Clinical Translationality of KCNJ5 Mutation in Aldosterone Producing Adenoma
Abstract
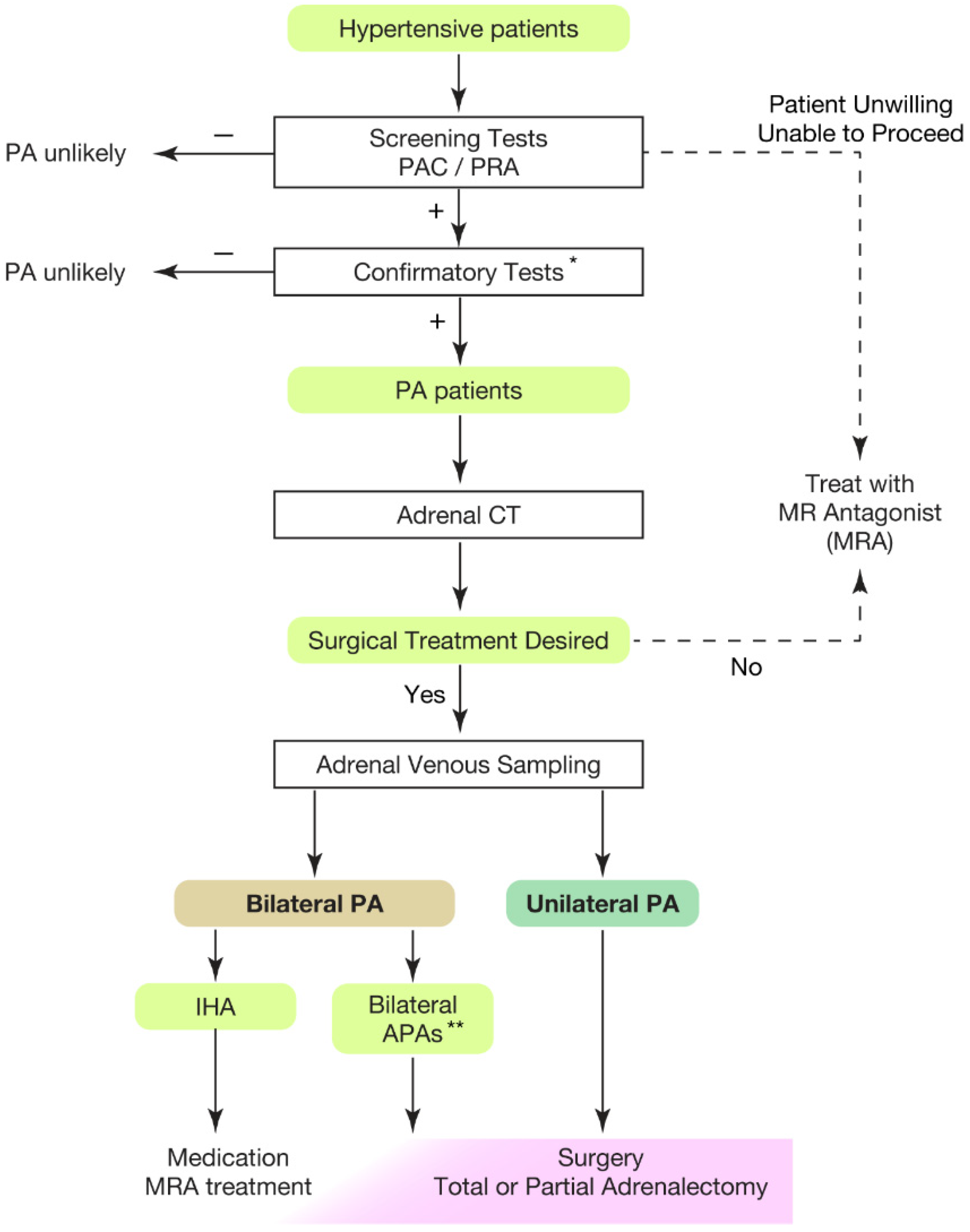
:1. Introduction
2. Cardiovascular Outcome of Primary Aldosteronism
3. Great Progress in Our Pathophysiological Understanding of PA
4. Pathological Insights into PA
5. Clinical Implication of KCNJ5 Somatic Mutation in APA
6. Development of Prediction Model for Somatic KCNJ5 Mutation in PA Patinets
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AVS | Adrenal Venous Sampling |
| PA | Primary Aldosteronism |
| sAVS | Segmental selective AVS |
| IHA | Idiopathic hyperaldosteronism |
| cAVS | Central AVS |
| APA | Aldosterone-producing adenoma |
References
- Gilmour, S.; Liao, Y.; Bilano, V.; Shibuya, K. Burden of disease in Japan: Using national and subnational data to inform local health policy. J. Prev. Med. Public Health 2014, 47, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Sakaue, S.; Gen, F.; Kanai, M.; Karjalainen, J.; Akiyama, M.; Kurki, M.; Matoba, N.; Takahashi, A.; Hirata, M.; Kubo, M.; et al. Trans-biobank analysis with 676,000 individuals elucidates the association of polygenic risk scores of complex traits with human lifespan. Nat. Med. 2020, 26, 542–548. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Umemura, S.; Arima, H.; Arima, S.; Asayama, K.; Dohi, Y.; Hirooka, Y.; Horio, T.; Hoshide, S.; Ikeda, S.; Ishimitsu, T.; et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens. Res. 2019, 42, 1235–1481. [Google Scholar] [PubMed]
- Gordon, R.D.; Ziesak, M.D.; Tunny, T.J.; Stowasser, M.; Klemm, S.A. Evidence that primary aldosteronism may not be uncommon: 12% incidence among antihypertensive drug trial volunteers. Clin. Exp. Pharm. Physiol. 1993, 20, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Sacchetto, A.; Chiesura-Corona, M.; De Toni, R.; Gallina, M.; Feltrin, G.P.; Pessina, A.C. Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: Results in 104 consecutive cases. J. Clin. Endocrinol Metab. 2001, 86, 1083–1090. [Google Scholar] [CrossRef]
- Omura, M.; Saito, J.; Yamaguchi, K.; Kakuta, Y.; Nishikawa, T. Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens. Res. 2004, 27, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Bernini, G.; Caliumi, C.; Desideri, G.; Fabris, B.; Ferri, C.; Ganzaroli, C.; Giacchetti, G.; Letizia, C.; Maccario, M.; et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J. Am. Coll Cardiol. 2006, 48, 2293–2300. [Google Scholar] [CrossRef] [PubMed]
- Monticone, S.; Burrello, J.; Tizzani, D.; Bertello, C.; Viola, A.; Buffolo, F.; Gabetti, L.; Mengozzi, G.; Williams, T.A.; Rabbia, F.; et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J. Am. Coll Cardiol. 2017, 69, 1811–1820. [Google Scholar] [CrossRef] [PubMed]
- Karashima, S.; Kometani, M.; Tsujiguchi, H.; Asakura, H.; Nakano, S.; Usukura, M.; Mori, S.; Ohe, M.; Sawamura, T.; Okuda, R.; et al. Prevalence of primary aldosteronism without hypertension in the general population: Results in Shika study. Clin. Exp. Hypertens. 2018, 40, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.M.; Siddiqui, M.; Calhoun, D.A.; Carey, R.M.; Hopkins, P.N.; Williams, G.H.; Vaidya, A. The Unrecognized Prevalence of Primary Aldosteronism: A Cross-sectional Study. Ann. Intern. Med. 2020, 173, 10–20. [Google Scholar] [CrossRef]
- Funder, J.W. Primary aldosteronism as a public health issue. Lancet Diabetes Endocrinol. 2016, 4, 972–973. [Google Scholar] [CrossRef]
- Mulatero, P.; Monticone, S.; Burrello, J.; Veglio, F.; Williams, T.A.; Funder, J. Guidelines for primary aldosteronism: Uptake by primary care physicians in Europe. J. Hypertens. 2016, 34, 2253–2257. [Google Scholar] [CrossRef]
- Jaffe, G.; Gray, Z.; Krishnan, G.; Stedman, M.; Zheng, Y.; Han, J.; Chertow, G.M.; Leppert, J.T.; Bhalla, V. Screening Rates for Primary Aldosteronism in Resistant Hypertension. Hypertension 2020, 75, 650–659. [Google Scholar] [CrossRef]
- Cohen, J.B.; Cohen, D.L.; Herman, D.S.; Leppert, J.T.; Byrd, J.B.; Bhalla, V. Testing for primary aldosteronism and mineralocorticoid receptor antagonist use among US veterans: A retrospective cohort study. Ann. Intern. Med. 2021, 174, 289–297. [Google Scholar] [CrossRef]
- Gkaniatsa, E.; Ekerstad, E.; Gavric, M.; Muth, A.; Trimpou, P.; Olsson, D.S.; Johannsson, G.; Ragnarsson, O. Increasing Incidence of Primary Aldosteronism in Western Sweden During 3 Decades-Yet An Underdiagnosed Disorder. J. Clin. Endocrinol. Metab. 2021, 106, e3603–e3610. [Google Scholar] [CrossRef]
- Liu, Y.-Y.; King, J.; Kline, G.A.; Padwal, R.S.; Pasieka, J.L.; Chen, G.; So, B.; Harvey, A.; Chin, A.; Leung, A.A. Outcomes of a Specialized Clinic on Rates of Investigation and Treatment of Primary Aldosteronism. JAMA Surg. 2021, 156, 541–549. [Google Scholar] [CrossRef]
- Funder, J.W.; Carey, R.M.; Mantero, F.; Murad, M.H.; Reincke, M.; Shibata, H.; Stowasser, M.; Young, W.F. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2016, 101, 1889–1916. [Google Scholar] [CrossRef] [PubMed]
- Mulatero, P.; Monticone, S.; Deinum, J.; Amar, L.; Prejbisz, A.; Zennaro, M.C.; Beuschlein, F.; Rossi, G.P.; Nishikawa, T.; Morganti, A.; et al. Genetics, prevalence, screening and confirmation of primary aldosteronism: A position statement and consensus of the Working Group on Endocrine Hypertension of The European Society of Hypertension. J. Hypertens. 2020, 38, 1919–1928. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Bisogni, V.; Bacca, A.V.; Belfiore, A.; Cesari, M.; Concistrè, A.; Del Pinto, R.; Fabris, B.; Fallo, F.; Fava, C.; et al. The 2020 Italian Society of Arterial Hypertension (SIIA) practical guidelines for the management of primary aldosteronism. Int. J. Cardiol. Hypertens. 2020, 5, 100029. [Google Scholar] [CrossRef] [PubMed]
- Naruse, M.; Katabami, T.; Shibata, H.; Sone, M.; Takahashi, K.; Tanabe, A.; Izawa, S.; Ichijo, T.; Otsuki, M.; Omura, M.; et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr. J. 2022, 69, 327–359. [Google Scholar] [CrossRef]
- Lubitz, C.C.; Economopoulos, K.P.; Sy, S.; Johanson, C.; Kunzel, H.E.; Reincke, M.; Gazelle, G.S.; Weinstein, M.C.; Gaziano, T.A. Cost-Effectiveness of Screening for Primary Aldosteronism and Subtype Diagnosis in the Resistant Hypertensive Patients. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 621–630. [Google Scholar] [CrossRef]
- Sato, M.; Morimoto, R.; Seiji, K.; Iwakura, Y.; Ono, Y.; Kudo, M.; Satoh, F.; Ito, S.; Ishibashi, T.; Takase, K. Cost-Effectiveness Analysis of the Diagnosis and Treatment of Primary Aldosteronism in Japan. Horm. Metab. Res. 2015, 47, 826–832. [Google Scholar] [CrossRef]
- Nanba, K.; Tsuiki, M.; Nakao, K.; Nanba, A.; Usui, T.; Tagami, T.; Hirokawa, Y.; Okuno, H.; Suzuki, T.; Shimbo, T.; et al. A subtype prediction score for primary aldosteronism. J. Hum. Hypertens. 2014, 28, 716–720. [Google Scholar] [CrossRef]
- Kocjan, T.; Janez, A.; Stankovic, M.; Vidmar, G.; Jensterle, M. A New Clinical Prediction Criterion Accurately Determines A Subset of Patients with Bilateral Primary Aldosteronism Before Adrenal Venous Sampling. Endocr. Pract. 2016, 22, 587–594. [Google Scholar] [CrossRef]
- Kamemura, K.; Wada, N.; Ichijo, T.; Matsuda, Y.; Fujii, Y.; Kai, T.; Fukuoka, T.; Sakamoto, R.; Ogo, A.; Suzuki, T.; et al. Significance of adrenal computed tomography in predicting laterality and indicating adrenal vein sampling in primary aldosteronism. J. Hum. Hypertens. 2017, 31, 195–199. [Google Scholar] [CrossRef]
- Burrello, J.; Burrello, A.; Pieroni, J.; Sconfienza, E.; Forestiero, V.; Rabbia, P.; Adolf, C.; Reincke, M.; Veglio, F.; Williams, T.A.; et al. Development and Validation of Prediction Models for Subtype Diagnosis of Patients With Primary Aldosteronism. J. Clin. Endocrinol. Metab. 2020, 105, e3706–e3717. [Google Scholar] [CrossRef]
- Kempers, M.J.; Lenders, J.W.; Van Outheusden, L.; van der Wilt, G.J.; Kool, L.J.S.; Hermus, A.R.; Deinum, J. Systematic review: Diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann. Intern. Med. 2009, 151, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Crimì, F.; Rossitto, G.; Amar, L.; Azizi, M.; Riester, A.; Reincke, M.; Degenhart, C.; Widimsky, J.; Naruse, M.; et al. Identification of Surgically Curable Primary Aldosteronism by Imaging in a Large, Multiethnic International Study. J. Clin. Endocrinol. Metab. 2021, 106, e4340–e4349. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.-C.; Hu, Y.-H.; Er, L.K.; Yen, R.-F.; Chang, C.-H.; Chang, Y.-L.; Lu, C.-C.; Chang, C.-C.; Lin, J.-H.; Lin, Y.-H.; et al. Case detection and diagnosis of primary aldosteronism-The consensus of Taiwan Society of Aldosteronism. J. Formos. Med. Assoc. 2017, 116, 993–1005. [Google Scholar] [CrossRef] [PubMed]
- Kitamoto, T.; Kitamoto, K.K.; Omura, M.; Takiguchi, T.; Tsurutani, Y.; Kubo, H.; Yamazaki, Y.; Sasano, H.; Saito, J.; Nishikawa, T. Precise Mapping of Intra-Adrenal Aldosterone Activities Provides a Novel Surgical Strategy for Primary Aldosteronism. Hypertension 2020, 76, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Satoh, F.; Morimoto, R.; Seiji, K.; Satani, N.; Ota, H.; Iwakura, Y.; Ono, Y.; Kudo, M.; Nezu, M.; Omata, K.; et al. Is there a role for segmental adrenal venous sampling and adrenal sparing surgery in patients with primary aldosteronism? Eur J. Endocrinol. 2015, 173, 465–477. [Google Scholar] [CrossRef]
- Milliez, P.; Girerd, X.; Plouin, P.F.; Blacher, J.; Safar, M.E.; Mourad, J.J. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J. Am. Coll Cardiol. 2005, 45, 1243–1248. [Google Scholar] [CrossRef]
- Catena, C.; Colussi, G.; Nadalini, E.; Chiuch, A.; Baroselli, S.; Lapenna, R.; Sechi, L.A. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch. Intern. Med. 2008, 168, 80–85. [Google Scholar] [CrossRef]
- Hundemer, G.L.; Curhan, G.C.; Yozamp, N.; Wang, M.; Vaidya, A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: A retrospective cohort study. Lancet Diabetes Endocrinol. 2018, 6, 51–59. [Google Scholar] [CrossRef]
- Monticone, S.; D’Ascenzo, F.; Moretti, C.; Williams, T.A.; Veglio, F.; Gaita, F.; Mulatero, P. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018, 6, 41–50. [Google Scholar] [CrossRef]
- Williams, T.A.; Lenders, J.W.M.; Mulatero, P.; Burrello, J.; Rottenkolber, M.; Adolf, C.; Satoh, F.; Amar, L.; Quinkler, M.; Deinum, J.; et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: An international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017, 5, 689–699. [Google Scholar] [CrossRef]
- Omura, M.; Sasano, H.; Saito, J.; Yamaguchi, K.; Kakuta, Y.; Nishikawa, T. Clinical characteristics of aldosterone-producing microadenoma, macroadenoma, and idiopathic hyperaldosteronism in 93 patients with primary aldosteronism. Hypertens. Res. 2006, 29, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.A.; Gomez-Sanchez, C.E.; Rainey, W.E.; Giordano, T.J.; Lam, A.K.; Marker, A.; Mete, O.; Yamazaki, Y.; Zerbini, M.C.N.; Beuschlein, F.; et al. International Histopathology Consensus for Unilateral Primary Aldosteronism. J. Clin. Endocrinol. Metab. 2021, 106, 42–54. [Google Scholar] [CrossRef] [PubMed]
- Satani, N.; Ota, H.; Seiji, K.; Morimoto, R.; Kudo, M.; Iwakura, Y.; Ono, Y.; Nezu, M.; Omata, K.; Ito, S.; et al. Intra-adrenal Aldosterone Secretion: Segmental Adrenal Venous Sampling for Localization. Radiology 2016, 278, 265–274. [Google Scholar] [CrossRef]
- Makita, K.; Nishimoto, K.; Kiriyama-Kitamoto, K.; Karashima, S.; Seki, T.; Yasuda, M.; Matsui, S.; Omura, M.; Nishikawa, T. A Novel Method: Super-selective Adrenal Venous Sampling. J. Vis. Exp. 2017, 127, e55716. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Sanchez, C.E.; Qi, X.; Velarde-Miranda, C.; Plonczynski, M.W.; Parker, C.R.; Rainey, W.; Satoh, F.; Maekawa, T.; Nakamura, Y.; Sasano, H.; et al. Development of monoclonal antibodies against human CYP11B1 and CYP11B2. Mol. Cell. Endocrinol. 2014, 383, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Maekawa, T.; Felizola, S.J.; Satoh, F.; Qi, X.; Velarde-Miranda, C.; Plonczynski, M.W.; Ise, K.; Kikuchi, K.; Rainey, W.E.; et al. Adrenal CYP11B1/2 expression in primary aldosteronism: Immunohistochemical analysis using novel monoclonal antibodies. Mol. Cell. Endocrinol. 2014, 392, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Meyer, L.S.; Handgriff, L.; Lim, J.S.; Udager, A.M.; Kinker, I.-S.; Ladurner, R.; Wildgruber, M.; Knösel, T.; Bidlingmaier, M.; Rainey, W.E.; et al. Single-Center Prospective Cohort Study on the Histopathology, Genotype, and Postsurgical Outcomes of Patients With Primary Aldosteronism. Hypertension 2021, 78, 738–746. [Google Scholar] [CrossRef]
- Choi, M.; Scholl, U.I.; Yue, P.; Björklund, P.; Zhao, B.; Nelson-Williams, C.; Ji, W.; Cho, Y.; Patel, A.; Men, C.J.; et al. K+ channel mutations in adrenal aldosterone-producing adenomas and hereditary hypertension. Science 2011, 331, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Åkerström, T.; Crona, J.; Verdugo, A.D.; Starker, L.F.; Cupisti, K.; Willenberg, H.S.; Knoefel, W.T.; Saeger, W.; Feller, A.; Ip, J.; et al. Comprehensive re-sequencing of adrenal aldosterone producing lesions reveal three somatic mutations near the KCNJ5 potassium channel selectivity filter. PLoS ONE 2012, 7, e41926. [Google Scholar] [CrossRef] [PubMed]
- Azizan, E.A.; Murthy, M.; Stowasser, M.; Gordon, R.; Kowalski, B.; Xu, S.; Brown, M.J.; O’Shaughnessy, K.M. Somatic mutations affecting the selectivity filter of KCNJ5 are frequent in 2 large unselected collections of adrenal aldosteronomas. Hypertension 2012, 59, 587–591. [Google Scholar] [CrossRef] [PubMed]
- Beuschlein, F.; Boulkroun, S.; Osswald, A.; Wieland, T.; Nielsen, H.N.; Lichtenauer, U.D.; Penton, D.; Schack, V.R.; Amar, L.; Fischer, E.; et al. Somatic mutations in ATP1A1 and ATP2B3 lead to aldosterone-producing adenomas and secondary hypertension. Nat. Genet. 2013, 45, 440–444, 444e1.1–444e.2. [Google Scholar] [CrossRef] [PubMed]
- Scholl, U.I.; Goh, G.; Stolting, G.; De Oliveira, R.C.; Choi, M.; Overton, J.D.; Fonseca, A.L.; Korah, R.; Starker, L.F.; Kunstman, J.; et al. Somatic and germline CACNA1D calcium channel mutations in aldosterone-producing adenomas and primary aldosteronism. Nat. Genet. 2013, 45, 1050–1054. [Google Scholar] [CrossRef]
- Wu, V.-C.; Huang, K.-H.; Peng, K.-Y.; Tsai, Y.-C.; Wu, C.-H.; Wang, S.-M.; Yang, S.-Y.; Lin, L.-Y.; Chang, C.-C.; Lin, Y.-H.; et al. Prevalence and clinical correlates of somatic mutation in aldosterone producing adenoma-Taiwanese population. Sci. Rep. 2015, 5, 11396. [Google Scholar] [CrossRef] [PubMed]
- Zheng, F.-F.; Zhu, L.-M.; Nie, A.-F.; Li, X.-Y.; Lin, J.-R.; Zhang, K.; Chen, J.; Zhou, W.-L.; Shen, Z.-J.; Zhu, Y.-C.; et al. Clinical characteristics of somatic mutations in Chinese patients with aldosterone-producing adenoma. Hypertension 2015, 65, 622–628. [Google Scholar] [CrossRef]
- Kitamoto, T.; Suematsu, S.; Yamazaki, Y.; Nakamura, Y.; Sasano, H.; Matsuzawa, Y.; Saito, J.; Omura, M.; Nishikawa, T. Clinical and Steroidogenic Characteristics of Aldosterone-Producing Adenomas With ATPase or CACNA1D Gene Mutations. J. Clin. Endocrinol. Metab. 2016, 101, 494–503. [Google Scholar] [CrossRef]
- Nanba, K.; Yamazaki, Y.; Bick, N.; Onodera, K.; Tezuka, Y.; Omata, K.; Ono, Y.; Blinder, A.R.; Tomlins, S.A.; Rainey, W.E.; et al. Prevalence of Somatic Mutations in Aldosterone-Producing Adenomas in Japanese Patients. J. Clin. Endocrinol. Metab. 2020, 105, e4066–e4073. [Google Scholar] [CrossRef] [PubMed]
- Boulkroun, S.; Beuschlein, F.; Rossi, G.P.; Golib-Dzib, J.F.; Fischer, E.; Amar, L.; Mulatero, P.; Samson-Couterie, B.; Hahner, S.; Quinkler, M.; et al. Prevalence, clinical, and molecular correlates of KCNJ5 mutations in primary aldosteronism. Hypertension 2012, 59, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.A.; Monticone, S.; Schack, V.R.; Stindl, J.; Burrello, J.; Buffolo, F.; Annaratone, L.; Castellano, I.; Beuschlein, F.; Reincke, M.; et al. Somatic ATP1A1, ATP2B3, and KCNJ5 mutations in aldosterone-producing adenomas. Hypertension 2014, 63, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Lenzini, L.; Rossitto, G.; Maiolino, G.; Letizia, C.; Funder, J.W.; Rossi, G.P. A Meta-Analysis of Somatic KCNJ5 K(+) Channel Mutations In 1636 Patients With an Aldosterone-Producing Adenoma. J. Clin. Endocrinol. Metab. 2015, 100, E1089–E1095. [Google Scholar] [CrossRef]
- Yang, Y.; Gomez-Sanchez, C.E.; Jaquin, D.; Aristizabal Prada, E.T.; Meyer, L.S.; Knösel, T.; Schneider, H.; Beuschlein, F.; Reincke, M.; Williams, T.A. Primary Aldosteronism: KCNJ5 Mutations and Adrenocortical Cell Growth. Hypertension 2019, 74, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Lerario, A.M.; Nanba, K.; Blinder, A.R.; Suematsu, S.; Omura, M.; Nishikawa, T.; Giordano, T.J.; Rainey, W.E.; Else, T. Genetics of aldosterone-producing adenomas with pathogenic KCNJ5 variants. Endocr. Relat. Cancer 2019, 26, 463. [Google Scholar]
- Tamura, A.; Nishimoto, K.; Seki, T.; Matsuzawa, Y.; Saito, J.; Omura, M.; Gomez-Sanchez, C.E.; Makita, K.; Matsui, S.; Moriya, N.; et al. Somatic KCNJ5 mutation occurring early in adrenal development may cause a novel form of juvenile primary aldosteronism. Mol. Cell. Endocrinol. 2017, 441, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Maria, A.G.; Suzuki, M.; Berthon, A.; Kamilaris, C.; Demidowich, A.; Lack, J.; Zilbermint, M.; Hannah-Shmouni, F.; Faucz, F.R.; A Stratakis, C. Mosaicism for KCNJ5 Causing Early-Onset Primary Aldosteronism due to Bilateral Adrenocortical Hyperplasia. Am. J. Hypertens. 2020, 33, 124–130. [Google Scholar] [CrossRef]
- De Sousa, K.; Boulkroun, S.; Baron, S.; Nanba, K.; Wack, M.; Rainey, W.E.; Rocha, A.; Giscos-Douriez, I.; Meatchi, T.; Amar, L.; et al. Genetic, Cellular, and Molecular Heterogeneity in Adrenals with Aldosterone-Producing Adenoma. Hypertension 2020, 75, 1034–1044. [Google Scholar] [CrossRef] [PubMed]
- Spat, A.; Hunyady, L. Control of aldosterone secretion: A model for convergence in cellular signaling pathways. Physiol. Rev. 2004, 84, 489–539. [Google Scholar] [CrossRef]
- Nishimoto, K.; Tomlins, S.A.; Kuick, R.; Cani, A.K.; Giordano, T.J.; Hovelson, D.H.; Liu, C.-J.; Sanjanwala, A.R.; Edwards, M.A.; Gomez-Sanchez, C.E.; et al. Aldosterone-stimulating somatic gene mutations are common in normal adrenal glands. Proc. Natl. Acad. Sci. USA 2015, 112, E4591–E4599. [Google Scholar] [CrossRef]
- Nishimoto, K.; Seki, T.; Hayashi, Y.; Mikami, S.; Al-Eyd, G.; Nakagawa, K.; Morita, S.; Kosaka, T.; Oya, M.; Mitani, F.; et al. Human Adrenocortical Remodeling Leading to Aldosterone-Producing Cell Cluster Generation. Int. J. Endocrinol. 2016, 2016, 1–6. [Google Scholar] [CrossRef]
- Nanba, K.; Vaidya, A.; Williams, G.H.; Zheng, I.; Else, T.; Rainey, W.E. Age-Related Autonomous Aldosteronism. Circulation 2017, 136, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Sanchez, C.E.; Gomez-Sanchez, E.P.; Nishimoto, K. Immunohistochemistry of the Human Adrenal CYP11B2 in Normal Individuals and in Patients with Primary Aldosteronism. Horm. Metab. Res. 2020, 52, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, K.; Nakagawa, K.; Li, D.; Kosaka, T.; Oya, M.; Mikami, S.; Shibata, H.; Itoh, H.; Mitani, F.; Yamazaki, T.; et al. Adrenocortical zonation in humans under normal and pathological conditions. J. Clin. Endocrinol. Metab. 2010, 95, 2296–2305. [Google Scholar] [CrossRef]
- Omata, K.; Anand, S.K.; Hovelson, D.H.; Liu, C.-J.; Yamazaki, Y.; Nakamura, Y.; Ito, S.; Satoh, F.; Sasano, H.; Rainey, W.E.; et al. Aldosterone-Producing Cell Clusters Frequently Harbor Somatic Mutations and Accumulate with Age in Normal Adrenals. J. Endocr. Soc. 2017, 1, 787–799. [Google Scholar] [CrossRef] [PubMed]
- Nanba, K.; Vaidya, A.; Rainey, W.E. Aging and Adrenal Aldosterone Production. Hypertension 2018, 71, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, K.; Seki, T.; Kurihara, I.; Yokota, K.; Omura, M.; Nishikawa, T.; Shibata, H.; Kosaka, T.; Oya, M.; Suematsu, M.; et al. Case Report: Nodule Development From Subcapsular Aldosterone-Producing Cell Clusters Causes Hyperaldosteronism. J. Clin. Endocrinol. Metab. 2016, 101, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Zennaro, M.C.; Boulkroun, S.; Fernandes-Rosa, F. Genetic Causes of Functional Adrenocortical Adenomas. Endocr. Rev. 2017, 38, 516–537. [Google Scholar] [CrossRef]
- Omata, K.; Satoh, F.; Morimoto, R.; Ito, S.; Yamazaki, Y.; Nakamura, Y.; Anand, S.K.; Guo, Z.; Stowasser, M.; Sasano, H.; et al. Cellular and Genetic Causes of Idiopathic Hyperaldosteronism. Hypertension 2018, 72, 874–880. [Google Scholar] [CrossRef]
- Yamazaki, Y.; Nakamura, Y.; Omata, K.; Ise, K.; Tezuka, Y.; Ono, Y.; Morimoto, R.; Nozawa, Y.; Gomez-Sanchez, C.E.; Tomlins, S.A.; et al. Histopathological Classification of Cross-Sectional Image-Negative Hyperaldosteronism. J. Clin. Endocrinol. Metab. 2017, 102, 1182–1192. [Google Scholar] [CrossRef]
- Brown, J.M.; Robinson-Cohen, C.; Luque-Fernandez, M.A.; Allison, M.A.; Baudrand, R.; Ix, J.H.; Kestenbaum, B.; De Boer, I.H.; Vaidya, A. The Spectrum of Subclinical Primary Aldosteronism and Incident Hypertension: A Cohort Study. Ann. Intern. Med. 2017, 167, 630–641. [Google Scholar] [CrossRef] [PubMed]
- Ono, Y.; Yamazaki, Y.; Omata, K.; Else, T.; A Tomlins, S.; Rhayem, Y.; Williams, T.A.; Reincke, M.; Carling, T.; Monticone, S.; et al. Histological Characterization of Aldosterone-producing Adrenocortical Adenomas with Different Somatic Mutations. J. Clin. Endocrinol. Metab. 2019, 105, e282–e289. [Google Scholar] [CrossRef]
- Nakamura, Y.; Kitada, M.; Satoh, F.; Maekawa, T.; Morimoto, R.; Yamazaki, Y.; Ise, K.; Gomez-Sanchez, C.E.; Ito, S.; Arai, Y.; et al. Intratumoral heterogeneity of steroidogenesis in aldosterone-producing adenoma revealed by intensive double-and triple-immunostaining for CYP11B2/B1 and CYP17. Mol. Cell. Endocrinol. 2016, 422, 57–63. [Google Scholar] [CrossRef]
- Tezuka, Y.; Yamazaki, Y.; Kitada, M.; Morimoto, R.; Kudo, M.; Seiji, K.; Takase, K.; Kawasaki, Y.; Mitsuzuka, K.; Ito, A.; et al. 18-Oxocortisol Synthesis in Aldosterone-Producing Adrenocortical Adenoma and Significance of KCNJ5 Mutation Status. Hypertension 2019, 73, 1283–1290. [Google Scholar] [CrossRef]
- Wannachalee, T.; Zhao, L.; Nanba, K.; Nanba, A.T.; Shields, J.J.; E Rainey, W.; Auchus, R.J.; Turcu, A.F. Three Discrete Patterns of Primary Aldosteronism Lateralization in Response to Cosyntropin During Adrenal Vein Sampling. J. Clin. Endocrinol. Metab. 2019, 104, 5867–5876. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Yamazaki, Y.; Kitamoto, T.; Hirose, R.; Saito, J.; Omura, M.; Sasano, H.; Nishikawa, T. Aldosterone Suppression by Dexamethasone in Patients with KCNJ5-Mutated Aldosterone-Producing Adenoma. J. Clin. Endocrinol. Metab. 2018, 103, 3477–3485. [Google Scholar] [CrossRef] [PubMed]
- Sawka, A.M.; Young, W.F.; Thompson, G.B.; Grant, C.S.; Farley, D.R.; Leibson, C.; Van Heerden, J.A. Primary aldosteronism: Factors associated with normalization of blood pressure after surgery. Ann. Intern. Med. 2001, 135, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Letavernier, E.; Peyrard, S.; Amar, L.; Zinzindohoue, F.; Fiquet, B.; Plouin, P.F. Blood pressure outcome of adrenalectomy in patients with primary hyperaldosteronism with or without unilateral adenoma. J. Hypertens. 2008, 26, 1816–1823. [Google Scholar] [CrossRef]
- Mourad, J.J.; Girerd, X.; Milliez, P.; Lopez-Sublet, M.; Lejeune, S.; Safar, M.E. Urinary aldosterone-to-active-renin ratio: A useful tool for predicting resolution of hypertension after adrenalectomy in patients with aldosterone-producing adenomas. Am. J. Hypertens. 2008, 21, 742–747. [Google Scholar] [CrossRef]
- Aronova, A.; Gordon, B.L.; Finnerty, B.M.; Zarnegar, R.; Fahey, T.J., 3rd. Aldosteronoma resolution score predicts long-term resolution of hypertension. Surgery 2014, 156, 1387–1392; discussion 1392-1383. [Google Scholar] [CrossRef]
- Taguchi, R.; Yamada, M.; Nakajima, Y.; Satoh, T.; Hashimoto, K.; Shibusawa, N.; Ozawa, A.; Okada, S.; Rokutanda, N.; Takata, D.; et al. Expression and mutations of KCNJ5 mRNA in Japanese patients with aldosterone-producing adenomas. J. Clin. Endocrinol. Metab. 2012, 97, 1311–1319. [Google Scholar] [CrossRef]
- Kitamoto, T.; Suematsu, S.; Matsuzawa, Y.; Saito, J.; Omura, M.; Nishikawa, T. Comparison of Cardiovascular Complications in Patients with and without KCNJ5 Gene Mutations Harboring Aldosterone-producing Adenomas. J. Atheroscler. Thromb. 2015, 22, 191–200. [Google Scholar] [CrossRef]
- Rossi, G.P.; Cesari, M.; Letizia, C.; Seccia, T.M.; Cicala, M.V.; Zinnamosca, L.; Kuppusamy, M.; Mareso, S.; Sciomer, S.; Iacobone, M.; et al. KCNJ5 gene somatic mutations affect cardiac remodelling but do not preclude cure of high blood pressure and regression of left ventricular hypertrophy in primary aldosteronism. J. Hypertens. 2014, 32, 1514–1521; discussion 1522. [Google Scholar] [CrossRef]
- Kitamoto, T.; Omura, M.; Suematsu, S.; Saito, J.; Nishikawa, T. KCNJ5 mutation as a predictor for resolution of hypertension after surgical treatment of aldosterone-producing adenoma. J. Hypertens. 2018, 36, 619–627. [Google Scholar] [CrossRef]
- Chang, Y.-Y.; Tsai, C.-H.; Peng, S.-Y.; Chen, Z.-W.; Chang, C.-C.; Lee, B.-C.; Liao, C.-W.; Pan, C.-T.; Chen, Y.-L.; Lin, L.-C.; et al. KCNJ5 Somatic Mutations in Aldosterone-Producing Adenoma Are Associated with a Worse Baseline Status and Better Recovery of Left Ventricular Remodeling and Diastolic Function. Hypertension 2021, 77, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Vilela, L.A.P.; Rassi-Cruz, M.; Guimaraes, A.G.; Moises, C.C.S.; Freitas, T.C.; Alencar, N.P.; Petenuci, J.; Goldbaum, T.S.; Maciel, A.A.W.; A Pereira, M.A.; et al. KCNJ5 Somatic Mutation Is a Predictor of Hypertension Remission after Adrenalectomy for Unilateral Primary Aldosteronism. J. Clin. Endocrinol. Metab. 2019, 104, 4695–4702. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.A.; Peitzsch, M.; Dietz, A.S.; Dekkers, T.; Bidlingmaier, M.; Riester, A.; Treitl, M.; Rhayem, Y.; Beuschlein, F.; Lenders, J.W.; et al. Genotype-Specific Steroid Profiles Associated with Aldosterone-Producing Adenomas. Hypertension 2016, 67, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Holler, F.; Heinrich, D.A.; Adolf, C.; Lechner, B.; Bidlingmaier, M.; Eisenhofer, G.; Williams, T.A.; Reincke, M. Steroid Profiling and Immunohistochemistry for Subtyping and Outcome Prediction in Primary Aldosteronism-a Review. Curr. Hypertens. Rep. 2019, 21, 77. [Google Scholar] [CrossRef] [PubMed]
- Eisenhofer, G.; Durán, C.; Cannistraci, C.V.; Peitzsch, M.; Williams, T.A.; Riester, A.; Burrello, J.; Buffolo, F.; Prejbisz, A.; Beuschlein, F.; et al. Use of Steroid Profiling Combined with Machine Learning for Identification and Subtype Classification in Primary Aldosteronism. JAMA Netw. Open 2020, 3, e2016209. [Google Scholar] [CrossRef] [PubMed]
- Tauber, P.; Penton, D.; Stindl, J.; Humberg, E.; Tegtmeier, I.; Sterner, C.; Beuschlein, F.; Reincke, M.; Barhanin, J.; Bandulik, S.; et al. Pharmacology and pathophysiology of mutated KCNJ5 found in adrenal aldosterone-producing adenomas. Endocrinology 2014, 155, 1353–1362. [Google Scholar] [CrossRef]
- Xie, C.B.; Shaikh, L.H.; Garg, S.; Tanriver, G.; Teo, A.E.D.; Zhou, J.; Maniero, C.; Zhao, W.; Kang, S.; Silverman, R.B.; et al. Regulation of aldosterone secretion by Cav1.3. Sci. Rep. 2016, 6, 24697. [Google Scholar] [CrossRef]
- Caroccia, B.; Prisco, S.; Seccia, T.M.; Piazza, M.; Maiolino, G.; Rossi, G.P. Macrolides Blunt Aldosterone Biosynthesis: A Proof-of-Concept Study in KCNJ5 Mutated Adenoma Cells Ex Vivo. Hypertension 2017, 70, 1238–1242. [Google Scholar] [CrossRef]
- Scholl, U.I.; Abriola, L.; Zhang, C.; Reimer, E.N.; Plummer, M.; Kazmierczak, B.I.; Zhang, J.; Hoyer, D.; Merkel, J.S.; Wang, W.; et al. Macrolides selectively inhibit mutant KCNJ5 potassium channels that cause aldosterone-producing adenoma. J. Clin. Investig. 2017, 127, 2739–2750. [Google Scholar] [CrossRef]
- Wang, F.; Ma, X.; Tong, A.; Zhang, Y.; Wen, J.; Li, Y. The Effects of Different Calcium Channel Blockers on Aldosterone-Producing Adenoma Cells. Front. Endocrinol. 2020, 11, 260. [Google Scholar] [CrossRef]
- Maiolino, G.; Ceolotto, G.; Battistel, M.; Barbiero, G.; Cesari, M.; Amar, L.; Caroccia, B.; Padrini, R.; Azizi, M.; Rossi, G.P. Macrolides for KCNJ5–mutated aldosterone-producing adenoma (MAPA): Design of a study for personalized diagnosis of primary aldosteronism. Blood Press. 2018, 27, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Buffolo, F.; Burrello, J.; Burrello, A.; Heinrich, D.; Adolf, C.; Müller, L.M.; Chen, R.; Forestiero, V.; Sconfienza, E.; Tetti, M.; et al. Clinical Score and Machine Learning-Based Model to Predict Diagnosis of Primary Aldosteronism in Arterial Hypertension. Hypertension 2021, 78, 1595–1604. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, H.; Umakoshi, H.; Ogata, M.; Wada, N.; Iwahashi, N.; Fukumoto, T.; Yokomoto-Umakoshi, M.; Nakano, Y.; Matsuda, Y.; Miyazawa, T.; et al. Machine learning based models for prediction of subtype diagnosis of primary aldosteronism using blood test. Sci. Rep. 2021, 11, 9140. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitamoto, T.; Nishikawa, T. Clinical Translationality of KCNJ5 Mutation in Aldosterone Producing Adenoma. Int. J. Mol. Sci. 2022, 23, 9042. https://doi.org/10.3390/ijms23169042
Kitamoto T, Nishikawa T. Clinical Translationality of KCNJ5 Mutation in Aldosterone Producing Adenoma. International Journal of Molecular Sciences. 2022; 23(16):9042. https://doi.org/10.3390/ijms23169042
Chicago/Turabian StyleKitamoto, Takumi, and Tetsuo Nishikawa. 2022. "Clinical Translationality of KCNJ5 Mutation in Aldosterone Producing Adenoma" International Journal of Molecular Sciences 23, no. 16: 9042. https://doi.org/10.3390/ijms23169042
APA StyleKitamoto, T., & Nishikawa, T. (2022). Clinical Translationality of KCNJ5 Mutation in Aldosterone Producing Adenoma. International Journal of Molecular Sciences, 23(16), 9042. https://doi.org/10.3390/ijms23169042





