Pharmacogenomic Profiling of Cisplatin-Resistant and -Sensitive Human Osteosarcoma Cell Lines by Multimodal Targeted Next Generation Sequencing
Abstract
:1. Introduction
2. Results
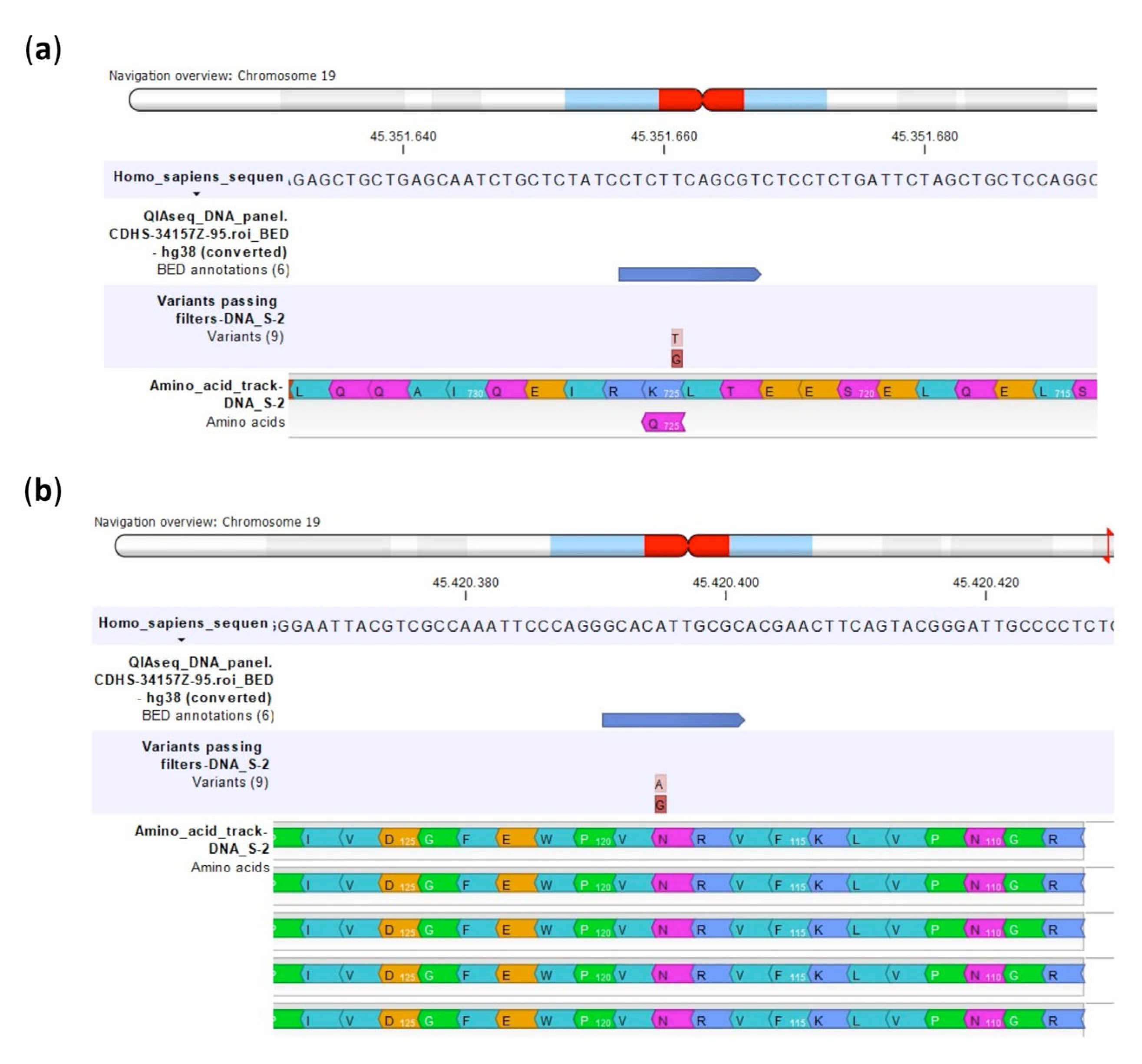
2.1. Validation of Custom Multimodal NGS Panel
2.2. DNA SNP Evaluation in Relation to Level of CDDP Resistance
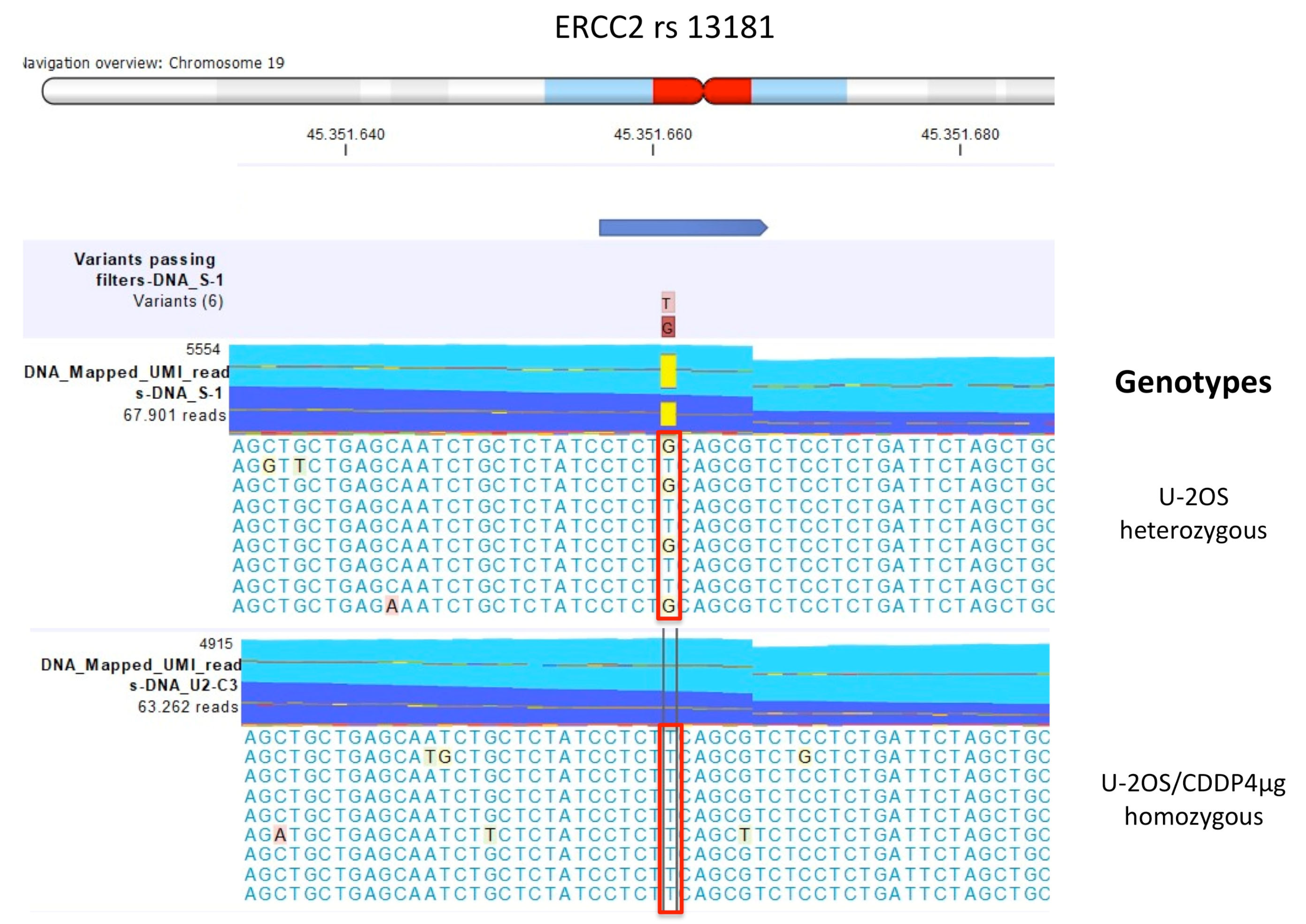
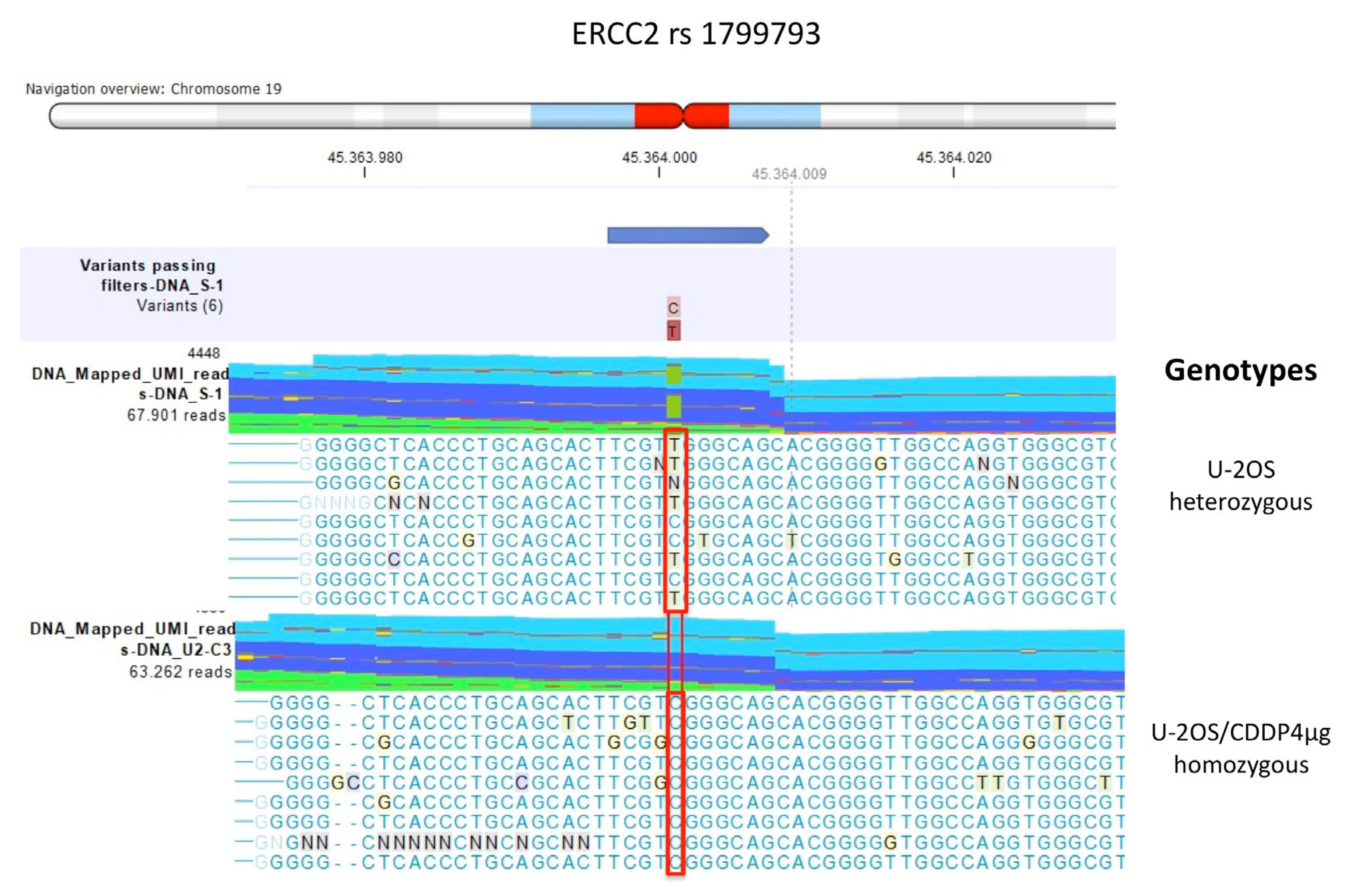
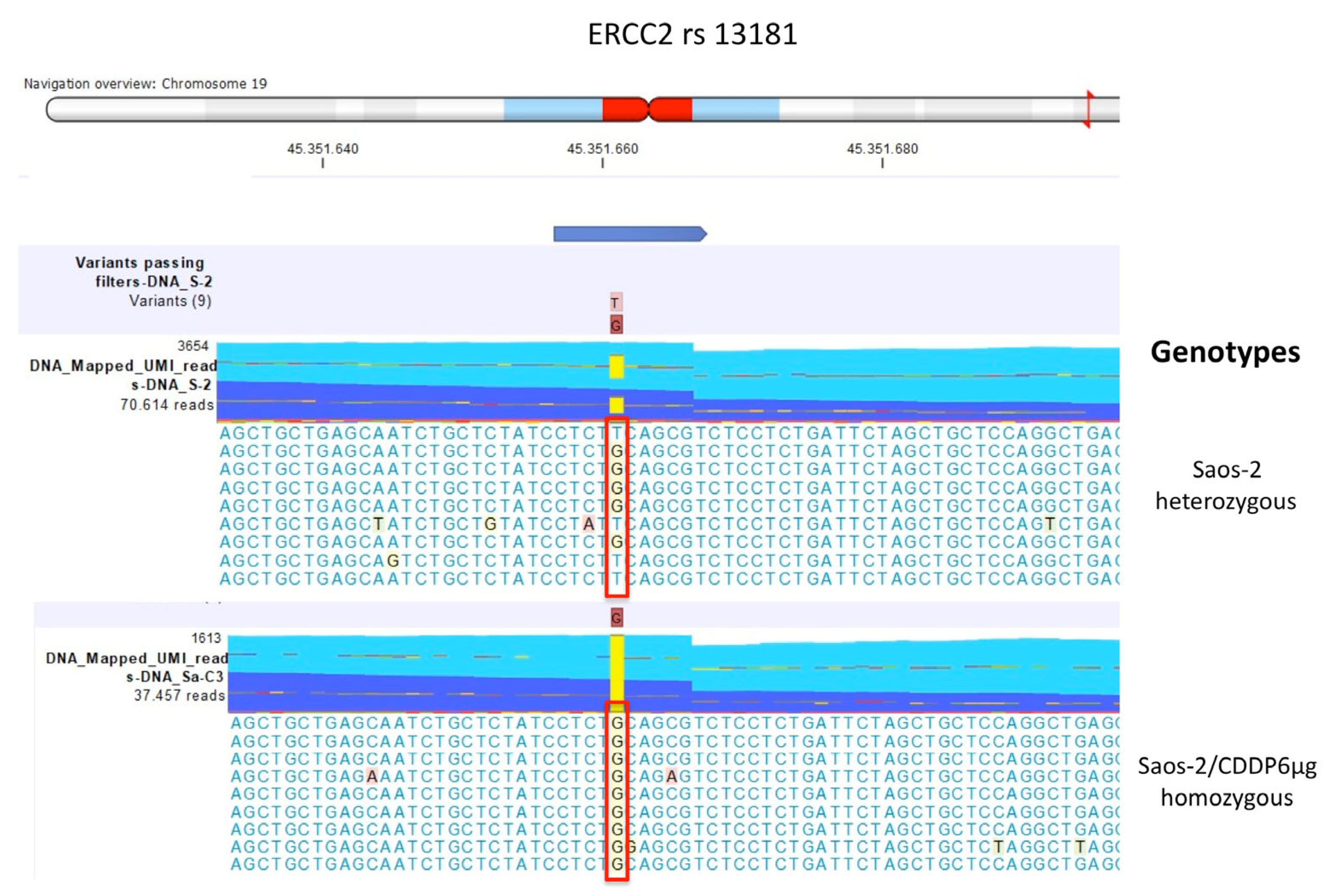
2.2.1. Comparison between U-2OS CDDP-Resistant Variants to Parental U-2OS Cell Line
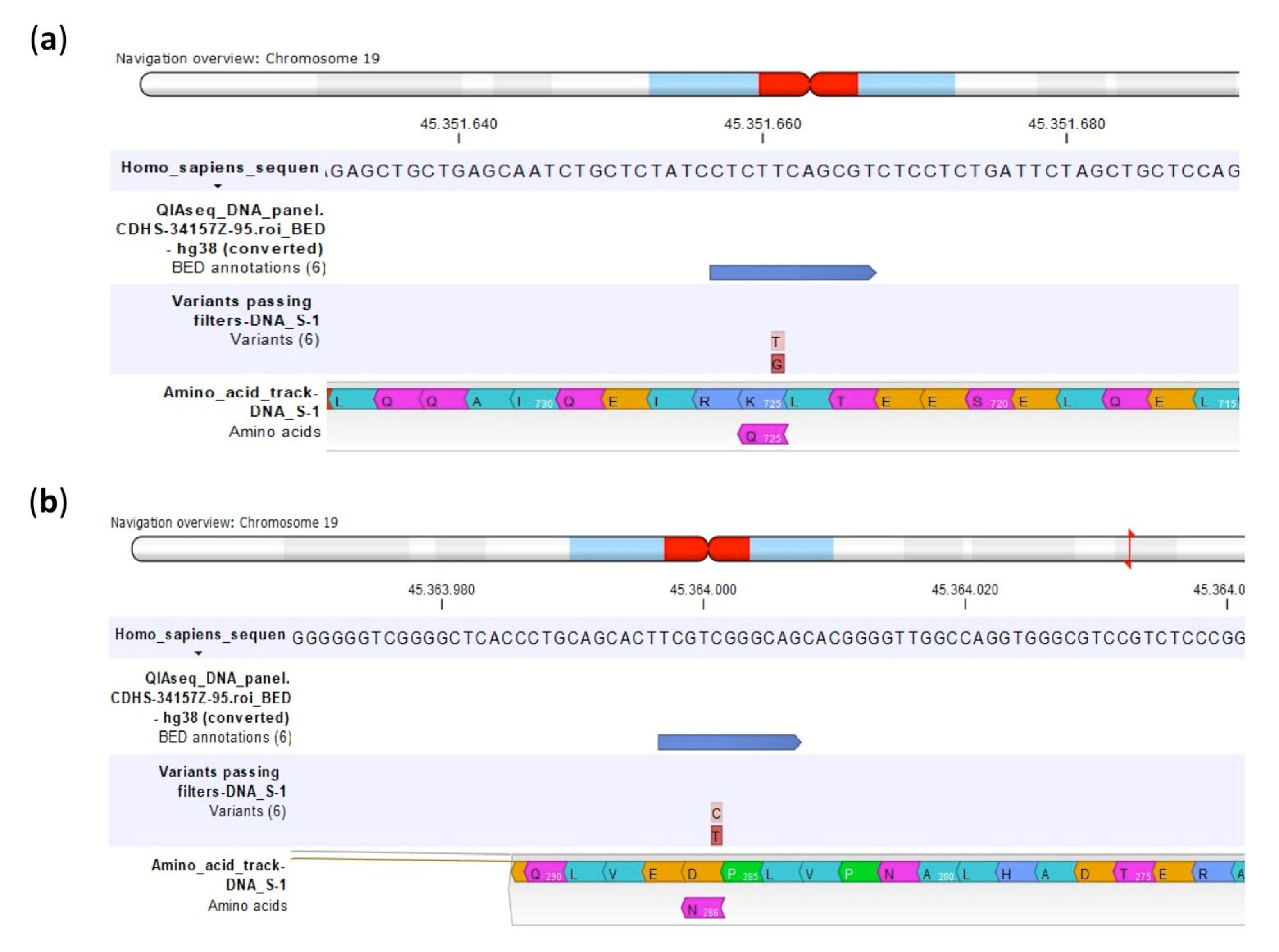
2.2.2. Comparison between Saos-2 CDDP-Resistant Variants to Parental Saos-2 Cell Line
2.3. RNA SNP Evaluation in Relation to Level of CDDP Resistance
2.3.1. Comparison between U-2OS Cell Line and U-2OS CDDP-Resistant Variants
2.3.2. Comparison between Saos-2 Cell Line and Saos-2 CDDP-Resistant Variants
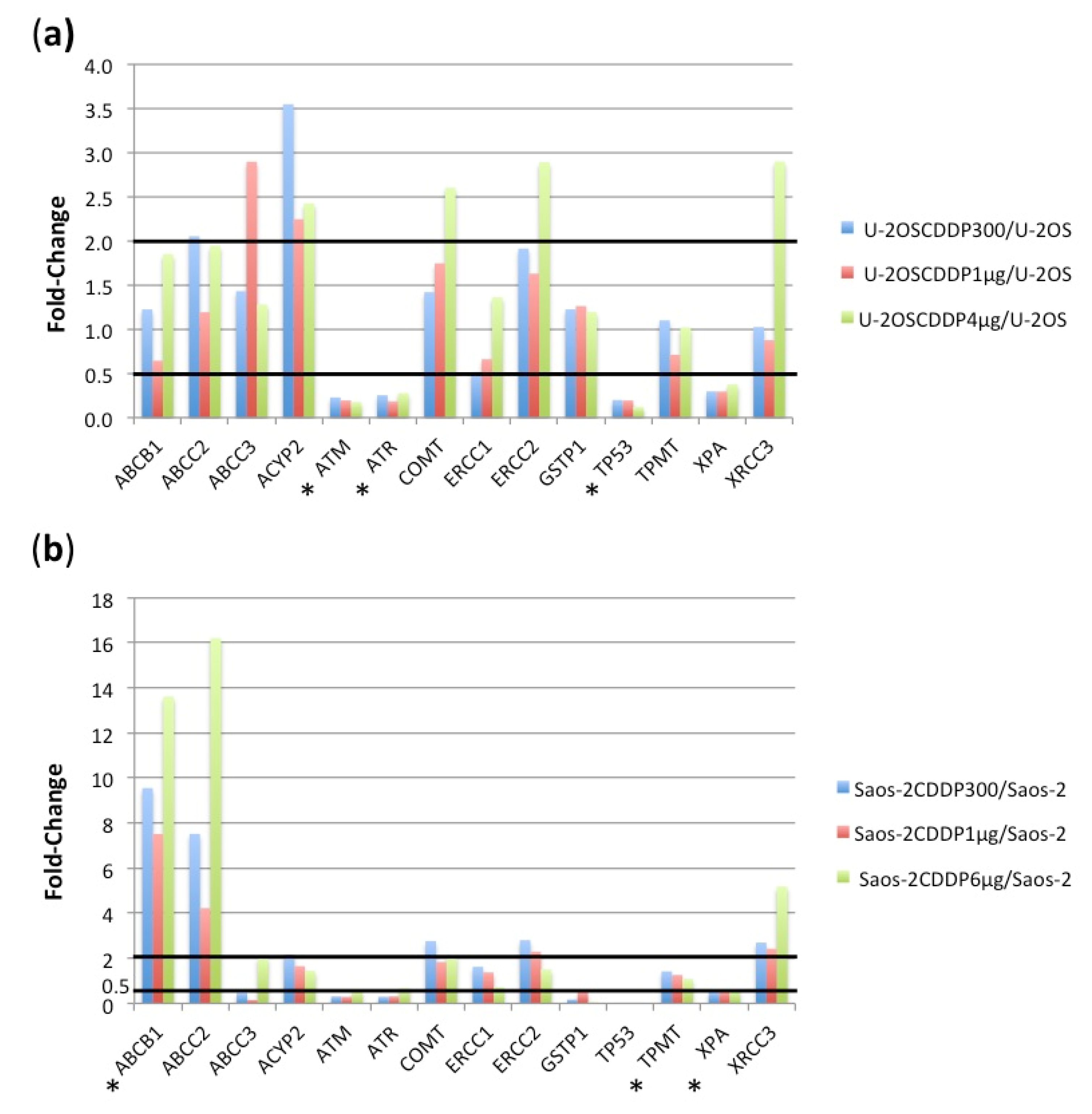
2.4. RNA Expression Analysis
3. Discussion
4. Materials and Methods
4.1. Cell Lines
4.2. Extraction of Nucleic Acids
4.3. Custom Multi-Modal Targeted Next Generation Sequencing (mmNGS)
4.4. mmNGS Data Analysis by CLC Genomics Workbench
4.5. SNP Genotyping by Real-Time PCR
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ABCB1 | ATP Binding Cassette Subfamily B Member 1 |
| ABCC2 | ATP Binding Cassette Subfamily C Member 2 |
| ABCC3 | ATP Binding Cassette Subfamily C Member 3 |
| ACYP2 | Acylphosphatase 2 |
| ATM | ATM Serine/Threonine Kinase |
| ATR | ATR Serine/Threonine Kinase |
| CDDP | Cisplatin |
| CLC GWB | CLC Genomics Workbench |
| COMT | Cathechol-O-Methyltransferase |
| ERCC1 | Excision Repair Cross-Complementing 1, Endonuclease Non-Catalytic Subunit |
| ERCC2 | Excision Repair Cross-Complementing 2, TFIIH Core Complex Helicase Subunit |
| GSTP1 | Glutathione S-Transferase Pi 1 |
| HGOS | High-Grade Osteosarcoma |
| IMDM | Iscove’s modified Dulbecco’s medium |
| mmNGS | Multimodal Targeted Next Generation Sequencing |
| MNV | Multi Nucleotide Variant |
| NER | Nucleotide Excision Repair |
| SNP | Single Nucleotide Polymorphism |
| TP53 | Tumor Protein P53 |
| TPM | Transcripts per Million |
| TPMT | Thiopurine S-Methyltransferase |
| UMI | Unique Molecular Indices |
| VAF | Variant Allele Frequency |
| XPA | XPA, DNA Damage Recognition and Repair Factor |
| XRCC3 | X-Ray Repair Cross Complementing 3 |
Appendix A
| Gene Name | Abbreviation | Function |
|---|---|---|
| ATP Binding Cassette Subfamily B Member 1 | ABCB1 | CDDP transport |
| ATP Binding Cassette Subfamily C Member 2 | ABCC2 | CDDP transport |
| ATP Binding Cassette Subfamily C Member 3 | ABCC3 | CDDP-related ototoxicity |
| Acylphosphatase 2 | ACYP2 | CDDP-related ototoxicity |
| ATM Serine/Threonine Kinase | ATM | DNA repair |
| ATR Serine/Threonine Kinase | ATR | DNA repair |
| Cathecol-O-Methyltransferase | COMT | CDDP-related ototoxicity |
| Excision Repair Cross-Complementing 1 | ERCC1 | DNA repair |
| Excision Repair Cross-Complementing 2 | ERCC2 | DNA repair |
| Glutathione S-Transferase P1 | GSTP1 | CDDP detoxification |
| Tumor Protein 53 | TP53 | Genomic stability |
| Thiopurine S-methyltransferase | TPMT | CDDP-related ototoxicity |
| Xeroderma pigmentosum group A | XPA | DNA repair |
| X-Ray Repair Cross Complementing 3 | XRCC3 | DNA repair |
| Gene_Reference Number | Assay ID | Assay Type | Reference Allele |
|---|---|---|---|
| ABCB1_rs1045642 | C___7586657_20 | DME | A |
| ABCB1_rs2032582 | C_11711720C_30 + C_11711720D_40 | DME | A |
| ABCB1_rs1128503 | C___7586662_10 | DME | A |
| ABCC2_rs717620 | C___2814642_10 | DME | T |
| ABCC2_rs2273697 | C__22272980_20 | DME | C |
| ABCC2_rs3740066 | C__11214910_20 | DME | G |
| ABCC2_rs17222723 | C__25591743_30 | DME | T |
| ABCC3_rs4793665 | Not done | Not done | C |
| ABCC3_rs1051640 | Not done | Not done | A |
| ACYP2_rs1872328 | C__11643398_10 | Funct. tested | G |
| ATM_rs664677 | C___2283171_1_ | Validated | C |
| ATM_rs664143 | C___1039783_10 | Validated | A |
| ATR_rs2229032 | C__26021082_10 | Funct. tested | C |
| ATR_rs2227928 | C____157700_10 | Validated | A |
| COMT_rs4646316 | C__29193982_10 | Funct. tested | C |
| COMT_rs9332377 | Not done | Not done | C |
| ERCC1_rs11615 | C___2532959_1_ | Validated | A |
| ERCC1_rs3212986 | Not done | Not done | C |
| ERCC2_rs13181 | C___3145033_10 | Validated | T |
| ERCC2_rs1799793 | C___3145050_10 | Funct. tested | C |
| GSTP1_rs1695 | C___3237198_20 | DME | A |
| TP53_rs1042522 | C___2403545_10 | Funct. tested | G |
| TP53_rs1642785 | C___2880090_10 | Funct. tested | G |
| TPMT_rs12201199 | C__31923406_10 | Funct. tested | A |
| TPMT_rs1142345 | C_____19567_20 | DME | T |
| TPMT_rs1800460 | C__30634116_20 | DME | C |
| XPA_rs1800975 | C____482935_1_ | Validated | T |
| XRCC3_rs861539 | C___8901525_10 | Funct. tested | G |
References
- Harrison, D.J.; Geller, D.S.; Gill, J.D.; Lewis, V.O.; Gorlick, R. Current and future therapeutic approaches for osteosarcoma. Expert Rev. Anticancer Ther. 2018, 18, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Lilienthal, I.; Herold, N. Targeting Molecular Mechanisms Underlying Treatment Efficacy and Resistance in Osteosarcoma: A Review of Current and Future Strategies. Int. J. Mol. Sci. 2020, 21, 6885. [Google Scholar] [CrossRef] [PubMed]
- Hattinger, C.M.; Patrizio, M.P.; Luppi, S.; Serra, M. Pharmacogenomics and Pharmacogenetics in Osteosarcoma: Translational Studies and Clinical Impact. Int. J. Mol. Sci. 2020, 21, 4659. [Google Scholar] [CrossRef] [PubMed]
- Roden, D.M.; McLeod, H.L.; Relling, M.V.; Williams, M.S.; Mensah, G.A.; Peterson, J.F.; Van Driest, S.L. Pharmacogenomics. Lancet 2019, 394, 521–532. [Google Scholar] [CrossRef]
- Kager, L.; Tamamyan, G.; Bielack, S. Novel insights and therapeutic interventions for pediatric osteosarcoma. Future Oncol. 2017, 13, 357–368. [Google Scholar] [CrossRef]
- Serra, M.; Hattinger, C.M. The pharmacogenomics of osteosarcoma. Pharmacogenomics J. 2017, 17, 11–20. [Google Scholar] [CrossRef]
- Vos, H.I.; Guchelaar, H.J.; Gelderblom, H.; de Bont, E.S.; Kremer, L.C.; Naber, A.M.; Hakobjan, M.H.; van der Graaf, W.T.; Coenen, M.J.; te Loo, D.M. Replication of a genetic variant in ACYP2 associated with cisplatin-induced hearing loss in patients with osteosarcoma. Pharmacogenet. Genomics 2016, 26, 243–247. [Google Scholar] [CrossRef]
- Windsor, R.E.; Strauss, S.J.; Kallis, C.; Wood, N.E.; Whelan, J.S. Germline genetic polymorphisms may influence chemotherapy response and disease outcome in osteosarcoma: A pilot study. Cancer 2012, 118, 1856–1867. [Google Scholar] [CrossRef]
- Ross, C.J.; Katzov-Eckert, H.; Dube, M.P.; Brooks, B.; Rassekh, S.R.; Barhdadi, A.; Feroz-Zada, Y.; Visscher, H.; Brown, A.M.; Rieder, M.J.; et al. Genetic variants in TPMT and COMT are associated with hearing loss in children receiving cisplatin chemotherapy. Nat. Genet. 2009, 41, 1345–1349. [Google Scholar] [CrossRef]
- Pussegoda, K.; Ross, C.J.; Visscher, H.; Yazdanpanah, M.; Brooks, B.; Rassekh, S.R.; Zada, Y.F.; Dube, M.P.; Carleton, B.C.; Hayden, M.R.; et al. Replication of TPMT and ABCC3 genetic variants highly associated with cisplatin-induced hearing loss in children. Clin. Pharmacol. Ther. 2013, 94, 243–251. [Google Scholar] [CrossRef]
- Hagleitner, M.M.; Coenen, M.J.; Patino-Garcia, A.; de Bont, E.S.; Gonzalez-Neira, A.; Vos, H.I.; van Leeuwen, F.N.; Gelderblom, H.; Hoogerbrugge, P.M.; Guchelaar, H.J.; et al. Influence of genetic variants in TPMT and COMT associated with cisplatin induced hearing loss in patients with cancer: Two new cohorts and a meta-analysis reveal significant heterogeneity between cohorts. PLoS ONE 2014, 9, e115869. [Google Scholar] [CrossRef] [Green Version]
- Pasello, M.; Michelacci, F.; Scionti, I.; Hattinger, C.M.; Zuntini, M.; Caccuri, A.M.; Scotlandi, K.; Picci, P.; Serra, M. Overcoming glutathione S-transferase P1-related cisplatin resistance in osteosarcoma. Cancer Res. 2008, 68, 6661–6668. [Google Scholar] [CrossRef] [Green Version]
- Li, J.Z.; Tian, Z.Q.; Jiang, S.N.; Feng, T. Effect of variation of ABCB1 and GSTP1 on osteosarcoma survival after chemotherapy. Genet. Mol. Res. 2014, 13, 3186–3192. [Google Scholar] [CrossRef]
- Liu, S.; Yi, Z.; Ling, M.; Shi, J.; Qiu, Y.; Yang, S. Predictive potential of ABCB1, ABCC3, and GSTP1 gene polymorphisms on osteosarcoma survival after chemotherapy. Tumour Biol. 2014, 35, 9897–9904. [Google Scholar] [CrossRef]
- Teng, J.W.; Yang, Z.M.; Li, J.; Xu, B. Predictive role of Glutathione S-transferases (GSTs) on the prognosis of osteosarcoma patients treated with chemotherapy. Pak. J. Med. Sci. 2013, 29, 1182–1186. [Google Scholar] [CrossRef]
- Zhang, S.L.; Mao, N.F.; Sun, J.Y.; Shi, Z.C.; Wang, B.; Sun, Y.J. Predictive potential of glutathione S-transferase polymorphisms for prognosis of osteosarcoma patients on chemotherapy. Asian Pac. J. Cancer Prev. 2012, 13, 2705–2709. [Google Scholar] [CrossRef] [Green Version]
- Yang, L.M.; Li, X.H.; Bao, C.F. Glutathione S-transferase P1 and DNA polymorphisms influence response to chemotherapy and prognosis of bone tumors. Asian Pac. J. Cancer Prev. 2012, 13, 5883–5886. [Google Scholar] [CrossRef] [Green Version]
- Goricar, K.; Kovac, V.; Jazbec, J.; Zakotnik, B.; Lamovec, J.; Dolzan, V. Genetic variability of DNA repair mechanisms and glutathione-S-transferase genes influences treatment outcome in osteosarcoma. Cancer Epidemiol. 2015, 39, 182–188. [Google Scholar] [CrossRef]
- Cao, Z.H.; Yin, H.P.; Jiang, N.; Yu, B. Association between ERCC1 and ERCC2 gene polymorphisms and chemotherapy response and overall survival in osteosarcoma. Genet. Mol. Res. 2015, 14, 10145–10151. [Google Scholar] [CrossRef]
- Ji, W.P.; He, N.B. Investigation on the DNA repaired gene polymorphisms and response to chemotherapy and overall survival of osteosarcoma. Int. J. Clin. Exp. Pathol. 2015, 8, 894–899. [Google Scholar]
- Sun, Y.; Wu, Y.; Li, W.; Kong, Z.; Zou, X. Genetic polymorphisms in nucleotide excision repair pathway influences response to chemotherapy and overall survival in osteosarcoma. Int. J. Clin. Exp. Pathol. 2015, 8, 7905–7912. [Google Scholar]
- Zhang, H.; Ge, J.; Hong, H.; Bi, L.; Sun, Z. Genetic polymorphisms in ERCC1 and ERCC2 genes are associated with response to chemotherapy in osteosarcoma patients among Chinese population: A meta-analysis. World J. Surg. Oncol. 2017, 15, 75. [Google Scholar] [CrossRef]
- Zhang, Q.; Lv, L.Y.; Li, B.J.; Zhang, J.; Wei, F. Investigation of ERCC1 and ERCC2 gene polymorphisms and response to chemotherapy and overall survival in osteosarcoma. Genet. Mol. Res. 2015, 14, 11235–11241. [Google Scholar] [CrossRef]
- Hao, T.; Feng, W.; Zhang, J.; Sun, Y.J.; Wang, G. Association of four ERCC1 and ERCC2 SNPs with survival of bone tumour patients. Asian Pac. J. Cancer Prev. 2012, 13, 3821–3824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, M.J.; Zhu, Y.; Guo, X.J.; Tian, Z.Z. Genetic variability of genes involved in DNA repair influence treatment outcome in osteosarcoma. Genet. Mol. Res. 2015, 14, 11652–11657. [Google Scholar] [CrossRef] [PubMed]
- Obiedat, H.; Alrabadi, N.; Sultan, E.; Al Shatti, M.; Zihlif, M. The effect of ERCC1 and ERCC2 gene polymorphysims on response to cisplatin based therapy in osteosarcoma patients. BMC Med. Genet. 2018, 19, 112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caronia, D.; Patino-Garcia, A.; Milne, R.L.; Zalacain-Diez, M.; Pita, G.; Alonso, M.R.; Moreno, L.T.; Sierrasesumaga-Ariznabarreta, L.; Benitez, J.; Gonzalez-Neira, A. Common variations in ERCC2 are associated with response to cisplatin chemotherapy and clinical outcome in osteosarcoma patients. Pharmacogenomics J. 2009, 9, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Biason, P.; Hattinger, C.M.; Innocenti, F.; Talamini, R.; Alberghini, M.; Scotlandi, K.; Zanusso, C.; Serra, M.; Toffoli, G. Nucleotide excision repair gene variants and association with survival in osteosarcoma patients treated with neoadjuvant chemotherapy. Pharmacogenomics J. 2012, 12, 476–483. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Liu, S.; Wang, W.; Zhang, K.; Liu, Z.; Zhang, C.; Chen, S.; Wu, S. ERCC polymorphisms and prognosis of patients with osteosarcoma. Tumour Biol. 2014, 35, 10129–10136. [Google Scholar] [CrossRef]
- Pasqui, A.; Boddi, A.; Campanacci, D.A.; Scoccianti, G.; Bernini, A.; Grasso, D.; Gambale, E.; Scolari, F.; Palchetti, I.; Palomba, A.; et al. Alteration of the Nucleotide Excision Repair (NER) Pathway in Soft Tissue Sarcoma. Int. J. Mol. Sci. 2022, 23, 8360. [Google Scholar] [CrossRef]
- Peissert, S.; Sauer, F.; Grabarczyk, D.B.; Braun, C.; Sander, G.; Poterszman, A.; Egly, J.M.; Kuper, J.; Kisker, C. In TFIIH the Arch domain of XPD is mechanistically essential for transcription and DNA repair. Nat. Commun. 2020, 11, 1667. [Google Scholar] [CrossRef] [Green Version]
- Kiss, R.C.; Xia, F.; Acklin, S. Targeting DNA Damage Response and Repair to Enhance Therapeutic Index in Cisplatin-Based Cancer Treatment. Int. J. Mol. Sci. 2021, 22, 8199. [Google Scholar] [CrossRef]
- Rocha, C.R.R.; Silva, M.M.; Quinet, A.; Cabral-Neto, J.B.; Menck, C.F.M. DNA repair pathways and cisplatin resistance: An intimate relationship. Clinics 2018, 73, e478s. [Google Scholar] [CrossRef]
- Benini, S.; Baldini, N.; Manara, M.C.; Chano, T.; Serra, M.; Rizzi, S.; Lollini, P.L.; Picci, P.; Scotlandi, K. Redundancy of autocrine loops in human osteosarcoma cells. Int. J. Cancer 1999, 80, 581–588. [Google Scholar] [CrossRef]


| Polymorphism | U-2OS | Saos-2 | IOR/OS9 | IOR/OS10 | IOR/OS14 | IOR/OS15 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | |
| ABCB1 rs1045642 | GA | GA | GA | GA | GA | GA | GG | GG | GG | GG | ||
| ABCB1 rs2032582 | CA | CA | CA | CA | CA | CA | CA | CA | CC | CC | CC | CC |
| ABCB1 rs1128503 | GG | GG | GA | GA | GA | GA | GA | GA | GG | GG | GG | GG |
| ABCC2 rs717620 | CT | CT | ||||||||||
| ABCC2 rs2273697 | GA | GA | AA | AA | ||||||||
| ABCC2 rs3740066 | CT | CT | TT | TT | TT | TT | ||||||
| ABCC2 rs17222723 | ||||||||||||
| ABCC3 rs4793665 | / | CT | / | TT | / | TC | ||||||
| ABCC3 rs1051640 | ||||||||||||
| ACYP2 rs1872328 | ||||||||||||
| ATM rs664677 | TT | TT | CT | CT | TT | TT | TT | TT | TT | TT | ||
| ATM C11orf65 rs664143 | GG | GG | GA | GA | GG | GG | GG | GG | GG | GG | ||
| ATR rs2229032 | TT | TT | ||||||||||
| ATR rs2227928 | GA | GA | GG | GG | GG | GG | GG/GA | GA | ||||
| COMT rs4646316 | TT | TT | TT | TT | CT | CT | ||||||
| COMT rs9332377 | ||||||||||||
| ERCC1 rs11615 | GA | GA | GA | GA | GA | GA | GG | GA | ||||
| ERCC1 rs3212986 | / | AC | / | AC | ||||||||
| ERCC2 rs13181 | GT | GT | GT | GT | GT | GT | GT | GT | GT | GT | GG | GG |
| ERCC2 rs1799793 | CT | CT | TT | TT | CT | CT | CC | TT | ||||
| GSTP1 rs1695 | AG | AG | AG | AG | AG | AG | AG | AG | ||||
| TP53 rs1042522 | CC | CC | CC | CC | ||||||||
| TP53 rs1642785 | CC | CC | ||||||||||
| TPMT rs12201199 | ||||||||||||
| TPMT rs1142345 | ||||||||||||
| TPMT rs1800460 | ||||||||||||
| XPA rs1800975 | CT | CC | CT | CT | CC | CC | CC | CC | ||||
| XRCC3;KLC1 rs861539 | AG | AG | AA | AA | AA | AA | GG | AG | AA | AA | ||
| Polymorphism | IOR/OS18 | IOR/OS20 | IOR/MOS | IOR/SARG | HOS | MG-63 | ||||||
| TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | |
| ABCB1 rs1045642 | GA | GA | GG | GG | GG | GA | GG | GG | ||||
| ABCB1 rs2032582 | CA | CA | CC | CC | CC | CC | CC | CC | ||||
| ABCB1 rs1128503 | GA | GA | GG | GG | GG | GG | GG | GG | ||||
| ABCC2 rs717620 | CT | CT | CT | CT | ||||||||
| ABCC2 rs2273697 | AA | AA | GA | GA | ||||||||
| ABCC2 rs3740066 | CT | CT | CT | CT | CT | CT | ||||||
| ABCC2 rs17222723 | ||||||||||||
| ABCC3 rs4793665 | / | TC | / | TC | / | CT | / | CT | / | TT | / | CT |
| ABCC3 rs1051640 | / | GA | / | GA | ||||||||
| ACYP2 rs1872328 | ||||||||||||
| ATM rs664677 | CT | CT | TT | TT | CT | CT | TT | TT | TT | TT | TT | TT |
| ATM;C11orf65 rs664143 | GA | GA | GG | GG | GA | GA | GG | GG | GG | GG | GG | GG |
| ATR rs2229032 | CT | CT | CT | CT | TT | TT | ||||||
| ATR rs2227928 | GG | GG | GG | GG | GG | GG | GG | GG | GG | GG | ||
| COMT rs4646316 | CT | CT | ||||||||||
| COMT rs9332377 | / | TT | ||||||||||
| ERCC1 rs11615 | GG | GG | GG | GG | GG | GG | GA | GA | ||||
| ERCC1 rs3212986 | / | AA | / | AC | / | AC | ||||||
| ERCC2 rs13181 | GT | GT | GG | GG | ||||||||
| ERCC2 rs1799793 | TT | TT | CC | TT | TT | TT | ||||||
| GSTP1 rs1695 | AG | AG | ||||||||||
| TP53 rs1042522 | CC | CC | CC | CC | CC | CC | CC | CC | CC | CC | ||
| TP53 rs1642785 | ||||||||||||
| TPMT rs12201199 | ||||||||||||
| TPMT rs1142345 | ||||||||||||
| TPMT rs1800460 | ||||||||||||
| XPA rs1800975 | CC | CC | CC | CC | CT | CC | ||||||
| XRCC3;KLC1 rs861539 | AA | AA | AG | AG | AG | AG | ||||||
| Polymorphism | U-2OS/ CDDP300 | U-2OS/ CDDP1μg | U-2OS/ CDDP4μg | Saos-2/ CDDP300 | Saos-2/ CDDP1μg | Saos-2/ CDDP6μg | ||||||
| TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | TaqM | NGS | |
| ABCB1 rs1045642 | GA | GA | GA | GA | GA | GA | ||||||
| ABCB1 rs2032582 | CA | CA | CA | CA | CA | CA | CA | CA | CA | CA | CA | CA |
| ABCB1 rs1128503 | GG | GG | GG | GG | GG | GG | GA | GA | GA | GA | GA | GA |
| ABCC2 rs717620 | ||||||||||||
| ABCC2 rs2273697 | ||||||||||||
| ABCC2 rs3740066 | CT | CT | CT | CT | CT | CT | TT | TT | TT | TT | TT | TT |
| ABCC2 rs17222723 | ||||||||||||
| ABCC3 rs4793665 | / | TT | / | TT | ||||||||
| ABCC3 rs1051640 | ||||||||||||
| ACYP2 rs1872328 | ||||||||||||
| ATM rs664677 | TT | TT | TT | TT | TT | TT | CT | CT | CT | CT | CT | CT |
| ATM;C11orf65 rs664143 | GG | GG | GG | GG | GG | GG | GA | GA | GA | GA | GA | GA |
| ATR rs2229032 | ||||||||||||
| ATR rs2227928 | GA | GA | GA | GA | GA | GA | ||||||
| COMT rs4646316 | TT | TT | TT | TT | TT | TT | TT | TT | TT | TT | TT | TT |
| COMT rs9332377 | ||||||||||||
| ERCC1 rs11615 | GA | GA | GA | GA | GG | GG | ||||||
| ERCC1 rs3212986 | ||||||||||||
| ERCC2 rs13181 | GT | GT | TT | GT | GT | GT | GT | GT | GG | GG | ||
| ERCC2 rs1799793 | CT | CT | CT | CT | TT | TT | TT | TT | TT | TT | ||
| GSTP1 rs1695 | AG | AG | AG | AG | AG | AG | AG | AG | AG | AG | AG | AG |
| TP53 rs1042522 | CC | CC | CC | CC | CC | CC | ||||||
| TP53 rs1642785 | ||||||||||||
| TPMT rs12201199 | ||||||||||||
| TPMT rs1142345 | ||||||||||||
| TPMT rs1800460 | ||||||||||||
| XPA rs1800975 | CC | CC | CC | CC | CC | CC | CT | CT | CT | CT | CT | CT |
| XRCC3;KLC1 rs861539 | AG | AG | AG | AG | GG | AG | AA | AA | AA | AA | AA | AA |
| Cell Line | Identified Variants | |
|---|---|---|
| ERCC2 rs13181 | ERCC2 rs1799793 | |
| U-2OS | GT | CT |
| U-2OS/CDDP300 | GT | CT |
| U-2OS/CDDP1μg | GT (a)/TT (b) | CT |
| U-2OS/CDDP4μg | TT | CC |
| Amino acid change | ||
| U-2OS | Lys725Gln | Asp286Asn |
| U-2OS/CDDP300 | Lys725Gln | Asp286Asn |
| U-2OS/CDDP1μg | Lys725Gln | Asp286Asn |
| U-2OS/CDDP4μg | / | / |
| Cell Line | Identified Variants | |
|---|---|---|
| ERCC2 rs13181 | ERCC1 rs11615 | |
| Saos-2 | GT | GA |
| Saos-2/CDDP300 | GT | GA |
| Saos-2/CDDP1μg | GT | GA |
| Saos-2/CDDP6μg | GG | GG |
| Amino Acid Change | ||
| Saos-2 | Lys725Gln | Synonymous |
| Saos-2/CDDP300 | Lys725Gln | Synonymous |
| Saos-2/CDDP1μg | Lys725Gln | Synonymous |
| Saos-2/CDDP6μg | Lys725Gln | Synonymous |
| Cell Line | Identified Variants | |
|---|---|---|
| GSTP1 rs1695 | ||
| DNA | RNA | |
| U-2OS | AG | AA |
| U-2OS/CDDP300 | AG | AG |
| U-2OS/CDDP1μg | AG | GAT |
| U-2OS/CDDP4μg | AG | AG |
| Amino acid change | ||
| U-2OS | / | |
| U-2OS/CDDP300 | Ile105Val | |
| U-2OS/CDDP1μg | Ile105Val | |
| U-2OS/CDDP4μg | Ile105Val | |
| Cell Line | Identified Variants | |
|---|---|---|
| GSTP1 rs1695 | ||
| DNA | RNA | |
| Saos-2 | AG | AA |
| Saos-2/CDDP300 | AG | AG |
| Saos-2/CDDP1μg | AG | AG |
| Saos-2/CDDP6μg | AG | AG |
| Amino acid change | ||
| Saos-2 | / | |
| Saos-2/CDDP300 | Ile105Val | |
| Saos-2/CDDP1μg | Ile105Val | |
| Saos-2/CDDP6μg | Ile105Val | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hattinger, C.M.; Casotti, C.; Patrizio, M.P.; Luppi, S.; Fantoni, L.; Scotlandi, K.; Ibrahim, T.; Serra, M. Pharmacogenomic Profiling of Cisplatin-Resistant and -Sensitive Human Osteosarcoma Cell Lines by Multimodal Targeted Next Generation Sequencing. Int. J. Mol. Sci. 2022, 23, 11787. https://doi.org/10.3390/ijms231911787
Hattinger CM, Casotti C, Patrizio MP, Luppi S, Fantoni L, Scotlandi K, Ibrahim T, Serra M. Pharmacogenomic Profiling of Cisplatin-Resistant and -Sensitive Human Osteosarcoma Cell Lines by Multimodal Targeted Next Generation Sequencing. International Journal of Molecular Sciences. 2022; 23(19):11787. https://doi.org/10.3390/ijms231911787
Chicago/Turabian StyleHattinger, Claudia Maria, Chiara Casotti, Maria Pia Patrizio, Silvia Luppi, Leonardo Fantoni, Katia Scotlandi, Toni Ibrahim, and Massimo Serra. 2022. "Pharmacogenomic Profiling of Cisplatin-Resistant and -Sensitive Human Osteosarcoma Cell Lines by Multimodal Targeted Next Generation Sequencing" International Journal of Molecular Sciences 23, no. 19: 11787. https://doi.org/10.3390/ijms231911787









