Polydeoxyribonucleotide and Shock Wave Therapy Sequence Efficacy in Regenerating Immobilized Rabbit Calf Muscles
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Animal Models
4.2. Immobilization by Cast
4.3. Injection
4.4. ESWT
4.5. Clinical Procedure
4.6. Tissue Preparation
4.7. Immunohistochemical Analysis
4.8. Tissue Western Blot
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fujino, H.; Kohzuki, H.; Takeda, I.; Kiyooka, T.; Miyasaka, T.; Mohri, S.; Shimizu, J.; Kajiya, F. Regression of capillary network in atrophied soleus muscle induced by hindlimb unweighting. J. Appl. Physiol. 2005, 98, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Dirks, M.L.; Wall, B.T.; Snijders, T.; Ottenbros, C.L.; Verdijk, L.B.; van Loon, L.J. Neuromuscular electrical stimulation prevents muscle disuse atrophy during leg immobilization in humans. Acta Physiol. 2014, 210, 628–641. [Google Scholar] [CrossRef]
- Bergouignan, A.; Rudwill, F.; Simon, C.; Blanc, S. Physical inactivity as the culprit of metabolic inflexibility: Evidence from bed-rest studies. J. Appl. Physiol. 2011, 111, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Chung, J.Y. Effectiveness of polydeoxyribonucleotide injection versus normal saline injection for treatment of chronic plantar fasciitis: A prospective randomised clinical trial. Int. Orthop. 2015, 39, 1329–1334. [Google Scholar] [CrossRef] [PubMed]
- Bitto, A.; Polito, F.; Irrera, N.; D’Ascola, A.; Avenoso, A.; Nastasi, G.; Campo, G.M.; Micali, A.; Bagnato, G.; Minutoli, L.; et al. Polydeoxyribonucleotide reduces cytokine production and the severity of collagen-induced arthritis by stimulation of adenosine A(₂A) receptor. Arthritis Rheum. 2011, 63, 3364–3371. [Google Scholar] [CrossRef] [PubMed]
- Bitto, A.; Galeano, M.; Squadrito, F.; Minutoli, L.; Polito, F.; Dye, J.F.; Clayton, E.A.; Calò, M.; Venuti, F.S.; Vaccaro, M.; et al. Polydeoxyribonucleotide improves angiogenesis and wound healing in experimental thermal injury. Crit. Care Med. 2008, 36, 1594–1602. [Google Scholar] [CrossRef]
- Galeano, M.; Bitto, A.; Altavilla, D.; Minutoli, L.; Polito, F.; Calò, M.; Lo Cascio, P.; Stagno d’Alcontres, F.; Squadrito, F. Polydeoxyribonucleotide stimulates angiogenesis and wound healing in the genetically diabetic mouse. Wound Repair Regen. 2008, 16, 208–217. [Google Scholar] [CrossRef]
- Assaly, R.; Giuliano, F.; Clement, P.; Laurin, M.; Favier, M.; Teo, P.; Bernabe, J.; Alexandre, L.; Behr-Roussel, D. Extracorporeal shock waves therapy delivered by aries improves erectile dysfunction in spontaneously hypertensive rats through penile tissue remodeling and neovascularization. Sex. Med. 2019, 7, 441–450. [Google Scholar] [CrossRef]
- Murata, R.; Ohtori, S.; Ochiai, N.; Takahashi, N.; Saisu, T.; Moriya, H.; Takahashi, K.; Wada, Y. Extracorporeal shockwaves induce the expression of ATF3 and GAP-43 in rat dorsal root ganglion neurons. Auton. Neurosci. 2006, 128, 96–100. [Google Scholar] [CrossRef]
- Rompe, J.D.; Decking, J.; Schoellner, C.; Nafe, B. Shock wave application for chronic plantar fasciitis in running athletes. A prospective, randomized, placebo-controlled trial. Am. J. Sports Med. 2003, 31, 268–275. [Google Scholar] [CrossRef]
- Spacca, G.; Necozione, S.; Cacchio, A. Radial shock wave therapy for lateral epicondylitis: A prospective randomised controlled single-blind study. Eura. Medicophys. 2005, 41, 17–25. [Google Scholar] [PubMed]
- Martínez, I.M.; Sempere-Rubio, N.; Navarro, O.; Faubel, R. Effectiveness of shock wave therapy as a treatment for spasticity: A systematic review. Brain Sci. 2020, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Hsu, P.C.; Chang, K.V.; Chiu, Y.H.; Wu, W.T.; Özçakar, L. Comparative effectiveness of botulinum toxin injections and extracorporeal shockwave therapy for post-stroke spasticity: A systematic review and network meta-analysis. EClinicalmedicine 2022, 43, 101222. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.P.; Lin, C.Y.; Kuo, Y.J.; Lee, O.K. Extracorporeal shockwave therapy in the treatment of trigger finger: A randomized controlled study. Arch. Phys. Med. Rehabil. 2021, 102, 2083–2090. [Google Scholar] [CrossRef]
- Zissler, A.; Steinbacher, P.; Zimmermann, R.; Pittner, S.; Stoiber, W.; Bathke, A.C.; Sänger, A.M. Extracorporeal shock wave therapy accelerates regeneration after acute skeletal muscle injury. Am. J. Sports Med. 2017, 45, 676–684. [Google Scholar] [CrossRef]
- Crupnik, J.; Silveti, S.; Wajnstein, N.; Rolon, A.; Vollhardt, A.; Stiller, P.; Schmitz, C. Is radial extracorporeal shock wave therapy combined with a specific rehabilitation program (rESWT + RP) more effective than sham-rESWT + RP for acute hamstring muscle complex injury type 3b in athletes? Study protocol for a prospective, randomized, double-blind, sham-controlled single centre trial. J. Orthop. Surg. Res. 2019, 14, 234. [Google Scholar] [CrossRef] [PubMed]
- Kisch, T.; Wuerfel, W.; Forstmeier, V.; Liodaki, E.; Stang, F.H.; Knobloch, K.; Mailaender, P.; Kraemer, R. Repetitive shock wave therapy improves muscular microcirculation. J. Surg. Res. 2016, 201, 440–445. [Google Scholar] [CrossRef]
- Astur, D.C.; Santos, B.; de Moraes, E.R.; Arliani, G.G.; Dos Santos, P.R.; Pochini Ade, C. Extracorporeal shockwave terapy to treat chronic muscle injury. Acta Ortop. Bras. 2015, 23, 247–250. [Google Scholar] [CrossRef][Green Version]
- Lee, J.H.; Cho, S.H. Effect of extracorporeal shock wave therapy on denervation atrophy and function caused by sciatic nerve injury. J. Phys. Ther. Sci. 2013, 25, 1067–1069. [Google Scholar] [CrossRef][Green Version]
- Kim, D.H.; Kwon, D.R.; Park, G.Y.; Moon, Y.S. Synergetic effects of shock waves with polydeoxyribonucleotides on rotator cuff tendon tear in a rabbit model. Biocell 2021, 45, 527–536. [Google Scholar] [CrossRef]
- Kauhanen, S.; von Boguslawsky, K.; Michelsson, J.E.; Leivo, I. Satellite cell proliferation in rabbit hindlimb muscle following immobilization and remobilization: An immunohistochemical study using MIB 1 antibody. Acta Neuropathol. 1998, 95, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, C.; Császár, N.B.; Milz, S.; Schieker, M.; Maffulli, N.; Rompe, J.D.; Furia, J.P. Efficacy and safety of extracorporeal shock wave therapy for orthopedic conditions: A systematic review on studies listed in the PEDro database. Br. Med. Bull. 2015, 116, 115–138. [Google Scholar] [CrossRef] [PubMed]
- Park, D.S.; Kwon, D.R.; Park, G.Y.; Lee, M.Y. Therapeutic effect of extracorporeal shock wave therapy according to treatment session on gastrocnemius muscle spasticity in children with spastic cerebral palsy: A pilot study. Ann. Rehabil. Med. 2015, 39, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.T.; Ke, M.J.; Chou, Y.C.; Chang, C.Y.; Lin, C.Y.; Li, T.Y.; Shih, F.M.; Chen, L.C. Effect of radial shock wave therapy for carpal tunnel syndrome: A prospective randomized, double-blind, placebo-controlled trial. J. Orthop. Res. 2016, 34, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Chen, S.Y.; Chen, W.S.; Tu, Y.K.; Chien, K.L. Comparative effectiveness of focused shock wave therapy of different intensity levels and radial shock wave therapy for treating plantar fasciitis: A systematic review and network meta-analysis. Arch. Phys. Med. Rehabil. 2012, 93, 1259–1268. [Google Scholar] [CrossRef]
- Park, K.D.; Lee, W.Y.; Park, M.H.; Ahn, J.K.; Park, Y. High- versus low-energy extracorporeal shock-wave therapy for myofascial pain syndrome of upper trapezius: A prospective randomized single blinded pilot study. Medicine 2018, 97, e11432. [Google Scholar] [CrossRef]
- Wang, C.J.; Huang, H.Y.; Pai, C.H. Shock wave-enhanced neovascularization at the tendon-bone junction: An experiment in dogs. J. Foot Ankle Surg. 2002, 41, 16–22. [Google Scholar] [CrossRef]
- Chen, Y.J.; Wang, C.J.; Yang, K.D.; Kuo, Y.R.; Huang, H.C.; Huang, Y.T.; Sun, Y.C.; Wang, F.S. Extracorporeal shock waves promote healing of collagenase-induced Achilles tendinitis and increase TGF-beta1 and IGF-I expression. J. Orthop. Res. 2004, 22, 854–861. [Google Scholar] [CrossRef]
- Zhang, D.; Kearney, C.J.; Cheriyan, T.; Schmid, T.M.; Spector, M. Extracorporeal shockwave-induced expression of lubricin in tendons and septa. Cell Tissue Res. 2011, 346, 255–262. [Google Scholar] [CrossRef]
- Mattyasovszky, S.G.; Langendorf, E.K.; Ritz, U.; Schmitz, C.; Schmidtmann, I.; Nowak, T.E.; Wagner, D.; Hofmann, A.; Rommens, P.M.; Drees, P. Exposure to radial extracorporeal shock waves modulates viability and gene expression of human skeletal muscle cells: A controlled in vitro study. J. Orthop. Surg. Res. 2018, 13, 75. [Google Scholar] [CrossRef]
- Holfeld, J.; Tepeköylü, C.; Blunder, S.; Lobenwein, D.; Kirchmair, E.; Dietl, M.; Kozaryn, R.; Lener, D.; Theurl, M.; Paulus, P.; et al. Low energy shock wave therapy induces angiogenesis in acute hind-limb ischemia via VEGF receptor 2 phosphorylation. PLoS ONE 2014, 9, e103982. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Wang, F.S.; Yang, K.D. Biological effects of extracorporeal shockwave in bone healing: A study in rabbits. Arch. Orthop. Trauma. Surg. 2008, 128, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Barnes, K.; Lanz, O.; Werre, S.; Clapp, K.; Gilley, R. Comparison of autogenous cancellous bone grafting and extracorporeal shock wave therapy on osteotomy healing in the tibial tuberosity advancement procedure in dogs. Radiographic densitometric evaluation. Vet. Comp. Orthop. Traumatol. 2015, 28, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Frey, S.P.; Jansen, H.; Raschke, M.J.; Meffert, R.H.; Ochman, S. VEGF improves skeletal muscle regeneration after acute trauma and reconstruction of the limb in a rabbit model. Clin. Orthop. Relat. Res. 2012, 470, 3607–3614. [Google Scholar] [CrossRef]
- DeLisser, H.M.; Christofidou-Solomidou, M.; Strieter, R.M.; Burdick, M.D.; Robinson, C.S.; Wexler, R.S.; Kerr, J.S.; Garlanda, C.; Merwin, J.R.; Madri, J.A.; et al. Involvement of endothelial PECAM-1/CD31 in angiogenesis. Am. J. Pathol. 1997, 151, 671–677. [Google Scholar]
- DiPietro, L.A. Angiogenesis and wound repair: When enough is enough. J. Leukoc. Biol. 2016, 100, 979–984. [Google Scholar] [CrossRef]
- Veronesi, F.; Dallari, D.; Sabbioni, G.; Carubbi, C.; Martini, L.; Fini, M. Polydeoxyribonucleotides (PDRNs) from skin to musculoskeletal tissue regeneration via adenosine A2A receptor involvement. J. Cell. Physiol. 2017, 232, 2299–2307. [Google Scholar] [CrossRef]
- Altavilla, D.; Bitto, A.; Polito, F.; Marini, H.; Minutoli, L.; Di Stefano, V.; Irrera, N.; Cattarini, G.; Squadrito, F. Polydeoxyribonucleotide (PDRN): A safe approach to induce therapeutic angiogenesis in peripheral artery occlusive disease and in diabetic foot ulcers. Cardiovasc. Hematol. Agents Med. Chem. 2009, 7, 313–321. [Google Scholar] [CrossRef]
- Rathbone, M.P.; Middlemiss, P.J.; Gysbers, J.W.; DeForge, S.; Costello, P.; Del Maestro, R.F. Purine nucleosides and nucleotides stimulate proliferation of a wide range of cell types. Vitr. Cell. Dev. Biol. 1992, 28, 529–536. [Google Scholar] [CrossRef]
- Rathbone, M.P.; Deforge, S.; Deluca, B.; Gabel, B.; Laurenssen, C.; Middlemiss, P.; Parkinson, S. Purinergic stimulation of cell division and differentiation: Mechanisms and pharmacological implications. Med. Hypotheses 1992, 37, 213–219. [Google Scholar] [CrossRef]
- Wang, D.J.; Huang, N.N.; Heppel, L.A. Extracellular ATP shows synergistic enhancement of DNA synthesis when combined with agents that are active in wound healing or as neurotransmitters. Biochem. Biophys. Res. Commun. 1990, 166, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.R.; Park, G.Y.; Lee, S.C. Treatment of full-thickness rotator cuff tendon tear using umbilical cord blood-derived mesenchymal stem cells and polydeoxyribonucleotides in a rabbit model. Stem Cells Int. 2018, 2018, 7146384. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Moretti, B. The biological effects of extracorporeal shock wave therapy (eswt) on tendon tissue. Muscles Ligaments Tendons J. 2012, 2, 33–37. [Google Scholar] [PubMed]
- Apfel, R.E. Acoustic cavitation: A possible consequence of biomedical uses of ultrasound. Br. J. Cancer Suppl. 1982, 5, 140–146. [Google Scholar]
- Gambihler, S.; Delius, M. In vitro interaction of lithotripter shock waves and cytotoxic drugs. Br. J. Cancer 1992, 66, 69–73. [Google Scholar] [CrossRef][Green Version]
- López-Marín, L.M.; Rivera, A.L.; Fernández, F.; Loske, A.M. Shock wave-induced permeabilization of mammalian cells. Phys. Life Rev. 2018, 26–27, 1–38. [Google Scholar] [CrossRef]
- Luh, J.J.; Huang, W.T.; Lin, K.H.; Huang, Y.Y.; Kuo, P.L.; Chen, W.S. Effects of extracorporeal shock wave-mediated transdermal local anesthetic drug delivery on rat caudal nerves. Ultrasound Med. Biol. 2018, 44, 214–222. [Google Scholar] [CrossRef]




| Atrophic Changes (%) | |||
|---|---|---|---|
| Circumference of Rt. Calf (cm) | CMAP on Rt. Tibial Nerve (mV) | Rt. GCM Muscle Thickness (mm) | |
| G1-Control | 24.1 ± 1.6 | 25.7 ± 2.0 | 23.6 ± 1.3 |
| G2-PDRN | 21.6 ± 4.0 * | 20.2 ± 5.0 * | 17.6 ± 3.1 * |
| G3-ESWT | 21.4 ± 3.6 * | 20.0 ± 3.9 * | 15.4 ± 3.4 * |
| G4-PDRN + ESWT | 5.3 ± 2.7 *,†,‡ | 11.8 ± 2.9 *,†,‡ | 9.3 ± 2.7 *,†,‡ |
| G5-ESWT + PDRN | 9.8 ± 4.7 *,†,‡ | 13.7 ± 3.3 *,†,‡ | 12.3 ± 3.2 *,†,‡ |
| G1-Control | G2-PDRN | G3-ESWT | G4-PDRN + ESWT | G5-ESWT + PDRN | |
|---|---|---|---|---|---|
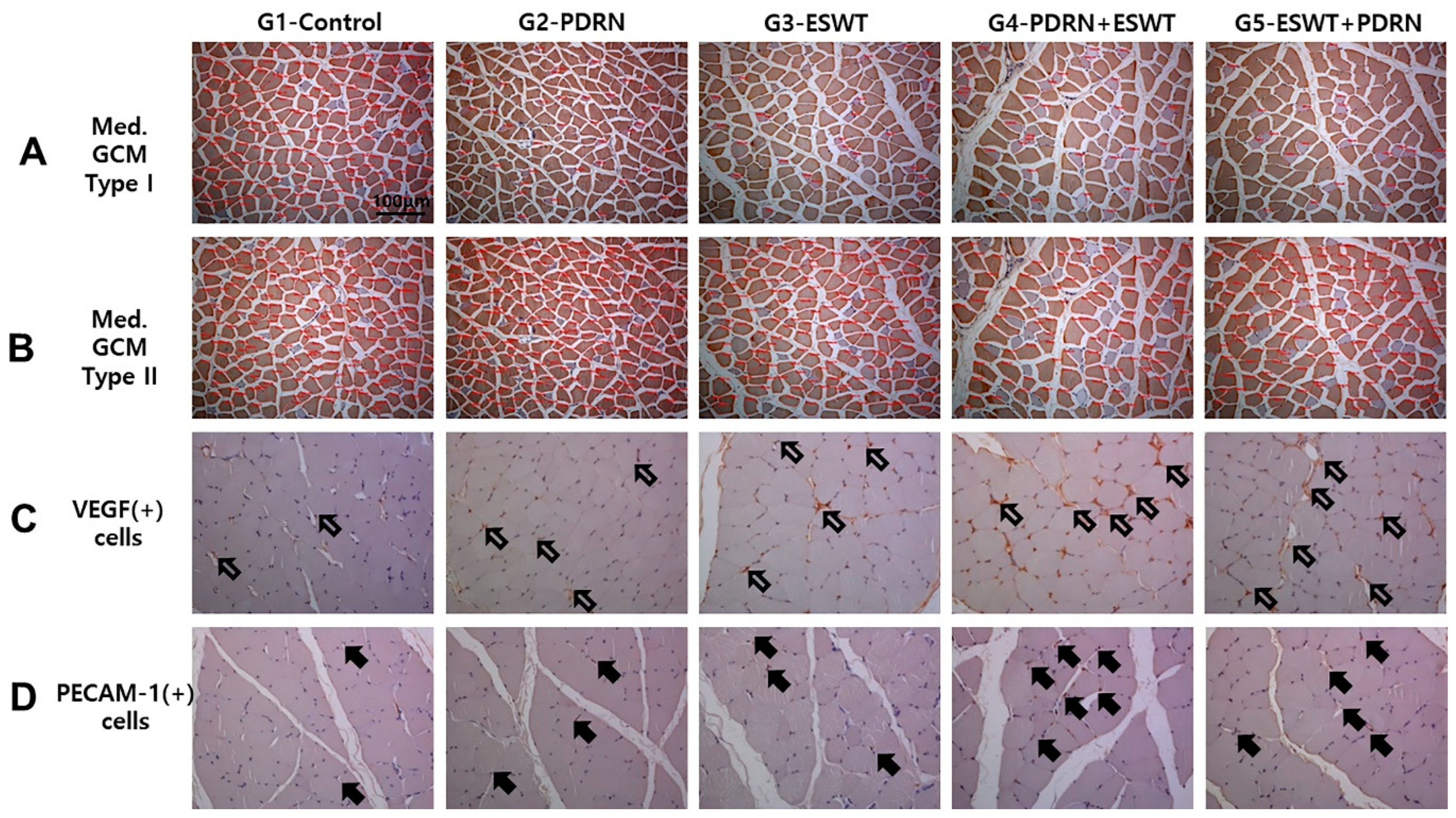
| Medial GCM | |||||
| Type I fiber CSA (μm2) | 287.6 ± 5.5 | 469.4 ± 12.5 * | 716.8 ± 18.9 * | 1391.9 ± 23.6 *,†,‡ | 1137.9 ± 21.1 *,†,‡ |
| Type II fiber CSA (μm2) | 443.1 ± 4.5 | 1554.4 ± 21.4 * | 1735.3 ± 26.2 * | 2458.0 ± 50.6 *,†,‡ | 2046.6 ± 33.8 *,†,‡ |
| Total muscle fiber CSA (μm2) | 399.0 ± 20.5 | 1394.0 ± 22.6 * | 1542.2 ± 25.6 * | 2162.0 ± 42.0 *,†,‡ | 1910.2 ± 31.5 *,†,‡ |
| VEGF ratio | 0.15 ± 0.07 | 0.27 ± 0.02 * | 0.32 ± 0.02 * | 0.59 ± 0.03 *,†,‡,§ | 0.44 ± 0.03 *,†,‡ |
| PECAM-1 ratio | 0.08 ± 0.05 | 0.21 ± 0.02 * | 0.28 ± 0.02 * | 0.59 ± 0.04 *,†,‡,§ | 0.42 ± 0.10 *,†,‡ |
| Lateral GCM | |||||
| Type I fiber CSA (μm2) | 286.2 ± 12.3 | 446.8 ± 15.3 * | 697.9 ± 16.2 * | 1441.2 ± 25.9 *,†,‡ | 1095.1 ± 22.0 *,†,‡ |
| Type II fiber CSA (μm2) | 420.1 ± 4.9 | 1450.6 ± 20.3 * | 1607.1 ± 17.6 * | 2460.4 ± 47.3 *,†,‡ | 1980.9 ± 27.6 *,†,‡ |
| Total muscle fiber CSA (μm2) | 400.73 ± 4.8 | 1366.6 ± 20.7 * | 1481.2 ± 18.5 * | 2173.5 ± 40.0 *,†,‡ | 1858.5 ± 26.4 *,†,‡ |
| VEGF ratio | 0.15 ± 0.05 | 0.29 ± 0.02 * | 0.35 ± 0.04 * | 0.57 ± 0.02 *,†,‡,§ | 0.47 ± 0.02 *,†,‡ |
| PECAM-1 ratio | 0.08 ± 0.06 | 0.28 ± 0.02 * | 0.29 ± 0.04 * | 0.58 ± 0.02 *,†,‡,§ | 0.44 ± 0.03 *,†,‡ |
| G1-Control | G2-PDRN | G3-ESWT | G4-PDRN + ESWT | G5-ESWT + PDRN | |
|---|---|---|---|---|---|
| Relative fold differences | |||||
| PECAM-1 | 1 | 1.19 ± 0.11 * | 1.32 ± 0.09 * | 1.72 ± 0.08 *,†,‡ | 1.77 ± 0.09 *,†,‡ |
| PCNA | 1 | 1.30 ± 0.08 * | 1.50 ± 0.12 * | 1.85 ± 0.13 *,†,‡ | 1.86 ± 0.11 *,†,‡ |
| VEGF | 1 | 1.38 ± 0.13 * | 1.60 ± 0.07 * | 1.90 ± 0.07 *,†,‡ | 1.88 ± 0.12 *,†,‡ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-J.; Moon, Y.S.; Kwon, D.R.; Cho, S.C.; Kim, E.H. Polydeoxyribonucleotide and Shock Wave Therapy Sequence Efficacy in Regenerating Immobilized Rabbit Calf Muscles. Int. J. Mol. Sci. 2023, 24, 12820. https://doi.org/10.3390/ijms241612820
Lee Y-J, Moon YS, Kwon DR, Cho SC, Kim EH. Polydeoxyribonucleotide and Shock Wave Therapy Sequence Efficacy in Regenerating Immobilized Rabbit Calf Muscles. International Journal of Molecular Sciences. 2023; 24(16):12820. https://doi.org/10.3390/ijms241612820
Chicago/Turabian StyleLee, Yoon-Jin, Yong Suk Moon, Dong Rak Kwon, Sung Cheol Cho, and Eun Ho Kim. 2023. "Polydeoxyribonucleotide and Shock Wave Therapy Sequence Efficacy in Regenerating Immobilized Rabbit Calf Muscles" International Journal of Molecular Sciences 24, no. 16: 12820. https://doi.org/10.3390/ijms241612820
APA StyleLee, Y.-J., Moon, Y. S., Kwon, D. R., Cho, S. C., & Kim, E. H. (2023). Polydeoxyribonucleotide and Shock Wave Therapy Sequence Efficacy in Regenerating Immobilized Rabbit Calf Muscles. International Journal of Molecular Sciences, 24(16), 12820. https://doi.org/10.3390/ijms241612820







