Associations between Endothelial Lipase, High-Density Lipoprotein, and Endothelial Function Differ in Healthy Volunteers and Metabolic Syndrome Patients
Abstract
:1. Introduction
2. Results
2.1. Demographics, Clinical Characteristics, and Medication
2.2. Standard Laboratory Data
2.3. HDL Subclasses, Lipid Content, and Function
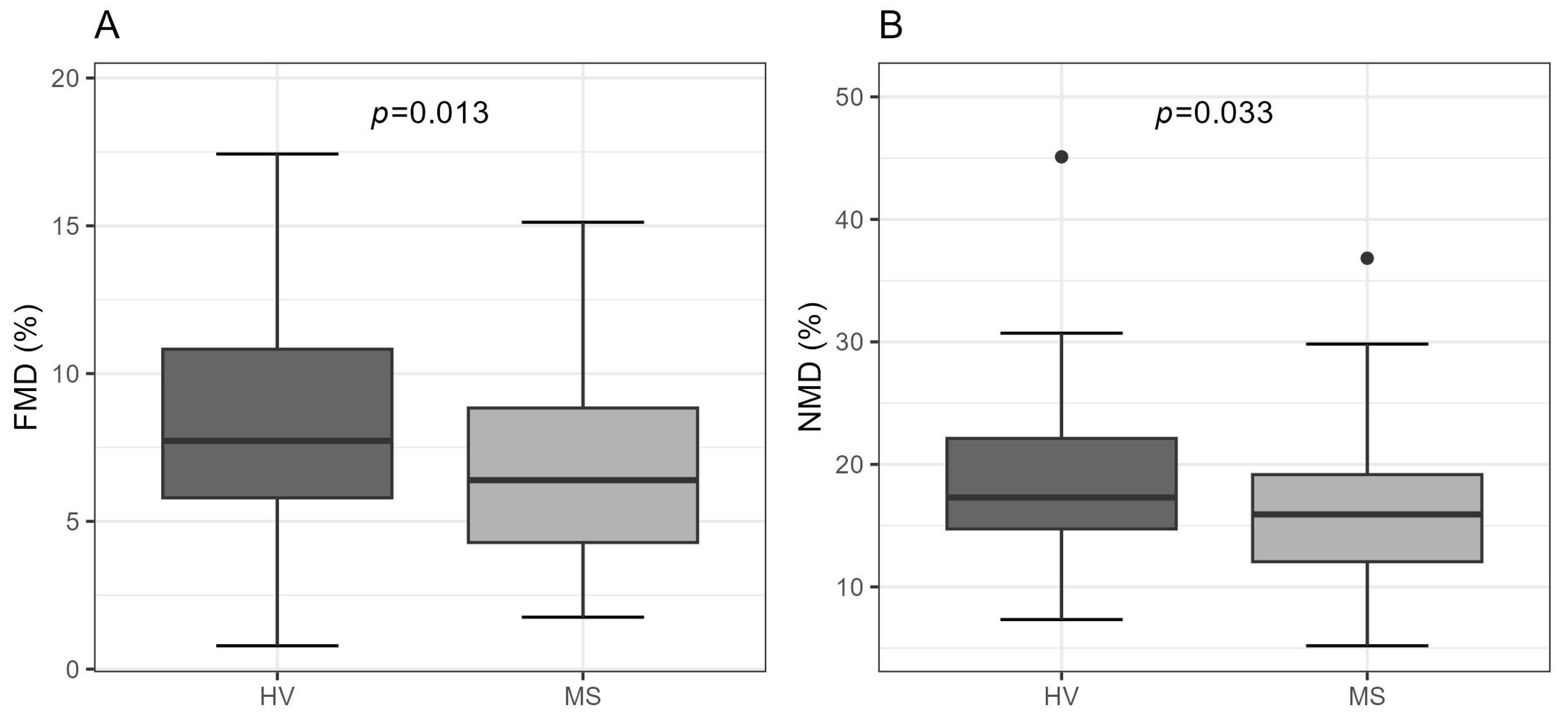
2.4. Brachial Artery Function
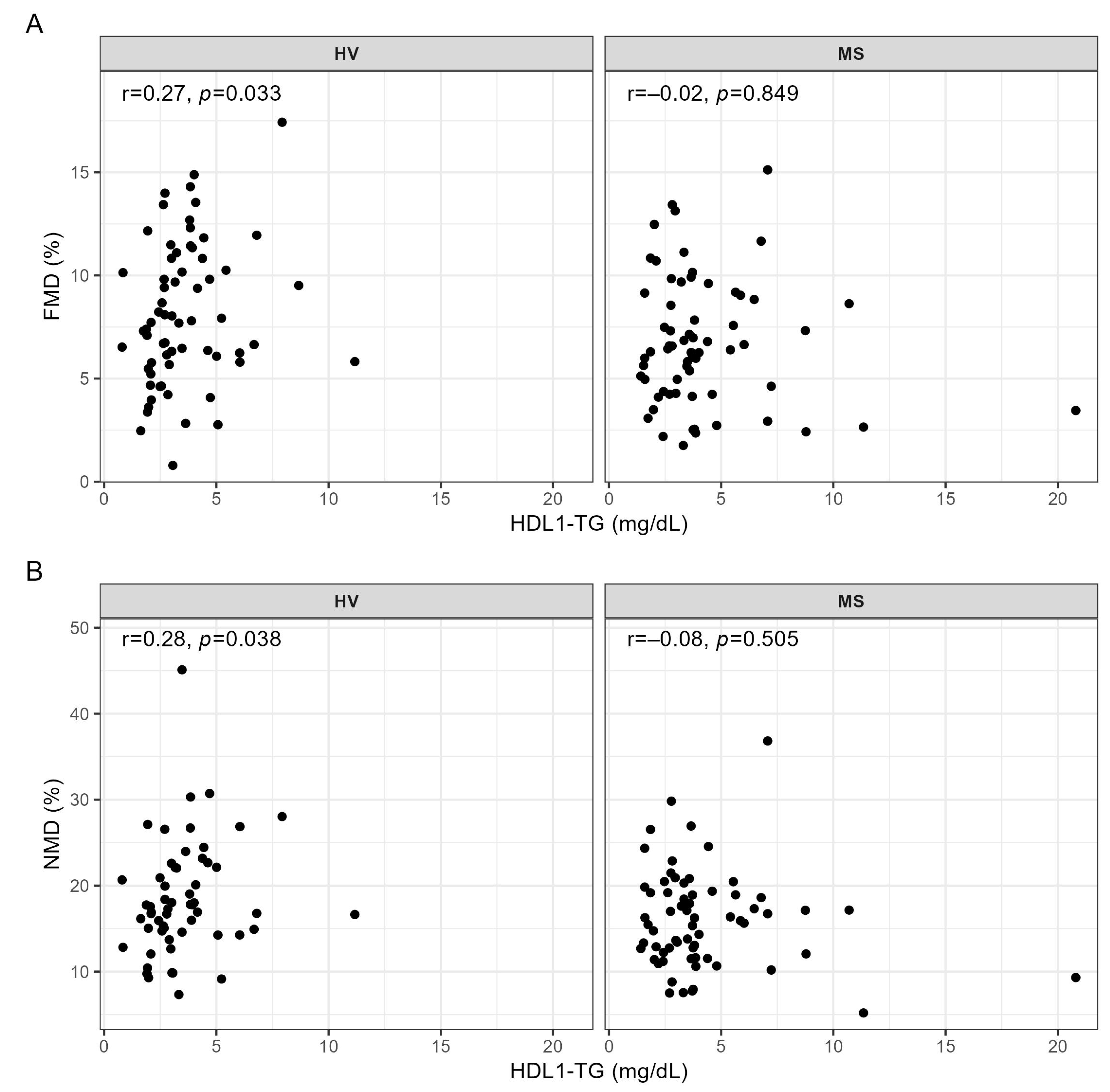
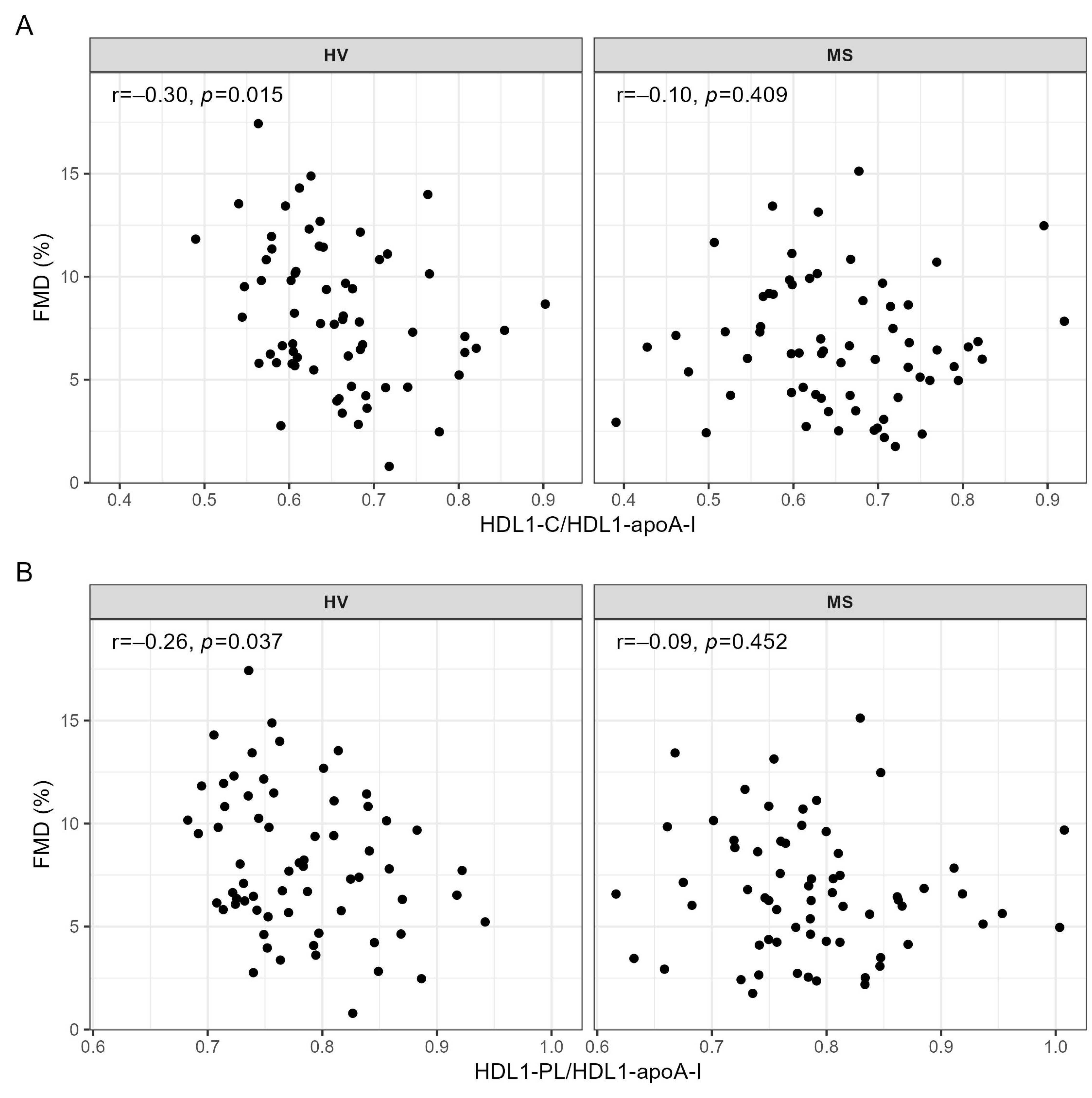
2.5. Correlation Analyses of HDL Subclasses, Lipid Content, and Function with FMD and NMD
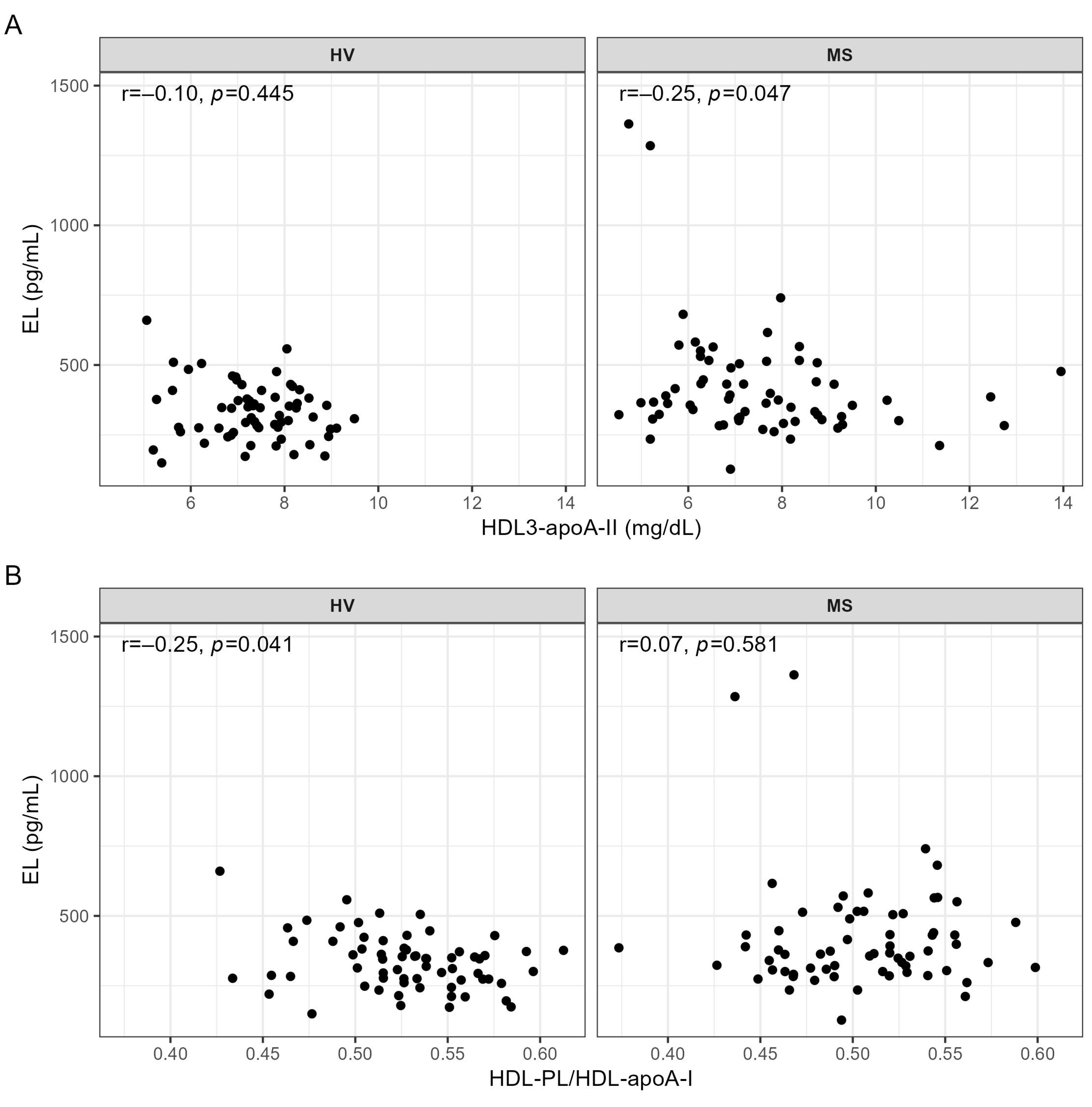
2.6. Correlation Analyses of EL with Metrics of Vessel Function, HDL Subclasses, Lipid Content, and Function
3. Discussion
4. Materials and Methods
4.1. Study Design and Participants
4.2. Laboratory Procedures
4.3. Lipoprotein Profiling Using Nuclear Magnetic Resonance (NMR) Spectroscopy
4.4. Metrics of HDL Function
4.5. Brachial Artery Function Assessment
4.6. Sample Size Calculations
4.7. Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AE | arylesterase |
| Apo A-I | apolipoprotein A-I |
| Apo A-II | apolipoprotein A-II |
| CEC | cholesterol efflux capacity |
| EL | endothelial lipase |
| FMD | flow-mediated dilation |
| HDL | high-density lipoprotein |
| HV | healthy volunteer |
| MS | metabolic syndrome |
| NMD | nitroglycerin-mediated dilation |
| NMR | nuclear magnetic resonance |
| PL | phospholipid |
| TG | triglyceride |
References
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. FGBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanhoutte, P.M.; Shimokawa, H.; Tang, E.H.; Feletou, M. Endothelial dysfunction and vascular disease. Acta. Physiol. 2009, 196, 193–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davignon, J.; Ganz, P. Role of endothelial dysfunction in atherosclerosis. Circulation 2004, 109 (Suppl. 1), III-27–III-32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Horke, S.; Forstermann, U. Vascular oxidative stress, nitric oxide and atherosclerosis. Atherosclerosis 2014, 237, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Poredos, P.; Jezovnik, M.K. Testing endothelial function and its clinical relevance. J. Atheroscler. Thromb. 2013, 20, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Rosenson, R.S.; Brewer, H.B., Jr.; Ansell, B.J.; Barter, P.; Chapman, M.J.; Heinecke, J.W.; Kontush, A.; Tall, A.R.; Webb, N.R. Dysfunctional HDL and atherosclerotic cardiovascular disease. Nat. Rev. Cardiol. 2016, 13, 48–60. [Google Scholar] [CrossRef]
- Kratzer, A.; Giral, H.; Landmesser, U. High-density lipoproteins as modulators of endothelial cell functions: Alterations in patients with coronary artery disease. Cardiovasc. Res. 2014, 103, 350–361. [Google Scholar] [CrossRef] [Green Version]
- Rohatgi, A.; Westerterp, M.; von Eckardstein, A.; Remaley, A.; Rye, K.A. HDL in the 21st Century: A Multifunctional Roadmap for Future HDL Research. Circulation 2021, 143, 2293–2309. [Google Scholar] [CrossRef]
- Jaye, M.; Lynch, K.J.; Krawiec, J.; Marchadier, D.; Maugeais, C.; Doan, K.; South, V.; Amin, D.; Perrone, M.; Rader, D.J. A novel endothelial-derived lipase that modulates HDL metabolism. Nat. Genet. 1999, 21, 424–428. [Google Scholar] [CrossRef]
- Ishida, T.; Choi, S.; Kundu, R.K.; Hirata, K.; Rubin, E.M.; Cooper, A.D.; Quertermous, T. Endothelial lipase is a major determinant of HDL level. J. Clin. Investig. 2003, 111, 347–355. [Google Scholar] [CrossRef]
- Edmondson, A.C.; Brown, R.J.; Kathiresan, S.; Cupples, L.A.; Demissie, S.; Manning, A.K.; Jensen, M.K.; Rimm, E.B.; Wang, J.; Rodrigues, A.; et al. Loss-of-function variants in endothelial lipase are a cause of elevated HDL cholesterol in humans. J. Clin. Investig. 2009, 119, 1042–1050. [Google Scholar] [CrossRef] [Green Version]
- Singaraja, R.R.; Sivapalaratnam, S.; Hovingh, K.; Dube, M.P.; Castro-Perez, J.; Collins, H.L.; Adelman, S.J.; Riwanto, M.; Manz, J.; Hubbard, B.; et al. The impact of partial and complete loss-of-function mutations in endothelial lipase on high-density lipoprotein levels and functionality in humans. Circ. Cardiovasc. Genet. 2013, 6, 54–62. [Google Scholar] [CrossRef] [Green Version]
- Gauster, M.; Oskolkova, O.V.; Innerlohinger, J.; Glatter, O.; Knipping, G.; Frank, S. Endothelial lipase-modified high-density lipoprotein exhibits diminished ability to mediate SR-BI (scavenger receptor B type I)-dependent free-cholesterol efflux. Biochem. J. 2004, 382 Pt 1, 75–82. [Google Scholar] [CrossRef] [Green Version]
- Radulovic, S.; Gottschalk, B.; Horl, G.; Zardoya-Laguardia, P.; Schilcher, I.; Hallstrom, S.; Vujic, N.; Schmidt, K.; Trieb, M.; Graier, W.F.; et al. Endothelial lipase increases eNOS activating capacity of high-density lipoprotein. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2020, 1865, 158612. [Google Scholar] [CrossRef]
- Schilcher, I.; Kern, S.; Hrzenjak, A.; Eichmann, T.O.; Stojakovic, T.; Scharnagl, H.; Duta-Mare, M.; Kratky, D.; Marsche, G.; Frank, S. Impact of Endothelial Lipase on Cholesterol Efflux Capacity of Serum and High-density Lipoprotein. Sci. Rep. 2017, 7, 12485. [Google Scholar] [CrossRef] [Green Version]
- Schilcher, I.; Ledinski, G.; Radulovic, S.; Hallstrom, S.; Eichmann, T.; Madl, T.; Zhang, F.; Leitinger, G.; Kolb-Lenz, D.; Darnhofer, B.; et al. Endothelial lipase increases antioxidative capacity of high-density lipoprotein. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2019, 1864, 1363–1374. [Google Scholar] [CrossRef]
- Schilcher, I.; Stadler, J.T.; Lechleitner, M.; Hrzenjak, A.; Berghold, A.; Pregartner, G.; Lhomme, M.; Holzer, M.; Korbelius, M.; Reichmann, F.; et al. Endothelial Lipase Modulates Paraoxonase 1 Content and Arylesterase Activity of HDL. Int. J. Mol. Sci. 2021, 22, 719. [Google Scholar] [CrossRef]
- Abbott, R.D.; Wilson, P.W.; Kannel, W.B.; Castelli, W.P. High density lipoprotein cholesterol, total cholesterol screening, and myocardial infarction. The Framingham Study. Arteriosclerosis 1988, 8, 207–211. [Google Scholar] [CrossRef] [Green Version]
- Fornoni, A.; Raij, L. Metabolic syndrome and endothelial dysfunction. Curr. Hypertens. Rep. 2005, 7, 88–95. [Google Scholar] [CrossRef]
- Badellino, K.O.; Wolfe, M.L.; Reilly, M.P.; Rader, D.J. Endothelial lipase concentrations are increased in metabolic syndrome and associated with coronary atherosclerosis. PLoS Med. 2006, 3, e22. [Google Scholar] [CrossRef]
- Denimal, D.; Monier, S.; Brindisi, M.C.; Petit, J.M.; Bouillet, B.; Nguyen, A.; Demizieux, L.; Simoneau, I.; Pais de Barros, J.P.; Verges, B.; et al. Impairment of the Ability of HDL From Patients with Metabolic Syndrome but without Diabetes Mellitus to Activate eNOS: Correction by S1P Enrichment. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 804–811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Potocnjak, I.; Trbusic, M.; Teresak, S.D.; Radulovic, B.; Pregartner, G.; Berghold, A.; Tiran, B.; Marsche, G.; Degoricija, V.; Frank, S. Metabolic Syndrome Modulates Association between Endothelial Lipase and Lipid/Lipoprotein Plasma Levels in Acute Heart Failure Patients. Sci. Rep. 2017, 7, 1165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuhanna, I.S.; Zhu, Y.; Cox, B.E.; Hahner, L.D.; Osborne-Lawrence, S.; Lu, P.; Marcel, Y.L.; Anderson, R.G.; Mendelsohn, M.E.; Hobbs, H.H.; et al. High-density lipoprotein binding to scavenger receptor-BI activates endothelial nitric oxide synthase. Nat. Med. 2001, 7, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Vanhoutte, P.M.; Zhao, Y.; Xu, A.; Leung, S.W. Thirty Years of Saying NO: Sources, Fate, Actions, and Misfortunes of the Endothelium-Derived Vasodilator Mediator. Circ. Res. 2016, 119, 375–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Besler, C.; Luscher, T.F.; Landmesser, U. Molecular mechanisms of vascular effects of High-density lipoprotein: Alterations in cardiovascular disease. EMBO Mol. Med. 2012, 4, 251–268. [Google Scholar] [CrossRef] [Green Version]
- Spieker, L.E.; Sudano, I.; Hurlimann, D.; Lerch, P.G.; Lang, M.G.; Binggeli, C.; Corti, R.; Ruschitzka, F.; Luscher, T.F.; Noll, G. High-density lipoprotein restores endothelial function in hypercholesterolemic men. Circulation 2002, 105, 1399–1402. [Google Scholar] [CrossRef] [Green Version]
- Li, X.P.; Zhao, S.P.; Zhang, X.Y.; Liu, L.; Gao, M.; Zhou, Q.C. Protective effect of high density lipoprotein on endothelium-dependent vasodilatation. Int. J. Cardiol. 2000, 73, 231–236. [Google Scholar] [CrossRef]
- Zeiher, A.M.; Schachlinger, V.; Hohnloser, S.H.; Saurbier, B.; Just, H. Coronary atherosclerotic wall thickening and vascular reactivity in humans. Elevated high-density lipoprotein levels ameliorate abnormal vasoconstriction in early atherosclerosis. Circulation 1994, 89, 2525–2532. [Google Scholar] [CrossRef] [Green Version]
- Hermann, F.; Enseleit, F.; Spieker, L.E.; Periat, D.; Sudano, I.; Hermann, M.; Corti, R.; Noll, G.; Ruschitzka, F.; Luscher, T.F. Cholesterylestertransfer protein inhibition and endothelial function in type II hyperlipidemia. Thromb. Res. 2009, 123, 460–465. [Google Scholar] [CrossRef]
- Benjo, A.M.; Maranhao, R.C.; Coimbra, S.R.; Andrade, A.C.; Favarato, D.; Molina, M.S.; Brandizzi, L.I.; da Luz, P.L. Accumulation of chylomicron remnants and impaired vascular reactivity occur in subjects with isolated low HDL cholesterol: Effects of niacin treatment. Atherosclerosis 2006, 187, 116–122. [Google Scholar] [CrossRef]
- Kuvin, J.T.; Patel, A.R.; Sidhu, M.; Rand, W.M.; Sliney, K.A.; Pandian, N.G.; Karas, R.H. Relation between high-density lipoprotein cholesterol and peripheral vasomotor function. Am. J. Cardiol. 2003, 92, 275–279. [Google Scholar] [CrossRef]
- Carvalho, L.S.; Panzoldo, N.; Santos, S.N.; Modolo, R.; Almeida, B.; Quinaglia, E.S.J.C.; Nadruz, W., Jr.; de Faria, E.C.; Sposito, A.C.; Brasilia Heart Study Group. HDL levels and oxidizability during myocardial infarction are associated with reduced endothelial-mediated vasodilation and nitric oxide bioavailability. Atherosclerosis 2014, 237, 840–846. [Google Scholar] [CrossRef]
- Chiesa, S.T.; Charakida, M.; McLoughlin, E.; Nguyen, H.C.; Georgiopoulos, G.; Motran, L.; Elia, Y.; Marcovecchio, M.L.; Dunger, D.B.; Dalton, R.N.; et al. Elevated high-density lipoprotein in adolescents with Type 1 diabetes is associated with endothelial dysfunction in the presence of systemic inflammation. Eur. Heart J. 2019, 40, 3559–3566. [Google Scholar] [CrossRef] [Green Version]
- Verwer, B.J.; Scheffer, P.G.; Vermue, R.P.; Pouwels, P.J.; Diamant, M.; Tushuizen, M.E. NAFLD is related to Post-prandial Triglyceride-enrichment of HDL Particles in Association with Endothelial and HDL Dysfunction. Liver Int. 2020, 40, 2439–2444. [Google Scholar] [CrossRef]
- Vigna, G.B.; Satta, E.; Bernini, F.; Boarini, S.; Bosi, C.; Giusto, L.; Pinotti, E.; Tarugi, P.; Vanini, A.; Volpato, S.; et al. Flow-mediated dilation, carotid wall thickness and HDL function in subjects with hyperalphalipoproteinemia. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 777–783. [Google Scholar] [CrossRef]
- Samsamshariat, S.Z.A.; Sakhaei, F.; Salehizadeh, L.; Keshvari, M.; Asgary, S. Relationship between Resistin, Endothelin-1, and Flow-Mediated Dilation in Patient with and without Metabolic Syndrome. Adv. Biomed. Res. 2019, 8, 16. [Google Scholar]
- Mineo, C.; Yuhanna, I.S.; Quon, M.J.; Shaul, P.W. High density lipoprotein-induced endothelial nitric-oxide synthase activation is mediated by Akt and MAP kinases. J. Biol. Chem. 2003, 278, 9142–9149. [Google Scholar] [CrossRef] [Green Version]
- Mineo, C.; Shaul, P.W. Novel biological functions of high-density lipoprotein cholesterol. Circ. Res. 2012, 111, 1079–1090. [Google Scholar] [CrossRef] [Green Version]
- Rothblat, G.H.; de la Llera-Moya, M.; Atger, V.; Kellner-Weibel, G.; Williams, D.L.; Phillips, M.C. Cell cholesterol efflux: Integration of old and new observations provides new insights. J. Lipid Res. 1999, 40, 781–796. [Google Scholar] [CrossRef]
- Yancey, P.G.; Kawashiri, M.A.; Moore, R.; Glick, J.M.; Williams, D.L.; Connelly, M.A.; Rader, D.J.; Rothblat, G.H. In vivo modulation of HDL phospholipid has opposing effects on SR-BI- and ABCA1-mediated cholesterol efflux. J. Lipid Res. 2004, 45, 337–346. [Google Scholar] [CrossRef] [Green Version]
- Kozina, A.; Opresnik, S.; Wong, M.S.; Hallstrom, S.; Graier, W.F.; Malli, R.; Schroder, K.; Schmidt, K.; Frank, S. Oleoyl-lysophosphatidylcholine limits endothelial nitric oxide bioavailability by induction of reactive oxygen species. PLoS ONE 2014, 9, e113443. [Google Scholar] [CrossRef] [PubMed]
- deLemos, A.S.; Wolfe, M.L.; Long, C.J.; Sivapackianathan, R.; Rader, D.J. Identification of genetic variants in endothelial lipase in persons with elevated high-density lipoprotein cholesterol. Circulation 2002, 106, 1321–1326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishida, T.; Miyashita, K.; Shimizu, M.; Kinoshita, N.; Mori, K.; Sun, L.; Yasuda, T.; Imamura, S.; Nakajima, K.; Stanhope, K.L.; et al. ELISA system for human endothelial lipase. Clin. Chem. 2012, 58, 1656–1664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kilic, H.; Atalar, E.; Lay, I.; Yazihan, N.; Buyukcam, F.; Saygisunar, U.; Aksoy, M.; Gunduz, H.; Akdemir, R. High-density lipoprotein subfractions and influence of endothelial lipase in a healthy Turkish population: A study in a land of low high-density lipoprotein cholesterol. Scand. J. Clin. Lab. Investig. 2014, 74, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Broedl, U.C.; Jin, W.; Fuki, I.V.; Millar, J.S.; Rader, D.J. Endothelial lipase is less effective at influencing HDL metabolism in vivo in mice expressing apoA-II. J. Lipid Res. 2006, 47, 2191–2197. [Google Scholar] [CrossRef] [Green Version]
- Gauster, M.; Rechberger, G.; Sovic, A.; Horl, G.; Steyrer, E.; Sattler, W.; Frank, S. Endothelial lipase releases saturated and unsaturated fatty acids of high density lipoprotein phosphatidylcholine. J. Lipid Res. 2005, 46, 1517–1525. [Google Scholar] [CrossRef] [Green Version]
- Hirata, K.; Dichek, H.L.; Cioffi, J.A.; Choi, S.Y.; Leeper, N.J.; Quintana, L.; Kronmal, G.S.; Cooper, A.D.; Quertermous, T. Cloning of a unique lipase from endothelial cells extends the lipase gene family. J. Biol. Chem. 1999, 274, 14170–14175. [Google Scholar] [CrossRef] [Green Version]
- Miksztowicz, V.; Schreier, L.; McCoy, M.; Lucero, D.; Fassio, E.; Billheimer, J.; Rader, D.J.; Berg, G. Role of SN1 lipases on plasma lipids in metabolic syndrome and obesity. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 669–675. [Google Scholar] [CrossRef] [Green Version]
- Moise, L.G.; Marta, D.S.; Rascu, A.; Moldoveanu, E. Serum Lipoprotein-Associated Phospholipase A2 in Males with Metabolic Syndrome and Obstructive Sleep Apnea. Acta Endocrinol. (Buchar.) 2018, 14, 36–42. [Google Scholar] [CrossRef]
- Kuefner, M.S. Secretory Phospholipase A2s in Insulin Resistance and Metabolism. Front. Endocrinol. 2021, 12, 732726. [Google Scholar] [CrossRef]
- Stadler, J.T.; Lackner, S.; Morkl, S.; Trakaki, A.; Scharnagl, H.; Borenich, A.; Wonisch, W.; Mangge, H.; Zelzer, S.; Meier-Allard, N.; et al. Obesity Affects HDL Metabolism, Composition and Subclass Distribution. Biomedicines. 2021, 9, 242. [Google Scholar] [CrossRef]
- Jin, W.; Wang, X.; Millar, J.S.; Quertermous, T.; Rothblat, G.H.; Glick, J.M.; Rader, D.J. Hepatic proprotein convertases modulate HDL metabolism. Cell Metab. 2007, 6, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Sylvers-Davie, K.L.; Davies, B.S.J. Regulation of lipoprotein metabolism by ANGPTL3, ANGPTL4, and ANGPTL8. Am. J. Physiol. Endocrinol. Metab. 2021, 321, E493–E508. [Google Scholar] [CrossRef]
- Gauster, M.; Hrzenjak, A.; Schick, K.; Frank, S. Endothelial lipase is inactivated upon cleavage by the members of the proprotein convertase family. J. Lipid Res. 2005, 46, 977–987. [Google Scholar] [CrossRef] [Green Version]
- Le Lay, J.E.; Du, Q.; Mehta, M.B.; Bhagroo, N.; Hummer, B.T.; Falloon, J.; Carlson, G.; Rosenbaum, A.I.; Jin, C.; Kimko, H.; et al. Blocking endothelial lipase with monoclonal antibody MEDI5884 durably increases high density lipoprotein in nonhuman primates and in a phase 1 trial. Sci. Transl. Med. 2021, 13, eabb0602. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Warnick, G.R.; Knopp, R.H.; Fitzpatrick, V.; Branson, L. Estimating low-density lipoprotein cholesterol by the Friedewald equation is adequate for classifying patients on the basis of nationally recommended cutpoints. Clin. Chem. 1990, 36, 15–19. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Klobucar, I.; Degoricija, V.; Potocnjak, I.; Trbusic, M.; Pregartner, G.; Berghold, A.; Fritz-Petrin, E.; Habisch, H.; Madl, T.; Frank, S. HDL-apoA-II Is Strongly Associated with 1-Year Mortality in Acute Heart Failure Patients. Biomedicines 2022, 10, 1668. [Google Scholar] [CrossRef]
- Khera, A.V.; Cuchel, M.; de la Llera-Moya, M.; Rodrigues, A.; Burke, M.F.; Jafri, K.; French, B.C.; Phillips, J.A.; Mucksavage, M.L.; Wilensky, R.L.; et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N. Engl. J. Med. 2011, 364, 127–135. [Google Scholar] [CrossRef] [Green Version]
- Marsche, G.; Zelzer, S.; Meinitzer, A.; Kern, S.; Meissl, S.; Pregartner, G.; Weghuber, D.; Almer, G.; Mangge, H. Adiponectin Predicts High-Density Lipoprotein Cholesterol Efflux Capacity in Adults Irrespective of Body Mass Index and Fat Distribution. J. Clin. Endocrinol. Metab. 2017, 102, 4117–4123. [Google Scholar] [CrossRef] [PubMed]
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J.; Celermajer, D.; Charbonneau, F.; Creager, M.A.; Deanfield, J.; Drexler, H.; Gerhard-Herman, M.; Herrington, D.; et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greyling, A.; van Mil, A.C.; Zock, P.L.; Green, D.J.; Ghiadoni, L.; Thijssen, D.H.; TIFN International Working Group on Flow Mediated Dilation. Adherence to guidelines strongly improves reproducibility of brachial artery flow-mediated dilation. Atherosclerosis 2016, 248, 196–202. [Google Scholar] [CrossRef] [Green Version]
- Thijssen, D.H.; Black, M.A.; Pyke, K.E.; Padilla, J.; Atkinson, G.; Harris, R.A.; Parker, B.; Widlansky, M.E.; Tschakovsky, M.E.; Green, D.J. Assessment of flow-mediated dilation in humans: A methodological and physiological guideline. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H2–H12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coolbaugh, C.L.; Bush, E.C.; Caskey, C.F.; Damon, B.M.; Towse, T.F. FloWave.US: Validated, open-source, and flexible software for ultrasound blood flow analysis. J. Appl. Physiol. 2016, 121, 849–857. [Google Scholar] [CrossRef]
| Variable | All (N = 130) | HV (N = 65) | MS (N = 65) | p |
|---|---|---|---|---|
| Age (years) | 56.0 (50.0, 60.0) | 56.0 (50.0, 59.0) | 57.0 (50.0, 60.0) | 0.440 |
| Sex (female) | 62 (47.7%) | 31 (47.7%) | 31 (47.7%) | 1.000 |
| Body weight (kg) | 87.5 (75.2, 102.8) | 77.0 (68.0, 88.0) | 98.0 (86.0, 113.5) | <0.001 |
| Body height (m) | 1.74 ± 0.10 | 1.75 ± 0.10 | 1.73 ± 0.11 | 0.243 |
| BMI (kg/m2) | 28.8 (25.1, 32.7) | 25.1 (23.7, 28.1) | 32.6 (29.8, 35.9) | <0.001 |
| Waist circumference (cm) | 103.1 ± 16.5 | 92.2 ± 11.6 | 113.9 ± 13.2 | <0.001 |
| Chronic diseases | ||||
| Arterial hypertension | 60 (46.2%) | 0 (0.0%) | 60 (92.3%) | <0.001 |
| Diabetes mellitus type 2 | 27 (20.8%) | 0 (0.0%) | 27 (41.5%) | <0.001 |
| Stable angina pectoris | 2 (1.5%) | 0 (0.0%) | 2 (3.1%) | 0.496 |
| Atrial fibrillation | 2 (1.5%) | 0 (0.0%) | 2 (3.1%) | 0.496 |
| CVI, TIA | 1 (0.8%) | 0 (0.0%) | 1 (1.5%) | 1.000 |
| Intermittent claudications | 4 (3.1%) | 0 (0.0%) | 4 (6.2%) | 0.119 |
| Deep venous thrombosis | 6 (4.6%) | 1 (1.5%) | 5 (7.7%) | 0.208 |
| Pulmonary embolism | 2 (1.5%) | 0 (0.0%) | 2 (3.1%) | 0.496 |
| Functions and habits | ||||
| Smoking | 34 (26.2%) | 16 (24.6%) | 18 (27.7%) | 0.842 |
| Physical activity (≥3 times/week) | 105 (80.8%) | 58 (89.2%) | 47 (72.3%) | 0.025 |
| Menstrual cycle (female) | 18/62 (29.0%) | 12/31 (38.7%) | 6/31 (19.4%) | 0.161 |
| Variable | All (N = 130) | HV (N = 65) | MS (N = 65) | p |
|---|---|---|---|---|
| EL (pg/mL) | 353.6 (285.0, 431.2) | 345.2 (272.1, 382.9) | 367.1 (305.4, 497.0) | 0.002 |
| Triglycerides (mmol/L) | 1.3 (0.9, 1.9) | 1.0 (0.8, 1.4) | 1.6 (1.1, 2.2) | <0.001 |
| Total cholesterol (mmol/L) | 5.3 (4.7, 6.1) | 5.5 (5.1, 6.0) | 5.0 (4.3, 6.2) | 0.057 |
| LDL-C (mmol/L) | 3.2 (2.5, 3.7) | 3.3 (2.8, 3.7) | 3.0 (2.3, 3.7) | 0.077 |
| HDL-C (mmol/L) | 1.4 (1.1, 1.7) | 1.6 (1.4, 1.8) | 1.2 (1.0, 1.4) | <0.001 |
| Glucose (mmol/L) | 5.3 (4.9, 5.7) | 4.9 (4.8, 5.2) | 5.7 (5.3, 6.5) | <0.001 |
| Protein (g/L) | 73.0 (70.0, 76.0) | 72.0 (69.0, 75.0) | 75.0 (71.0, 77.0) | 0.002 |
| Albumin (g/L) | 48.0 (46.0, 49.0) | 47.0 (46.0, 49.0) | 48.0 (45.0, 49.0) | 0.465 |
| CRP (µg/mL) | 1.8 (0.8, 3.7) | 1.2 (0.6, 2.3) | 2.4 (1.2, 5.5) | <0.001 |
| IL-6 (pg/mL) | 3.0 (2.1, 5.3) | 2.3 (1.7, 3.0) | 4.1 (2.7, 6.8) | <0.001 |
| Bilirubin (µmol/L) | 8.5 (6.0, 11.6) | 9.6 (7.4, 13.3) | 7.4 (5.5, 10.4) | 0.012 |
| AST (U/L) | 23.0 (20.0, 27.0) | 23.0 (20.0, 25.0) | 23.0 (19.0, 32.0) | 0.244 |
| ALT (U/L) | 24.0 (19.0, 36.0) | 22.0 (18.0, 29.0) | 30.0 (22.0, 43.0) | <0.001 |
| AP (U/L) | 61.0 (51.0, 73.0) | 60.0 (49.0, 70.0) | 65.0 (52.0, 81.0) | 0.065 |
| GGT (U/L) | 24.5 (15.2, 38.0) | 16.0 (13.0, 30.0) | 31.0 (21.0, 44.0) | <0.001 |
| CK (U/L) | 124.5 (83.0, 186.8) | 115.0 (81.0, 153.0) | 133.0 (86.0, 226.0) | 0.048 |
| LDH (U/L) | 172.0 (150.5, 192.0) | 168.0 (147.0, 191.0) | 176.0 (158.0, 193.0) | 0.365 |
| Urea (mmol/L) | 5.3 (4.5, 6.3) | 5.0 (4.2, 6.0) | 5.6 (4.8, 6.5) | 0.004 |
| Urate (µmol/L) | 297.5 (249.9, 345.1) | 273.7 (232.0, 327.2) | 315.3 (279.7, 362.9) | <0.001 |
| Creatinine (µmol/L) | 77.9 (67.3, 87.6) | 77.9 (69.0, 89.4) | 76.6 (65.5, 87.0) | 0.414 |
| eGFR (mL/min/1.73 m2) | 88.0 (78.0, 97.1) | 87.5 (77.2, 93.6) | 88.9 (79.1, 98.0) | 0.358 |
| Sodium (mmol/L) | 139.0 (138.0, 141.0) | 140.0 (138.0, 141.0) | 139.0 (138.0, 140.0) | 0.041 |
| Potassium (mmol/L) | 4.2 (4.1, 4.6) | 4.3 (4.1, 4.5) | 4.2 (4.1, 4.6) | 0.703 |
| Chloride (mmol/L) | 100.0 (98.2, 102.8) | 101.0 (99.0, 103.0) | 100.0 (98.0, 101.0) | 0.006 |
| Variable (mg/dL) | All (N = 130) | HV (N = 65) | MS (N = 65) | p |
|---|---|---|---|---|
| HDL-C | 58.6 (51.3, 69.2) | 65.2 (57.7, 74.5) | 52.7 (47.9, 60.6) | <0.001 |
| HDL1-C | 17.2 (13.8, 22.5) | 18.4 (15.1, 26.8) | 15.7 (12.9, 20.1) | 0.001 |
| HDL2-C | 8.6 (7.5, 10.2) | 9.5 (8.3, 12.6) | 8.2 (7.3, 9.7) | 0.001 |
| HDL3-C | 11.2 (10.0, 13.2) | 12.2 (10.7, 13.6) | 10.4 (9.6, 11.9) | <0.001 |
| HDL4-C | 20.5 (17.2, 23.9) | 22.3 (18.2, 24.7) | 19.0 (16.0, 22.7) | 0.001 |
| HDL-TG | 10.5 (9.0, 13.3) | 9.9 (8.7, 11.8) | 11.4 (9.7, 13.6) | 0.006 |
| HDL1-TG | 3.3 (2.6, 4.4) | 3.0 (2.5, 4.2) | 3.6 (2.7, 4.6) | 0.326 |
| HDL2-TG | 1.8 (1.5, 2.3) | 1.6 (1.3, 2.1) | 2.0 (1.6, 2.5) | 0.001 |
| HDL3-TG | 2.3 (1.9, 2.8) | 2.1 (1.7, 2.5) | 2.7 (2.1, 3.1) | <0.001 |
| HDL4-TG | 3.6 (3.0, 4.3) | 3.4 (2.5, 3.9) | 3.7 (3.3, 4.7) | <0.001 |
| HDL-PL | 81.9 (72.1, 93.2) | 89.4 (79.2, 99.8) | 77.1 (67.5, 84.5) | <0.001 |
| HDL1-PL | 20.5 (16.8, 26.5) | 22.1 (18.6, 33.9) | 18.9 (14.8, 22.9) | 0.002 |
| HDL2-PL | 13.8 (11.7, 15.9) | 14.4 (12.6, 18.6) | 13.2 (10.9, 15.4) | 0.017 |
| HDL3-PL | 18.2 (15.9, 20.6) | 19.1 (17.4, 20.9) | 17.1 (15.2, 19.6) | 0.004 |
| HDL4-PL | 28.8 (25.4, 31.8) | 29.9 (26.4, 32.7) | 26.3 (23.1, 30.7) | 0.003 |
| HDL-apoA-I | 159.3 (144.5, 178.2) | 167.8 (155.7, 183.7) | 149.2 (138.1, 166.2) | <0.001 |
| HDL1-apoA-I | 26.3 (20.0, 34.7) | 27.5 (22.3, 45.4) | 24.9 (18.5, 30.1) | 0.007 |
| HDL2-apoA-I | 18.7 (16.3, 22.1) | 19.6 (17.2, 23.3) | 17.5 (15.2, 20.6) | 0.004 |
| HDL3-apoA-I | 30.2 (26.7, 33.3) | 30.8 (27.5, 33.5) | 28.8 (24.9, 32.5) | 0.040 |
| HDL4-apoA-I | 79.5 (70.8, 89.0) | 81.9 (72.7, 91.1) | 75.5 (68.3, 86.5) | 0.023 |
| HDL-apoA-II | 35.2 (32.2, 38.4) | 36.0 (33.6, 38.6) | 33.8 (31.5, 37.5) | 0.039 |
| HDL1-apoA-II | 2.4 (1.9, 3.5) | 2.5 (2.1, 4.1) | 2.1 (1.6, 3.0) | 0.006 |
| HDL2-apoA-II | 3.9 (3.2, 4.6) | 4.0 (3.5, 4.6) | 3.7 (3.0, 4.5) | 0.111 |
| HDL3-apoA-II | 7.3 (6.5, 8.2) | 7.3 (6.9, 8.1) | 7.1 (6.3, 8.4) | 0.739 |
| HDL4-apoA-II | 19.8 (17.5, 22.6) | 20.9 (18.4, 23.2) | 19.2 (17.0, 21.9) | 0.060 |
| Variable | All (N = 130) | HV (N = 65) | MS (N = 65) | p |
|---|---|---|---|---|
| HDL-C / HDL-apoA-I | 0.37 (0.35, 0.40) | 0.39 (0.36, 0.41) | 0.36 (0.33, 0.38) | <0.001 |
| HDL1-C / HDL1-apoA-I | 0.65 (0.60, 0.71) | 0.64 (0.60, 0.69) | 0.65 (0.60, 0.72) | 0.869 |
| HDL2-C / HDL2-apoA-I | 0.48 (0.45, 0.51) | 0.49 (0.45, 0.53) | 0.47 (0.43, 0.50) | 0.011 |
| HDL3-C / HDL3-apoA-I | 0.39 (0.37, 0.40) | 0.40 (0.38, 0.41) | 0.38 (0.36, 0.39) | <0.001 |
| HDL4-C / HDL4-apoA-I | 0.26 (0.24, 0.27) | 0.26 (0.25, 0.28) | 0.24 (0.23, 0.26) | <0.001 |
| HDL-TG / HDL-apoA-I | 0.06 (0.06, 0.08) | 0.06 (0.05, 0.07) | 0.08 (0.06, 0.10) | <0.001 |
| HDL1-TG / HDL1-apoA-I | 0.12 (0.09, 0.17) | 0.11 (0.08, 0.13) | 0.15 (0.11, 0.19) | <0.001 |
| HDL2-TG / HDL2-apoA-I | 0.10 (0.08, 0.13) | 0.08 (0.07, 0.11) | 0.12 (0.09, 0.16) | <0.001 |
| HDL3-TG / HDL3-apoA-I | 0.08 (0.06, 0.10) | 0.07 (0.06, 0.08) | 0.09 (0.07, 0.12) | <0.001 |
| HDL4-TG / HDL4-apoA-I | 0.04 (0.04, 0.05) | 0.04 (0.03, 0.05) | 0.05 (0.04, 0.06) | <0.001 |
| HDL-PL / HDL-apoA-I | 0.52 (0.49, 0.54) | 0.53 (0.50, 0.55) | 0.51 (0.47, 0.54) | 0.002 |
| HDL1-PL / HDL1-apoA-I | 0.78 (0.74, 0.83) | 0.76 (0.73, 0.82) | 0.78 (0.74, 0.83) | 0.460 |
| HDL2-PL / HDL2-apoA-I | 0.74 (0.68, 0.78) | 0.73 (0.68, 0.79) | 0.74 (0.68, 0.76) | 0.694 |
| HDL3-PL / HDL3-apoA-I | 0.61 (0.60, 0.63) | 0.62 (0.60, 0.63) | 0.61 (0.59, 0.63) | 0.145 |
| HDL4-PL / HDL4-apoA-I | 0.36 (0.34, 0.37) | 0.36 (0.35, 0.37) | 0.35 (0.33, 0.37) | 0.001 |
| Variable | All (N = 129) | HV (N = 65) | MS (N = 64) | p |
|---|---|---|---|---|
| AE activity | 125.3 (104.5, 145.4) | 130.3 (107.5, 151.9) | 120.0 (102.1, 135.5) | 0.030 |
| AE activity / HDL-apoA-I | 0.76 (0.65, 0.90) | 0.74 (0.65, 0.88) | 0.77 (0.64, 0.90) | 0.614 |
| CEC | 18.3 (17.1, 19.9) | 18.8 (17.8, 20.3) | 17.5 (16.1, 19.5) | <0.001 |
| CEC / HDL-apoA-I | 0.11 (0.11, 0.12) | 0.11 (0.11, 0.12) | 0.11 (0.11, 0.12) | 0.277 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klobučar, I.; Stadler, J.T.; Klobučar, L.; Lechleitner, M.; Trbušić, M.; Pregartner, G.; Berghold, A.; Habisch, H.; Madl, T.; Marsche, G.; et al. Associations between Endothelial Lipase, High-Density Lipoprotein, and Endothelial Function Differ in Healthy Volunteers and Metabolic Syndrome Patients. Int. J. Mol. Sci. 2023, 24, 2073. https://doi.org/10.3390/ijms24032073
Klobučar I, Stadler JT, Klobučar L, Lechleitner M, Trbušić M, Pregartner G, Berghold A, Habisch H, Madl T, Marsche G, et al. Associations between Endothelial Lipase, High-Density Lipoprotein, and Endothelial Function Differ in Healthy Volunteers and Metabolic Syndrome Patients. International Journal of Molecular Sciences. 2023; 24(3):2073. https://doi.org/10.3390/ijms24032073
Chicago/Turabian StyleKlobučar, Iva, Julia T. Stadler, Lucija Klobučar, Margarete Lechleitner, Matias Trbušić, Gudrun Pregartner, Andrea Berghold, Hansjörg Habisch, Tobias Madl, Gunther Marsche, and et al. 2023. "Associations between Endothelial Lipase, High-Density Lipoprotein, and Endothelial Function Differ in Healthy Volunteers and Metabolic Syndrome Patients" International Journal of Molecular Sciences 24, no. 3: 2073. https://doi.org/10.3390/ijms24032073







