Evaluation of In Vitro Synergistic Effects of Tetracycline with Alkaloid-Related Compounds against Diarrhoeic Bacteria
Abstract
1. Introduction
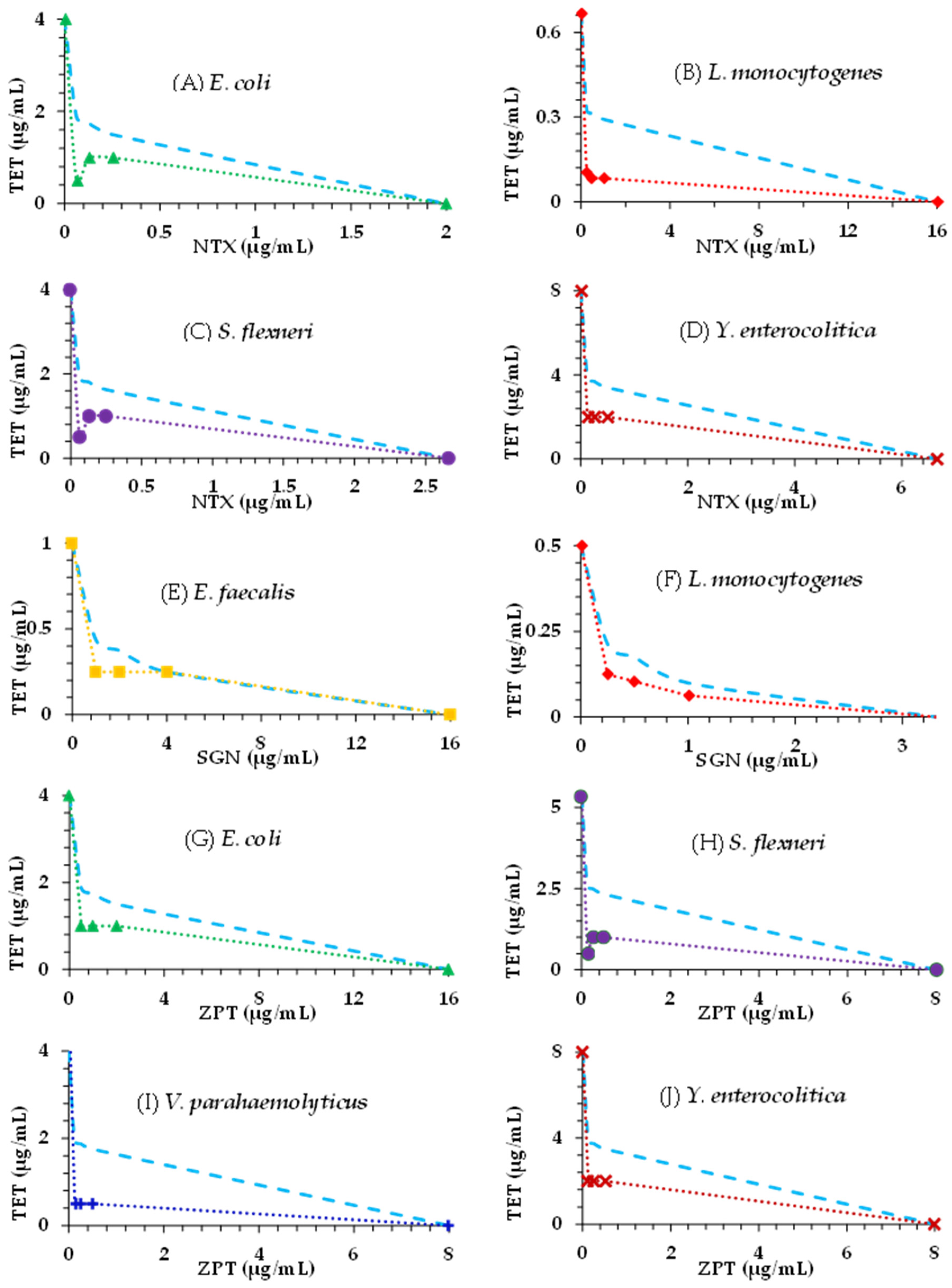
2. Results
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Bacterial Strains and Growth Media
4.3. Chequerboard Assay
4.4. Evaluation of Combination Effects
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the global burden of disease study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [Google Scholar] [CrossRef] [PubMed]
- Kosek, M.; Bern, C.; Guerrant, R.L. The magnitude of the global burden of diarrhea from studies published 1992–2000. Bull. World Health Organ. 2003, 81, 197–204. [Google Scholar] [PubMed]
- Diarrhoeal Disease. 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease (accessed on 29 July 2022).
- Cooke, M.L. Causes and management of diarrhoea in children in a clinical setting. South. Afr. J. Clin. Nutr. 2010, 23, 42–46. [Google Scholar] [CrossRef]
- Sah, R.; Khadka, S.; Shah, D.; Adhikari, M.; Shrestha, N.; Kattel, H.P.; Sharma, S.; Mishra, S.; Parajuli, K.; Sherchand, J.; et al. Vancomycin resistant Enterococcus faecalis causing diarrhea in renal transplant patient. Int. Educ. Sci. Res. J. 2019, 2, 9. [Google Scholar]
- Al-Dahmoshi, H.O.M.; Rabeea, H.W.S.; Aridhee, A.S.A.; Al-Khafaji, N.S.K.; Al-Allak, M.H.; Lazm, A.M.; Jebur, M.S. Phenotypic investigation of vancomycin, teicoplanin and linezolid resistance among Enterococcus spp. isolated from children diarrhea. J. Pure Appl. Microbiol. 2019, 13, 531–536. [Google Scholar] [CrossRef]
- Ünüvar, S. Microbial Foodborne Diseases. In Handbook of Food Bioengineering, Foodborne Diseases; Holban, A.M., Grumezescu, A.M., Eds.; Academic Press: New York NY, USA, 2018; pp. 1–31. [Google Scholar]
- Quraishi, F.; Shaheen, S.; Memon, Z.; Fatima, G. Culture and sensitivity patterns of various antibiotics used for the treatment of pediatric infectious diarrhea in children under 5 years of age: A tertiary care experience from Karachi. Int. J. Clin. Med. 2018, 9, 684–696. [Google Scholar] [CrossRef]
- Santosham, M.; Reid, R. Diarrhoea Management. Available online: https://iris.who.int/bitstream/handle/10665/53517/WH-1986-Apr-p8-9-eng.pdf?sequence=1 (accessed on 21 April 2024).
- Guidelines for the Control of Shigellosis, Including Epidemics due to Shigella dysenteriae Type 1. 2005. Available online: https://iris.who.int/bitstream/handle/10665/43252/924159330X.pdf?sequence=1 (accessed on 4 April 2024).
- Global Taskforce on Cholerae Control. Recommendations for the Use of Antibiotics for the Treatment of Cholera. 2022. Available online: https://www.gtfcc.org/wp-content/uploads/2019/10/gtfcc-technical-note-on-use-of-antibiotics-for-the-treatment-of-cholera-1.pdf (accessed on 4 April 2024).
- Jandhyala, S.M.; Talukdar, R.; Subramanyam, C.; Vuyyuru, H.; Sasikala, M.; Nageshwar, R.D. Role of the normal gut microbiota. World J. Gastroenterol. 2015, 21, 8787–8803. [Google Scholar] [CrossRef] [PubMed]
- Rolhion, N.; Chassaing, B. When pathogenic bacteria meet the intestinal microbiota. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2016, 371, 20150504. [Google Scholar] [CrossRef]
- Vogt, S.L.; Finlay, B.B. Gut microbiota-mediated protection against diarrheal infections. J. Travel. Med. 2017, 24, S39–S43. [Google Scholar] [CrossRef]
- Cunha, B.A. Nosocomial diarrhea. Crit. Care Clin. 1998, 14, 329–338. [Google Scholar] [CrossRef]
- World Health Organization. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 5 August 2022).
- Zhang, Z.; Li, J.; Ma, L.; Yang, X.; Fei, B.; Leung, P.H.M.; Tao, X. Mechanistic study of synergistic antimicrobial effects between poly (3-hydroxybutyrate) oligomer and polyethylene glycol. Polymers 2020, 12, 2735. [Google Scholar] [CrossRef] [PubMed]
- Peña-Miller, R.; Lähnemann, D.; Schulenburg, H.; Ackermann, M.; Beardmore, R. The optimal deployment of synergistic antibiotics: A control-theoretic approach. J. R. Soc. Interface 2012, 9, 2488–2502. [Google Scholar] [CrossRef]
- Doldán-Martelli, V.; Míguez, D.G. Synergistic interaction between selective drugs in cell populations models. PLoS ONE 2015, 10, e0117558. [Google Scholar] [CrossRef]
- Windiasti, G.; Feng, J.; Ma, L.; Hu, Y.; Hakeem, M.J.; Amoako, K.; Delaquis, P.; Lu, X. Investigating the synergistic antimicrobial effect of carvacrol and zinc oxide nanoparticles against Campylobacter jejuni. Food Control 2019, 96, 39–46. [Google Scholar] [CrossRef]
- Olajuyigbe, O.O. Synergistic influence of tetracycline on the antibacterial activities of amoxicillin against resistant bacteria. J. Pharm. Allied Health Sci. 2012, 2, 12–20. [Google Scholar] [CrossRef]
- UNASYN-Ampicillin Sodium and Sulbactam Sodium Injection, Powder, for Solution Roerig. Available online: https://labeling.pfizer.com/showlabeling.aspx?id=617 (accessed on 23 October 2023).
- Khin-Maung-U; Myo-Khin; Nyunt-Nyunt-Wai; Aye-Kyaw; Tin-U. Clinical trial of berberine in acute watery diarrhoea. Br. Med. J. (Clin. Res. Ed.) 1985, 291, 1601–1605. [Google Scholar] [CrossRef]
- Hamoud, R.; Reichling, J.; Wink, M. Synergistic antibacterial activity of the combination of the alkaloid sanguinarine with EDTA and the antibiotic streptomycin against multidrug resistant bacteria. J. Pharm. Pharmacol. 2015, 67, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Jean, B.; Hatton, C.K. Pharmacognosy Phytochemistry Medicinal Plants, 2nd ed.; Lavoisier Pub.: Paris, France, 1999. [Google Scholar]
- Dey, A.; Mukherjee, A.; Chaudhury, M. Alkaloids From Apocynaceae: Origin, pharmacotherapeutic properties, and structure-activity studies. Stud. Nat. Prod. Chem. 2017, 52, 373–488. [Google Scholar]
- Awuchi, C. The biochemistry, toxicology, and uses of the pharmacologically active phytochemicals: Alkaloids, terpenes, polyphenols, and glycosides. J. Food Pharm. Sci. 2019, 7, 131–150. [Google Scholar] [CrossRef]
- Croaker, A.; King, G.J.; Pyne, J.H.; Anoopkumar-Dukie, S.; Liu, L. Sanguinaria canadensis: Traditional medicine, phytochemical composition, biological activities and current uses. Int. J. Mol. Sci. 2016, 17, 1414. [Google Scholar] [CrossRef]
- Tenenbaum, H.; Dahan, M.; Soell, M. Effectiveness of a sanguinarine regimen after scaling and root planing. J. Periodontol. 1999, 70, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Kuete, V. Health Effects of Alkaloids from African Medicinal Plants. In Toxicological Survey of African Medicinal Plants; Elsevier: New York, NY, USA, 2014; pp. 611–634. [Google Scholar]
- Osei-Owusu, H.; Kudera, T.; Strakova, M.; Rondevaldova, J.; Skrivanova, E.; Novy, P.; Kokoska, L. In vitro selective combinatory effect of ciprofloxacin with nitroxoline, sanguinarine, and zinc pyrithione against diarrhea-causing and gut beneficial bacteria. Microbiol. Spectr. 2022, 10, e0106322. [Google Scholar] [CrossRef] [PubMed]
- Kresken, M.; Körber-Irrgang, B. In vitro activity of nitroxoline against Escherichia coli urine isolates from outpatient departments in Germany. Antimicrob. Agents Chemother. 2014, 58, 7019–7020. [Google Scholar] [CrossRef]
- Vivanco, J.M.; Bais, H.P.; Stermitz, F.R.; Thelen, G.C.; Callaway, R.M. Biogeographical variation in community response to root allelochemistry: Novel weapons and exotic invasion. Ecol. Lett. 2004, 7, 285–292. [Google Scholar] [CrossRef]
- Han, G.; Bingxiang, X.; Xiaopeng, W. Studies on active principles of Polyalthia nemoralis-I. The isolation and identification of natural zinc compound. Acta Chim. Sin. 1981, 39, 433–437. [Google Scholar]
- Saunders, C.W.; Scheynius, A.; Heitman, J. Malassezia fungi are specialized to live on skin and associated with dandruff, eczema, and other skin diseases. PLoS Pathog. 2012, 8, 100270. [Google Scholar] [CrossRef]
- Leong, C.; Wang, J.; Toi, M.J.; Lam, Y.I.; Goh, J.P.; Lee, S.M.; Dawson, T.L. Effect of zinc pyrithione shampoo treatment on skin commensal Malassezia. Med. Mycol. 2021, 59, 210–213. [Google Scholar] [CrossRef]
- Britannica, The Editors of Encyclopaedia. “Tetracycline”. Encyclopedia Britannica. Available online: https://www.britannica.com/science/tetracycline (accessed on 7 April 2022).
- Dwivedi, G.R.; Maurya, A.; Yadav, D.K.; Singh, V.; Khan, F.; Gupta, M.K.; Singh, M.; Darokar, M.P.; Srivastava, S.K. Synergy of clavine alkaloid ‘chanoclavine’ with tetracycline against multi-drug-resistant E. coli. J. Biomol. Struct. Dyn. 2019, 37, 1307–1325. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; Approved Standard; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020. [Google Scholar]
- Sirichoat, A.; Flórez, A.B.; Vázquez, L.; Buppasiri, P.; Panya, M.; Lulitanond, V.; Mayo, B. Antibiotic resistance-susceptibility profiles of Enterococcus faecalis and Streptococcus spp. from the human vagina, and genome analysis of the genetic basis of intrinsic and acquired resistances. Front. Microbiol. 2020, 11, 1438. [Google Scholar] [CrossRef]
- Pohl, A.; Lübke-Becker, A.; Heuwieser, W. Minimum inhibitory concentrations of frequently used antibiotics against Escherichia coli and Trueperella pyogenes isolated from uteri of postpartum dairy cows. J. Dairy. Sci. 2018, 101, 1355–1364. [Google Scholar] [CrossRef]
- Han, F.; Walker, R.D.; Janes, M.E.; Prinyawiwatkul, W.; Ge, B. Antimicrobial susceptibilities of Vibrio parahaemolyticus and Vibrio vulnificus isolates from Louisiana Gulf and retail raw oysters. Appl. Environ. Microbiol. 2007, 73, 7096–7098. [Google Scholar] [CrossRef] [PubMed]
- Stock, I.; Wiedemann, B. An in-vitro study of the antimicrobial susceptibilities of Yersinia enterocolitica and the definition of a database. J. Antimicrob. Chemother. 1999, 43, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Sherwood, J.S.; Logue, C.M. Antimicrobial resistance of Listeria spp. recovered from processed bison. Lett. Appl. Microbiol. 2007, 44, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Madiyarov, R.S.; Bektemirov, A.M.; Ibadova, G.A.; Abdukhalilova, G.K.; Khodiev, A.V.; Bodhidatta, L.; Sethabutr, O.; Mason, C.J. Antimicrobial resistance patterns and prevalence of class 1 and 2 integrons in Shigella flexneri and Shigella sonnei isolated in Uzbekistan. Gut Pathog. 2010, 2, 18. [Google Scholar] [CrossRef] [PubMed]
- Kudera, T.; Doskocil, I.; Salmonova, H.; Petrtyl, M.; Skrivanova, E.; Kokoska, L. In vitro selective growth-inhibitory activities of phytochemicals, synthetic phytochemical analogs, and antibiotics against diarrheagenic/probiotic bacteria and cancer/normal intestinal cells. Pharmaceuticals 2020, 13, 233. [Google Scholar] [CrossRef] [PubMed]
- Omoya, F.O.; Ajayi, K.O. Synergistic effect of combined antibiotics against some selected multidrug resistant human pathogenic bacteria isolated from poultry droppings in Akure, Nigeria. Adv. Microbiol. 2016, 6, 1075–1090. [Google Scholar] [CrossRef]
- Chopra, I.; Roberts, M. Tetracycline antibiotics: Mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol. Mol. Biol. Rev. 2001, 65, 232–260. [Google Scholar] [CrossRef] [PubMed]
- Grossman, T.H. Tetracycline antibiotics and resistance. Cold Spring Harb. Perspect. Med. 2016, 6, 025387. [Google Scholar] [CrossRef]
- White, J.P.; Cantor, C.R. Role of magnesium in the binding of tetracycline to Escherichia coli ribosomes. J. Mol. Biol. 1971, 58, 397–400. [Google Scholar] [CrossRef]
- Repac, A.D.; Parčina, M.; Gobin, I.; Petković, D.M. Chelation in antibacterial drugs: From nitroxoline to cefiderocol and beyond. Antibiotics 2022, 11, 1105. [Google Scholar] [CrossRef]
- Wang, T.; Flint, S.; Palmer, J. Magnesium and calcium ions: Roles in bacterial cell attachment and biofilm structure maturation. Biofouling 2019, 35, 959–974. [Google Scholar] [CrossRef]
- Dinning, A.J.; Al-Adham, I.S.; Austin, P.; Charlton, M.; Collier, P.J. Pyrithione biocide interactions with bacterial phospholipid, head groups. J. Appl. Microbiol. 1998, 85, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Obiang-Obounou, B.W.; Kang, O.H.; Choi, J.G.; Keum, J.H.; Kim, S.B.; Mun, S.H.; Shin, D.W.; Kim, K.W.; Park, C.B.; Kim, Y.G.; et al. The mechanism of action of sanguinarine against methicillin-resistant Staphylococcus aureus. J. Toxicol. Sci. 2011, 36, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Shutter, M.C.; Akhondi, H. Tetracycline. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK549905/ (accessed on 10 April 2023).
- Poiger, H.; Schlatter, C. Interaction of cations and chelators with the intestinal absorption of tetracycline. Naunyn Schmiedebergs Arch. Pharmacol. 1979, 306, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Smith, L.P.; Gurney, M.; Lee, K.; Weinberg, W.G.; Longfield, J.N.; Tauber, W.B.; Karney, W.W. Comparison of single-dose tetracycline hydrochloride to conventional therapy of urinary tract infections. Antimicrob. Agents Chemother. 1985, 27, 652–654. [Google Scholar] [CrossRef] [PubMed]
- Naber, K.G.; Niggemann, H.; Stein, G. Review of the literature and individual patients’ data meta-analysis on efficacy and tolerance of nitroxoline in the treatment of uncomplicated urinary tract infections. BMC Infect. Dis. 2014, 14, 628. [Google Scholar] [CrossRef] [PubMed]
- Wijma, R.A.; Huttner, A.; Koch, B.C.P.; Mouton, J.W.; Muller, A.E. Review of the pharmacokinetic properties of nitrofurantoin and nitroxoline. J. Antimicrob. Chemother. 2018, 73, 2916–2926. [Google Scholar] [CrossRef] [PubMed]
- Becci, P.J.; Schwartz, H.; Barnes, H.H.; Southard, G.L. Short-term toxicity studies of sanguinarine and of two alkaloid extracts of Sanguinaria canadensis L. J. Toxicol. Environ. Health 1987, 20, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Scientific Committee on Consumer Safety (SCCS). Opinion on Zinc Pyrithione. Available online: https://health.ec.europa.eu/system/files/2021-11/sccs_o_236.pdf (accessed on 12 April 2023).
- Schwartz, J.R.; Shah, R.; Krigbaum, H.; Sacha, J.; Vogt, A.; Blume-Peytavi, U. New insights on dandruff/seborrhoeic dermatitis: The role of the scalp follicular infundibulum in effective treatment strategies. Br. J. Dermatol. 2011, 165 (Suppl. 2), 18–23. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically, 10th ed.; Approved Standard; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2015. [Google Scholar]
- Leber, A. Synergism testing: Broth microdilution checkerboard and broth microdilution methods. In Clinical Microbiology Procedures Handbook, 4th ed.; ASM Press: Washington, DC, USA, 2016; Volume 1–3, pp. 1–23. [Google Scholar]
- Cos, P.; Vlietinck, A.J.; Vanden Berghe, D.; Maes, L. Anti-infective potential of natural products: How to develop a stronger in vitro ‘proof-of-concept’. J. Ethnopharmacol. 2006, 106, 290–302. [Google Scholar] [CrossRef]
- Jorgensen, J.H.; Turnidge, J.D.; Washington, J.A. Antibacterial susceptibility tests: Dilution and disk diffusion methods. In Manual of Clinical Microbiology, 7th ed.; Murray, P.R., Baron, E.J., Pfaller, M.A., Tenover, F.C., Yolken, R.H., Eds.; ASM Press: Washington, DC, USA, 1999; pp. 1526–1543. [Google Scholar]
- Okoliegbe, I.N.; Hijazi, K.; Cooper, K.; Ironside, C.; Gould, I.M. Antimicrobial synergy testing: Comparing the tobramycin and ceftazidime gradient diffusion methodology used in assessing synergy in cystic fibrosis-derived multidrug-resistant Pseudomonas aeruginosa. Antibiotics 2021, 10, 967. [Google Scholar] [CrossRef] [PubMed]
- Frankova, A.; Vistejnova, L.; Merinas-Amo, T.; Leheckova, Z.; Doskocil, I.; Wong Soon, J.; Kudera, T.; Laupua, F.; Alonso-Moraga, A.; Kokoska, L. In vitro antibacterial activity of extracts from Samoan medicinal plants and their effect on proliferation and migration of human fibroblasts. J. Ethnopharmacol. 2021, 264, 113220. [Google Scholar] [CrossRef] [PubMed]
- European Committee for Antimicrobial Susceptibility Testing (EUCAST) of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID). EUCAST Definitive Document E. Def 1.2. Terminology relating to methods for the determination of susceptibility of bacteria to antimicrobial agents. Clin. Microbiol. Infect. 2000, 6, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Rakholiya, K.D.; Kaneria, M.J.; Chanda, S.V. Medicinal plants as alternative sources of therapeutics against multidrug-resistant pathogenic microorganisms based on their antimicrobial potential and synergistic properties. In Fighting Multidrug Resistance with Herbal Extracts, Essential Oils and Their Components; Rai, M.K., Kon, K.V., Eds.; Academic Press: New York, NY, USA, 2013; pp. 165–179. [Google Scholar]
- Odds, F.C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 2003, 52, 1. [Google Scholar] [CrossRef]
- Williamson, E.M. Synergy and other interactions in phytomedicines. Phytomedicine 2001, 8, 401–409. [Google Scholar] [CrossRef]
| Bacterium | MIC a Alone | NTX MIC (in Bold) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TET | NTX | 8 | 4 | 2 | 1 | 0.5 | 0.25 | |||||||
| TET MIC | FIC I b | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | |||
| E. faecalis | 1 | 16 | 0.031 | 0.531 | 0.25 | 0.5 | 0.25 | 0.375 | 0.25 | 0.313 | 1 | 1.031 | 1 | 1.016 |
| L. monocytogenes | 0.667 | 16 | 0.052 | 0.578 | 0.109 | 0.413 | 0.083 | 0.249 | 0.083 | 0.187 | 0.083 | 0.156 | 0.104 | 0.172 |
| 2 | 1 | 0.5 | 0.25 | 0.125 | 0.063 | |||||||||
| E. coli O175:H7 | 4 | 2 | 0.063 | 1.016 | 1 | 0.75 | 4 | 1.25 | 1 | 0.375 | 1 | 0.313 | 0.5 | 0.157 |
| S. flexneri | 4 | 2.667 | 0.063 | 0.766 | 2.333 | 0.958 | 3 | 0.937 | 1 | 0.344 | 1 | 0.297 | 0.25 | 0.086 |
| V. parahaemolyticus | 2 | 2 | 0.016 | 1.008 | 0.016 | 0.508 | 0.5 | 0.50 | 0.5 | 0.375 | 0.5 | 0.313 | 0.5 | 0.282 |
| 1 | 0.5 | 0.25 | 0.125 | 0.063 | 0.031 | |||||||||
| Y. enterocolitica | 8 | 6.667 | 2 | 0.400 | 2 | 0.325 | 2 | 0.287 | 2 | 0.269 | 2 | 0.259 | 2 | 0.255 |
| Bacterium | MIC a Alone | ZPT MIC (in Bold) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TET | ZPT | 4 | 2 | 1 | 0.5 | 0.25 | 0.125 | |||||||
| TET MIC | FICI b | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | |||
| S. flexneri | 5.333 | 8 | 1 | 0.688 | 1 | 0.438 | 1 | 0.313 | 1 | 0.250 | 1 | 0.219 | 0.5 | 0.109 |
| V. parahaemolyticus | 4 | 8 | 0.016 | 0.504 | 0.031 | 0.258 | 0.031 | 0.133 | 0.5 | 0.188 | 0.5 | 0.156 | 0.5 | 0.141 |
| 2 | 1 | 0.5 | 0.25 | 0.125 | 0.063 | |||||||||
| E. coli O175:H7 | 4 | 16 | 1 | 0.375 | 1 | 0.313 | 1 | 0.281 | 2 | 0.516 | 2 | 0.508 | 1 | 0.254 |
| E. faecalis | 1 | 8 | 0.5 | 0.75 | 1 | 1.125 | 1 | 1.063 | 1 | 1.031 | 1 | 1.016 | 1 | 1.008 |
| Y. enterocolitica | 8 | 8 | 1 | 0.375 | 1 | 0.25 | 2 | 0.313 | 2 | 0.281 | 2 | 0.266 | 2 | 0.258 |
| 1 | 0.5 | 0.25 | 0.125 | 0.063 | 0.031 | |||||||||
| L. monocytogenes | 0.5 | 8 | 0.125 | 0.375 | 0.208 | 0.479 | 0.208 | 0.447 | 0.125 | 0.266 | 0.125 | 0.258 | 0.125 | 0.254 |
| Bacterium | MIC a Alone | SGN MIC (in Bold) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TET | SGN | 16 | 8 | 4 | 2 | 1 | 0.5 | |||||||
| TET MIC | FICI b | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | TET MIC | FICI | |||
| E. coli O175:H7 | 4 | 128 | 4 | 1.125 | 4 | 1.063 | 4 | 1.031 | 4 | 1.016 | 2 | 0.508 | 2 | 0.504 |
| 8 | 4 | 2 | 1 | 0.5 | 0.25 | |||||||||
| E. faecalis | 1 | 16 | 0.031 | 0.531 | 0.25 | 0.5 | 0.25 | 0.375 | 0.25 | 0.313 | 1 | 1.031 | 1 | 1.016 |
| Y. enterocolitica | 2 | 64 | 2 | 1.125 | 2 | 1.063 | 2 | 1.031 | 2 | 1.016 | 2 | 1.008 | 2 | 1.004 |
| 4 | 2 | 1 | 0.5 | 0.25 | 0.125 | |||||||||
| L. monocytogenes | 0.5 | 3.333 | 0.016 | 1.232 | 0.031 | 0.662 | 0.063 | 0.458 | 0.104 | 0.358 | 0.125 | 0.325 | 0.125 | 0.288 |
| 2 | 1 | 0.5 | 0.25 | 0.125 | 0.063 | |||||||||
| S. flexneri | 1 | 16 | 1 | 1.125 | 1 | 1.063 | 0.5 | 0.531 | 0.5 | 0.516 | 1 | 1.008 | 1 | 1.004 |
| V. parahaemolyticus | 1 | 16 | 0.5 | 0.625 | 0.5 | 0.563 | 1 | 1.031 | 1 | 1.016 | 1 | 1.008 | 1 | 1.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osei-Owusu, H.; Rondevaldova, J.; Houdkova, M.; Kudera, T.; Needham, T.; Mascellani, A.; Kokoska, L. Evaluation of In Vitro Synergistic Effects of Tetracycline with Alkaloid-Related Compounds against Diarrhoeic Bacteria. Int. J. Mol. Sci. 2024, 25, 6038. https://doi.org/10.3390/ijms25116038
Osei-Owusu H, Rondevaldova J, Houdkova M, Kudera T, Needham T, Mascellani A, Kokoska L. Evaluation of In Vitro Synergistic Effects of Tetracycline with Alkaloid-Related Compounds against Diarrhoeic Bacteria. International Journal of Molecular Sciences. 2024; 25(11):6038. https://doi.org/10.3390/ijms25116038
Chicago/Turabian StyleOsei-Owusu, Hayford, Johana Rondevaldova, Marketa Houdkova, Tomas Kudera, Tersia Needham, Anna Mascellani, and Ladislav Kokoska. 2024. "Evaluation of In Vitro Synergistic Effects of Tetracycline with Alkaloid-Related Compounds against Diarrhoeic Bacteria" International Journal of Molecular Sciences 25, no. 11: 6038. https://doi.org/10.3390/ijms25116038
APA StyleOsei-Owusu, H., Rondevaldova, J., Houdkova, M., Kudera, T., Needham, T., Mascellani, A., & Kokoska, L. (2024). Evaluation of In Vitro Synergistic Effects of Tetracycline with Alkaloid-Related Compounds against Diarrhoeic Bacteria. International Journal of Molecular Sciences, 25(11), 6038. https://doi.org/10.3390/ijms25116038











