The Role of ABC Transporters in Skin Cells Exposed to UV Radiation
Abstract
:1. Introduction
2. ABC Transporters
3. ABC Transporters in the Skin
3.1. Activation and Suppression According to Oxidative Conditions
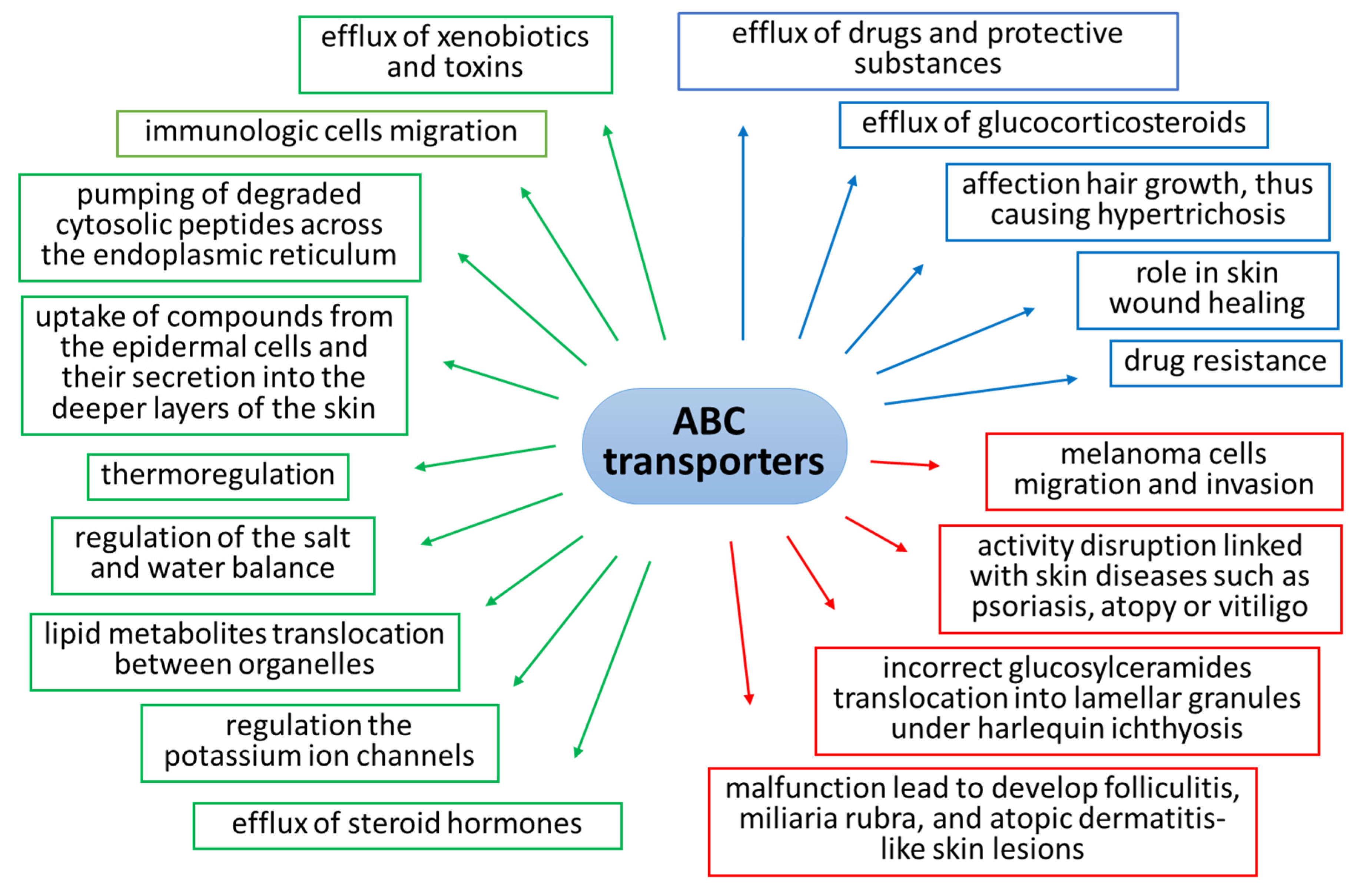
3.2. Main Functions in the Skin
4. UV Radiation and ABC Transporters’ Activity
4.1. Multi-Drug Resistance Transporters (MDR1/3)
4.2. Transporter Associated with Antigen Processing 1/2 (TAP1/2)The physiological
4.3. Cystic Fibrosis Transmembrane Conductance Regulator (CFTR)
4.4. Sulfonylurea Receptors (SUR1/2)
4.5. Breast Cancer Resistance Protein (BCRP)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elias, P.M.; Wakefield, J.S. Skin barrier function. In Nutrition for Healthy Skin: Strategies for Clinical and Cosmetic Practice; Springer: Berlin/Heidelberg, Germany, 2011; pp. 35–48. ISBN 9783642122637. [Google Scholar]
- Sleeman, M.A.; Watson, J.D.; Murison, J.G. Neonatal murine epidermal cells express a functional multidrug-resistant pump. J. Invest. Dermatol. 2000, 115, 19–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Potts, R. Skin Barrier: Principles of Percutaneous Absorption. Arch. Dermatol. 1997, 133, 924. [Google Scholar] [CrossRef]
- Prausnitz, M.R.; Mitragotri, S.; Langer, R. Current status and future potential of transdermal drug delivery. Nat. Rev. Drug Discov. 2004, 3, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Takenaka, S.; Itoh, T.; Fujiwara, R. Expression pattern of human ATP-binding cassette transporters in skin. Pharmacol. Res. Perspect. 2013, 1, prp2.5. [Google Scholar] [CrossRef] [PubMed]
- Osman-Ponchet, H.; Boulai, A.; Kouidhi, M.; Sevin, K.; Alriquet, M.; Gaborit, A.; Bertino, B.; Comby, P.; Ruty, B. Characterization of ABC transporters in human skin. Drug Metabol. Drug Interact. 2014, 29, 91–100. [Google Scholar] [CrossRef]
- Hendig, D.; Langmann, T.; Kocken, S.; Zarbock, R.; Szliska, C.; Schmitz, G.; Kleesiek, K.; Götting, C. Gene expression profiling of ABC transporters in dermal fibroblasts of pseudoxanthoma elasticum patients identifies new candidates involved in PXE pathogenesis. Lab. Investig. 2008, 88, 1303–1315. [Google Scholar] [CrossRef] [Green Version]
- Colone, M.; Calcabrini, A.; Toccacieli, L.; Bozzuto, G.; Stringaro, A.; Gentile, M.; Cianfriglia, M.; Ciervo, A.; Caraglia, M.; Budillon, A.; et al. The multidrug transporter P-glycoprotein: A mediator of melanoma invasion? J. Invest. Dermatol. 2008, 128, 957–971. [Google Scholar] [CrossRef] [Green Version]
- Oldham, M.L.; Davidson, A.L.; Chen, J. Structural insights into ABC transporter mechanism. Curr. Opin. Struct. Biol. 2008, 18, 726–733. [Google Scholar] [CrossRef] [Green Version]
- Kobuchi, H.; Moriya, K.; Ogino, T.; Fujita, H.; Inoue, K.; Shuin, T.; Yasuda, T.; Utsumi, K.; Utsumi, T. Mitochondrial Localization of ABC Transporter ABCG2 and Its Function in 5-Aminolevulinic Acid-Mediated Protoporphyrin IX Accumulation. PLoS ONE 2012, 7, e50082. [Google Scholar] [CrossRef] [Green Version]
- Mahringer, A.; Fricker, G. ABC transporters at the blood-brain barrier. Expert Opin. Drug Metab. Toxicol. 2016, 12, 499–508. [Google Scholar] [CrossRef]
- Wilkens, S. Structure and mechanism of ABC transporters. F1000Prime Rep. 2015, 7, 14. [Google Scholar] [CrossRef]
- Jones, P.M.; George, A.M. Mechanism of ABC transporters: A molecular dynamics simulation of a well characterized nucleotide-binding subunit. Proc. Natl. Acad. Sci. USA 2002, 99, 12639–12644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beis, K. Structural basis for the mechanism of ABC transporters. Biochem. Soc. Trans. 2015, 43, 889–893. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dean, M.; Moitra, K.; Allikmets, R. The human ATP-binding cassette (ABC) transporter superfamily. Hum. Mutat. 2022, 43, 1162–1182. [Google Scholar] [CrossRef] [PubMed]
- Bates, S.E.; Robey, R.; Knutsen, T.; Honjo, Y.; Litman, T.; Dean, M. New ABC transporters in multi-drug resistance. Expert Opin. Ther. Targets 2000, 4, 561–580. [Google Scholar] [CrossRef]
- Grewal, G.K.; Kukal, S.; Kanojia, N.; Saso, L.; Kukreti, S.; Kukreti, R. Effect of oxidative stress on ABC transporters: Contribution to epilepsy pharmacoresistance. Molecules 2017, 22, 365. [Google Scholar] [CrossRef] [Green Version]
- Yuan, T.; Hu, J.; Zhu, X.; Yin, H.; Yin, J. Oxidative stress-mediated up-regulation of ABC transporters in lung cancer cells. J. Biochem. Mol. Toxicol. 2022, 36, e23095. [Google Scholar] [CrossRef]
- Järvinen, E.; Deng, F.; Kiander, W.; Sinokki, A.; Kidron, H.; Sjöstedt, N. The Role of Uptake and Efflux Transporters in the Disposition of Glucuronide and Sulfate Conjugates. Front. Pharmacol. 2022, 12, 802539. [Google Scholar] [CrossRef]
- Rubio, V.; García-Pérez, A.I.; Herráez, A.; Diez, J.C. Different roles of Nrf2 and NFKB in the antioxidant imbalance produced by esculetin or quercetin on NB4 leukemia cells. Chem. Biol. Interact. 2018, 294, 158–166. [Google Scholar] [CrossRef]
- Miller, D.S. Regulation of ABC Transporters Blood-Brain Barrier. The Good, the Bad, and the Ugly. In Advances in Cancer Research; Academic Press Inc.: Cambridge, MA, USA, 2015; Volume 125, pp. 43–70. [Google Scholar]
- Di, Q.; Yu, N.; Liu, H.; Hu, Y.; Jiang, Y.; Yan, Y.K.; Zhang, Y.F.; Zhang, Y.D. Nuclear factor-kappa B activity regulates brain expression of P-glycoprotein in the kainic acid-induced seizure rats. Mediators Inflamm. 2011, 2011, 670613. [Google Scholar]
- Wang, X.; Campos, C.R.; Peart, J.C.; Smith, L.K.; Boni, J.L.; Cannon, R.E.; Miller, D.S. Nrf2 upregulates ATP binding cassette transporter expression and activity at the blood-brain and blood-spinal cord barriers. J. Neurosci. 2014, 34, 8585–8593. [Google Scholar] [CrossRef] [PubMed]
- Maher, J.M.; Dieter, M.Z.; Aleksunes, L.M.; Slitt, A.L.; Guo, G.; Tanaka, Y.; Scheffer, G.L.; Chan, J.Y.; Manautou, J.E.; Chen, Y.; et al. Oxidative and electrophilic stress induces multidrug resistance-associated protein transporters via the nuclear factor-E2-related factor-2 transcriptional pathway. Hepatology 2007, 46, 1597–1610. [Google Scholar] [CrossRef] [PubMed]
- Son, Y.; Cheong, Y.-K.; Kim, N.-H.; Chung, H.-T.; Kang, D.G.; Pae, H.-O. Mitogen-Activated Protein Kinases and Reactive Oxygen Species: How Can ROS Activate MAPK Pathways? J. Signal Transduct. 2011, 2011, 792639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stolarczyk, E.I.; Reiling, C.J.; Paumi, C.M. Regulation of ABC Transporter Function via Phosphorylation by Protein Kinases. Curr. Pharm. Biotechnol. 2011, 12, 621–635. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Cataisson, C.; Flowers, B.; Fraser, E.; Sanchez, V.; Day, C.P.; Yuspa, S.H. Topical Application of a Dual ABC Transporter Substrate and NF-κB Inhibitor Blocks Multiple Sources of Cutaneous Inflammation in Mouse Skin. J. Invest. Dermatol. 2019, 139, 1506–1515.e7. [Google Scholar] [CrossRef]
- Zecchinati, F.; Barranco, M.M.; Arana, M.R.; Tocchetti, G.N.; Domínguez, C.J.; Perdomo, V.G.; Ruiz, M.L.; Mottino, A.D.; García, F.; Villanueva, S.S.M. Reversion of down-regulation of intestinal multidrug resistance-associated protein 2 in fructose-fed rats by geraniol and vitamin C: Potential role of inflammatory response and oxidative stress. J. Nutr. Biochem. 2019, 68, 7–15. [Google Scholar] [CrossRef]
- Atalay, S.; Dobrzyńska, I.; Gęgotek, A.; Skrzydlewska, E. Cannabidiol protects keratinocyte cell membranes following exposure to UVB and hydrogen peroxide. Redox Biol. 2020, 36, 101613. [Google Scholar] [CrossRef]
- Di Pietro, A.; Conseil, G.; Pérez-Victoria, J.M.; Dayan, G.; Baubichon-Cortay, H.; Trompier, D.; Steinfels, E.; Jault, J.M.; De Wet, H.; Maitrejean, M.; et al. Modulation by flavonoids of cell multidrug resistance mediated by P-glycoprotein and related ABC transporters. Cell. Mol. Life Sci. 2002, 59, 307–322. [Google Scholar] [CrossRef]
- Morris, M.E.; Zhang, S. Flavonoid-drug interactions: Effects of flavonoids on ABC transporters. Life Sci. 2006, 78, 2116–2130. [Google Scholar] [CrossRef]
- Skazik, C.; Wenzel, J.; Marquardt, Y.; Kim, A.; Merk, H.F.; Bickers, D.R.; Baron, J.M. P-Glycoprotein (ABCB1) expression in human skin is mainly restricted to dermal components. Exp. Dermatol. 2011, 20, 450–452. [Google Scholar] [CrossRef]
- Heise, R.; Skazik, C.; Rodriguez, F.; Stanzel, S.; Marquardt, Y.; Joussen, S.; Wendel, A.F.; Wosnitza, M.; Merk, H.F.; Baron, J.M. Active transport of contact allergens and steroid hormones in epidermal keratinocytes is mediated by multidrug resistance related proteins. J. Invest. Dermatol. 2010, 130, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.M.K.; Aryal, E.; Safari, E.; Mojsoska, B.; Jenssen, H.; Prabhala, B.K. Current state of slc and abc transporters in the skin and their relation to sweat metabolites and skin diseases. Proteomes 2021, 9, 23. [Google Scholar] [CrossRef] [PubMed]
- van de Ven, R.; de Jong, M.C.; Reurs, A.W.; Schoonderwoerd, A.J.N.; Jansen, G.; Hooijberg, J.H.; Scheffer, G.L.; de Gruijl, T.D.; Scheper, R.J. Dendritic Cells Require Multidrug Resistance Protein 1 (ABCC1) Transporter Activity for Differentiation. J. Immunol. 2006, 176, 5191–5198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Randolph, G.J.; Beaulieu, S.; Pope, M.; Sugawara, I.; Hoffman, L.; Steinman, R.M.; Muller, W.A. A physiologic function for p-glycoprotein (MDR-1) during the migration of dendritic cells from skin via afferent lymphatic vessels. Proc. Natl. Acad. Sci. USA 1998, 95, 6924–6929. [Google Scholar] [CrossRef] [Green Version]
- Tarling, E.J.; Vallim, T.Q.d.A.; Edwards, P.A. Role of ABC transporters in lipid transport and human disease. Trends Endocrinol. Metab. 2013, 24, 342–350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, C.A.; Rajpopat, S.; Di, W.L. Harlequin ichthyosis: ABCA12 mutations underlie defective lipid transport, reduced protease regulation and skin-barrier dysfunction. Cell Tissue Res. 2013, 351, 281–288. [Google Scholar] [CrossRef]
- Heimerl, S.; Bosserhoff, A.K.; Langmann, T.; Ecker, J.; Schmitz, G. Mapping ATP-binding cassette transporter gene expression profiles in melanocytes and melanoma cells. Melanoma Res. 2007, 17, 265–273. [Google Scholar] [CrossRef]
- Keshet, G.I.; Goldstein, I.; Itzhaki, O.; Cesarkas, K.; Shenhav, L.; Yakirevitch, A.; Treves, A.J.; Schachter, J.; Amariglio, N.; Rechavi, G. MDR1 expression identifies human melanoma stem cells. Biochem. Biophys. Res. Commun. 2008, 368, 930–936. [Google Scholar] [CrossRef]
- Fukunaga-Kalabis, M.; Herlyn, M. Beyond ABC: Another mechanism of drug resistance in melanoma side population. J. Invest. Dermatol. 2012, 132, 2317–2319. [Google Scholar] [CrossRef] [Green Version]
- Thinnes, F.P. Nonmelanoma skin cancer is associated with reduced alzheimer disease risk. Neurology 2013, 81, 2056. [Google Scholar] [CrossRef] [Green Version]
- Elliott, A.M.; Al-Hajj, M.A. ABCB8 mediates doxorubicin resistance in melanoma cells by protecting the mitochondrial genome. Mol. Cancer Res. 2009, 7, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.G.; Valencia, J.C.; Gillet, J.-P.; Hearing, V.J.; Gottesman, M.M. Involvement of ABC transporters in melanogenesis and the development of multidrug resistance of melanoma. Pigment Cell Melanoma Res. 2009, 22, 740–749. [Google Scholar] [CrossRef]
- Kalal, B.S.; Upadhya, D.; Pai, V.R. Chemotherapy resistance mechanisms in advanced skin cancer. Oncol. Rev. 2017, 11, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Setia, N.; Abbas, O.; Sousa, Y.; Garb, J.L.; Mahalingam, M. Profiling of ABC transporters ABCB5, ABCF2 and nestin-positive stem cells in nevi, in situ and invasive melanoma. Mod. Pathol. 2012, 25, 1169–1175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gęgotek, A.; Rybałtowska-Kawałko, P.; Skrzydlewska, E. Rutin as a Mediator of Lipid Metabolism and Cellular Signaling Pathways Interactions in Fibroblasts Altered by UVA and UVB Radiation. Oxid. Med. Cell. Longev. 2017, 2017, 4721352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gegotek, A.; Biernacki, M.; Ambrozewicz, E.; Surazyński, A.; Wroński, A.; Skrzydlewska, E. The cross-talk between electrophiles, antioxidant defence and the endocannabinoid system in fibroblasts and keratinocytes after UVA and UVB irradiation. J. Dermatol. Sci. 2016, 81, 107–117. [Google Scholar] [CrossRef]
- de Gruijl, F.R. Photocarcinogenesis: UVA vs. UVB Radiation. Skin Pharmacol. Physiol. 2002, 15, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Fivenson, D.; Sabzevari, N.; Qiblawi, S.; Blitz, J.; Norton, B.B.; Norton, S.A. Sunscreens: UV filters to protect us: Part 2-Increasing awareness of UV filters and their potential toxicities to us and our environment. Int. J. Women’s Dermatol. 2021, 7, 45–69. [Google Scholar] [CrossRef]
- Gęgotek, A.; Bielawska, K.; Biernacki, M.; Dobrzyńska, I.; Skrzydlewska, E. Time-dependent effect of rutin on skin fibroblasts membrane disruption following UV radiation. Redox Biol. 2017, 12, 733–744. [Google Scholar] [CrossRef]
- Jarocka-Karpowicz, I.; Biernacki, M.; Wroński, A.; Gęgotek, A.; Skrzydlewska, E. Cannabidiol Effects on Phospholipid Metabolism in Keratinocytes from Patients with Psoriasis Vulgaris. Biomolecules 2020, 10, 367. [Google Scholar] [CrossRef] [Green Version]
- Dumitriu, I.E.; Voll, R.E.; Kolowos, W.; Gaipl, U.S.; Heyder, P.; Kalden, J.R.; Herrmann, M. UV irradiation inhibits ABC transporters via generation of ADP-ribose by concerted action of poly(ADP-ribose) polymerase-1 and glycohydrolase. Cell Death Differ. 2004, 11, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Baron, J.M.; Höller, D.; Schiffer, R.; Frankenberg, S.; Neis, M.; Merk, H.F.; Jugert, F.K. Expression of multiple cytochrome P450 enzymes and multidrug resistance-associated transport proteins in human skin keratinocytes. J. Invest. Dermatol. 2001, 116, 541–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abe, Y.; Shimizu, K.; Katayama, I. Significance of MDR1-Gene and P-Glycoprotein (P-gp) Expressions in the Lesional Skin of Psoriasis Vulgaris. Acta. Med. Nagasaki 2001, 46, 19–24. [Google Scholar]
- Kemény, L.; Varga, E.; Novak, Z. Advances in phototherapy for psoriasis and atopic dermatitis. Expert Rev. Clin. Immunol. 2019, 15, 1205–1214. [Google Scholar] [CrossRef]
- Chao, C.C.K.; Sun, N.K. Overexpression of a UV-damage recognition protein in a UV-sensitive human colon cancer cell line that features multidrug-resistant phenotype. Biochem. Biophys. Res. Commun. 1993, 191, 1252–1260. [Google Scholar] [CrossRef] [PubMed]
- Trindade, G.S.; Capella, M.A.M.; Capella, L.S.; Affonso-Mitidieri, O.R.; Rumjanek, V.M. Differences in Sensitivity to UVC, UVB and UVA Radiation of a Multidrug-Resistant Cell Line Overexpressing P-Glycoprotein. Photochem. Photobiol. 1999, 69, 694–699. [Google Scholar] [CrossRef] [PubMed]
- Abele, R.; Tampé, R. The ABCs of immunology: Structure and function of TAP, the transporter associated with antigen processing. Physiology 2004, 19, 216–224. [Google Scholar] [CrossRef]
- Stoitzner, P.; Tripp, C.H.; Eberhart, A.; Price, K.M.; Jung, J.Y.; Bursch, L.; Ronchese, F.; Romani, N. Langerhans cells cross-present antigen derived from skin. Proc. Natl. Acad. Sci. USA 2006, 103, 7783–7788. [Google Scholar] [CrossRef] [Green Version]
- Ruedl, C.; Storni, T.; Lechner, F.; Bächi, T.; Bachmann, M.F. Cross-presentation of virus-like particles by skin-derived CD8– dendritic cells: A dispensable role for TAP. Eur. J. Immunol. 2002, 32, 818. [Google Scholar] [CrossRef]
- Ritz, U.; Seliger, B. The transporter associated with antigen processing (TAP): Structural integrity, expression, function, and its clinical relevance. Mol. Med. 2001, 7, 149–158. [Google Scholar] [CrossRef] [Green Version]
- Witkowska-Tobola, A.M.; Szczerkowska-Dobosz, A.; Nedoszytko, B.; Roszkiewicz, J. Polymorphism of the TAP1 gene in Polish patients with psoriasis vulgaris. J. Appl. Genet. 2004, 45, 391–393. [Google Scholar] [PubMed]
- Vašků, V.; Vašků, A.; Izakovičová Hollá, L.; Tschöplová, S.; Kaňková, K.; Benáková, N.; Semrádová, V. Polymorphisms in inflammation genes (angiotensinogen, TAP1 and TNF-β) in psoriasis. Arch. Dermatol. Res. 2000, 292, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Ismaïl, A.; Bousaffara, R.; Kaziz, J.; Zili, J.; El Kamel, A.; Sfar, M.T.; Remadi, S.; Chouchane, L. Polymorphism in transporter antigen peptides gene (TAPI) associated with atopy in Tunisians. J. Allergy Clin. Immunol. 1997, 99, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Jadeja, S.D.; Mansuri, M.S.; Singh, M.; Dwivedi, M.; Laddha, N.C.; Begum, R. A case-control study on association of proteasome subunit beta 8 (PSMB8) and transporter associated with antigen processing 1 (TAP1) polymorphisms and their transcript levels in vitiligo from Gujarat. PLoS ONE 2017, 12, e0180958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Law-Ping-Man, S.; Toutain, F.; Rieux-Laucat, F.; Picard, C.; Kammerer-Jacquet, S.; Magérus-Chatinet, A.; Dupuy, A.; Adamski, H. Chronic granulomatous skin lesions leading to a diagnosis of TAP1 deficiency syndrome. Pediatr. Dermatol. 2018, 35, e375–e377. [Google Scholar] [CrossRef]
- Darazam, I.; Shahrooei, M.; Hakamifard, A.; Olyaei, N.A.; Zerehpoosh, E.; Gharehbagh, F.; Hatami, F.; Lotfollahi, L.; Mansouri, N.; Casanova, J.; et al. Chronic necrotizing granulomatous skin lesions and MHC class I deficiency syndrome due to TAP2 deficiency. Res. Square. 2022. [Google Scholar] [CrossRef]
- Kamarashev, J.; Ferrone, S.; Seifert, B.; Boni, R.; Nestle, F.; Burg, G.; Dummer, R. TAP1 down-regulation in primary melanoma lesions: An independent marker of poor prognosis. Int. J. Cancer 2001, 95, 23–28. [Google Scholar] [CrossRef]
- Shoaib Mansuri, M.; Singh, M.; Shoab Mansuri, M.; Jadeja, S.D.; Gani, A.R.; Patel, R.; Dwivedi, M.; Laddha, N.C.; Begum, R. Could ER Stress Be a Major Link between Oxidative Stress and Autoimmunity in Vitiligo? Artic. J. Pigment. Disord. 2014, 1, 3. [Google Scholar] [CrossRef] [Green Version]
- Glassman, S.J. Vitiligo, reactive oxygen species and T-cells. Clin. Sci. 2011, 120, 99–120. [Google Scholar] [CrossRef] [Green Version]
- Linsdell, P. Cystic fibrosis transmembrane conductance regulator (CFTR): Making an ion channel out of an active transporter structure. Channels 2018, 12, 284–290. [Google Scholar] [CrossRef] [Green Version]
- Hanukoglu, I.; Boggula, V.R.; Vaknine, H.; Sharma, S.; Kleyman, T.; Hanukoglu, A. Expression of epithelial sodium channel (ENaC) and CFTR in the human epidermis and epidermal appendages. Histochem. Cell Biol. 2017, 147, 733–748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engelhardt, J.F.; Smith, S.S.; Allen, E.; Yankaskas, J.R.; Dawson, D.C.; Wilson, J.M. Coupled secretion of chloride and mucus in skin of Xenopus laevis: Possible role for CFTR. Am. J. Physiol.—Cell Physiol. 1994, 267, C491–C500. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Jiang, X.; Zhang, X.; Liu, K.S.; Zhang, J.; Chen, J.; Yu, M.K.; Tsang, L.L.; Chung, Y.W.; Wang, Y.; et al. Dynamically Regulated CFTR Expression and Its Functional Role in Cutaneous Wound Healing. J. Cell. Physiol. 2015, 230, 2049–2058. [Google Scholar] [CrossRef]
- Larsen, E.H.; Amstrup, J.; Willumsen, N.J. β-Adrenergic receptors couple to CFTR chloride channels of intercalated mitochondria-rich cells in the heterocellular toad skin epithelium. Biochim. Biophys. Acta—Biomembr. 2003, 1618, 140–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, A.-Y. Recent progress in melasma pathogenesis. Pigment Cell Melanoma Res. 2015, 28, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y. An updated review of melasma pathogenesis. Dermatol. Sin. 2014, 32, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Hussar, D.A.; Eckel, S.P. Ivacaftor, vismodegib, and ingenol mebutate. J. Am. Pharm. Assoc. 2012, 52, 418–422. [Google Scholar] [CrossRef]
- Burke, M.A.; Mutharasan, R.K.; Ardehali, H. The sulfonylurea receptor, an atypical ATP-binding cassette protein, and its regulation of the KATP channel. Circ. Res. 2008, 102, 164–176. [Google Scholar] [CrossRef] [Green Version]
- Bryan, J.; Crane, A.; Vila-Carriles, W.; Babenko, A.; Aguilar-Bryan, L. Insulin Secretagogues, Sulfonylurea Receptors and KATP Channels. Curr. Pharm. Des. 2005, 11, 2699–2716. [Google Scholar] [CrossRef]
- Rafiq, M.; Flanagan, S.E.; Patch, A.M.; Shields, B.M.; Ellard, S.; Hattersley, A.T.; Batra, C.; Bruining, J.; Carson, D.; Codner, E.; et al. Effective treatment with oral sulfonylureas in patients with diabetes due to sulfonylurea receptor 1 (SUR1) mutations. Diabetes Care 2008, 31, 204–209. [Google Scholar] [CrossRef] [Green Version]
- Vigneri, R.; Pezzino, V.; Wong, K.Y.; Goldfine, I.D. Comparison of the in Vitro Effect of Biguanides and Sulfonylureas on Insulin Binding to Its Receptors in Target Cells. J. Clin. Endocrinol. Metab. 1982, 54, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Sánchez, A.Y.; Hinojosa, L.M.; Parraguirre-Martínez, S.; González, A.; Morales, F.; Montalvo, G.; Vera, E.; Hernández-Gallegos, E.; Camacho, J. Expression of KATP channels in human cervical cancer: Potential tools for diagnosis and therapy. Oncol. Lett. 2018, 15, 6302–6308. [Google Scholar] [PubMed]
- Newfield, R.S. Topical sulfonylurea as a novel therapy for hypertrichosis secondary to diazoxide, and potentially for other conditions with excess hair growth. Med. Hypotheses 2015, 85, 969–971. [Google Scholar] [CrossRef] [PubMed]
- Bednarczyk, P.; Kicinska, A.; Laskowski, M.; Kulawiak, B.; Kampa, R.; Walewska, A.; Krajewska, M.; Jarmuszkiewicz, W.; Szewczyk, A. Evidence for a mitochondrial ATP-regulated potassium channel in human dermal fibroblasts. Biochim. Biophys. Acta—Bioenerg. 2018, 1859, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Gier, B.; Krippeit-Drews, P.; Sheiko, T.; Aguilar-Bryan, L.; Bryan, J.; Düfer, M.; Drews, G. Suppression of KATP channel activity protects murine pancreatic β cells against oxidative stress. J. Clin. Invest. 2009, 119, 3246–3256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatti, J.S.; Sehrawat, A.; Mishra, J.; Sidhu, I.S.; Navik, U.; Khullar, N.; Kumar, S.; Bhatti, G.K.; Reddy, P.H. Oxidative stress in the pathophysiology of type 2 diabetes and related complications: Current therapeutics strategies and future perspectives. Free Radic. Biol. Med. 2022, 184, 114–134. [Google Scholar] [CrossRef]
- Liu, Y.; Gutterman, D.D. Oxidative Stress and Potassium Channel Function. Clin. Exp. Pharmacol. Physiol. 2002, 29, 305–311. [Google Scholar] [CrossRef]
- Robey, R.W.; To, K.K.K.; Polgar, O.; Dohse, M.; Fetsch, P.; Dean, M.; Bates, S.E. ABCG2: A perspective. Adv. Drug Deliv. Rev. 2009, 61, 3–13. [Google Scholar] [CrossRef]
- Natarajan, K.; Xie, Y.; Baer, M.R.; Ross, D.D. Role of breast cancer resistance protein (BCRP/ABCG2) in cancer drug resistance. Biochem. Pharmacol. 2012, 83, 1084–1103. [Google Scholar] [CrossRef] [Green Version]
- Ven, R.; Lindenberg, J.J.; Reurs, A.W.; Scheper, R.J.; Scheffer, G.L.; Gruijl, T.D. Preferential Langerhans cell differentiation from CD34 + precursors upon introduction of ABCG2 (BCRP). Immunol. Cell Biol. 2012, 90, 206–215. [Google Scholar] [CrossRef]
- Wang, P.; Sachar, M.; Lu, J.; Shehu, A.I.; Zhu, J.; Chen, J.; Liu, K.; Anderson, K.E.; Xie, W.; Gonzalez, F.J.; et al. The essential role of the transporter ABCG2 in the pathophysiology of erythropoietic protoporphyria. Sci. Adv. 2019, 5, 6127–6145. [Google Scholar] [CrossRef] [PubMed]


| Subfamily | Transporters | Main Function |
|---|---|---|
| ABCA | ABCA 1-9, 12 | transport of cholesterol and lipids |
| ABCB | ABCB 1 (MDR1), ABCB 2-3 (TAP1-2), ABCB 4 (MDR3), ABCB 5-11 | transport of peptides and metabolites |
| ABCC | ABCC 1-6 (MRP1-6), ABCC 7 (CFTR), ABCC 8-9 (SUR1-2), ABCC 10-12 (MRP7-9) | transport of ions, cell-surface receptors |
| ABCD | ABCD 1-4 | participate in peroxisome activation |
| ABCE | ABCE 1 | multidrug resistance |
| ABCF | ABCF 1-3 | regulation of innate immune response |
| ABCG | ABCG 1, ABCG 2 (BCRP), ABCG 4,5,8 | transport of drugs, toxins, lipids, cholesterol and other steroids |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gęgotek, A.; Skrzydlewska, E. The Role of ABC Transporters in Skin Cells Exposed to UV Radiation. Int. J. Mol. Sci. 2023, 24, 115. https://doi.org/10.3390/ijms24010115
Gęgotek A, Skrzydlewska E. The Role of ABC Transporters in Skin Cells Exposed to UV Radiation. International Journal of Molecular Sciences. 2023; 24(1):115. https://doi.org/10.3390/ijms24010115
Chicago/Turabian StyleGęgotek, Agnieszka, and Elżbieta Skrzydlewska. 2023. "The Role of ABC Transporters in Skin Cells Exposed to UV Radiation" International Journal of Molecular Sciences 24, no. 1: 115. https://doi.org/10.3390/ijms24010115
APA StyleGęgotek, A., & Skrzydlewska, E. (2023). The Role of ABC Transporters in Skin Cells Exposed to UV Radiation. International Journal of Molecular Sciences, 24(1), 115. https://doi.org/10.3390/ijms24010115






