Evidence for Angiotensin II as a Naturally Existing Suppressor for the Guanylyl Cyclase A Receptor and Cyclic GMP Generation
Abstract
:1. Introduction
2. Results
2.1. Study Population
2.2. Correlations between ANGII and Natriuretic Peptides in Humans
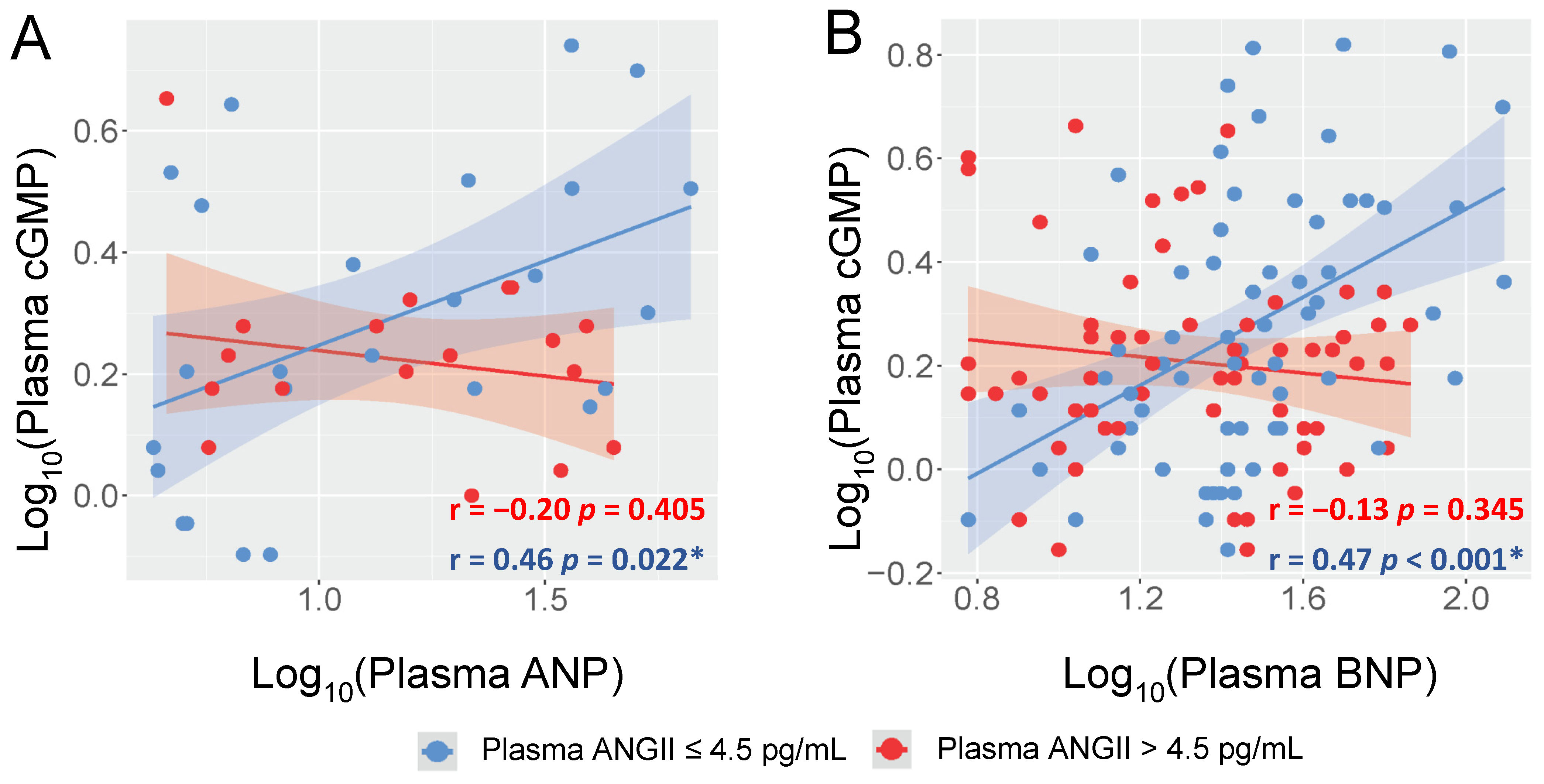
2.3. ANGII Interacts with the Correlations between cGMP and ANP/BNP in Humans
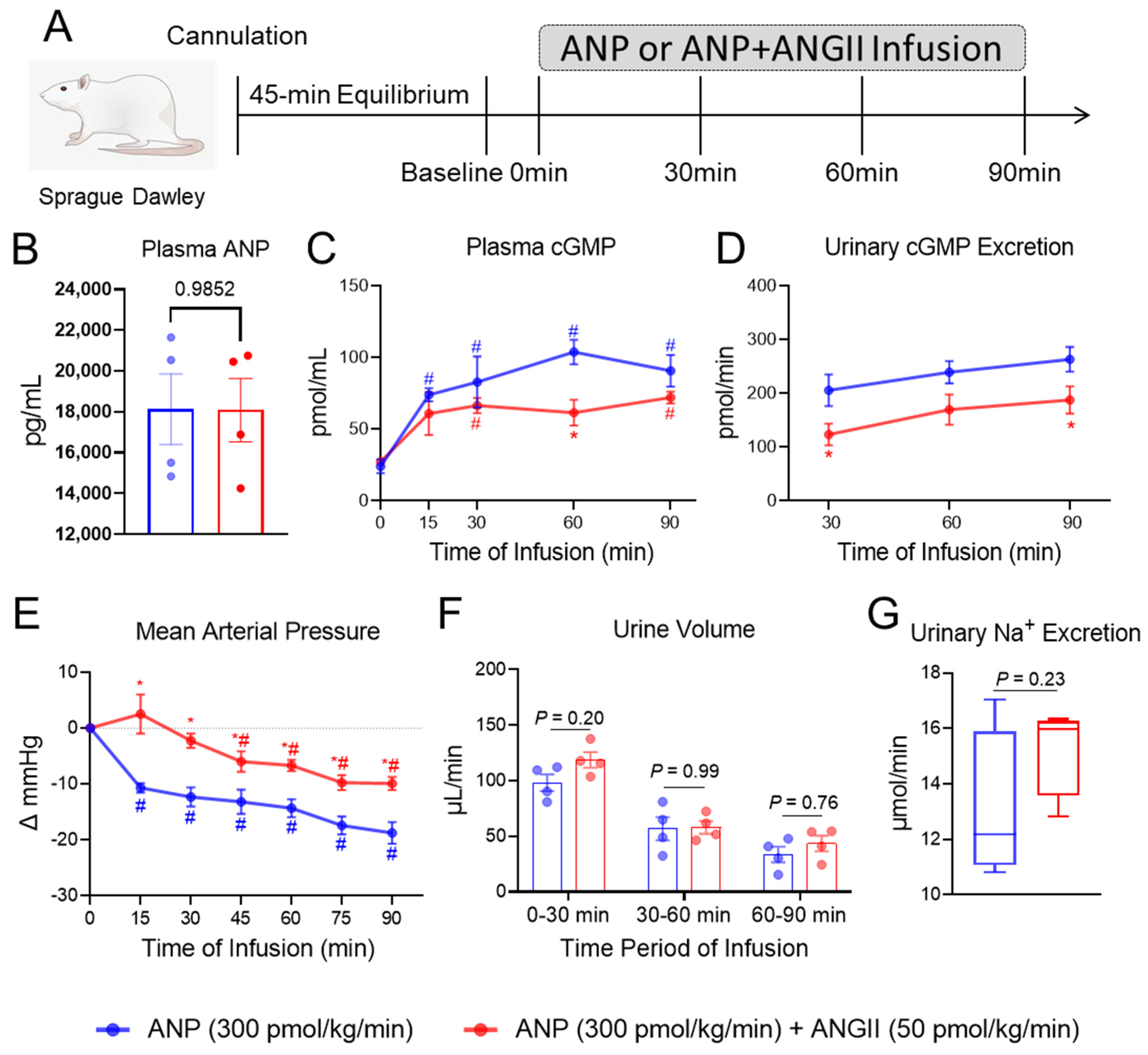
2.4. ANGII Attenuates ANP-Induced cGMP Production In Vivo
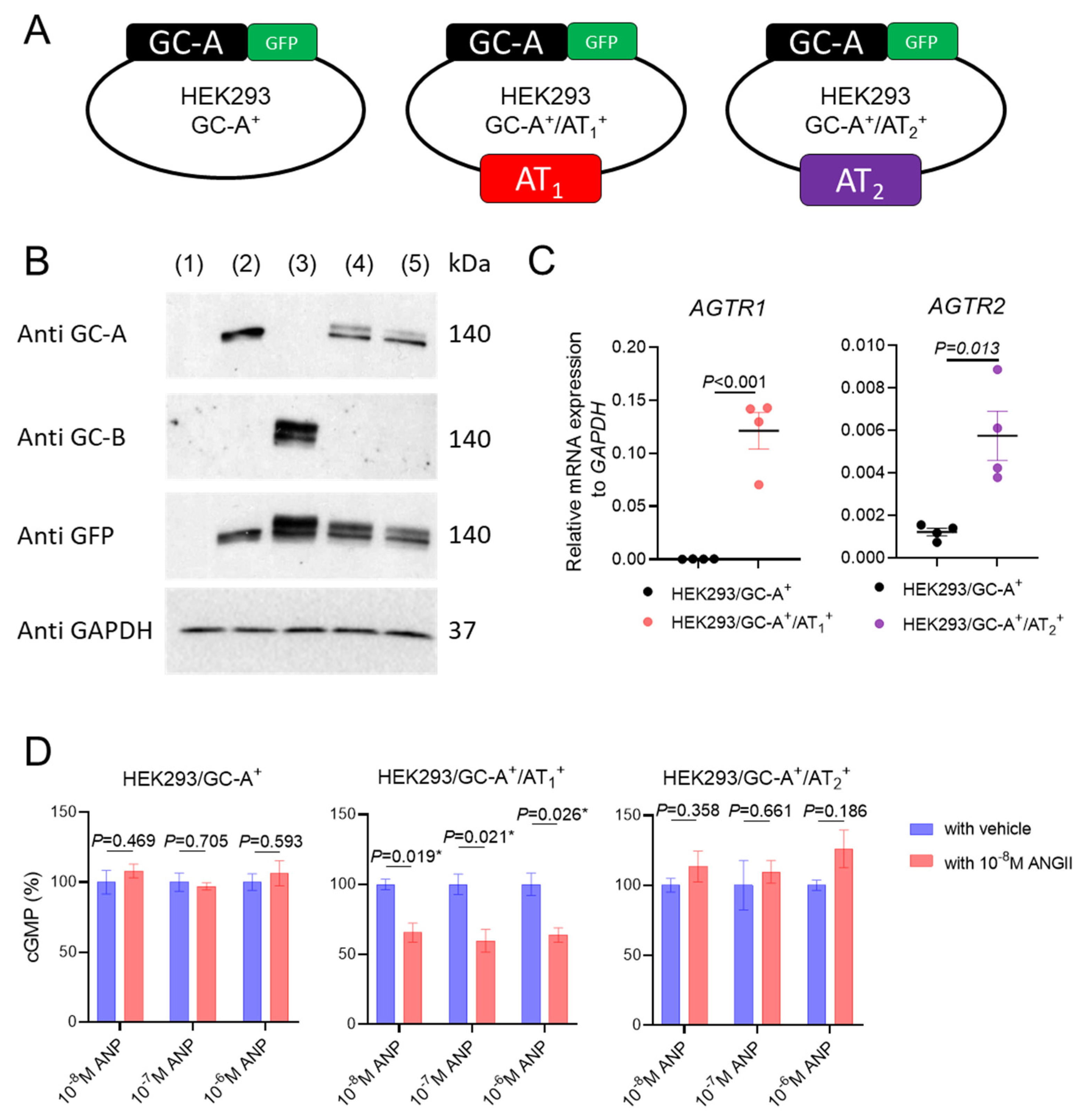
2.5. ANGII Suppresses GC-A Activity via AT1 Receptor
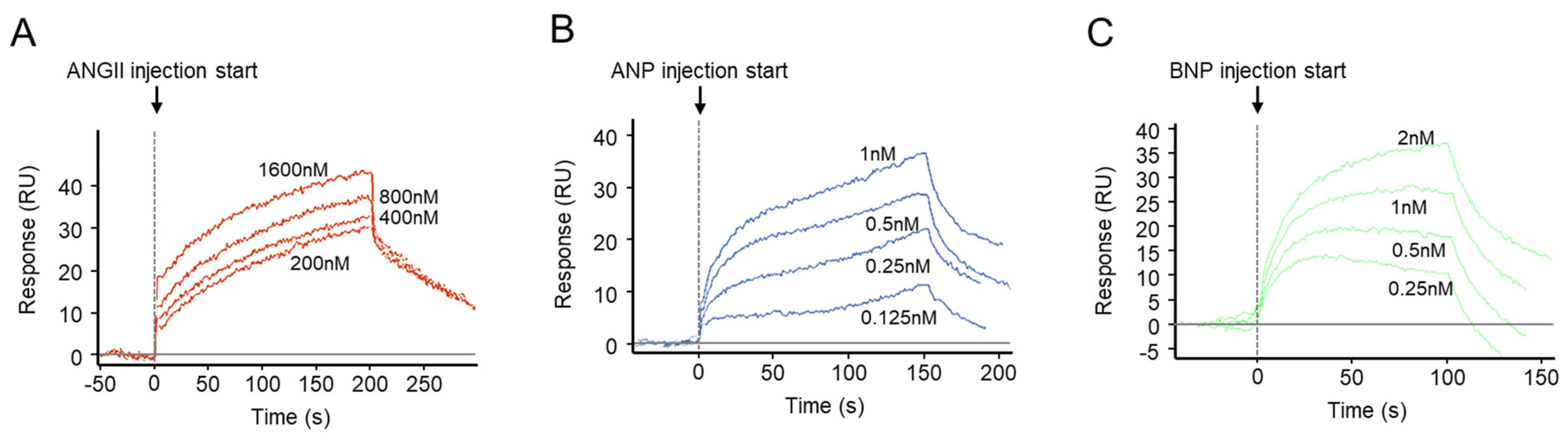
2.6. Binding Kinetics of ANGII to the Extracellular Domain of Human GC-A Receptor
2.7. Involvement of Protein Kinase C in the Interaction between ANGII/AT1 and GC-A
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Study Population
4.2. Biomarker Measurements in Human Plasma
4.3. Synthetic Peptides
4.4. In Vivo Rat Experiments
4.5. Generation and Maintenance of HEK293 Transfected Cell Lines
4.6. Intracellular cGMP Generation in HEK293 Transfected Cell Lines and Human Primary Renal Cells
4.7. Membrane and Cytosol Fractionation on HEK293 Transfected Cell Lines
4.8. Western Blotting
4.9. Real-Time Quantitative PCR
4.10. GC-A Binding Studies
4.11. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Non-Standard Abbreviations and Acronyms
| ACE | angiotensin converting enzyme |
| ARBs | AT1 receptor blockers |
| ANGII | angiotensin II |
| AT1 | ANGII type 1 receptor |
| BP | blood pressure |
| cGMP | 3′, 5′ cyclic guanosine monophosphate |
| CV | cardiovascular |
| GC-A | particulate guanylyl cyclase A |
| NPS | natriuretic peptide system |
| NP | natriuretic peptide |
| PKC | protein kinase C |
| RAAS | renin angiotensin aldosterone system |
| S/V | sacubitril/valsartan |
References
- Lee, C.Y.; Burnett, J.C., Jr. Natriuretic peptides and therapeutic applications. Heart Fail. Rev. 2007, 12, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Volpe, M.; Carnovali, M.; Mastromarino, V. The natriuretic peptides system in the pathophysiology of heart failure: From molecular basis to treatment. Clin. Sci. 2016, 130, 57–77. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M. Molecular Physiology of Membrane Guanylyl Cyclase Receptors. Physiol. Rev. 2016, 96, 751–804. [Google Scholar] [CrossRef] [PubMed]
- Pandey, K.N. Molecular and genetic aspects of guanylyl cyclase natriuretic peptide receptor-A in regulation of blood pressure and renal function. Physiol. Genom. 2018, 50, 913–928. [Google Scholar] [CrossRef]
- McFarlane, S.I.; Winer, N.; Sowers, J.R. Role of the natriuretic peptide system in cardiorenal protection. Arch. Intern. Med. 2003, 163, 2696–2704. [Google Scholar] [CrossRef]
- Sangaralingham, S.J.; Kuhn, M.; Cannone, V.; Chen, H.H.; Burnett, J.C. Natriuretic peptide pathways in heart failure: Further therapeutic possibilities. Cardiovasc. Res. 2023, 118, 3416–3433. [Google Scholar] [CrossRef] [PubMed]
- Goetze, J.P.; Bruneau, B.G.; Ramos, H.R.; Ogawa, T.; de Bold, M.K.; de Bold, A.J. Cardiac natriuretic peptides. Nat. Rev. Cardiol. 2020, 17, 698–717. [Google Scholar] [CrossRef]
- Stingo, A.J.; Clavell, A.L.; Heublein, D.M.; Wei, C.M.; Pittelkow, M.R.; Burnett, J.C., Jr. Presence of C-type natriuretic peptide in cultured human endothelial cells and plasma. Am. J. Physiol. 1992, 263, H1318–H1321. [Google Scholar] [CrossRef]
- Mattingly, M.T.; Brandt, R.R.; Heublein, D.M.; Wei, C.M.; Nir, A.; Burnett, J.C., Jr. Presence of C-type natriuretic peptide in human kidney and urine. Kidney Int. 1994, 46, 744–747. [Google Scholar] [CrossRef]
- Sangaralingham, S.J.; Heublein, D.M.; Grande, J.P.; Cataliotti, A.; Rule, A.D.; McKie, P.M.; Martin, F.L.; Burnett, J.C., Jr. Urinary C-type natriuretic peptide excretion: A potential novel biomarker for renal fibrosis during aging. Am. J. Physiol. Renal Physiol. 2011, 301, F943–F952. [Google Scholar] [CrossRef]
- Ma, X.; Chen, Y.; Reginauld, S.H.; Scott, C.G.; Iyer, S.R.; Schaefer, J.J.; Ichiki, T.; Chen, H.H.; Rule, A.D.; Burnett, J.C., Jr.; et al. Prognostic Value of Urinary and Plasma C-Type Natriuretic Peptide in Acute Decompensated Heart Failure. JACC Heart Fail. 2021, 9, 613–623. [Google Scholar] [CrossRef] [PubMed]
- Meems, L.M.G.; Burnett, J.C., Jr. Innovative Therapeutics: Designer Natriuretic Peptides. JACC Basic Transl. Sci. 2016, 1, 557–567. [Google Scholar] [CrossRef]
- Braunwald, E. The path to an angiotensin receptor antagonist-neprilysin inhibitor in the treatment of heart failure. J. Am. Coll. Cardiol. 2015, 65, 1029–1041. [Google Scholar] [CrossRef]
- Potter, L.R.; Yoder, A.R.; Flora, D.R.; Antos, L.K.; Dickey, D.M. Natriuretic peptides: Their structures, receptors, physiologic functions and therapeutic applications. Handb. Exp. Pharmacol. 2009, 2009, 341–366. [Google Scholar] [CrossRef]
- Suga, S.; Nakao, K.; Hosoda, K.; Mukoyama, M.; Ogawa, Y.; Shirakami, G.; Arai, H.; Saito, Y.; Kambayashi, Y.; Inouye, K.; et al. Receptor selectivity of natriuretic peptide family, atrial natriuretic peptide, brain natriuretic peptide, and C-type natriuretic peptide. Endocrinology 1992, 130, 229–239. [Google Scholar] [CrossRef]
- Chen, Y.; Zheng, Y.; Iyer, S.R.; Harders, G.E.; Pan, S.; Chen, H.H.; Ichiki, T.; Burnett, J.C., Jr.; Sangaralingham, S.J. C53: A novel particulate guanylyl cyclase B receptor activator that has sustained activity in vivo with anti-fibrotic actions in human cardiac and renal fibroblasts. J. Mol. Cell. Cardiol. 2019, 130, 140–150. [Google Scholar] [CrossRef]
- Lavoie, J.L.; Sigmund, C.D. Minireview: Overview of the renin-angiotensin system—An endocrine and paracrine system. Endocrinology 2003, 144, 2179–2183. [Google Scholar] [CrossRef]
- Ferrario, C.M.; Strawn, W.B. Role of the renin-angiotensin-aldosterone system and proinflammatory mediators in cardiovascular disease. Am. J. Cardiol. 2006, 98, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Paz Ocaranza, M.; Riquelme, J.A.; Garcia, L.; Jalil, J.E.; Chiong, M.; Santos, R.A.S.; Lavandero, S. Counter-regulatory renin-angiotensin system in cardiovascular disease. Nat. Rev. Cardiol. 2020, 17, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; Gonzalez-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.; Fonarow, G.C.; Givertz, M.M.; et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J. Am. Coll. Cardiol. 2016, 68, 1476–1488. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef]
- Arendse, L.B.; Danser, A.H.J.; Poglitsch, M.; Touyz, R.M.; Burnett, J.C., Jr.; Llorens-Cortes, C.; Ehlers, M.R.; Sturrock, E.D. Novel Therapeutic Approaches Targeting the Renin-Angiotensin System and Associated Peptides in Hypertension and Heart Failure. Pharmacol. Rev. 2019, 71, 539–570. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.I.; Hodsman, P.G.; Kohzuki, M.; Casley, D.J.; Fabris, B.; Phillips, P.A. Interaction between atrial natriuretic peptide and the renin angiotensin aldosterone system. Endogenous antagonists. Am. J. Med. 1989, 87, 24S–28S. [Google Scholar] [CrossRef]
- Richards, A.M. The renin-angiotensin-aldosterone system and the cardiac natriuretic peptides. Heart 1996, 76, 36–44. [Google Scholar] [CrossRef] [PubMed]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin-Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Velazquez, E.J.; Morrow, D.A.; DeVore, A.D.; Duffy, C.I.; Ambrosy, A.P.; McCague, K.; Rocha, R.; Braunwald, E.; Investigators, P.-H. Angiotensin-Neprilysin Inhibition in Acute Decompensated Heart Failure. N. Engl. J. Med. 2019, 380, 539–548. [Google Scholar] [CrossRef]
- Jackson, A.M.; Jhund, P.S.; Anand, I.S.; Dungen, H.D.; Lam, C.S.P.; Lefkowitz, M.P.; Linssen, G.; Lund, L.H.; Maggioni, A.P.; Pfeffer, M.A.; et al. Sacubitril-valsartan as a treatment for apparent resistant hypertension in patients with heart failure and preserved ejection fraction. Eur. Heart J. 2021, 42, 3741–3752. [Google Scholar] [CrossRef]
- Vellaichamy, E.; Zhao, D.; Somanna, N.; Pandey, K.N. Genetic disruption of guanylyl cyclase/natriuretic peptide receptor-A upregulates ACE and AT1 receptor gene expression and signaling: Role in cardiac hypertrophy. Physiol. Genomics 2007, 31, 193–202. [Google Scholar] [CrossRef]
- Periyasamy, R.; Das, S.; Pandey, K.N. Genetic disruption of guanylyl cyclase/natriuretic peptide receptor-A upregulates renal (pro) renin receptor expression in Npr1 null mutant mice. Peptides 2019, 114, 17–28. [Google Scholar] [CrossRef]
- Smith, J.B.; Lincoln, T.M. Angiotensin decreases cyclic GMP accumulation produced by atrial natriuretic factor. Am. J. Physiol. 1987, 253, C147–C150. [Google Scholar] [CrossRef]
- Ichiki, T.; Huntley, B.K.; Sangaralingham, S.J.; Burnett, J.C., Jr. Pro-Atrial Natriuretic Peptide: A Novel Guanylyl Cyclase-A Receptor Activator That Goes Beyond Atrial and B-Type Natriuretic Peptides. JACC Heart Fail. 2015, 3, 715–723. [Google Scholar] [CrossRef]
- Carey, R.M. AT2 Receptors: Potential Therapeutic Targets for Hypertension. Am. J. Hypertens. 2017, 30, 339–347. [Google Scholar] [CrossRef]
- Guo, D.F.; Sun, Y.L.; Hamet, P.; Inagami, T. The angiotensin II type 1 receptor and receptor-associated proteins. Cell Res. 2001, 11, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Forrester, S.J.; O’Brien, S.; Baggett, A.; Rizzo, V.; Eguchi, S. AT1 receptor signaling pathways in the cardiovascular system. Pharmacol. Res 2017, 125, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Potter, L.R.; Garbers, D.L. Dephosphorylation of the guanylyl cyclase-A receptor causes desensitization. J. Biol. Chem. 1992, 267, 14531–14534. [Google Scholar] [CrossRef]
- Potter, L.R.; Garbers, D.L. Protein kinase C-dependent desensitization of the atrial natriuretic peptide receptor is mediated by dephosphorylation. J. Biol. Chem. 1994, 269, 14636–14642. [Google Scholar] [CrossRef]
- Omland, T.; Aakvaag, A.; Bonarjee, V.V.; Caidahl, K.; Lie, R.T.; Nilsen, D.W.; Sundsfjord, J.A.; Dickstein, K. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction. Comparison with plasma atrial natriuretic peptide and N-terminal proatrial natriuretic peptide. Circulation 1996, 93, 1963–1969. [Google Scholar] [CrossRef] [PubMed]
- Cataliotti, A.; Malatino, L.S.; Jougasaki, M.; Zoccali, C.; Castellino, P.; Giacone, G.; Bellanuova, I.; Tripepi, R.; Seminara, G.; Parlongo, S.; et al. Circulating natriuretic peptide concentrations in patients with end-stage renal disease: Role of brain natriuretic peptide as a biomarker for ventricular remodeling. Mayo. Clin. Proc. 2001, 76, 1111–1119. [Google Scholar] [CrossRef]
- Wang, K.; Basu, R.; Poglitsch, M.; Bakal, J.A.; Oudit, G.Y. Elevated Angiotensin 1-7/Angiotensin II Ratio Predicts Favorable Outcomes in Patients with Heart Failure. Circ. Heart Fail. 2020, 13, e006939. [Google Scholar] [CrossRef]
- Zhao, D.; Guallar, E.; Vaidya, D.; Ndumele, C.E.; Ouyang, P.; Post, W.S.; Lima, J.A.; Ying, W.; Kass, D.A.; Hoogeveen, R.C.; et al. Cyclic Guanosine Monophosphate and Risk of Incident Heart Failure and Other Cardiovascular Events: The ARIC Study. J. Am. Heart Assoc. 2020, 9, e013966. [Google Scholar] [CrossRef]
- Buglioni, A.; Burnett, J.C., Jr. New Pharmacological Strategies to Increase cGMP. Annu. Rev. Med. 2016, 67, 229–243. [Google Scholar] [CrossRef]
- Ding, J.; Yu, M.; Jiang, J.; Luo, Y.; Zhang, Q.; Wang, S.; Yang, F.; Wang, A.; Wang, L.; Zhuang, M.; et al. Angiotensin II Decreases Endothelial Nitric Oxide Synthase Phosphorylation via AT(1)R Nox/ROS/PP2A Pathway. Front. Physiol. 2020, 11, 566410. [Google Scholar] [CrossRef]
- Crassous, P.A.; Couloubaly, S.; Huang, C.; Zhou, Z.; Baskaran, P.; Kim, D.D.; Papapetropoulos, A.; Fioramonti, X.; Duran, W.N.; Beuve, A. Soluble guanylyl cyclase is a target of angiotensin II-induced nitrosative stress in a hypertensive rat model. Am. J. Physiol. Heart Circ. Physiol. 2012, 303, H597–H604. [Google Scholar] [CrossRef]
- Petraina, A.; Nogales, C.; Krahn, T.; Mucke, H.; Luscher, T.F.; Fischmeister, R.; Kass, D.A.; Burnett, J.C.; Hobbs, A.J.; Schmidt, H. Cyclic GMP modulating drugs in cardiovascular diseases: Mechanism-based network pharmacology. Cardiovasc. Res. 2021, 118, 2085–2102. [Google Scholar] [CrossRef]
- Blanton, R.M. cGMP Signaling and Modulation in Heart Failure. J. Cardiovasc. Pharmacol. 2020, 75, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Abraham, W.T.; Hensen, J.; Kim, J.K.; Durr, J.; Lesnefsky, E.J.; Groves, B.M.; Schrier, R.W. Atrial natriuretic peptide and urinary cyclic guanosine monophosphate in patients with chronic heart failure. J. Am. Soc. Nephrol. 1992, 2, 1697–1703. [Google Scholar] [CrossRef] [PubMed]
- Jakob, G.; Mair, J.; Vorderwinkler, K.P.; Judmaier, G.; Konig, P.; Zwierzina, H.; Pichler, M.; Puschendorf, B. Clinical significance of urinary cyclic guanosine monophosphate in diagnosis of heart failure. Clin. Chem. 1994, 40, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Reginauld, S.H.; Cannone, V.; Iyer, S.; Scott, C.; Bailey, K.; Schaefer, J.; Chen, Y.; Sangaralingham, S.J.; Burnett, J.C., Jr. Differential Regulation of ANP and BNP in Acute Decompensated Heart Failure: Deficiency of ANP. JACC Heart Fail. 2019, 7, 891–898. [Google Scholar] [CrossRef]
- Cambien, F.; Poirier, O.; Lecerf, L.; Evans, A.; Cambou, J.P.; Arveiler, D.; Luc, G.; Bard, J.M.; Bara, L.; Ricard, S.; et al. Deletion polymorphism in the gene for angiotensin-converting enzyme is a potent risk factor for myocardial infarction. Nature 1992, 359, 641–644. [Google Scholar] [CrossRef]
- Lisy, O.; Huntley, B.K.; McCormick, D.J.; Kurlansky, P.A.; Burnett, J.C., Jr. Design, synthesis, and actions of a novel chimeric natriuretic peptide: CD-NP. J. Am. Coll. Cardiol. 2008, 52, 60–68. [Google Scholar] [CrossRef]
- McKie, P.M.; Cataliotti, A.; Huntley, B.K.; Martin, F.L.; Olson, T.M.; Burnett, J.C., Jr. A human atrial natriuretic peptide gene mutation reveals a novel peptide with enhanced blood pressure-lowering, renal-enhancing, and aldosterone-suppressing actions. J. Am. Coll. Cardiol. 2009, 54, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Harty, G.J.; Zheng, Y.; Iyer, S.R.; Sugihara, S.; Sangaralingham, S.J.; Ichiki, T.; Grande, J.P.; Lee, H.C.; Wang, X.; et al. Crrl269. Circ. Res. 2019, 124, 1462–1472. [Google Scholar] [CrossRef]
- Savarirayan, R.; Irving, M.; Day, J. C-Type Natriuretic Peptide Analogue Therapy in Children with Achondroplasia. Reply. N. Engl. J. Med. 2019, 381, 1291–1292. [Google Scholar] [CrossRef]
- Sangaralingham, S.J.; Whig, K.; Peddibhotla, S.; Kirby, R.J.; Sessions, H.E.; Maloney, P.R.; Hershberger, P.M.; Mose-Yates, H.; Hood, B.L.; Vasile, S.; et al. Discovery of small molecule guanylyl cyclase A receptor positive allosteric modulators. Proc. Natl. Acad. Sci. USA 2021, 118, e2109386118. [Google Scholar] [CrossRef]
- Kohzuki, M.; Hodsman, G.P.; Johnston, C.I. Attenuated response to atrial natriuretic peptide in rats with myocardial infarction. Am. J. Physiol. 1989, 256, H533–H538. [Google Scholar] [CrossRef]
- Kim, D.; Aizawa, T.; Wei, H.; Pi, X.; Rybalkin, S.D.; Berk, B.C.; Yan, C. Angiotensin II increases phosphodiesterase 5A expression in vascular smooth muscle cells: A mechanism by which angiotensin II antagonizes cGMP signaling. J. Mol. Cell. Cardiol. 2005, 38, 175–184. [Google Scholar] [CrossRef]
- Gopi, V.; Subramanian, V.; Manivasagam, S.; Vellaichamy, E. Angiotensin II down-regulates natriuretic peptide receptor-A expression and guanylyl cyclase activity in H9c2 (2-1) cardiac myoblast cells: Role of ROS and NF-kappaB. Mol. Cell. Biochem. 2015, 409, 67–79. [Google Scholar] [CrossRef]
- Arise, K.K.; Kumar, P.; Garg, R.; Samivel, R.; Zhao, H.; Pandya, K.; Nguyen, C.; Lindsey, S.; Pandey, K.N. Angiotensin II represses Npr1 expression and receptor function by recruitment of transcription factors CREB and HSF-4a and activation of HDACs. Sci. Rep. 2020, 10, 4337. [Google Scholar] [CrossRef]
- Haneda, M.; Kikkawa, R.; Maeda, S.; Togawa, M.; Koya, D.; Horide, N.; Kajiwara, N.; Shigeta, Y. Dual mechanism of angiotensin II inhibits ANP-induced mesangial cGMP accumulation. Kidney Int. 1991, 40, 188–194. [Google Scholar] [CrossRef]
- Mollnau, H.; Wendt, M.; Szocs, K.; Lassegue, B.; Schulz, E.; Oelze, M.; Li, H.; Bodenschatz, M.; August, M.; Kleschyov, A.L.; et al. Effects of angiotensin II infusion on the expression and function of NAD(P)H oxidase and components of nitric oxide/cGMP signaling. Circ. Res. 2002, 90, E58–E65. [Google Scholar] [CrossRef]
- Nakamura, M.; Arakawa, N.; Yoshida, H.; Makita, S.; Hiramori, K. Vasodilatory effects of C-type natriuretic peptide on forearm resistance vessels are distinct from those of atrial natriuretic peptide in chronic heart failure. Circulation 1994, 90, 1210–1214. [Google Scholar] [CrossRef]
- Nakamura, M.; Arakawa, N.; Yoshida, H.; Makita, S.; Niinuma, H.; Hiramori, K. Vasodilatory effects of B-type natriuretic peptide are impaired in patients with chronic heart failure. Am. Heart J. 1998, 135, 414–420. [Google Scholar] [CrossRef]
- Margulies, K.B.; Perrella, M.A.; McKinley, L.J.; Burnett, J.C., Jr. Angiotensin inhibition potentiates the renal responses to neutral endopeptidase inhibition in dogs with congestive heart failure. J. Clin. Investig. 1991, 88, 1636–1642. [Google Scholar] [CrossRef] [PubMed]
- Bottari, S.P.; King, I.N.; Reichlin, S.; Dahlstroem, I.; Lydon, N.; de Gasparo, M. The angiotensin AT2 receptor stimulates protein tyrosine phosphatase activity and mediates inhibition of particulate guanylate cyclase. Biochem. Biophys. Res. Commun. 1992, 183, 206–211. [Google Scholar] [CrossRef]
- Potter, L.R.; Hunter, T. Phosphorylation of the kinase homology domain is essential for activation of the A-type natriuretic peptide receptor. Mol. Cell. Biol. 1998, 18, 2164–2172. [Google Scholar] [CrossRef]
- Garg, R.; Pandey, K.N. Angiotensin II-mediated negative regulation of Npr1 promoter activity and gene transcription. Hypertension 2003, 41, 730–736. [Google Scholar] [CrossRef]
- Burnett, J.C., Jr.; Kao, P.C.; Hu, D.C.; Heser, D.W.; Heublein, D.; Granger, J.P.; Opgenorth, T.J.; Reeder, G.S. Atrial natriuretic peptide elevation in congestive heart failure in the human. Science 1986, 231, 1145–1147. [Google Scholar] [CrossRef]
- Chen, Y.; Schaefer, J.J.; Iyer, S.R.; Harders, G.E.; Pan, S.; Sangaralingham, S.J.; Chen, H.H.; Redfield, M.M.; Burnett, J.C., Jr. Long-term blood pressure lowering and cGMP-activating actions of the novel ANP analog MANP. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2020, 318, R669–R676. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total (N = 128) | High ANGII Group (N = 61) | Low ANGII Group (N = 67) | p Value |
|---|---|---|---|---|
| Age, years | 57 ± 12 | 55 ± 13 | 59 ± 12 | 0.08 |
| Sex, female | 71% | 67% | 73% | 0.46 |
| BMI, kg/m2 | 27 ± 5 | 27 ± 5 | 27 ± 5 | 0.95 |
| eGFR, mL/min/1.73 m2 | 84 ± 13 | 86 ± 13 | 83 ± 13 | 0.18 |
| Plasma Variables | ||||
| ANP, pg/mL | 4.0 (4, 6.4) | 4.0 (4.0, 6.1) | 4.0 (4.0, 6.8) | 0.54 |
| BNP, pg/mL | 26.0 (15.0, 38.5) | 22.0 (12.0, 36.5) | 27.0 (19.5, 40.0) | 0.04 |
| CNP, pg/mL | 11.6 (9.4, 15.0) | 11.3 (9.4, 14.7) | 12.8 (9.0, 16.0) | 0.45 |
| cGMP, pmol/mL | 1.6 (1.2, 2.4) | 1.6 (1.2, 1.9) | 1.7 (1.2, 2.9) | 0.20 |
| ANGII, pg/mL | 4.5 (3.4, 6.1) | 6.1 (5.3, 8.4) | 3.5 (2.4, 4.1) | <0.001 |
| Renin, ng/mL/hour | 0.97 (0.54, 2.05) | 1.37 (0.68, 2.38) | 0.74 (0.33, 1.79) | 0.003 |
| Aldosterone, ng/dL | 6.3 (3.9, 11.4) | 6.1 (3.8, 11.3) | 6.9 (4.0, 11.5) | 0.23 |
| Model | R2 | ΔR2 | Pmodel | Pinteraction |
|---|---|---|---|---|
| ANP base model # | 0.275 | --- | 0.039 | --- |
| ANP base model # + ANGII + ANP * ANGII | 0.330 | 0.055 | 0.028 | 0.06 |
| BNP base model | 0.133 | --- | 0.006 | --- |
| BNP base model + ANGII + BNP * ANGII | 0.225 | 0.092 | <0.001 | <0.001 |
| CNP base model | 0.143 | --- | 0.009 | --- |
| CNP base model + ANGII + CNP * ANGII | 0.166 | 0.014 | 0.012 | 0.20 |
| Peptide | Ka (M−1s−1) | Kd (s−1) | KD (nM) |
|---|---|---|---|
| ANGII | 7.6 × 103 | 2.0 × 10−3 | 258 |
| ANP | 4.1 × 107 | 1.4 × 10−2 | 0.342 |
| BNP | 4.6 × 107 | 3.9 × 10−2 | 0.843 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, X.; Iyer, S.R.; Ma, X.; Reginauld, S.H.; Chen, Y.; Pan, S.; Zheng, Y.; Moroni, D.G.; Yu, Y.; Zhang, L.; et al. Evidence for Angiotensin II as a Naturally Existing Suppressor for the Guanylyl Cyclase A Receptor and Cyclic GMP Generation. Int. J. Mol. Sci. 2023, 24, 8547. https://doi.org/10.3390/ijms24108547
Ma X, Iyer SR, Ma X, Reginauld SH, Chen Y, Pan S, Zheng Y, Moroni DG, Yu Y, Zhang L, et al. Evidence for Angiotensin II as a Naturally Existing Suppressor for the Guanylyl Cyclase A Receptor and Cyclic GMP Generation. International Journal of Molecular Sciences. 2023; 24(10):8547. https://doi.org/10.3390/ijms24108547
Chicago/Turabian StyleMa, Xiao, Seethalakshmi R. Iyer, Xiaoyu Ma, Shawn H. Reginauld, Yang Chen, Shuchong Pan, Ye Zheng, Dante G. Moroni, Yue Yu, Lianwen Zhang, and et al. 2023. "Evidence for Angiotensin II as a Naturally Existing Suppressor for the Guanylyl Cyclase A Receptor and Cyclic GMP Generation" International Journal of Molecular Sciences 24, no. 10: 8547. https://doi.org/10.3390/ijms24108547






