Abstract
The transient receptor potential melastatin 4 (TRPM4) channel is a non-selective cation channel that activates in response to increased intracellular Ca2+ levels but does not allow Ca2+ to pass through directly. It plays a crucial role in regulating diverse cellular functions associated with intracellular Ca2+ homeostasis/dynamics. TRPM4 is widely expressed in the heart and is involved in various physiological and pathological processes therein. Specifically, it has a significant impact on the electrical activity of cardiomyocytes by depolarizing the membrane, presumably via Na+ loading. The TRPM4 channel likely contributes to the development of cardiac arrhythmias associated with specific genetic backgrounds and cardiac remodeling. This short review aims to overview what is known so far about the TRPM4 channel in cardiac electrophysiology and arrhythmogenesis, highlighting its potential as a novel therapeutic target to effectively prevent and treat cardiac arrhythmias.
1. Introduction
The transient receptor potential melastatin 4 (TRPM4) channel is a Ca2+-activated non-selective cationic (NSca) channel, with a unitary conductance of approximately 20pS [1]. The TRPM4 channel protein is ubiquitously expressed in many kinds of cells, where it participates in intracellular Ca2+ homeostasis and modify excitability by influencing the membrane potential. Among the widespread expressed tissues, TRPM4 protein is also abundant in the heart [2]. Several lines of evidence suggest that TRPM4 channels may be involved in arrhythmogenicity in the heart, with both inherited and acquired traits. For example, a gain-of-function mutation (GOF) on its distal N-terminal domain has been reported to produce degenerative changes in the cardiac Purkinje system, and has been identified in a few pedigrees of Jewish and French families that manifest progressive conduction blocks and associated sudden death [3]. In spontaneously hypertensive rats (SHRs), long-term pressure overload produces hypertrophic changes in the heart accompanied by upregulation of TRPM4 channel proteins and their excessive activities [4]. These changes are further associated with the prolongation of QT interval in electrocardiogram, which is a risk factor for lethal arrhythmias. In murine hearts exposed to acute anoxic insults, early afterdepolarization (EAD)-like oscillations in the repolarization phase of action potential (AP) occur, which are selectively inhibited by a TRPM4 channel blocker, 9-phenathrol [5]. All these observations are consistent with the idea that the TRPM4 channel may play non-trivial roles in arrhythmogenesis.
This review succinctly summarizes the characteristic properties of the TRPM4 channel and discusses its implications in cardiac arrhythmogenicity.
2. Biophysical Properties of TRPM4
The TRPM4 channel has a large cytosolic domain. Until 2017, the structure of the TRPM4 channel remained unknown. However, since then, several TRPM4 structures have been resolved in different ligand-bound states using single-particle cryo-electron microscopy (EM). All of these structures were determined for the closed state of the TRPM4 channel, while its open-state conformation is still elusive [6,7,8,9].
Like many other TRPM subfamily members, TRPM4 has an N-terminal TRPM homology region (MHR) domain, a transmembrane domain (TMD) that includes six transmembrane helices, a C-terminal coiled-coil domain, a TRP helix, and a C-terminal domain (CTD). The ion-conducting pore domain is formed by the transmembrane S5 and S6 helices and surrounded by the S1–S4 domain. These two crucial domains are connected through the S4–S5 linker, forming a domain-swapped conformation that may play an important role in the gating of the TRPM4 channel [6]. The S1–S4 domain of the TRPM4 channel contains binding sites for Ca2+ and other ligands [8], as well as a voltage sensor-like domain (VSLD) reminiscent of the counterpart of classical voltage-gated ion channels [10]. However, the VSLD of TRP channels shows a small number of gating charges; in TRPM4, it is only −0.7e [11], which may be mediated by polar residues in and around the putative fourth transmembrane domain. Nonetheless, this charge appears important for the channel’s voltage dependence, though more compelling evidence such as from mutagenesis studies is necessary.
While not primary itself, the membrane depolarization strongly modulates the TRPM4 channel’s activity; hence, the TRPM4 channel shows a prominent dependence on the physiological range of membrane potentials, once activated by an increase in the intracellular Ca2+ level ([Ca2+]i). This is similar to other types of Ca2+-activated channels, such as BKCa [12]. The voltage dependence of the TRPM4 channel is an important feature in cardiac tissues, where it affects the membrane potential over a wide range. Incorporation of this property into simulation models shows that the TRPM4 channel is most prominently activated at the late repolarization phase of action potentials (APs) and when the resting [Ca2+]i is high (in the high submicromolar and micromolar ranges), and is substantially active even near the maximum diastolic potential (MDP) [13]. Therefore, TRPM4 may contribute primarily to the prolongation of APs and, to a lesser extent, to the generation of abnormal diastolic depolarizations that can occur after complete termination of APs. While TRPM4 may not be a major contributor to pace-making potentials, it can still play a role in modulating cardiac excitability and arrhythmogenesis.
The Ca2+ binding sites of the TRPM4 channel are thought to exist within a hydrophilic pocket (Glu828, Gln831, Asn865) of the cytosolic parts of S2 and S3 transmembrane helices. Beneath these binding sites is a very narrow space that allows cytosolic Ca2+ to pass through, between the S2-S3 linker and the TRP domain. One of the only two positively charged amino acid residues of the S4 domain (Arg905) is located just above the S2–S3 linker [6]. This positioning may facilitate coordination and priming effects for voltage-dependent opening. It has also been reported that phosphatidylinositol bisphosphate (PIP2) binding as well as calmodulin interaction are involved in maintaining and enhancing the Ca2+ sensitivity of the TRPM4 channel [14]. Therefore, understanding and evaluating the Ca2+ sensitivity of the TRPM4 channel at physiological or submicromolar Ca2+ levels is very important in elucidating its exact roles in arrhythmogenicity [13].
3. Physiological Roles of TRPM4 in the Heart
- (1)
- Contribution of TRPM4 to sinoatrial (SA) nodal and other cardiac automaticity
In the SA node (SAN), intracellular Ca2+ oscillations generated by the Ca2+ clock play a critical role in regulating cardiac automaticity. During the diastolic depolarization phase, the voltage-dependent Cav1.3 L-type Ca2+ channels (LTCC) activate, then Ca2+ influx into the SAN cell triggers Ca2+ release from the sarcoplasmic reticulum (SR) via the ryanodine receptors (RyR) [15]. A subsequent rise in [Ca2+]i activates the Na+-Ca2+ exchange (NCX), which in turn extrudes Ca2+ from the cell in exchange for Na+. This generates an inward Na+ current that contributes to the depolarization of the membrane potential and increases the rate of pace-making diastolic depolarization (DD) [16].
TRPM4 channels possibly contribute to the regulation of cardiac automaticity by modulating both the Ca2+ clock and membrane clock in the SAN [17]. It has been suggested that the TRPM4 channel may contribute to the inward Na+ current during the DD phase [18]. The TRPM4 channel may also have additional effects on the cardiac automaticity, such as modulating the inward driving force for Ca2+ and [Ca2+]i [19]. It has been reported that inhibition of TRPM4 channels by 9-phenanthrol reduces the heart rate in mice, rats and rabbits, suggesting that the TRPM4 channel may act as an accelerator of DD when the heart rate is decreased, to avoid bradycardia [18,20].
Overall, the TRPM4 channel plays a critical role in regulating cardiac automaticity by modulating the DD slope and [Ca2+]i in the SAN, and its precise contribution to the inward Na+ current and the DD phase is still an ongoing focus of investigation.
- (2)
- Role of TRPM4 channel in the atrial myocardium
The TRPM4 channel has been shown to be involved in atrial electrophysiology [21]. It is expressed in mice, rats, and human atrial cardiomyocytes [21,22,23]. The electrophysiological function of the TRPM4 channel in atrial APs was evaluated in isolated atrial cardiomyocytes by using TRPM4 knockout (Trpm4 KO) mice and a selective inhibitor, 9-phenanthrol. Inhibition of the TRPM4 channel shortened the AP duration of isolated atrial cardiomyocytes compared to those in wild-type (WT), but not knockout animals. The duration of atrial APs was also shorter in Trpm4 KO compared to WT animals [21].
The TRPM4 channel is reported to be responsive to shear stress induced by IP3 receptor-mediated Ca2+ releases in rat atrial cardiomyocytes [23]. TRPM4 has also been implicated in aldosterone-induced atrial arrhythmias [24]. In the same study, disorganization of connexin-43 (Cx43) in atria was observed in Trpm4 KO mice, more than in WT mice. This phenomenon may be involved in the occurrence of atrial electrical disturbances. Additionally, TRPM4 channel may contribute to the growth of human and mice atrial fibroblasts; both expression and functional currents of TRPM4 has been shown to increase under cultured conditions [25]. Presumably, the TRPM4 channel may be engaged in some way commit to the process of atrial fibrosis [25,26].
In summary, the physiological role of TRPM4 in the atrial myocardium appears to be complex and context-dependent, with a variety of consequences observed under different conditions. It may thus be reasonable to speculate a nontrivial role(s) of TRPM4 in the pathogenesis of atrial fibrillation (AF), through alterations of both atrial electrophysiology and remodeling.
- (3)
- Role of TRPM4 channel in the ventricular myocardium and Purkinje conduction system
The physiological role of the TRPM4 channel in the ventricular myocardium remains controversial. Discrepancies in the contribution of the TRPM4 channel between the atrium and ventricle has been reported, following comparisons of both the transcript level and functional current. Although highly detected in the atrium, the TRPM4 channel is much less expressed in the ventricular myocardium [27]. The definitive contribution of the TRPM4 channel to the AP duration of canine ventricular cardiomyocytes has been confirmed in the latest study by using a potent and highly selective inhibitor, 4-chloro-2-[[2-(2-chlorophenoxy) acetyl] amino] benzoic acid (CBA) [28]. In contrast, the Trpm4 mRNA detection and functional Ca2+-activated nonselective cation current were greatly enhanced in the ventricular cardiomyocytes of SHRs compared to those in the Wistar-Kyoto (WKY) rat [4]. The same study observed QT prolongation in SHRs, which is accompanied by an increased TRPM4 channel activity. Furthermore, the TRPM4 channel was involved in the positive inotropic effect of β-adrenergic stimulation in the ventricular myocardium [29].
The network of terminal Purkinje fibers (PFs) carries electrical impulses to the ventricular myocardium, playing a central role in the excitation-contraction cycle of the ventricle. PFs demonstrate a unique electrophysiology with complicated intracellular Ca2+ cycling [30]. The TRPM4 channel is most abundantly expressed in PFs, compared to the other human heart tissues [31], suggesting its significant contribution to the electrical properties of PFs [32]. The propagation failure of PFs caused by TRPM4 channel overexpression has been observed in silico [33]. More intriguingly, optical mapping of ectopic activation induced by mechanical stimulation in PFs demonstrated a clear link with the activation of TRPM4 channels [34]. The involvement of the TRPM4 channel in the electrophysiology of PFs suggests its potential role in cardiac conduction and ventricular arrhythmias.
4. Involvement of TRPM4 in Cardiac Arrhythmias under Pathophysiological Conditions
- (1)
- Pathophysiology of the TRPM4 channel under hypertrophic and remodeling conditions
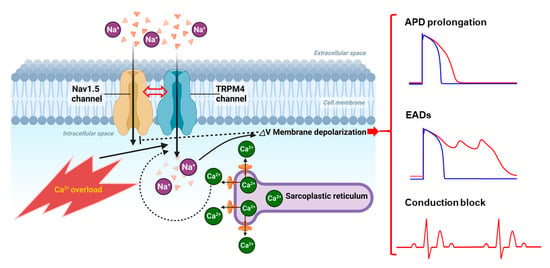
Both Trpm4 mRNA expression and TRPM4-like currents were found to be increased in hypertrophied ventricular cardiomyocytes from SHRs, compared to normotensive WKY rats [4]. These changes were also accompanied by abnormal prolongation of QT intervals. Thus, the authors speculated that, in hypertrophied hearts, overactivation of TRPM4 channels may act as a proarrhythmic substrate for early and delayed depolarizations. Subsequent studies employing genetically engineered TRPM4-transgenic mice and numerical simulations confirmed this possibility [13,35,36,37]. Intriguingly, using the same cardiomyocyte-specific Trpm4 KO mice [29], TRPM4 channels were shown to act differently as either negative or positive regulators for angiotensin II-induced cardiac hypertrophy [29] and pressure overload-induced cardiac hypertrophy [38]. At present, the reason for this discrepancy is unclear and awaits further investigation. It is likely that compromised Ca2+ homeostasis and Ca2+ overload, two prominent features of remodeling and stressed hearts, facilitate TRPM4 overactivation and concurrent arrhythmias (Figure 1). The TRPM4 channel specifically contributes to Ca2+ overload-induced background current that enhances ectopic excitability, and its nonspecific blocker, meclofenamate, significantly suppresses catecholaminergic polymorphic ventricular tachycardia (CPVT)-associated arrhythmias at doses appropriate for TRPM4 channel inhibition [39].
Figure 1.
Ca2+ overloading conditions lead to TRPM4 overactivation inducing pleiotropic electrical abnormalities in cardiomyocytes. Under pathological conditions such as ischemia and heart failure, Ca2+ overload occurs with spontaneous Ca2+ release events [40], leading to the overactivation of TRPM4 channels. This may result in increased Na+ influx through TRPM4 channels particularly during the late phase of AP or even after AP termination, which in turn causes AP prolongation as well as a depolarizing shift of the resting membrane potential. When this is combined with genetic mutations and/or tissue remodeling, both of which could facilitate TRPM4 overactivation, early after-depolarizations (EADs) can be triggered, or reduction of the conduction velocity or conduction block can ensue, due to substantial inactivation of Nav1.5 channels. Moreover, there is evidence for a functional coupling between TRPM4 and Nav1.5 channels [41], which may further complicate the consequences of TRPM4 overactivation. (More details are provided in the text).
Increased expression and activation of the TRPM4 channel could lead to higher susceptibility to hypertrophy- and stress-induced ventricular arrhythmias in association with aberrant Ca2+ homeostasis [42]. TRPM7, albeit much less abundant in the atrium than TRPM4, is significantly upregulated in human atrial myocytes isolated from the patients with atrial fibrillation [43]. Mice subjected to subcutaneous aldosterone infusion and high-salt diet underwent proarrhythmic changes in the atrium, such as enhanced triggered arrhythmias (EAD, DAD) and shortened AP, both of which were eliminated by ablation of the Trpm4 gene. In contrast, complex morphologic changes occurred due to the Trpm4 gene ablation, specifically, dilation of the left atrium and thickening of the septum and ventricular posterior wall. Intriguingly, only the latter two of these changes were abolished by aldosterone and high-salt treatment. The basal heart rate was insensitive to aldosterone and high salt in normal mice, but was responsive to it in the Trpm4 KO mice [24]. Although the mechanisms underlying remain unclear, the above findings strongly favor the vital participation of TRPM4 channels in electrical and remodeling.
- (2)
- Role of TRPM4 in ischemia-reperfusion-related arrhythmias
Reperfusion of an ischemic heart could cause severe additional damage to the myocardium and induce lethal arrhythmias [44]. Excessive production of reactive oxygen species (ROS) and intracellular Ca2+ overload during ischemia-reperfusion play crucial roles in the genesis of both tissue injury and arrhythmias [45]. It has been reported that in the Langendorff ischemia-reperfusion model of rat hearts pretreated with the TRPM4 channel blocker 9-phenanthrol significantly improved contractile function and limited the infarcted area [46]. Furthermore, TRPM4 channel inhibition and silencing greatly suppressed ROS-induced injury on H9C2 cardiomyocytes [47]. The destructive contribution of TRPM4 to ROS-induced cardiac injury is potentially linked to the reduction of mitochondrial membrane potential and intracellular ATP level [48]. During ischemia-reperfusion, the electrical disturbances from PFs, where the TRPM4 channel is most abundantly and functionally expressed [32], account for the occurrence of ventricular arrhythmias [49]. The first report on the anti-arrhythmic effect of the TRPM4 channel-selective blocker 9-phenanthrol was from the treatment of arrhythmias induced by hypoxia and re-oxygenation in murine ventricles: perfusion with 9-phenanthrol demonstrated a spectacular dose-dependent abolishment of EADs [5]. Interestingly, an in vivo study of a mouse model, where acute ischemia was induced by ligation of the left anterior descending (LAD) coronary artery for 30 min, showed that Trpm4 KO mice are much less likely to develop ischemia-induced arrhythmias. In contrast, no significant difference in arrhythmic responses between Trpm4 KO mice and WT mice was observed after effective reperfusion [39].
5. TRPM4 Channelopathy in Inherited Cardiac Arrhythmias
Inherited cardiac arrhythmias are a group of genetic disorders that affect the electrical activity of the heart, to cause abnormal heart rhythms and potentially life-threatening arrhythmias. These disorders could be caused by mutations in the genes encoding ion channels that are responsible for controlling the flow of ions across the cell membrane and maintaining the normal rhythm of the heart [50]. Different kinds of inherited cardiac arrhythmias, including conduction blocks, Brugada syndrome (BrS), and long QT syndrome (LQTS), have been linked to dozens of Trpm4 gene mutations, as evidenced by genetic linkage analyses and subsequent cohort studies (Table 1) [2,51,52]. It was often found that the same genotype variant of TRPM4 produces multiple phenotypes of arrhythmias while its multiple genotype mutations cause an arrhythmia with similar clinical features. The exact mechanism(s) underlying this redundancy is not yet fully understood.
- (1)
- TRPM4 variants in cardiac conduction block
The TRPM4-p.E7K mutant was the first to be identified as a point mutation of the TRPM4 channel in a few pedigrees of patient families that manifest progressive familial conduction block type I (PFHB I) [31]. Due to impaired deregulation of the small ubiquitin modifier conjunction (SUMOylation), the TRPM4-p.E7K mutant exhibited a GOF effect, associated with greater current density and increased protein expression at the plasma membrane [31]. It has also been reported that enhanced PIP2 affinity and altered channel kinetics can facilitate its activation, especially around the resting membrane potential, presumably contributive to brady-arrhythmogenicity [53,54]. Several other GOF mutations of the TRM4 channel (p.R164W, p.A432T, and p.G844D) have been discovered in patient families suffering from heart block, which also involves with the same mechanism of reduced SUMOylation [3]. In contrast, electrophysiological kinetic analysis of the TRPM4-p.A432T mutant suggested that a four-fold slower deactivation, rather than excessive cell surface expression, accounted for the augmented membrane current [64]. Using a combination of electrophysiology, rapid treatments of intracellular Ca2+ with UV-flash photolysis, and molecular docking analysis, this research group further investigated another GOF mutant, TRPM4-p.K914R, identified from two patients with heart disease in the same family [63]. TRPM4-p.K914R demonstrated slower activation and deactivation kinetics leading to increased membrane currents. Furthermore, the 914th lysine residue was crucial as the nanoscopic interface between the S4-S5 linker, the MHR, and TRP-domain, which determines TRPM4’s functional behavior [63].
The majority of TRPM4 variations related to familial conduction block are, thus far, GOF phenotypes. However, several loss-of-function (LOF) mutations of TRPM4 are also identified in inherited cardiac conduction defects [57,60]. The mechanism underlying such complex genotype-to-phenotype relationships is unclear. For instance, a LOF mutation, TRPM4-p.T286T, was found in patients with ventricular noncompaction and cardiac conduction disease, which eventually requires implantation of a permanent pacemaker [60]. This study revealed that inhibition of TRPM4 channel activity by its selective blocker 9-phenanthrol in human induced pluripotent stem cell–derived cardiomyocytes (hiPSC-CMs) resulted in decreased mRNA levels of HEY2, TBX5, and NKX2-5, transcription factors that play important roles in postnatal conduction system maturation [60,65]. This result is consistent with that of a gene invalidation study: Trpm4 KO mice displayed Luciani–Wenckebach atrioventricular blocks [66]. Taken together, the above lines of evidence support the view that downregulated function of the TRPM4 channel in immature hearts could influence the development of the conduction system and myocardial structures.
- (2)
- TRPM4 variants in BrS
BrS is an inherited cardiac disease associated with a significant risk of lethal arrhythmias that lead to sudden death [67]. About 25% of BrS patients have the LOF mutations in the SCN5A gene that encode the α-subunit of the cardiac voltage-dependent sodium channel (Nav1.5) [68]. Among the other genes, TRPM4 variants explain 2.7% to 6% of total BrS cases [52,62]. However, the exact pathogenic mechanism by which both LOF and GOF mutations of TRPM4 can lead to BrS remain elusive [52].
By systematically analyzing the genotype-to-phenotype relationship of TRPM4 mutation for BrS, new evidence was found of LOF mutations of TRPM4, especially in a heterozygous status, that may not be sufficient to generate BrS [62]. However, an important physical interaction between TRPM4 and Nav1.5 was revealed: a significant decrease in the Nav1.5 current was observed in cardiomyocytes from Trpm4 KO mice [41]. Further studies are needed to understand how such interactions modulate cardiac electrical activity and the significance of the interactions in the pathogenesis of BrS.
- (3)
- TRPM4 variants in LQTS
LQTS is a congenital and arrhythmogenic ion channel disorder characterized by QT prolongation in the electrocardiogram (ECG) [69]. It is potentially life-threatening because of delayed ventricular repolarization. Mutations in three major LQTS genes (KCNQ1, KCNH2, and SCN5A) were shown to impair the AP repolarization and contribute to approximately 75% of the disorder [70]. TRPM4 variants were also found to be involved in approximately 2% of LQTS cases [51], and two of these variants, p.R499W and p.V441M, were shown to display smaller TRPM4-mediated currents compared to those in wild type [51]. There is however a caveat against simply interpreting this result as the direct cause for abnormal delayed AP repolarization. It is suggested that the role of TRPM4 variants on QT interval might be multifactorial [51], as they may modulate other membrane currents as well. It is also possible that the impact of TRPM4 mutations may only become apparent in concert with the dysfunction of other AP formation channels such as KCNQ1, KCNJ2, and CACNA1C. These channels are known to alter the QT interval via a more complex mechanism than directly affecting the AP duration. For instance, a heterozygous KCNQ1/TRPM4 dual mutation has been found in a LQTS patient, in whom verapamil treatment successfully reduced defibrillator discharge frequency by shortening the QT interval [71]. However, the underlying mechanism in the contribution of TRPM4 variants to LQTS still remains unclear.
6. Conclusions and Perspective
TRPM4 has recently emerged as a new factor in cardiac arrhythmogenesis of both acquired and inherited types. More than thirty single mutations in the TRPM4 gene are now connected to risky arrhythmic manifestations, and functional upregulation/dysregulation of TRPM4 channels with ECG abnormalities is reported to be involved in pathological cardiac remodeling (in heart failure and other hypertrophic cardiomyopathies). To fully understand such multiplicity and complexity and to develop effective therapeutic interventions against them, mechanistically focused studies, that delve deeper than studies of genotype-phenotype associations, are needed. In this regard, there are several challenging but promising directions. For example, transgenic animal models can be more avidly combined with optogenetic approaches to deepen our tissue-level knowledge, in vivo or ex vivo [72,73]. The single nuclei RNA sequencing can be utilized to acquire more direct information about the geometrical heterogeneity of TRPM4 and the other arrhythmic substrates across the whole heart tissue [74], in which, appropriate heterocellular cardiac organoid models could be fabricated to disentangle the tissue-level complexity in more depth [75]. Continuous monitoring of genetically at-risk individuals, using wearable detection devices, may facilitate the uncovering of otherwise unknown triggers for TRPM4-associated arrhythmias [76]. Atomic-level structural analysis will also increase detailed knowledge of processes involved in the altered gating of the TRPM4 channel which predisposes individuals to arrhythmias [77]. All these lines of quantitative information could be integrated into multi-scale, multi-hierarchical numerical models to simulate the 2- or 3-dimensional propagation of excitation waves and their disturbances (reentries, blocks) in a more precise fashion, ultimately providing a useful tool for risk evaluation and in silico design of treatments.
The pathophysiological impact of TRPM4 dysfunction is further complicated by its tight link with [Ca2+]i dynamics and possible modification of the other types of cardiac ion channels. Although the primary consequence of TRPM4 channel activation is presumed to prolong AP duration or QT intervals, it is also known that genetic deletion of this channel induces pleiotropic changes in the ECG [66]. In this respect, the latest finding that TRPM4 interacts with Nav1.5 [41] might offer an additional clue to deciphering why a single mutation of the TRPM4 gene results in multiple phenotypes and vice versa, as observed in LQTS and BrS.
In preclinical studies using transgenic mice, a number of selective TRPM4 blockers have been shown to suppress arrhythmias [5,13,39,78], suggesting that targeting this channel may serve as a new therapeutic strategy. In most investigations, however, only low concentrations of 9-phenanthrol inhibited TRPM4 channels relatively selectively. Intriguingly, recent investigations identified two promising aryloxyacyl-anthranilic acid compounds, NBA and CBA, as novel TRPM4 antagonists. In particular, CBA exhibited a greater potency than 9-phenanthrol in inhibiting human TRPM4; however, had no effect on its mouse homologue [79]. These unique features may serve as a good starting point to design a new generation of TRPM4 blockers with better pharmacological profiles.
In future studies, advancements in gene editing technologies like CRISPR-Cas9 may enable direct modification of the TRPM4 gene in cells, tissues or organs. Gene editing could be utilized to correct deleterious mutations associated with TRPM4-related arrhythmias or to prevent the overactivation of TRPM4 channels in cardiac tissues undergoing pathological remodeling, which would otherwise increase the arrhythmogenicity.
Obviously, further detailed investigations about TRPM4 physiology and pathophysiology are needed to substantiate the utility of the above-mentioned therapeutic means and elucidate their true clinical benefits for arrhythmia treatments.
Author Contributions
Conceptualization, Y.H. and R.I.; Software, Y.H., J.C. and K.H.; Validation, Y.H. and R.I.; Writing—Original Draft Preparation, Y.H. and R.I.; Writing—Review & Editing, Y.H., T.F. and R.I.; Visualization, Y.H. and J.C.; Project Administration, Y.H. and R.I.; Funding Acquisition, Y.H. and R.I. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by JSPS grants-in-aid to R.I. (No. 20K07269) and Y.H. (No. 20K16126), and by funding from Fukuoka University to Y.H. (No. GW2312).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The research data described in this paper are available on request.
Acknowledgments
Part of Figure 1 was created with BioRender.com.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Launay, P.; Fleig, A.; Perraud, A.-L.; Scharenberg, A.M.; Penner, R.; Kinet, J.-P. TRPM4 is a Ca2+-activated nonselective cation channel mediating cell membrane depolarization. Cell 2002, 109, 397–407. [Google Scholar] [PubMed]
- Guinamard, R.; Bouvagnet, P.; Hof, T.; Liu, H.; Simard, C.; Sallé, L. TRPM4 in cardiac electrical activity. Cardiovasc. Res. 2015, 108, 21–30. [Google Scholar]
- Liu, H.; El Zein, L.; Kruse, M.; Guinamard, R.; Beckmann, A.; Bozio, A.; Kurtbay, G.; Mégarbané, A.; Ohmert, I.; Blaysat, G. Gain-of-function mutations in TRPM4 cause autosomal dominant isolated cardiac conduction disease. Circ. Cardiovasc. Genet. 2010, 3, 374–385. [Google Scholar] [PubMed]
- Guinamard, R.; Demion, M.; Magaud, C.; Potreau, D.; Bois, P. Functional expression of the TRPM4 cationic current in ventricular cardiomyocytes from spontaneously hypertensive rats. Hypertension 2006, 48, 587–594. [Google Scholar] [CrossRef]
- Simard, C.; Sallé, L.; Rouet, R.; Guinamard, R. Transient receptor potential melastatin 4 inhibitor 9-phenanthrol abolishes arrhythmias induced by hypoxia and re-oxygenation in mouse ventricle. Br. J. Pharmacol. 2012, 165, 2354–2364. [Google Scholar]
- Autzen, H.E.; Myasnikov, A.G.; Campbell, M.G.; Asarnow, D.; Julius, D.; Cheng, Y. Structure of the human TRPM4 ion channel in a lipid nanodisc. Science 2018, 359, 228–232. [Google Scholar]
- Duan, J.; Li, Z.; Li, J.; Santa-Cruz, A.; Sanchez-Martinez, S.; Zhang, J.; Clapham, D.E. Structure of full-length human TRPM4. Proc. Natl. Acad. Sci. USA 2018, 115, 2377–2382. [Google Scholar] [PubMed]
- Guo, J.; She, J.; Zeng, W.; Chen, Q.; Bai, X.-C.; Jiang, Y. Structures of the calcium-activated, non-selective cation channel TRPM4. Nature 2017, 552, 205–209. [Google Scholar]
- Winkler, P.A.; Huang, Y.; Sun, W.; Du, J.; Lü, W. Electron cryo-microscopy structure of a human TRPM4 channel. Nature 2017, 552, 200–204. [Google Scholar]
- Zhao, Y.; McVeigh, B.M.; Moiseenkova-Bell, V.Y. Structural pharmacology of TRP channels. J. Mol. Biol. 2021, 433, 166914. [Google Scholar]
- Nilius, B.; Prenen, J.; Droogmans, G.; Voets, T.; Vennekens, R.; Freichel, M.; Wissenbach, U.; Flockerzi, V. Voltage dependence of the Ca2+-activated cation channel TRPM4. J. Biol. Chem. 2003, 278, 30813–30820. [Google Scholar]
- Lee, U.S.; Cui, J. BK channel activation: Structural and functional insights. Trends Neurosci. 2010, 33, 415–423. [Google Scholar] [PubMed]
- Hu, Y.; Duan, Y.; Takeuchi, A.; Hai-Kurahara, L.; Ichikawa, J.; Hiraishi, K.; Numata, T.; Ohara, H.; Iribe, G.; Nakaya, M. Uncovering the arrhythmogenic potential of TRPM4 activation in atrial-derived HL-1 cells using novel recording and numerical approaches. Cardiovasc. Res. 2017, 113, 1243–1255. [Google Scholar] [PubMed]
- Nilius, B.; Prenen, J.; Tang, J.; Wang, C.; Owsianik, G.; Janssens, A.; Voets, T.; Zhu, M.X. Regulation of the Ca2+ sensitivity of the nonselective cation channel TRPM4. J. Biol. Chem. 2005, 280, 6423–6433. [Google Scholar] [PubMed]
- Torrente, A.G.; Mesirca, P.; Neco, P.; Rizzetto, R.; Dubel, S.; Barrere, C.; Sinegger-Brauns, M.; Striessnig, J.; Richard, S.; Nargeot, J. L-type Cav1. 3 channels regulate ryanodine receptor-dependent Ca2+ release during sino-atrial node pacemaker activity. Cardiovasc. Res. 2016, 109, 451–461. [Google Scholar] [PubMed]
- Capel, R.A.; Terrar, D.A. The importance of Ca2+-dependent mechanisms for the initiation of the heartbeat. Front. Physiol. 2015, 6, 80. [Google Scholar]
- Lakatta, E.G.; Maltsev, V.A.; Vinogradova, T.M. A coupled SYSTEM of intracellular Ca2+ clocks and surface membrane voltage clocks controls the timekeeping mechanism of the heart’s pacemaker. Circ. Res. 2010, 106, 659–673. [Google Scholar]
- Hof, T.; Simard, C.; Rouet, R.; Sallé, L.; Guinamard, R. Implication of the TRPM4 nonselective cation channel in mammalian sinus rhythm. Heart Rhythm 2013, 10, 1683–1689. [Google Scholar] [CrossRef]
- Abriel, H.; Syam, N.; Sottas, V.; Amarouch, M.Y.; Rougier, J.-S. TRPM4 channels in the cardiovascular system: Physiology, pathophysiology, and pharmacology. Biochem. Pharmacol. 2012, 84, 873–881. [Google Scholar]
- Demion, M.; Bois, P.; Launay, P.; Guinamard, R. TRPM4, a Ca2+-activated nonselective cation channel in mouse sino-atrial node cells. Cardiovasc. Res. 2007, 73, 531–538. [Google Scholar] [CrossRef]
- Simard, C.; Hof, T.; Keddache, Z.; Launay, P.; Guinamard, R. The TRPM4 non-selective cation channel contributes to the mammalian atrial action potential. J. Mol. Cell. Cardiol. 2013, 59, 11–19. [Google Scholar] [PubMed]
- Guinamard, R.; Chatelier, A.; Demion, M.; Potreau, D.; Patri, S.; Rahmati, M.; Bois, P. Functional characterization of a Ca2+-activated non-selective cation channel in human atrial cardiomyocytes. J. Physiol. 2004, 558, 75–83. [Google Scholar] [PubMed]
- Son, M.J.; Kim, J.C.; Kim, S.W.; Chidipi, B.; Muniyandi, J.; Singh, T.D.; So, I.; Subedi, K.P.; Woo, S.H. Shear stress activates monovalent cation channel transient receptor potential melastatin subfamily 4 in rat atrial myocytes via type 2 inositol 1, 4, 5-trisphosphate receptors and Ca2+ release. J. Physiol. 2016, 594, 2985–3004. [Google Scholar]
- Simard, C.; Ferchaud, V.; Sallé, L.; Milliez, P.; Manrique, A.; Alexandre, J.; Guinamard, R. TRPM4 participates in aldosterone-salt-induced electrical atrial remodeling in mice. Cells 2021, 10, 636. [Google Scholar] [CrossRef]
- Simard, C.; Magaud, C.; Adjlane, R.; Dupas, Q.; Sallé, L.; Manrique, A.; Bois, P.; Faivre, J.-F.; Guinamard, R. TRPM4 non-selective cation channel in human atrial fibroblast growth. Pflügers Arch. -Eur. J. Physiol. 2020, 472, 1719–1732. [Google Scholar]
- Dienes, C.; Kovács, Z.M.; Hézső, T.; Almássy, J.; Magyar, J.; Bányász, T.; Nánási, P.P.; Horváth, B.; Szentandrássy, N. Pharmacological Modulation and (Patho) Physiological Roles of TRPM4 Channel—Part 2: TRPM4 in Health and Disease. Pharmaceuticals 2022, 15, 40. [Google Scholar]
- Guinamard, R.; Demion, M.; Chatelier, A.; Bois, P. Calcium-activated nonselective cation channels in mammalian cardiomyocytes. Trends Cardiovasc. Med. 2006, 16, 245–250. [Google Scholar] [CrossRef]
- Dienes, C.; Hézső, T.; Kiss, D.Z.; Baranyai, D.; Kovács, Z.M.; Szabó, L.; Magyar, J.; Bányász, T.; Nánási, P.P.; Horváth, B. Electrophysiological Effects of the Transient Receptor Potential Melastatin 4 Channel Inhibitor (4-Chloro-2-(2-chlorophenoxy) acetamido) Benzoic Acid (CBA) in Canine Left Ventricular Cardiomyocytes. Int. J. Mol. Sci. 2021, 22, 9499. [Google Scholar] [CrossRef]
- Kecskés, M.; Jacobs, G.; Kerselaers, S.; Syam, N.; Menigoz, A.; Vangheluwe, P.; Freichel, M.; Flockerzi, V.; Voets, T.; Vennekens, R. The Ca 2+-activated cation channel TRPM4 is a negative regulator of angiotensin II-induced cardiac hypertrophy. Basic Res. Cardiol. 2015, 110, 43. [Google Scholar] [CrossRef]
- Haissaguerre, M.; Vigmond, E.; Stuyvers, B.; Hocini, M.; Bernus, O. Ventricular arrhythmias and the His–Purkinje system. Nat. Rev. Cardiol. 2016, 13, 155–166. [Google Scholar]
- Kruse, M.; Schulze-Bahr, E.; Corfield, V.; Beckmann, A.; Stallmeyer, B.; Kurtbay, G.; Ohmert, I.; Schulze-Bahr, E.; Brink, P.; Pongs, O. Impaired endocytosis of the ion channel TRPM4 is associated with human progressive familial heart block type I. J. Clin. Investig. 2009, 119, 2737–2744. [Google Scholar] [CrossRef]
- Hof, T.; Sallé, L.; Coulbault, L.; Richer, R.; Alexandre, J.; Rouet, R.; Manrique, A.; Guinamard, R. TRPM4 non-selective cation channels influence action potentials in rabbit Purkinje fibres. J. Physiol. 2016, 594, 295–306. [Google Scholar] [CrossRef]
- Gaur, N.; Hof, T.; Haissaguerre, M.; Vigmond, E.J. Propagation failure by TRPM4 overexpression. Biophys. J. 2019, 116, 469–476. [Google Scholar] [CrossRef]
- Hurley, M.; Kaur, S.; Walton, R.; Power, A.; Haïssaguerre, M.; Bernus, O.; Ward, M.-L.; White, E. Endocardial role in arrhythmias induced by acute ventricular stretch and the involvement of Purkinje fibres, in isolated rat hearts. Curr. Res. Physiol. 2023, 6, 100098. [Google Scholar] [CrossRef] [PubMed]
- Hedon, C.; Lambert, K.; Chakouri, N.; Thireau, J.; Aimond, F.; Cassan, C.; Bideaux, P.; Richard, S.; Faucherre, A.; Le Guennec, J.-Y. New role of TRPM4 channel in the cardiac excitation-contraction coupling in response to physiological and pathological hypertrophy in mouse. Prog. Biophys. Mol. Biol. 2021, 159, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Kaschitza, D.R.; Essers, M.; Arullampalam, P.; Fujita, T.; Abriel, H.; Inoue, R. Pathological activation of CaMKII induces arrhythmogenicity through TRPM4 overactivation. Pflügers Arch.-Eur. J. Physiol. 2021, 473, 507–519. [Google Scholar] [CrossRef] [PubMed]
- Pironet, A.; Syam, N.; Vandewiele, F.; Van den Haute, C.; Kerselaers, S.; Pinto, S.; Vande Velde, G.; Gijsbers, R.; Vennekens, R. AAV9-mediated overexpression of TRPM4 increases the incidence of stress-induced ventricular arrhythmias in mice. Front. Physiol. 2019, 10, 802. [Google Scholar] [CrossRef]
- Guo, Y.; Yu, Z.-Y.; Wu, J.; Gong, H.; Kesteven, S.; Iismaa, S.E.; Chan, A.Y.; Holman, S.; Pinto, S.; Pironet, A. The Ca2+-activated cation channel TRPM4 is a positive regulator of pressure overload-induced cardiac hypertrophy. eLife 2021, 10, e66582. [Google Scholar] [CrossRef]
- Vandewiele, F.; Pironet, A.; Jacobs, G.; Kecskés, M.; Wegener, J.; Kerselaers, S.; Hendrikx, L.; Verelst, J.; Philippaert, K.; Oosterlinck, W. TRPM4 inhibition by meclofenamate suppresses Ca2+-dependent triggered arrhythmias. Eur. Heart J. 2022, 43, 4195–4207. [Google Scholar] [CrossRef] [PubMed]
- Györke, S.; Carnes, C. Dysregulated sarcoplasmic reticulum calcium release: Potential pharmacological target in cardiac disease. Pharmacol. Ther. 2008, 119, 340–354. [Google Scholar] [CrossRef]
- Ozhathil, L.C.; Rougier, J.-S.; Arullampalam, P.; Essers, M.C.; Ross-Kaschitza, D.; Abriel, H. Deletion of Trpm4 alters the function of the Nav1. 5 channel in murine cardiac myocytes. Int. J. Mol. Sci. 2021, 22, 3401. [Google Scholar] [CrossRef]
- Robson, A. A nonsteroidal anti-inflammatory drug suppresses Ca2+-dependent triggered arrhythmias. Nat. Cardiovasc. Res. 2022, 1, 697. [Google Scholar] [CrossRef]
- Zhang, Y.-H.; Sun, H.-Y.; Chen, K.-H.; Du, X.-L.; Liu, B.; Cheng, L.-C.; Li, X.; Jin, M.-W.; Li, G.-R. Evidence for functional expression of TRPM7 channels in human atrial myocytes. Basic Res. Cardiol. 2012, 107, 282. [Google Scholar] [CrossRef] [PubMed]
- Neri, M.; Riezzo, I.; Pascale, N.; Pomara, C.; Turillazzi, E. Ischemia/reperfusion injury following acute myocardial infarction: A critical issue for clinicians and forensic pathologists. Mediat. Inflamm. 2017, 2017, 7018393. [Google Scholar] [CrossRef]
- Perrelli, M.-G.; Pagliaro, P.; Penna, C. Ischemia/reperfusion injury and cardioprotective mechanisms: Role of mitochondria and reactive oxygen species. World J. Cardiol. 2011, 3, 186. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Takahashi, K.; Piao, H.; Qu, P.; Naruse, K. 9-Phenanthrol, a TRPM4 inhibitor, protects isolated rat hearts from ischemia–reperfusion injury. PLoS ONE 2013, 8, e70587. [Google Scholar] [CrossRef]
- Piao, H.; Takahashi, K.; Yamaguchi, Y.; Wang, C.; Liu, K.; Naruse, K. Transient receptor potential melastatin-4 is involved in hypoxia-reoxygenation injury in the cardiomyocytes. PLoS ONE 2015, 10, e0121703. [Google Scholar] [CrossRef]
- Wang, C.; Chen, J.; Wang, M.; Naruse, K.; Takahashi, K. Role of the TRPM4 channel in mitochondrial function, calcium release, and ROS generation in oxidative stress. Biochem. Biophys. Res. Commun. 2021, 566, 190–196. [Google Scholar] [CrossRef]
- Ideker, R.E.; Kong, W.; Pogwizd, S. Purkinje fibers and arrhythmias. Pacing Clin. Electrophysiol. PACE 2009, 32, 283. [Google Scholar] [CrossRef]
- Schwartz, P.J.; Ackerman, M.J.; Antzelevitch, C.; Bezzina, C.R.; Borggrefe, M.; Cuneo, B.F.; Wilde, A.A. Inherited cardiac arrhythmias. Nat. Rev. Dis. Primers 2020, 6, 58. [Google Scholar] [CrossRef] [PubMed]
- Hof, T.; Liu, H.; Sallé, L.; Schott, J.-J.; Ducreux, C.; Millat, G.; Chevalier, P.; Probst, V.; Guinamard, R.; Bouvagnet, P. TRPM4 non-selective cation channel variants in long QT syndrome. BMC Med. Genet. 2017, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Chatel, S.; Simard, C.; Syam, N.; Salle, L.; Probst, V.; Morel, J.; Millat, G.; Lopez, M.; Abriel, H. Molecular genetics and functional anomalies in a series of 248 Brugada cases with 11 mutations in the TRPM4 channel. PLoS ONE 2013, 8, e54131. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Li, Q.; Kurahara, L.-H.; Shioi, N.; Hiraishi, K.; Fujita, T.; Zhu, X.; Inoue, R. An Arrhythmic mutation E7K facilitates TRPM4 channel activation via enhanced PIP2 interaction. Cells 2021, 10, 983. [Google Scholar] [CrossRef]
- Hu, Y.; Li, Q.; Shen, Y.; Fujita, T.; Zhu, X.; Inoue, R. Theoretical Investigation of the Mechanism by which A Gain-of-Function Mutation of the TRPM4 Channel Causes Conduction Block. Int. J. Mol. Sci. 2021, 22, 8513. [Google Scholar] [CrossRef]
- Syam, N.; Chatel, S.; Ozhathil, L.C.; Sottas, V.; Rougier, J.S.; Baruteau, A.; Baron, E.; Amarouch, M.Y.; Daumy, X.; Probst, V. Variants of transient receptor potential melastatin member 4 in childhood atrioventricular block. J. Am. Heart Assoc. 2016, 5, e001625. [Google Scholar] [CrossRef]
- Subbotina, E.; Williams, N.; Sampson, B.A.; Tang, Y.; Coetzee, W.A. Functional characterization of TRPM4 variants identified in sudden unexpected natural death. Forensic Sci. Int. 2018, 293, 37–46. [Google Scholar] [CrossRef]
- Bianchi, B.; Ozhathil, L.C.; Medeiros-Domingo, A.; Gollob, M.H.; Abriel, H. Four TRPM4 cation channel mutations found in cardiac conduction diseases lead to altered protein stability. Front. Physiol. 2018, 9, 177. [Google Scholar] [CrossRef]
- Stallmeyer, B.; Zumhagen, S.; Denjoy, I.; Duthoit, G.; Hébert, J.L.; Ferrer, X.; Maugenre, S.; Schmitz, W.; Kirchhefer, U.; Schulze-Bahr, E. Mutational spectrum in the Ca2+-activated cation channel gene TRPM4 in patients with cardiac conductance disturbances. Hum. Mutat. 2012, 33, 109–117. [Google Scholar] [CrossRef]
- Zhao, Y.; Feng, M.; Shang, L.-X.; Sun, H.-x.; Zhou, X.-H.; Lu, Y.-M.; Zhang, L.; Xing, Q.; Li, Y.-d.; Tang, B.-P. KCNQ1 G219E and TRPM4 T160M polymorphisms are involved in the pathogenesis of long QT syndrome: A case report. Medicine 2021, 100, e24032. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Nakamura, K.; Nishi, N.; Igawa, O.; Yoshida, M.; Miyoshi, T.; Watanabe, A.; Morita, H.; Ito, H. TRPM4 mutation in patients with ventricular noncompaction and cardiac conduction disease. Circ. Genom. Precis. Med. 2018, 11, e002103. [Google Scholar] [CrossRef] [PubMed]
- Daumy, X.; Amarouch, M.-Y.; Lindenbaum, P.; Bonnaud, S.; Charpentier, E.; Bianchi, B.; Nafzger, S.; Baron, E.; Fouchard, S.; Thollet, A. Targeted resequencing identifies TRPM4 as a major gene predisposing to progressive familial heart block type I. Int. J. Cardiol. 2016, 207, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Janin, A.; Bessière, F.; Georgescu, T.; Chanavat, V.; Chevalier, P.; Millat, G. TRPM4 mutations to cause autosomal recessive and not autosomal dominant Brugada type 1 syndrome. Eur. J. Med. Genet. 2019, 62, 103527. [Google Scholar] [CrossRef] [PubMed]
- Xian, W.; Wang, H.; Moretti, A.; Laugwitz, K.-L.; Flockerzi, V.; Lipp, P. Domain zipping and unzipping modulates TRPM4’s properties in human cardiac conduction disease. Biophys. J. 2020, 118, 21a–22a. [Google Scholar] [CrossRef]
- Xian, W.; Hui, X.; Tian, Q.; Wang, H.; Moretti, A.; Laugwitz, K.-L.; Flockerzi, V.; Ruppenthal, S.; Lipp, P. Aberrant deactivation-induced gain of function in TRPM4 mutant is associated with human cardiac conduction block. Cell Rep. 2018, 24, 724–731. [Google Scholar] [CrossRef]
- Asatryan, B.; Medeiros-Domingo, A. Molecular and genetic insights into progressive cardiac conduction disease. EP Eur. 2019, 21, 1145–1158. [Google Scholar] [CrossRef]
- Demion, M.; Thireau, J.; Gueffier, M.; Finan, A.; Khoueiry, Z.; Cassan, C.; Serafini, N.; Aimond, F.; Granier, M.; Pasquié, J.-L. Trpm4 gene invalidation leads to cardiac hypertrophy and electrophysiological alterations. PLoS ONE 2014, 9, e115256. [Google Scholar] [CrossRef]
- Brugada, P.; Brugada, J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome: A multicenter report. J. Am. Coll. Cardiol. 1992, 20, 1391–1396. [Google Scholar] [CrossRef]
- Veerman, C.C.; Wilde, A.A.; Lodder, E.M. The cardiac sodium channel gene SCN5A and its gene product NaV1. 5: Role in physiology and pathophysiology. Gene 2015, 573, 177–187. [Google Scholar] [CrossRef]
- Mizusawa, Y.; Horie, M.; Wilde, A.A. Genetic and clinical advances in congenital long QT syndrome. Circ. J. 2014, 78, 2827–2833. [Google Scholar] [CrossRef]
- Tester, D.J.; Ackerman, M.J. Genetics of long QT syndrome. Methodist DeBakey Cardiovasc. J. 2014, 10, 29. [Google Scholar] [CrossRef]
- Wang, F.; Han, Y.; Sang, W.; Wang, L.; Liang, X.; Wang, L.; Xing, Q.; Guo, Y.; Zhang, J.; Zhang, L. In Vitro Drug Screening Using iPSC-Derived Cardiomyocytes of a Long QT-Syndrome Patient Carrying KCNQ1 & TRPM4 Dual Mutation: An Experimental Personalized Treatment. Cells 2022, 11, 2495. [Google Scholar] [PubMed]
- Bruegmann, T.; Smith, G.L.; Lehnart, S.E. Cardiac optogenetics: Using light to observe and excite the heart. Front. Physiol. 2022, 13, 1031062. [Google Scholar] [CrossRef] [PubMed]
- Entcheva, E.; Kay, M.W. Cardiac optogenetics: A decade of enlightenment. Nat. Rev. Cardiol. 2021, 18, 349–367. [Google Scholar] [CrossRef] [PubMed]
- Tucker, N.R.; Chaffin, M.; Fleming, S.J.; Hall, A.W.; Parsons, V.A.; Bedi Jr, K.C.; Akkad, A.-D.; Herndon, C.N.; Arduini, A.; Papangeli, I. Transcriptional and cellular diversity of the human heart. Circulation 2020, 142, 466–482. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Lei, W.; Hu, S. Cardiac organoid—A promising perspective of preclinical model. Stem Cell Res. Ther. 2021, 12, 272. [Google Scholar] [CrossRef] [PubMed]
- Hughes, A.; Shandhi, M.M.H.; Master, H.; Dunn, J.; Brittain, E. Wearable devices in cardiovascular medicine. Circ. Res. 2023, 132, 652–670. [Google Scholar] [CrossRef]
- Jiang, D.; Zhang, J.; Xia, Z. Structural Advances in Voltage-Gated Sodium Channels. Front. Pharmacol. 2022, 13, 908867. [Google Scholar] [CrossRef]
- Guinamard, R.; Hof, T.; Del Negro, C. The TRPM 4 channel inhibitor 9-phenanthrol. Br. J. Pharmacol. 2014, 171, 1600–1613. [Google Scholar] [CrossRef]
- Arullampalam, P.; Preti, B.; Ross-Kaschitza, D.; Lochner, M.; Rougier, J.-S.; Abriel, H. Species-specific effects of cation channel TRPM4 small-molecule inhibitors. Front. Pharmacol. 2021, 12, 712354. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).