The Role of Metalloproteinases and Their Tissue Inhibitors on Ocular Diseases: Focusing on Potential Mechanisms
Abstract
1. Introduction
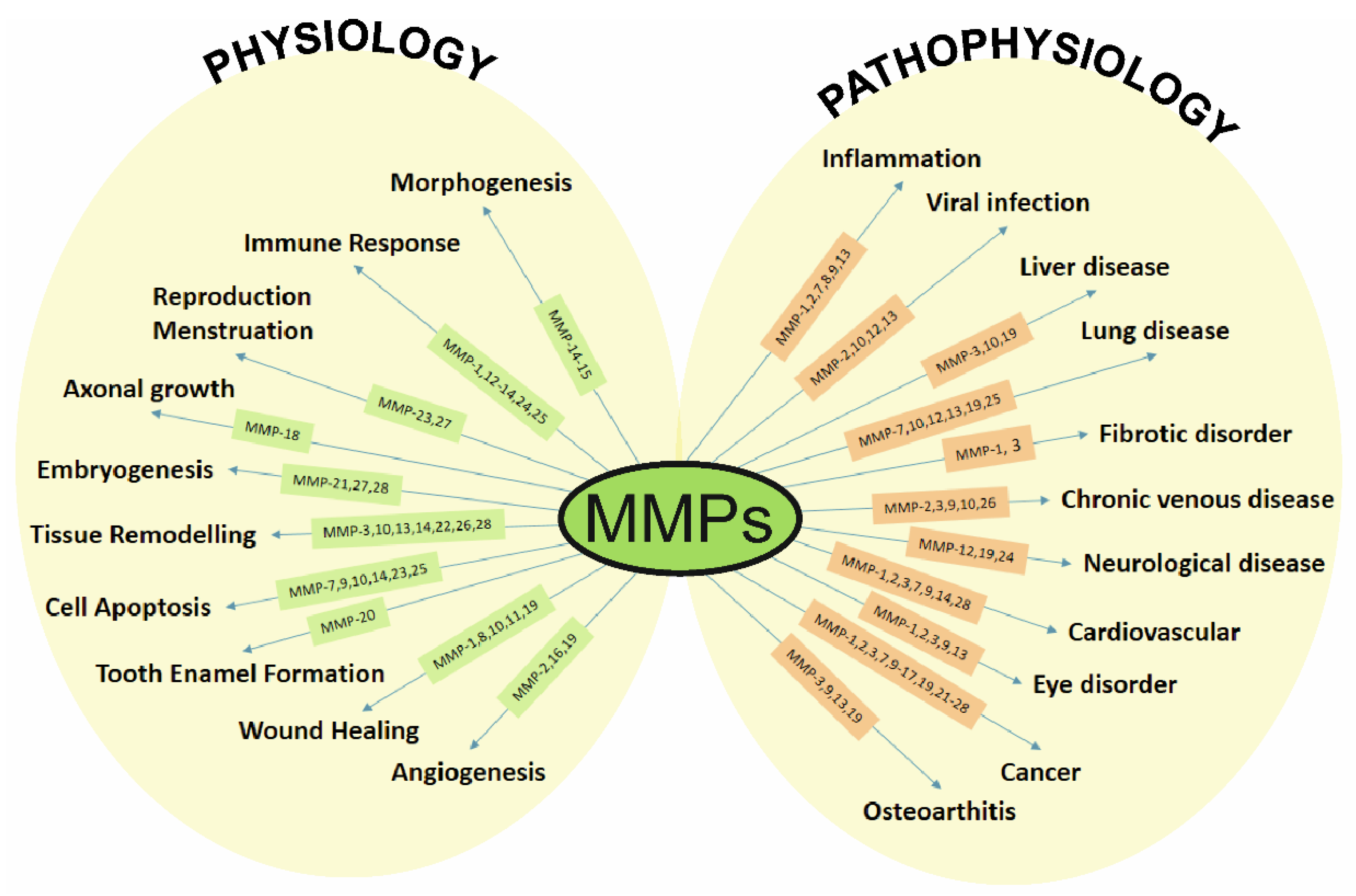
2. Metalloproteinases (MMPs)
3. The MMPs and TIMPs in Eye Diseases
3.1. Ocular Cancers
3.1.1. Uveal Melanoma
3.1.2. Retinoblastoma
3.2. Age-Related Macular Degeneration
3.3. Diabetic Retinopathy
3.4. Cataract and Posterior Capsule Opacification
3.5. Dry Eye Syndrome
3.6. Glaucoma
4. Novel Agents Modulating the Expression and Activity of MMPs and TIMPs in Eye Diseases
4.1. Natural Agents
4.2. Synthetic Agents
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, X.; Vimalin Jeyalatha, M.; Qu, Y.; He, X.; Ou, S.; Bu, J.; Jia, C.; Wang, J.; Wu, H.; Liu, Z.; et al. Dry eye management: Targeting the ocular surface microenvironment. Int. J. Mol. Sci. 2017, 18, 1398. [Google Scholar] [CrossRef] [PubMed]
- Lu, B.; Yin, H.; Tang, Q.; Wang, W.; Luo, C.; Chen, X.; Zhang, X.; Lai, K.; Xu, J.; Chen, X.; et al. Multiple cytokine analyses of aqueous humor from the patients with retinitis pigmentosa. Cytokine 2020, 127, 154943. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.K.; Erb, C.; Hoffmann, E.M.; Dietlein, T.; Pfeiffer, N. The diagnosis and treatment of glaucoma. Dtsch. Arztebl. Int. 2020, 117, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Kowluru, R.A.; Mishra, M. Regulation of Matrix Metalloproteinase in the Pathogenesis of Diabetic Retinopathy, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2017; Volume 148. [Google Scholar]
- Pflugfelder, S.C.; de Paiva, C.S. The Pathophysiology of Dry Eye Disease. Ophthalmology 2017, 124, S4–S13. [Google Scholar] [CrossRef]
- Mitchell, P.; Liew, G.; Gopinath, B.; Wong, T.Y. Age-related macular degeneration. Lancet 2018, 392, 1147–1159. [Google Scholar] [CrossRef]
- Astuti, G.D.N.; van den Born, L.I.; Khan, M.I.; Hamel, C.P.; Bocquet, B.; Manes, G.; Quinodoz, M.; Ali, M.; Toomes, C.; McKibbin, M.; et al. Identification of inherited retinal disease-associated genetic variants in 11 candidate genes. Genes 2018, 9, 21. [Google Scholar] [CrossRef]
- Bourne, R.R.A.; Steinmetz, J.D.; Saylan, M.; Mersha, A.M.; Weldemariam, A.H.; Wondmeneh, T.G.; Sreeramareddy, C.T.; Pinheiro, M.; Yaseri, M.; Yu, C.; et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e144–e160. [Google Scholar] [CrossRef]
- Kehlet, S.N.; Willumsen, N.; Armbrecht, G.; Dietzel, R.; Brix, S.; Henriksen, K.; Karsdal, M.A. Age-related collagen turnover of the interstitial matrix and basement membrane: Implications of age- and sex-dependent remodeling of the extracellular matrix. PLoS ONE 2018, 13, e0194458. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, X.; Clark, M.E.; Curcio, C.A.; Owsley, C. Imaging of age-related macular degeneration by adaptive optics scanning laser ophthalmoscopy in eyes with aged lenses or intraocular lenses. Transl. Vis. Sci. Technol. 2020, 9, 41. [Google Scholar] [CrossRef]
- Ghasemi, H.; Yaraee, R.; Faghihzadeh, S.; Ghassemi-Broumand, M.; Mahmoudi, M.; Babaei, M.; Naderi, M.; Safavi, M.; Ghazanfari, Z.; Rastin, M.; et al. Tear and serum MMP-9 and serum TIMPs levels in the severe sulfur mustard eye injured exposed patients. Int. Immunopharmacol. 2019, 77, 105812. [Google Scholar] [CrossRef]
- Wang, T.; Zhang, Y.; Bai, J.; Xue, Y.; Peng, Q. MMP1 and MMP9 are potential prognostic biomarkers and targets for uveal melanoma. BMC Cancer 2021, 21, 1068. [Google Scholar] [CrossRef] [PubMed]
- Cui, N.; Hu, M.; Khalil, R.A. Biochemical and Biological Attributes of Matrix Metalloproteinases, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2017; Volume 147. [Google Scholar]
- Theocharis, A.D.; Skandalis, S.S.; Gialeli, C.; Karamanos, N.K. Extracellular matrix structure. Adv. Drug Deliv. Rev. 2016, 97, 4–27. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, R.N.; Robinson, M.R.; Dibas, M.; Stamer, W.D. Matrix Metalloproteinases and Glaucoma Treatment. J. Ocul. Pharmacol. Ther. 2020, 36, 208–228. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, C.; Vaidya, S.; Wadhwan, V.; Hitesh; Kaur, G.; Pathak, A. Seesaw of matrix metalloproteinases (MMPs). J. Cancer Res. Ther. 2016, 12, 28–35. [Google Scholar] [CrossRef]
- Lee, J.I.; Kil, J.H.; Yu, G.H.; Karadeniz, F.; Oh, J.H.; Seo, Y.; Kong, C.S. 3,5-Dicaffeoyl-epi-quinic acid inhibits the PMA-stimulated activation and expression of MMP-9 but not MMP-2 via downregulation of MAPK pathway. Z. Naturforsch. Sect. C J. Biosci. 2020, 75, 113–120. [Google Scholar] [CrossRef]
- Elhadidy, M.G.; El Nashar, E.M.; Alghamdi, M.A.; Samir, S.M. A novel gastroprotective effect of zeaxanthin against stress-induced gastritis in male rats targeting the expression of HIF-1α, TFF-1 and MMP-9 through PI3K/Akt/JNK signaling pathway. Life Sci. 2021, 273, 119297. [Google Scholar] [CrossRef]
- Peck, T.J.; Patel, S.N.; Ho, A.C. Endophthalmitis after cataract surgery: An update on recent advances. Curr. Opin. Ophthalmol. 2021, 32, 62–68. [Google Scholar] [CrossRef]
- Liu, J.; Khalil, R.A. Matrix Metalloproteinase Inhibitors as Investigational and Therapeutic Tools in Unrestrained Tissue Remodeling and Pathological Disorders, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2017; Volume 148. [Google Scholar]
- Mannello, F.; Gazzanelli, G. Tissue inhibitors of metalloproteinases and programmed cell death: Conundrums, controversies and potential implications. Apoptosis 2001, 6, 479–482. [Google Scholar] [CrossRef]
- DeLeon-Pennell, K.Y.; Meschiari, C.A.; Jung, M.; Lindsey, M.L. Matrix Metalloproteinases in Myocardial Infarction and Heart Failure, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2017; Volume 147. [Google Scholar]
- Rivera, S.; García-González, L.; Khrestchatisky, M.; Baranger, K. Metalloproteinases and their tissue inhibitors in Alzheimer’s disease and other neurodegenerative disorders. Cell. Mol. Life Sci. 2019, 76, 3167–3191. [Google Scholar] [CrossRef]
- Buttacavoli, M.; Di Cara, G.; Roz, E.; Pucci-Minafra, I.; Feo, S.; Cancemi, P. Integrated multi-omics investigations of metalloproteinases in colon cancer: Focus on mmp2 and mmp9. Int. J. Mol. Sci. 2021, 22, 12389. [Google Scholar] [CrossRef]
- Kiani, A.; Kamankesh, M.; Vaisi-Raygani, A.; Moradi, M.R.; Tanhapour, M.; Rahimi, Z.; Elahi-Rad, S.; Bahrehmand, F.; Aliyari, M.; Aghaz, F.; et al. Activities and polymorphisms of MMP-2 and MMP-9, smoking, diabetes and risk of prostate cancer. Mol. Biol. Rep. 2020, 47, 9373–9383. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.; Zheng, Z. The role and function of matrix metalloproteinase-8 in rhegmatogenous retinal detachment. Int. J. Clin. Exp. Pathol. 2017, 10, 7325–7332. [Google Scholar] [PubMed]
- Bian, F.; Wang, C.; Tukler-Henriksson, J.; Pflugfelder, S.C.; Camodeca, C.; Nuti, E.; Rossello, A.; Li, D.Q.; de Paiva, C.S. MMP-8 Is Critical for Dexamethasone Therapy in Alkali-Burned Corneas Under Dry Eye Conditions. J. Cell. Physiol. 2016, 231, 2506–2516. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.H.; Huang, Y.H.; Cunningham, C.M.; Han, K.Y.; Chang, M.; Seiki, M.; Zhou, Z.; Azar, D.T. Matrix metalloproteinase 14 modulates signal transduction and angiogenesis in the cornea. Surv. Ophthalmol. 2016, 61, 478–497. [Google Scholar] [CrossRef] [PubMed]
- Abu El-Asrar, A.M.; Mohammad, G.; Allegaert, E.; Ahmad, A.; Siddiquei, M.M.; Alam, K.; Gikandi, P.W.; De Hertogh, G.; Opdenakker, G. Matrix metalloproteinase-14 is a biomarker of angiogenic activity in proliferative diabetic retinopathy. Mol. Vis. 2018, 24, 394–406. [Google Scholar] [PubMed]
- Cheng, Y.; Zheng, S.; Pan, C.T.; Yuan, M.; Chang, L.; Yao, Y.; Zhao, M.; Liang, J. Analysis of aqueous humor concentrations of cytokines in retinoblastoma. PLoS ONE 2017, 12, e0177337. [Google Scholar] [CrossRef]
- Zaleska-Zmijewska, A.; Strzemecka, E.; Wawrzyniak, Z.M.; Szaflik, J.P. Extracellular MMP-9-Based Assessment of Ocular Surface Inflammation in Patients with Primary Open-Angle Glaucoma. J. Ophthalmol. 2019, 2019, 1240537. [Google Scholar] [CrossRef]
- Cabral-Pacheco, G.A.; Garza-Veloz, I.; la Rosa, C.C.D.; Ramirez-Acuña, J.M.; Perez-Romero, B.A.; Guerrero-Rodriguez, J.F.; Martinez-Avila, N.; Martinez-Fierro, M.L. The roles of matrix metalloproteinases and their inhibitors in human diseases. Int. J. Mol. Sci. 2020, 21, 9739. [Google Scholar] [CrossRef]
- Clemens, D.L.; Duryee, M.J.; Sarmiento, C.; Chiou, A.; McGowan, J.D.; Hunter, C.D.; Schlichte, S.L.; Tian, J.; Klassen, L.W.; O’dell, J.R.; et al. Novel antioxidant properties of doxycycline. Int. J. Mol. Sci. 2018, 19, 4078. [Google Scholar] [CrossRef]
- Zhang, M.G.; Lee, J.Y.; Gallo, R.A.; Tao, W.; Tse, D.; Doddapaneni, R.; Pelaez, D. Therapeutic targeting of oncogenic transcription factors by natural products in eye cancer. Pharmacol. Res. 2018, 129, 365–374. [Google Scholar] [CrossRef]
- Chojnacka, K.; Lewandowska, U. Chemopreventive effects of polyphenol-rich extracts against cancer invasiveness and metastasis by inhibition of type IV collagenases expression and activity. J. Funct. Foods 2018, 46, 295–311. [Google Scholar] [CrossRef]
- Lai, K.; Conway, R.M.; Crouch, R.; Jager, M.J.; Madigan, M.C. Expression and distribution of MMPs and TIMPs in human uveal melanoma. Exp. Eye Res. 2008, 86, 936–941. [Google Scholar] [CrossRef]
- Xue, M.; Shang, J.; Chen, B.; Yang, Z.; Song, Q.; Sun, X.; Chen, J.; Yang, J. Identification of prognostic signatures for predicting the overall survival of uveal melanoma patients. J. Cancer 2019, 10, 4921–4931. [Google Scholar] [CrossRef] [PubMed]
- Sahin, A.; Kiratli, H.; Soylemezoglu, F.; Tezel, G.G.; Bilgic, S.; Saracbasi, O. Expression of vascular endothelial growth factor-A, matrix metalloproteinase-9, and extravascular matrix patterns and their correlations with clinicopathologic parameters in posterior uveal melanomas. Jpn. J. Ophthalmol. 2007, 51, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Grossniklaus, H.E.; Zhang, Q.; You, S.; McCarthy, C.; Heegaard, S.; Coupland, S.E. Metastatic ocular melanoma to the liver exhibits infiltrative and nodular growth patterns. Hum. Pathol. 2016, 57, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Lüke, J.; Vukoja, V.; Brandenbusch, T.; Nassar, K.; Rohrbach, J.M.; Grisanti, S.; Lüke, M.; Tura, A. CD147 and matrix-metalloproteinase-2 expression in metastatic and non-metastatic uveal melanomas. BMC Ophthalmol. 2016, 16, 74. [Google Scholar] [CrossRef]
- Hou, Q.; Han, S.; Yang, L.; Chen, S.; Chen, J.; Ma, N.; Wang, C.; Tang, J.; Chen, X.; Chen, F.; et al. The Interplay of MicroRNA-34a, LGR4, EMT-Associated Factors, and MMP2 in Regulating Uveal Melanoma Cells. Investig. Ophthalmol. Vis. Sci. 2019, 60, 4503–4510. [Google Scholar] [CrossRef]
- Nareyeck, G.; Zeschnigk, M.; Von Der Haar, D.; Schilling, H.; Bornfeld, N.; Anastassiou, G. Differential expression of tissue inhibitor of matrix metalloproteinases 3 in uveal melanoma. Ophthalmic Res. 2005, 37, 23–28. [Google Scholar] [CrossRef]
- Anfuso, C.D.; Longo, A.; Distefano, A.; Amorini, A.M.; Salmeri, M.; Zanghì, G.; Giallongo, C.; Giurdanella, G.; Lupo, G. Uveal melanoma cells elicit retinal pericyte phenotypical and biochemical changes in an in vitro model of coculture. Int. J. Mol. Sci. 2020, 21, 5557. [Google Scholar] [CrossRef]
- Alyahya, G.A.; Kolko, M.; Prause, J.U.; Nielsen, B.S.; Wang, J.; Heegaard, S. Matrix metalloproteinase-2 is expressed in melanoma-associated spongiform scleropathy. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2806–2811. [Google Scholar] [CrossRef]
- Chen, M.; Li, Y.; Sun, X.; Zhang, B.; Li, W.; Wang, S.; Zhu, X.; Li, F.; Shi, L. Grb2-associated binder 2 expression and its roles in uveal melanoma invasion. Mol. Med. Rep. 2017, 16, 4577–4582. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ding, C.; Luo, J.; Li, L.; Li, S.; Yang, L.; Pan, H.; Liu, Q.; Qin, H.; Chen, C.; Feng, J. Gab2 facilitates epithelial-to-mesenchymal transition via the MEK/ERK/MMP signaling in colorectal cancer. J. Exp. Clin. Cancer Res. 2016, 35, 5. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Cheng, T.; Zhao, Y.; Qu, Y. HMGA1 exacerbates tumor progression by activating miR-222 through PI3K/Akt/MMP-9 signaling pathway in uveal melanoma. Cell. Signal. 2019, 63, 109386. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Sun, Q.; Chen, J.; Li, J.; Zeng, Y.; Zhai, S.; Li, P.; Wang, B.; Wang, X. MicroRNA-9 suppresses uveal melanoma cell migration and invasion through the NF-κB1 pathway. Oncol. Rep. 2012, 28, 961–968. [Google Scholar] [CrossRef]
- Hu, D.N.; Rosen, R.B.; Chan, C.C.; Yang, W.E.; Yang, S.F. Uveal melanocytes express high constitutive levels of MMP-8 which can be upregulated by TNF-α via the MAPK pathway. Exp. Eye Res. 2018, 175, 181–191. [Google Scholar] [CrossRef]
- Rossi, S.; Cordella, M.; Tabolacci, C.; Nassa, G.; D’Arcangelo, D.; Senatore, C.; Pagnotto, P.; Magliozzi, R.; Salvati, A.; Weisz, A.; et al. TNF-alpha and metalloproteases as key players in melanoma cells aggressiveness. J. Exp. Clin. Cancer Res. 2018, 37, 326. [Google Scholar] [CrossRef]
- Maacha, S.; Anezo, O.; Foy, M.; Liot, G.; Mery, L.; Laurent, C.; Sastre-Garau, X.; Piperno-Neumann, S.; Cassoux, N.; Planque, N.; et al. Protein tyrosine phosphatase 4A3 (PTP4A3) promotes human uveal melanoma aggressiveness through membrane accumulation of matrix metalloproteinase 14 (MMP14). Investig. Ophthalmol. Vis. Sci. 2016, 57, 1982–1990. [Google Scholar] [CrossRef]
- Ancona-Lezama, D.; Dalvin, L.A.; Shields, C.L. Modern treatment of retinoblastoma: A 2020 review. Indian J. Ophthalmol. 2020, 68, 2356–2365. [Google Scholar] [CrossRef]
- Zhu, J.; Zhang, X.; Ai, L.; Yuan, R.; Ye, J. Clinicohistopathological implications of MMP/VEGF expression in retinoblastoma: A combined meta-analysis and bioinformatics analysis. J. Transl. Med. 2019, 17, 226. [Google Scholar] [CrossRef]
- Long, H.; Zhou, B.; Jiang, F.G. Expression of MMP-2 and MMP-9 in retinoblastoma and their significance. Int. J. Ophthalmol. 2011, 4, 489–491. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, J.H.; Cho, C.S.; Jun, H.O.; Kim, D.H.; Yu, Y.S.; Kim, K.W. Differential roles of matrix metalloproteinase-9 and -2, depending on proliferation or differentiation of retinoblastoma cells. Investig. Ophthalmol. Vis. Sci. 2010, 51, 1783–1788. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.L.; Li, L. Correlation between matrix metalloproteinase-9 and vascular endothelial growth factor expression in lung adenocarcinoma. Genet. Mol. Res. 2015, 14, 19342–19348. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhao, H.; Yu, J. HOXB5 promotes retinoblastoma cell migration and invasion via ERK1/2 pathway-mediated MMPs production. Am. J. Transl. Res. 2018, 10, 1703–1712. [Google Scholar] [PubMed]
- Adithi, M.; Nalini, V.; Kandalam, M.; Krishnakumar, S. Expression of matrix metalloproteinases and their inhibitors in retinoblastoma. J. Pediatr. Hematol. Oncol. 2007, 29, 399–405. [Google Scholar] [CrossRef]
- Reinhard, J.; Wagner, N.; Krämer, M.M.; Jarocki, M.; Joachim, S.C.; Dick, H.B.; Faissner, A.; Kakkassery, V. Expression changes and impact of the extracellular matrix on etoposide resistant human retinoblastoma cell lines. Int. J. Mol. Sci. 2020, 21, 4322. [Google Scholar] [CrossRef]
- Venkatesan, N.; Krishnakumar, S.; Deepa, P.R.; Deepa, M.; Khetan, V.; Ashwin Reddy, M. Molecular deregulation induced by silencing of the high mobility group protein A2 gene in retinoblastoma cells. Mol. Vis. 2012, 18, 2420–2437. [Google Scholar]
- Zhou, M.; Sun, J.; Liu, Y.; Ma, J. Suppressor of zeste 12 homolog RNA interference inhibits retinoblastoma cell invasion. Oncol. Lett. 2014, 8, 1933–1936. [Google Scholar] [CrossRef]
- Wu, T.; Wang, L.N.; Tang, D.R.; Sun, F.Y. SOST silencing promotes proliferation and invasion and reduces apoptosis of retinoblastoma cells by activating Wnt/β-catenin signaling pathway. Gene Ther. 2017, 24, 399–407. [Google Scholar] [CrossRef]
- Mu, Y.T.; Feng, H.H.; Yu, J.Q.; Liu, Z.K.; Wang, Y.; Shao, J.; Li, R.H.; Li, D.K. Curcumin suppressed proliferation and migration of human retinoblastoma cells through modulating NF-κB pathway. Int. Ophthalmol. 2020, 40, 2435–2440. [Google Scholar] [CrossRef]
- Wen, S.; Hu, M.; Xiong, Y. Effect of Eriodictyol on Retinoblastoma via the PI3K/Akt Pathway. J. Healthc. Eng. 2021, 2021, 6091585. [Google Scholar] [CrossRef]
- Livia Bajenaru, M.; Piña, Y.; Murray, T.G.; Cebulla, C.M.; Feuer, W.; Jockovich, M.E.; Castaño, A.E.M. Gelatinase expression in retinoblastoma: Modulation of LHBETATAG retinal tumor development by anecortave acetate. Investig. Ophthalmol. Vis. Sci. 2010, 51, 2860–2864. [Google Scholar] [CrossRef]
- Webb, A.H.; Gao, B.T.; Goldsmith, Z.K.; Irvine, A.S.; Saleh, N.; Lee, R.P.; Lendermon, J.B.; Bheemreddy, R.; Zhang, Q.; Brennan, R.C.; et al. Inhibition of MMP-2 and MMP-9 decreases cellular migration, and angiogenesis in in vitro models of retinoblastoma. BMC Cancer 2017, 17, 434. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.X.; Yang, Y.; Li, K. Long noncoding RNA DANCR aggravates retinoblastoma through miR-34c and miR-613 by targeting MMP-9. J. Cell. Physiol. 2018, 233, 6986–6995. [Google Scholar] [CrossRef] [PubMed]
- Meng, N.; Zhao, Z.; Shi, C.; Xia, L. Inhibiting the Progression of Human Retinoblastoma Cell by Downregulation of MMP-2/MMP-9 Using Short Hairpin RNAs (shRNAs) in Vitro. J. Ophthalmol. 2020, 2020, 4912347. [Google Scholar] [CrossRef] [PubMed]
- Kaarniranta, K.; Tokarz, P.; Koskela, A.; Paterno, J.; Blasiak, J. Autophagy regulates death of retinal pigment epithelium cells in age-related macular degeneration. Cell Biol. Toxicol. 2017, 33, 113–128. [Google Scholar] [CrossRef] [PubMed]
- Tong, Y.; Wang, S. Not All Stressors Are Equal: Mechanism of Stressors on RPE Cell Degeneration. Front. Cell Dev. Biol. 2020, 8, 1399. [Google Scholar] [CrossRef]
- Nashine, S. Potential therapeutic candidates for age-related macular degeneration (Amd). Cells 2021, 10, 2483. [Google Scholar] [CrossRef] [PubMed]
- Nita, M.; Strzałka-Mrozik, B.; Grzybowski, A.; Mazurek, U.; Romaniuk, W. Age-related macular degeneration and changes in the extracellular matrix. Med. Sci. Monit. 2014, 20, 1003–1016. [Google Scholar] [CrossRef]
- García-Onrubia, L.; Valentín-Bravo, F.J.; Coco-Martin, R.M.; González-Sarmiento, R.; Pastor, J.C.; Usategui-Martín, R.; Pastor-Idoate, S. Matrix metalloproteinases in age-related macular degeneration (Amd). Int. J. Mol. Sci. 2020, 21, 5934. [Google Scholar] [CrossRef]
- Plantner, J.J.; Jiang, C.; Smine, A. Increase in interphotoreceptor matrix gelatinase A (MMP-2) associated with age-related macular degeneration. Exp. Eye Res. 1998, 67, 637–645. [Google Scholar] [CrossRef]
- Chau, K.Y.; Sivaprasad, S.; Patel, N.; Donaldson, T.A.; Luthert, P.J.; Chong, N.V. Plasma levels of matrix metalloproteinase-2 and -9 (MMP-2 and MMP-9) in age-related macular degeneration. Eye 2008, 22, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; Wen, F.; Zhang, X.; Su, Y. Serum levels of matrix metalloproteinase 2 and matrix metalloproteinase 9 elevated in polypoidal choroidal vasculopathy but not in age-related macular degeneration. Mol. Vis. 2013, 19, 729–736. [Google Scholar] [PubMed]
- Leu, S.T.; Batni, S.; Radeke, M.J.; Johnson, L.V.; Anderson, D.H.; Clegg, D.O. Drusen are cold spots for proteolysis: Expression of matrix metalloproteinases and their tissue inhibitor proteins in age-related macular degeneration. Exp. Eye Res. 2002, 74, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Alcazar, O.; Cousins, S.W.; Marin-Castaño, M.E. MMP-14 and TIMP-2 overexpression protects against hydroquinone-induced oxidant injury in RPE: Implications for extracellular matrix turnover. Investig. Ophthalmol. Vis. Sci. 2007, 48, 5662–5670. [Google Scholar] [CrossRef]
- Hussain, A.A.; Lee, Y.; Zhang, J.J.; Marshall, J. Disturbed matrix metalloproteinase activity of Bruch’s membrane in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4459–4466. [Google Scholar] [CrossRef]
- Hsu, K.S.; Otsu, W.; Li, Y.; Wang, H.C.; Chen, S.; Tsang, S.H.; Chuang, J.Z.; Sung, C.H. CLIC4 regulates late endosomal trafficking and matrix degradation activity of MMP14 at focal adhesions in RPE cells. Sci. Rep. 2019, 9, 11452. [Google Scholar] [CrossRef]
- Alge-Priglinger, C.S.; Kreutzer, T.; Obholzer, K.; Wolf, A.; Mempel, M.; Kernt, M.; Kampik, A.; Priglinger, S.G. Oxidative stress-mediated induction of MMP-1 and MMP-3 in human RPE cells. Investig. Ophthalmol. Vis. Sci. 2009, 50, 5495–5503. [Google Scholar] [CrossRef]
- Tatar, O.; Adam, A.; Shinoda, K.; Eckert, T.; Scharioth, G.B.; Klein, M.; Yoeruek, E.; Bartz-Schmidt, K.U.; Grisanti, S. Matrix metalloproteinases in human choroidal neovascular membranes excised following verteporfin photodynamic therapy. Br. J. Ophthalmol. 2007, 91, 1183–1189. [Google Scholar] [CrossRef]
- Zeng, S.; Whitmore, S.S.; Sohn, E.H.; Riker, M.J.; Wiley, L.A.; Scheetz, T.E.; Stone, E.M.; Tucker, B.A.; Mullins, R.F. Molecular response of chorioretinal endothelial cells to complement injury: Implications for macular degeneration. J. Pathol. 2016, 238, 446–456. [Google Scholar] [CrossRef]
- Ecker, S.M.; Pfahler, S.M.; Hines, J.C.; Lovelace, A.S.; Glaser, B.M. Sequential in-office vitreous aspirates demonstrate vitreous matrix metalloproteinase 9 levels correlate with the amount of subretinal fluid in eyes with wet age-related macular degeneration. Mol. Vis. 2012, 18, 1658–1667. [Google Scholar]
- Xu, J.; Zhu, D.; Sonoda, S.; He, S.; Spee, C.; Ryan, S.J.; Hinton, D.R. Over-expression of BMP4 inhibits experimental choroidal neovascularization by modulating VEGF and MMP-9. Angiogenesis 2012, 15, 213–227. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.H.; Pierce, C.O.; De Salvo, G.; Griffiths, H.; Nelson, M.; Cree, A.J.; Menon, G.; Lotery, A.J. The effect of systemic levels of TNF-alpha and complement pathway activity on outcomes of VEGF inhibition in neovascular AMD. Eye 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, S.; He, S.; Ehren, M.; Ryan, S.J.; Wiedemann, P.; Hinton, D.R. MMP-2 and MMP-9 secretion by RPE is stimulated by angiogenic molecules found in choroidal neovascular membranes. Retina 2006, 26, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Mousa, S.A.; Lorelli, W.; Campochiaro, P.A. Role of hypoxia and extracellular matrix-integrin binding in the modulation of angiogenic growth factors secretion by retinal pigmented epithelial cells. J. Cell. Biochem. 1999, 74, 135–143. [Google Scholar] [CrossRef]
- Hollborn, M.; Stathopoulos, C.; Steffen, A.; Wiedemann, P.; Kohen, L.; Bringmann, A. Positive feedback regulation between MMP-9 and VEGF in human RPE cells. Investig. Ophthalmol. Vis. Sci. 2007, 48, 4360–4367. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Godino, R.; Bujakowska, K.M.; Pierce, E.A. Changes in extracellular matrix cause RPE cells to make basal deposits and activate the alternative complement pathway. Hum. Mol. Genet. 2018, 27, 147–159. [Google Scholar] [CrossRef]
- Striker, G.E.; Praddaude, F.; Alcazar, O.; Cousins, S.W.; Marin-Castaño, M.E. Regulation of angiotensin II receptors and extracellular matrix turnover in human retinal pigment epithelium: Role of angiotensin II. Am. J. Physiol.Cell Physiol. 2008, 295, C1633–C1646. [Google Scholar] [CrossRef]
- Pons, M.; Cousins, S.W.; Alcazar, O.; Striker, G.E.; Marin-Castaño, M.E. Angiotensin II-induced MMP-2 activity and MMP-14 and basigin protein expression are mediated via the angiotensin ii receptor type 1-mitogen-activated protein kinase 1 pathway in retinal pigment epithelium: Implications for age-related macular degeneration. Am. J. Pathol. 2011, 178, 2665–2681. [Google Scholar] [CrossRef]
- Kamei, M.; Hollyfield, J.G. TIMP-3 in Bruch’s membrane: Changes during aging and in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 1999, 40, 2367–2375. [Google Scholar]
- Bailey, T.A.; Alexander, R.A.; Dubovy, S.R.; Luthert, P.J.; Victor Chong, N.H. Measurement of TIMP-3 expression and Bruch’s membrane thickness in human macula. Exp. Eye Res. 2001, 73, 851–858. [Google Scholar] [CrossRef]
- Krogh Nielsen, M.; Subhi, Y.; Rue Molbech, C.; Nilsson, L.L.; Nissen, M.H.; Sørensen, T.L. Imbalances in tissue inhibitors of metalloproteinases differentiate choroidal neovascularization from geographic atrophy. Acta Ophthalmol. 2019, 97, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Lechner, J.; O’Leary, O.E.; Stitt, A.W. The pathology associated with diabetic retinopathy. Vis. Res. 2017, 139, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Peeters, S.A.; Engelen, L.; Buijs, J.; Chaturvedi, N.; Fuller, J.H.; Schalkwijk, C.G.; Stehouwer, C.D.; Karamanos, B.; Kofinis, A.; Petrou, K.; et al. Plasma levels of matrix metalloproteinase-2, -3, -10, and tissue inhibitor of metalloproteinase-1 are associated with vascular complications in patients with type 1 diabetes: The EURODIAB Prospective Complications Study. Cardiovasc. Diabetol. 2015, 14, 31. [Google Scholar] [CrossRef] [PubMed]
- Kowluru, R.A.; Santos, J.M.; Zhong, Q. Sirt1, A negative regulator of matrix metalloproteinase-9 in diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2014, 55, 5653–5660. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.Y.; Liang, I.C.; Li, H.J.; Wu, C.C.; Lo, H.M.; Chang, D.C.; Hung, C.F. Chrysin inhibits high glucose-induced migration on chorioretinal endothelial cells via VEGF and VEGFR down-regulation. Int. J. Mol. Sci. 2020, 21, 5541. [Google Scholar] [CrossRef]
- Chen, B.; He, T.; Xing, Y.; Cao, T. Effects of quercetin on the expression of MCP-1, MMP-9 and VEGF in rats with diabetic retinopathy. Exp. Ther. Med. 2017, 14, 6022–6026. [Google Scholar] [CrossRef]
- Zhou, L.; Li, F.F.; Wang, S.M. Circ-ITCH restrains the expression of MMP-2, MMP-9 and TNF-α in diabetic retinopathy by inhibiting miR-22. Exp. Mol. Pathol. 2021, 118, 104594. [Google Scholar] [CrossRef]
- Giebel, S.J.; Menicucci, G.; McGuire, P.G.; Das, A. Matrix metalloproteinases in early diabetic retinopathy and their role in alternation of the blood-retinal barrier. Lab. Investig. 2005, 85, 597–607. [Google Scholar] [CrossRef]
- Drankowska, J.; Kos, M.; Kościuk, A.; Marzęda, P.; Boguszewska-Czubara, A.; Tylus, M.; Święch-Zubilewicz, A. MMP targeting in the battle for vision: Recent developments and future prospects in the treatment of diabetic retinopathy. Life Sci. 2019, 229, 149–156. [Google Scholar] [CrossRef]
- Kinuthia, U.M.; Wolf, A.; Langmann, T. Microglia and Inflammatory Responses in Diabetic Retinopathy. Front. Immunol. 2020, 11, 2888. [Google Scholar] [CrossRef]
- Kwon, J.W.; Choi, J.A.; Jee, D. Matrix Metalloproteinase-1 and matrix metalloproteinase-9 in the aqueous humor of diabetic macular edema patients. PLoS ONE 2016, 11, e0159720. [Google Scholar] [CrossRef] [PubMed]
- Rangasamy, S.; McGuire, P.G.; Das, A. Diabetic retinopathy and inflammation: Novel therapeutic targets. Middle East Afr. J. Ophthalmol. 2012, 19, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Ucgun, N.I.; Zeki-Fikret, C.; Yildirim, Z. Inflammation and diabetic retinopathy. Mol. Vis. 2020, 26, 718–721. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, H.; Yan, L.; Du, W.; Zhang, M.; Chen, H.; Zhang, L.; Li, G.; Li, J.; Dong, Y.; et al. MMP-2 and MMP-9 contribute to the angiogenic effect produced by hypoxia/15-HETE in pulmonary endothelial cells. J. Mol. Cell. Cardiol. 2018, 121, 36–50. [Google Scholar] [CrossRef]
- Zhang, D.; Lv, F.L.; Wang, G.H. Effects of HIF-1α on diabetic retinopathy angiogenesis and VEGF expression. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 5071–5076. [Google Scholar] [CrossRef]
- Rodrigues, M.; Xin, X.; Jee, K.; Babapoor-Farrokhran, S.; Kashiwabuchi, F.; Ma, T.; Bhutto, I.; Hassan, S.J.; Daoud, Y.; Baranano, D.; et al. VEGF secreted by hypoxic Müller cells induces MMP-2 expression and activity in endothelial cells to promote retinal neovascularization in proliferative diabetic retinopathy. Diabetes 2013, 62, 3863–3873. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, W.; Liu, F.; Tang, L.; Tang, R.; Li, W. Apoptotic effect of mtrix metalloproteinases 9 in the development of diabetic retinopathy. Int. J. Clin. Exp. Pathol. 2015, 8, 10452–10459. [Google Scholar]
- Abu El-Asrar, A.M.; Mohammad, G.; Nawaz, M.I.; Siddiquei, M.M.; Van Den Eynde, K.; Mousa, A.; De Hertogh, G.; Opdenakker, G. Relationship between vitreous levels of matrix metalloproteinases and vascular endothelial growth factor in proliferative diabetic retinopathy. PLoS ONE 2013, 8, e85857. [Google Scholar] [CrossRef]
- Abu El-Asrar, A.M.; Ahmad, A.; Bittoun, E.; Siddiquei, M.M.; Mohammad, G.; Mousa, A.; De Hertogh, G.; Opdenakker, G. Differential expression and localization of human tissue inhibitors of metalloproteinases in proliferative diabetic retinopathy. Acta Ophthalmol. 2018, 96, e27–e37. [Google Scholar] [CrossRef]
- Saucedo, L.; Pfister, I.B.; Zandi, S.; Gerhardt, C.; Garweg, J.G. Ocular TGF-β, Matrix Metalloproteinases, and TIMP-1 Increase with the Development and Progression of Diabetic Retinopathy in Type 2 Diabetes Mellitus. Mediat. Inflamm. 2021, 2021, 9811361. [Google Scholar] [CrossRef]
- Abu El-Asrar, A.M.; Ahmad, A.; Nawaz, M.I.; Siddiquei, M.M.; De Zutter, A.; Vanbrabant, L.; Gikandi, P.W.; Opdenakker, G.; Struyf, S. Tissue Inhibitor of Metalloproteinase-3 Ameliorates Diabetes-Induced Retinal Inflammation. Front. Physiol. 2022, 12, 2432. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M.; Afshari, N.A. The global state of cataract blindness. Curr. Opin. Ophthalmol. 2017, 28, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.; Lakhani, N.; Thompson, J.; Lakhani, N. Cataracts. Prim. Care Clin. Off. Pract. 2015, 42, 409–423. [Google Scholar] [CrossRef] [PubMed]
- Lam, D.; Rao, S.K.; Ratra, V.; Liu, Y.; Mitchell, P.; King, J.; Tassignon, M.J.; Jonas, J.; Pang, C.P.; Chang, D.F. Cataract. Nat. Rev. Dis. Prim. 2015, 1, 15014. [Google Scholar] [CrossRef]
- Alapure, B.V.; Praveen, M.R.; Gajjar, D.; Vasavada, A.R.; Rajkumar, S.; Johar, K. Matrix metalloproteinase-9 activity in human lens epithelial cells of cortical, posterior subcapsular, and nuclear cataracts. J. Cataract Refract. Surg. 2008, 34, 2063–2067. [Google Scholar] [CrossRef] [PubMed]
- Nathu, Z.; Dwivedi, D.J.; Reddan, J.R.; Sheardown, H.; Margetts, P.J.; West-Mays, J.A. Temporal changes in MMP mRNA expression in the lens epithelium during anterior subcapsular cataract formation. Exp. Eye Res. 2009, 88, 323–330. [Google Scholar] [CrossRef]
- Li, K.; Ai, W. Investigation of expression and effects of TGF-β1 and MMP-9 in lens epithelial cells of diabetic cataract rats. Exp. Ther. Med. 2019, 17, 4522–4526. [Google Scholar] [CrossRef]
- Alapure, B.V.; Praveen, M.R.; Gajjar, D.U.; Vasavada, A.R.; Parmar, T.J.; Arora, A.I. Matrix metalloproteinase-2 and -9 activities in the human lens epithelial cells and serum of steroid induced posterior subcapsular cataracts. Mol. Vis. 2012, 18, 64–73. [Google Scholar]
- Dwivedi, D.J.; Pino, G.; Banh, A.; Nathu, Z.; Howchin, D.; Margetts, P.; Sivak, J.G.; West-Mays, J.A. Matrix metalloproteinase inhibitors suppress transforming growth factor-β-induced subcapsular cataract formation. Am. J. Pathol. 2006, 168, 69–79. [Google Scholar] [CrossRef]
- Lamouille, S.; Xu, J.; Derynck, R. Molecular mechanisms of epithelial-mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2014, 15, 178–196. [Google Scholar] [CrossRef]
- Scheau, C.; Badarau, I.A.; Costache, R.; Caruntu, C.; Mihai, G.L.; Didilescu, A.C.; Constantin, C.; Neagu, M. The role of matrix metalloproteinases in the epithelial-mesenchymal transition of hepatocellular carcinoma. Anal. Cell. Pathol. 2019, 2019, 9423907. [Google Scholar] [CrossRef]
- Korol, A.; Pino, G.; Dwivedi, D.; Robertson, J.V.; Deschamps, P.A.; West-Mays, J.A. Matrix metalloproteinase-9-null mice are resistant to TGF-β-induced anterior subcapsular cataract formation. Am. J. Pathol. 2014, 184, 2001–2012. [Google Scholar] [CrossRef] [PubMed]
- Turan, M.; Turan, G. Immunoreactivity of ICAM-1, MMP-2, and Nesfatin-1 in lens epithelial cells of patients with diabetes mellitus with or without diabetic retinopathy. Eur. J. Ophthalmol. 2022, 32, 255–262. [Google Scholar] [CrossRef]
- Jackson, H.W.; Defamie, V.; Waterhouse, P.; Khokha, R. TIMPs: Versatile extracellular regulators in cancer. Nat. Rev. Cancer 2017, 17, 38–53. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Hu, D.N.; Sun, J.; Zhou, J. Correlations Between MMPs and TIMPs Levels in Aqueous Humor from High Myopia and Cataract Patients. Curr. Eye Res. 2017, 42, 600–603. [Google Scholar] [CrossRef] [PubMed]
- Kubo, E.; Shibata, T.; Singh, D.P.; Sasaki, H. Roles of TGF β and FGF signals in the lens: Tropomyosin regulation for posterior capsule opacity. Int. J. Mol. Sci. 2018, 19, 3093. [Google Scholar] [CrossRef]
- Shimada, A.; Miyata, Y.; Kosano, H. Type i collagen accelerates the spreading of lens epithelial cells through the expression and activation of matrix metalloproteinases. Curr. Eye Res. 2014, 39, 460–471. [Google Scholar] [CrossRef]
- Hazra, S.; Guha, R.; Jongkey, G.; Palui, H.; Mishra, A.; Vemuganti, G.K.; Basak, S.K.; Mandal, T.K.; Konar, A. Modulation of matrix metalloproteinase activity by EDTA prevents posterior capsular opacification. Mol. Vis. 2012, 18, 1701–1711. [Google Scholar]
- Awasthi, N.; Wang-Su, S.T.; Wagner, B.J. Downregulation of MMP-2 and -9 by proteasome inhibition: A possible mechanism to decrease LEC migration and prevent posterior capsular opacification. Investig. Ophthalmol. Vis. Sci. 2008, 49, 1998–2003. [Google Scholar] [CrossRef]
- Yao, J.; Yang, W.; Liu, Y.; Sun, Y.X.; Jiang, Q. Dexamethasone inhibits TGF-β2-induced migration of human lens epithelial cells: Implications for posterior capsule opacification prevention. Mol. Med. Rep. 2012, 5, 1509–1513. [Google Scholar] [CrossRef]
- Chang, K.C.; Petrash, J.M. Aldose reductase mediates transforming growth factor β2 (TGF-β2)–inducedmigration and epithelial-to-mesenchymal transition of lens-derived epithelial cells. Investig. Ophthalmol. Vis. Sci. 2015, 56, 4198–4210. [Google Scholar] [CrossRef] [PubMed]
- Taiyab, A.; Korol, A.; Deschamps, P.A.; West-Mays, J.A. β-catenin/CBP–dependent signaling regulates TGF-β– induced epithelial to mesenchymal transition of lens epithelial cells. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5736–5747. [Google Scholar] [CrossRef]
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. The Ocular Surface TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Bron, A.J.; de Paiva, C.S.; Chauhan, S.K.; Bonini, S.; Gabison, E.E.; Jain, S.; Knop, E.; Markoulli, M.; Ogawa, Y.; Perez, V.; et al. TFOS DEWS II pathophysiology report. Ocul. Surf. 2017, 15, 438–510. [Google Scholar] [CrossRef]
- Jamerson, E.C.; Elhusseiny, A.M.; ElSheikh, R.H.; Eleiwa, T.K.; El Sayed, Y.M. Role of Matrix Metalloproteinase 9 in Ocular Surface Disorders. Eye Contact Lens 2020, 46, S57–S63. [Google Scholar] [CrossRef] [PubMed]
- Shoari, A.; Kanavi, M.R.; Rasaee, M.J. Inhibition of matrix metalloproteinase-9 for the treatment of dry eye syndrome; a review study. Exp. Eye Res. 2021, 205, 108523. [Google Scholar] [CrossRef]
- Tamhane, M.; Cabrera-Ghayouri, S.; Abelian, G.; Viswanath, V. Review of Biomarkers in Ocular Matrices: Challenges and Opportunities. Pharm. Res. 2019, 36, 40. [Google Scholar] [CrossRef]
- Wiechmann, A.F.; Ceresa, B.P.; Howard, E.W. Diurnal Variation of Tight Junction Integrity Associates Inversely with Matrix Metalloproteinase Expression in Xenopus laevis Corneal Epithelium: Implications for Circadian Regulation of Homeostatic Surface Cell Desquamation. PLoS ONE 2014, 9, e113810. [Google Scholar] [CrossRef]
- Pflugfelder, S.C. Tear Dysfunction and the Cornea: LXVIII Edward Jackson Memorial Lecture. Am. J. Ophthalmol. 2011, 152, 900–909.e1. [Google Scholar] [CrossRef]
- Li, J.; Deng, R.; Hua, X.; Zhang, L.; Lu, F.; Coursey, T.G.; Pflugfelder, S.C.; Li, D.Q. Blueberry Component Pterostilbene Protects Corneal Epithelial Cells from Inflammation via Anti-oxidative Pathway. Sci. Rep. 2016, 6, srep19408. [Google Scholar] [CrossRef]
- Seo, M.J.; Kim, J.M.; Lee, M.J.; Sohn, Y.S.; Kang, K.K.; Yoo, M. The Therapeutic Effect of DA-6034 on Ocular Inflammation via Suppression of MMP-9 and Inflammatory Cytokines and Activation of the MAPK Signaling Pathway in an Experimental Dry Eye Model. Curr. Eye Res. 2010, 35, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Shim, W.; Kim, C.E.; Choi, S.Y.; Lee, H.; Yang, J. Therapeutic efficacy of nanocomplex of poly(ethylene glycol) and catechin for dry eye disease in a mouse model. Investig. Ophthalmol. Vis. Sci. 2017, 58, 1682–1691. [Google Scholar] [CrossRef] [PubMed]
- Xiao, F.; Cui, H.; Zhong, X. Beneficial effect of daidzin in dry eye rat model through the suppression of inflammation and oxidative stress in the cornea. Saudi J. Biol. Sci. 2016, 25, 832–837. [Google Scholar] [CrossRef]
- Shim, W.; Eun, C.; Lee, M.; Hyeon, S.; Park, J.; Do, M. Catechin solubilization by spontaneous hydrogen bonding with poly (ethylene glycol) for dry eye therapeutics. J. Control. Release 2019, 307, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Sambursky, R.; Davitt, W.F., 3rd; Latkany, R.; Tauber, S.; Starr, C.; Friedberg, M.; Dirks, M.S.; Mcdonald, M. Sensitivity and Specificity of a Point-of-Care Matrix Metalloproteinase 9 Immunoassay for Diagnosing Inflammation Related to Dry Eye. JAMA Ophthalmol. 2013, 131, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Lanza, N.L.; Mcclellan, A.; Batawi, H.; Felix, E.R.; Sarantopoulos, K.D.; Levitt, R.C.; Galor, A. Dry Eye Profiles in Patients with a Positive Elevated Surface Matrix Metalloproteinase 9 Point-of-Care Test Versus Negative Patients. Ocul. Surf. 2016, 14, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Vandermeid, K.R.; Su, S.P.; Ward, K.W.; Zhang, J.Z. Correlation of tear inflammatory cytokines and matrix metalloproteinases with four dry eye diagnostic tests. Investig. Ophthalmol. Vis. Sci. 2012, 53, 1512–1518. [Google Scholar] [CrossRef]
- Kook, K.Y.; Jin, R.; Li, L.; Yoon, H.J.; Yoon, K.C. Tear osmolarity and matrix metallopeptidase-9 in dry eye associated with Sjögren’s syndrome. Korean J. Ophthalmol. 2020, 34, 179–186. [Google Scholar] [CrossRef]
- Aragona, P.; Aguennouz, M.H.; Rania, L.; Postorino, E.; Sommario, M.S.; Roszkowska, A.M.; de Pasquale, M.G.; Pisani, A.; Puzzolo, D. Matrix Metalloproteinase 9 and Transglutaminase 2 Expression at the Ocular Surface in Patients with Different Forms of Dry Eye Disease. Ophthalmology 2015, 122, 62–71. [Google Scholar] [CrossRef]
- Lee, Y.H.; Bang, S.P.; Shim, K.Y.; Son, M.J.; Kim, H.; Jun, J.H. Association of tear matrix metalloproteinase 9 immunoassay with signs and symptoms of dry eye disease: A cross-sectional study using qualitative, semiquantitative, and quantitative strategies. PLoS ONE 2021, 16, e0258203. [Google Scholar] [CrossRef]
- Schargus, M.; Ivanova, S.; Kakkassery, V.; Dick, H.B.; Joachim, S. Correlation of tear film osmolarity and 2 different MMP-9 tests with common dry eye tests in a cohort of non-dry eye patients. Cornea 2015, 34, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Shen, G.; Ma, X. High levels of 17 β -estradiol are associated with increased matrix metalloproteinase-2 and metalloproteinase-9 activity in tears of postmenopausal women with dry eye. J. Ophthalmol. 2016, 2016, 2415867. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.C.; Ryu, H.W.; Lee, H.J.; Kim, M.S. Bevacizumab eye drops delay corneal epithelial wound healing and increase the stromal response to epithelial injury in rats. Clin. Exp. Ophthalmol. 2013, 41, 694–701. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Stankowska, D.L.; Ellis, D.Z.; Krishnamoorthy, R.R.; Yorio, T. Targets of Neuroprotection in Glaucoma. J. Ocul. Pharmacol. Ther. 2018, 34, 85–106. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.M. Glaucoma. Med. Clin. N. Am. 2021, 105, 493–510. [Google Scholar] [CrossRef]
- Tabak, S.; Schreiber-Avissar, S.; Beit-Yannai, E. Trabecular meshwork’s collagen network formation is inhibited by non-pigmented ciliary epithelium-derived extracellular vesicles. J. Cell. Mol. Med. 2021, 25, 3339–3347. [Google Scholar] [CrossRef]
- Nga, A.D.; Yap, S.L.; Samsudin, A.; Abdul-Rahman, P.S.; Hashim, O.H.; Mimiwati, Z. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in the aqueous humour of patients with primary angle closure glaucoma—A quantitative study. BMC Ophthalmol. 2014, 14, 33. [Google Scholar] [CrossRef]
- Markiewicz, L.; Pytel, D.; Mucha, B.; Szymanek, K.; Szaflik, J.; Szaflik, J.P.; Majsterek, I. Altered expression levels of MMP1, MMP9, MMP12, TIMP1, and IL-1 β as a risk factor for the elevated IOP and optic nerve head damage in the primary open-angle glaucoma patients. BioMed Res. Int. 2015, 2015, 812503. [Google Scholar] [CrossRef]
- Sahay, P.; Rao, A.; Padhy, D.; Sarangi, S.; Das, G.; Reddy, M.M.; Modak, R. Functional activity of matrix metalloproteinases 2 and 9 in tears of patients with glaucoma. Investig. Ophthalmol. Vis. Sci. 2017, 58, 106–113. [Google Scholar] [CrossRef]
- Robertson, J.V.; Siwakoti, A.; West-Mays, J.A. Altered expression of transforming growth factor beta 1 and matrix metalloproteinase-9 results in elevated intraocular pressure in mice. Mol. Vis. 2013, 19, 684–695. [Google Scholar]
- O’callaghan, J.; Cassidy, P.S.; Humphries, P. Open-angle glaucoma: Therapeutically targeting the extracellular matrix of the conventional outflow pathway. Expert Opin. Ther. Targets 2017, 21, 1037–1050. [Google Scholar] [CrossRef] [PubMed]
- De Groef, L.; Andries, L.; Siwakoti, A.; Geeraerts, E.; Bollaerts, I.; Noterdaeme, L.; Etienne, I.; Papageorgiou, A.; Stalmans, I.; Billen, J.; et al. Aberrant Collagen Composition of the Trabecular Meshwork Results in Reduced Aqueous Humor Drainage and Elevated IOP in MMP-9 Null Mice. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5984–5995. [Google Scholar] [CrossRef] [PubMed]
- Filla, M.S.; Dimeo, K.D.; Tong, T.; Peters, D.M. Disruption of fi bronectin matrix affects type IV collagen, fi brillin and laminin deposition into extracellular matrix of human trabecular meshwork (HTM) cells. Exp. Eye Res. 2017, 165, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yan, H.; Li, G.; Zhang, Y. Higher TGF-β1, TGF-β2, MMP-2, and TIMP-1 Levels in the Aqueous Humor of Patients with Acute Primary Angle Closure. Ophthalmic Res. 2021, 64, 62–67. [Google Scholar] [CrossRef]
- Schlötzer-Schrehardt, U.; Lommatzsch, J.; Küchle, M.; Konstas, A.G.P.; Naumann, G.O.H. Matrix Metalloproteinases and Their Inhibitors in Aqueous Humor of Patients with Pseudoexfoliation Syndrome / Glaucoma and Primary Open-Angle Glaucoma. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1117–1125. [Google Scholar] [CrossRef]
- Määttä, M.; Tervahartiala, T.; Harju, M.; Airaksinen, J.; Autio-Harmainen, H.; Sorsa, T. Matrix metalloproteinases and their tissue inhibitors in aqueous humor of patients with primary open-angle glaucoma, exfoliation syndrome, and exfoliation glaucoma. J. Glaucoma 2005, 14, 64–69. [Google Scholar] [CrossRef]
- Rönkkö, S.; Rekonen, P.; Kaarniranta, K. Matrix metalloproteinases and their inhibitors in the chamber angle of normal eyes and patients with primary open-angle glaucoma and exfoliation glaucoma. Graefes Arch. Clin. Exp. Ophthalmol. 2007, 245, 697–704. [Google Scholar] [CrossRef]
- Qian, T.; Fu, M.; Hu, C.; Zhang, Z.; Xu, X.; Zou, H. Imbalance of Matrix Metalloproteinases and Their Inhibitors Is Correlated With Trabeculectomy Outcomes in Acute Primary Angle Closure. Am. J. Ophthalmol. 2020, 212, 144–152. [Google Scholar] [CrossRef]
- Fountoulakis, N.; Labiris, G.; Aristeidou, A.; Katsanos, A.; Tentes, I.; Kortsaris, A.; Kozobolis, V.P. Tissue inhibitor of metalloproteinase 4 in aqueous humor of patients with primary open angle glaucoma, pseudoexfoliation syndrome and pseudoexfoliative glaucoma and its role in proteolysis imbalance. BMC Ophthalmol. 2013, 13, 69. [Google Scholar] [CrossRef]
- Ashworth Briggs, E.L.; Toh, T.; Eri, R.; Hewitt, A.W.; Cook, A.L. TIMP1, TIMP2, and TIMP4 are increased in aqueous humor from primary open angle glaucoma patients. Mol. Vis. 2015, 21, 1162–1172. [Google Scholar]
- Gerometta, R.; Spiga, M.; Borra, T. Treatment of Sheep Steroid-Induced Ocular Hypertension with a Glucocorticoid-Inducible MMP1 Gene Therapy Virus. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3042–3048. [Google Scholar] [CrossRef] [PubMed]
- Spiga, M.; Borrás, T. Development of a Gene Therapy Virus with a Glucocorticoid-Inducible MMP1 for the Treatment of Steroid Glaucoma. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3029–3041. [Google Scholar] [CrossRef] [PubMed]
- Gaton, D.D.; Sagara, T.; Lindsey, J.D.; Weinreb, R.N. Matrix metalloproteinase-1 localization in the normal human uveoscleral outflow pathway. Investig. Ophthalmol. Vis. Sci. 1999, 40, 363–369. [Google Scholar]
- O’Callaghan, J.; Crosbie, D.E.; Cassidy, P.S.; Sherwood, J.M.; Flügel-Koch, C.; Lütjen-Drecoll, E.; Humphries, M.M.; Reina-Torres, E.; Wallace, D.; Kiang, A.S.; et al. Therapeutic potential of AAV-mediated MMP-3 secretion from corneal endothelium in treating glaucoma. Hum. Mol. Genet. 2017, 26, 1230–1246. [Google Scholar] [CrossRef]
- Medina-Ortiz, W.E.; Belmares, R.; Neubauer, S.; Wordinger, R.J.; Clark, A.F. Cellular Fibronectin Expression in Human Trabecular Meshwork and Induction by Transforming Growth Factor-β2. Investig. Ophthalmol. Vis. Sci. 2013, 54, 6779–6788. [Google Scholar] [CrossRef]
- Acott, T.S.; Kelley, M.J.; Keller, K.E.; Vranka, J.A.; Abu-Hassan, D.W.; Li, X.; Aga, M.; Bradley, J.M. Intraocular Pressure Homeostasis: Maintaining Balance in a High-Pressure Environment. J. Ocul. Pharnacol Ther. 2014, 30, 94–101. [Google Scholar] [CrossRef]
- Rajashekhar, G.; Shivanna, M.; Kompella, U.B.; Wang, Y.; Srinivas, S.P. Role of MMP-9 in the breakdown of barrier integrity of the corneal endothelium in response to TNF-α. Exp. Eye Res. 2014, 122, 77–85. [Google Scholar] [CrossRef]
- Clark, A.F.; Steely, H.T.; Dickerson Jr, J.E.; English-Wright, S.; Stropki, K.; McCartney, M.D.; Jacobson, N.; Shepard, A.R.; Clark, J.I.; Matsushima, H.; et al. Glucocorticoid induction of the glaucoma gene MYOC in human and monkey trabecular meshwork cells and tissues. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1769–1780. [Google Scholar]
- Snyder, R.W.; Stamer, W.D.; Kramer, T.R.; Seftor, R.E. Corticosteroid treatment and trabecular meshwork proteases in cell and organ culture supernatants. Exp. Eye Res. 1993, 57, 461–468. [Google Scholar] [CrossRef]
- el-Shabrawi, Y.; Eckhardt, M.; Berghold, A.; Faulborn, J.; Auboeck, L.; Mangge, H.; Ardjomand, N. Synthesis pattern of matrix metalloproteinases (MMPs) and inhibitors (TIMPs) in human explant organ cultures after treatment with latanoprost and dexamethasone. Eye 2000, 14, 375–383. [Google Scholar] [CrossRef]
- Heo, J.Y.; Ooi, Y.H.; Rhee, D.J. Effect of prostaglandin analogs: Latanoprost, bimatoprost, and unoprostone on matrix metalloproteinases and their inhibitors in human trabecular meshwork endothelial cells. Exp. Eye Res. 2020, 194, 108019. [Google Scholar] [CrossRef] [PubMed]
- Zalewska, R.; Reszeć, J.; Kisielewski, W.; Mariak, Z. Metalloproteinase 9 and TIMP-1 expression in retina and optic nerve in absolute angle closure glaucoma. Adv. Med. Sci. 2016, 61, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Manabe, S.; Gu, Z.; Lipton, S.A. Activation of Matrix Metalloproteinase-9 via Neuronal Nitric Oxide Synthase Contributes to NMDA-Induced Retinal Ganglion Cell Death. Investig. Ophthalmol. Vis. Sci. 2005, 46, 4747–4753. [Google Scholar] [CrossRef]
- Burugula, B.; Ganesh, B.S.; Chintala, S.K. Curcumin attenuates staurosporine-mediated death of retinal ganglion cells. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4263–4273. [Google Scholar] [CrossRef]
- Santibanez, J.F.; Obradović, H.; Kukolj, T.; Krstić, J. Transforming growth factor-β, matrix metalloproteinases, and urokinase-type plasminogen activator interaction in the cancer epithelial to mesenchymal transition. Dev. Dyn. 2018, 247, 382–395. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.; Zhao, T.; Sullivan, R.D.; Reed, G.L. N EUROSCIENCE Matrix Metalloproteinase-9 Expression is Enhanced by Ischemia and Tissue Plasminogen Activator and Induces Hemorrhage, Disability and Mortality in Experimental Stroke. Neuroscience 2021, 460, 120–129. [Google Scholar] [CrossRef]
- Caban, M.; Lewandowska, U. Polyphenols and Posterior Segment Eye Diseases: Effects on Angiogenesis, Invasion, Migration and Epithelial-Mesenchymal Transition. Food Rev. Int. 2021, 1–29. [Google Scholar] [CrossRef]
- De Groef, L.; Salinas-Navarro, M.; Van Imschoot, G.; Libert, C.; Vandenbroucke, R.E.; Moons, L. Decreased TNF Levels and Improved Retinal Ganglion Cell Survival in MMP-2 Null Mice Suggest a Role for MMP-2 as TNF Sheddase. Mediat. Inflamm. 2015, 2015, 108617. [Google Scholar] [CrossRef]
- Bachu, R.D.; Chowdhury, P.; Al-Saedi, Z.H.F.; Karla, P.K.; Boddu, S.H.S. Ocular drug delivery barriers—role of nanocarriers in the treatment of anterior segment ocular diseases. Pharmaceutics 2018, 10, 28. [Google Scholar] [CrossRef]
- Suri, R.; Neupane, Y.R.; Mehra, N.; Jain, G.K.; Kohli, K. Sirolimus loaded Polyol modified liposomes for the treatment of Posterior Segment Eye Diseases. Med. Hypotheses 2019, 136, 109518. [Google Scholar] [CrossRef]
- Chojnacka, K.; Sosnowska, D.; Polka, D.; Owczarek, K.; Gorlach-Lira, K.; Oliveira De Verasa, B.; Lewandowska, U. Comparison of phenolic compounds, antioxidant and cytotoxic activity of extracts prepared from Japanese quince (Chaenomeles japonica L.) leaves. J. Physiol. Pharmacol. 2020, 71, 213–222. [Google Scholar] [CrossRef]
- Chojnacka, K.; Owczarek, K.; Caban, M.; Sosnowska, D.; Polka, D.; Koziolkiewicz, M.; Fichna, J.; Lewandowska, U. Japanese quince (Chaenomeles japonica) leaf phenol extract as modulator of the inflammatory response in lipopolysaccharide-triggered murine macrophage raw 264.7 cells. J. Physiol. Pharmacol. 2020, 71, 833–843. [Google Scholar] [CrossRef]
- Caban, M.; Owczarek, K.; Chojnacka, K.; Lewandowska, U. Overview of Polyphenols and Polyphenol-rich Extracts as Modulators of Inflammatory Response in Dry Eye Syndrome. Food Rev. Int. 2021, 1–28. [Google Scholar] [CrossRef]
- Caban, M.; Lewandowska, U. Inhibiting effects of polyphenols on angiogenesis and epithelial-mesenchymal transition in anterior segment eye diseases. J. Funct. Foods 2021, 87, 104761. [Google Scholar] [CrossRef]
- Lee, H.S.; Jun, J.H.; Jung, E.H.; Koo, B.A.; Kim, Y.S. Epigalloccatechin-3-gallate inhibits ocular neovascularization and vascular permeability in human retinal pigment epithelial and human retinal microvascular endothelial cells via suppression of MMP-9 and VEGF activation. Molecules 2014, 19, 12150–12172. [Google Scholar] [CrossRef]
- Shanmuganathan, S.; Angayarkanni, N. Chebulagic acid Chebulinic acid and Gallic acid, the active principles of Triphala, inhibit TNFα induced pro-angiogenic and pro-inflammatory activities in retinal capillary endothelial cells by inhibiting p38, ERK and NFkB phosphorylation. Vascul. Pharmacol. 2018, 108, 23–35. [Google Scholar] [CrossRef]
- Cheng, S.C.; Wu, Y.H.; Huang, W.C.; Pang, J.H.S.; Huang, T.H.; Cheng, C.Y. Anti-inflammatory property of quercetin through downregulation of ICAM-1 and MMP-9 in TNF-α-activated retinal pigment epithelial cells. Cytokine 2019, 116, 48–60. [Google Scholar] [CrossRef]
- Chen, L.X.; He, Y.J.; Zhao, S.Z.; Wu, J.G.; Wang, J.T.; Zhu, L.M.; Lin, T.T.; Sun, B.C.; Li, X.R. Inhibition of tumor growth and vasculogenic mimicry by cucumin through downregulation of the EphA2/PI3K/MMP pathway in a murine choroidal melanoma model. Cancer Biol. Ther. 2011, 11, 229–235. [Google Scholar] [CrossRef]
- Razali, N.; Agarwal, R.; Agarwal, P.; Tripathy, M.; Kapitonova, M.Y.; Kutty, M.K.; Smirnov, A.; Khalid, Z.; Ismail, N.M. Topical trans-resveratrol ameliorates steroid-induced anterior and posterior segment changes in rats. Exp. Eye Res. 2016, 143, 9–16. [Google Scholar] [CrossRef]
- Razali, N.; Agarwal, R.; Agarwal, P.; Froemming, G.R.A.; Tripathy, M.; Ismail, N.M. IOP lowering effect of topical trans-resveratrol involves adenosine receptors and TGF-β2 signaling pathways. Eur. J. Pharmacol. 2018, 838, 1–10. [Google Scholar] [CrossRef]
- Miyata, Y.; Tatsuzaki, J.; Yang, J.; Kosano, H. Potential therapeutic agents, polymethoxylated flavones isolated from Kaempferia parviflora for cataract prevention through inhibition of matrix metalloproteinase-9 in lens epithelial cells. Biol. Pharm. Bull. 2019, 42, 1658–1664. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.H.; Liu, B.Q.; Hao, M.J.; Fan, Y.X.; Qian, C.; Teng, P.; Zhou, X.W.; Hu, L.; Liu, W.T.; Yuan, Z.L.; et al. Paeoniflorin Suppressed High Glucose-Induced Retinal Microglia MMP-9 Expression and Inflammatory Response via Inhibition of TLR4/NF-κB Pathway Through Upregulation of SOCS3 in Diabetic Retinopathy. Inflammation 2017, 40, 1475–1486. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.L.; Cheng, Y.W.; Yu, M.; Ho, J.-D.; Kuo, Y.C.; Chiou, G.C.Y.; Chang, H.M.; Lee, T.H.; Hsiao, G. The fungus-derived retinoprotectant theissenolactone C improves glaucoma-like injury mediated by MMP-9 inhibition. Phytomedicine 2019, 56, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Bi, M.; Hose, N.; Xu, C.; Zhang, C.; Sassoon, J.; Song, E. Nonlethal Levels of Zeaxanthin Inhibit Cell Migration, Invasion, and Secretion of MMP-2 via NF-κB Pathway in Cultured Human Uveal Melanoma Cells. J. Ophthalmol. 2016, 2016, 8734309. [Google Scholar] [CrossRef] [PubMed]
- Rahmawaty, S.; Charlton, K.; Meyer, B.J. Development and validation of a food frequency questionnaire to assess omega-3 long chain polyunsaturated fatty acid intake in Australian children aged 9–13 years. J. Hum. Nutr. Diet. 2016, 30, 429–438. [Google Scholar] [CrossRef]
- Suzumura, A.; Terao, R.; Kaneko, H. Protective Effects and Molecular Signaling of n-3 Fatty Acids on Oxidative Stress and Inflammation in Retinal Diseases. Antioxidants 2020, 9, 920. [Google Scholar] [CrossRef]
- Fu, Z.; Liegl, R.; Wang, Z.; Gong, Y.; Liu, C.; Sun, Y.; Cakir, B.; Burnim, S.B.; Meng, S.S.; Löfqvist, C.; et al. Adiponectin Mediates Dietary Omega-3 Long-Chain Polyunsaturated Fatty Acid Protection Against Choroidal Neovascularization in Mice. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3862–3870. [Google Scholar] [CrossRef]
- Epitropoulos, A.T.; Donnenfeld, E.D.; Shah, Z.A.; Holland, E.J.; Gross, M.; Faulkner, W.J.; Matossian, C.; Lane, S.S.; Toyos, M.; Bucci, F.A.; et al. Effect of oral re-esterified Omega-3 nutritional supplementation on dry eyes. Cornea 2016, 35, 1185–1191. [Google Scholar] [CrossRef]
- Park, J.; Yoo, Y.S.; Shin, E.; Han, G.; Shin, K.; Lim, D.H.; Chung, T.Y. Effects of the re-esterified triglyceride (rTG) form of omega-3 supplements on dry eye following cataract surgery. Br. J. Ophthalmol. 2021, 105, 1504–1509. [Google Scholar] [CrossRef]
- Djordjevic, B.; Cvetkovic, T.; Stoimenov, T.J.; Despotovic, M.; Zivanovic, S.; Basic, J.; Veljkovic, A.; Velickov, A.; Kocic, G.; Pavlovic, D.; et al. Oral supplementation with melatonin reduces oxidative damage and concentrations of inducible nitric oxide synthase, VEGF and matrix metalloproteinase 9 in the retina of rats with streptozotocin/nicotinamide induced pre-diabetes. Eur. J. Pharmacol. 2018, 833, 290–297. [Google Scholar] [CrossRef]
- Zhou, J.; Jin, B.; Jin, Y.; Liu, Y.; Pan, J. The antihelminthic drug niclosamide effectively inhibits the malignant phenotypes of uveal melanoma in vitro and in vivo. Theranostics 2017, 7, 1447–1462. [Google Scholar] [CrossRef] [PubMed]
- Maddineni, P.; Kasetti, R.B.; Kodati, B.; Yacoub, S.; Zode, G.S. Sodium 4-phenylbutyrate reduces ocular hypertension by degrading extracellular matrix deposition via activation of MMP9. Int. J. Mol. Sci. 2021, 22, 10095. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.L.; Sung, K.R.; Kwon, J.; Shin, J.A. Statins suppress TGF-β2-Mediated MMP-2 and MMP-9 expression and activation through RhoA/ROCK inhibition in astrocytes of the human optic nerve head. Investig. Ophthalmol. Vis. Sci. 2020, 61, 29. [Google Scholar] [CrossRef] [PubMed]

| Agent | Cell Line | Concentration/Duration | Biological Effects/Findings | Reference |
|---|---|---|---|---|
| Diabetic retinopathy | ||||
| Chrysin (5,7-dihydroxyflavone) | Glucose-induced rhesus macaque choroid-retinal endothelial cells (RF/6A) | 3, 10, 30 μM for 0.5, 16, 24 h | ↓MMP-2 protein; ↓VEGFR1, VEGFR2 mRNA and protein; ↓VEGF, HIF1α protein; ↓p-Akt, p-ERK protein; ↓ migration | [99] |
| Paeoniflorin | Glucose-induced BV2 cells | 0.1. 1, 10 μM for 6 h | ↓MMP-9 activity; ↓p-p38 protein; ↓NF-κB translocation from the cytosol to the nucleus | [206] |
| Age-related macular degeneration | ||||
| Chebulagic acid | TNF-α-induced Rhesus monkey choroidal- retinal endothelial cells (RF/6A) | 1, 5, 10, 25, 50, 100 μM for 4, 48 h | ↓MMP-9 mRNA, protein, activity; ↓PDGF-BB, IL-6, IL-8, MCP-1, MIP-1b, p-ERK1/2, p-NF-κB, p-p38 protein; ↓tube formation | [200] |
| Chebulinic acid | TNF-α-induced rhesus monkey choroidal- retinal endothelial cells (RF/6A) | 1, 5, 10, 25, 50, 100 μM for 4, 48 h | ↓MMP-9 mRNA, protein, activity; ↓PDGF-BB, IL-6, IL-8, MCP-1, MIP-1b, p-ERK1/2, p-NF-κB, p-p38 protein; ↓tube formation | [200] |
| EGCG | H2O2/TPA/ TNF-α-induced human retinal pigment epithelial cells (ARPE-19) + VEGF-induced human retinal microvascular endothelial cells | 1, 10, 25, 50 μM for 24 h | ↓MMP-9 mRNA, protein, activity; ↓MMP-2 activity; ↓VEGF, VEGFR-2 mRNA; ↓tube formation | [199] |
| Gallic acid (3,4,5-Trihydroxybenzoic acid) | TNF-α-induced Rhesus monkey choroidal- retinal endothelial cells (RF/6A) | 1, 10, 50, 100 μM for 4, 48 h | ↓MMP-9 mRNA, protein, activity; ↓IL-6, IL-8, MCP-1, p-ERK1/2, p-NF-κB, p-p38 protein; ↓tube formation | [200] |
| Quercetin (3,3′,4′,5,7-pentahydroxyflavone) | TNF-α-induced human retinal pigment epithelial cells (ARPE-19) | 5, 10, 50, 100 μM for 1, 4, 6, 48 h | ↓MMP-9 mRNA and activity; ↓ICAM-1 mRNA and protein; ↓p-JNK1, p-JNK2, p-ERK1, p-ERK2, p-p65 protein | [201] |
| Dry eye syndrome | ||||
| Pterostilbene (trans-3,5-dimethoxy-4-hydroxystilbene) | Hyperosmotic stress-induced primary human corneal epithelial cells | For mRNA expression: 5, 10, 20 μM for 4 h For protein expression and MMPs activity: 5, 10, 20 μM for 24 h | ↓MMP-2 mRNA and activity ↓MMP-9 mRNA and activity ↓IL-1β, IL-6, TNF-α mRNA and protein ↓COX-2 mRNA and protein ↑SOD1 mRNA and protein ↑PRDX4 mRNA and protein | [144] |
| Ocular cancers | ||||
| Eriodictyol | Y79 cells | 25, 50, 100 μM for 24 h | ↓MMP-2 and MMP-9 protein; ↓ p-Akt, p-PI3K protein; ↑cleaved caspase-3 protein; ↓invasion; ↓migration | [64] |
| Niclosamide | 92.1, Mel270, Omm1, Omm2.3 cells | 1–10 μmol/L for 24, 36, 48 h | ↓MMP-9 protein; ↑active caspase-3 protein; ↓NF-κB activation; ↓p-GSK3β, p-β-catenin protein; ↓invasion; ↓migration; ↓proliferation | [215] |
| Zeaxanthin | C918 cells | 3–10 μM for 0.5, 8, 16, 24 h | ↓MMP-2 protein; ↓NF-κB protein; ↓invasion; ↓migration | [208] |
| Posterior capsule opacification | ||||
| Flavones isolated from Kaempferia parviflora (5,7-dimethoxyflavone; 3,5,7-trimethoxyflavone; 3,5,7,4′-tetramethoxyflavone; 3,5,7,3′,4′-pentamethoxyflavone) | Phorbol-ester-stimulated human lens epithelial cells (SRA01/04) | 0.25, 1, 4, 16, 64 μM for 24 h | ↓pro-MMP-2, pro-MMP-9 activity; ↓MMP-9 mRNA; ↑TIMP-2 protein; ↓p-JNK1, p-JNK2, p-ERK1/2, p-p38 protein | [205] |
| Glaucoma | ||||
| Sodium 4-phenylbutyrate | Dexamethasone-stimulated human primary trabecular meshwork cells | 5 mM for 24 h/7d | ↑MMP-9 mRNA and activity; ↓fibronectin, collagen I, laminin protein; ↓GRP-94, GRP-78, CHOP protein | [216] |
| Statins (simvastatin, lovastatin, atorvastatin) | TGF-β2-stimulated human primary astrocytes of optic nerve head | 5 μg/mL for 1 h | ↓MMP-2 and MMP-9 protein; ↓MMP-2 and MMP-9 activity; ↓p-MYPT1, p-mic protein | [217] |
| Agent | Animal Model | Dose/Duration | Biological Effects/Findings | Reference |
|---|---|---|---|---|
| Diabetic retinopathy | ||||
| Melatonin | Streptozotocin/nicotinamide-induced Wistar rats | 85 μg/d orally for 14 days | ↓MMP-9 protein; ↓VEGF, iNOS protein; ↓advanced oxidation protein products | [214] |
| Paeoniflorin | Streptozocin-stimulated CD-1 mice | 20, 40 mg/kg/d for 5 weeks | ↓MMP-9 activity; ↓IL-1β protein; | [206] |
| Age-related macular degeneration | ||||
| Dietary Omega-3 Long-Chain Polyunsaturated Fatty Acids | Laser-induced C57BL/6J and Apn−/− mice | Defined rodent diets with 2% omega 3-long-chain-polyunsaturated-fatty-acids (1% docosahexaenoic acid and 1% eicosapentaenoic acid) for 7 days before and after laser photocoagulation | ↓MMP-2 and MMP-9 mRNA ↓choroidal neovessels | [211] |
| Dry eye syndrome | ||||
| Catechin (flavon-3-ol) | Desiccation stress-induced NOD.B10.H2b mice | 1% catechin or 1% nanocomplex PEG/catechin as eye drops for 10 days | ↓MMP-2 protein ↓MMP-9 protein ↓IL-1β, IL-6, IL-17 protein ↓TNF-α protein ↓ICAM-1 protein ↓VCAM-1 protein ↑goblet cell density ↑tear production ↓corneal epithelium irregularities and desquamation | [146] |
| Catechin | Desiccation stress-induced NOD.B10.H2b mice | 1% catechin or 11% hydrogen nanocomplex PEG/catechin as eye drops for 10 days | ↓MMP-2 protein ↓MMP-9 protein ↓IL-1β, IL-6, IL-17 protein ↓TNF-α protein ↓ICAM-1 protein ↓VCAM-1 protein ↑goblet cell density | [148] |
| Ocular cancers | ||||
| Curcumin | C57/BL mice with the subretinal injection of melanoma B16/F10 cells | 100 mg/kg intraperitoneally for 18 days | ↓MMP-2, MMP-9 mRNA and protein; ↓PI3K, EphA2 mRNA and protein; ↓tumor size | [202] |
| Glaucoma | ||||
| Resveratrol | Steroid-stimulated Sprague-Dawley rats | Topical, 0.2% twice-daily for 3 weeks | ↑MMP-2 protein; ↑improvement of morphology of trabecular meshwork and retina; ↓IOP | [203] |
| Resveratrol | Steroid-stimulated Sprague-Dawley rats | Topical, 0.2% twice-daily for 1 week | ↑MMP-2 protein; ↑uPA, tPA protein; ↓IOP | [204] |
| Theissenolactone C | Sprague-Dawley rats with normal saline injection into the anterior chamber | Single intraperitoneal injection of 10 mg/kg | ↓MMP-9 protein and activity; ↓IL-1β, MCP-1 protein | [207] |
| Sodium 4-phenylbutyrate | Dexamethasone-stimulated C57BL/6J | 1% sodium 4-phenylbutyrate as eye drops twice daily for 5 weeks | ↓IOP; ↓fibronectin, collagen I protein | [216] |
| Agent | ClinicalTrials.gov Identifier/Phase (if Specified) | Participants/Enrollment | Dosage/Duration | Biological Effects/Findings | Reference |
|---|---|---|---|---|---|
| Dry eye syndrome | |||||
| Re-esterified omega-3 fatty acids | multicenter, prospective, interventional, placebo-controlled, double-masked study | 105 patients with DES; the omega-3 group (n = 54) or placebo group (n = 51) | 4 softgels daily with meals containing a total of either 1680 mg of eicosapentaenoic acid/560 mg of docosahexaenoic acid re-esterified omega-3 group or 3136 mg linoleic acid safflower oil as the control group for 12 weeks | ↓tear MMP-9 ↓OSDI score ↑TBUT ↓tear film osmolarity | [212] |
| Re-esterified triglyceride form of omega-3 fatty acids | prospective comparative cohort study | 66 patients complaining of new-onset non-specific typical dry eye 1 month after uncomplicated cataract surgery; the omega-3 group (n = 32) or placebo group (n = 34) | 2 tablets containing a total of 1680 mg of eicosapentaenoic acid/506 mg of docosahexaenoic acid re-esterified triglyceride form of omega-3 two times per day for 2 months along with artificial teardrops | ↓tear MMP-9 ↓OSDI score ↑tear production ↓Dry Eye Questionnaire score | [213] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caban, M.; Owczarek, K.; Lewandowska, U. The Role of Metalloproteinases and Their Tissue Inhibitors on Ocular Diseases: Focusing on Potential Mechanisms. Int. J. Mol. Sci. 2022, 23, 4256. https://doi.org/10.3390/ijms23084256
Caban M, Owczarek K, Lewandowska U. The Role of Metalloproteinases and Their Tissue Inhibitors on Ocular Diseases: Focusing on Potential Mechanisms. International Journal of Molecular Sciences. 2022; 23(8):4256. https://doi.org/10.3390/ijms23084256
Chicago/Turabian StyleCaban, Miłosz, Katarzyna Owczarek, and Urszula Lewandowska. 2022. "The Role of Metalloproteinases and Their Tissue Inhibitors on Ocular Diseases: Focusing on Potential Mechanisms" International Journal of Molecular Sciences 23, no. 8: 4256. https://doi.org/10.3390/ijms23084256
APA StyleCaban, M., Owczarek, K., & Lewandowska, U. (2022). The Role of Metalloproteinases and Their Tissue Inhibitors on Ocular Diseases: Focusing on Potential Mechanisms. International Journal of Molecular Sciences, 23(8), 4256. https://doi.org/10.3390/ijms23084256






