heart rate ↓ GAPDH, LDH Ethanol as end product Increased brain blood flow Suspend some sensory functions | Glycogen stored in liver High affinity Haemoglobin | ↓ Glutamate and aspartate ↑ GABA and Glycine | Hypothermia p53R2 paralogs Hypothermia ↓ Ca influx | Lactate transported to muscle and converted to ethanol by PDHc | ||
| Pond turtle T.Scripta C.Picta Ref: [4,38,39,40,41,42] |
Months of anoxia during hibernation Experimental: 30 hours at 20 °C 7 weeks at 3 °C | Reversible coma ↓ energy demand ↓ proteins involved in ATP supply ↓ heart rate and heat production Low balanced ATP levels Channel arrest | Brain glycogen stores ↑ glycolysis ↓ protein synthesis Constant ADP in heart | ↑ GABAR and AR ↓ excitatory NT and NMDAR activity Katp channel activation ↑ DOR Check for signal arousal | Hypothermia ↑ Bcl2: Bax ↓ PDCD6IP ↑ PI3K, AKT, ERK, p53 ↑ HIFα ↑ JAK/STAT in liver Antioxidant defense preconditioning: antioxidants, HSP, adenosine, Ngb and succinate/fumarate ratio ↓ VCP, GAPDH | Lactate is buffered by calcium carbonate realease from the shell | ||
| Mammals | Artic ground squirrel U.Paryii Ref: [5,43,44,45] |
Natural: hypoxemia during arousal from hibenation and euthermy Experimental: 8 min anoxia (euthermic) | ↓ metabolism up to 1–2% of basal when hibernating | Lipid metabolism | ↓ NMDAR ↓ excitotoxicity (↓ NR1 subunit) ↓ NKA activity | ↑ antioxidant defense↓ NKA and Na channelsHypothermiaImmunosuppression, Anticoagulant blood↑ HIF1α | Good pH bufferingArousal: ↑ lactate | |
| Naked mole rat H.glaber Ref: [46,47,48] |
Natural: chronic hypoxia living in burrows Experimental anoxia: 18 min at 33 °C 6 min at 37 °C | Awake and active during hypoxia Loss of consciousness with sporadic breathing during anoxia ↓ metabolism ↓ heart and respiratory rate | Hypoxia:↑ glycolysis Anoxia: fuelled by fructose |
Maintenance of synaptic transmission NMDAR isoforms less permeable to calcium | ↑ GLUT5 mRNA and protein levels ↑ KHK-A KHK-C ↓ intracellular calcium Maintained mitochondrial membrane integrity |
No signs of acidosis Cardiac function facilitates lactate clearance | ||
| Diving mammals Whales, seals Ref: [49,50,51] | Behavioural pattern (diving) at 3–4 °C | ↓ metabolism in some organs Anaerobic metabolism (lactate at the end of the dive) ↓ heart rate |
Large glycogen stores Oxygen in Hg, Mgb and Ngb and splenic contraction but critical at the end of the dive | Maintain spiking in vitro Reconfiguration of neuronal activity ↓ NMDA activity ↓ Ca influx | Stress tolerance (antioxidants) Ngb ↑ HIF1α | Positive selection genes in cetaceans (LDHA, LDHD, PC, PCK1, FBP1, and GPI) | ||
| Human Ref: [52,53,54] |
High altitude adapted Tibetans Ischemic preconditioning | ↑ glucose uptake and glycolysis ↓ mitochondrial glucose oxidation ↑ free fatty acids Changes in haemoglobin levels | ↑ glucose ↓ lipid metabolism | Mutations in EGNL1 (↑ O2 affinity and ↓ p23 affinity), EPAS (↑ anaerobic shift) and PPARA genes ↑ NO ↑ cerebral perfusion ↑ HSP-27, NOS, GDNF, VEGFa, TGF β1, LIF and TIMP-1 ↓ inflammation (↓ MCP1) and coagulation | ↑ lactate |
| Target | Treatment | Species | Regime | Stroke Model | Outcome | Time |
|---|---|---|---|---|---|---|
| eIF5a | GC7 Ref. [67] | Mice C57BL/6 | 2 h before MCAO (i.p,) 2 h after MCAO (i.p,) | tMCAO for 60 min | ↓ infarct volume ↑ neurological recovery | 24 h and 4 days |
| FOXO3a | Viral over-expression Ref. [68] | Rat Sprague-Dawley | 1 week before MCAO | tMCAO for 2 h | ↓ infarct volume | 24 h |
| HIF-1α | Mice nPHD2 KO Ref. [69] | pMCAO | ↓ infarct volume ↑ sensory motor function ↑ VEGF | 7 and 30 days | ||
| DFO Ref. [70] | Rat Sprague-Dawley | 48 h before MCAO at 3 h intervals (i.n.) | pMCAO | ↓ infarct volume ↓ neurologic deficit | 5 days | |
| GSK360A Ref. [71] | Rat Sprague-Dawley | 18 h and 5 h before MCAO (p.o.) | tMCAO for 2 h | ↓ infarct volume ↓ neurological deficit ↑ EPO and VEGF | 4 weeks, | |
| Reduction of VCP ATPase activity | KUS121 Ref. [72] | Mice C57BL/6 and B17 | After occlusion + after reperfusión | B17: distal tMCAO for 22 min C57BL/6: distal pMCAO + 30 min hypoxia (10%O2) | B17: ↓ infarction volume and ↑ NeuN C57BL/6: ↓ infarction volume, ↑ rotarod and removal test performance | 24 h |
| Bcl-2 induction | Bcl-2 viral over-expresion Ref. [73] | Rat Sprague-Dawley | 14 h before MCAO (Cortical infusion) | Distal tMCAO for 3 h Distal pMCAO | =infarct volume ↓ neuronal death per infected cell ↓ cytochrome C release ↓ Caspase-3 | 48 h |
| PACAP Ref. [74] | Mice C57BL/6 and PACAP −/− | 1 h after MCAO (i.c.v./i.v.) | pMCAO | ↓ infarct volume ↑ functional recovery (NSS score) ↓ cytochrome C release | 24 h | |
| PACAP deficiency Ref. [75] | Mice PACAP +/− (C57BL/6) | tMCAO for 12 min | ↑ neurogenesis | 7 days | ||
| PI3K/Akt activation | Melatonin Ref. [76] | Mice C57BL/6 | Right after reperfusion (i.p.) | tMCAO for 30 or 90 min | ↓ infarct volume ↑ BBB integrity | 24 and 72 h |
| Electo Acupuncture Ref. [77] | Rat Sprague-Dawley | 24 h after MCAO (30 min/day for 3 days) | tMCAO for 2 h | ↓ infarct volume ↓ caspase-3 ↓ autophagy | 72 h | |
| FGF10 Ref. [78] | Mice C57BL/6 | 30 min before MCAO (i.c.v.) | tMCAO for 2 h | ↓ infarcted area↓ neurological deficit ↓ TUNEL+ cells, Caspase-3, 8 and 9 ↓ TNFα, IL6 | 24 h | |
| Caspase-6 inhibition | Z-VEID-FMK Ref. [79] | Rat | 0 h and 24 h after reperfusion (i.v.) | thromboembolic focal cerebral ischemia | ↓ infarct volume and brain edema ↓ neurological deficit (Benderson´s) ↓ caspase-3, 6 and 8 ↑ prolifeRat ing cells | 48 h and 7 days |
| Caspase-8 inhibition | Z-IETD-FMK Ref. [79] | Rat | 0 h and 24 h after reperfusion (i.v.) | thromboembolic focal cerebral ischemia | ↓ infarct volume ↓ edema ↓ neurological deficit (Benderson´s) ↓ caspase-3, 6 and 8 ↑ prolifeRat ing cells | 48 h and 7 days |
| Caspase-3 inhibition | Z-DEVD Ref. [80] | Rat Sprague-Dawley | 5 h after MCAO (i.v.) | tMCAO for 2 h | ↓ infarction range ↓ caspase-3 and apoptosis ↓ neurological deficit (Benderson´s) | 48 h |
| Therapeutic hypothermia | HSP-201 (NTR1 agonist) Ref. [81] | Mice C57BL/6 | 30 min after MCAO plus repeated doses (i.p.) for constant 33 °C 6 h | Distal pMCAO | ↓ infarct volume ↓ edema ↑ neurological performance (corner and cylinder tests) ↓ TNFα, IL1β, MCP-1, IBA-1 ↑ IL10 ↓ M1 ↑ M2 | 6, 24 and 72 h |
| Notch1 activity | DAPT/DBZ (γ-secretase inhibitors) Ref. [82] | Mice C57BL/6 | 30 min before occlusion/ 4 h after/6 h after | tMCAO for 1 h | ↓ infarct volume ↑ neurological performance | 3 h |
| Notch1Tg Antisense Ref [82] | Mice NAS Tg (C57BL/6) | tMCAO for 1 h | ↓ infarct volume ↑ neurological performance | 3 h | ||
| Simvastatin (↑ activity) Ref [83] | Rat Wistar | 24 h before MCAO (daily, 7 days, p.o.) | tMCAO for 2 h | ↑ arterial density ↑ vascular cell prolifeRat ion | 14 days | |
| JAK/STAT3 inhibition | STAT3 siRNA Ref. [84] | Rat Adult hypertensive | 1 h before MCAO (i.c.v.) | tMCAO for 1 h | ↓ infarct volume ↓ TUNEL+ cells ↓ neurological deficit | 24 h |
| AG490 (JAK inhibitor) Ref. [84] | Rat Adult hypertensive | 24 h before MCAO (i.c.v. infusion) | tMCAO for 1 h | ↓ infarct volume ↓ TUNEL+ cells ↓ neurological deficit | 24 h | |
| SMND-309 (JAK/STAT activator) Ref. [85] | Rat Sprague-Dawley | 9 h after reperfusion (i.v.) | tMCAO for 90 min | ↓ infarct volume ↑ functional recovery (NSS score) ↑ EPO ↓ vascular permeability | 7 and 14 days | |
| Na+/K+ ATPase activity | ↓ NKAα1 activity Ref. [86] | Mice NKAα1 +/− (C57BL/6) | tMCAO for 1 h | ↑ infarct volume | 24 h | |
| DR-Ab (↑ activity) Ref. [86] | Mice C57BL/6 | 1 h before/1 h after MCAO (i.c.v.) | tMCAO for 1 h | ↓ infarct volume | 24 h | |
| HSP-70 | rHSP70 Ref. [87] | Rat Wistar | 20 min before or 2 h after MCAO (i.v.)/s.c. alginate | tMCAO for 45 min | ↓ infarct volume | 48 and 72 h |
| 17-DMAG (HSP90 inhibitor) Ref. [88] | Mice C57BL/6 | 7 days before ischemia every other day (p.o.) | tMCAO for 1 h | ↓ infarct volume ↓ neurological deficit ↓ IBA1, MHCII, NFκB, TNFα, IL1β, ICAM1, iNOS | 24 h | |
| Hsp70 viral over- expresión Ref. [89] | Rat Sprague-Dawley | 12 h before and 0.5, 1 and 2 h after ischemia (i.c.v.) | ICA occlusion for 1 h | Profilactic: ↑ neuronal survival Therapeutic: =infarct size | 48 h | |
| HSP27 | hHSP27 Ref. [90] | Mice C57BL/6 | 1 h after reperfusion (i.v.) | tMCAO for 1 h | ↓ infarct volume ↓ neurological deficit ↓ apoptosis ↓ oxidative DNA damage, lipid peroxidation and glial activation | 24 and 72 h |
| prHSP27 Ref. [91] | Mice C57BL/6 | 2 h after reperfusion (i.v.) | tMCAO for 1 h + D-glucose for hemorrhagic transformation | ↓ infarct volume and edema ↓ BBB permeability ↓ MMP9 ↓ neurological severity ↓ mortality and hemorrhagic transformation | 24 h | |
| HSP27 overexpression Ref. [92] | Mice Hsp27 Transgenic C57BL/6 | tMCAO for 1 h | ↓ infarct volume ↓ Behavioural deficit ↓ BBB permeability and apoptosis in microvessel walls ↓ Brain water content ↓ Neuropil infiltRat ion and | 24 and 96 h | ||
| GABA receptor modulation | L-655,708 (GABA inverse agonist) | Rat Sprague-Dawley Ref. [93] | 7 days before stroke for 2 weeks (s.c.) | Intracortical ET1 | ↓ infarct volume ↓ neurological severity | 3 weeks |
| Mice C57BL/6 Ref. [94] | 3 days after stroke (i.v. minipump) | Photothrombosis | ↑ functional recovery | 7 days | ||
| Adenosine receptor modulation | AR1 KO Ref. [95] | Mice AR1 −/− (C57BL/6) | Bilateral common artery occlusion | =neuronal damage | 4 days | |
| 8-CPT (AR1 antagonist) Ref. [95] | Mice C57BL/6 | 30 min before ischemia (i.p.) | Bilateral common artery occlusion | ↑ neuronal damage | 4 days | |
| AR2 KO Ref. [96] | Mice AR2 −/− (C57BL/6) | tMCAO for 2 h | ↓ infarct volume ↓ neurological deficit score ↓ brain water content and glutamate | 2, 22 and 26 h | ||
| AMPA receptor antagonism | Perampanel Ref. [66] | Rat Sprague-Dawley | After reperfusion (i.p.) | tMCAO for 90 min | ↓ infarct volume and edema ↓ inflammation (IBA1, TNF-α, IL1β) ↓ oxidative stress ↓ Bax ↑ Akt ↑ Bcl-XL | 7 days |
| YM872 Ref. [97] | Rat Sprague-Dawley | 2, 3 or 4 h after reperfusion (i.v.) | tMCAO for 3 h | ↓ infarct volume ↓ neurological deficit | 24 h and 7 days | |
| Reduction of NMDA receptor activation | Tat-NR2B9c (NA-1) Ref. [98] | Rat Sprague-Dawley | 45 min before MCAO (i.v.) | tMCAO for 90 min | ↓ infarct volume | 24 h |
| Tat-K13 Ref. [99] | Rat Sprague-Dawley | 2 or 6 h after MCAO (i.v.) | tMCAO for 90 min | ↓ infarct volume ↓ neurological deficit (grip and swimming test) | 28 days | |
| TAT-Panx308 Ref. [100] | Rat Sprague-Dawley | 30 min before or 2 h after MCAO (i.p.) | tMCAO for 1 h | ↓ infarct volume ↓ motor deficit | 2 and 14 weeks | |
| δ-Opioid receptor agonism | Tan-67 Ref. [101] | Rat Sprague-Dawley | 12, 24 or 48 h before MCAO (i.v.) | pMCAO | ↓ infarct volume ↑ functional outcome | 24 h |
| DADLE Ref. [101] | Rat Sprague-Dawley | 30 min before MCAO (i.p.) | tMCAO for 2 h | ↓ infarct volume ↓ apoptosis | 72 h | |
| Katp opening | Diazoxide Ref. [102] | Rat Wistar | 24 h before MCAO (i.p.) | tMCAO for 90 min | ↓ infarct volume ↓ neurological score (six different tests) | 72 h |
| BMS-191095 Ref. [103] | Rat Wistar | 24 h before MCAO (i.c.v.) | tMCAO for 90 min | ↓ infarct volume No effect when administered 30 min before | 72 h | |
| Kir 6.2 over-expression Ref. [104] | Mice Kir 6.2 Tg (C57BL/6) | pMCAO + systemic hypoxia (8% O2 for 20 min) | ↓ cortical infarct | 72 h | ||
| Kir 6.1 Ref. [105] | Mice Kir 6.1 +/− (C57BL/6) | tMCAO for 1 h | ↑ Infarct size and neuronal loss ↑ Neurological deficit and ↑ ECM degeneRat ion and ER stress | 24 h | ||
| Ngb over- expression | Ngb transgene Ref. [106] | Mice Ngb-Tg2 (C57BL/6) | pMCAO | ↓ Infarct area | 24 h | |
| Ngb viral over- expression | Rat Sprague-Dawley Ref. [106] | 3 weeks before MCAO (i.c.v.) | tMCAO for 90 min | ↓ infarct volume ↓ Neurological deficit (NSS score) | 24 h | |
| Rat Wistar Ref. [107] | 14 days before ischemia | tGCI for 10 min | ↑ Cell survival in the CA1 area ↑ Atpb1 expression and Na/K ATPase activity | 7 days | ||
| TAT-mNgb Ref. [108] | Mice C57BL/6 | 2 h before the occlusion (i.v.) | tMCAO for 2 h | ↓ infarct volume ↓ Neurological deficit | 24 h | |
| Modulation of the antioxidant defense system | GSH infusion Ref. [109] | Rat Sprague-Dawley | 10 min after MCAO (i.v.) | tMCAO for 1 h | ↓ infarct volume ↓ ROS, Foxo-3 ↑ Bcl-2, PI3K/Akt | 48 h |
| GPX viral delivery Ref: [110] | Rat Sprague-Dawley | 12 h before/2 or 5 h after MCAO | tMCAO for 1 h | ↑ Neuronal survival ↓ Apoptosis, cytochrome C release | 24 h | |
| Catalase transgene Ref. [111] | Mice CAT-Tg (C57BL/6) | tMCAO for 40 min | ↑ infarct volume | 48 h | ||
| NAD +/− NADPH Ref. [112] | Mice ICR | 0 h after reperfusion (i.v.) | tMCAO for 2 h | ↓ infarct volume | 28 days |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
del Río, C.; Montaner, J. Hypoxia Tolerant Species: The Wisdom of Nature Translated into Targets for Stroke Therapy. Int. J. Mol. Sci. 2021, 22, 11131. https://doi.org/10.3390/ijms222011131
del Río C, Montaner J. Hypoxia Tolerant Species: The Wisdom of Nature Translated into Targets for Stroke Therapy. International Journal of Molecular Sciences. 2021; 22(20):11131. https://doi.org/10.3390/ijms222011131
Chicago/Turabian Styledel Río, Carmen, and Joan Montaner. 2021. "Hypoxia Tolerant Species: The Wisdom of Nature Translated into Targets for Stroke Therapy" International Journal of Molecular Sciences 22, no. 20: 11131. https://doi.org/10.3390/ijms222011131
APA Styledel Río, C., & Montaner, J. (2021). Hypoxia Tolerant Species: The Wisdom of Nature Translated into Targets for Stroke Therapy. International Journal of Molecular Sciences, 22(20), 11131. https://doi.org/10.3390/ijms222011131






