Current Concepts of Biomaterial Scaffolds and Regenerative Therapy for Spinal Cord Injury
Abstract
1. Introduction
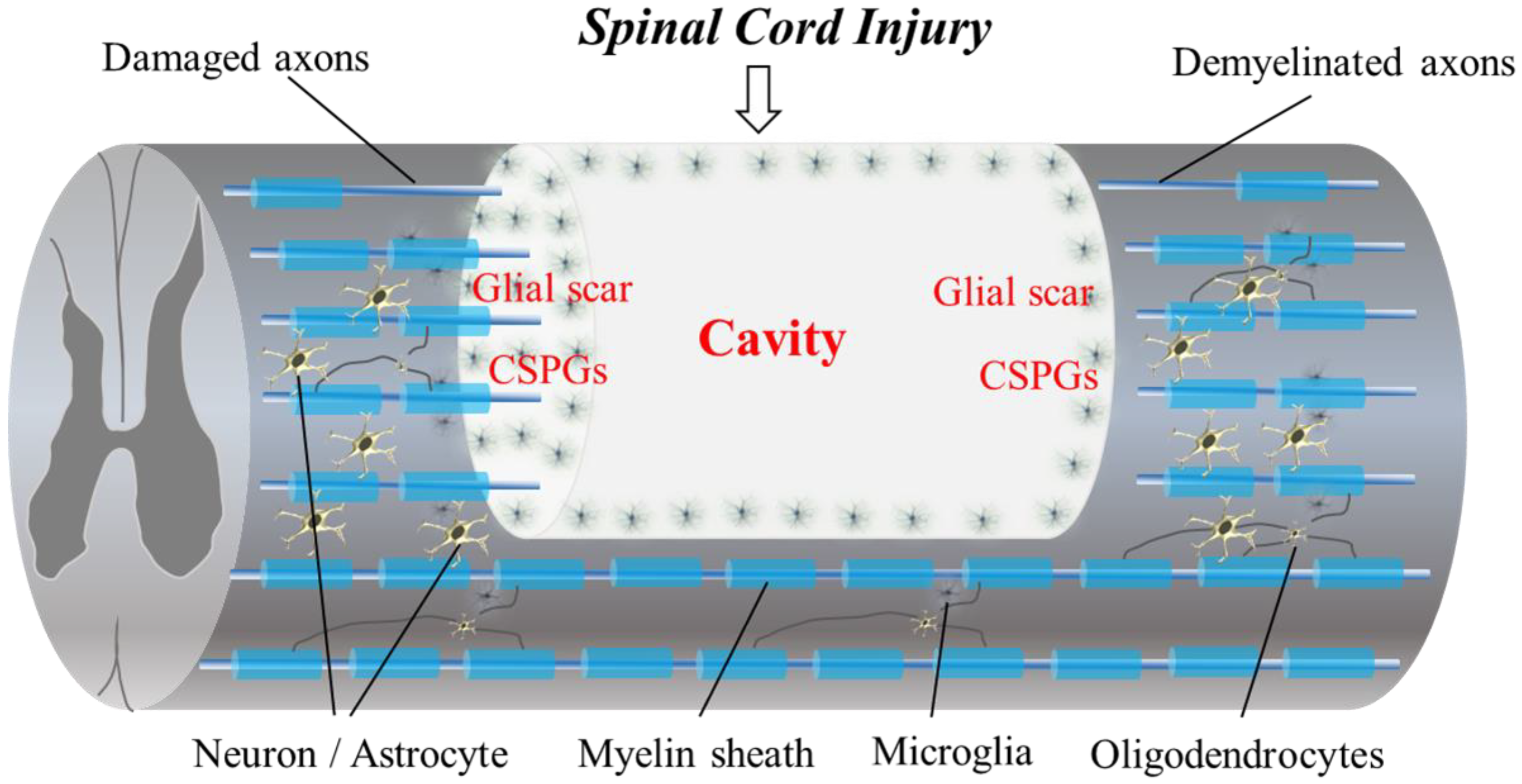
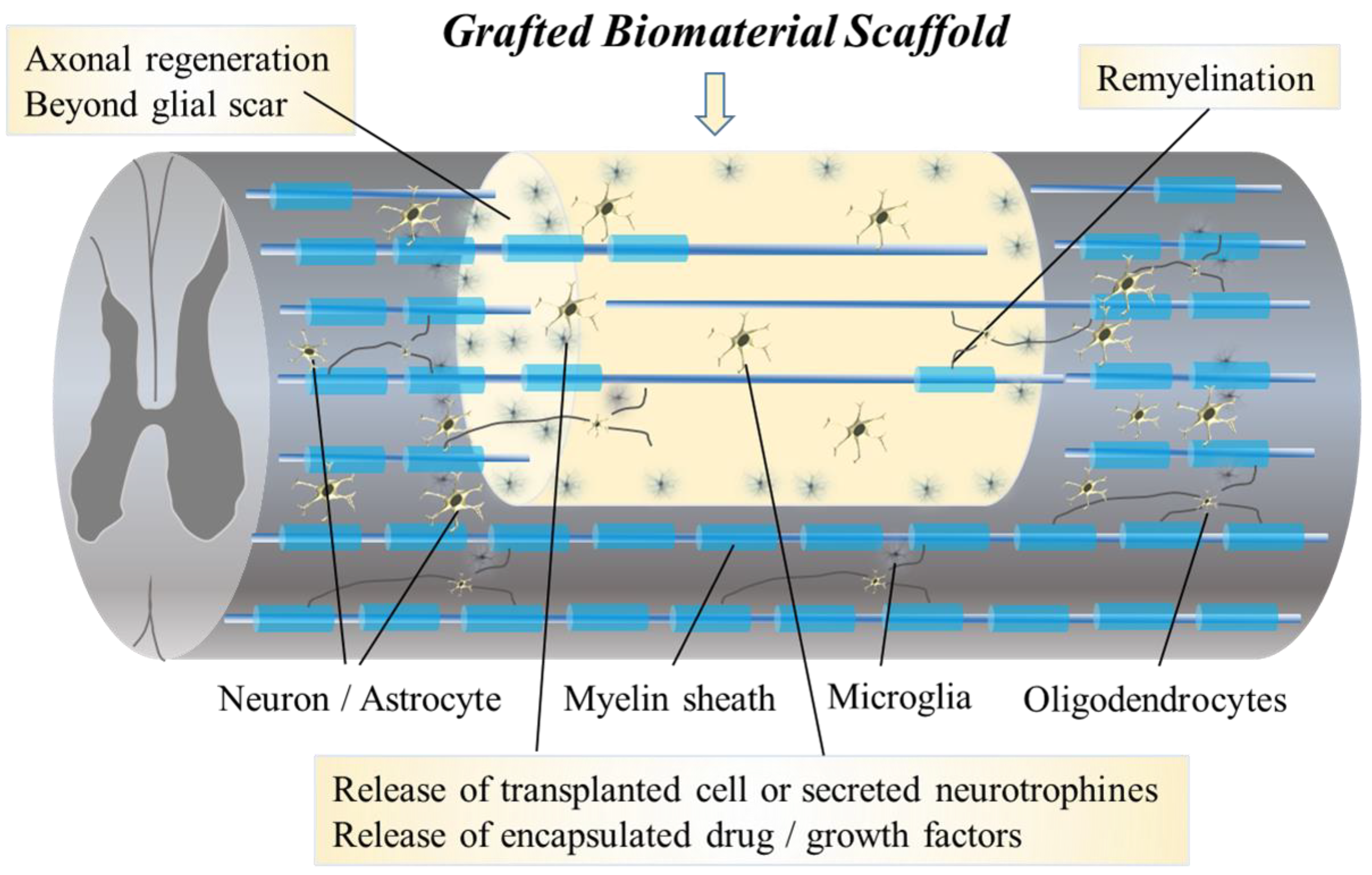
2. Barriers to Regeneration and the Pathophysiology of SCI (Figure 1)
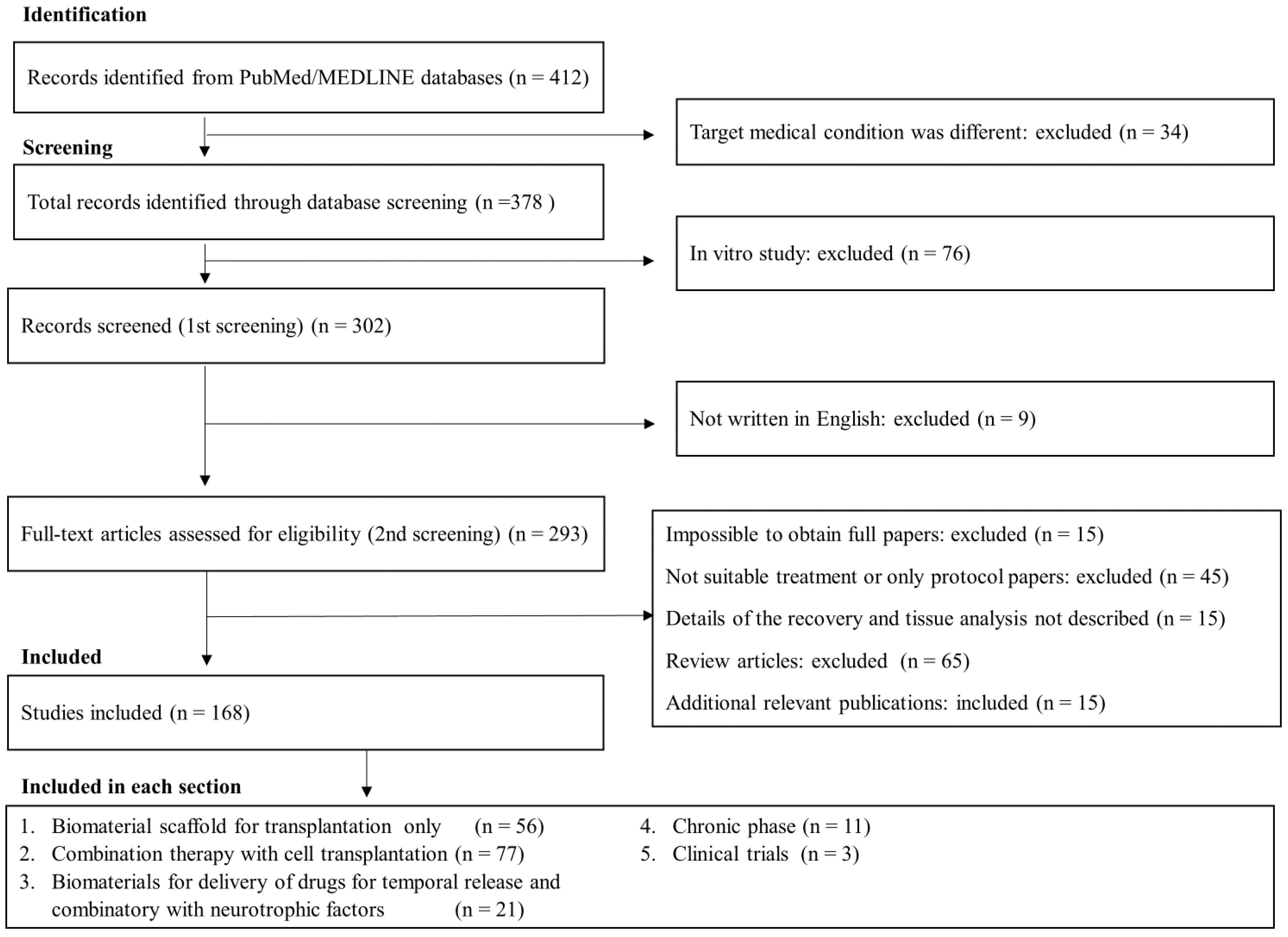
3. Systematic Review of Biomaterial Scaffolds Applied for SCI
3.1. Literature Search and Inclusion Criteria
3.2. Study Selection
3.3. Assessment of Quality and Risk of Bias
4. Categories of Biomaterial Scaffolds Applied in Regeneration Therapy for SCI
4.1. Hydrogels
4.2. Biodegradable Scaffolds
4.3. Nano- and Micro-Scale Scaffolds as Instructive Biomaterials for SCI
5. Biomaterial Scaffolds in Combinatory Treatment Used for DDSs in SCI Treatment
6. Biomaterial Scaffolds in Combinatory Treatment with Cell Therapy for SCI
6.1. Exogenous Neural Stem/Progenitor Cells and Biomaterial Scaffolds
6.2. Nanoscaffolds and Stem Cell Grafts
6.3. Mescenchymal Stem Cells (MSCs) and Biomaterial Scaffolds: Bone Marrow MSCs, Umbilical MSCs, Wharton’s Jelly-Derived MSCs and Adipose-Derived MSCs
6.4. Schwann Cells, Olfactory Ensheathing Cells, Astrocytes and Other Cell Grafts and Biomaterial Scaffolds
7. Biomaterial Scaffolds in Regeneration Therapy for Chronic SCI
8. Biomaterial Scaffolds in Clinical Trials for SCI
9. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fehlings, M.G.; Martin, A.R.; Tetreault, L.A.; Aarabi, B.; Anderson, P.; Arnold, P.M.; Brodke, D.; Burns, A.; Chiba, K.; Dettori, J.R.; et al. A clinical practice guideline for the management of patients with acute spinal cord injury: Recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Glob. Spine J. 2017, 7, 221S–230S. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Kim, K.D.; Aarabi, B.; Rizzo, M.; Bond, L.M.; McKerracher, L.; Vaccaro, A.R.; Okonkwo, D.O. Rho Inhibitor VX-210 in Acute Traumatic Subaxial Cervical Spinal Cord Injury: Design of the SPinal Cord Injury Rho INhibition InvestiGation (SPRING) Clinical Trial. J. Neurotrauma 2018, 35, 1049–1056. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A.; Fehlings, M.G. Global prevalence and incidence of traumatic spinal cord injury. Clin. Epidemiol. 2014, 6, 309–331. [Google Scholar] [CrossRef]
- Spinal Cord Injury (SCI) 2016 Facts and Figures at a Glance. J. Spinal Cord Med. 2016, 39, 493–494. [CrossRef]
- Costăchescu, B.; Niculescu, A.-G.; Dabija, M.G.; Teleanu, R.I.; Grumezescu, A.M.; Eva, L. Novel Strategies for Spinal Cord Regeneration. Int. J. Mol. Sci. 2022, 23, 4552. [Google Scholar] [CrossRef]
- Ahuja, C.S.; Fehlings, M. Concise Review: Bridging the Gap: Novel Neuroregenerative and Neuroprotective Strategies in Spinal Cord Injury. Stem Cells Transl. Med. 2016, 5, 914–924. [Google Scholar] [CrossRef]
- Zweckberger, K.; Ahuja, C.S.; Liu, Y.; Wang, J.; Fehlings, M.G. Self-assembling peptides optimize the post-traumatic milieu and synergistically enhance the effects of neural stem cell therapy after cervical spinal cord injury. Acta Biomater. 2016, 42, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, S.; Takano, M.; Numasawa-Kuroiwa, Y.; Itakura, G.; Kobayashi, Y.; Nishiyama, Y.; Sugai, K.; Nishimura, S.; Iwai, H.; Isoda, M.; et al. Grafted Human iPS Cell-Derived Oligodendrocyte Precursor Cells Contribute to Robust Remyelination of Demyelinated Axons after Spinal Cord Injury. Stem Cell Rep. 2016, 6, 1–8. [Google Scholar] [CrossRef]
- Lu, P.; Kadoya, K.; Tuszynski, M.H. Axonal growth and connectivity from neural stem cell grafts in models of spinal cord injury. Curr. Opin. Neurobiol. 2014, 27, 103–109. [Google Scholar] [CrossRef]
- Lis, A.; Szarek, D.; Laska, J. Strategie inzynierii biomateriałów dla regeneracji rdzenia kregowego: Aktualny stan wiedzy. Polym. Med. 2013, 43, 59–80. [Google Scholar]
- Imagama, T.; Ogino, K.; Takemoto, K.; Kato, Y.; Kataoka, H.; Suzuki, H.; Ran, Z.; Setiawan, H.; Fujikura, Y.; Taguchi, T. Regulation of nitric oxide generation by up-regulated arginase I in rat spinal cord injury. J. Clin. Biochem. Nutr. 2012, 51, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Murakami, T.; Kanchiku, T.; Suzuki, H.; Imajo, Y.; Yoshida, Y.; Nomura, H.; Cui, D.; Ishikawa, T.; Ikeda, E.; Taguchi, T. Anti-interleukin-6 receptor antibody reduces neuropathic pain following spinal cord injury in mice. Exp. Ther. Med. 2013, 6, 1194–1198. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Taguchi, T.; Kato, Y.; Kanchiku, T.; Imagama, T.; Yara, T.; Moriya, A.; Muramatsu, K.; Tanaka, H.; Gondo, T. Transplantation of neurospheres derived from bone marrow stromal cells promotes neurological recovery in rats with spinal cord injury. Med. Mol. Morphol. 2011, 44, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, J.T.; Satkunendrarajah, K.; Zuccato, J.A.; Nassiri, F.; Fehlings, M.G. Neural Precursor Cell Transplantation Enhances Functional Recovery and Reduces Astrogliosis in Bilateral Compressive/Contusive Cervical Spinal Cord Injury. Stem Cells Transl. Med. 2014, 3, 1148–1159. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Ahuja, C.S.; Salewski, R.P.; Li, L.; Satkunendrarajah, K.; Nagoshi, N.; Shibata, S.; Fehlings, M.G. Neural stem cell mediated recovery is enhanced by Chondroitinase ABC pretreatment in chronic cervical spinal cord injury. PLoS ONE 2017, 12, e0182339. [Google Scholar] [CrossRef] [PubMed]
- Ramon y Cajal, S. Degeneration and Regeneration of the Nervous System; Oxford University Press: London, UK, 1928. [Google Scholar]
- Bradbury, E.J.; Moon, L.D.F.; Popat, R.J.; King, V.R.; Bennett, G.S.; Patel, P.N.; Fawcett, J.W.; McMahon, S.B. Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 2002, 416, 636–640. [Google Scholar] [CrossRef]
- Suzuki, H.; Imajo, Y.; Funaba, M.; Nishida, N.; Sakamoto, T.; Sakai, T. Current Concepts of Neural Stem/Progenitor Cell Therapy for Chronic Spinal Cord Injury. Front. Cell. Neurosci. 2022, 15, 794692. [Google Scholar] [CrossRef]
- Suzuki, H.; Sakai, T. Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury. Int. J. Mol. Sci. 2021, 22, 7435. [Google Scholar] [CrossRef]
- Ahuja, C.S.; Nori, S.; Tetreault, L.; Wilson, J.; Kwon, B.; Harrop, J.; Choi, D.; Fehlings, M.G. Traumatic Spinal Cord Injury—Repair and Regeneration. Neurosurgery 2017, 80, S9–S22. [Google Scholar] [CrossRef]
- Cofano, F.; Boido, M.; Monticelli, M.; Zenga, F.; Ducati, A.; Vercelli, A.; Garbossa, D. Mesenchymal Stem Cells for Spinal Cord Injury: Current Options Limitations, and Future of Cell Therapy. Int. J. Mol. Sci. 2019, 20, 2698. [Google Scholar] [CrossRef]
- Hutson, T.H.; Di Giovanni, S. The translational landscape in spinal cord injury: Focus on neuroplasticity and regeneration. Nat. Rev. Neurol. 2019, 15, 732–745. [Google Scholar] [CrossRef] [PubMed]
- Badhiwala, J.H.; Wilson, J.R.; Kwon, B.K.; Casha, S.; Fehlings, M.G. A Review of Clinical Trials in Spinal Cord Injury Including Biomarkers. J. Neurotrauma 2018, 35, 1906–1917. [Google Scholar] [CrossRef] [PubMed]
- Shinozaki, M.; Nagoshi, N.; Nakamura, M.; Okano, H. Mechanisms of Stem Cell Therapy in Spinal Cord Injuries. Cells 2021, 10, 2676. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, C.S.; Mothe, A.; Khazaei, M.; Badhiwala, J.H.; Gilbert, E.A.; van der Kooy, D.; Morshead, C.M.; Tator, C.; Fehlings, M.G. The leading edge: Emerging neuroprotective and neuroregenerative cell-based therapies for spinal cord injury. Stem Cells Transl. Med. 2020, 9, 1509–1530. [Google Scholar] [CrossRef] [PubMed]
- Gabel, B.C.; Curtis, E.I.; Marsala, M.; Ciacci, J.D. A Review of Stem Cell Therapy for Spinal Cord Injury: Large Animal Models and the Frontier in Humans. World Neurosurg. 2017, 98, 438–443. [Google Scholar] [CrossRef]
- Zipser, C.M.; Cragg, J.J.; Guest, J.D.; Fehlings, M.G.; Jutzeler, C.R.; Anderson, A.J.; Curt, A. Cell-based and stem-cell-based treatments for spinal cord injury: Evidence from clinical trials. Lancet Neurol. 2022, 21, 659–670. [Google Scholar] [CrossRef]
- Kiyotake, E.A.; Martin, M.D.; Detamore, M.S. Regenerative rehabilitation with conductive biomaterials for spinal cord injury. Acta Biomater. 2022, 139, 43–64. [Google Scholar] [CrossRef]
- Ghane, N.; Beigi, M.-H.; Labbaf, S.; Nasr-Esfahani, M.-H.; Kiani, A. Design of hydrogel-based scaffolds for the treatment of spinal cord injuries. J. Mater. Chem. B 2020, 8, 10712–10738. [Google Scholar] [CrossRef]
- Pina, S.; Ribeiro, V.P.; Marques, C.F.; Maia, F.R.; Silva, T.H.; Reis, R.L.; Oliveira, J.M. Scaffolding Strategies for Tissue Engineering and Regenerative Medicine Applications. Materials 2019, 12, 1824. [Google Scholar] [CrossRef]
- Estrada, V.; Tekinay, A.; Müller, H.W. Neural ECM mimetics. Prog. Brain Res. 2014, 214, 391–413. [Google Scholar] [CrossRef]
- Khaing, Z.Z.; Seidlits, S.K. Hyaluronic acid and neural stem cells: Implications for biomaterial design. J. Mater. Chem. B 2015, 3, 7850–7866. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Yang, C.; Zhu, X.; Wang, J.-J.; Liu, X.-Y.; Yang, X.-P.; An, X.-W.; Liang, J.; Dong, H.-J.; Jiang, W.; et al. 3D printing collagen/chitosan scaffold ameliorated axon regeneration and neurological recovery after spinal cord injury. J. Biomed. Mater. Res. Part A 2019, 107, 1898–1908. [Google Scholar] [CrossRef] [PubMed]
- Marchand, R.; Woerly, S. Transected spinal cords grafted with in situ self-assembled collagen matrices. Neuroscience 1990, 36, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.; Dauzvardis, M.; Sayers, S. Carbon filament implants promote axonal growth across the transected rat spinal cord. Brain Res. 1991, 541, 139–145, Erratum in Brain Res. 1991, 546, 360. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Xu, B.; Xue, W.; Yang, B.; Fan, Y.; Chen, B.; Xiao, Z.; Xue, X.; Sun, Z.; Shu, M.; et al. A functional scaffold to promote the migration and neuronal differentiation of neural stem/progenitor cells for spinal cord injury repair. Biomaterials 2020, 243, 119941. [Google Scholar] [CrossRef]
- Fan, C.; Li, X.; Xiao, Z.; Zhao, Y.; Liang, H.; Wang, B.; Han, S.; Li, X.; Xu, B.; Wang, N.; et al. A modified collagen scaffold facilitates endogenous neurogenesis for acute spinal cord injury repair. Acta Biomater. 2017, 51, 304–316. [Google Scholar] [CrossRef]
- Yang, B.; Liang, C.; Chen, D.; Cheng, F.; Zhang, Y.; Wang, S.; Shu, J.; Huang, X.; Wang, J.; Xia, K.; et al. A conductive supramolecular hydrogel creates ideal endogenous niches to promote spinal cord injury repair. Bioact. Mater. 2022, 15, 103–119. [Google Scholar] [CrossRef]
- Martín-López, E.; Darder, M.; Ruiz-Hitzky, E.; Sampedro, M.N. Agar-based bridges as biocompatible candidates to provide guide cues in spinal cord injury repair. Bio-Med. Mater. Eng. 2013, 23, 405–421. [Google Scholar] [CrossRef]
- Gros, T.; Sakamoto, J.S.; Blesch, A.; Havton, L.A.; Tuszynski, M.H. Regeneration of long-tract axons through sites of spinal cord injury using templated agarose scaffolds. Biomaterials 2010, 31, 6719–6729. [Google Scholar] [CrossRef]
- Kataoka, K.; Suzuki, Y.; Kitada, M.; Hashimoto, T.; Chou, H.; Bai, H.; Ohta, M.; Wu, S.; Suzuki, K.; Ide, C. Alginate Enhances Elongation of Early Regenerating Axons in Spinal Cord of Young Rats. Tissue Eng. 2004, 10, 493–504. [Google Scholar] [CrossRef]
- Prang, P.; Mueller, R.; Eljaouhari, A.; Heckmann, K.; Kunz, W.; Weber, T.; Faber, C.; Vroemen, M.; Bogdahn, U.; Weidner, N. The promotion of oriented axonal regrowth in the injured spinal cord by alginate-based anisotropic capillary hydrogels. Biomaterials 2006, 27, 3560–3569. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Yao, S.; Xiong, Y.; Zhang, Z.; Yang, Y.; He, F.; Zhao, H.; Guo, Y.; Wang, G.; Xie, S.; et al. Directional axonal regrowth induced by an aligned fibrin nanofiber hydrogel contributes to improved motor function recovery in canine L2 spinal cord injury. J. Mater. Sci. Mater. Med. 2020, 31, 40. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.; Xue, W.; Zhu, H.; Shen, H.; Xiao, Z.; Wu, S.; Zhao, Y.; Cao, Y.; Tan, J.; Li, J.; et al. Scar tissue removal-activated endogenous neural stem cells aid Taxol-modified collagen scaffolds in repairing chronic long-distance transected spinal cord injury. Biomater. Sci. 2021, 9, 4778–4792. [Google Scholar] [CrossRef]
- Altinova, H.; Hammes, S.; Palm, M.; Achenbach, P.; Gerardo-Nava, J.; Deumens, R.; Führmann, T.; van Neerven, S.G.; Hermans, E.; Weis, J.; et al. Dense fibroadhesive scarring and poor blood vessel-maturation hamper the integration of implanted collagen scaffolds in an experimental model of spinal cord injury. Biomed. Mater. 2020, 15, 015012. [Google Scholar] [CrossRef] [PubMed]
- Gholami, M.; Gilanpour, H.; Sadeghinezhad, J.; Asghari, A. Facile fabrication of an erythropoietin-alginate/chitosan hydrogel and evaluation of its local therapeutic effects on spinal cord injury in rats. DARU J. Pharm. Sci. 2021, 29, 255–265. [Google Scholar] [CrossRef]
- Stokols, S.; Tuszynski, M.H. Freeze-dried agarose scaffolds with uniaxial channels stimulate and guide linear axonal growth following spinal cord injury. Biomaterials 2006, 27, 443–451. [Google Scholar] [CrossRef]
- Zhang, Z.; Yao, S.; Xie, S.; Wang, X.; Chang, F.; Luo, J.; Wang, J.; Fu, J. Effect of hierarchically aligned fibrin hydrogel in regeneration of spinal cord injury demonstrated by tractography: A pilot study. Sci. Rep. 2017, 7, 40017. [Google Scholar] [CrossRef]
- Fukushima, K.; Enomoto, M.; Tomizawa, S.; Takahashi, M.; Wakabayashi, Y.; Itoh, S.; Kuboki, Y.; Shinomiya, K. The axonal regeneration across a honeycomb collagen sponge applied to the transected spinal cord. J. Med. Dent. Sci. 2008, 55, 71–79. [Google Scholar]
- Zhao, X.; Wang, H.; Zou, Y.; Xue, W.; Zhuang, Y.; Gu, R.; Shen, H.; Dai, J. Optimized, visible light-induced crosslinkable hybrid gelatin/hyaluronic acid scaffold promotes complete spinal cord injury repair. Biomed. Mater. 2022, 17, 024104. [Google Scholar] [CrossRef]
- King, V.R.; Alovskaya, A.; Wei, D.; Brown, R.A.; Priestley, J.V. The use of injectable forms of fibrin and fibronectin to support axonal ingrowth after spinal cord injury. Biomaterials 2010, 31, 4447–4456. [Google Scholar] [CrossRef]
- Cheng, H.; Huang, Y.-C.; Chang, P.-T.; Huang, Y.-Y. Laminin-incorporated nerve conduits made by plasma treatment for repairing spinal cord injury. Biochem. Biophys. Res. Commun. 2007, 357, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Lee, J.Y.; Heo, E.Y.; Kwon, I.K.; Yune, T.Y.; Youn, I. Implantation of a Matrigel-loaded agarose scaffold promotes functional regeneration of axons after spinal cord injury in rat. Biochem. Biophys. Res. Commun. 2018, 496, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, A.; Fisher, O.; Dagci, T.; Himes, B.T.; Fischer, I.; Lowman, A. Mechanically engineered hydrogel scaffolds for axonal growth and angiogenesis after transplantation in spinal cord injury. J. Neurosurg. Spine 2004, 1, 322–329. [Google Scholar] [CrossRef]
- Zhai, H.; Zhou, J.; Xu, J.; Sun, X.; Xu, Y.; Qiu, X.; Zhang, C.; Wu, Z.; Long, H.; Bai, Y.; et al. Mechanically strengthened hybrid peptide-polyester hydrogel and potential applications in spinal cord injury repair. Biomed. Mater. 2020, 15, 055031. [Google Scholar] [CrossRef] [PubMed]
- Hejčl, A.; Růžička, J.; Kekulová, K.; Svobodová, B.; Proks, V.; Macková, H.; Jiránková, K.; Kárová, K.; Urdziková, L.M.; Kubinová, Š.; et al. Modified Methacrylate Hydrogels Improve Tissue Repair after Spinal Cord Injury. Int. J. Mol. Sci. 2018, 19, 2481. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Yan, S.; You, R.; Kaplan, D.L.; Liu, Y.; Qu, J.; Li, X.; Li, M.; Wang, X. Multichannel silk protein/laminin grafts for spinal cord injury repair. J. Biomed. Mater. Res. Part A 2016, 104, 3045–3057. [Google Scholar] [CrossRef]
- Chai, Y.; Long, Y.; Dong, X.; Liu, K.; Wei, W.; Chen, Y.; Qiu, T.; Dai, H. Improved functional recovery of rat transected spinal cord by peptide-grafted PNIPAM based hydrogel. Colloids Surf. B Biointerfaces 2022, 210, 112220. [Google Scholar] [CrossRef]
- Silva, N.A.; Salgado, A.J.; Sousa, R.A.; Oliveira, J.T.; Pedro, A.J.; Leite-Almeida, H.; Cerqueira, R.; Almeida, A.; Mastronardi, F.; Mano, J.F.; et al. Development and Characterization of a Novel Hybrid Tissue Engineering–Based Scaffold for Spinal Cord Injury Repair. Tissue Eng. Part A 2010, 16, 45–54. [Google Scholar] [CrossRef]
- Yang, Y.; Fan, Y.; Zhang, H.; Zhang, Q.; Zhao, Y.; Xiao, Z.; Liu, W.; Chen, B.; Gao, L.; Sun, Z.; et al. Small molecules combined with collagen hydrogel direct neurogenesis and migration of neural stem cells after spinal cord injury. Biomaterials 2021, 269, 120479. [Google Scholar] [CrossRef]
- Suzuki, H.; Kanchiku, T.; Imajo, Y.; Yoshida, Y.; Nishida, N.; Gondo, T.; Yoshii, S.; Taguchi, T. Artificial collagen-filament scaffold promotes axon regeneration and long tract reconstruction in a rat model of spinal cord transection. Med. Mol. Morphol. 2015, 48, 214–224. [Google Scholar] [CrossRef]
- Yara, T.; Kato, Y.; Kataoka, H.; Kanchiku, T.; Suzuki, H.; Gondo, T.; Yoshii, S.; Taguchi, T. Environmental factors involved in axonal regeneration following spinal cord transection in rats. Med. Mol. Morphol. 2009, 42, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Nair, L.S.; Laurencin, C.T. Biodegradable polymers as biomaterials. Prog. Polym. Sci. 2007, 32, 762–798. [Google Scholar] [CrossRef]
- Cheng, Y.; Zhang, Y.; Wu, H. Polymeric Fibers as Scaffolds for Spinal Cord Injury: A Systematic Review. Front. Bioeng. Biotechnol. 2022, 9, 807533. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Wilcox, J.T.; Nishimura, Y.; Zweckberger, K.; Suzuki, H.; Wang, J.; Liu, Y.; Karadimas, S.K.; Fehlings, M.G. Synergistic effects of self-assembling peptide and neural stem/progenitor cells to promote tissue repair and forelimb functional recovery in cervical spinal cord injury. Biomaterials 2014, 35, 2617–2629. [Google Scholar] [CrossRef]
- Kubinová, Š.; Horák, D.; Hejčl, A.; Plichta, Z.; Kotek, J.; Proks, V.; Forostyak, S.; Syková, E. SIKVAV-modified highly superporous PHEMA scaffolds with oriented pores for spinal cord injury repair. J. Tissue Eng. Regen. Med. 2015, 9, 1298–1309. [Google Scholar] [CrossRef]
- Hejčl, A.; Urdzikova, L.M.; Sedy, J.; Lesny, P.; Pradny, M.; Michálek, J.; Burian, M.; Hajek, M.; Zamecnik, J.; Jendelova, P.; et al. Acute and delayed implantation of positively charged 2-hydroxyethyl methacrylate scaffolds in spinal cord injury in the rat. J. Neurosurg. Spine 2008, 8, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Shi, T.; Zhou, T.; Dong, D.; Xie, J.; Wang, R.; An, X.; Chen, M.; Cai, J. 3D Poly(Lactic-co-glycolic acid) Scaffolds for Treating Spinal Cord Injury. J. Biomed. Nanotechnol. 2017, 13, 290–302. [Google Scholar] [CrossRef]
- Slotkin, J.R.; Pritchard, C.D.; Luque, B.; Ye, J.; Layer, R.T.; Lawrence, M.S.; O’Shea, T.M.; Roy, R.R.; Zhong, H.; Vollenweider, I.; et al. Biodegradable scaffolds promote tissue remodeling and functional improvement in non-human primates with acute spinal cord injury. Biomaterials 2017, 123, 63–76. [Google Scholar] [CrossRef]
- Silva, N.A.; Sousa, R.A.; Fraga, J.S.; Fontes, M.; Leite-Almeida, H.; Cerqueira, R.; Almeida, A.; Sousa, N.; Reis, R.L.; Salgado, A.J. Benefits of Spine Stabilization with Biodegradable Scaffolds in Spinal Cord Injured Rats. Tissue Eng. Part C Methods 2013, 19, 101–108. [Google Scholar] [CrossRef]
- Thomas, A.M.; Kubilius, M.B.; Holland, S.J.; Seidlits, S.K.; Boehler, R.M.; Anderson, A.J.; Cummings, B.J.; Shea, L.D. Channel density and porosity of degradable bridging scaffolds on axon growth after spinal injury. Biomaterials 2013, 34, 2213–2220. [Google Scholar] [CrossRef]
- Man, W.; Yang, S.; Cao, Z.; Lu, J.; Kong, X.; Sun, X.; Zhao, L.; Guo, Y.; Yao, S.; Wang, G.; et al. A multi-modal delivery strategy for spinal cord regeneration using a composite hydrogel presenting biophysical and biochemical cues synergistically. Biomaterials 2021, 276, 120971. [Google Scholar] [CrossRef] [PubMed]
- Kubinová, Š.; Horák, D.; Hejčl, A.; Plichta, Z.; Kotek, J.; Syková, E. Highly superporous cholesterol-modified poly(2-hydroxyethyl methacrylate) scaffolds for spinal cord injury repair. J. Biomed. Mater. Res. Part A 2011, 99A, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Guest, J.D.; Moore, S.W.; Aimetti, A.A.; Kutikov, A.B.; Santamaria, A.J.; Hofstetter, C.P.; Ropper, A.E.; Theodore, N.; Ulich, T.R.; Layer, R.T. Internal decompression of the acutely contused spinal cord: Differential effects of irrigation only versus biodegradable scaffold implantation. Biomaterials 2018, 185, 284–300. [Google Scholar] [CrossRef] [PubMed]
- Hakim, J.S.; Rodysill, B.R.; Chen, B.K.; Schmeichel, A.M.; Yaszemski, M.J.; Windebank, A.J.; Madigan, N.N. Combinatorial tissue engineering partially restores function after spinal cord injury. J. Tissue Eng. Regen. Med. 2019, 13, 857–873. [Google Scholar] [CrossRef]
- Anzalone, A.; Chacko, J.V.; Nishi, R.A.; Dumont, C.; Smith, D.; Shea, L.D.; Digman, M.A.; Cummings, B.J.; Anderson, A.J. Feasibility study on mouse live imaging after spinal cord injury and poly(lactide-co-glycolide) bridge implantation. J. Biomed. Opt. 2018, 23, 065007. [Google Scholar] [CrossRef] [PubMed]
- De Laporte, L.; Yan, A.L.; Shea, L.D. Local gene delivery from ECM-coated poly(lactide-co-glycolide) multiple channel bridges after spinal cord injury. Biomaterials 2009, 30, 2361–2368. [Google Scholar] [CrossRef]
- Wong, D.Y.; Leveque, J.-C.; Brumblay, H.; Krebsbach, P.H.; Hollister, S.J.; LaMarca, F. Macro-Architectures in Spinal Cord Scaffold Implants Influence Regeneration. J. Neurotrauma 2008, 25, 1027–1037. [Google Scholar] [CrossRef]
- Ribeiro-Samy, S.; Silva, N.A.; Correlo, V.M.; Fraga, J.S.; Pinto, L.; Teixeira-Castro, A.; Leite-Almeida, H.; Almeida, A.; Gimble, J.M.; Sousa, N.; et al. Development and Characterization of a PHB-HV-based 3D Scaffold for a Tissue Engineering and Cell-therapy Combinatorial Approach for Spinal Cord Injury Regeneration. Macromol. Biosci. 2013, 13, 1576–1592. [Google Scholar] [CrossRef]
- Pawar, K.; Cummings, B.J.; Thomas, A.; Shea, L.D.; Levine, A.; Pfaff, S.; Anderson, A.J. Biomaterial bridges enable regeneration and re-entry of corticospinal tract axons into the caudal spinal cord after SCI: Association with recovery of forelimb function. Biomaterials 2015, 65, 1–12. [Google Scholar] [CrossRef]
- Rooney, G.E.; Vaishya, S.; Ameenuddin, S.; Currier, B.L.; Schiefer, T.K.; Knight, A.; Chen, B.; Mishra, P.K.; Spinner, R.J.; Macura, S.I.; et al. Rigid Fixation of the Spinal Column Improves Scaffold Alignment and Prevents Scoliosis in the Transected Rat Spinal Cord. Spine 2008, 33, E914–E919. [Google Scholar] [CrossRef] [PubMed]
- Shu, B.; Sun, X.; Liu, R.; Jiang, F.; Yu, H.; Xu, N.; An, Y. Restoring electrical connection using a conductive biomaterial provides a new therapeutic strategy for rats with spinal cord injury. Neurosci. Lett. 2019, 692, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Fan, L.; Yi, X.; Zhou, Z.; Liu, C.; Fu, R.; Dai, C.; Wang, Z.; Chen, X.; Yu, P.; et al. Soft Conducting Polymer Hydrogels Cross-Linked and Doped by Tannic Acid for Spinal Cord Injury Repair. ACS Nano 2018, 12, 10957–10967. [Google Scholar] [CrossRef] [PubMed]
- Pertici, V.; Trimaille, T.; Laurin, J.; Felix, M.-S.; Marqueste, T.; Pettmann, B.; Chauvin, J.-P.; Gigmes, D.; Decherchi, P. Repair of the injured spinal cord by implantation of a synthetic degradable block copolymer in rat. Biomaterials 2014, 35, 6248–6258. [Google Scholar] [CrossRef] [PubMed]
- Reis, K.P.; Sperling, L.E.; Teixeira, C.; Sommer, L.; Colombo, M.; Koester, L.S.; Pranke, P. VPA/PLGA microfibers produced by coaxial electrospinning for the treatment of central nervous system injury. Braz. J. Med. Biol. Res. 2020, 53, e8993. [Google Scholar] [CrossRef] [PubMed]
- Novikova, L.N.; Kolar, M.K.; Kingham, P.J.; Ullrich, A.; Oberhoffner, S.; Renardy, M.; Doser, M.; Müller, E.; Wiberg, M.; Novikov, L.N. Trimethylene carbonate-caprolactone conduit with poly-p-dioxanone microfilaments to promote regeneration after spinal cord injury. Acta Biomater. 2018, 66, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.H.; Agrawal, N.K.; Griffin, J.M.; Schmidt, C.E. Recent advances in nanotherapeutic strategies for spinal cord injury repair. Adv. Drug Deliv. Rev. 2019, 148, 38–59. [Google Scholar] [CrossRef] [PubMed]
- Gerardo-Nava, J.; Führmann, T.; Klinkhammer, K.; Seiler, N.; Mey, J.; Klee, D.; Möller, M.; Dalton, P.D.; Brook, G.A. Human neural cell interactions with orientated electrospun nanofibers in vitro. Nanomedicine 2009, 4, 11–30. [Google Scholar] [CrossRef]
- Zamani, F.; Amani-Tehran, M.; Latifi, M.; Shokrgozar, M.A.; Zaminy, A. Promotion of spinal cord axon regeneration by 3D nanofibrous core-sheath scaffolds. J. Biomed. Mater. Res. Part A 2014, 102, 506–513. [Google Scholar] [CrossRef]
- Sun, X.; Bai, Y.; Zhai, H.; Liu, S.; Zhang, C.; Xu, Y.; Zou, J.; Wang, T.; Chen, S.; Zhu, Q.; et al. Devising micro/nano-architectures in multi-channel nerve conduits towards a pro-regenerative matrix for the repair of spinal cord injury. Acta Biomater. 2019, 86, 194–206. [Google Scholar] [CrossRef]
- Cigognini, D.; Silva, D.; Paloppi, S.; Gelain, F. Evaluation of mechanical properties and therapeutic effect of injectable self-assembling hydrogels for spinal cord injury. J. Biomed. Nanotechnol. 2014, 10, 309–323. [Google Scholar] [CrossRef]
- Yao, S.; Yu, S.; Cao, Z.; Yang, Y.; Yu, X.; Mao, H.-Q.; Wang, L.-N.; Sun, X.; Zhao, L.; Wang, X. Hierarchically aligned fibrin nanofiber hydrogel accelerated axonal regrowth and locomotor function recovery in rat spinal cord injury. Int. J. Nanomed. 2018, 13, 2883–2895. [Google Scholar] [CrossRef] [PubMed]
- Altinova, H.; Möllers, S.; Deumens, R.; Gerardo-Nava, J.; Führmann, T.; van Neerven, S.G.A.; Bozkurt, A.; Mueller, C.A.; Hoff, H.J.; Heschel, I.; et al. Functional recovery not correlated with axon regeneration through olfactory ensheathing cell-seeded scaffolds in a model of acute spinal cord injury. Tissue Eng. Regen. Med. 2016, 13, 585–600. [Google Scholar] [CrossRef]
- Usmani, S.; Biagioni, A.F.; Medelin, M.; Scaini, D.; Casani, R.; Aurand, E.R.; Padro, D.; Egimendia, A.; Cabrer, P.R.; Scarselli, M.; et al. Functional rewiring across spinal injuries via biomimetic nanofiber scaffolds. Proc. Natl. Acad. Sci. USA 2020, 117, 25212–25218. [Google Scholar] [CrossRef]
- Sever-Bahcekapili, M.; Yilmaz, C.; Demirel, A.; Kilinc, M.C.; Dogan, I.; Caglar, Y.S.; Guler, M.O.; Tekinay, A.B. Neuroactive Peptide Nanofibers for Regeneration of Spinal Cord after Injury. Macromol. Biosci. 2021, 21, e2000234. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Jing, Y.; Zhou, X.; Wang, J.; Huang, X.; Gao, L.; Zhu, Y.; Wang, L.; Gou, Z.; Liang, C.; et al. PHBV/PLA/Col-Based Nanofibrous Scaffolds Promote Recovery of Locomotor Function by Decreasing Reactive Astrogliosis in a Hemisection Spinal Cord Injury Rat Model. J. Biomed. Nanotechnol. 2018, 14, 1921–1933. [Google Scholar] [CrossRef] [PubMed]
- Chedly, J.; Soares, S.; Montembault, A.; von Boxberg, Y.; Veron-Ravaille, M.; Mouffle, C.; Benassy, M.-N.; Taxi, J.; David, L.; Nothias, F. Physical chitosan microhydrogels as scaffolds for spinal cord injury restoration and axon regeneration. Biomaterials 2017, 138, 91–107. [Google Scholar] [CrossRef]
- Cigognini, D.; Satta, A.; Colleoni, B.; Silva, D.; Donegà, M.; Antonini, S.; Gelain, F. Evaluation of Early and Late Effects into the Acute Spinal Cord Injury of an Injectable Functionalized Self-Assembling Scaffold. PLoS ONE 2011, 6, e19782. [Google Scholar] [CrossRef] [PubMed]
- Palejwala, A.H.; Fridley, J.S.; Mata, J.A.; Samuel, E.L.G.; Luerssen, T.G.; Perlaky, L.; Kent, T.A.; Tour, J.M.; Jea, A. Biocompatibility of reduced graphene oxide nanoscaffolds following acute spinal cord injury in rats. Surg. Neurol. Int. 2016, 7, 75. [Google Scholar] [CrossRef]
- Pawelec, K.M.; Koffler, J.; Shahriari, D.; Galvan, A.; Tuszynski, M.H.; Sakamoto, J. Microstructure and in vivo characterization of multi-channel nerve guidance scaffolds. Biomed. Mater. 2018, 13, 044104. [Google Scholar] [CrossRef]
- Milbreta, U.; Nguyen, L.H.; Diao, H.; Lin, J.; Wu, W.; Sun, C.-Y.; Wang, J.; Chew, S.Y. Three-Dimensional Nanofiber Hybrid Scaffold Directs and Enhances Axonal Regeneration after Spinal Cord Injury. ACS Biomater. Sci. Eng. 2016, 2, 1319–1329. [Google Scholar] [CrossRef]
- Tysseling, V.M.; Sahni, V.; Pashuck, E.T.; Birch, D.; Hebert, A.; Czeisler, C.; Stupp, S.I.; Kessler, J.A. Self-assembling peptide amphiphile promotes plasticity of serotonergic fibers following spinal cord injury. J. Neurosci. Res. 2010, 88, 3161–3170. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ye, H.; Satkunendrarajah, K.; Yao, G.S.; Bayon, Y.; Fehlings, M.G. A self-assembling peptide reduces glial scarring, attenuates post-traumatic inflammation and promotes neurological recovery following spinal cord injury. Acta Biomater. 2013, 9, 8075–8088. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Tan, H.; Hui, X. Biomaterial Scaffolds in Regenerative Therapy of the Central Nervous System. BioMed Res. Int. 2018, 2018, 7848901. [Google Scholar] [CrossRef]
- Furuya, T.; Hashimoto, M.; Koda, M.; Murata, A.; Okawa, A.; Dezawa, M.; Matsuse, D.; Tabata, Y.; Takahashi, K.; Yamazaki, M. Treatment with basic fibroblast growth factor-incorporated gelatin hydrogel does not exacerbate mechanical allodynia after spinal cord contusion injury in rats. J. Spinal Cord Med. 2013, 36, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Chvatal, S.A.; Kim, Y.-T.; Bratt-Leal, A.M.; Lee, H.; Bellamkonda, R.V. Spatial distribution and acute anti-inflammatory effects of Methylprednisolone after sustained local delivery to the contused spinal cord. Biomaterials 2008, 29, 1967–1975. [Google Scholar] [CrossRef] [PubMed]
- McKay, C.A.; Pomrenke, R.D.; McLane, J.S.; Schaub, N.J.; DeSimone, E.K.; Ligon, L.A.; Gilbert, R.J. An Injectable, Calcium Responsive Composite Hydrogel for the Treatment of Acute Spinal Cord Injury. ACS Appl. Mater. Interfaces 2014, 6, 1424–1438. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; McKeon, R.J.; Brady-Kalnay, S.M.; Bellamkonda, R.V. Sustained Delivery of Activated Rho GTPases and BDNF Promotes Axon Growth in CSPG-Rich Regions Following Spinal Cord Injury. PLoS ONE 2011, 6, e16135. [Google Scholar] [CrossRef]
- Wen, Y.; Yu, S.; Wu, Y.; Ju, R.; Wang, H.; Liu, Y.; Wang, Y.; Xu, Q. Spinal cord injury repair by implantation of structured hyaluronic acid scaffold with PLGA microspheres in the rat. Cell Tissue Res. 2016, 364, 17–28. [Google Scholar] [CrossRef]
- Chen, B.; He, J.; Yang, H.; Zhang, Q.; Zhang, L.; Zhang, X.; Xie, E.; Liu, C.; Zhang, R.; Wang, Y.; et al. Repair of spinal cord injury by implantation of bFGF-incorporated HEMA-MOETACL hydrogel in rats. Sci. Rep. 2015, 5, 9017. [Google Scholar] [CrossRef]
- Chan, G.; Mooney, D.J. New materials for tissue engineering: Towards greater control over the biological response. Trends Biotechnol. 2008, 26, 382–392. [Google Scholar] [CrossRef]
- Straley, K.S.; Foo, C.W.P.; Heilshorn, S.C. Biomaterial Design Strategies for the Treatment of Spinal Cord Injuries. J. Neurotrauma 2010, 27, 1–19. [Google Scholar] [CrossRef]
- Kalotra, S.; Saini, V.; Singh, H.; Sharma, A.; Kaur, G. 5-Nonyloxytryptamine oxalate–embedded collagen–laminin scaffolds augment functional recovery after spinal cord injury in mice. Ann. N. Y. Acad. Sci. 2020, 1465, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Anopas, D.; Milbreta, U.; Lin, P.H.; Chin, J.S.; Zhang, N.; Wee, S.K.; Tow, A.; Ang, W.T.; Chew, S.Y. Regenerative rehabilitation: Exploring the synergistic effects of rehabilitation and implantation of a bio-functional scaffold in enhancing nerve regeneration. Biomater. Sci. 2019, 7, 5150–5160. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Gao, W.; Han, X.; Zhu, X.; Sun, J.; Xie, F.; Hou, X.; Yang, H.; Dai, J.; Chen, L. Collagen scaffolds modified with collagen-binding bFGF promotes the neural regeneration in a rat hemisected spinal cord injury model. Sci. China Life Sci. 2014, 57, 232–240. [Google Scholar] [CrossRef]
- Wang, X.; Li, Y.; Gao, Y.; Chen, X.; Yao, J.; Lin, W.; Chen, Y.; Liu, J.; Yang, Y.; Wang, X. Combined use of spinal cord-mimicking partition type scaffold architecture and neurotrophin-3 for surgical repair of completely transected spinal cord in rats. J. Biomater. Sci. Polym. Ed. 2013, 24, 927–939. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Che, M.-T.; Zhang, K.; Qin, L.-N.; Zhang, Y.-T.; Chen, R.-Q.; Rong, L.-M.; Liu, S.; Ding, Y.; Shen, H.-Y.; et al. Graft of the NT-3 persistent delivery gelatin sponge scaffold promotes axon regeneration, attenuates inflammation, and induces cell migration in rat and canine with spinal cord injury. Biomaterials 2016, 83, 233–248. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.-T.; He, Y.; Xu, C.-L.; Wang, Y.; Liu, B.-F.; Wang, X.-M.; Sun, X.-D.; Cui, F.-Z.; Xu, Q.-Y. Hyaluronic acid hydrogel modified with nogo-66 receptor antibody and poly-L-lysine to promote axon regrowth after spinal cord injury. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 95B, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Bighinati, A.; Focarete, M.L.; Gualandi, C.; Pannella, M.; Giuliani, A.; Beggiato, S.; Ferraro, L.; Lorenzini, L.; Giardino, L.; Calzà, L. Improved Functional Recovery in Rat Spinal Cord Injury Induced by a Drug Combination Administered with an Implantable Polymeric Delivery System. J. Neurotrauma 2020, 37, 1708–1719. [Google Scholar] [CrossRef]
- Ehsanipour, A.; Sathialingam, M.; Rad, L.M.; de Rutte, J.; Bierman, R.D.; Liang, J.; Xiao, W.; Di Carlo, D.; Seidlits, S.K. Injectable, macroporous scaffolds for delivery of therapeutic genes to the injured spinal cord. APL Bioeng. 2021, 5, 016104. [Google Scholar] [CrossRef]
- Xie, J.; Li, J.; Ma, J.; Li, M.; Wang, X.; Fu, X.; Ma, Y.; Yang, H.; Li, B. Saijilafu Magnesium Oxide/Poly(l-lactide-co-ε-caprolactone) Scaffolds Loaded with Neural Morphogens Promote Spinal Cord Repair through Targeting the Calcium Influx and Neuronal Differentiation of Neural Stem Cells. Adv. Healthc. Mater. 2022, 11, 2200386. [Google Scholar] [CrossRef]
- Xi, K.; Gu, Y.; Tang, J.; Chen, H.; Xu, Y.; Wu, L.; Cai, F.; Deng, L.; Yang, H.; Shi, Q.; et al. Microenvironment-responsive immunoregulatory electrospun fibers for promoting nerve function recovery. Nat. Commun. 2020, 11, 4504, Erratum in Nat. Commun. 2021, 12, 2882. [Google Scholar] [CrossRef]
- Rooney, G.E.; Knight, A.M.; Madigan, N.N.; Gross, L.; Chen, B.; Giraldo, C.V.; Seo, S.; Nesbitt, J.J.; Dadsetan, M.; Yaszemski, M.J.; et al. Sustained Delivery of Dibutyryl Cyclic Adenosine Monophosphate to the Transected Spinal Cord Via Oligo [(Polyethylene Glycol) Fumarate] Hydrogels. Tissue Eng. Part A 2011, 17, 1287–1302. [Google Scholar] [CrossRef]
- Stropkovska, A.; Kisucka, A.; Bimbova, K.; Bacova, M.; Galik, J.; Medvecky, L.; Sulla, I.; Karasova, M.; Lukacova, N. Combined therapy (Rho-A-kinase inhibitor and chitosan/collagen porous scaffold) provides a supportive environment for endogenous regenerative processes after spinal cord trauma. Arch. Ital. Biol. 2021, 159, 159–177. [Google Scholar] [CrossRef]
- Ji, W.-C.; Li, M.; Jiang, W.-T.; Ma, X.; Li, J. Protective effect of brain-derived neurotrophic factor and neurotrophin-3 overexpression by adipose-derived stem cells combined with silk fibroin/chitosan scaffold in spinal cord injury. Neurol. Res. 2020, 42, 361–371. [Google Scholar] [CrossRef]
- Katz, J.S.; Burdick, J.A. Hydrogel mediated delivery of trophic factors for neural repair. WIREs Nanomed. Nanobiotechnol. 2008, 1, 128–139. [Google Scholar] [CrossRef]
- Johnson, P.J.; Tatara, A.; McCreedy, D.A.; Shiu, A.; Sakiyama-Elbert, S.E. Tissue-engineered fibrin scaffolds containing neural progenitors enhance functional recovery in a subacute model of SCI. Soft Matter 2010, 6, 5127–5137. [Google Scholar] [CrossRef]
- Smith, D.R.; Dumont, C.M.; Park, J.; Ciciriello, A.J.; Guo, A.; Tatineni, R.; Cummings, B.J.; Anderson, A.J.; Shea, L.D. Polycistronic Delivery of IL-10 and NT-3 Promotes Oligodendrocyte Myelination and Functional Recovery in a Mouse Spinal Cord Injury Model. Tissue Eng. Part A 2020, 26, 672–682. [Google Scholar] [CrossRef]
- Jain, A.; Kim, Y.-T.; McKeon, R.J.; Bellamkonda, R.V. In situ gelling hydrogels for conformal repair of spinal cord defects, and local delivery of BDNF after spinal cord injury. Biomaterials 2006, 27, 497–504. [Google Scholar] [CrossRef]
- Breen, B.A.; Kraskiewicz, H.; Ronan, R.; Kshiragar, A.; Patar, A.; Sargeant, T.; Pandit, A.; McMahon, S.S. Therapeutic Effect of Neurotrophin-3 Treatment in an Injectable Collagen Scaffold Following Rat Spinal Cord Hemisection Injury. ACS Biomater. Sci. Eng. 2017, 3, 1287–1295. [Google Scholar] [CrossRef]
- Rosenzweig, E.S.; Brock, J.H.; Lu, P.; Kumamaru, H.; Salegio, E.A.; Kadoya, K.; Weber, J.L.; Liang, J.J.; Moseanko, R.; Hawbecker, S.; et al. Restorative effects of human neural stem cell grafts on the primate spinal cord. Nat. Med. 2018, 24, 484–490. [Google Scholar] [CrossRef]
- Zhao, Y.; Tang, F.; Xiao, Z.; Han, G.; Wang, N.; Yin, N.; Chen, B.; Jiang, X.; Yun, C.; Han, W.; et al. Clinical Study of NeuroRegen Scaffold Combined with Human Mesenchymal Stem Cells for the Repair of Chronic Complete Spinal Cord Injury. Cell Transplant. 2017, 26, 891–900. [Google Scholar] [CrossRef]
- Chen, W.; Zhang, Y.; Yang, S.; Sun, J.; Qiu, H.; Hu, X.; Niu, X.; Xiao, Z.; Zhao, Y.; Zhou, Y.; et al. NeuroRegen Scaffolds Combined with Autologous Bone Marrow Mononuclear Cells for the Repair of Acute Complete Spinal Cord Injury: A 3-Year Clinical Study. Cell Transplant. 2020, 29, 963689720950637. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Chueng, S.-T.D.; Li, Y.; Patel, M.; Rathnam, C.; Dey, G.; Wang, L.; Cai, L.; Lee, K.-B. A biodegradable hybrid inorganic nanoscaffold for advanced stem cell therapy. Nat. Commun. 2018, 9, 3147. [Google Scholar] [CrossRef]
- Guo, J.; Su, H.; Zeng, Y.; Liang, Y.-X.; Wong, W.M.; Ellis-Behnke, R.G.; So, K.-F.; Wu, W. Reknitting the injured spinal cord by self-assembling peptide nanofiber scaffold. Nanomed. Nanotechnol. Biol. Med. 2007, 3, 311–321. [Google Scholar] [CrossRef]
- Kim, S.-H.; Hwang, K.; Lee, H.A.; Kim, J.; Cho, M.; Kim, M.; Shin, J.E.; Lee, H.; Park, K.I.; Jang, J.-H. Pastable, Adhesive, Injectable, Nanofibrous, and Tunable (PAINT) Biphasic Hybrid Matrices as Versatile Therapeutic Carriers. ACS Appl. Mater. Interfaces 2021, 13, 42429–42441. [Google Scholar] [CrossRef]
- Xu, B.; Zhao, Y.; Xiao, Z.; Wang, B.; Liang, H.; Li, X.; Fang, Y.; Han, S.; Li, X.; Fan, C.; et al. A Dual Functional Scaffold Tethered with EGFR Antibody Promotes Neural Stem Cell Retention and Neuronal Differentiation for Spinal Cord Injury Repair. Adv. Healthc. Mater. 2017, 6, 1601279. [Google Scholar] [CrossRef]
- Li, X.; Xiao, Z.; Han, J.; Chen, L.; Xiao, H.; Ma, F.; Hou, X.; Li, X.; Sun, J.; Ding, W.; et al. Promotion of neuronal differentiation of neural progenitor cells by using EGFR antibody functionalized collagen scaffolds for spinal cord injury repair. Biomaterials 2013, 34, 5107–5116. [Google Scholar] [CrossRef]
- Tang, S.; Liao, X.; Shi, B.; Qu, Y.; Huang, Z.; Lin, Q.; Guo, X.; Pei, F. The Effects of Controlled Release of Neurotrophin-3 from PCLA Scaffolds on the Survival and Neuronal Differentiation of Transplanted Neural Stem Cells in a Rat Spinal Cord Injury Model. PLoS ONE 2014, 9, e107517. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Neeley, W.L.; Pritchard, C.D.; Slotkin, J.R.; Woodard, E.J.; Langer, R.; Teng, Y.D. Blockade of Peroxynitrite-Induced Neural Stem Cell Death in the Acutely Injured Spinal Cord by Drug-Releasing Polymer. Stem Cells 2009, 27, 1212–1222, Erratum in Stem Cells 2009, 27, 3121. [Google Scholar] [CrossRef]
- Ham, T.R.; Pukale, D.D.; Hamrangsekachaee, M.; Leipzig, N.D. Subcutaneous priming of protein-functionalized chitosan scaffolds improves function following spinal cord injury. Mater. Sci. Eng. C 2020, 110, 110656. [Google Scholar] [CrossRef]
- Liu, X.; Hao, M.; Chen, Z.; Zhang, T.; Huang, J.; Dai, J.; Zhang, Z. 3D bioprinted neural tissue constructs for spinal cord injury repair. Biomaterials 2021, 272, 120771. [Google Scholar] [CrossRef] [PubMed]
- Rauch, M.F.; Hynes, S.R.; Bertram, J.; Redmond, A.; Robinson, R.; Williams, C.; Xu, H.; Madri, J.A.; Lavik, E.B. Engineering angiogenesis following spinal cord injury: A coculture of neural progenitor and endothelial cells in a degradable polymer implant leads to an increase in vessel density and formation of the blood-spinal cord barrier. Eur. J. Neurosci. 2009, 29, 132–145. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Fan, C.; Xiao, Z.; Zhao, Y.; Zhang, H.; Sun, J.; Zhuang, Y.; Wu, X.; Shi, J.; Chen, Y.; et al. A collagen microchannel scaffold carrying paclitaxel-liposomes induces neuronal differentiation of neural stem cells through Wnt/β-catenin signaling for spinal cord injury repair. Biomaterials 2018, 183, 114–127. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Xie, Y.-Y.; Wang, L.-D.; Tai, C.-X.; Chen, D.; Mu, D.; Cui, Y.-Y.; Wang, B. A multi-channel collagen scaffold loaded with neural stem cells for the repair of spinal cord injury. Neural Regen. Res. 2021, 16, 2284–2292. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Ma, D.; Shen, H.; Zhao, Y.; Xu, B.; Fan, Y.; Sun, Z.; Chen, B.; Xue, W.; Shi, Y.; et al. Aligned collagen scaffold combination with human spinal cord-derived neural stem cells to improve spinal cord injury repair. Biomater. Sci. 2020, 8, 5145–5156. [Google Scholar] [CrossRef]
- Martínez-Ramos, C.; Doblado, L.R.; Mocholi, E.L.; Alastrue-Agudo, A.; Petidier, M.S.; Giraldo, E.; Pradas, M.M.; Moreno-Manzano, V. Biohybrids for spinal cord injury repair. J. Tissue Eng. Regen. Med. 2019, 13, 509–521. [Google Scholar] [CrossRef]
- Shin, J.E.; Jung, K.; Kim, M.; Hwang, K.; Lee, H.; Kim, I.-S.; Lee, B.H.; Lee, I.-S.; Park, K.I. Brain and spinal cord injury repair by implantation of human neural progenitor cells seeded onto polymer scaffolds. Exp. Mol. Med. 2018, 50, 1–18. [Google Scholar] [CrossRef]
- Nomura, H.; Zahir, T.; Kim, H.; Katayama, Y.; Kulbatski, I.; Morshead, C.M.; Shoichet, M.S.; Tator, C.H. Extramedullary Chitosan Channels Promote Survival of Transplanted Neural Stem and Progenitor Cells and Create a Tissue Bridge After Complete Spinal Cord Transection. Tissue Eng. Part A 2008, 14, 649–665. [Google Scholar] [CrossRef]
- Ma, Y.-H.; Shi, H.-J.; Wei, Q.-S.; Deng, Q.-W.; Sun, J.-H.; Liu, Z.; Lai, B.-Q.; Li, G.; Ding, Y.; Niu, W.-T.; et al. Developing a mechanically matched decellularized spinal cord scaffold for the in situ matrix-based neural repair of spinal cord injury. Biomaterials 2021, 279, 121192. [Google Scholar] [CrossRef]
- Chen, G.; Hu, Y.R.; Wan, H.; Deng, Q.W.; Sun, J.H.; Liu, Z.; Lai, B.Q.; Li, G.; Ding, Y.; Niu, W.T.; et al. Functional recovery following traumatic spinal cord injury mediated by a unique polymer scaffold seeded with neural stem cells and Schwann cells. Chin. Med. J. 2010, 123, 2424–2431. [Google Scholar]
- Ruzicka, J.; Romanyuk, N.; Jirakova, K.; Hejcl, A.; Janouskova, O.; Machova, L.U.; Bochin, M.; Pradny, M.; Vargova, L.; Jendelova, P. The Effect of iPS-Derived Neural Progenitors Seeded on Laminin-Coated pHEMA-MOETACl Hydrogel with Dual Porosity in a Rat Model of Chronic Spinal Cord Injury. Cell Transplant. 2019, 28, 400–412. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, F.; Zhong, W.; Liu, Y.; He, Q.; Yang, M.; Chen, H.; Xu, X.; Bian, K.; Xu, J.; et al. Transplantation of neural scaffolds consisting of dermal fibroblast-reprogrammed neurons and 3D silk fibrous materials promotes the repair of spinal cord injury. J. Mater. Chem. B 2019, 7, 7525–7539. [Google Scholar] [CrossRef]
- Olson, H.E.; Rooney, G.E.; Gross, L.; Nesbitt, J.J.; Galvin, K.E.; Knight, A.; Chen, B.; Yaszemski, M.J.; Windebank, A.J. Neural Stem Cell– and Schwann Cell–Loaded Biodegradable Polymer Scaffolds Support Axonal Regeneration in the Transected Spinal Cord. Tissue Eng. Part A 2009, 15, 1797–1805. [Google Scholar] [CrossRef]
- Kourgiantaki, A.; Tzeranis, D.S.; Karali, K.; Georgelou, K.; Bampoula, E.; Psilodimitrakopoulos, S.; Yannas, I.V.; Stratakis, E.; Sidiropoulou, K.; Charalampopoulos, I.; et al. Neural stem cell delivery via porous collagen scaffolds promotes neuronal differentiation and locomotion recovery in spinal cord injury. NPJ Regen. Med. 2020, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Wan, H.; Hao, S.-Y.; Li, D.-Z.; Chen, G.; Gao, C.-C.; Li, J.-H.; Yang, F.; Wang, S.-G.; Liu, S. Co-transplantation of neural stem cells and Schwann cells within poly (L-lactic-co-glycolic acid) scaffolds facilitates axonal regeneration in hemisected rat spinal cord. Chin. Med. J. 2013, 126, 909–917. [Google Scholar] [PubMed]
- Zarei-Kheirabadi, M.; Sadrosadat, H.; Mohammadshirazi, A.; Jaberi, R.; Sorouri, F.; Khayyatan, F.; Kiani, S. Human embryonic stem cell-derived neural stem cells encapsulated in hyaluronic acid promotes regeneration in a contusion spinal cord injured rat. Int. J. Biol. Macromol. 2020, 148, 1118–1129. [Google Scholar] [CrossRef]
- Sugai, K.; Nishimura, S.; Kato-Negishi, M.; Onoe, H.; Iwanaga, S.; Toyama, Y.; Matsumoto, M.; Takeuchi, S.; Okano, H.; Nakamura, M. Neural stem/progenitor cell-laden microfibers promote transplant survival in a mouse transected spinal cord injury model. J. Neurosci. Res. 2015, 93, 1826–1838. [Google Scholar] [CrossRef]
- Kim, B.G.; Kang, Y.M.; Phi, J.H.; Kim, Y.-H.; Hwang, D.H.; Choi, J.Y.; Ryu, S.; Elastal, A.-E.; Paek, S.H.; Wang, K.-C.; et al. Implantation of polymer scaffolds seeded with neural stem cells in a canine spinal cord injury model. Cytotherapy 2010, 12, 841–845. [Google Scholar] [CrossRef]
- McCreedy, D.A.; Wilems, T.S.; Xu, H.; Butts, J.C.; Brown, C.R.; Smith, A.W.; Sakiyama-Elbert, S.E. Survival, differentiation, and migration of high-purity mouse embryonic stem cell-derived progenitor motor neurons in fibrin scaffolds after sub-acute spinal cord injury. Biomater. Sci. 2014, 2, 1672–1682. [Google Scholar] [CrossRef]
- Jian, R.; Yixu, Y.; Sheyu, L.; Jianhong, S.; Yaohua, Y.; Xing, S.; Qingfeng, H.; Xiaojian, L.; Lei, Z.; Yan, Z.; et al. Repair of spinal cord injury by chitosan scaffold with glioma ECM and SB216763 implantation in adult rats. J. Biomed. Mater. Res. Part A 2015, 103, 3259–3272. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chu, R.; Ni, N.; Nan, G. The effect of Matrigel as scaffold material for neural stem cell transplantation for treating spinal cord injury. Sci. Rep. 2020, 10, 2576. [Google Scholar] [CrossRef]
- Zou, Y.; Zhao, Y.; Xiao, Z.; Chen, B.; Ma, D.; Shen, H.; Gu, R.; Dai, J. Comparison of Regenerative Effects of Transplanting Three-Dimensional Longitudinal Scaffold Loaded-Human Mesenchymal Stem Cells and Human Neural Stem Cells on Spinal Cord Completely Transected Rats. ACS Biomater. Sci. Eng. 2020, 6, 1671–1680. [Google Scholar] [CrossRef]
- Yang, L.; Conley, B.M.; Cerqueira, S.R.; Pongkulapa, T.; Wang, S.; Lee, J.K.; Lee, K.-B. Effective Modulation of CNS Inhibitory Microenvironment using Bioinspired Hybrid-Nanoscaffold-Based Therapeutic Interventions. Adv. Mater. 2020, 32, 2002578. [Google Scholar] [CrossRef]
- Nori, S.; Khazaei, M.; Ahuja, C.S.; Yokota, K.; Ahlfors, J.-E.; Liu, Y.; Wang, J.; Shibata, S.; Chio, J.; Hettiaratchi, M.H.; et al. Human Oligodendrogenic Neural Progenitor Cells Delivered with Chondroitinase ABC Facilitate Functional Repair of Chronic Spinal Cord Injury. Stem Cell Rep. 2018, 11, 1433–1448. [Google Scholar] [CrossRef]
- Sun, X.; Zhang, C.; Xu, J.; Zhai, H.; Liu, S.; Xu, Y.; Hu, Y.; Long, H.; Bai, Y.; Quan, D. Neurotrophin-3-Loaded Multichannel Nanofibrous Scaffolds Promoted Anti-Inflammation, Neuronal Differentiation, and Functional Recovery after Spinal Cord Injury. ACS Biomater. Sci. Eng. 2020, 6, 1228–1238. [Google Scholar] [CrossRef]
- Hatami, M.; Mehrjardi, N.Z.; Kiani, S.; Hemmesi, K.; Azizi, H.; Shahverdi, A.; Baharvand, H. Human embryonic stem cell-derived neural precursor transplants in collagen scaffolds promote recovery in injured rat spinal cord. Cytotherapy 2009, 11, 618–630. [Google Scholar] [CrossRef]
- Lu, P.; Graham, L.; Wang, Y.; Wu, D.; Tuszynski, M. Promotion of Survival and Differentiation of Neural Stem Cells with Fibrin and Growth Factor Cocktails after Severe Spinal Cord Injury. J. Vis. Exp. 2014, e50641. [Google Scholar] [CrossRef]
- Lu, P.; Wang, Y.; Graham, L.; McHale, K.; Gao, M.; Wu, D.; Brock, J.; Blesch, A.; Rosenzweig, E.S.; Havton, L.A.; et al. Long-Distance Growth and Connectivity of Neural Stem Cells after Severe Spinal Cord Injury. Cell 2012, 150, 1264–1273. [Google Scholar] [CrossRef]
- Mothe, A.J.; Tam, R.Y.; Zahir, T.; Tator, C.H.; Shoichet, M.S. Repair of the injured spinal cord by transplantation of neural stem cells in a hyaluronan-based hydrogel. Biomaterials 2013, 34, 3775–3783. [Google Scholar] [CrossRef]
- Führmann, T.; Tam, R.Y.; Ballarin, B.; Coles, B.; Donaghue, I.E.; van der Kooy, D.; Nagy, A.; Tator, C.H.; Morshead, C.M.; Shoichet, M.S. Injectable hydrogel promotes early survival of induced pluripotent stem cell-derived oligodendrocytes and attenuates longterm teratoma formation in a spinal cord injury model. Biomaterials 2016, 83, 23–36. [Google Scholar] [CrossRef]
- Koffler, J.; Zhu, W.; Qu, X.; Platoshyn, O.; Dulin, J.N.; Brock, J.; Graham, L.; Lu, P.; Sakamoto, J.; Marsala, M.; et al. Biomimetic 3D-printed scaffolds for spinal cord injury repair. Nat. Med. 2019, 25, 263–269. [Google Scholar] [CrossRef]
- Fan, L.; Liu, C.; Chen, X.; Zou, Y.; Zhou, Z.; Lin, C.; Tan, G.; Zhou, L.; Ning, C.; Wang, Q. Directing Induced Pluripotent Stem Cell Derived Neural Stem Cell Fate with a Three-Dimensional Biomimetic Hydrogel for Spinal Cord Injury Repair. ACS Appl. Mater. Interfaces 2018, 10, 17742–17755. [Google Scholar] [CrossRef]
- Zhang, L.; Fan, C.; Hao, W.; Zhuang, Y.; Liu, X.; Zhao, Y.; Chen, B.; Xiao, Z.; Chen, Y.; Dai, J. NSCs Migration Promoted and Drug Delivered Exosomes-Collagen Scaffold via a Bio-Specific Peptide for One-Step Spinal Cord Injury Repair. Adv. Healthc. Mater. 2021, 10, e2001896. [Google Scholar] [CrossRef]
- Zhou, X.; Shi, G.; Fan, B.; Cheng, X.; Zhang, X.; Wang, X.; Liu, S.; Hao, Y.; Wei, Z.; Wang, L.; et al. Polycaprolactone electrospun fiber scaffold loaded with iPSCs-NSCs and ASCs as a novel tissue engineering scaffold for the treatment of spinal cord injury. Int. J. Nanomed. 2018, 13, 6265–6277. [Google Scholar] [CrossRef]
- Shao, R.; Li, C.; Chen, Y.; Zhang, L.; Yang, H.; Zhang, Z.; Yue, J.; Gao, W.; Zhu, H.; Pan, H.; et al. LncRNA-GAS5 promotes spinal cord repair and the inhibition of neuronal apoptosis via the transplantation of 3D printed scaffold loaded with induced pluripotent stem cell-derived neural stem cells. Ann. Transl. Med. 2021, 9, 931. [Google Scholar] [CrossRef]
- Zarepour, A.; Öztürk, A.B.; Irmak, D.K.; Yaşayan, G.; Gökmen, A.; Karaöz, E.; Zarepour, A.; Zarrabi, A.; Mostafavi, E. Combination Therapy Using Nanomaterials and Stem Cells to Treat Spinal Cord Injuries. Eur. J. Pharm. Biopharm. 2022, 177, 224–240. [Google Scholar] [CrossRef]
- Nejati, K.; Mehdi, D.; Ghareghomi, S.; Mostafavi, E.; Ebrahimi-Kalan, A.; Biglari, A.; Alizadeh, E.; Mortazavi, Y.; Zarghami, N. GDNF gene-engineered adipose-derived stem cells seeded Emu oil-loaded electrospun nanofibers for axonal regeneration following spinal cord injury. J. Drug Deliv. Sci. Technol. 2020, 60, 102095. [Google Scholar] [CrossRef]
- Lv, B.; Zhang, X.; Yuan, J.; Chen, Y.; Ding, H.; Cao, X.; Huang, A. Biomaterial-supported MSC transplantation enhances cell–cell communication for spinal cord injury. Stem Cell Res. Ther. 2021, 12, 36. [Google Scholar] [CrossRef]
- Papa, S.; Vismara, I.; Mariani, A.; Barilani, M.; Rimondo, S.; De Paola, M.; Panini, N.; Erba, E.; Mauri, E.; Rossi, F.; et al. Mesenchymal stem cells encapsulated into biomimetic hydrogel scaffold gradually release CCL2 chemokine in situ preserving cytoarchitecture and promoting functional recovery in spinal cord injury. J. Control. Release 2018, 278, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-S.; Lee, Y.J.; Lee, S.H.; Lee, D.; Choi, K.; Kim, W.-H.; Kweon, O.-K.; Han, H.J. Functional recovery after spinal cord injury in dogs treated with a combination of Matrigel and neural-induced adipose-derived mesenchymal Stem cells. Cytotherapy 2012, 14, 584–597. [Google Scholar] [CrossRef]
- Raynald, S.B.; Liu, X.-B.; Zhou, J.F.; Huang, H.; Wang, J.-Y.; Sun, X.-D.; Qin, C.; An, Y.-H. Polypyrrole/polylactic acid nanofibrous scaffold cotransplanted with bone marrow stromal cells promotes the functional recovery of spinal cord injury in rats. CNS Neurosci. Ther. 2019, 25, 951–964. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Xu, H.-H.; Liu, X.-Y.; Zhang, Y.-S.; Zhong, L.; Wang, Y.-W.; Xu, L.; Wei, P.; Chen, Y.-X.; Liu, P.; et al. 3D printed collagen/silk fibroin scaffolds carrying the secretome of human umbilical mesenchymal stem cells ameliorated neurological dysfunction after spinal cord injury in rats. Regen. Biomater. 2022, 9, rbac014. [Google Scholar] [CrossRef]
- Zaviskova, K.; Tukmachev, D.; Dubisova, J.; Vackova, I.; Hejcl, A.; Bystronova, J.; Pravda, M.; Scigalkova, I.; Sulakova, R.; Velebny, V.; et al. Injectable hydroxyphenyl derivative of hyaluronic acid hydrogel modified with RGD as scaffold for spinal cord injury repair. J. Biomed. Mater. Res. Part A 2018, 106, 1129–1140. [Google Scholar] [CrossRef] [PubMed]
- Jiao, G.; Lou, G.; Mo, Y.; Pan, Y.; Zhang, Z.; Guo, R.; Li, Z. A combination of GDNF and hUCMSC transplantation loaded on SF/AGs composite scaffolds for spinal cord injury repair. Mater. Sci. Eng. C 2017, 74, 230–237. [Google Scholar] [CrossRef]
- Cholas, R.; Hsu, H.P.; Spector, M. Collagen Scaffolds Incorporating Select Therapeutic Agents to Facilitate a Reparative Response in a Standardized Hemiresection Defect in the Rat Spinal Cord. Tissue Eng. Part A 2012, 18, 2158–2172. [Google Scholar] [CrossRef]
- Terraf, P.; Kouhsari, S.M.; Ai, J.; Babaloo, H. Tissue-Engineered Regeneration of Hemisected Spinal Cord Using Human Endometrial Stem Cells, Poly ε-Caprolactone Scaffolds, and Crocin as a Neuroprotective Agent. Mol. Neurobiol. 2017, 54, 5657–5667. [Google Scholar] [CrossRef]
- Günther, M.I.; Weidner, N.; Müller, R.; Blesch, A. Cell-seeded alginate hydrogel scaffolds promote directed linear axonal regeneration in the injured rat spinal cord. Acta Biomater. 2015, 27, 140–150. [Google Scholar] [CrossRef]
- Zhang, J.; Cheng, T.; Chen, Y.; Gao, F.; Guan, F.; Yao, M.-H. A chitosan-based thermosensitive scaffold loaded with bone marrow-derived mesenchymal stem cells promotes motor function recovery in spinal cord injured mice. Biomed. Mater. 2020, 15, 035020. [Google Scholar] [CrossRef]
- Li, Y.; Yang, L.; Hu, F.; Xu, J.; Ye, J.; Liu, S.; Wang, L.; Zhuo, M.; Ran, B.; Zhang, H.; et al. Novel Thermosensitive Hydrogel Promotes Spinal Cord Repair by Regulating Mitochondrial Function. ACS Appl. Mater. Interfaces 2022, 14, 25155–25172. [Google Scholar] [CrossRef]
- Blaško, J.; Szekiova, E.; Slovinska, L.; Kafka, J.; Cizkova, D. Axonal outgrowth stimulation after alginate/mesenchymal stem cell therapy in injured rat spinal cord. Acta Neurobiol. Exp. 2017, 77, 337–350. [Google Scholar] [CrossRef]
- Zurita, M.; Otero, L.; Aguayo, C.; Bonilla, C.; Ferreira, E.; Parajón, A.; Vaquero, J. Cell therapy for spinal cord repair: Optimization of biologic scaffolds for survival and neural differentiation of human bone marrow stromal cells. Cytotherapy 2010, 12, 522–537. [Google Scholar] [CrossRef] [PubMed]
- An, H.; Li, Q.; Wen, J. Bone marrow mesenchymal stem cells encapsulated thermal-responsive hydrogel network bridges combined photo-plasmonic nanoparticulate system for the treatment of urinary bladder dysfunction after spinal cord injury. J. Photochem. Photobiol. B Biol. 2019, 203, 111741. [Google Scholar] [CrossRef]
- Chen, X.; Yang, Y.; Yao, J.; Lin, W.; Li, Y.; Chen, Y.; Gao, Y.; Yang, Y.; Gu, X.; Wang, X. Bone marrow stromal cells-loaded chitosan conduits promote repair of complete transection injury in rat spinal cord. J. Mater. Sci. Mater. Med. 2011, 22, 2347–2356. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Liu, Y.; Ding, J.; Dai, Y.; Le, L.; Wang, L.; Ding, E.; Yang, J. Thermosensitive quaternized chitosan hydrogel scaffolds promote neural differentiation in bone marrow mesenchymal stem cells and functional recovery in a rat spinal cord injury model. Cell Tissue Res. 2021, 385, 65–85. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Li, X.; Xiao, Z.; Yin, W.; Zhao, Y.; Tan, J.; Chen, B.; Jiang, X.; Dai, J. Different functional bio-scaffolds share similar neurological mechanism to promote locomotor recovery of canines with complete spinal cord injury. Biomaterials 2019, 214, 119230. [Google Scholar] [CrossRef]
- Wiseman, T.M.; Baron-Heeris, M.D.; Houwers, I.G.J.; Keenan, R.; Williams, R.J.; Nisbet, D.R.; Harvey, A.R.; Hodgetts, S.I. Peptide Hydrogel Scaffold for Mesenchymal Precursor Cells Implanted to Injured Adult Rat Spinal Cord. Tissue Eng. Part A 2021, 27, 993–1007. [Google Scholar] [CrossRef]
- Wang, X.-H.; Tang, X.-C.; Li, X.; Qin, J.-Z.; Zhong, W.-T.; Wu, P.; Zhang, F.; Shen, Y.-X.; Dai, T.-T. Implantation of nanofibrous silk scaffolds seeded with bone marrow stromal cells promotes spinal cord regeneration (6686 words). Artif. Cells, Nanomed. Biotechnol. 2021, 49, 699–708. [Google Scholar] [CrossRef]
- Han, I.-B.; Thakor, D.K.; Ropper, A.E.; Yu, D.; Wang, L.; Kabatas, S.; Zeng, X.; Kim, S.-W.; Zafonte, R.D.; Teng, Y.D. Physical impacts of PLGA scaffolding on hMSCs: Recovery neurobiology insight for implant design to treat spinal cord injury. Exp. Neurol. 2019, 320, 112980. [Google Scholar] [CrossRef]
- Kang, K.N.; Kim, D.Y.; Yoon, S.M.; Lee, J.Y.; Lee, B.N.; Kwon, J.S.; Seo, H.W.; Lee, I.W.; Shin, H.C.; Kim, Y.M.; et al. Tissue engineered regeneration of completely transected spinal cord using human mesenchymal stem cells. Biomaterials 2012, 33, 4828–4835. [Google Scholar] [CrossRef]
- Kang, K.N.; Lee, J.Y.; Kim, D.Y.; Lee, B.N.; Ahn, H.H.; Lee, B.; Khang, G.; Park, S.R.; Min, B.H.; Kim, J.H.; et al. Regeneration of Completely Transected Spinal Cord Using Scaffold of Poly(D,L-Lactide-co-Glycolide)/Small Intestinal Submucosa Seeded with Rat Bone Marrow Stem Cells. Tissue Eng. Part A 2011, 17, 2143–2152. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Gao, W.; Yue, B.; Jiang, J.; Gu, Y.; Dai, J.; Chen, L.; Shi, Q. Promotion of neurological recovery in rat spinal cord injury by mesenchymal stem cells loaded on nerve-guided collagen scaffold through increasing alternatively activated macrophage polarization. J. Tissue Eng. Regen. Med. 2018, 12, e1725–e1736. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Yuan, W.; Ding, L.; Shi, M.; Luo, L.; Wan, Y.; Oh, J.; Zhou, Y.; Bian, L.; Deng, D.Y.B. Cell-adaptable dynamic hydrogel reinforced with stem cells improves the functional repair of spinal cord injury by alleviating neuroinflammation. Biomaterials 2021, 279, 121190. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wan, J.; Dai, M.; Ye, X.; Liu, C.; Tang, C.; Zhu, L. Effects of oxygen generating scaffolds on cell survival and functional recovery following acute spinal cord injury in rats. J. Mater. Sci. Mater. Med. 2020, 31, 115. [Google Scholar] [CrossRef] [PubMed]
- Ropper, A.E.; Thakor, D.K.; Han, I.; Yu, D.; Zeng, X.; Anderson, J.E.; Aljuboori, Z.; Kim, S.-W.; Wang, H.; Sidman, R.L.; et al. Defining recovery neurobiology of injured spinal cord by synthetic matrix-assisted hMSC implantation. Proc. Natl. Acad. Sci. USA 2017, 114, E820–E829. [Google Scholar] [CrossRef]
- Li, X.; Tan, J.; Xiao, Z.; Zhao, Y.; Han, S.; Liu, D.; Yin, W.; Li, J.; Li, J.; Wanggou, S.; et al. Transplantation of hUC-MSCs seeded collagen scaffolds reduces scar formation and promotes functional recovery in canines with chronic spinal cord injury. Sci. Rep. 2017, 7, 43559. [Google Scholar] [CrossRef]
- Li, L.; Xiao, B.; Mu, J.; Zhang, Y.; Zhang, C.; Cao, H.; Chen, R.; Patra, H.K.; Yang, B.; Feng, S.; et al. A MnO2 Nanoparticle-Dotted Hydrogel Promotes Spinal Cord Repair via Regulating Reactive Oxygen Species Microenvironment and Synergizing with Mesenchymal Stem Cells. ACS Nano 2019, 13, 14283–14293. [Google Scholar] [CrossRef]
- Li, Y.; Cao, X.; Deng, W.; Yu, Q.; Sun, C.; Ma, P.; Shao, F.; Yusif, M.M.; Ge, Z.; Wang, K.; et al. 3D printable Sodium alginate-Matrigel (SA-MA) hydrogel facilitated ectomesenchymal stem cells (EMSCs) neuron differentiation. J. Biomater. Appl. 2021, 35, 709–719. [Google Scholar] [CrossRef] [PubMed]
- Monje, P.V.; Deng, L.; Xu, X.-M. Human Schwann Cell Transplantation for Spinal Cord Injury: Prospects and Challenges in Translational Medicine. Front. Cell. Neurosci. 2021, 15, 690894. [Google Scholar] [CrossRef] [PubMed]
- Hakim, J.S.; Rad, M.E.; Grahn, P.J.; Chen, B.K.; Knight, A.M.; Schmeichel, A.M.; Isaq, N.A.; Dadsetan, M.; Yaszemski, M.J.; Windebank, A.J. Positively Charged Oligo[Poly(Ethylene Glycol) Fumarate] Scaffold Implantation Results in a Permissive Lesion Environment after Spinal Cord Injury in Rat. Tissue Eng. Part A 2015, 21, 2099–2114. [Google Scholar] [CrossRef]
- Hurtado, A.; Moon, L.D.; Maquet, V.; Blits, B.; Jérôme, R.; Oudega, M. Poly (d,l-lactic acid) macroporous guidance scaffolds seeded with Schwann cells genetically modified to secrete a bi-functional neurotrophin implanted in the completely transected adult rat thoracic spinal cord. Biomaterials 2006, 27, 430–442. [Google Scholar] [CrossRef]
- Liu, S.; Sandner, B.; Schackel, T.; Nicholson, L.; Chtarto, A.; Tenenbaum, L.; Puttagunta, R.; Müller, R.; Weidner, N.; Blesch, A. Regulated viral BDNF delivery in combination with Schwann cells promotes axonal regeneration through capillary alginate hydrogels after spinal cord injury. Acta Biomater. 2017, 60, 167–180. [Google Scholar] [CrossRef]
- Moore, M.J.; Friedman, J.A.; Lewellyn, E.B.; Mantila, S.M.; Krych, A.J.; Ameenuddin, S.; Knight, A.M.; Lu, L.; Currier, B.L.; Spinner, R.J.; et al. Multiple-channel scaffolds to promote spinal cord axon regeneration. Biomaterials 2006, 27, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Oudega, M.; Gautier, S.E.; Chapon, P.; Fragoso, M.; Bates, M.L.; Parel, J.M.; Bunge, M.B. Axonal regeneration into Schwann cell grafts within resorbable poly(α-hydroxyacid) guidance channels in the adult rat spinal cord. Biomaterials 2001, 22, 1125–1136. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.K.; Knight, A.M.; de Ruiter, G.C.; Spinner, R.J.; Yaszemski, M.J.; Currier, B.L.; Windebank, A.J. Axon regeneration through scaffold into distal spinal cord after transection. J. Neurotrauma 2009, 6, 1759–1771. [Google Scholar] [CrossRef] [PubMed]
- Novikov, L.N.; Novikova, L.N.; Mosahebi, A.; Wiberg, M.; Terenghi, G.; Kellerth, J.-O. A novel biodegradable implant for neuronal rescue and regeneration after spinal cord injury. Biomaterials 2002, 23, 3369–3376. [Google Scholar] [CrossRef]
- Novikova, L.N.; Pettersson, J.; Brohlin, M.; Wiberg, M.; Novikov, L.N. Biodegradable poly-β-hydroxybutyrate scaffold seeded with Schwann cells to promote spinal cord repair. Biomaterials 2008, 29, 1198–1206. [Google Scholar] [CrossRef] [PubMed]
- Babaloo, H.; Ebrahimi-Barough, S.; Derakhshan, M.A.; Yazdankhah, M.; Lotfibakhshaiesh, N.; Soleimani, M.; Joghataei, M.-T.; Ai, J. PCL/gelatin nanofibrous scaffolds with human endometrial stem cells/Schwann cells facilitate axon regeneration in spinal cord injury. J. Cell. Physiol. 2019, 234, 11060–11069. [Google Scholar] [CrossRef] [PubMed]
- Yang, E.-Z.; Zhang, G.-W.; Xu, J.-G.; Chen, S.; Wang, H.; Cao, L.-L.; Liang, B.; Lian, X.-F. Multichannel polymer scaffold seeded with activated Schwann cells and bone mesenchymal stem cells improves axonal regeneration and functional recovery after rat spinal cord injury. Acta Pharmacol. Sin. 2017, 38, 623–637. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, X.; Feng, G.; Gu, Z.; Sun, Y.; Bao, G.; Xu, G.; Lu, Y.; Chen, J.; Xu, L.; et al. Chitosan scaffolds induce human dental pulp stem cells to neural differentiation: Potential roles for spinal cord injury therapy. Cell Tissue Res. 2016, 366, 129–142. [Google Scholar] [CrossRef]
- Li, X.; Yang, C.; Li, L.; Xiong, J.; Xie, L.; Yang, B.; Yu, M.; Feng, L.; Jiang, Z.; Guo, W.; et al. A Therapeutic Strategy for Spinal Cord Defect: Human Dental Follicle Cells Combined with Aligned PCL/PLGA Electrospun Material. BioMed Res. Int. 2015, 2015, 197183. [Google Scholar] [CrossRef]
- Thompson, R.E.; Pardieck, J.; Smith, L.; Kenny, P.; Crawford, L.; Shoichet, M.; Sakiyama-Elbert, S. Effect of hyaluronic acid hydrogels containing astrocyte-derived extracellular matrix and/or V2a interneurons on histologic outcomes following spinal cord injury. Biomaterials 2018, 162, 208–223. [Google Scholar] [CrossRef]
- Wang, C.; Sun, C.; Hu, Z.; Huo, X.; Yang, Y.; Liu, X.; Botchway, B.O.A.; Davies, H.; Fang, M. Improved Neural Regeneration with Olfactory Ensheathing Cell Inoculated PLGA Scaffolds in Spinal Cord Injury Adult Rats. Neurosignals 2017, 25, 1–14. [Google Scholar] [CrossRef]
- Ferrero-Gutierrez, A.; Menendez-Menendez, Y.; Alvarez-Viejo, M.; Meana, A.; Otero, J. New serum-derived albumin scaffold seeded with adipose-derived stem cells and olfactory ensheathing cells used to treat spinal cord injured rats. Histol. Histopathol. 2013, 28, 89–100. [Google Scholar] [CrossRef]
- Wang, N.; Xiao, Z.; Zhao, Y.; Wang, B.; Li, X.; Li, J.; Dai, J. Collagen scaffold combined with human umbilical cord-derived mesenchymal stem cells promote functional recovery after scar resection in rats with chronic spinal cord injury. J. Tissue Eng. Regen. Med. 2018, 12, e1154–e1163. [Google Scholar] [CrossRef]
- Amr, S.M.; Gouda, A.; Koptan, W.T.; Galal, A.A.; Abdel-Fattah, D.S.; Rashed, L.A.; Atta, H.M.; Abdel-Aziz, M.T. Bridging defects in chronic spinal cord injury using peripheral nerve grafts combined with a chitosan-laminin scaffold and enhancing regeneration through them by co-transplantation with bone-marrow-derived mesenchymal stem cells: Case series of 14 patients. J. Spinal Cord Med. 2014, 37, 54–71. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Prabhakaran, M.P.; Ramakrishna, S. Strategies for regeneration of components of nervous system: Scaffolds, cells and biomolecules. Regen. Biomater. 2015, 2, 31–45. [Google Scholar] [CrossRef]
- Raspa, A.; Marchini, A.; Pugliese, R.; Mauri, M.; Maleki, M.; Vasita, R.; Gelain, F. A biocompatibility study of new nanofibrous scaffolds for nervous system regeneration. Nanoscale 2016, 8, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, D.; Xiao, Z.; Zhao, Y.; Han, S.; Chen, B.; Dai, J. Scaffold-facilitated locomotor improvement post complete spinal cord injury: Motor axon regeneration versus endogenous neuronal relay formation. Biomaterials 2019, 197, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Bajo, A.; González-Mayorga, A.; Guerrero, C.R.; Palomares, F.J.; García, R.; López-Dolado, E.; Serrano, M.C. Myelinated axons and functional blood vessels populate mechanically compliant rGO foams in chronic cervical hemisected rats. Biomaterials 2019, 192, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Austin, J.W.; Kang, C.E.; Baumann, M.D.; DiDiodato, L.; Satkunendrarajah, K.; Wilson, J.R.; Stanisz, G.J.; Shoichet, M.S.; Fehlings, M.G. The effects of intrathecal injection of a hyaluronan-based hydrogel on inflammation, scarring and neurobehavioural outcomes in a rat model of severe spinal cord injury associated with arachnoiditis. Biomaterials 2012, 33, 4555–4564. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Wang, Y.; Zhu, M.; Wan, X.; Zhang, H.; Lei, T.; Blesch, A.; Liu, S. Anisotropic Alginate Hydrogels Promote Axonal Growth across Chronic Spinal Cord Transections after Scar Removal. ACS Biomater. Sci. Eng. 2020, 6, 2274–2286. [Google Scholar] [CrossRef] [PubMed]
- Tavakol, S.; Saber, R.; Hoveizi, E.; Aligholi, H.; Ai, J.; Rezayat, S.M. Chimeric Self-assembling Nanofiber Containing Bone Marrow Homing Peptide’s Motif Induces Motor Neuron Recovery in Animal Model of Chronic Spinal Cord Injury; an In Vitro and In Vivo Investigation. Mol. Neurobiol. 2016, 53, 3298–3308. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Gao, M.; Lin, J.; Wu, W.; Wang, J.; Chew, S.Y. Three-dimensional aligned nanofibers-hydrogel scaffold for controlled non-viral drug/gene delivery to direct axon regeneration in spinal cord injury treatment. Sci. Rep. 2017, 7, srep42212, Erratum in Sci. Rep. 2018, 8, 13057. [Google Scholar] [CrossRef] [PubMed]
- López-Dolado, E.; González-Mayorga, A.; Gutiérrez, M.C.; Serrano, M.C. Immunomodulatory and angiogenic responses induced by graphene oxide scaffolds in chronic spinal hemisected rats. Biomaterials 2016, 99, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Gelain, F.; Panseri, S.; Antonini, S.; Cunha, C.; Donega, M.; Lowery, J.; Taraballi, F.; Cerri, G.; Montagna, M.; Baldissera, F.; et al. Transplantation of Nanostructured Composite Scaffolds Results in the Regeneration of Chronically Injured Spinal Cords. ACS Nano 2011, 5, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Tang, F.; Zhao, Y.; Han, G.; Yin, N.; Li, X.; Chen, B.; Han, S.; Jiang, X.; Yun, C.; et al. Significant Improvement of Acute Complete Spinal Cord Injury Patients Diagnosed by a Combined Criteria Implanted with NeuroRegen Scaffolds and Mesenchymal Stem Cells. Cell Transplant. 2018, 27, 907–915. [Google Scholar] [CrossRef]
| Effect on Pathophysiological Events | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Location of Injury | Species | Application | Hydrogel (Character) | Anti-Inflammation | Scar/Cavity | Axon Growth | Angiogenesis | Motor Functional Recovery |
| Sun Y, et al., 2019 [33] | Thoracic | Rat | Implant | Collagen/Chitosan (3D printing) | NA | + | + | NA | + |
| Marchand R, et al., 1990 [34] | Thoracic | Rat | Implant | Collagen (Self assembling) | NA | + | + | NA | NA |
| Khan T, et al., 1991 [35] | Thoracic | Rat | Implant | Carbon (Filament) | NA | + | + | NA | NA |
| Liu W, et al., 2020 [36] | Thoracic | Rat | Implant | Collagen (modified with N-cadherin) | NA | + | + | NA | + |
| Fan C, et al., 2017 [37] | Thoracic | Rat | Implant | Collagen (binding with EGFR antibody Fab fragment) | NA | + | + | NA | + |
| Yang B, et al., 2017 [38] | Thoracic | Rat | Implant | Agarose/gelatin/polypyrrole (similar conductivity as the spinal cord) | + | + | + | NA | + |
| Martín-López E, et al., 2013 [39] | Thoracic | Rat | Implant | Agarose with κ-carrageenan, gelatin, xanthan gum and polysulfone | NA | + | + | NA | NA |
| Gros T, et al., 2010 [40] | Cervical | Rat | Implant | Agarose | NA | + | + | NA | NA |
| Kataoka K, et al., 2004 [41] | Thoracic | Rat | Implant | Alginate (Freeze-dried sponge ) | NA | + | + | NA | NA |
| Prang P, et al., 2006 [42] | Cervical | Rat | Implant | Alginate (Anisotropic capillary) | NA | + | + | NA | NA |
| Cao Z, et al., 2020 [43] | Lumbar | Canine | Implant | Fibrin (Hierarchically aligned fibrin hydrogel) | NA | + | + | NA | + |
| Yin W, et al., 2021 [44] | Thoracic | Canine | Implant | Collagen (Taxol-modified linear-ordered scaffold) | NA | + | + | NA | NA |
| Altinova H, et al., 2020 [45] | Cervical | Rat | Implant | Collagen | NA | + | + | + | NA |
| Gholami M, et al., 2021 [46] | Thoracic | Rat | Implant | Chitosan/alginate/erythropoietin | + | + | + | NA | NA |
| Stokols S, et al., 2006 [47] | Cervical | Rat | Implant | Alginate (recombinant BDNF protein) | NA | + | + | NA | NA |
| Zhang Z, et al., 2017 [48] | Lumbar | Canine | Implant | Biomaterial-aligned fibrin | + | + | + | NA | + |
| Fukushima K, et al., 2008 [49] | Thoracic | Rat | Implant | Collagen (Honeycomb) | NA | NA | + | NA | NA |
| Zhao X, et al., 2022 [50] | Thoracic | Rat | Implant | Gelatin/hyaluronic acid | + | + | + | NA | + |
| King VR, et al., 2010 [51] | Thoracic | Rat | Implant | Collagen (viscous fibronectin gel) | NA | NA | + | NA | NA |
| Cheng H, et al., 2007 [52] | Thoracic | Rat | Implant | Chitosan | NA | + | + | NA | - |
| Han S, et al., 2018 [53] | Thoracic | Rat | Implant | Agarose (Matrigel) | NA | NA | + | NA | + |
| Bakshi A, et al., 2004 [54] | Cervical | Rat | Implant | Nonbiodegradable hydrogel (pPHEMA) | + | + | + | + | NA |
| Zhai H, et al., 2020 [55] | Thoracic | Rat | Implant | ADA16 peptide hydrogel | NA | + | + | + | NA |
| Hejčl A, et al., 2018 [56] | Thoracic | Rat | Implant | 3 Methacrylate hydrogel | NA | + | + | + | + |
| Zhang Q, et al., 2016 [57] | Thoracic | Rat | Implant | Silk protein/laminin | NA | + | + | + | + |
| Chai Y, et al., 2022 [58] | Thoracic | Rat | Implant | Bioactive isoleucine-lysine-valine-alanine-valine | NA | + | + | + | + |
| Yang Y, et al., 2021 [60] | Thoracic | Rat | Implant | Injectable collagen hydrogel | NA | + | + | NA | + |
| Silva NA, et al., 2010 [59] | Thoracic | Rat | Implant | Starch/poly-e-caprolactone blend and gellan gum | + | NA | NA | NA | NA |
| Suzuki H, et al., 2015 [61] | Thoracic | Rat | Implant | Collagen filaments | NA | + | + | NA | NA |
| Yara T, et al., 2009 [62] | Thoracic | Rat | Implant | Collagen filaments | NA | + | + | NA | NA |
| Effect On Pathophysiological Events | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Location of Injury | Species | Application | Biodegradable Scaffold/(Character) | Anti-Inflammation | Scar/Cavity | Axon Growth | Angiogenesis | Motor Functional Recovery |
| Kubinová Š, et al., 2015 [66] | Thoracic | Rat | Implant | SIKVAV-modified PHEMA | NA | + | + | + | NA |
| Hejcl A, et al., 2008 [67] | Thoracic | Rat | Implant | 2-hydroxyethyl methacrylate | NA | + | + | + | NA |
| Slotkin JR, et al., 2017 [69] | Thoracic | The green monkey | Implant | Poly-lactic-co-glycolic acid and Poly-l-lysine | + | + | + | NA | NA |
| Silva NA, et al., 2013 [70] | Thoracic | Rat | Implant | Starch with polycaprolactone | NA | + | + | NA | + |
| Thomas AM, et al., 2013 [71] | Thoracic | Rat/Mouse | Implant | Poly(lactide-co-glycolide) multiple channel bridges | NA | + | + | NA | NA |
| Man W, et al., 2021 [72] | Thoracic | Rat | Implant | Hierarchically aligned fibrin hydrogel and functionalized self-assembling peptides | NA | + | + | + | + |
| Kubinová S, et al., 2011 [73] | Thoracic | Rat | Implant | Highly superporous cholesterol-modified poly(2-hydroxyethyl methacrylate) scaffolds | NA | + | + | + | NA |
| Guest JD, et al., 2018 [74] | Thoracic | Thoracic | Implant | PLGA-PLL | NA | + | + | NA | - |
| Hakim JS, et al., 2019 [75] | Thoracic | Rat | Implant | PLGA-PLL | NA | + | + | NA | - |
| Anzalone A, et al., 2018 [76] | Cervical | Mouse | Implant | Poly-lactic-co-glycolic | NA | NA | + | NA | NA |
| De Laporte L, et al., 2009 [77] | Thoracic | Rat | Implant | Poly-lactic-co-glycolic/(Lipoplex incubation on ECM-coated PLG) | NA | NA | NA | NA | NA |
| Wong DY, et al., 2008 [78] | Thoracic | Rat | Implant | Salt-leached porous poly (epsilon-caprolactone) | NA | NA | + | NA | NA |
| Ribeiro-Samy S, et al., 2013 [79] | Thoracic | Rat | Implant | Poly(3-hydroxybutyrateco- 3-hydroxyvalerate) (PHB-HV) | NA | NA | NA | NA | - |
| Pawar K, et al., 2015 [80] | Cervical | Mouse | Implant | Poly-lactic-co-glycolic | NA | NA | + | NA | + |
| Rooney GE, et al., 2008 [81] | Thoracic | Rat | Implant | Radiopaque barium sulfate-impregnated poly-lactic-co-glycolic acid | NA | NA | NA | NA | NA |
| Shu B, et al., 2019 [82] | Thoracic | Rat | Implant | PLA-PPy | + | + | + | NA | + |
| Zhou L, et al., 2018 [83] | Thoracic | Mouse | Implant | Plant-derived polyphenol, tannic acid (TA), cross-linking and doping conducting polypyrrole (PPy) chains | NA | + | + | NA | + |
| Pertici VA, et al., 2014 [84] | Thoracic | Rat | Implant | PLA-b-PHEMA block copolymer | + | + | + | + | + |
| Reis KP, et al., 2020 [85] | Thoracic | Rat | Implant | Valproic acid (VPA)/PLGA (Microfiber) | + | + | + | + | + |
| Novikova LN, et al., 2017 [86] | Cervical | Rat | Implant | Trimethylene carbonate and e-caprolactone (TC) containing poly-p-dioxanone microfilaments (PDO) | - | + | + | NA | NA |
| Effect on Pathophysiological Events | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Location of Injury | Species | Application | Nanomaterial Scaffold/Material | Anti-Inflammation | Scar/Cavity | Axon Growth | Angiogenesis | Motor Functional Recovery |
| Zamani F, et al., 2014 [89] | Thoracic | Rat | Implant | 3D nanofibrous core–sheath scaffold/PLGA | NA | NA | + | + | + |
| Sun X, et al., 2019 [90] | Thoracic | Rat | Implant | Nano-fibrous channel wall/PLLA | + | + | + | NA | + |
| Cigognini D, et al., 2014 [91] | Thoracic | Rat | Injected | Nanostructures of two self-assembling peptides B24 and biotin-LDLK12 | NA | NA | + | NA | NA |
| Yao S, et al., 2018 [92] | Thoracic | Rat | Implant | Hierarchically aligned fibrin nanofiber/Fibrin hydrogel | NA | + | + | + | + |
| Altinova H, et al., 2016 [93] | Cervical | Rat | Implant | Microstructured scaffold/Collagen | + | + | + | + | + |
| Usmani S, et al., 2020 [94] | Thoracic | Rat | Implant | Artificial nanotube/Carbon | + | + | + | NA | + |
| Sever-Bahcekapili M, et al., 2020 [95] | Thoracic | Rat | Implant | Neuroactive peptide nanofibers/ LN-PA, GAG-PA | NA | + | + | NA | + |
| Zhao T, et al., 2018 [96] | Thoracic | Rat | Implant | Nanofibrous scaffolds/ PHBV, PLA, Collagen | NA | + | + | NA | - |
| Chedly JL, et al., 2017 [97] | Thoracic | Rat | Implant | Microhydrogel scaffold/Chitosan | + | + | + | + | + |
| Cigognini D, et al., 2011 [98] | Thoracic | Rat | Implant | Nanomaterial SAPs with bone marrow homing motif (BMHP1) | + | + | + | + | + |
| Palejwala AH, et al., 2016 [99] | Thoracic | Rat | Implant | Poly (3-hydroxybutyrateco- 3-hydroxyvalerate) (PHB-HV) | NA | NA | NA | NA | - |
| Palejwala AH, et al., 2016 [99] | Thoracic | Rat | Implant | Nanoscaffolds | NA | + | + | + | NA |
| Pawelec KM, et al., 2018 [100] | Thoracic | Rat | Implant | Microstructure multi-channel scaffold/PCL | NA | NA | + | NA | NA |
| Milbreta U, 2016 [101] | Cervical | Rat | Implant | 3D nanofiber scaffold/Collagen | + | + | + | NA | NA |
| Tysseling VM, et al., 2010 [102] | Thoracic | Rat | Injected | Peptide amphiphile (PA) molecules that self-assemble and display the laminin epitope IKVAV | NA | + | + | NA | + |
| Liu Y, et al., 2013 [103] | Thoracic | Rat | Injected | A self-assembling peptide/ K2(QL)6K2 (QL6) | + | + | + | NA | + |
| Effect on Pathophysiological Events | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Location of Injury | Species | Combinatory Agent | Biomaterial Scaffold | Anti-Inflammation | Scar/Cavity | Axon Growth | Angiogenesis | Facilitation of Cell Migration | Motor Functional Recovery |
| Furuya T, et al., 2013 [105] | Thoracic | Rat | bFGF | Gelatin hydrogel | NA | NA | NA | NA | NA | NA |
| Chantal SA, et al., 2008 [106] | Thoracic | Rat | Methylprednisolone | Biodegradable PLGA-based nanoparticles | + | + | NA | NA | + | NA |
| Jain A, et al., 2011 [108] | Thoracic | Rat | Constitutively active Cdc42, Rac1, BDNF | Microtubule-mediated slow release of BDNF | + | + | + | NA | + | NA |
| Wen Y et al., 2016 [109] | Thoracic | Rat | Anti-Nogo receptor antibody | PLGA microspheres containing BDNF and VEGF | + | + | + | + | + | + |
| Chen B, et al., 2015 [110] | Thoracic | Rat | bFGF | HEMA-MOETACL hydrogel | NA | + | + | NA | NA | + |
| Lin J, et al., 2019 [114] | Thoracic | Rat | Rehabilitation | Hybrid fiber-hydrogel scaffold | + | + | + | NA | + | + |
| Shi Q, et al., 2014 [115] | Thoracic | Rat | bFGF | Collagen scaffold | NA | + | + | NA | + | + |
| Wang X, et al., 2013 [116] | Thoracic | Rat | NT-3 | Chitosan-based tube scaffold | NA | + | + | NA | + | + |
| Li G, et al., 2016 [117] | Thoracic | Rat and canine | NT-3 | Fibrin-coated gelatin sponge scaffold | + | + | + | NA | + | + |
| Wei YT, et al., 2010 [118] | Thoracic | Rat | Nogo-66 receptor antibody | Hyaluronic acid -based hydrogels modified with poly-L-lysine (PLL) | + | + | + | + | + | NA |
| Bighinati A, et al., 2020 [119] | Thoracic | Rat | Ibuprofen and triiodothyronine | PLLA | + | + | + | NA | + | + |
| Ehsanipour A, et al., 2021 [120] | Thoracic | Mouse | BDNF | Hyaluronic acid (HA)-based, spherical microparticle | + | + | + | NA | + | + |
| Xie J, et al., 2022 [121] | Thoracic | Mouse | Sonic hedgehog (Shh) and retinoic acid (RA) | Magnesium oxide (MgO)/ poly (l-lactide-co-ε-caprolactone) (PLCL) scaffold | + | + | + | NA | + | NA |
| Xi K, et al., 2020 [122] | Thoracic | Rat | NGF | Microenvironment-responsive immunoregulatory electrospun fibers | + | + | + | NA | + | + |
| Rooney GE, et al., 2011 [123] | Thoracic | Rat | Dibutyryl cyclic adenosine monophosphate (dbcAMP) | Oligo [(polyethylene glycol) fumarate] (OPF) hydrogel scaffolds | NA | NA | + | NA | NA | NA |
| Stropkovská A, et al., 2022 [124] | Thoracic | Rat | Rho-A-kinase inhibitor | Chitosan/collagen porous scaffold | + | + | + | NA | + | NA |
| Man W, et al., 2021 [72] | Thoracic | Rat | Hierarchically aligned fibrin hydrogel | Functionalized self-assembling peptides (fSAP) | + | + | + | + | + | + |
| Smith DR, et al., 2020 [128] | Cervical | Mouse | IL-10 and NT-3 | Multiple channel PLG | + | NA | + | NA | + | + |
| Breen BA, et al., 2017 [130] | Thoracic | Rat | NT-3 | Injectable collagen scaffold | NA | + | + | NA | + | + |
| Wen Y et al., 2016 [109] | Thoracic | Rat | AntiNogo, BDNF and vascular endothelial growth factor | Hyaluronic acid (HA) hydrogel | + | + | + | + | + | + |
| Jain A, et al., 2006 [129] | Thoracic | Rat | BDNF | Gelling agarose hydrogels | NA | + | + | NA | + | NA |
| Type of Grafted Cells | Biomaterial Scaffold | Results/Advantages | Limitations/Disadvantages |
|---|---|---|---|
| NPCs |
|
|
|
| BMCSs |
|
|
|
| Umbilical MSCs/Wharton’s jelly-derived MSCs |
| ||
| Adipose-derived stem/stromal cells |
| ||
| Schwann cells (SCs) |
|
|
|
| OECs |
|
|
|
| Spinal cord-derived ependymal progenitor cells |
|
|
|
| Dental pulp stem cells/Dental follicle cells |
|
|
|
| NPCs and Schwann cells |
|
|
|
| BMSCs and Schwann cells |
|
|
|
| Endometrial stem cells and Schwann cells |
|
|
|
| Dermal fibroblast-reprogrammed neurons |
|
|
|
| Adipose-derived stem cells and OECs |
|
|
|
| NPCs and MSCs |
|
|
|
| Effect on Pathophysiological Events | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Location of Injury | Ongoing Clinical Trials (Identifier) | Phase | Combinatory Agent | Biomaterial Scaffold | Motor Function | Sensory Function | Anti-Inflammation | Scar/Cavity | Axon Growth | Angiogenesis | Facilitation of Cell Migration |
| - | Cervical/Thoracic | NCT02688049 | Phase 1 Phase 2 | NSCs and MSCs | NeuroRegen scaffold | - | - | - | - | - | - | - |
| - | Cervical/Thoracic | NCT02352077 | Phase 1 | Bone marrow mononuclear cells and MSCs | NeuroRegen scaffold | - | - | - | - | - | - | - |
| - | Cervical/Thoracic | NCT02688062 | Phase 1 Phase 2 | Bone marrow mononuclear cells | NeuroRegen scaffold | - | - | - | - | - | - | - |
| - | Thoracic | NCT02138110 | Not Applicable | Poly(lactic-co-glycolic acid)-b-poly(L-lysine) scaffold | - | - | - | - | - | - | - | |
| - | Thoracic | NCT03762655 | Not Applicable | Poly(lactic-co-glycolic acid)-b-poly(L-lysine) scaffold | - | - | - | - | - | - | - | |
| - | Thoracic | NCT02510365 | Phase 1 | Collagen scaffold | - | - | - | - | - | - | - | |
| - | Cervical/Thoracic | NCT03966794 | Phase 1 Phase 2 | Epidural Electrical Stimulation | Collagen scaffold | - | - | - | - | - | - | - |
| - | Thoracic/Lumbar | NCT02326662 | Phase 1 Phase 2 | Autologous NSCs | RMx Biomatrix | - | - | - | - | - | - | - |
| Amr SM, et al., 2014 [226] | Thoracic | - | - | BMSCs/peripheral nerve grafts | Chitosan-laminin scaffold | Several cases improved | Several cases improved | NA | NA | NA | NA | NA |
| Xiao Z, et al., 2018 [237] | Cervical/Thoracic | - | - | MSCs | NeuroRegen scaffold | Several cases improved | Several cases improved | NA | NA | NA | NA | NA |
| Chen W, et al., 2020 [133] | Thoracic | - | - | Bone marrow mononuclear cells | NeuroRegen scaffold | - | Several cases improved | NA | NA | NA | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, H.; Imajo, Y.; Funaba, M.; Ikeda, H.; Nishida, N.; Sakai, T. Current Concepts of Biomaterial Scaffolds and Regenerative Therapy for Spinal Cord Injury. Int. J. Mol. Sci. 2023, 24, 2528. https://doi.org/10.3390/ijms24032528
Suzuki H, Imajo Y, Funaba M, Ikeda H, Nishida N, Sakai T. Current Concepts of Biomaterial Scaffolds and Regenerative Therapy for Spinal Cord Injury. International Journal of Molecular Sciences. 2023; 24(3):2528. https://doi.org/10.3390/ijms24032528
Chicago/Turabian StyleSuzuki, Hidenori, Yasuaki Imajo, Masahiro Funaba, Hiroaki Ikeda, Norihiro Nishida, and Takashi Sakai. 2023. "Current Concepts of Biomaterial Scaffolds and Regenerative Therapy for Spinal Cord Injury" International Journal of Molecular Sciences 24, no. 3: 2528. https://doi.org/10.3390/ijms24032528
APA StyleSuzuki, H., Imajo, Y., Funaba, M., Ikeda, H., Nishida, N., & Sakai, T. (2023). Current Concepts of Biomaterial Scaffolds and Regenerative Therapy for Spinal Cord Injury. International Journal of Molecular Sciences, 24(3), 2528. https://doi.org/10.3390/ijms24032528







