Plasma miR-486-5p Expression Is Upregulated in Atrial Fibrillation Patients with Broader Low-Voltage Areas
Abstract
:1. Introduction
2. Results
2.1. Characteristics of AF Cohort
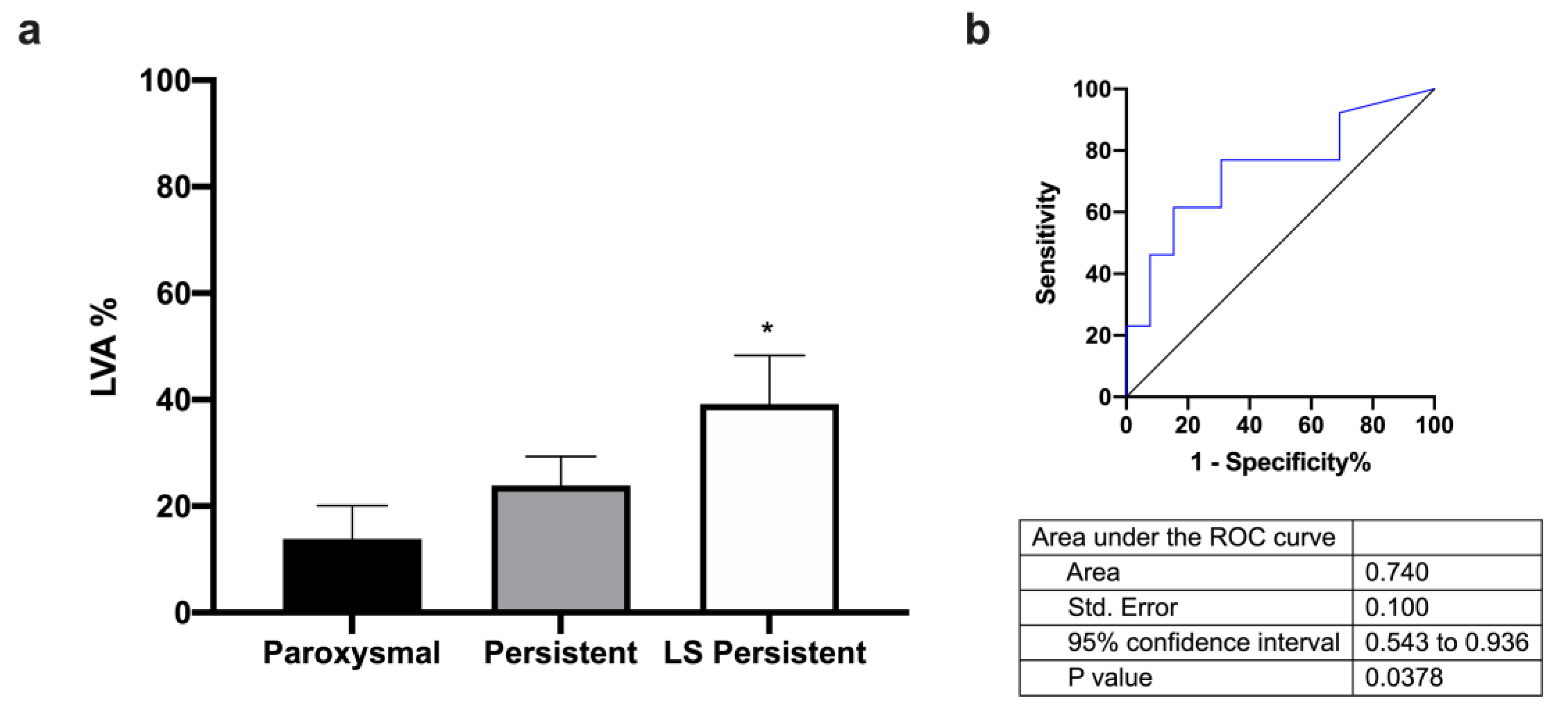
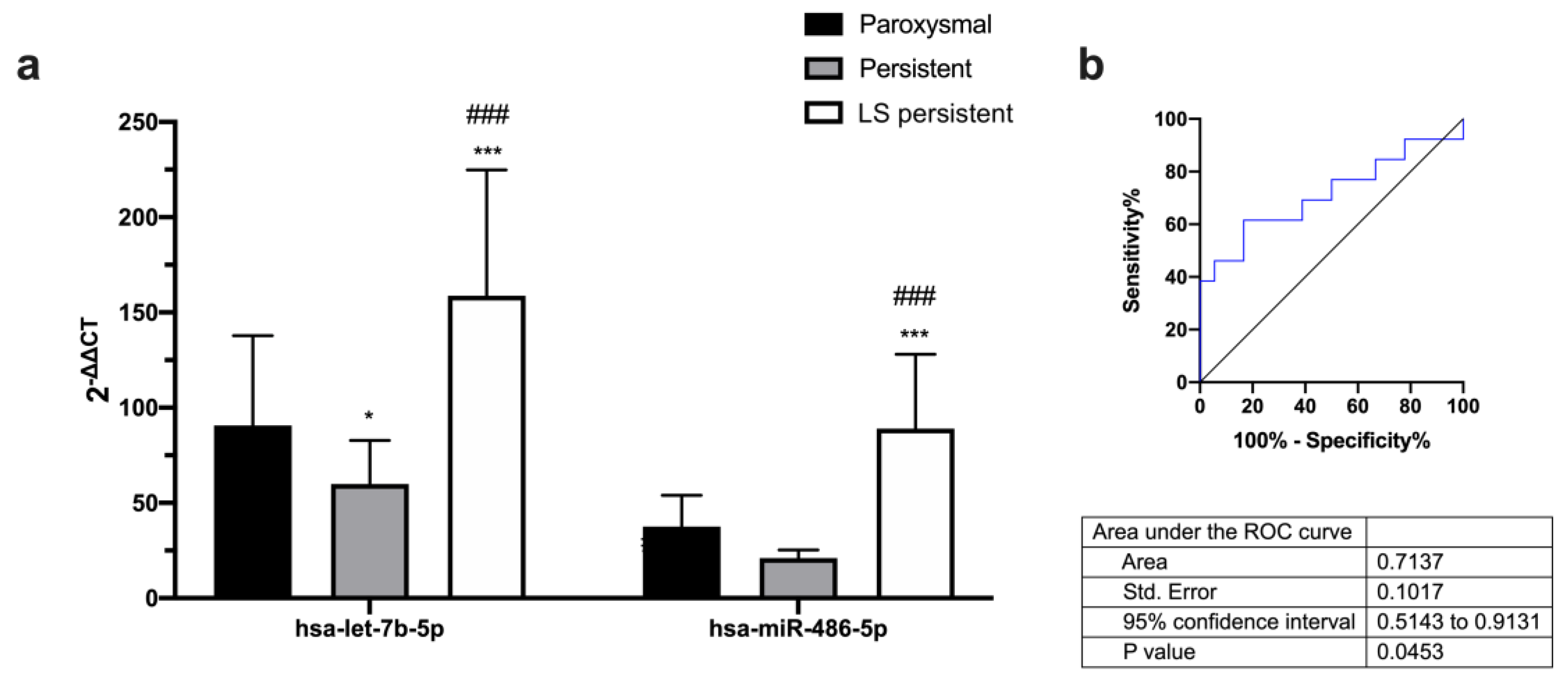
2.2. Different Expression of microRNAs with LVA in AF Patients
2.3. Different Expression of microRNAs with AF Type
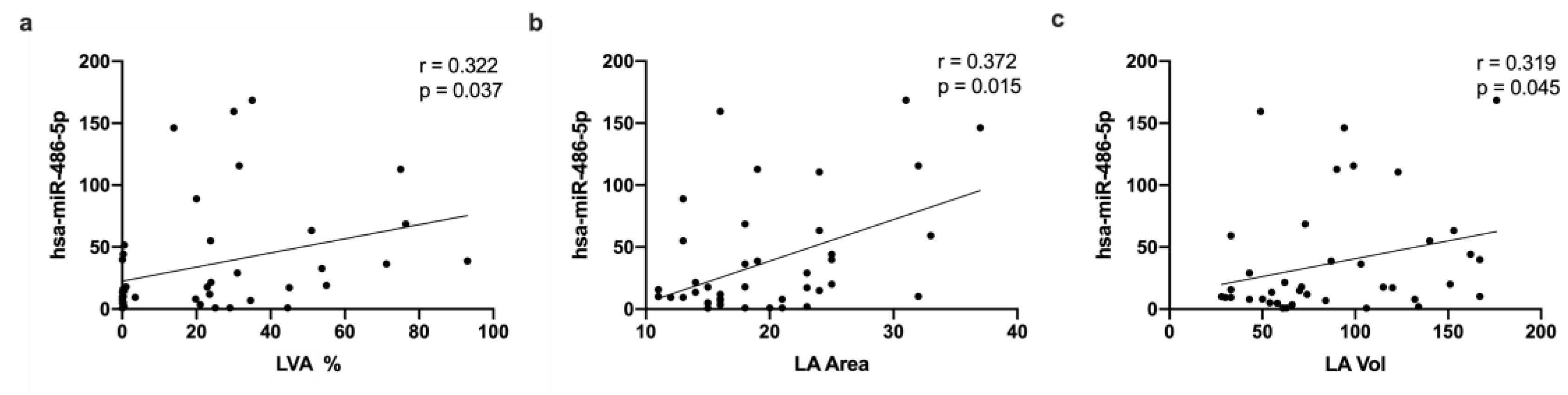
2.4. MicroRNA Correlation with Clinical Data
2.5. KEGG Pathways and Prediction Targets
3. Discussion
Limitations
4. Materials and Methods
4.1. Patients
4.2. AF Assessment
4.3. Surgery Intervention and Sample Collection
4.4. Ablation, Acquisition of Electroanatomical Voltage Maps, and Patient Follow-Up
4.5. RNA Extraction and miRNA Quantification
4.6. Bioinformatics Analysis for miRNA Target Genes and Biological Pathways
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kornej, J.; Börschel, C.S.; Benjamin, E.J.; Schnabel, R.B. Epidemiology of Atrial Fibrillation in the 21st Century: Novel Methods and New Insights. Circ. Res. 2020, 127, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Rottner, L.; Bellmann, B.; Lin, T.; Reissmann, B.; Tönnis, T.; Schleberger, R.; Nies, M.; Jungen, C.; Dinshaw, L.; Klatt, N.; et al. Catheter Ablation of Atrial Fibrillation: State of the Art and Future Perspectives. Cardiol. Ther. 2020, 9, 45–58. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.H.; Linz, D.; Sanders, P. New Findings in Atrial Fibrillation Mechanisms. Card. Electrophysiol. Clin. 2019, 11, 563–571. [Google Scholar] [CrossRef]
- Böhm, A.; Vachalcova, M.; Snopek, P.; Bacharova, L.; Komarova, D.; Hatala, R. Molecular Mechanisms, Diagnostic Aspects and Therapeutic Opportunities of Micro Ribonucleic Acids in Atrial Fibrillation. Int. J. Mol. Sci. 2020, 21, 2742. [Google Scholar] [CrossRef] [PubMed]
- Marrouche, N.F.; Wilber, D.; Hindricks, G.; Jais, P.; Akoum, N.; Marchlinski, F.; Kholmovski, E.; Burgon, N.; Hu, N.; Mont, L.; et al. Association of Atrial Tissue Fibrosis Identified by Delayed Enhancement MRI and Atrial Fibrillation Catheter Ablation. JAMA 2014, 311, 498. [Google Scholar] [CrossRef] [PubMed]
- Barletta, V.; Mazzocchetti, L.; Parollo, M.; Spatafora, D.; Bongiorni, M.G.; Zucchelli, G. Multimodality Imaging for Atrial Fibrosis Detection in the Era of Precision Medicine. J. Cardiovasc. Echogr. 2021, 31, 189–197. [Google Scholar] [CrossRef]
- La Cartografía Electroanatómica (CARTO) En La Ablación de La Fibrilación Auricular. Available online: https://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1405-99402006000600028 (accessed on 13 September 2022).
- Rodríguez-Mañero, M.; Valderrábano, M.; Baluja, A.; Kreidieh, O.; Martínez-Sande, J.L.; García-Seara, J.; Saenen, J.; Iglesias-Álvarez, D.; Bories, W.; Villamayor-Blanco, L.M.; et al. Validating Left Atrial Low Voltage Areas During Atrial Fibrillation and Atrial Flutter Using Multielectrode Automated Electroanatomic Mapping. JACC Clin. Electrophysiol. 2018, 4, 1541–1552. [Google Scholar] [CrossRef]
- Anter, E.; Tschabrunn, C.M.; Josephson, M.E. High-Resolution Mapping of Scar-Related Atrial Arrhythmias Using Smaller Electrodes with Closer Interelectrode Spacing. Circ. Arrhythm. Electrophysiol. 2015, 8, 537–545. [Google Scholar] [CrossRef]
- Ammar-Busch, S.; Buiatti, A.; Tatzber, A.; Reents, T.; Bourier, F.; Semmler, V.; Telishevska, M.; Hessling, G.; Deisenhofer, I. Predictors of Low Voltage Areas in Persistent Atrial Fibrillation: Is It Really a Matter of Time? J. Interv. Card. Electrophysiol. 2020, 57, 345–352. [Google Scholar] [CrossRef]
- Luo, X.; Yang, B.; Nattel, S. MicroRNAs and Atrial Fibrillation: Mechanisms and Translational Potential. Nat. Rev. Cardiol. 2015, 12, 80–90. [Google Scholar] [CrossRef]
- Komal, S.; Yin, J.J.; Wang, S.H.; Huang, C.Z.; Tao, H.L.; Dong, J.Z.; Han, S.N.; Zhang, L.R. MicroRNAs: Emerging Biomarkers for Atrial Fibrillation. J. Cardiol. 2019, 74, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Maleck, C.; von Ungern-Sternberg, S.N.I.; Neupane, B.; Heinzmann, D.; Marquardt, J.; Duckheim, M.; Scheckenbach, C.; Stimpfle, F.; Gawaz, M.; et al. Circulating MicroRNA-21 Correlates With Left Atrial Low-Voltage Areas and Is Associated With Procedure Outcome in Patients Undergoing Atrial Fibrillation Ablation. Circ. Arrhythm. Electrophysiol. 2018, 11, e006242. [Google Scholar] [CrossRef]
- Hao, H.; Dai, C.; Han, X.; Li, Y. A Novel Therapeutic Strategy for Alleviating Atrial Remodeling by Targeting Exosomal MiRNAs in Atrial Fibrillation. Biochim. Biophys. Acta Mol. Cell Res. 2022, 1869, 119365. [Google Scholar] [CrossRef]
- Barwari, T.; Joshi, A.; Mayr, M. MicroRNAs in Cardiovascular Disease. J. Am. Coll. Cardiol. 2016, 68, 2577–2584. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.M.G.; de Araújo, J.N.G.; de Freitas, R.C.C.; Silbiger, V.N. Circulating MicroRNAs as Potential Biomarkers of Atrial Fibrillation. Biomed. Res. Int. 2017, 2017, 7804763. [Google Scholar] [CrossRef] [PubMed]
- Akoum, N.; Wilber, D.; Hindricks, G.; Jais, P.; Cates, J.; Marchlinski, F.; Kholmovski, E.; Burgon, N.; Hu, N.; Mont, L.; et al. MRI Assessment of Ablation-Induced Scarring in Atrial Fibrillation: Analysis from the DECAAF Study. J. Cardiovasc. Electrophysiol. 2015, 26, 473–480. [Google Scholar] [CrossRef]
- Lange, S.; Banerjee, I.; Carrion, K.; Serrano, R.; Habich, L.; Kameny, R.; Lengenfelder, L.; Dalton, N.; Meili, R.; Börgeson, E.; et al. MiR-486 Is Modulated by Stretch and Increases Ventricular Growth. JCI Insight 2019, 4, e125507. [Google Scholar] [CrossRef]
- Wang, J.; Song, S.; Xie, C.; Han, J.; Li, Y.; Shi, J.; Xin, M.; Wang, J.; Luo, T.; Meng, X.; et al. MicroRNA Profiling in the Left Atrium in Patients with Non-Valvular Paroxysmal Atrial Fibrillation. BMC Cardiovasc. Disord. 2015, 15, 97. [Google Scholar] [CrossRef]
- Slagsvold, K.H.; Johnsen, A.B.; Rognmo, Ø.; Høydal, M.A.; Wisløff, U.; Wahba, A. Mitochondrial Respiration and MicroRNA Expression in Right and Left Atrium of Patients with Atrial Fibrillation. Physiol. Genom. 2014, 46, 505–511. [Google Scholar] [CrossRef]
- Mun, D.; Kim, H.; Kang, J.-Y.; Park, H.; Park, H.; Lee, S.-H.; Yun, N.; Joung, B. Expression of MiRNAs in Circulating Exosomes Derived from Patients with Persistent Atrial Fibrillation. FASEB J. 2019, 33, 5979–5989. [Google Scholar] [CrossRef]
- Li, N.; Artiga, E.; Kalyanasundaram, A.; Hansen, B.J.; Webb, A.; Pietrzak, M.; Biesiadecki, B.; Whitson, B.; Mokadam, N.A.; Janssen, P.M.L.; et al. Altered MicroRNA and MRNA Profiles during Heart Failure in the Human Sinoatrial Node. Sci. Rep. 2021, 11, 19328. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Ruan, Z.; Wang, F.; Chen, G.; Zhu, J.; Ren, Y.; Zhu, L. Construction of Atrial Fibrillation-related circRNA/lncRNA-miRNA-mRNA Regulatory Network and Analysis of Potential Biomarkers. J. Clin. Lab. Anal. 2023, 37, e24833. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Tian, L.; Yan, Z.; Wang, J.; Xue, T.; Sun, Q. Diagnostic and Prognostic Value of MiR-486-5p, MiR-451a, MiR-21-5p and Monocyte to High-Density Lipoprotein Cholesterol Ratio in Patients with Acute Myocardial Infarction. Heart Vessels 2023, 38, 318–331. [Google Scholar] [CrossRef] [PubMed]
- Niculescu, L.S.; Simionescu, N.; Sanda, G.M.; Carnuta, M.G.; Stancu, C.S.; Popescu, A.C.; Popescu, M.R.; Vlad, A.; Dimulescu, D.R.; Simionescu, M.; et al. MiR-486 and MiR-92a Identified in Circulating HDL Discriminate between Stable and Vulnerable Coronary Artery Disease Patients. PLoS ONE 2015, 10, e0140958. [Google Scholar] [CrossRef]
- Platonov, P.G.; Mitrofanova, L.B.; Orshanskaya, V.; Ho, S.Y. Structural Abnormalities in Atrial Walls Are Associated with Presence and Persistency of Atrial Fibrillation but Not with Age. J. Am. Coll. Cardiol. 2011, 58, 2225–2232. [Google Scholar] [CrossRef]
- Yamamoto, C.; Trayanova, N.A. Atrial Fibrillation: Insights from Animal Models, Computational Modeling, and Clinical Studies. EBioMedicine 2022, 85, 104310. [Google Scholar] [CrossRef]
- Zhang, R.; Zhao, J.; Mandveno, A.; Potter, J.D. Cardiac Troponin I Phosphorylation Increases the Rate of Cardiac Muscle Relaxation. Circ. Res. 1995, 76, 1028–1035. [Google Scholar] [CrossRef]
- Zhu, N.; Yi, B.; Guo, Z.; Zhang, G.; Huang, S.; Qin, Y.; Zhao, X.; Sun, J. Pim-1 Kinase Phosphorylates Cardiac Troponin I and Regulates Cardiac Myofilament Function. Cell Physiol. Biochem. 2018, 45, 2174–2186. [Google Scholar] [CrossRef]
- Emmert, D.B.; Vukovic, V.; Dordevic, N.; Weichenberger, C.X.; Losi, C.; D’Elia, Y.; Volpato, C.; Hernandes, V.V.; Gögele, M.; Foco, L.; et al. Genetic and Metabolic Determinants of Atrial Fibrillation in a General Population Sample: The CHRIS Study. Biomolecules 2021, 11, 1663. [Google Scholar] [CrossRef]
- Cao, W.; Shi, P.; Ge, J.-J. MiR-21 Enhances Cardiac Fibrotic Remodeling and Fibroblast Proliferation via CADM1/STAT3 Pathway. BMC Cardiovasc. Disord. 2017, 17, 88. [Google Scholar] [CrossRef]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation 2014, 130, 2071–2104. [Google Scholar] [CrossRef] [PubMed]
- López-Canoa, J.N.; Couselo-Seijas, M.; González-Ferrero, T.; Almengló, C.; Álvarez, E.; González-Maestro, A.; González-Melchor, L.; Martínez-Sande, J.L.; García-Seara, J.; Fernández-López, J.; et al. The Role of Fatty Acid-Binding Protein 4 in the Characterization of Atrial Fibrillation and the Prediction of Outcomes after Catheter Ablation. Int. J. Mol. Sci. 2022, 23, 11107. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Wazni, O.M.; Marrouche, N.F.; Martin, D.O.; Kilicaslan, F.; Minor, S.; Schweikert, R.A.; Saliba, W.; Cummings, J.; Burkhardt, J.D.; et al. Pre-Existent Left Atrial Scarring in Patients Undergoing Pulmonary Vein Antrum Isolation: An Independent Predictor of Procedural Failure. J. Am. Coll. Cardiol. 2005, 45, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Rottner, L.; Heeger, C.-H.; Lemes, C.; Wohlmuth, P.; Maurer, T.; Reissmann, B.; Fink, T.; Mathew, S.; Ouyang, F.; Kuck, K.-H.; et al. Quantification of Left Atrial Fibrosis in Patients After Pulmonary Vein Isolation Using the Second-Generation Cryoballoon. Int. Heart J. 2021, 62, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Lage, R.; Cebro-Márquez, M.; Vilar-Sánchez, M.E.; González-Melchor, L.; García-Seara, J.; Martínez-Sande, J.L.; Fernández-López, X.A.; Aragón-Herrera, A.; Martínez-Monzonís, M.A.; González-Juanatey, J.R.; et al. Circulating MiR-451a Expression May Predict Recurrence in Atrial Fibrillation Patients after Catheter Pulmonary Vein Ablation. Cells 2023, 12, 638. [Google Scholar] [CrossRef]



| Parameter | Total | All Patients | ||
|---|---|---|---|---|
| n = 44 | Stage 1 (n = 18) | Stage 2 (n = 18) | Stage 3 (n = 8) | |
| Age (years) | 58.6 (62.5–54.8) | 56.3 (60.4–52.1) | 58.7 (62.9–54.5) | 66.8 (73.6–59.9) |
| Male | 31 (70.5%) | 14 (73.7%) | 13 (72.2%) | 4 (50%) |
| BMI | 29.2 (31.3–28.2) | 29.6 (32.2–27.1) | 29.8 (31.9–27.7) | 30.0 (35.7–24.3) |
| Pre-existing Conditions | ||||
| Hypertension | 25 (56.8%) | 8 (44.4%) | 11 (61.1%) | 6 (75%) |
| Diabetes | 7 (15.9%) | 1 (5.5%) | 3 (16.6%) | 3 (37.5%) |
| Smoking | 14 (31.8%) | 6 (33.3%) | 6 (33.3%) | 2 (33.3%) |
| LVA % | 24.7 (32.9–16.5) | 0.4 (0.9–0) | 28.3 (32.4–24.2) *** | 71.1 (85.6–56.7) ***,### |
| Statines | 21 (47.7%) | 8 (44.4%) | 7 (38.8%) | 6 (75%) |
| ACEi | 11 (25%) | 5 (27.7%) | 6 (33.3%) | 0 (0%) |
| ARB | 12 (27.3%) | 2 (11.1%) | 4 (22.2%) | 6 (75%) **,## |
| DHP Ca channel blockers | 5 (11.4%) | 1 (5.5%) | 1 (5.5%) | 3 (37.5%) *,# |
| Acenocoumarol | 18 (40.9%) | 6 (33.3%) | 8 (44.4%) | 4 (50%) |
| NOAG | 26 (59.1%) | 12 (66.6%) | 10 (55.5%) | 4 (50%) |
| Class I ADT | 15 (34.1%) | 9 (50%) | 4 (22.2%) | 2 (33.3%) |
| Class II ADT | 34 (77.3%) | 15 (83.3%) | 12 (66.6%) | 7 (87.5%) |
| Class III ADT | 13 (29.6%) | 3 (16.7%) | 8 (44.4%) | 2 (33.3%) |
| Class IV ADT | 4 (9.1%) | 1 (5.6%) | 2 (11.1%) | 1 (16.6%) |
| Cholesterol | 187.1 ± 43.2 | 185.7 ± 33.4 | 189.4 ± 55.4 | 184.9 ± 34.1 |
| LDLc | 108.9 ± 32.5 | 113.5 ± 26.6 | 106.4 ± 43.7 | 103.9 ± 15.2 |
| HDLc | 53.4 (59.2–47.5) | 51.5 (62.8–40.2) | 52.1 (60.6–43.7) | 59.9 (73.7–46.0) |
| TG | 121.7 (137.8–105.5) | 127.0 (147.0–107.0) | 123.8 (157.5–90.0) | 105.6 (137.7–73.6) **,# |
| FA type | ||||
| Paroxysmal | 13 (29.5%) | 8 (44.4%) | 4 (22.2%) | 1 (16.6%) |
| Persistent | 18 (40.9%) | 7 (38.8%) | 8 (44.4%) | 3 (37.5%) |
| Long-standing persistent | 13 (29.5%) | 3 (16.6%) | 6 (33.3%) | 4 (50%) |
| Echocardiographic Parameters | ||||
| LVEF (%) | 59.8 (62.4–55.9) | 59.8 (64.7–55.0) | 58.3 (64.8–52.4) | 59.8 (66.7–55.1) |
| LA Area (cm2) | 18.7 (21.3–17.7) | 18.2 (21.4–15.0) | 19.7 (22.6–16.7) | 22.0 (26.2–17.8) |
| LA Vol (mL) | 86.5 (104.2–76.4) | 83.7 (110.5–56.9) | 89.3 (109.8–68.9) | 108.7 (135.0–82.5) **,# |
| LVEDV (mL) | 64.7 (74.4–52.7) | 58.7 (72.9–44.5) | 77.3 (99.1–55.4) ** | 43.0 (55.4–30.6) ### |
| LVESV (mL) | 25.3 (31.3–19.1) | 22.4 (27.9–16.9) | 32.1 (46.4–17.8) | 15.8 (20.9–10.8) # |
| LVTDD (mm) | 40.4 (43.3–37.6) | 39.7 (43.2–36.2) | 43.9 (49.3–38.5) | 34.5 (42.5–26.5) |
| LVTSD (mm) | 27.8 (30.2–25.9) | 28.4 (31.9–25.0) | 29.5 (33.3–25.7) | 23.8 (27.3–20.4) |
| EAT Vol (mL) | 81 (99.3–62.7) | 65.2 (78.5–51.9) | 101.4 (141.2–61.7) *** | 78.9 (155.7–2.1) # |
| ECG Parameters | ||||
| HR | 74.3 (80–67.1) | 78.7 (92.4–65.1) | 66.8 (73.0–60.7) * | 77.3 (93.2–61.3) |
| PR | 159.1 ± 25.0 | 148.8 ± 26.6 | 164.0 ± 25.3 | 165.5 ± 7.8 |
| QRS | 94.7 (98.7–91.1) | 92.6 (97.1–88.0) | 96.3 (102.1–90.6) | 96.8 (113.7–79.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cebro-Márquez, M.; Rodríguez-Mañero, M.; Serrano-Cruz, V.; Vilar-Sánchez, M.E.; González-Melchor, L.; García-Seara, J.; Martínez-Sande, J.L.; Aragón-Herrera, A.; Martínez-Monzonís, M.A.; González-Juanatey, J.R.; et al. Plasma miR-486-5p Expression Is Upregulated in Atrial Fibrillation Patients with Broader Low-Voltage Areas. Int. J. Mol. Sci. 2023, 24, 15248. https://doi.org/10.3390/ijms242015248
Cebro-Márquez M, Rodríguez-Mañero M, Serrano-Cruz V, Vilar-Sánchez ME, González-Melchor L, García-Seara J, Martínez-Sande JL, Aragón-Herrera A, Martínez-Monzonís MA, González-Juanatey JR, et al. Plasma miR-486-5p Expression Is Upregulated in Atrial Fibrillation Patients with Broader Low-Voltage Areas. International Journal of Molecular Sciences. 2023; 24(20):15248. https://doi.org/10.3390/ijms242015248
Chicago/Turabian StyleCebro-Márquez, María, Moisés Rodríguez-Mañero, Valentina Serrano-Cruz, Marta E. Vilar-Sánchez, Laila González-Melchor, Javier García-Seara, José Luis Martínez-Sande, Alana Aragón-Herrera, María Amparo Martínez-Monzonís, José Ramón González-Juanatey, and et al. 2023. "Plasma miR-486-5p Expression Is Upregulated in Atrial Fibrillation Patients with Broader Low-Voltage Areas" International Journal of Molecular Sciences 24, no. 20: 15248. https://doi.org/10.3390/ijms242015248
APA StyleCebro-Márquez, M., Rodríguez-Mañero, M., Serrano-Cruz, V., Vilar-Sánchez, M. E., González-Melchor, L., García-Seara, J., Martínez-Sande, J. L., Aragón-Herrera, A., Martínez-Monzonís, M. A., González-Juanatey, J. R., Lage, R., & Moscoso, I. (2023). Plasma miR-486-5p Expression Is Upregulated in Atrial Fibrillation Patients with Broader Low-Voltage Areas. International Journal of Molecular Sciences, 24(20), 15248. https://doi.org/10.3390/ijms242015248






