Assessment of Apolipoprotein(a) Isoform Size Using Phenotypic and Genotypic Methods
Abstract
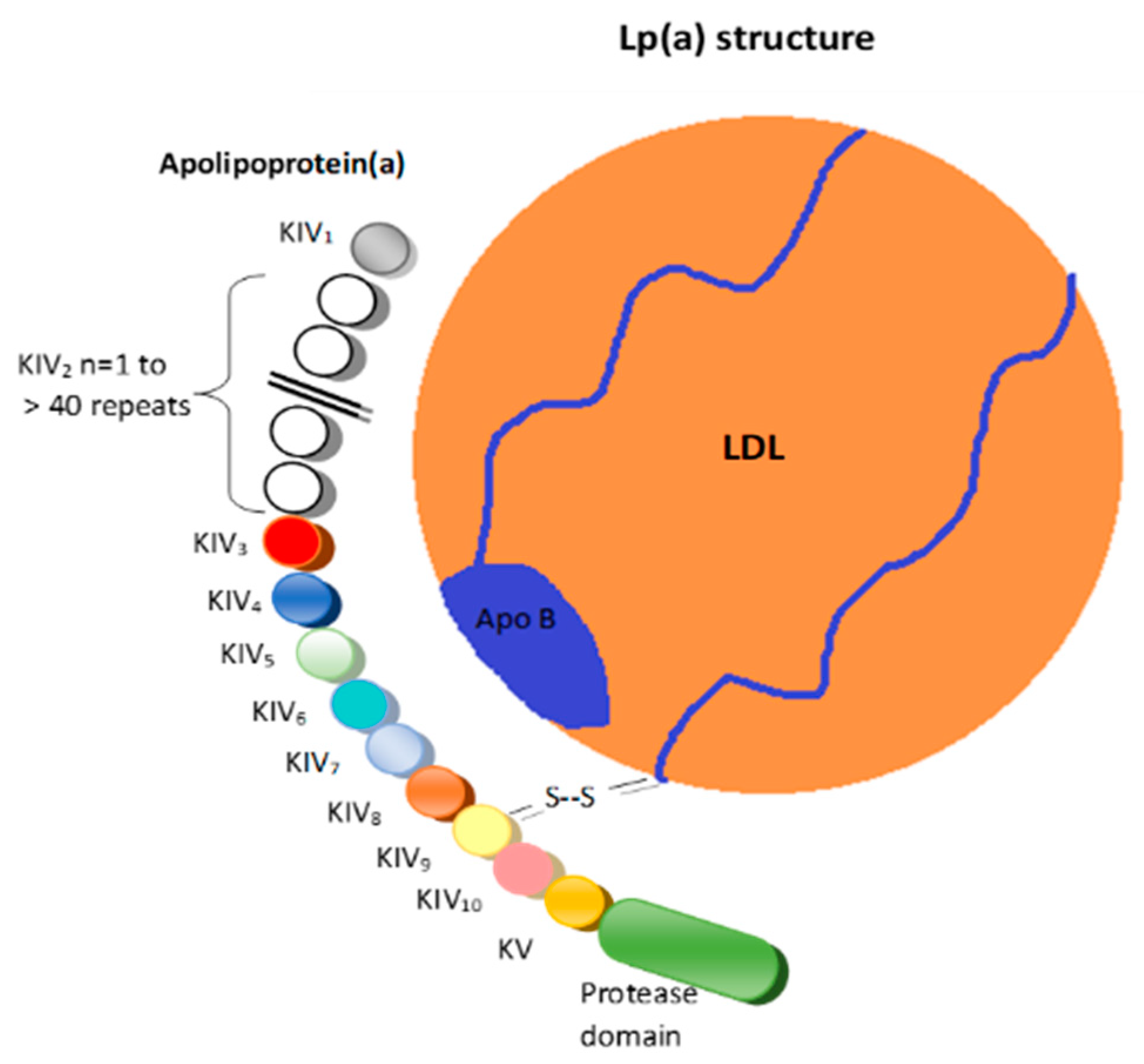
:1. Introduction
2. Techniques to Assess the Size of KIV-2 CNV
2.1. Genotyping Techniques
2.1.1. Pulsed-Field Gel Electrophoresis (PFGE)/Southern Blot
2.1.2. Quantitative Polymerase Chain Reaction (qPCR)
2.1.3. Fiber Fluorescence In Situ Hybridization (Fiber-FISH)
2.2. Phenotyping Techniques
Western Blot Using Antibodies for apo(a) (Immunoblotting)
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koschinsky, M.L.; Kronenberg, F. The long journey of lipoprotein(a) from cardiovascular curiosity to therapeutic target. Atherosclerosis 2022, 349, 1–6. [Google Scholar] [CrossRef]
- Arsenault, B.J.; Kamstrup, P.R. Lipoprotein(a) and cardiovascular and valvular diseases: A genetic epidemiological perspective. Atherosclerosis 2022, 349, 7–16. [Google Scholar] [CrossRef]
- Wang, H.; Wu, P.; Jiang, D.; Zhang, H.; Zhang, J.; Zong, Y.; Han, Y. Relationship between serum homocysteine, fibrinogen, lipoprotein-a level, and peripheral arterial disease: A dose-response meta-analysis. Eur. J. Med. Res. 2022, 27, 261. [Google Scholar] [CrossRef]
- Singh, S.; Baars, D.P.; Desai, R.; Singh, D.; Pinto-Sietsma, S.J. Association between Lipoprotein(a) and risk of atrial fibrillation: A Systematic Review and Meta-analysis of Mendelian Randomization Studies. Curr. Probl. Cardiol. 2023, 49, 102024. [Google Scholar] [CrossRef] [PubMed]
- Amiri, M.; Raeisi-Dehkordi, H.; Verkaar, A.J.C.F.; Wu, Y.; van Westing, A.C.; Berk, K.A.; Bramer, W.M.; Aune, D.; Voortman, T. Circulating lipoprotein (a) and all-cause and cause-specific mortality: A systematic review and dose-response meta-analysis. Eur. J. Epidemiol. 2023, 38, 485–499. [Google Scholar] [CrossRef] [PubMed]
- Chemello, K.; Chan, D.C.; Lambert, G.; Watts, G.F. Recent advances in demystifying the metabolism of lipoprotein(a). Atherosclerosis 2022, 349, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Marcovina, S.M.; Morrisett, J.D. Structure and metabolism of lipoprotein(a). Curr. Opin. Lipidol. 1995, 6, 136–145. [Google Scholar] [CrossRef]
- Coassin, S.; Kronenberg, F. Lipoprotein(a) beyond the kringle IV repeat polymorphism: The complexity of genetic variation in the LPA gene. Atherosclerosis 2022, 349, 17–35. [Google Scholar] [CrossRef]
- Fogacci, F.; Cicero, A.F.G.; D’Addato, S.; Giovannini, M.; Borghi, C.; Brisighella Heart Study Group. Effect of spontaneous changes in dietary components and lipoprotein(a) levels: Data from the Brisighella Heart Study. Atherosclerosis 2017, 262, 202–204. [Google Scholar] [CrossRef]
- Matveyenko, A.; Matienzo, N.; Ginsberg, H.; Nandakumar, R.; Seid, H.; Ramakrishnan, R.; Holleran, S.; Thomas, T.; Reyes-Soffer, G. Relationship of apolipoprotein(a) isoform size with clearance and production of lipoprotein(a) in a diverse cohort. J. Lipid. Res. 2023, 64, 100336. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Fogacci, F.; Derosa, G.; D’Angelo, A.; Ventura, F.; Rizzoli, E.; D’Addato, S.; Borghi, C.; On Behalf of The Brisighella Heart Study Group. Lipoprotein(a) Serum Levels Predict Pulse Wave Velocity in Subjects in Primary Prevention for Cardiovascular Disease with Large Apo(a) Isoforms: Data from the Brisighella Heart Study. Biomedicines 2022, 10, 656. [Google Scholar] [CrossRef] [PubMed]
- Grüneis, R.; Lamina, C.; Di Maio, S.; Schönherr, S.; Zoescher, P.; Forer, L.; Streiter, G.; Peters, A.; Gieger, C.; Köttgen, A.; et al. The effect of LPA Thr3888Pro on lipoprotein(a) and coronary artery disease is modified by the LPA KIV-2 variant 4925G>A. Atherosclerosis 2022, 349, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Sandholzer, C.; Saha, N.; Kark, J.D.; Rees, A.; Jaross, W.; Dieplinger, H.; Hoppichler, F.; Boerwinkle, E.; Utermann, G. Apo(a) isoforms predict risk for coronary heart disease. A study in six populations. Arterioscler. Thromb. 1992, 12, 1214–1226. [Google Scholar] [CrossRef]
- Rader, D.J.; Cain, W.; Ikewaki, K.; Talley, G.; Zech, L.A.; Usher, D.; Brewer, H.B., Jr. The inverse association of plasma lipoprotein(a) concentrations with apolipoprotein(a) isoform size is not due to differences in Lp(a) catabolism but to differences in production rate. J. Clin. Investig. 1994, 93, 2758–2763. [Google Scholar] [CrossRef]
- Ma, L.; Chan, D.C.; Ooi, E.M.M.; Marcovina, S.M.; Barrett, P.H.R.; Watts, G.F. Apolipoprotein(a) Kinetics in Statin-Treated Patients with Elevated Plasma Lipoprotein(a) Concentration. J. Clin. Endocrinol. Metab. 2019, 104, 6247–6255. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.C.; Watts, G.F.; Coll, B.; Wasserman, S.M.; Marcovina, S.M.; Barrett, P.H.R. Lipoprotein(a) Particle Production as a Determinant of Plasma Lipoprotein(a) Concentration Across Varying Apolipoprotein(a) Isoform Sizes and Background Cholesterol-Lowering Therapy. J. Am. Heart Assoc. 2019, 8, e011781. [Google Scholar] [CrossRef]
- Jenner, J.L.; Seman, L.J.; Millar, J.S.; Lamon-Fava, S.; Welty, F.K.; Dolnikowski, G.G.; Marcovina, S.M.; Lichtenstein, A.H.; Barrett, P.H.; deLuca, C.; et al. The metabolism of apolipoproteins (a) and B-100 within plasma lipoprotein (a) in human beings. Metabolism. 2005, 54, 361–369. [Google Scholar] [CrossRef]
- Kronenberg, F. Lipoprotein(a). In Prevention and Treatment of Atherosclerosis. Handbook of Experimental Pharmacology; von Eckardstein, A., Binder, C.J., Eds.; Springer: Cham, Switzerland, 2021; Volume 270, pp. 201–232. [Google Scholar] [CrossRef]
- Mehta, A.; Jain, V.; Saeed, A.; Saseen, J.J.; Gulati, M.; Ballantyne, C.M.; Virani, S.S. Lipoprotein(a) and ethnicities. Atherosclerosis 2022, 349, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Kraft, H.G.; Lingenhel, A.; Pang, R.W.; Delport, R.; Trommsdorff, M.; Vermaak, H.; Janus, E.D.; Utermann, G. Frequency distributions of apolipoprotein(a) kringle IV repeat alleles and their effects on lipoprotein(a) levels in Caucasian, Asian, and African populations: The distribution of null alleles is non-random. Eur. J. Hum. Genet. 1996, 4, 74–87. [Google Scholar] [CrossRef]
- Fogacci, F.; Cicero, A.F.; D’Addato, S.; D’Agostini, L.; Rosticci, M.; Giovannini, M.; Bertagnin, E.; Borghi, C.; Brisighella Heart Study Group. Serum lipoprotein(a) level as long-term predictor of cardiovascular mortality in a large sample of subjects in primary cardiovascular prevention: Data from the Brisighella Heart Study. Eur. J. Intern. Med. 2017, 37, 49–55. [Google Scholar] [CrossRef]
- Erqou, S.; Thompson, A.; Di Angelantonio, E.; Saleheen, D.; Kaptoge, S.; Marcovina, S.; Danesh, J. Apolipoprotein(a) isoforms and the risk of vascular disease: Systematic review of 40 studies involving 58,000 participants. J. Am. Coll. Cardiol. 2010, 55, 2160–2167. [Google Scholar] [CrossRef]
- Kraft, H.G.; Lingenhel, A.; Köchl, S.; Hoppichler, F.; Kronenberg, F.; Abe, A.; Mühlberger, V.; Schönitzer, D.; Utermann, G. Apolipoprotein(a) kringle IV repeat number predicts risk for coronary heart disease. Arterioscler. Thromb. Vasc. Biol. 1996, 16, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Wild, S.H.; Fortmann, S.P.; Marcovina, S.M. A prospective case-control study of lipoprotein(a) levels and apo(a) size and risk of coronary heart disease in Stanford Five-City Project participants. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Mueller, P.A.; Yerkes, E.; Bergstrom, P.; Rosario, S.; Hay, J.; Pamir, N. A method for lipoprotein (a) Isolation from a small volume of plasma with applications for clinical research. Sci. Rep. 2022, 12, 9138. [Google Scholar] [CrossRef] [PubMed]
- Neidhoefer, C. Structural Analysis of Apolipoprotein(a) Kringle IV Type 2 A Genetical, Key Tandem-Repeat Factor in Cardiovascular Diseases. Ph.D. Thesis, University of Pavia, Pavia, Italy, 2018. [Google Scholar] [CrossRef]
- Maher, K.; Persa, L.; Barry, D.; Lee-Eng, J.; Dichek, H.; Joshi, S.; Amlie-Lefond, C. Thrombophilia screening in the routine clinical care of children with arterial ischemic stroke. Pediatr. Blood. Cancer. 2023, 70, e30381. [Google Scholar] [CrossRef] [PubMed]
- Paciullo, F.; Giannandrea, D.; Virgili, G.; Cagini, C.; Gresele, P. Role of Increased Lipoprotein (a) in Retinal Vein Occlusion: A Systematic Review and Meta-analysis. TH Open 2021, 5, e295–e302. [Google Scholar] [CrossRef]
- Sticchi, E.; Magi, A.; Kamstrup, P.R.; Marcucci, R.; Prisco, D.; Martinelli, I.; Mannucci, P.M.; Abbate, R.; Giusti, B. Apolipoprotein(a) Kringle-IV Type 2 Copy Number Variation Is Associated with Venous Thromboembolism. PLoS ONE 2016, 11, e0149427. [Google Scholar] [CrossRef]
- Ren, X.; Zhang, Z.; Yan, Z. Association Between Lipoprotein (A) and Diabetic Nephropathy in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis. Front. Endocrinol. 2021, 12, 633529. [Google Scholar] [CrossRef]
- Ulloque-Badaracco, J.R.; Mosquera-Rojas, M.D.; Hernandez-Bustamante, E.A.; Alarcón-Braga, E.A.; Ulloque-Badaracco, R.R.; Al-Kassab-Córdova, A.; Herrera-Añazco, P.; Benites-Zapata, V.A.; Hernandez, A.V. Association between Lipid Profile and Apolipoproteins with Risk of Diabetic Foot Ulcer: A Systematic Review and Meta-Analysis. Int. J. Clin. Pract. 2022, 2022, 5450173. [Google Scholar] [CrossRef]
- Tsimikas, S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. J. Am. Coll. Cardiol. 2017, 69, 692–711. [Google Scholar] [CrossRef]
- Nordestgaard, B.G.; Chapman, M.J.; Kausik, R.; Borén, J.; Andreotti, F.; Watts, G.F.; Ginsberg, H.; Amarenco, P.; Catapano, A.; Descamps, O.S.; et al. Lipoprotein(a) as a cardiovascular risk factor: Current status. Eur. Heart 2010, 23, 2844–2853. [Google Scholar] [CrossRef]
- Vazirian, F.; Sadeghi, M.; Kelesidis, T.; Budoff, M.J.; Zandi, Z.; Samadi, S.; Mohammadpour, A.H. Predictive value of lipoprotein(a) in coronary artery calcification among asymptomatic cardiovascular disease subjects: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2023, in press. [Google Scholar] [CrossRef]
- Motawea, K.R.; Elhalag, R.H.; Aboelenein, M.; Ibrahim, N.; Swed, S.; Fathy, H.; Awad, D.M.; Belal, M.M.; Talaat, N.E.; Rozan, S.S.; et al. Association of Aortic Valve Calcification and High Levels of Lipoprotein (a): Systematic Review and Meta-Analysis. Curr. Probl. Cardiol. 2023, 48, 101746. [Google Scholar] [CrossRef] [PubMed]
- Tsarouhas, K.; Hoursalas, A.; Vardavas, A.I.; Tsitsimpikou, C. Lipoprotein a: An emerging risk identifier and evolving clinical target. Public Health Toxicol. 2022, 2, 2. [Google Scholar] [CrossRef]
- Kamstrup, P.R. Lipoprotein(a) and Cardiovascular Disease. Clin. Chem. 2021, 67, 154–166. [Google Scholar] [CrossRef] [PubMed]
- Zysow, B.R.; Lindahl, G.E.; Wade, D.P.; Knight, B.L.; Lawn, R.M. C/T polymorphism in the 5’ untranslated region of the apolipoprotein(a) gene introduces an upstream ATG and reduces in vitro translation. Arterioscler. Thromb. Vasc. Biol. 1995, 15, 58–64. [Google Scholar] [CrossRef]
- Gu, J.X.; Huang, J.; Li, S.S.; Zhou, L.H.; Yang, M.; Li, Y.; Zhang, A.M.; Yin, Y.; Zhang, N.; Jia, M.; et al. Elevated lipoprotein(a) and genetic polymorphisms in the LPA gene may predict cardiovascular events. Sci. Rep. 2022, 12, 3588. [Google Scholar] [CrossRef] [PubMed]
- Kraft, H.G.; Köchl, S.; Menzel, H.J.; Sandholzer, C.; Utermann, G. The apolipoprotein (a) gene: A transcribed hypervariable locus controlling plasma lipoprotein (a) concentration. Hum. Genet. 1992, 90, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Anglés-Cano, E.; Loyau, S.; Cardoso-Saldaña, G.; Couderc, R.; Gillery, P. A novel kringle-4 number-based recombinant apo[a] standard for human apo[a] phenotyping. J. Lipid. Res. 1999, 40, 354–359. [Google Scholar] [CrossRef]
- Lackner, C.; Boerwinkle, E.; Leffert, C.C.; Rahmig, T.; Hobbs, H.H. Molecular basis of apolipoprotein (a) isoform size hetero-geneity as revealed by pulsed-field gel electrophoresis. J. Clin. Investig. 1991, 87, 2153–2161. [Google Scholar] [CrossRef]
- Chiou, C.S.; Wei, H.L.; Yang, L.C. Comparison of pulsed-field gel electrophoresis and coagulase gene restriction profile analysis techniques in the molecular typing of Staphylococcus aureus. J. Clin. Microbiol. 2000, 38, 2186–2190. [Google Scholar] [CrossRef]
- Li, Y.; Wang, Y.; Gong, F.; Yu, X.; Zhang, T. A novel deletion mutation in the LPA gene in a middle-aged woman with ischaemic stroke. BMC Med. Genom. 2021, 14, 132. [Google Scholar] [CrossRef] [PubMed]
- Lanktree, M.B.; Rajakumar, C.; Brunt, J.H.; Koschinsky, M.L.; Connelly, P.W.; Hegele, R.A. Determination of lipoprotein(a) krin-gle repeat number from genomic DNA: Copy number variation genotyping using qPCR. J. Lipid. Res. 2009, 50, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, K.; Noureen, A.; Kronenberg, F.; Utermann, G. Structure, function, and genetics of lipoprotein (a). J. Lipid. Res. 2016, 57, 1339–1359. [Google Scholar] [CrossRef] [PubMed]
- Erdel, M.; Hubalek, M.; Lingenhel, A.; Kofler, K.; Duba, H.-C.; Utermann, G. Counting the repetitive kringle-IV repeats in the gene encoding human apolipoprotein(a) by fibre-FISH. Nat. Genet. 1999, 21, 357–358. [Google Scholar] [CrossRef]
- Enkhmaa, B.; Anuurad, E.; Zhang, W.; Tran, T.; Berglund, L. Lipoprotein(a): Genotype-phenotype relationship and impact on atherogenic risk. Metab. Syndr. Relat. Disord. 2011, 9, 411–418. [Google Scholar] [CrossRef]
- Pradhan, S.; Apaydin, S.; Bucevičius, J.; Gerasimaitė, R.; Kostiuk, G.; Lukinavičius, G. Sequence-specific DNA labelling for fluorescence microscopy. Biosens. Bioelectron 2023, 230, 115256. [Google Scholar] [CrossRef]
- Zekavat, S.M.; Ruotsalainen, S.; Handsaker, R.E.; Alver, M.; Bloom, J.; Poterba, T.; Seed, C.; Ernst, J.; Chaffin, M.; Engreitz, J.; et al. Deep coverage whole genome sequences and plasma lipoprotein(a) in individuals of European and African ancestries. Nat. Commun. 2018, 9, 2606. [Google Scholar] [CrossRef]
- Mazur, P.; Dumnicka, P.; Tisończyk, J.; Ząbek-Adamska, A.; Drożdż, R. SDS Electrophoresis on Gradient Polyacrylamide Gels as a Semiquantitative Tool for the Evaluation of Proteinuria. Diagnostics 2023, 13, 1513. [Google Scholar] [CrossRef]
- Koschinsky, M.L.; Beisiegel, U.; Henne-Bruns, D.; Eaton, D.L.; Lawn, R.M. Apolipoprotein(a) size heterogeneity is related to variable number of repeat sequences in its mRNA. Biochemistry 1990, 29, 640–644. [Google Scholar] [CrossRef]
- Kamboh, M.I.; Ferrell, R.E.; Kottke, B.A. Expressed hypervariable polymorphism of apolipoprotein (a). Am. J. Hum. Genet. 1991, 49, 1063–1074. [Google Scholar] [PubMed]
- Geroldi, D.; Bellotti, V.; Buscaglia, P.; Bonetti, G.; Gazzaruso, C.; Caprioli, A.; Fratino, P. Characterization of apo(a) polymorphism by a modified immunoblotting technique in an Italian population sample. Clin. Chim. Acta 1993, 221, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Koschinsky, M.L.; Stroes, E.S.G.; Kronenberg, F. Daring to dream: Targeting lipoprotein(a) as a causal and risk-enhancing factor. Pharmacol. Res. 2023, 194, 106843. [Google Scholar] [CrossRef]
- Santos, H.O.; Kones, R.; Rumana, U.; Earnest, C.P.; Izidoro, L.F.M.; Macedo, R.C.O. Lipoprotein(a): Current Evidence for a Physiologic Role and the Effects of Nutraceutical Strategies. Clin. Ther. 2019, 41, 1780–1797. [Google Scholar] [CrossRef]
- Willeit, P.; Ridker, P.M.; Nestel, P.J.; Simes, J.; Tonkin, A.M.; Pedersen, T.R.; Schwartz, G.G.; Olsson, A.G.; Colhoun, H.M.; Kronenberg, F.; et al. Baseline and on-statin treatment lipoprotein(a) levels for prediction of cardiovascular events: Individual patient-data meta-analysis of statin outcome trials. Lancet 2018, 392, 1311–1320. [Google Scholar] [CrossRef]
- Schandelmaier, S.; Briel, M.; Saccilotto, R.; Olu, K.K.; Arpagaus, A.; Hemkens, L.G.; Nordmann, A.J. Niacin for primary and secondary prevention of cardiovascular events. Cochrane Database Syst. Rev. 2017, 6, CD009744. [Google Scholar] [CrossRef]
- Parish, S.; Hopewell, J.C.; Hill, M.R.; Marcovina, S.; Valdes-Marquez, E.; Haynes, R.; Offer, A.; Pedersen, T.R.; Baigent, C.; Collins, R.; et al. Impact of Apolipoprotein(a) Isoform Size on Lipoprotein(a) Lowering in the HPS2-THRIVE Study. Circ. Genom. Precis. Med. 2018, 11, e001696. [Google Scholar] [CrossRef] [PubMed]
- Fogacci, F.; Ferri, N.; Toth, P.P.; Ruscica, M.; Corsini, A.; Cicero, A.F.G. Efficacy and Safety of Mipomersen: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Drugs 2019, 79, 751–766. [Google Scholar] [CrossRef]
- Gencer, B.; Mach, F. Potential of Lipoprotein(a)-Lowering Strategies in Treating Coronary Artery Disease. Drugs 2020, 80, 229–239. [Google Scholar] [CrossRef]
- Zhou, J.; Zhang, Q.; Wang, Y.; Gao, P.; Chen, D. The effect and safety of anacetrapib in the treatment of dyslipidemia: A systematic review and meta-analysis. Postgrad Med. 2018, 130, 129–136. [Google Scholar] [CrossRef]
- Nicholls, S.J.; Ruotolo, G.; Brewer, H.B.; Wang, M.D.; Liu, L.; Willey, M.B.; Deeg, M.A.; Krueger, K.A.; Nissen, S.E. Evacetrapib alone or in combination with statins lowers lipoprotein(a) and total and small LDL particle concentrations in mildly hypercholesterolemic patients. J. Clin. Lipidol. 2016, 10, 519–527.e4. [Google Scholar] [CrossRef] [PubMed]
- Afanasieva, O.I.; Ezhov, M.V.; Razova, O.A.; Afanasieva, M.I.; Utkina, E.A.; Pokrovsky, S.N. Apolipoprotein(a) phenotype determines the correlations of lipoprotein(a) and proprotein convertase subtilisin/kexin type 9 levels in patients with potential familial hypercholesterolemia. Atherosclerosis 2018, 277, 477–482. [Google Scholar] [CrossRef]
- Chan, D.C.; Watts, G.F. The Promise of PCSK9 and Lipoprotein(a) as Targets for Gene Silencing Therapies. Clin. Ther. 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, Y.; Pantea Stoian, A.; Cicero, A.F.G.; Fogacci, F.; Nikolic, D.; Sachinidis, A.; Rizvi, A.A.; Janez, A.; Rizzo, M. Inclisiran: A small interfering RNA strategy targeting PCSK9 to treat hypercholesterolemia. Expert Opin. Drug Saf. 2022, 21, 9–20. [Google Scholar] [CrossRef]
- Yu, Z.; Hu, L.; Sun, C.; Wang, Z.; Zhang, X.; Wu, M.; Liu, L. Effect of Different Types and Dosages of Proprotein Convertase Subtilisin/Kexin Type 9 Inhibitors on Lipoprotein(a) Levels: A Network Meta-analysis. J. Cardiovasc. Pharmacol. 2023, 81, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.G.; Fogacci, F.; Zambon, A.; Toth, P.P.; Borghi, C. Efficacy and safety of inclisiran a newly approved FDA drug: A systematic review and pooled analysis of available clinical studies. Am. Heart J. 2022, 13, 100127. [Google Scholar] [CrossRef]
- Hanssen, R.; Gouni-Berthold, I. Lipoprotein(a) Management: Pharmacological and Apheretic Treatment. Curr. Med. Chem. 2017, 24, 957–968. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, V.; Chemello, K.; Hollstein, T.; Hong-Fong, C.C.; Schumann, F.; Grenkowitz, T.; Nativel, B.; Coassin, S.; Croyal, M.; Kassner, U.; et al. The size of apolipoprotein (a) is an independent determinant of the reduction in lipoprotein (a) induced by PCSK9 inhibitors. Cardiovasc Res. 2022, 118, 2103–2111. [Google Scholar] [CrossRef]
- Alhomoud, I.S.; Talasaz, A.; Mehta, A.; Kelly, M.S.; Sisson, E.M.; Bucheit, J.D.; Brown, R.; Dixon, D.L. Role of lipoprotein(a) in atherosclerotic cardiovascular disease: A review of current and emerging therapies. Pharmacotherapy 2023, in press. [CrossRef]
- Karwatowska-Prokopczuk, E.; Clouet-Foraison, N.; Xia, S.; Viney, N.J.; Witztum, J.L.; Marcovina, S.M.; Tsimikas, S. Prevalence and influence of LPA gene variants and isoform size on the Lp(a)-lowering effect of pelacarsen. Atherosclerosis 2021, 324, 102–108. [Google Scholar] [CrossRef]
- Kotani, K.; Serban, M.C.; Penson, P.; Lippi, G.; Banach, M. Evidence-based assessment of lipoprotein(a) as a risk biomarker for cardiovascular diseases—Some answers and still many questions. Crit. Rev. Clin. Lab. Sci. 2016, 53, 370–378. [Google Scholar] [CrossRef]
- Kamstrup, P.R.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Genetic evidence that lipoprotein(a) associates with atherosclerotic stenosis rather than venous thrombosis. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 1732–1741. [Google Scholar] [CrossRef]
- Coassin, S.; Erhart, G.; Weissensteiner, H.; Eca Guimarães de Araújo, M.; Lamina, C.; Schönherr, S.; Forer, L.; Haun, M.; Losso, J.L.; Köttgen, A.; et al. A novel but frequent variant in LPA KIV-2 is associated with a pronounced Lp(a) and cardiovascular risk reduction. Eur Heart J. 2017, 38, 1823–1831. [Google Scholar] [CrossRef] [PubMed]
- Schachtl-Riess, J.F.; Kheirkhah, A.; Grüneis, R.; Di Maio, S.; Schoenherr, S.; Streiter, G.; Losso, J.L.; Paulweber, B.; Eckardt, K.U.; Köttgen, A.; et al. Frequent LPA KIV-2 Variants Lower Lipoprotein(a) Concentrations and Protect Against Coronary Artery Disease. J. Am. Coll. Cardiol. 2021, 78, 437–449. [Google Scholar] [CrossRef]
- Saleheen, D.; Haycock, P.C.; Zhao, W.; Rasheed, A.; Taleb, A.; Imran, A.; Abbas, S.; Majeed, F.; Akhtar, S.; Qamar, N.; et al. Apolipoprotein(a) isoform size, lipoprotein(a) concentration, and coronary artery disease: A mendelian randomisation analysis. Lancet Diabetes Endocrinol. 2017, 5, 524–533. [Google Scholar] [CrossRef] [PubMed]
- Lanktree, M.B.; Anand, S.S.; Yusuf, S.; Hegele, R.A.; SHARE Investigators. Comprehensive analysis of genomic variation in the LPA locus and its relationship to plasma lipoprotein(a) in South Asians, Chinese, and European Caucasians. Circ. Cardiovasc. Genet. 2010, 3, 39–46. [Google Scholar] [CrossRef]
- Yeang, C.; Clopton, P.C.; Tsimikas, S. Lipoprotein(a)-cholesterol levels estimated by vertical auto profile correlate poorly with Lp(a) mass in hyperlipidemic subjects: Implications for clinical practice interpretation of Lp(a)-mediated risk. J. Clin. Lipidol. 2016, 10, 1389–1396. [Google Scholar] [CrossRef]
- Enkhmaa, B.; Anuurad, E.; Berglund, L. Lipoprotein (a): Impact by ethnicity and environmental and medical conditions. J. Lipid Res. 2016, 57, 1111–1125. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, B.G.; Langsted, A. Lipoprotein (a) as a cause of cardiovascular disease: Insights from epidemiology, genetics, and biology. J. Lipid Res. 2016, 57, 1953–1975. [Google Scholar] [CrossRef]
- Barlera, S.; Specchia, C.; Farrall, M.; Chiodini, B.D.; Franzosi, M.G.; Rust, S.; Green, F.; Nicolis, E.B.; Peden, J.; Assmann, G.; et al. Multiple QTL influence the serum Lp(a) concentration: A genome-wide linkage screen in the PROCARDIS study. Eur. J. Hum. Genet. 2007, 15, 221–227. [Google Scholar] [CrossRef]
- Simó, J.M.; Camps, J.; Martín, S.; Pedro-Botet, J.; Ferré, N.; Gómez, F.; Joven, J. Differences between genotyping and phenotyp-ing methods for assessing apolipoprotein(a) size polymorphisms. Clin. Chem. Lab. Med. 2003, 41, 1340–1344. [Google Scholar] [CrossRef]
- Di Maio, S.; Grüneis, R.; Streiter, G.; Lamina, C.; Maglione, M.; Schoenherr, S.; Öfner, D.; Thorand, B.; Peters, A.; Eckardt, K.U.; et al. Investigation of a nonsense mutation located in the complex KIV-2 copy number variation region of apolipoprotein(a) in 10,910 individuals. Genome Med. 2020, 12, 74. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Cheng, Y.C.; Chen, K.; Wang, H.; Gerhard, G.S.; Still, C.D.; Chu, X.; Yang, R.; Parihar, A.; O’Connell, J.R.; et al. Evidence for several independent genetic variants affecting lipoprotein (a) cholesterol levels. Hum. Mol. Genet. 2015, 24, 2390–2400. [Google Scholar] [CrossRef]
- Behera, S.; Belyeu, J.R.; Chen, X.; Paulin, L.F.; Nguyen, N.Q.H.; Newman, E.; Mahmoud, M.; Menon, V.K.; Qi, Q.; Joshi, P.; et al. Identification of allele-specific KIV-2 repeats and impact on Lp(a) measurements for cardiovascular disease risk. bioRxiv 2023. [Google Scholar] [CrossRef]
- Schwaninger, G.; Forer, L.; Ebenbichler, C.; Dieplinger, H.; Kronenberg, F.; Zschocke, J.; Witsch-Baumgartner, M. Filling the gap: Genetic risk assessment in hypercholesterolemia using LDL-C and LPA genetic scores. Clin. Genet. 2023, 104, 334–343. [Google Scholar] [CrossRef]
- Wei, W.Q.; Li, X.; Feng, Q.; Kubo, M.; Kullo, I.J.; Peissig, P.L.; Karlson, E.W.; Jarvik, G.P.; Lee, M.T.M.; Shang, N.; et al. LPA Variants Are Associated with Residual Cardiovascular Risk in Patients Receiving Statins. Circulation 2018, 138, 1839–1849. [Google Scholar] [CrossRef] [PubMed]
- Alankar, A.; Brar, P.C.; Kohn, B. Lipoprotein(a): A Case for Universal Screening in Youth. Curr. Atheroscler. Rep. 2023, 25, 487–493. [Google Scholar] [CrossRef]
- Ronald, J.; Rajagopalan, R.; Cerrato, F.; Nord, A.S.; Hatsukami, T.; Kohler, T.; Marcovina, S.; Heagerty, P.; Jarviket, G.P. Genetic variation in LPAL2, LPA, and PLG predicts plasma lipoprotein(a) level and carotid artery disease risk. Stroke 2011, 42, 2–9. [Google Scholar] [CrossRef]
- Noureen, A.; Fresser, F.; Utermann, G.; Schmidt, K. Sequence variation within the KIV-2 copy number polymorphism of the human LPA gene in African, Asian, and European populations. PLoS ONE 2015, 10, e0121582. [Google Scholar] [CrossRef]
- Kamstrup, P.R.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Extreme lipoprotein(a) levels and improved cardiovascular risk pre-diction. J. Am. Coll. Cardiol. 2013, 61, 1146–1156. [Google Scholar] [CrossRef]
- Kamstrup, P.R.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J. Am. Coll. Cardiol. 2014, 63, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Puckey, L.H.; Lawn, R.M.; Knight, B.L. Polymorphisms in the apolipoprotein(a) gene and their relationship to allele size and plasma lipoprotein(a) concentration. Hum. Mol. Genet. 1997, 6, 1099–1107. [Google Scholar] [CrossRef] [PubMed]

| Experimental Technique | Level of Information | Investigated Molecule | Outcome | Setting | Main Strengths | Main Limitations |
|---|---|---|---|---|---|---|
| Western Blot (SDS-PAGE agarose) | Phenotype | apo(a) (protein) | Double-band visualization in heterozygotes | Clinical Practice |
|
|
| PFGE | Genotype | DNA | Displaying the sum of KIV-2 CNV over alleles | Clinical Practice |
|
|
| qPCR | Genotype | DNA | Displaying the sum of KIV-2 CNV over alleles | Clinical Practice |
|
|
| Fiber-FISH | Genotype | DNA | Microscopic visualization of KIV-2 CNV on both alleles separately | Population Studies |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fogacci, F.; Di Micoli, V.; Avagimyan, A.; Giovannini, M.; Imbalzano, E.; Cicero, A.F.G. Assessment of Apolipoprotein(a) Isoform Size Using Phenotypic and Genotypic Methods. Int. J. Mol. Sci. 2023, 24, 13886. https://doi.org/10.3390/ijms241813886
Fogacci F, Di Micoli V, Avagimyan A, Giovannini M, Imbalzano E, Cicero AFG. Assessment of Apolipoprotein(a) Isoform Size Using Phenotypic and Genotypic Methods. International Journal of Molecular Sciences. 2023; 24(18):13886. https://doi.org/10.3390/ijms241813886
Chicago/Turabian StyleFogacci, Federica, Valentina Di Micoli, Ashot Avagimyan, Marina Giovannini, Egidio Imbalzano, and Arrigo F. G. Cicero. 2023. "Assessment of Apolipoprotein(a) Isoform Size Using Phenotypic and Genotypic Methods" International Journal of Molecular Sciences 24, no. 18: 13886. https://doi.org/10.3390/ijms241813886
APA StyleFogacci, F., Di Micoli, V., Avagimyan, A., Giovannini, M., Imbalzano, E., & Cicero, A. F. G. (2023). Assessment of Apolipoprotein(a) Isoform Size Using Phenotypic and Genotypic Methods. International Journal of Molecular Sciences, 24(18), 13886. https://doi.org/10.3390/ijms241813886









