Blue-Green (~480 nm) versus Blue (~460 nm) Light for Newborn Phototherapy—Safety Considerations
Abstract
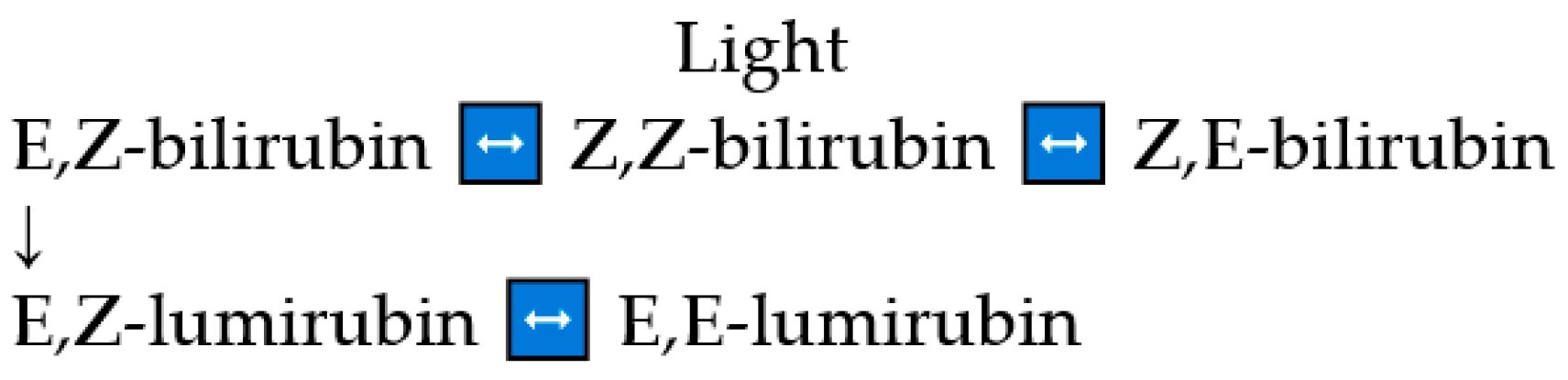
:1. Introduction
2. Results
2.1. Immediate Side Effects
2.1.1. In Vitro Studies
2.1.2. Animal Studies
2.1.3. Neonatal Studies
2.2. Extremely Low Birth Neonates
2.3. Riboflavin Level
2.4. Bronze Baby Syndrome
2.5. Immune System
2.6. Hemodynamic Changes
2.7. Transepidermal Water Loss
2.8. Hyper- and Hypothermia
2.9. Vision
2.10. Hypocalcemia
2.11. Loose Stools
2.12. Parent–Neonate Attachment and Breastfeeding
3. Long-Term Side Effects (Epidemiologic Studies)
3.1. Cancer
3.2. Allergic Diseases
3.3. Diabetes Type 1
3.4. Childhood Epilepsy
3.5. Autism Spectrum Disorders
4. Summary
5. Material and Methods
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Alken, J.; Håkansson, S.; Ekeus, C.; Gustafson, P.; Norman, M. Rates of extreme neonatal hyperbilirubinemia and kernicterus in children and adherence to national for screening, diagnosis, and treatment in Sweden. JAMA Netw. Open 2019, 2, e190858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mreihil, K.; Benth, J.S.; Stensvold, H.J.; Nakstad, B.; Hansen, T.W.R. Phototherapy is commonly used for neonatal jaundice but greater control is needed to avoid toxicity in the most vulnerable infants. Acta Paediatr. 2018, 107, 611–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDonagh, A.F.; Agati, G.; Fusi, F.; Pratesi, R. Quantum yields for laser photocyclization of bilirubin in the presence of human serum albumin. Dependence of quantum yield on excitation wavelength. Photochem. Photobiol. 1989, 50, 305–319. [Google Scholar] [CrossRef]
- Onishi, S.; Isobe, K.; Itoh, S.; Manabe, M.; Sasaki, K.; Fukuzaki, R.; Yamakawa, T. Metabolism of bilirubin and its photoisomers in newborn infants during phototherapy. J. Biochem. 1986, 100, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Lightner, D.A.; McDonagh, A.F. Molecular mechanisms of phototherapy for neonatal jaundice. Acc. Chem. Res. 1984, 17, 417–424. [Google Scholar] [CrossRef]
- Jasprova, J.; Ben, M.D.; Hurny, D.; Hwang, S.; Zizalova, K.; Kotek, J.; Wong, R.J.; Stevenson, D.K.; Gazzin, S.; Tiribelli, C.; et al. Neuro-inflammatory effects of photodegradative products of bilirubin. Sci. Rep. 2018, 8, 7444. [Google Scholar] [CrossRef]
- Onishi, S.; Itoh, S.; Isobe, K. Wavelength-dependence of the relative rate constants for the main geometric and structural photoisomerization of bilirubin IX alpha bound to human serum albumin. J. Biochem. 1986, 236, 23–29. [Google Scholar] [CrossRef]
- Pratesi, R.; Ronchi, L.; Cecchi, G.; Sbrana, G.; Migliorini, M.G.; Vecchi, C.; Donzelli, G. Skin optics and phototherapy of jaundice. Photochem. Photobiol. 1984, 40, 77–83. [Google Scholar] [CrossRef]
- Agati, G.; Fusi, F.; Donzelli, G.P.; Pratesi, R. Quantum yield and skin filtering effects on the formation rate of lumirubin. J. Photochem. Photobiol. B 1993, 18, 197–203. [Google Scholar] [CrossRef]
- Lamola, A.A. A pharmacologic view of phototherapy. Clin. Perinatol. 2016, 43, 259–276. [Google Scholar] [CrossRef]
- Ebbesen, F.; Rodrigo-Domingo, M.; Moeller, A.M.; Vreman, H.J.; Donneborg, M.L. Effect of blue LED phototherapy centered at 478 nm versus 459 nm in hyperbilirubinemic neonates: A randomized study. Pediatr. Res. 2021, 89, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Ebbesen, F.; Vandborg, P.K.; Donneborg, M.L. The effectiveness of phototherapy using blue-green light for neonatal hyperbilirubinemia—Danish clinical trials. Semin. Perinatol. 2021, 45, 51358. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics; Bhutani, V.; The Committee on Fetus and Newborn. Phototherapy to prevent severe hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2011, 128, e1046–e1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebbesen, F.; Madsen, P.; Stovring, S.; Hundborg, H.; Agati, G. Therapeutic effect of turquoise versus blue light with equal irradiances in preterm infants with jaundice. Acta Paediatr. 2007, 96, 837–841. [Google Scholar] [CrossRef] [PubMed]
- Ebbesen, F.; Madsen, P.; Vandborg, P.K.; Jakobsen, L.H.; Trydal, T.; Vreman, H.J. Bilirubin isomer distribution in jaundiced neonates during phototherapy with LED light centered at 497 nm (turquoise) vs. 459 nm (blue). Pediatr. Res. 2016, 80, 511–515. [Google Scholar] [CrossRef] [Green Version]
- Donneborg, M.L.; Vandborg, P.K.; Hansen, B.M.; Rodrigo-Domingo, M.; Ebbesen, F. The impact of hemoglobin on the efficacy of phototherapy in hyperbilirubinemic infants. Pediatr. Res. 2019, 82, 947–951. [Google Scholar] [CrossRef] [Green Version]
- Stocker, R.; Yamamoto, Y.; McDonagh, A.F.; Glazer, A.N.; Ames, B.N. Bilirubin is an antioxidant of possible physiological importance. Science 1987, 235, 1043–1046. [Google Scholar]
- Ayyappan, S.; Philip, S.; Bharathy, N.; Ramesh, V.; Kumar, C.N.; Swathi, S.; Kumar, A.A. Antioxidant status in neonatal jaundice before and after phototherapy. J. Pharm. Biol. Sci. 2015, 7, S16–S21. [Google Scholar]
- Shahab, M.S.; Kumar, P.; Sharma, N.; Narang, A.; Prasad, R. Evaluation of oxidant and antioxidant status in term neonates: A plausible protective role of bilirubin. Mol. Cell. Biochem. 2008, 317, 51–59. [Google Scholar] [CrossRef]
- Dani, C.; Poggi, C.; Pratesi, S. Bilirubin and oxidative stress in term and preterm infants. Free Radic. Res. 2019, 53, 2–7. [Google Scholar] [CrossRef]
- Parshad, R.; Sanford, K.K.; Taylor, W.G.; Tarone, R.E.; Jones, G.M.; Baeck, A.E. Effect of intensity and wavelength of fluorescent light on chromosome damage in cultured mouse cells. Photochem. Photobiol. 1979, 29, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Christensen, T.; Reitan, J.B.; Kinn, G. Single-strand breaks in the DNA of human cells exposed to visible light from phototherapy lamps in the presence and absence of bilirubin. J. Photochem. Photobiol. B Biol. 1990, 7, 337–346. [Google Scholar] [CrossRef]
- Christensen, T.; Kinn, G.; Granli, T.; Amundsen, I. Cells, bilirubin and light: Formation of bilirubin photoproducts and cellular damage at defined wavelengths. Acta Pediatr. 1994, 83, 7–12. [Google Scholar] [CrossRef]
- Roll, E.B.; Christensen, T. Formation of photoproducts and cytotoxicity of bilirubin irradiated with turquoise and blue phototherapy light. Acta Paediatr. 2005, 94, 1448–1454. [Google Scholar] [CrossRef] [PubMed]
- Jasprova, J.; Ben, M.D.; Vianello, E.; Goncharova, I.; Urbanova, M.; Vyroubalova, K.; Gazzin, S.; Tiribelli, C.; Sticha, M.; Cerna, M.; et al. The biologic effects of bilirubin photoisomers. PLoS ONE 2016, 11, e0148126. [Google Scholar] [CrossRef] [PubMed]
- Dvorak, A.; Pospisilova, K.; Zizalova, K.; Capkova, N.; Muchova, L.; Vecka, M.; Vrzackova, N.; Krizova, J.; Zelenka, J.; Vitek, L. The effects of bilirubin and lumirubin on metabolic and oxidative stress markers. Front. Pharmacol. 2021, 12, 7001. [Google Scholar] [CrossRef]
- Uchida, Y.; Morimoto, Y.; Uchiike, T.; Kamamoto, T.; Hayashi, T.; Arai, I.; Nishikubo, T.; Takahashi, Y. Phototherapy with blue and green mixed-light is as effective against unconjugated jaundice as blue light and reduces oxidative stress in the Gunn rat model. Early Hum. Dev. 2015, 97, 381–385. [Google Scholar] [CrossRef]
- Van der Schoor, L.W.E.; Hulzebos, C.V.; van Faassen, M.H.; Kema, I.P.; de Bruin, A.; Havinga, R.; Koster, M.; Youssef, S.A.; Bongiovanni, L.; Jonker, J.W.; et al. LED-phototherapy does not induce oxidative DNA damage in hyperbilirubinemic Gunn rats. Pediatr. Res. 2019, 85, 1041–1047. [Google Scholar] [CrossRef]
- Bulut, O.; Erek, A.; Duruyen, S. Effects of hyperbilirubinemia on markers of genotoxicity and total oxidant and antioxidant status in newborns. Drug Chem. Toxicol. 2020, 45, 451–455. [Google Scholar] [CrossRef]
- Iwase, T.; Kusaka, T.; Ito, S. (EZ)-cyclobilirubin formation from bilirubin in complex with serum albumin derived from various species. J. Photochem. Photobiol. B Biol. 2010, 98, 138–143. [Google Scholar] [CrossRef]
- Onishi, S.; Ogino, T.; Yokoyama, T.; Isobe, K.; Itoh, S.; Yamakawa, T.; Hashimoto, T. Biliary and urinary excretion rates and serum concentration changes of our bilirubin photoproducts in Gunn rats during total darkness and low or high illumination. J. Biochem. 1984, 221, 717–721. [Google Scholar] [CrossRef] [Green Version]
- Mohamed, W.W.; Niazy, W.H. Genotoxic effect of phototherapy in term newborn infants with hyperbilirubinemia. J. Neonat.-Perinat. Med. 2012, 5, 381–387. [Google Scholar] [CrossRef]
- Demirel, G.; Uras, N.; Celik, I.H.; Aksoy, H.T.; Oguz, S.S.; Erdeve, O.; Erel, O.; Dilmen, U. Comparison of total oxidant/antioxidant status in unconjugated hyperbilirubinemia of newborn before and after conventional and LED phototherapy: A prospective randomized controlled trial. Clin. Investig. Med. 2010, 3, 335–342. [Google Scholar] [CrossRef] [Green Version]
- Kale, Y.; Aydemir, O.; Celik, U.; Kuvurt, S.; Isikoglu, S.; Bas, A.Y.; Demirel, N. Effects of phototherapy using different light sources on oxidant and antioxidant status of neonates with jaundice. Early Hum. Dev. 2013, 89, 957–960. [Google Scholar] [CrossRef] [PubMed]
- Mokhtar, W.A.; Sherief, L.M.; Elsayed, H.; Shehab, M.M.; Gebaly, S.M.; Khalil, A.M.M.; Sobhy, M.; Kamal, N.M. Conventional intensive versus LED intensive phototherapy oxidative stress burden in neonatal hyperbilirubinemia of haemolytic origin. Pediatr. Int. Child Health 2020, 40, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Karadag, A.; Yesilyurt, A.; Unal, S.; Keskin, I.; Demirin, H.; Uras, N.; Dilmen, U.; Tatli, M.M. A chromosomal-effect study of intensive phototherapy versus phototherapy in newborns with jaundice. Mutat. Res. 2009, 676, 17–20. [Google Scholar] [CrossRef]
- Van der Schoor, L.W.E.; van Faassen, M.H.J.R.; Kema, I.; Babtist, D.H.; Olthuis, A.J.; Jonker, J.W.; Verkade, H.J.; Groen, H.; Hulzebos, C. Blue LED phototherapy in preterm infants: Effects on an oxidative marker of DNA damage. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 105, F628–F633. [Google Scholar] [CrossRef]
- Morris, B.H.; Oh, W.; Tyson, J.E.; Stevenson, D.K.; Phelps, D.L.; O’Shea, T.M.; McDavid, G.E.; Perritt, R.L.; van Meurs, K.P.; Vohr, B.R.; et al. Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N. Engl. J. Med. 2008, 359, 885–896. [Google Scholar] [CrossRef] [Green Version]
- Tyson, J.E.; Pedroza, C.; Langer, J.; Green, C.; Morris, B.; Stevenson, D.; van Meurs, K.P.; Oh, W.; Phelps, D.; O’Shea, M.; et al. Does aggressive phototherapy increase mortality while decreasing profound impairment among the smallest and sickest newborns? J. Perinatol. 2012, 32, 677–682. [Google Scholar] [CrossRef] [Green Version]
- Arnold, C.; Pedroza, C.; Tyson, J.E. Phototherapy in ELBW newborns: Does it work? Is it safe? Evidence from randomized clinical trials. Semin. Perinatol. 2014, 38, 452–464. [Google Scholar] [CrossRef] [Green Version]
- Stevenson, D.K.; Wong, R.J.; Arnold, C.C.; Pedroza, C.; Tyson, J.E. Phototherapy and the risk of photo-oxidative injury in extremely low birth weight infants. Clin. Perinatol. 2016, 43, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Itoh, S.; Okada, H.; Kuboi, T.; Kusaka, T. Phototherapy for neonatal hyperbilirubinemia. Pediatr. Int. 2017, 59, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Morris, B.H.; Tyson, J.E.; Stevenson, D.K.; Oh, W.; Phelps, D.L.; O’Shea, T.M.; McDavid, G.E.; van Meurs, K.P.; Vohr, B.R.; Grisby, C.; et al. Efficacy of phototherapy devices and outcomes among extremely low birth weight infants: Multi-center observational study. J. Perinatol. 2013, 33, 126–133. [Google Scholar] [CrossRef] [Green Version]
- Capkova, N.; Pospisilova, V.; Fedorova, V.; Raska, J.; Pospisilova, K.; Ben, M.D.; Dvorak, A.; Viktorova, J.; Bohaciakova, D.; Vitek, L. The effects of bilirubin and lumirubin on differentiation of human pluripotent cell-derived neural stem cells. Antioxidants 2021, 10, 1532. [Google Scholar] [CrossRef]
- Sisson, T.R.C. Photodegradation of riboflavin in neonates. Fed. Proc. 1987, 46, 1883–1885. [Google Scholar]
- Rubaltelli, F.F.; Allegri, G.; Costa, C.; De Antoni, A. Urinary excretion of tryptophan metabilities during phototherapy. J. Pediatr. 1974, 85, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Amin, H.J.; Shukla, A.K.; Snyder, F.; Fung, E.; Anderson, N.M.; Parsons, H.G. Significance of phototherapy-induced riboflavin deficiency in the full-term neonate. Biol. Neonate 1992, 61, 76–81. [Google Scholar] [CrossRef]
- Gromisch, D.S.; Lopez, R.; Cole, H.S.; Cooperman, J.M. Light (phototherapy)-induced riboflavin deficiency in the neonate. J. Pediatr. 1977, 90, 118–122. [Google Scholar] [CrossRef]
- Sanvordeker, D.R.; Kostenbauder, H.B. Mechanism for riboflavin enhancement of bilirubin photodecomposition in vitro. J. Pharm. Sci. 1974, 63, 404–408. [Google Scholar] [CrossRef]
- Kostenbauder, H.B.; Sanvordeker, D.R. Riboflavin enhancement of bilirubin catabolism in vivo. Experientia 1973, 29, 282–283. [Google Scholar] [CrossRef]
- Ballowitz, L.; Bunjamin, A.; Hanefeld, F.; Lietz, L.; Stuttgen, G.; Wirjadi, D. Effects of riboflavin on Gunn rats under phototherapy. Pediatr. Res. 1979, 13, 1307–1315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, K.L.; Cow, M.T.; Karim, S.M.M. Effect of phototherapy on neonatal riboflavin status. J. Pediatr. 1978, 93, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Onishi, S.; Itoh, S.; Isobe, K.; Togari, H.; Hideyuki, H.; Nishimura, Y. Mechanism of development of bronze baby syndrome in neonates treated with phototherapy. Pediatrics 1982, 69, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Rubaltelli, F.F.; Da Riol, R.; D’Amore, E.S.G.; Jori, G. The bronze baby syndrome: Evidence of increased tissue concentration of copper porphyrins. Acta Paediatr. 1996, 85, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Ebbesen, F. Low reserve albumin for binding of bilirubin in neonates with deficiency of bilirubin excretion and bronze baby syndrome. Acta Paediatr. Scand. 1982, 71, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Bertini, G.; Dani, C.; Fonda, C.; Zorzi, C.; Rubaltelli, F.F. Bronze baby syndrome and the risk of kernicterus. Acta Paediatr. 2005, 94, 968–971. [Google Scholar] [CrossRef]
- McDonagh, A.F. Bilirubin, copper-porphyrins, and the bronze-baby syndrome. J. Pediatr. 2011, 158, 160–164. [Google Scholar] [CrossRef]
- Kurt, A.; Aygun, A.D.; Kurt, A.N.C.; Godekmerdan, A.; Akarsu, S.; Yilmaz, E. Use of phototherapy for neonatal hyperbilirubinemia affects cytokine production and lymphocyte subsets. Neonatology 2009, 95, 262–266. [Google Scholar] [CrossRef]
- Procianoy, R.S.; Silveira, R.C.; Fonseca, L.T.; Heidemann, L.A.; Neto, E.C. The influence of phototherapy on serum cytokine concentrations in newborn infants. J. Perinatol. 2010, 27, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Sirota, L.; Straussberg, R.; Gurary, N.; Aloni, D.; Bessler, H. Phototherapy for neonatal hyperbilirubinemia affects cytokine production by peripheral blood mononuclear cell. Eur. J. Pediatr. 1999, 158, 910–913. [Google Scholar] [CrossRef]
- Oh, W.; Yao, A.C.; Hanson, J.S.; Lind, J. Peripheral circulatory response to phototherapy in newborn infants. Acta Paediatr. Scand. 1973, 62, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.Y.K.; Wong, W.H.; Hodgeman, J.E.; Levan, N. Changes in blood flow in the skin and muscle with phototherapy. Pediatr. Res. 1974, 8, 259–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertini, G.; Perugi, S.; Elia, S.; Pratesi, S.; Dani, C.; Rubaltelli, F.F. Transepidermal water loss and cerebral hemodynamics in preterm infants: Conventional versus LED phototherapy. Eur. J. Pediatr. 2008, 167, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Pezzati, M.; Biagiotti, R.; Vangi, V.; Lombardi, E.; Wiechmann, L.; Rubaltelli, F.F. Changes in mesenteric blood flow response to feeding: Conventional versus fiber-optic phototherapy. Pediatrics 2000, 105, 350–353. [Google Scholar] [CrossRef]
- Benders, M.J.N.L.; van Bel, F.; van de Bor, M. Effect of phototherapy on renal blood flow velocity in preterm infants. Biol. Neonate 1998, 73, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Benders, M.J.N.L.; van Bel, F.; van de Bor, M. Cardiac output and ductal reopening during phototherapy in preterm infants. Acta Paediatr. 1999, 88, 1014–1019. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.-S.; Wu, H.; Wu, B.-Q.; Huang, R.-Z.; Zhao, L.-H.; Wen, Y. Effect of phototherapy on blood endothelin and nitric oxide levels: Clinical significance in preterm infants. World J. Pediatr. 2008, 4, 31–35. [Google Scholar] [CrossRef]
- Barefield, E.S.; Dwyer, M.D.; Cassady, G. Association of patent ductus arteriosus and phototherapy in infants weighing less than 1000 grams. J. Perinatol. 1993, 13, 376–380. [Google Scholar]
- Kjartansson, S.; Hamarlund, K.; Riesenfeld, T.; Sedin, G. Respiratory water loss and consumption in newborn infants during phototherapy. Acta Paediatr. Scand. 1991, 81, 769–773. [Google Scholar] [CrossRef]
- Oh, W.; Karecki, H. Phototherapy and insensible water loss in the newborn infant. Am. J. Dis. Child. 1972, 124, 230–232. [Google Scholar] [CrossRef]
- Aydemir, O.; Soysaldi, E.; Kale, Y.; Kavurt, S.; Bas, A.Y.; Demirel, N. Body temperature changes of newborns under fluorescent versus LED phototherapy. Indian J. Pediatr. 2014, 81, 751–754. [Google Scholar] [CrossRef] [PubMed]
- Brandao, D.C.B.; Draque, C.M.; Sanudo, A.; Filho, F.A.R.G.; Almeida, M.F.B. LED versus daylight phototherapy at low irradiance in newborns ≥35 weeks of gestation: Randomized controlled trial. J. Matern.-Fetal Neonatal Med. 2014, 28, 1725–1730. [Google Scholar] [CrossRef] [PubMed]
- Noel, W.K.; Walker, V.S.; Kang, B.S.; Berman, S. Retinal damage by light in rats. Investig. Ophthalmol. 1966, 5, 450–473. [Google Scholar]
- Kuwabara, T.; Funahashi, M. Light damage in the developing rat retina. Arch. Ophthalmol. 1976, 94, 1369–1374. [Google Scholar] [CrossRef] [PubMed]
- Strauss, K.A.; Robinson, D.L.; Vreman, H.J.; Puffenberger, E.G.; Hart, G.; Morton, D.H. Management of hyperbilirubinemia and prevention of kernicterus in 20 patients with Crigler-Najjar disease. Eur. J. Pediatr. 2006, 165, 306–319. [Google Scholar] [CrossRef] [PubMed]
- Strauss, K.A.; Ahlfors, C.E.; Soltys, K.; Mazareigos, G.V.; Young, M.; Bowser, L.E.; Fox, M.D.; Squires, J.E.; McKierman, P.; Brigatti, K.W.; et al. Crigler-Najjar syndrome type 1: Pathophysiology, natural history, and therapeutic frontier. Hepatology 2019, 71, 1923–1939. [Google Scholar] [CrossRef] [PubMed]
- Eghbalian, F.; Monsef, A. Phototherapy-induced hypocalcemia in icteric newborns. Iran J. Med. Sci. 2002, 27, 169–171. [Google Scholar]
- Karamifar, H.; Pishva, N.; Amirhakimi, G.H. Prevalence of phototherapy-induced hypocalcemia. Iran J. Med. Sci. 2002, 27, 166–168. [Google Scholar]
- Vigneshwar, N.K.V.; Basu, S.; Naithani, M.; Vivekanand, N.; Chacham, S.; Singh, P. Serum calcium and melatonin levels in neonates undergo phototherapy. Indian J. Pediatr. 2021, 88, 805–808. [Google Scholar] [CrossRef]
- Asghar, I.; Khan, I.A.; Hassan, F. Effect of head covering on phototherapy induced hypocalcemia in term neonates with hyperbilirubinemia: A randomized controlled study. J. Neonatal-Perinatal Med. 2021, 14, 245–251. [Google Scholar] [CrossRef]
- Hakanson, D.O.; Bergstrom, W.H. Phototherapy-induced hypocalcemia in newborn rats: Prevention by melatonin. Science 1981, 214, 807–809. [Google Scholar] [CrossRef] [PubMed]
- Ebbesen, F.; Edelsten, D.; Hertel, J. Gut transit time and lactose malabsorption during phototherapy. A study using lactose-free human mature milk. Acta Paediatr. Scand. 1980, 69, 65–68, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Gounaris, A.; Alexiou, N.; Costalos, C.; Daniilidou, M.; Bakoleas, V.; Constantellou, E. Gut hormone levels in neonates under phototherapy. Early Hum. Dev. 1998, 51, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Newman, T.B.; Wickremasinghe, A.C.; Walsh, E.M.; Grimes, B.A.; McCulloch, C.E.; Kuzniewicz, M.W. Retrospective cohort study of phototherapy and childhood cancer in Northern California. Pediatrics 2016, 137, e20151354. [Google Scholar] [CrossRef] [Green Version]
- Auger, N.; Laverdiere, C.; Ayoub, A.; Lo, E.; Luu, T.M. Neonatal phototherapy and future risk of childhood cancer. Int. J. Cancer 2019, 145, 2061–2069. [Google Scholar] [CrossRef]
- Wickremasinghe, A.C.; Kuzniewicz, M.W.; Grimes, B.A.; McCulloch, C.E.; Newman, T.B. Neonatal phototherapy and infantile cancer. Pediatrics 2016, 137, e20151353. [Google Scholar] [CrossRef] [Green Version]
- Podwin, D.; Kuehn, C.M.; Mueller, B.A.; Williams, M. Maternal and birth characteristics in relation to childhood leukaemia. Pediatr. Perinatal Epidemiol. 2006, 20, 312–322. [Google Scholar]
- Cnattingius, S.; Zack, M.; Ekbom, A.; Gunnarskog, J.; Linet, M.; Adami, H.O. Prenatal and neonatal risk factors for childhood myeloid leukemia. Cancer Epidemiol. Biomark. Prev. 1995, 4, 441–445. [Google Scholar]
- Olsen, J.H.; Hertz, H.; Kjaer, S.K.; Bautz, A.; Mellemkjaer, L.; Boice, J.D. Childhood leukemia following phototherapy for neonatal hyperbilirubinemia (Denmark). Cancer Causes Control. 1996, 7, 411–414. [Google Scholar] [CrossRef]
- Roman, E.; Ansell, P.; Bull, D. Leukaemia and non-Hodgkin’s lymphoma in children and young adults: Are prenatal and neonatal factors important determinants of disease? Br. J. Cancer 1997, 76, 406–415. [Google Scholar] [CrossRef] [Green Version]
- Gloria-Bottini, F.; Bottini, E. Is there a role of early neonatal events in susceptibility to allergy? Int. J. Biochem. Biomed. Sci. 2010, 6, 8–12. [Google Scholar]
- Aspberg, S.; Dahlquist, G.; Kahan, T.; Kaellen, B. Confirmed association between phototherapy or neonatal icterus and risk of childhood asthma. Pediatr. Allergy Immunol. 2010, 21, e733–e739. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.-C.; Lin, C.-L.; Shen, T.-C.; Kao, C.-H. Neonatal jaundice and risks of childhood allergic diseases: A population-based study. Pediatr. Res. 2015, 78, 223–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safar, H.; Elsary, A.Y. Neonatal jaundice: The other side of the coin in the development of allergy. Am. J. Perinatol. 2020, 37, 1357–1363. [Google Scholar] [CrossRef]
- Beken, S.; Aydin, B.; Zencirogglu, A.; Dilli, D.; Oskan, E.; Dursun, A.; Okumus, N. The effects of phototherapy on eosinophil and eosinophilic cationic protein in newborns with hyperbilirubinemia. Fetal Pediatr. Pathol. 2014, 33, 151–156. [Google Scholar] [CrossRef]
- Aydin, B.; Beken, S.; Zenciroglu, A.A.; Dilli, D.; Okumus, N. Blood eosinophil levels in newborns with severe indirect hyperbilirubinemia treated with phototherapy. Iran J. Pediatr. 2014, 24, 267–272. [Google Scholar]
- Can, C.; Hamilcikan, S. Effect of neonatal phototherapy on eosinophil levels in nonsevere hyperbilirubinemia. Am. J. Perinatol. 2020, 37, 929–932. [Google Scholar] [CrossRef]
- Dahlquist, G.; Kaellen, B. Indications that phototherapy is a risk factor for insulin-dependent diabetes. Diabetes Care 2003, 26, 247–248. [Google Scholar] [CrossRef] [Green Version]
- McNamee, M.B.; Cardwell, C.R.; Patterson, C.C. Neonatal jaundice is associated with a small increase in the risk of childhood type 1 diabetes: A meta-analysis of observational studies. Acta Diabetol. 2012, 49, 83–87. [Google Scholar] [CrossRef]
- Newman, T.B.; Wickremasinghe, A.C.; Walsh, E.M.; Grimes, B.A.; McCulloch, C.E.; Kuzniewicz, M.W. Phototherapy and risk of type 1 diabetes. Pediatrics 2016, 138, e20160687. [Google Scholar] [CrossRef] [Green Version]
- Maimburg, R.D.; Olsen, J.; Sun, Y. Neonatal hyperbilirubinemia and the risk of febrile seizures and childhood epilepsy. Epilepsy Res. 2016, 124, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Newman, T.B.; Wu, Y.W.; Kuzniewicz, M.W.; Grimes, B.A.; McCulloch, C.E. Childhood seizers after phototherapy. Pediatrics 2018, 142, e20180648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cansu, A.; Serdaroglu, A.; Yuksel, D.; Dogan, V.; Ozkan, S.; Hirfanoglu, T.; Senbil, N.; Gucuyener, K.; Soysal, S.; Camurdan, A.; et al. Prevalence of some risk factors in children with epilepsy compared with controls. Seizure 2007, 16, 338–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huseyinoglu, N.; Ozben, S.; Arhan, E.; Palanci, Y.; Gunes, N. Prevalence and risk factors of epilepsy among school children in Eastern Turkey. Pediatr. Neurol. 2012, 47, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Maimburg, R.D.; Bech, H.; Vaeth, M.; Møller-Madsen, B.; Olsen, J. Neonatal jaundice, autism, and other disorders of psychological development. Pediatrics 2010, 126, 872–878. [Google Scholar] [CrossRef]
- Lozada, L.E.; Nylund, C.M.; Gorman, G.H.; Hisle-Gorman, E.; Erdie-Lalena, C.R.; Kuehn, D. Association of autism spectrum disorders with neonatal hyperbilirubinemia. Glob. Pediatr. Health 2015, 2, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Gardener, H.; Spiegelman, D.; Buka, S.L. Perinatal and neonatal risk factors for autism: A comprehensive meta-analysis. Pediatrics 2011, 128, 344–355. [Google Scholar] [CrossRef]
- Hung, T.-W.; Tsai, J.-D.; Pan, H.-H.; Chen, H.-J.; Liao, P.-F.; Sheu, J.-N. Is neonatal hyperbilirubinemia exposure associated with a risk of autism spectrum disorder? A nationwide cohort study. Am. J. Perinatol. 2020, 38, 1244–1253. [Google Scholar] [CrossRef]
- Croen, L.A.; Yoshida, C.K.; Odouli, R.; Newman, T.B. Neonatal hyperbilirubinemia and risk of autism spectrum disorders. Pediatrics 2005, 115, e135–e138. [Google Scholar] [CrossRef]
| TNF-α | IL-1ß | IL-2 | IL-3 | IL-6 | IL-8 | IL-10 | CD3+ | |
|---|---|---|---|---|---|---|---|---|
| Kurt, A. et al. [58] | ↑ | ↑ | No change | ↑ | ↓ | |||
| Sirota, L. et al. [60] | No difference | ↓ | ↑ | No change | No change | ↑ | ||
| Procianoy, R. S. et al. [59] | No change | No change | ↓ * | No change | No change | |||
| Jasprova, J. et al. [6] ** | ↑ | ↑ | ↑ |
| Parameters | Effect | Reason | References |
|---|---|---|---|
| Photo-dynamic damage | Decrease | Reduced photo-oxidation and geno-cytotoxicity | [21,22,23,24,27,28] |
| Mortality of ELBW neonates | Decrease | Reduced photo-dynamic damage and hemodynamic responses | [21,22,23,24,27,28,42] |
| Riboflavin deficiency | Decrease | Photo-oxidation of riboflavin | [45,46,47,48] |
| Bronze Baby Syndrome | Increase | Increased production and retention of bronze pigments | [42] |
| Immune response | Increase | Increased production of pre-inflammatory cytokines | [6] |
| Hemodynamic responses | Decrease | Decreased exposure to visible light with wavelength >530 nm and infrared light (heat) | [63] |
| Transepidermal water loss | Decrease | As under hemodynamic responses | [63] |
| Hypo-/hyperthermia | Increase/Decrease | As under hemodynamic responses | [71,72] |
| Parent–neonate attachment and breast feeding | Increase | Shorter duration of phototherapy | [11] |
| Cancer frequency | Decrease | Decreased photo-dynamic damage | [84,85] |
| Allergic diseases | Increase | Increased immune response | [6] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ebbesen, F.; Vreman, H.J.; Hansen, T.W.R. Blue-Green (~480 nm) versus Blue (~460 nm) Light for Newborn Phototherapy—Safety Considerations. Int. J. Mol. Sci. 2023, 24, 461. https://doi.org/10.3390/ijms24010461
Ebbesen F, Vreman HJ, Hansen TWR. Blue-Green (~480 nm) versus Blue (~460 nm) Light for Newborn Phototherapy—Safety Considerations. International Journal of Molecular Sciences. 2023; 24(1):461. https://doi.org/10.3390/ijms24010461
Chicago/Turabian StyleEbbesen, Finn, Hendrik Jan Vreman, and Thor Willy Ruud Hansen. 2023. "Blue-Green (~480 nm) versus Blue (~460 nm) Light for Newborn Phototherapy—Safety Considerations" International Journal of Molecular Sciences 24, no. 1: 461. https://doi.org/10.3390/ijms24010461





