Recombinant ADAMTS-13 Improves Survival of Mice Subjected to Endotoxemia
Abstract
1. Introduction
2. Results
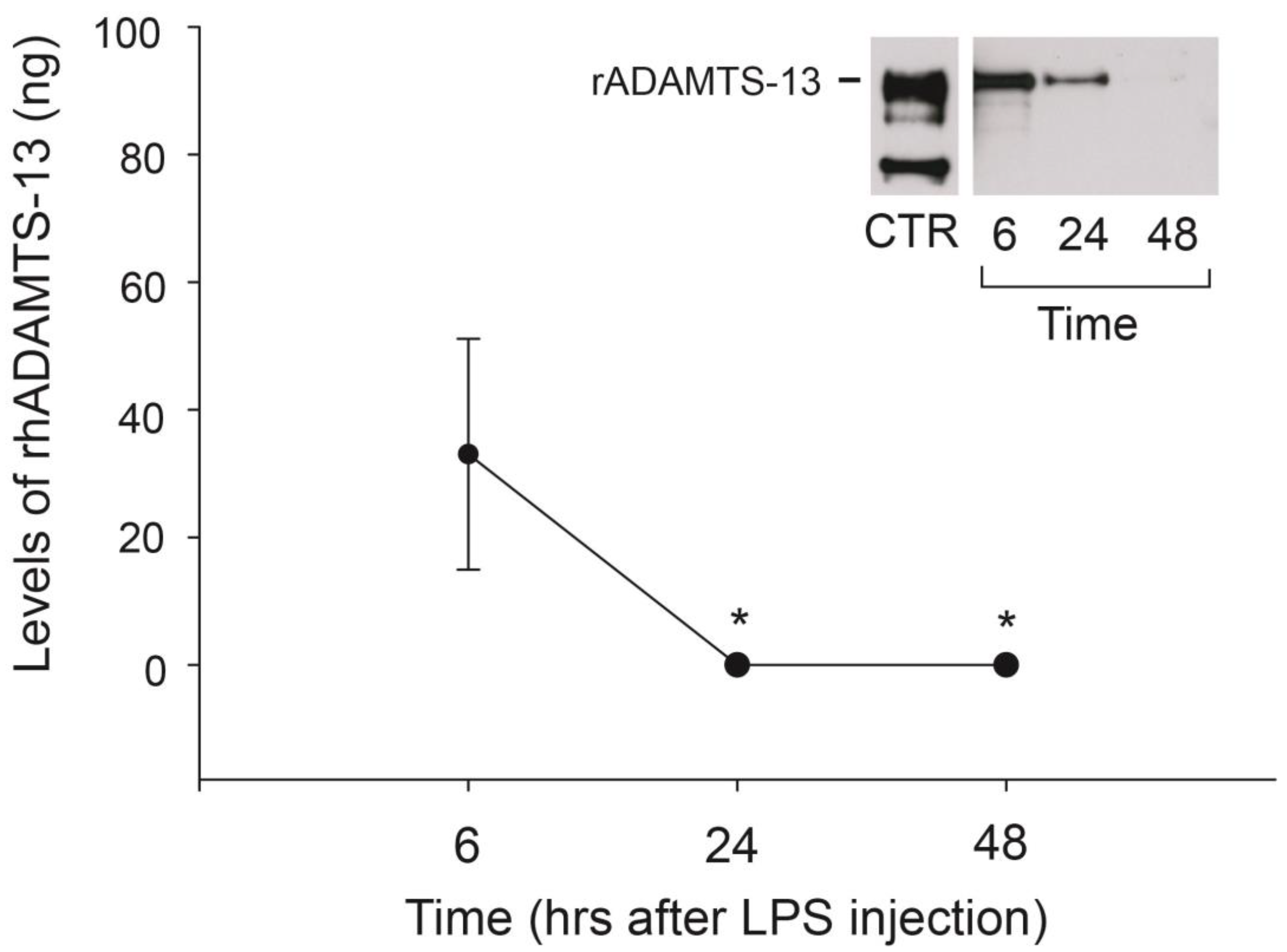
2.1. rhADAMTS-13 Had a Relatively Slow Rate of Clearance
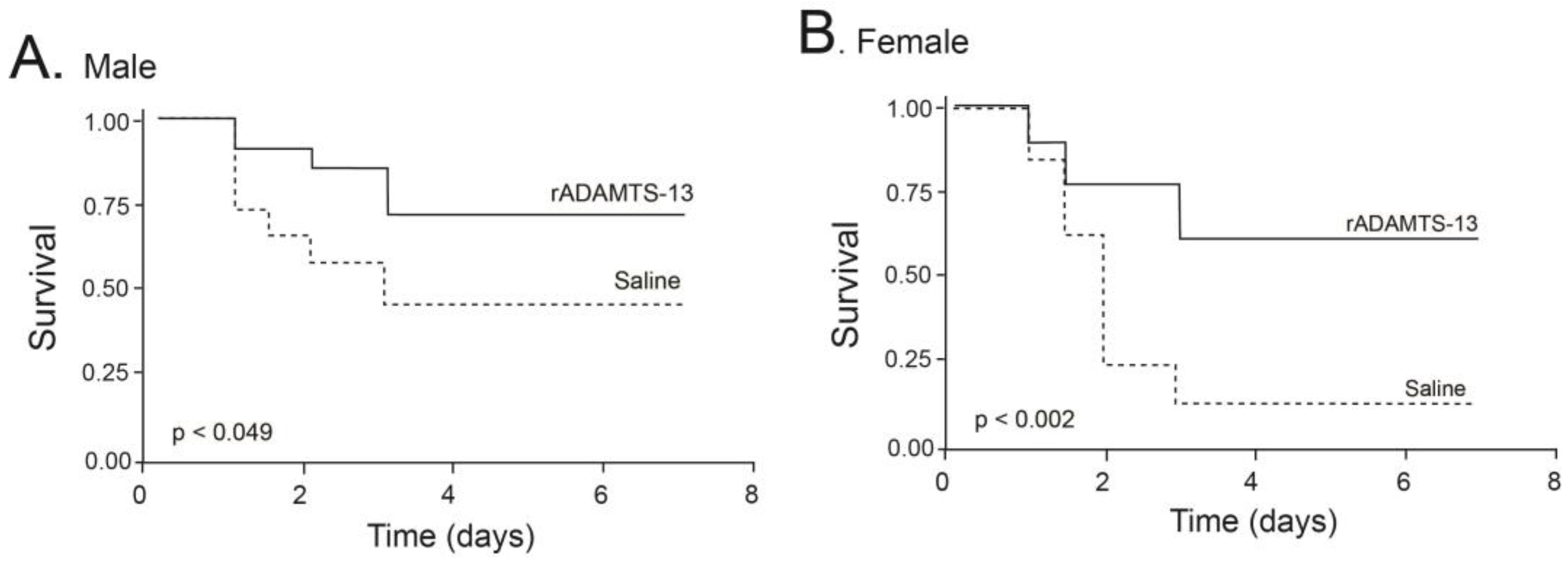
2.2. Infusion of rhADAMTS-13 Improved Survival of Mice with Endotoxemia
2.3. Infusion of rhADAMTS-13 Improved Thrombocytopenia
2.4. Endotoxemia Decreased ADAMTS-13 Activity
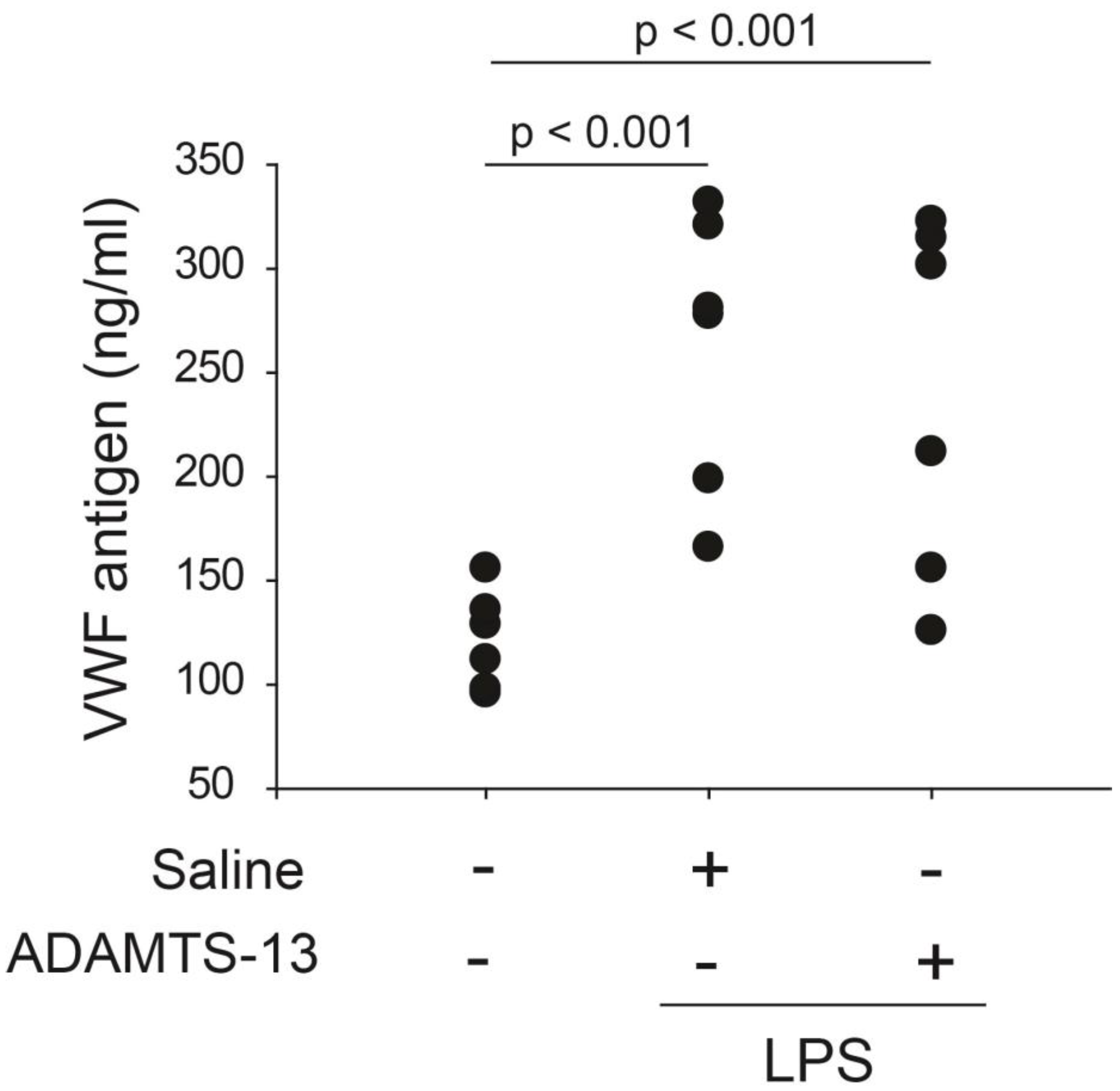
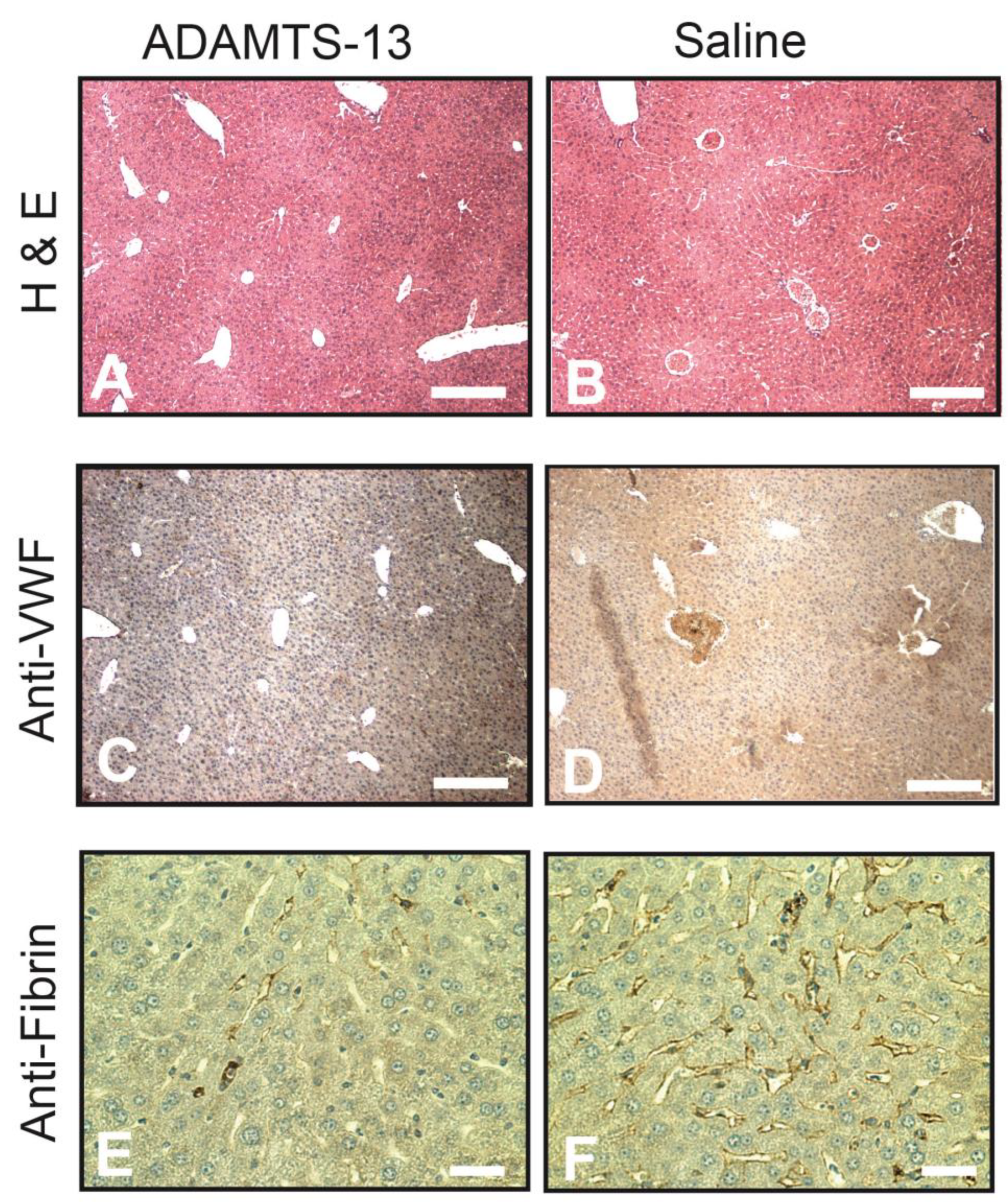
2.5. Infusion of rhADAMTS-13 Reduced Thrombosis
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Expression and Purification of Recombinant ADAMTS-13
4.2. Mouse Model and Treatment Schedule
4.3. Clearance of Infused rhADAMTS-13
4.4. ADAMTS-13 Activity under Flow Conditions
4.5. Plasma VWF Antigen, Platelet Counts, and D-Dimer
4.6. Immunohistochemistry
4.7. Data Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gragnano, F.; Sperlongano, S.; Golia, E.; Natale, F.; Bianchi, R.; Crisci, M.; Fimiani, F.; Pariggiano, I.; Diana, V.; Carbone, A.; et al. The Role of von Willebrand Factor in Vascular Inflammation: From Pathogenesis to Targeted Therapy. Mediat. Inflamm. 2017, 2017, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lenting, P.J.; Christophe, O.D.; Denis, C.V. von Willebrand factor biosynthesis, secretion, and clearance: Connecting the far ends. Blood 2015, 125, 2019–2028. [Google Scholar] [CrossRef] [PubMed]
- Arya, M.; Anvari, B.; Romo, G.M.; Cruz, M.A.; Dong, J.-F.; McIntire, L.V.; Moake, J.L.; López, J.A. Ultralarge multimers of von Willebrand factor form spontaneous high-strength bonds with the platelet glycoprotein Ib-IX complex: Studies using optical tweezers. Blood 2002, 99, 3971–3977. [Google Scholar] [CrossRef] [PubMed]
- Ju, L.; Dong, J.-F.; Cruz, M.A.; Zhu, C. The N-terminal Flanking Region of the A1 Domain Regulates the Force-dependent Binding of von Willebrand Factor to Platelet Glycoprotein Ibα. J. Biol. Chem. 2013, 288, 32289–32301. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chung, D.W. Inflammation, von Willebrand factor, and ADAMTS13. Blood 2018, 132, 141–147. [Google Scholar] [CrossRef]
- Dong, J.-F.; Moake, J.L.; Nolasco, L.; Bernardo, A.; Arceneaux, W.; Shrimpton, C.N.; Schade, A.J.; McIntire, L.V.; Fujikawa, K.; López, J.A. ADAMTS-13 rapidly cleaves newly secreted ultralarge von Willebrand factor multimers on the endothelial surface under flowing conditions. Blood 2002, 100, 4033–4039. [Google Scholar] [CrossRef]
- Dong, J.-F. Cleavage of ultra-large von Willebrand factor by ADAMTS-13 under flow conditions. J. Thromb. Haemost. 2005, 3, 1710–1716. [Google Scholar] [CrossRef]
- DeYoung, V.; Singh, K.; Kretz, C.A. Mechanisms of ADAMTS13 regulation. J. Thromb. Haemost. 2022, 20, 2722–2732. [Google Scholar] [CrossRef]
- Zheng, X.L. ADAMTS13 and von Willebrand Factor in Thrombotic Thrombocytopenic Purpura. Annu. Rev. Med. 2015, 66, 211–225. [Google Scholar] [CrossRef]
- Levy, G.G.; Nichols, W.C.; Lian, E.C.; Foroud, T.; McClintick, J.N.; McGee, B.M.; Yang, A.Y.; Siemieniak, D.R.; Stark, K.R.; Gruppo, R.; et al. Mutations in a member of the ADAMTS gene family cause thrombotic thrombocytopenic purpura. Nature 2001, 413, 488–494. [Google Scholar] [CrossRef]
- Thomas, M.R.; de Groot, R.; Scully, M.A.; Crawley, J.T.B. Pathogenicity of Anti-ADAMTS13 Autoantibodies in Acquired Thrombotic Thrombocytopenic Purpura. EBioMedicine 2015, 2, 942–952. [Google Scholar] [CrossRef]
- Jiang, Y.; McIntosh, J.J.; Reese, J.A.; Deford, C.C.; Kremer Hovinga, J.A.; Lämmle, B.; Terrell, D.R.; Vesely, S.K.; Knudtson, E.J.; George, J.N. Pregnancy outcomes following recovery from acquired thrombotic thrombocytopenic purpura. Blood 2014, 123, 1674–1680. [Google Scholar] [CrossRef]
- Nguyen, T.C.; Liu, A.; Liu, L.; Ball, C.; Choi, H.; May, W.S.; Aboulfatova, K.; Bergeron, A.L.; Dong, J.-F. Acquired ADAMTS-13 deficiency in pediatric patients with severe sepsis. Haematologica 2007, 92, 121–124. [Google Scholar] [CrossRef]
- Schwameis, M.; Schörgenhofer, C.; Assinger, A.; Steiner, M.M.; Jilma, B. VWF excess and ADAMTS13 deficiency: A unifying pathomechanism linking inflammation to thrombosis in DIC, malaria, and TTP. Thromb. Haemost. 2015, 113, 708–718. [Google Scholar] [CrossRef]
- Lin, E.; Calvano, S.E.; Lowry, S.F. Inflammatory cytokines and cell response in surgery. Surgery 2000, 127, 117–126. [Google Scholar] [CrossRef]
- Ono, T.; Mimuro, J.; Madoiwa, S.; Soejima, K.; Kashiwakura, Y.; Ishiwata, A.; Takano, K.; Ohmori, T.; Sakata, Y. Severe secondary deficiency of von Willebrand factor-cleaving protease (ADAMTS13) in patients with sepsis-induced disseminated intravascular coagulation: Its correlation with development of renal failure. Blood 2006, 107, 528–534. [Google Scholar] [CrossRef]
- Karim, F.; Adil, S.N.; Afaq, B.; ul Haq, A. Deficiency of ADAMTS-13 in pediatric patients with severe sepsis and impact on in-hospital mortality. BMC Pediatr. 2013, 13, 44. [Google Scholar] [CrossRef]
- Nguyen, T.C.; Han, Y.Y.; Kiss, J.E.; Hall, M.W.; Hassett, A.C.; Jaffe, R.; Orr, R.A.; Janosky, J.; Carcillo, J.A. Intensive plasma exchange increases a disintegrin and metalloprotease with thrombospondin motifs-13 activity and reverses organ dysfunction in children with thrombocytopenia-associated multiple organ failure. Crit. Care Med. 2008, 36, 2878–2887. [Google Scholar] [CrossRef]
- Reiter, R.A.; Knöbl, P.; Varadi, K.; Turecek, P.L. Changes in von Willebrand factor-cleaving protease (ADAMTS13) activity after infusion of desmopressin. Blood 2003, 101, 946–948. [Google Scholar] [CrossRef]
- Takaya, H.; Namisaki, T.; Asada, S.; Iwai, S.; Kubo, T.; Suzuki, J.; Enomoto, M.; Tsuji, Y.; Fujinaga, Y.; Nishimura, N.; et al. ADAMTS13, VWF, and Endotoxin Are Interrelated and Associated with the Severity of Liver Cirrhosis via Hypercoagulability. J. Clin. Med. 2022, 11, 1835. [Google Scholar] [CrossRef]
- Mannucci, P.M.; Capoferri, C.; Canciani, M.T. Plasma levels of von Willebrand factor regulate ADAMTS-13, its major cleaving protease. Br. J. Haematol. 2004, 126, 213–218. [Google Scholar] [CrossRef]
- Crawley, J.T.B.; Lam, J.K.; Rance, J.B.; Mollica, L.R.; O’Donnell, J.S.; Lane, D.A. Proteolytic inactivation of ADAMTS13 by thrombin and plasmin. Blood 2005, 105, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, A.K.; Motto, D.G.; Lamb, C.B.; Bergmeier, W.; Dockal, M.; Plaimauer, B.; Scheiflinger, F.; Ginsburg, D.; Wagner, D.D. Systemic antithrombotic effects of ADAMTS13. J. Exp. Med. 2006, 203, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Camerer, E.; Cornelissen, I.; Kataoka, H.; Duong, D.N.; Zheng, Y.-W.; Coughlin, S.R. Roles of protease-activated receptors in a mouse model of endotoxemia. Blood 2006, 107, 3912–3921. [Google Scholar] [CrossRef] [PubMed]
- Netea, M.G.; Demacker, P.N.; Kullberg, B.J.; Boerman, O.C.; Verschueren, I.; Stalenhoef, A.F.; van der Meer, J.W. Low-density lipoprotein receptor-deficient mice are protected against lethal endotoxemia and severe gram-negative infections. J. Clin. Investig. 1996, 97, 1366–1372. [Google Scholar] [CrossRef]
- Motto, D.G.; Chauhan, A.K.; Zhu, G.; Homeister, J.; Lamb, C.B.; Desch, K.C.; Zhang, W.; Tsai, H.-M.; Wagner, D.D.; Ginsburg, D. Shigatoxin triggers thrombotic thrombocytopenic purpura in genetically susceptible ADAMTS13-deficient mice. J. Clin. Investig. 2005, 115, 2752–2761. [Google Scholar] [CrossRef]
- Galgano, L.; Guidetti, G.F.; Torti, M.; Canobbio, I. The Controversial Role of LPS in Platelet Activation In Vitro. Int. J. Mol. Sci. 2022, 23, 10900. [Google Scholar] [CrossRef]
- Bernardo, A.; Ball, C.; Nolasco, L.; Moake, J.F.; Dong, J.-F. Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von Willebrand factor multimers under flow. Blood 2004, 104, 100–106. [Google Scholar] [CrossRef]
- Novelli, E.M.; Kato, G.J.; Hildesheim, M.E.; Barge, S.; Meyer, M.P.; Lozier, J.; Hassett, A.C.; Ragni, M.V.; Isenberg, J.S.; Gladwin, M.T. Thrombospondin-1 inhibits ADAMTS13 activity in sickle cell disease. Haematologica 2013, 98, e132–e134. [Google Scholar] [CrossRef]
- Padilla, A.; Moake, J.L.; Bernardo, A.; Ball, C.; Wang, Y.; Arya, M.; Nolasco, L.; Turner, N.; Berndt, M.C.; Anvari, B.; et al. P-selectin anchors newly released ultralarge von Willebrand factor multimers to the endothelial cell surface. Blood 2004, 103, 2150–2156. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, J.; Ling, M.; López, J.A.; Chung, D.W.; Fu, X. Hypochlorous acid generated by neutrophils inactivates ADAMTS13: An oxidative mechanism for regulating ADAMTS13 proteolytic activity during inflammation. J. Biol. Chem. 2015, 290, 1422–1431. [Google Scholar] [CrossRef]
- Wang, X.; Zhao, J.; Zhang, Y.; Xue, X.; Yin, J.; Liao, L.; Xu, C.; Hou, Y.; Yan, S.; Liu, J. Kinetics of plasma von Willebrand factor in acute myocardial infarction patients: A meta-analysis. Oncotarget 2017, 8, 90371–90379. [Google Scholar] [CrossRef]
- Edvardsen, M.S.; Hindberg, K.; Hansen, E.-S.; Morelli, V.M.; Ueland, T.; Aukrust, P.; Brækkan, S.K.; Evensen, L.H.; Hansen, J.-B. Plasma levels of von Willebrand factor and future risk of incident venous thromboembolism. Blood Adv. 2021, 5, 224–232. [Google Scholar] [CrossRef]
- Han, Y.; Xiao, J.; Falls, E.; Zheng, X.L. A shear-based assay for assessing plasma ADAMTS13 activity and inhibitors in patients with thrombotic thrombocytopenic purpura. Transfusion 2011, 51, 1580–1591. [Google Scholar] [CrossRef]
- Dong, J.-F.; Whitelock, J.; Bernardo, A.; Ball, C.; Cruz, M.A. Variations among normal individuals in the cleavage of endothelial-derived ultra-large von Willebrand factor under flow. J. Thromb. Haemost. 2004, 2, 1460–1466. [Google Scholar] [CrossRef]
- Cao, W.J.; Niiya, M.; Zheng, X.W.; Shang, D.Z.; Zheng, X.L. Inflammatory cytokines inhibit ADAMTS13 synthesis in hepatic stellate cells and endothelial cells. J. Thromb. Haemost. 2008, 6, 1233–1235. [Google Scholar] [CrossRef]
- Tao, Z.; Wang, Y.; Choi, H.; Bernardo, A.; Nishio, K.; Sadler, J.E.; López, J.A.; Dong, J.-F. Cleavage of ultra-large multimers of Von Willebrand factor by C-terminal truncated mutants of ADAMTS-13 under flow. Blood. 2005, 106, 141–143. [Google Scholar] [CrossRef]

| Vehicle Control | ADAMTS-13 | |
|---|---|---|
| Age (weeks) | ||
| Male | 10.6 ± 0.2 | 10.7 ± 0.3 |
| Female | 10.0 ± 0.3 | 10.8 ± 0.4 |
| Body weight (g) | ||
| Male | 25.6 ± 0.3 | 23.6 ± 0.7 |
| Female | 19.9 ± 0.3 | 20.1 ± 0.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, D.; Zhou, Z.; Ma, R.; Wu, H.; Nguyen, T.; Liu, L.; Dong, J. Recombinant ADAMTS-13 Improves Survival of Mice Subjected to Endotoxemia. Int. J. Mol. Sci. 2023, 24, 11782. https://doi.org/10.3390/ijms241411782
Gao D, Zhou Z, Ma R, Wu H, Nguyen T, Liu L, Dong J. Recombinant ADAMTS-13 Improves Survival of Mice Subjected to Endotoxemia. International Journal of Molecular Sciences. 2023; 24(14):11782. https://doi.org/10.3390/ijms241411782
Chicago/Turabian StyleGao, Daniel, Zhou Zhou, Ruidong Ma, Huaizhu Wu, Trung Nguyen, Li Liu, and Jingfei Dong. 2023. "Recombinant ADAMTS-13 Improves Survival of Mice Subjected to Endotoxemia" International Journal of Molecular Sciences 24, no. 14: 11782. https://doi.org/10.3390/ijms241411782
APA StyleGao, D., Zhou, Z., Ma, R., Wu, H., Nguyen, T., Liu, L., & Dong, J. (2023). Recombinant ADAMTS-13 Improves Survival of Mice Subjected to Endotoxemia. International Journal of Molecular Sciences, 24(14), 11782. https://doi.org/10.3390/ijms241411782






