In Vitro Study of the Therapeutic Potential of Brown Crude Fucoidans in Osteoarthritis Treatment
Abstract
:1. Introduction
2. Results
2.1. Characterization of Crude Fucoidans
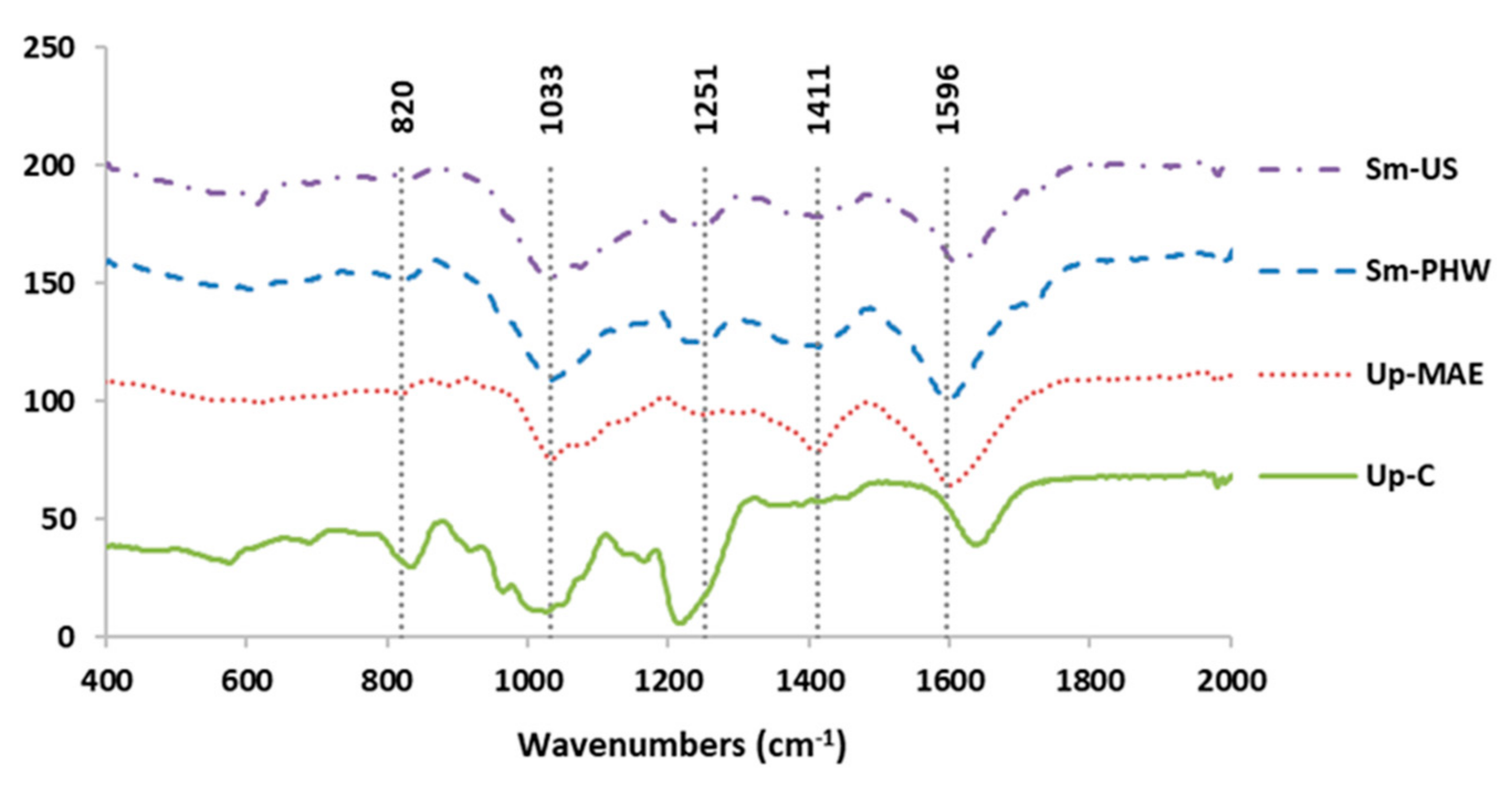
2.1.1. Fourier-Transform Infrared Spectroscopy (FTIR)
2.1.2. High-Performance Size-Exclusion Chromatography
2.1.3. Proton Nuclear Magnetic Resonance (1H NMR)
2.1.4. Scanning Electron Microscope (SEM)
2.2. Effect of Crude Fucoidans on Cell Viability and Inflammatory Response in Human Chondrocytes
2.3. Effect of Crude Fucoidans on Cell Viability and Inflammatory Response in Chondrocyte Cell Line
2.4. Effect of Crude Fucoidans on Antioxidant Response
2.5. Effect of Crude Fucoidans on Cellular Senescence Modulation
3. Discussion
4. Materials and Methods
4.1. Raw Materials for Crude Fucoidan Extraction
4.2. Extraction Technologies
4.2.1. Ultrasound-Assisted Extraction (US)
4.2.2. Pressurized Hot-Water Extraction (PHW)
4.2.3. Microwave-Assisted Extraction (MAE)
4.3. Fourier-Transform Infrared Spectroscopy (FTIR)
4.4. High-Performance Size-Exclusion Chromatography (HPSEC)
4.5. Proton Nuclear Magnetic Resonance (1H NMR)
4.6. Scanning Electron Microscope Analysis (SEM)
4.7. Cell Culture and Stimulation of Human Articular Chondrocyte
4.8. MTT Viability Assay
4.9. ELISA
4.10. RNA Analysis
4.11. Western Blot
4.12. Measurement of β-Galactosidase Activity
4.13. Cell-Proliferation Assay
4.14. Measurement of ROS Production
4.15. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 1H NMR | Proton nuclear magnetic resonance |
| BrdU | 5-bromo-2′-deoxyuridine |
| CBS | Cystathionine β-synthase |
| cDNA | Complementary desoxyribonucleic acid |
| CTH | Cystathionine γ-lyase |
| DCFDA | 2′,7′-Dichlorodihydrofluorescein diacetate |
| DMEM | Dulbecco’s modified eagle medium |
| ECM | Extracellular matrix |
| ELISA | Enzyme-linked immunosorbent assay |
| FBS | Fetal bovine serum |
| FDG | Fluorescein di-β-galactopyranoside |
| FTIR | Fourier transform infrared spectroscopy |
| HO-1 | Heme oxygenase-1 |
| HPRT | Hypoxanthine phosphoribosyl transferase |
| HPSEC | High-performance size exclusion chromatography |
| HRP | Horseradish peroxidase |
| IL-1β | Interleukin 1β |
| IL-6 | Interleukin 6 |
| IL-8 | Interleukin 8 |
| MAE | Microwave-assisted extraction |
| MMPs | Metalloproteinases |
| mRNA | Messenger ribonucleic acid |
| MTT | 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide |
| NSAIDs | Nonsteroidal anti-inflammatory drugs |
| Nrf-2 | Nuclear factor erythroid-2 related factor |
| OA | Osteoarthritis |
| P/S | Penicillin/streptomycin |
| PHW | Pressurized hot-water extraction |
| PBS | Phosphate-buffered saline |
| PMSF | Phenylmethylsulfonyl fluoride |
| qPCR | Quantitative polymerase chain reaction |
| RNA | Ribonucleic acid |
| ROS | Reactive oxygen species |
| SASP | Senescence-associated secretory phenotype |
| SDS | Sodium dodecylsulfate |
| sem | Standard error of median |
| SEM | Scanning electron microscope analysis |
| Sm | Sargassum muticum |
| TNF-α | Tumor necrosis factor α |
| Up | Undaria pinnatifida |
| US | Ultrasound-assisted extraction |
References
- Hwang, H.S.; Kim, H.A. Chondrocyte apoptosis in the pathogenesis of osteoarthritis. Int. J. Mol. Sci. 2015, 16, 26035–26054. [Google Scholar] [CrossRef] [PubMed]
- Carballo, C.B.; Nakagawa, Y.; Sekiya, I.; Rodeo, S.A. Basic Science of Articular Cartilage. Clin. Sports Med. 2017, 36, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Armiento, A.R.; Alini, M.; Stoddart, M.J. Articular fibrocartilage—Why does hyaline cartilage fail to repair? Adv. Drug Deliv. Rev. 2019, 146, 289–305. [Google Scholar] [CrossRef] [PubMed]
- Decker, R.S. Articular cartilage and joint development from embryogenesis to adulthood. Semin. Cell Dev. Biol. 2017, 62, 50–56. [Google Scholar] [CrossRef]
- Mobasheri, A.; Batt, M. An update on the pathophysiology of osteoarthritis. Ann. Phys. Rehabil. Med. 2016, 59, 333–339. [Google Scholar] [CrossRef]
- Hunter, D.J.; Bierma Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef]
- Blanco, F.J.; Silva Díaz, M.; Quevedo Vila, V.; Seoane Mato, D.; Pérez Ruiz, F.; Juan Mas, A.; Pego Reigosa, J.M.; Narváez, J.; Quilis, N.; Cortés, R.; et al. Prevalence of symptomatic osteoarthritis in Spain: EPISER2016 study. Reumatol. Clin. 2021, 17, 461–470. [Google Scholar] [CrossRef]
- Zhang, X.X.; He, S.-H.; Liang, X.; Li, W.; Li, T.-F.; Li, D.-F. Aging, Cell Senescence, the Pathogenesis and Targeted Therapies of Osteoarthritis. Front. Pharmacol. 2021, 12, 728100. [Google Scholar] [CrossRef]
- Maneiro, E.; Martín, M.A.; de Andres, M.C.; López-Armada, M.J.; Fernández-Sueiro, J.L.; del Hoyo, P.; Galdo, F.; Arenas, J.; Blanco, F.J. Mitochondrial respiratory activity is altered in osteoarthritic human articular chondrocytes. Arthritis Rheum. 2003, 48, 700–708. [Google Scholar] [CrossRef]
- Vaamonde García, C.; López Armada, M.J. Role of mitochondrial dysfunction on rheumatic diseases. Biochem. Pharmacol. 2019, 165, 181–195. [Google Scholar] [CrossRef]
- Roškar, S.; Hafner-Bratkovič, I. The Role of Inflammasomes in Osteoarthritis and Secondary Joint Degeneration Diseases. Life 2022, 12, 731. [Google Scholar] [CrossRef] [PubMed]
- Caramés, B.; Taniguchi, N.; Otsuki, S.; Blanco, F.J.; Lotz, M. Autophagy is a protective mechanism in normal cartilage, and its aging-related loss is linked with cell death and osteoarthritis. Arthritis Rheum. 2010, 62, 791–801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kundu, J.; Kim, D.H.; Kundu, J.K.; Chun, K.S. Thymoquinone induces heme oxygenase-1 expression in HaCaT cells via Nrf2/ARE activation: Akt and AMPKα as upstream targets. Food. Chem. Toxicol. 2014, 65, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Shilovsky, G.A. Lability of the Nrf2/Keap/ARE Cell Defense System in Different Models of Cell Aging and Age-Related Pathologies. Biochemistry 2022, 87, 70–85. [Google Scholar] [CrossRef]
- Kapoor, M.; Martel Pelletier, J.; Lajeunesse, D.; Pelletier, J.P.; Fahmi, H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 33–42. [Google Scholar] [CrossRef]
- Rim, Y.A.; Nam, Y.; Ju, J.H. The role of chondrocyte hypertrophy and senescence in osteoarthritis initiation and progression. Int. J. Mol. Sci. 2020, 21, 2358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coryell, P.R.; Diekman, B.O.; Loeser, R.F. Mechanisms and therapeutic implications of cellular senescence in osteoarthritis. Nat. Rev. Rheumatol. 2021, 17, 47–57. [Google Scholar] [CrossRef]
- Diekman, B.O.; Sessions, G.A.; Collins, J.A.; Knecht, A.K.; Strum, S.L.; Mitin, N.K.; Carlson, C.S.; Loeser, R.F.; Sharpless, N.E. Expression of p16INK 4a is a biomarker of chondrocyte aging but does not cause osteoarthritis. Aging Cell 2018, 17, e12771. [Google Scholar] [CrossRef]
- Del Rey, M.J.; Valín, A.; Usategui, A.; Ergueta, S.; Martín, E.; Municio, C.; Cañete, J.D.; Blanco, F.J.; Criado, D.; Pablos, J.L. Senescent synovial fibroblasts accumulate prematurely in rheumatoid arthritis tissues and display an enhanced inflammatory phenotype. Immun. Ageing 2019, 16, 29. [Google Scholar] [CrossRef] [Green Version]
- Jeon, O.H.; Kim, C.; Laberge, R.M.; Demaria, M.; Rathod, S.; Vasserot, A.P.; Wook Chung, J.; Hun Kim, D.; Poon, Y.; David, N.; et al. Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment. Nat. Med. 2017, 23, 775–781. [Google Scholar] [CrossRef] [Green Version]
- Faust, H.J.; Zhang, H.; Han, J.; Wolf, M.T.; Jeon, O.H.; Sadtler, K.; Peña, A.N.; Chung, L.; Maestas, D.R., Jr.; Tam, A.J.; et al. IL-17 and immunologically induced senescence regulate response to injury in osteoarthritis. J. Clin. Investig. 2020, 130, 5493–5507. [Google Scholar] [CrossRef] [PubMed]
- Herranz, N.; Gil, J. Mechanisms and functions of cellular senescence. J. Clin. Investig. 2018, 128, 1238–1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birch, J.; Gil, J. Senescence and the SASP: Many therapeutic avenues. Genes Dev. 2020, 34, 1565–1576. [Google Scholar] [CrossRef]
- Park, C.; Hong, S.H.; Shin, S.S.; Lee, D.S.; Han, M.H.; Cha, H.J.; Kim, S.; Kim, H.S.; Kim, G.Y.; Park, E.K.; et al. Activation of the Nrf2/HO-1 signaling pathway contributes to the protective effects of Sargassum serratifolium extract against oxidative stress-induced DNA damage and apoptosis in SW1353 human chondrocytes. Int. J. Environ Res. Public Health 2018, 15, 1173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, C.; Jeong, J.W.; Lee, D.S.; Yim, M.J.; Lee, J.M.; Han, M.H.; Kim, S.; Kim, H.S.; Kim, G.Y.; Park, E.K.; et al. Sargassum serratifolium extract attenuates interleukin-1β-induced oxidative stress and inflammatory response in chondrocytes by suppressing the activation of NF-κB, p38 MAPK, and PI3K/Akt. Int. J. Mol. Sci. 2018, 19, 2308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alyammahi, J.; Rambabu, K.; Thanigaivelan, A.; Govindan, B.; Hasan, S.; Pau Loke, S.; Banat, F. Advances of non-conventional green technologies for phytosaccharides extraction: Current status and future perspectives. Phytochem. Rev. 2022. [Google Scholar] [CrossRef]
- Apostolova, E.; Lukova, P.; Baldzhieva, A.; Katsarov, P.; Nikolova, M.; Iliev, I.; Peychev, L.; Trica, B.; Oancea, F.; Delattre, C.; et al. Immunomodulatory and anti-inflammatory effects of fucoidan: A review. Polymers 2020, 12, 2338. [Google Scholar] [CrossRef]
- Anisha, G.S.; Padmakumari, S.; Patel, A.K.; Pandey, A.; Singhania, R.R. Fucoidan from marine macroalgae: Biological actions and applications in regenerative medicine, drug delivery systems and food industry. Bioengineering 2022, 9, 472. [Google Scholar] [CrossRef]
- Li, Y.; Zheng, Y.; Zhang, Y.; Yang, Y.; Wang, P.; Imre, B.; Wong, A.; Hsieh, Y.; Wang, D. Brown algae carbohydrates: Structures, pharmaceutical properties, and research challenges. Mar. Drugs 2021, 19, 620. [Google Scholar] [CrossRef]
- Fitton, J.H. Therapies from fucoidan; multifunctional marine polymers. Mar. Drugs 2011, 9, 1731–1760. [Google Scholar] [CrossRef] [Green Version]
- Piñeiro Ramil, M.; Flórez Fernández, N.; Ramil Gómez, O.; Torres, M.D.; Domínguez, H.; Blanco, F.J.; Meijide Faílde, R.; Vaamonde García, C. Antifibrotic effect of brown algae-derived fucoidans on osteoarthritic fibroblast-like synoviocytes. Carbohydr. Polym. 2022, 282, 119134. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.C.; Hwang, H.J.; Kang, K.J.; Lee, B.H. An antioxidative and antiinflammatory agent for potential treatment of osteoarthritis from Ecklonia cava. Arch. Pharm. Res. 2006, 29, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Luthuli, S.; Wu, S.; Cheng, Y.; Zheng, X.; Wu, M.; Tong, H. Therapeutic effects of fucoidan: A review on recent studies. Mar. Drugs 2019, 17, 487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitton, H.J.; Stringer, D.S.; Park, A.Y.; Karpiniec, S.N. Therapies from fucoidan: New developments. Mar. Drugs 2019, 17, 571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeon, O.H.; Yoon, W.J.; Ham, Y.M.; Yoon, S.A.; Kan, S.C. Anti-arthritis effect through the anti-inflammatory effect of Sargassum muticum extract in collagen-induced arthritic (CIA) mice. Molecules 2019, 24, 276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Myers, S.P.; O’Connor, J.; Fitton, J.H.; Brooks, L.; Rolfe, M.; Connellan, P.; Wohlmuth, H.; Cheras, P.A.; Morris, C. A combined phase I and II open label study on the effects of a seaweed extract nutrient complex on osteoarthritis. Biologics 2010, 4, 33–44. [Google Scholar] [CrossRef] [Green Version]
- Vaamonde García, C.; Flórez Fernández, N.; Torres, M.D.; Lamas Vázquez, M.J.; Blanco, F.J.; Domínguez, H.; Meijide Faílde, R. Study of fucoidans as natural biomolecules for therapeutical applications in osteoarthritis. Carbohydr. Polym. 2021, 258, 117692. [Google Scholar] [CrossRef]
- Queffelec, J.; Flórez Fernández, N.; Domínguez, H.; Torres, M.D. Microwave hydrothermal processing of Undaria pinnatifida for bioactive peptides. Bioresour. Technol. 2021, 342, 125882. [Google Scholar] [CrossRef]
- Álvarez Viñas, M.; Flórez Fernández, N.; Torres, M.D.; Domínguez, H. Influence of molecular weight on the properties of Sargassum muticum fucoidan. Algal Res. 2019, 38, 101393. [Google Scholar] [CrossRef]
- Flórez Fernández, N.; López García, M.; González Muñoz, M.J.; López Vilariño, J.M.; Domínguez, H. Ultrasound-assisted extraction of fucoidan from Sargassum muticum. J. Appl. Phycol. 2017, 29, 1553–1561. [Google Scholar] [CrossRef]
- Piñeiro Ramil, M.; Sanjurjo Rodríguez, C.; Castro Viñuelas, R.; Rodríguez Fernández, S.; Hermida Gómez, T.; Fuentes Boquete, I.M.; Blanco, F.J.; Díaz Prado, S.M. Generation of an immortalized chondrocyte cell line from osteoarthritis articular cartilage. Osteoarthr. Cartil. 2021, 29, S208–S209. [Google Scholar] [CrossRef]
- Tamamori Adachi, M.; Koga, A.; Susa, T.; Fujii, H.; Tsuchiya, M.; Okinaga, H.; Hisaki, H.; Iizuka, M.; Kitajima, S.; Okazaki, T. DNA damage response induced by etoposide promotes steroidogenesis via GADD45A in cultured adrenal cells. Sci. Rep. 2018, 8, 9636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, S.G.; Zeng, C.; Li, L.J.; Luo, W.; Zhang, F.J.; Tian, J.; Cheng, C.; Tu, M.; Xiong, Y.L.; Jiang, W.; et al. Correlation between senescence-associated beta-galactosidase expression in articular cartilage and disease severity of patients with knee osteoarthritis. Int. J. Rheum. Dis. 2016, 19, 226–232. [Google Scholar] [CrossRef]
- Puhari, S.S.M.; Yuvaraj, S.; Vasudevan, V.; Ramprasath, T.; Rajkumar, P.; Arunkumar, K.; Amutha, C.; Selvam, G.S. Isolation and characterization of fucoidan from four brown algae and study of the cardioprotective effect of fucoidan from Sargassum wightii against high glucose-induced oxidative stress in H9c2 cardiomyoblast cells. J. Food Biochem. 2022, e14412. [Google Scholar] [CrossRef] [PubMed]
- Camara, R.B.; Costa, L.S.; Fidelis, G.P.; Nobre, L.T.; Dantas Santos, N.; Cordeiro, S.L.; Costa, M.S.; Alves, L.G.; Rocha, H.A. Heterofucans from the brown seaweed Canistrocarpus cervicornis with anticoagulant and antioxidant activities. Mar. Drugs 2011, 9, 124–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernando, I.P.S.; Asanka Sanjeewa, K.K.; Samarakoon, K.W.; Lee, W.W.; Kim, H.S.; Kim, E.A.; Gunasekara, U.K.D.S.S.; Abeytunga, D.T.U.; Nanayakkara, C.; de Silva, E.D.; et al. FTIR characterization and antioxidant activity of water soluble crude polysaccharides of Sri Lankan marine algae. Algae 2017, 32, 75–86. [Google Scholar] [CrossRef] [Green Version]
- Negreanu Pirjol, B.S.; Negreanu Pirjol, T.; Popoviciu, D.R.; Anton, R.E.; Prelipcean, A.M. Marine bioactive compounds derived from macroalgae as new potential players in drug delivery systems: A review. Pharmaceutics 2022, 14, 1781. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Xu, J.; Ge, K.; Tian, Q.; Zhao, P.; Guo, Y. Anti-inflammatory effect of low molecular weight fucoidan from Saccharina japonica on atherosclerosis in apoE-knockout mice. Int. J. Biol. Macromol. 2018, 118 Pt A, 365–374. [Google Scholar] [CrossRef]
- Mazepa, E.; Biscaia, S.; de L. Bellan, D.; da S. Trindade, E.; Simas, F.F. Structural characteristics of native and chemically sulfated polysaccharides from seaweed and their antimelanoma effects. Carbohydr. Polym. 2022, 289, 119436. [Google Scholar] [CrossRef]
- Tanniou, A.; Vandanjon, L.; Gonçalves, O.; Kervarec, N.; Stiger Pouvreau, V. Rapid geographical differentiation of the European spread brown macroalga Sargassum muticum using HRMAS NMR and Fourier-transform infrared spectroscopy. Talanta 2015, 132, 451–456. [Google Scholar] [CrossRef]
- Koh, H.S.A.; Lu, J.; Zhou, W. Structure characterization and antioxidant activity of fucoidan isolated from Undaria pinnatifida grown in New Zealand. Carbohydr. Polym. 2019, 212, 178–185. [Google Scholar] [CrossRef]
- Yu, J.; Li, Q.; Wu, J.; Yang, X.; Yang, S.; Zhu, W.; Liu, Y.; Tang, W.; Nie, S.; Hassouna, A.; et al. Fucoidan extracted from Sporophyll of Undaria pinnatifida grown in Weihai, China—Chemical composition and comparison of antioxidant activity of different molecular weight fractions. Front. Nutr. 2021, 8, 636930. [Google Scholar] [CrossRef]
- Saraswati; Giriwono, P.E.; Iskandriati, D.; Andarwulan, N. Screening of in vitro anti-inflammatory and antioxidant activity of Sargassum ilicifolium crude lipid extracts from different coastal areas in Indonesia. Mar. Drugs 2021, 19, 252. [Google Scholar] [CrossRef]
- Pham, T.H.; Nguyen, V.T.A.; Do, T.T.T.; Do, A.D.; Dam, D.T.; Tran, T.T.V.; Pham, Q.L.; Le, T.T. Lipidomics and anti-inflammation activity of brown algae, Lobophora sp., in Vietnam. J. Chem. 2020, 2020, 1–10. [Google Scholar] [CrossRef]
- Shin, Y.S.; Kim, K.J.; Park, H.; Lee, M.-G.; Cho, S.; Choi, S.-I.; Heo, H.J.; Kim, D.-O.; Kim, G.-H. Effects of Ecklonia cava Extract on Neuronal Damage and Apoptosis in PC-12 Cells against Oxidative Stress. J. Microbiol. Biotechnol. 2021, 31, 584–591. [Google Scholar] [CrossRef]
- Dias, M.K.H.M.; Madusanka, D.; Han, E.J.; Kim, H.S.; Jeon, Y.J.; Jee, Y.; Kim, K.N.; Lee, K.; Fernando, I.; Ahn, G. Sargassum horneri (Turner) C. Agardh ethanol extract attenuates fine dust-induced inflammatory responses and impaired skin barrier functions in HaCaT keratinocytes. J. Ethnopharmacol. 2021, 273, 114003. [Google Scholar] [CrossRef]
- Phull, A.R.; Majid, M.; Haq, I.U.; Khan, M.R.; Kim, S.J. In vitro and in vivo evaluation of anti-arthritic, antioxidant efficacy of fucoidan from Undaria pinnatifida (Harvey) Suringar. Int. J. Biol. Macromol. 2017, 97, 468–480. [Google Scholar] [CrossRef]
- Niture, S.K.; Khatri, R.; Jaiswal, A.K. Regulation of Nrf2-an update. Free Radic. Biol. Med. 2014, 66, 36–44. [Google Scholar] [CrossRef] [Green Version]
- O’Connell, M.A.; Hayes, J.D. The Keap1/Nrf2 pathway in health and disease: From the bench to the clinic. Biochem. Soc. Trans. 2015, 43, 687–689. [Google Scholar] [CrossRef] [Green Version]
- Kubo, Y.; Beckmann, R.; Fragoulis, A.; Conrads, C.; Pavanram, P.; Nebelung, S.; Wolf, M.; Wruck, C.J.; Jahr, H.; Pufe, T. Nrf2/ARE signaling directly regulates SOX9 to potentially alter age-dependent cartilage degeneration. Antioxidants 2022, 11, 263. [Google Scholar] [CrossRef]
- Piñeiro Ramil, M.; Burguera, E.F.; Hermida Gómez, T.; Caramés, B.; Oreiro Villar, N.; Meijide Faílde, R.; Blanco, F.J.; Vaamonde García, C. Reduced levels of H2S in diabetes-associated osteoarthritis are linked to hyperglycaemia, Nrf-2/HO-1 signalling downregulation and chondrocyte dysfunction. Antioxidants 2022, 11, 628. [Google Scholar] [CrossRef]
- Wang, L.; Cui, Y.R.; Lee, H.G.; Fu, X.; Wang, K.; Xu, J.; Gao, X.; Jeon, Y.J. Fucoidan isolated from fermented Sargassum fusiforme suppresses oxidative stress through stimulating the expression of superoxidase dismutase and catalase by regulating Nrf2 signaling pathway. Int. J. Biol. Macromol. 2022, 209 Pt A, 935–941. [Google Scholar] [CrossRef]
- Zahan, M.S.; Hasan, A.; Rahman, M.H.; Meem, K.N.; Moni, A.; Hannan, M.A.; Uddin, M.J. Protective effects of fucoidan against kidney diseases: Pharmacological insights and future perspectives. Int. J. Biol. Macromol. 2022, 209 Pt B, 2119–2129. [Google Scholar] [CrossRef]
- Boas, S.M.; Joyce, K.L.; Cowell, R.M. The NRF2-dependent transcriptional regulation of antioxidant defense pathways: Relevance for cell type-specific vulnerability to neurodegeneration and therapeutic intervention. Antioxidants 2021, 11, 8. [Google Scholar] [CrossRef]
- Wang, R.; Zhang, S.; Previn, R.; Chen, D.; Jin, Y.; Zhou, G. Role of Forkhead Box O Transcription Factors in Oxidative Stress-Induced Chondrocyte Dysfunction: Possible Therapeutic Target for Osteoarthritis? Int. J. Mol. Sci. 2018, 19, 3794. [Google Scholar] [CrossRef] [Green Version]
- Murata, M.; Yudoh, K.; Masuko, K. The potential role of vascular endothelial growth factor (VEGF) in cartilage: How the angiogenic factor could be involved in the pathogenesis of osteoarthritis? Osteoarthr. Cartil. 2008, 16, 279–286. [Google Scholar] [CrossRef] [Green Version]
- McCulloch, K.; Litherland, G.J.; Rai, T.S. Cellular senescence in osteoarthritis pathology. Aging Cell 2017, 16, 210–218. [Google Scholar] [CrossRef]
- Dimri, G.P.; Lee, X.; Basile, G.; Acosta, M.; Scott, G.; Roskelley, C.; Medrano, E.E.; Linskens, M.; Rubelj, I.; Pereira Smith, O. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc. Natl. Acad. Sci. USA 1995, 92, 9363–9367. [Google Scholar] [CrossRef] [Green Version]
- Jun, E.S.; Kim, Y.J.; Kim, H.H.; Park, S.Y. Gold nanoparticles using Ecklonia stolonifera protect human dermal fibroblasts from UVA-induced senescence through inhibiting MMP-1 and MMP-3. Mar. Drugs 2020, 18, 433. [Google Scholar] [CrossRef]
- Victorelli, S.; Passos, J.F. Reactive oxygen species detection in senescent cells. Methods Mol. Biol. 2019, 1896, 21–29. [Google Scholar]
- Del Río, P.G.; Gullón, B.; Pérez Pérez, A.; Romaní, A.; Garrote, G. Microwave hydrothermal processing of the invasive macroalgae Sargassum muticum within a green biorefinery scheme. Bioresour. Technol. 2021, 340, 125733. [Google Scholar] [CrossRef]








| Sample/Composition (%, g/100 g) | Sm-PHW | Sm-US | Up-MAE | Up-C |
|---|---|---|---|---|
| Glucose | 7.06 * | 2.88 * | 2.75 * | - |
| Gal+Xyl+Man | 28.13 * | 10.45 * | 10.64 * | 24.78 * |
| Rhamnose | - | 0.84 * | 0.96 * | - |
| Fucose | 29.69 * | 8.79 * | 11.40 * | 27.10 * |
| Formic acid | 1.28 * | - | 1.84 * | - |
| Acetyl group | 1.57 * | - | 2.57 * | - |
| Galacturonic acid | 7.05 * | - | - | - |
| Fuc:Gal+Xyl+Man:Glu | 1:0.94:0.24 | 1:1.19:0.33 | 1:0.93:0.24 | 1:0.91:0 |
| Sulphate content | 3.28 ± 0.01 | 37.57 ± 0.01 mg/g | 17.01 ± 0.91 mg/g | 384.44 ± 1.93 mg/g |
| Phloroglucinol | 3.22 ± 0.01 | 2.41 ± 0.02 | 3.99 ± 0.12 mg/g | 4.26 ± 0.04 |
| TEAC value | 1.29 ± 0.01 | 4.11 ± 0.01 | 7.37 ± 0.82 mg/g | 5.36 ± 2.09 |
| Reference | [39] | [40] | [38] | Current work |
| Gene | Reference Sequence | Forward Primer | Reverse Primer |
|---|---|---|---|
| CBS | NM_000071.3 | 5′-AGGAGAAGTGTCCTGGATGC-3′ | 5′-TAGGTTGTCTGCTCCGTCTG-3′ |
| CTH | NM_001902.6 | 5′-GCATTTCAAAAACGGAATGG-3′ | 5′-CTCATGCTGTGGATGAGAGG-3′ |
| HMOX1 | NM_002133.3 | 5′-TCCGATGGGTCCTTACACTC-3′ | 5′-TAAGGAAGCAGCAAGAGA-3′ |
| SOD-2 | NM_000636.4 | 5′-CTGGACAAACCTCAGCCCTA-3′ | 5′-TGATGGCTTCCAGCAACTC-3′ |
| IL-6 | NM_000600.5 | 5′-GATGAGTACAAAAGTCCTGATCCA-3′ | 5′-CTGCAGCCACTGGTTCTGT-3′ |
| IL-8 | NM 000584.3 | 5′-GAGCACTCCATAAGGCACAAA-3′ | 5′-ATGGTTCCTTCCGGTGGT-3′ |
| HPRT | NM_000194.3 | 5′-TGATAGATCCATTCCTATGACTGTAGA-3′ | 5′-CAAGACATTCTTTCCAGTTAAAGTTG-3′ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaamonde-García, C.; Capelo-Mera, E.; Flórez-Fernández, N.; Torres, M.D.; Rivas-Murias, B.; Mejide-Faílde, R.; Blanco, F.J.; Domínguez, H. In Vitro Study of the Therapeutic Potential of Brown Crude Fucoidans in Osteoarthritis Treatment. Int. J. Mol. Sci. 2022, 23, 14236. https://doi.org/10.3390/ijms232214236
Vaamonde-García C, Capelo-Mera E, Flórez-Fernández N, Torres MD, Rivas-Murias B, Mejide-Faílde R, Blanco FJ, Domínguez H. In Vitro Study of the Therapeutic Potential of Brown Crude Fucoidans in Osteoarthritis Treatment. International Journal of Molecular Sciences. 2022; 23(22):14236. https://doi.org/10.3390/ijms232214236
Chicago/Turabian StyleVaamonde-García, Carlos, Emma Capelo-Mera, Noelia Flórez-Fernández, María Dolores Torres, Beatriz Rivas-Murias, Rosa Mejide-Faílde, Francisco J. Blanco, and Herminia Domínguez. 2022. "In Vitro Study of the Therapeutic Potential of Brown Crude Fucoidans in Osteoarthritis Treatment" International Journal of Molecular Sciences 23, no. 22: 14236. https://doi.org/10.3390/ijms232214236
APA StyleVaamonde-García, C., Capelo-Mera, E., Flórez-Fernández, N., Torres, M. D., Rivas-Murias, B., Mejide-Faílde, R., Blanco, F. J., & Domínguez, H. (2022). In Vitro Study of the Therapeutic Potential of Brown Crude Fucoidans in Osteoarthritis Treatment. International Journal of Molecular Sciences, 23(22), 14236. https://doi.org/10.3390/ijms232214236







