Translational Experimental Basis of Indirect Adenosine Receptor Agonist Stimulation for Bone Regeneration: A Review
Abstract
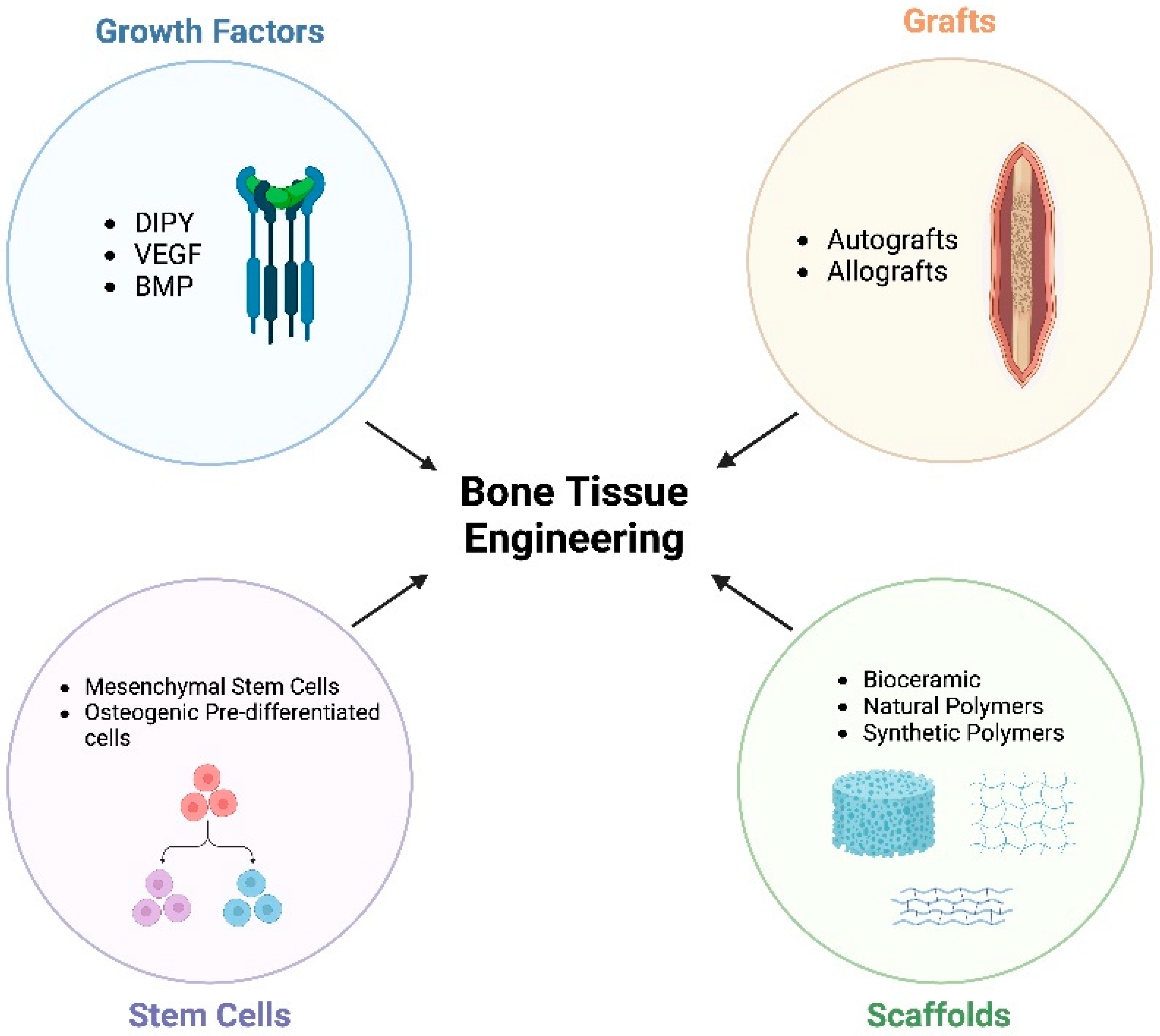
:1. Introduction
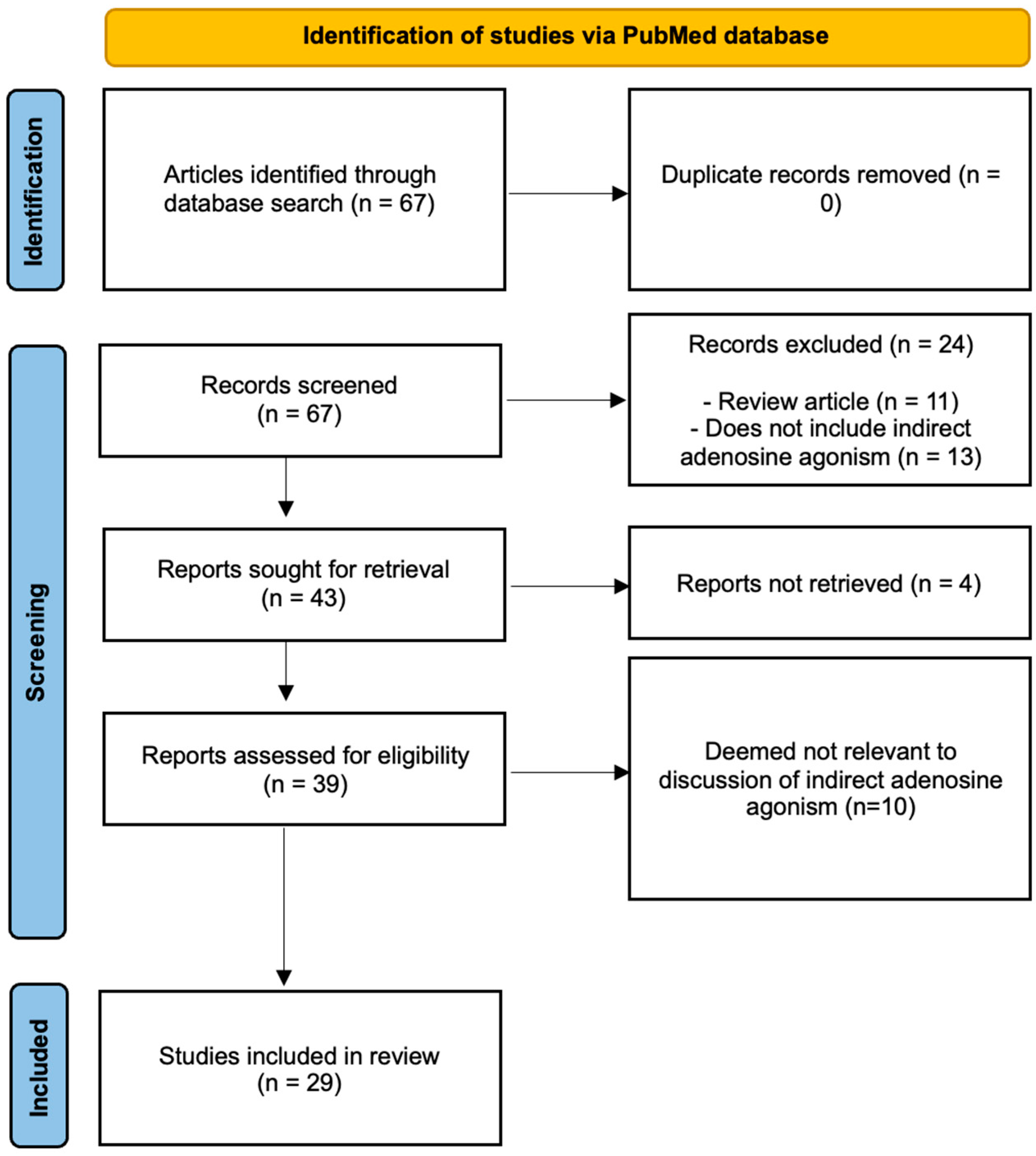
2. Methods
3. Results
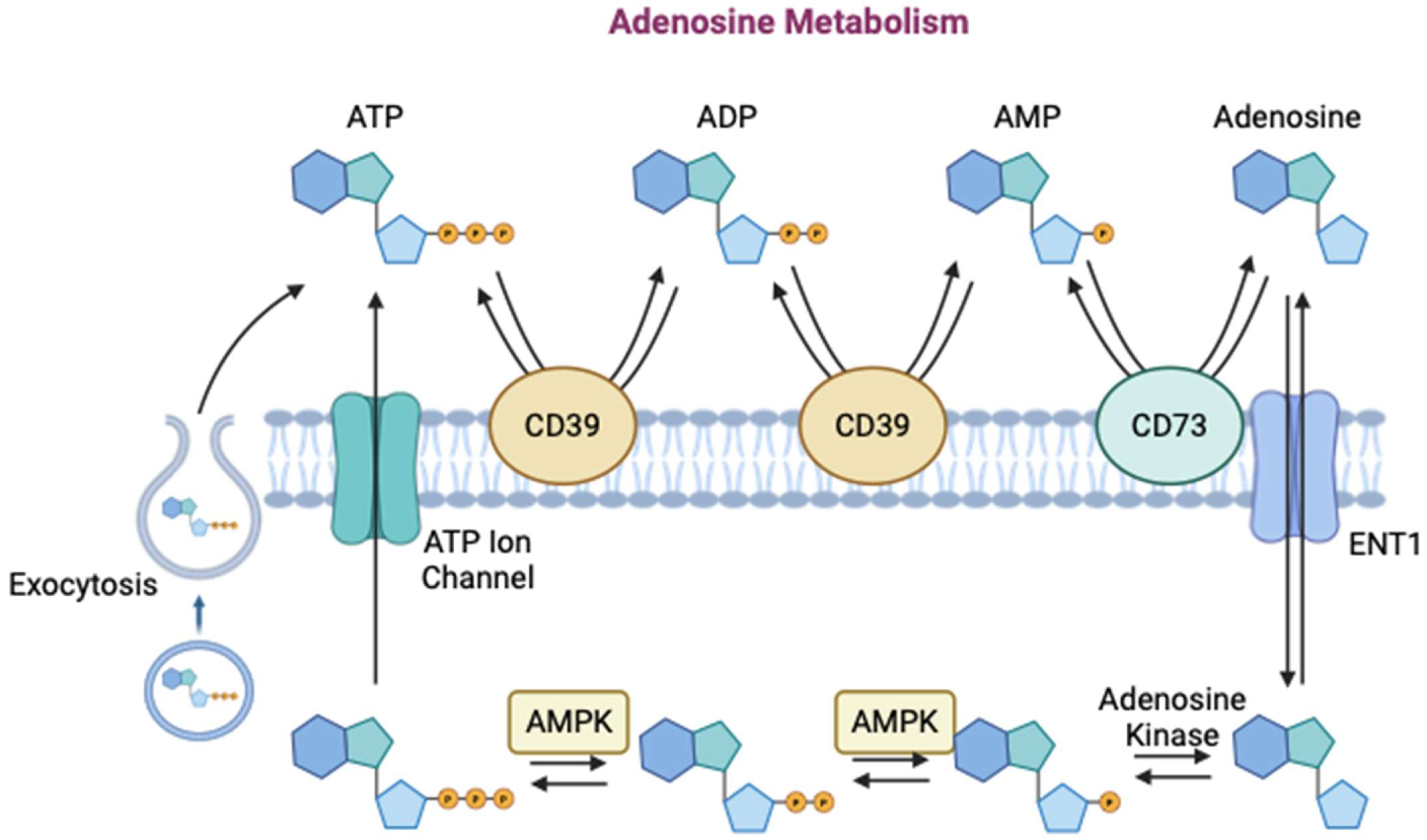
3.1. Adenosine’s Role in Bone Regeneration
3.2. Function of Adenosine Receptors
3.3. Indirect Agonists
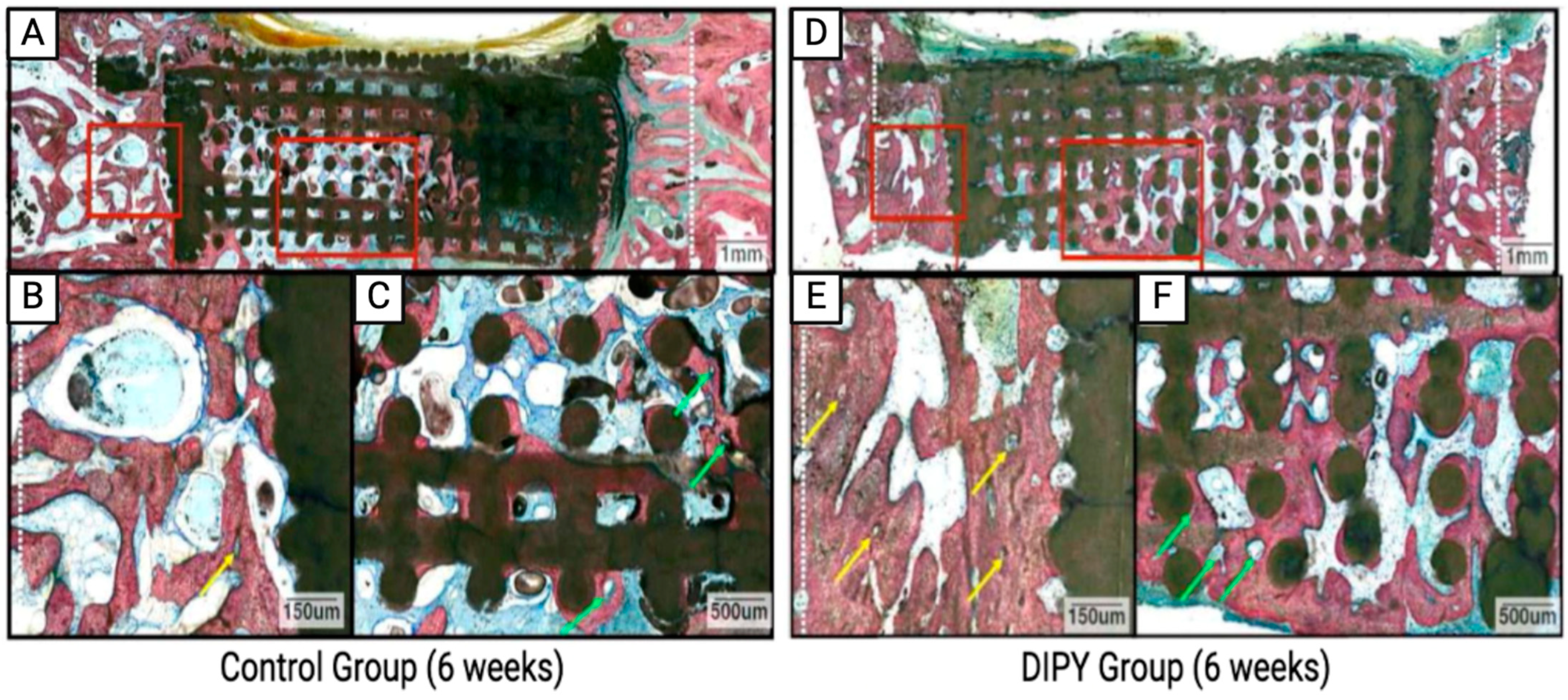
3.3.1. DIPY
3.3.2. Ticagrelor
3.3.3. ENT-1 Inhibitors
3.3.4. CD39/73 Agonist
3.3.5. Other Adenosine Metabolism Inhibitors
3.4. Future Directions
3.4.1. Controlled Release of Adenosine for Bone Regeneration, Tendon Healing, and Reversal of Osteoarthritis
3.4.2. Core–Shell Nanofibers
3.4.3. Microgels
3.4.4. Nanoparticles and Liposomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hak, D.J.; Fitzpatrick, D.; Bishop, J.A.; Marsh, J.L.; Tilp, S.; Schnettler, R.; Simpson, H.; Alt, V. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury 2014, 45, S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Huber, F.G. Surgical treatment of orthopaedic trauma. J. Trauma Inj. Infect. Crit. Care 2007, 63, 450. [Google Scholar] [CrossRef]
- Quan, K.; Xu, Q.; Zhu, M.; Liu, X.; Dai, M. Analysis of Risk Factors for Non-union After Surgery for Limb Fractures: A Case-Control Study of 669 Subjects. Front. Surg. 2021, 8, 754150. [Google Scholar] [CrossRef] [PubMed]
- Kostenuik, P.; Mirza, F.M. Fracture healing physiology and the quest for therapies for delayed healing and nonunion. J. Orthop. Res. 2017, 35, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Cornell, C.N. Osteobiologics. Bull. NYU Hosp. Jt. Dis. 2004, 62, 13. [Google Scholar]
- Esenlik, E.; DeMitchell-Rodriguez, E.M. Alveolar Distraction. Clin. Plast. Surg. 2021, 48, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Ferrier, M.B.; Spuesens, E.B.; Le Cessie, S.; Baatenburg de Jong, R.J. Comorbidity as a major risk factor for mortality and complications in head and neck surgery. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; D’Agostino, A.; Nocini, P.F.; Signoriello, A.; Zangani, A.; Pardo, A.; Lonardi, F.; Trevisiol, L. Clinical outcomes and periodontal conditions of dental implants placed in free fibula flaps (FFF): A retrospective study with a mean follow-up of 6 years. Clin. Oral Investig. 2023, 27, 7737–7751. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, D.A. Condyle transplantation in free flap mandible reconstruction. Plast. Reconstr. Surg. 1994, 93, 770–781. [Google Scholar] [CrossRef]
- Hidalgo, D.A.; Rekow, A. A review of 60 consecutive fibula free flap mandible reconstructions. Plast. Reconstr. Surg. 1995, 96, 585–596. [Google Scholar] [CrossRef]
- Masquelet, A. Muscle reconstruction in reconstructive surgery: Soft tissue repair and long bone reconstruction. Langenbeck’s Arch. Surg. 2003, 388, 344–346. [Google Scholar] [CrossRef]
- Soucacos, P.N.; Dailiana, Z.; Beris, A.E.; Johnson, E.O. Vascularised bone grafts for the management of non-union. Injury 2006, 37, S41–S50. [Google Scholar] [CrossRef]
- Black, C.R.; Goriainov, V.; Gibbs, D.; Kanczler, J.; Tare, R.S.; Oreffo, R.O. Bone tissue engineering. Curr. Mol. Biol. Rep. 2015, 1, 132–140. [Google Scholar] [CrossRef]
- Perez, J.R.; Kouroupis, D.; Li, D.J.; Best, T.M.; Kaplan, L.; Correa, D. Tissue Engineering and Cell-Based Therapies for Fractures and Bone Defects. Front. Bioeng. Biotechnol. 2018, 6, 105. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.K.; Lee, J.S.; Kim, M.S.; Choi, S.H.; Cho, K.S.; Jung, U.W. Sinus augmentation using BMP-2 in a bovine hydroxyapatite/collagen carrier in dogs. J. Clin. Periodontol. 2014, 41, 86–93. [Google Scholar] [CrossRef]
- Liu, Y.; Ming, L.; Luo, H.; Liu, W.; Zhang, Y.; Liu, H.; Jin, Y. Integration of a calcined bovine bone and BMSC-sheet 3D scaffold and the promotion of bone regeneration in large defects. Biomaterials 2013, 34, 9998–10006. [Google Scholar] [CrossRef] [PubMed]
- Mediero, A.; Wilder, T.; Perez-Aso, M.; Cronstein, B.N. Direct or indirect stimulation of adenosine A2A receptors enhances bone regeneration as well as bone morphogenetic protein-2. FASEB J. 2015, 29, 1577–1590. [Google Scholar] [CrossRef]
- Riley, E.H.; Lane, J.M.; Urist, M.R.; Lyons, K.M.; Lieberman, J.R. Bone morphogenetic protein-2: Biology and applications. Clin. Orthop. Relat. Res. 1996, 324, 39–46. [Google Scholar] [CrossRef]
- Carragee, E.J.; Hurwitz, E.L.; Weiner, B.K. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: Emerging safety concerns and lessons learned. Spine J. 2011, 11, 471–491. [Google Scholar] [CrossRef]
- Glassman, S.D.; Howard, J.; Dimar, J.; Sweet, A.; Wilson, G.; Carreon, L. Complications with recombinant human bone morphogenic protein-2 in posterolateral spine fusion: A consecutive series of 1037 cases. Spine 2011, 36, 1849–1854. [Google Scholar] [CrossRef]
- Spiro, A.S.; Beil, F.T.; Baranowsky, A.; Barvencik, F.; Schilling, A.F.; Nguyen, K.; Khadem, S.; Seitz, S.; Rueger, J.M.; Schinke, T.; et al. BMP-7-induced ectopic bone formation and fracture healing is impaired by systemic NSAID application in C57BL/6-mice. J. Orthop. Res. 2010, 28, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Balseiro, S.; Nottmeier, E.W. Vertebral osteolysis originating from subchondral cyst end plate defects in transforaminal lumbar interbody fusion using rhBMP-2. Report of two cases. Spine J. 2010, 10, e6–e10. [Google Scholar] [CrossRef] [PubMed]
- Kawai, M.; Bessho, K.; Kaihara, S.; Sonobe, J.; Oda, K.; Iizuka, T.; Maruyama, H. Ectopic bone formation by human bone morphogenetic protein-2 gene transfer to skeletal muscle using transcutaneous electroporation. Hum. Gene Ther. 2003, 14, 1547–1556. [Google Scholar] [CrossRef]
- Sebastian, A.S.; Wanderman, N.R.; Currier, B.L.; Pichelmann, M.A.; Treder, V.M.; Fogelson, J.L.; Clarke, M.J.; Nassr, A.N. Prospective Evaluation of Radiculitis following Bone Morphogenetic Protein-2 Use for Transforaminal Interbody Arthrodesis in Spine Surgery. Asian Spine J. 2019, 13, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Drury, A.; Szent-Györgyi, A.v. The physiological activity of adenine compounds with especial reference to their action upon the mammalian heart. J. Physiol. 1929, 68, 213–237. [Google Scholar] [CrossRef] [PubMed]
- Hasko, G.; Linden, J.; Cronstein, B.; Pacher, P. Adenosine receptors: Therapeutic aspects for inflammatory and immune diseases. Nat. Rev. Drug Discov. 2008, 7, 759–770. [Google Scholar] [CrossRef]
- Day, Y.J.; Li, Y.; Rieger, J.M.; Ramos, S.I.; Okusa, M.D.; Linden, J. A2A adenosine receptors on bone marrow-derived cells protect liver from ischemia-reperfusion injury. J. Immunol. 2005, 174, 5040–5046. [Google Scholar] [CrossRef] [PubMed]
- Day, Y.J.; Huang, L.; McDuffie, M.J.; Rosin, D.L.; Ye, H.; Chen, J.F.; Schwarzschild, M.A.; Fink, J.S.; Linden, J.; Okusa, M.D. Renal protection from ischemia mediated by A2A adenosine receptors on bone marrow-derived cells. J. Clin. Investig. 2003, 112, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Day, Y.J.; Toufektsian, M.C.; Xu, Y.; Ramos, S.I.; Marshall, M.A.; French, B.A.; Linden, J. Myocardial infarct-sparing effect of adenosine A2A receptor activation is due to its action on CD4+ T lymphocytes. Circulation 2006, 114, 2056–2064. [Google Scholar] [CrossRef]
- Peirce, S.M.; Skalak, T.C.; Rieger, J.M.; Macdonald, T.L.; Linden, J. Selective A(2A) adenosine receptor activation reduces skin pressure ulcer formation and inflammation. Am. J. Physiol. Heart Circ. Physiol. 2001, 281, H67–H74. [Google Scholar] [CrossRef]
- Ryzhov, S.; Zaynagetdinov, R.; Goldstein, A.E.; Novitskiy, S.V.; Blackburn, M.R.; Biaggioni, I.; Feoktistov, I. Effect of A2B adenosine receptor gene ablation on adenosine-dependent regulation of proinflammatory cytokines. J. Pharmacol. Exp. Ther. 2008, 324, 694–700. [Google Scholar] [CrossRef]
- Hasko, G.; Kuhel, D.G.; Chen, J.F.; Schwarzschild, M.A.; Deitch, E.A.; Mabley, J.G.; Marton, A.; Szabo, C. Adenosine inhibits IL-12 and TNF-[alpha] production via adenosine A2a receptor-dependent and independent mechanisms. FASEB J. 2000, 14, 2065–2074. [Google Scholar] [CrossRef]
- Kreckler, L.M.; Wan, T.C.; Ge, Z.D.; Auchampach, J.A. Adenosine inhibits tumor necrosis factor-alpha release from mouse peritoneal macrophages via A2A and A2B but not the A3 adenosine receptor. J. Pharmacol. Exp. Ther. 2006, 317, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Montesinos, M.C.; Gadangi, P.; Longaker, M.; Sung, J.; Levine, J.; Nilsen, D.; Reibman, J.; Li, M.; Jiang, C.K.; Hirschhorn, R.; et al. Wound healing is accelerated by agonists of adenosine A2 (G alpha s-linked) receptors. J. Exp. Med. 1997, 186, 1615–1620. [Google Scholar] [CrossRef] [PubMed]
- Feoktistov, I.; Goldstein, A.E.; Ryzhov, S.; Zeng, D.; Belardinelli, L.; Voyno-Yasenetskaya, T.; Biaggioni, I. Differential expression of adenosine receptors in human endothelial cells: Role of A2B receptors in angiogenic factor regulation. Circ. Res. 2002, 90, 531–538. [Google Scholar] [CrossRef]
- Mediero, A.; Cronstein, B.N. Adenosine and bone metabolism. Trends Endocrinol. Metab. 2013, 24, 290–300. [Google Scholar] [CrossRef]
- Hoebertz, A.; Arnett, T.R.; Burnstock, G. Regulation of bone resorption and formation by purines and pyrimidines. Trends Pharmacol. Sci. 2003, 24, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Kazemzadeh-Narbat, M.; Annabi, N.; Tamayol, A.; Oklu, R.; Ghanem, A.; Khademhosseini, A. Adenosine-associated delivery systems. J. Drug Target. 2015, 23, 580–596. [Google Scholar] [CrossRef]
- Zimmermann, H. Extracellular metabolism of ATP and other nucleotides. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2000, 362, 299–309. [Google Scholar] [CrossRef]
- Hassanian, S.M.; Dinarvand, P.; Rezaie, A.R. Adenosine regulates the proinflammatory signaling function of thrombin in endothelial cells. J. Cell. Physiol. 2014, 229, 1292–1300. [Google Scholar] [CrossRef]
- Milne, G.R.; Palmer, T.M. Anti-inflammatory and immunosuppressive effects of the A2A adenosine receptor. Sci. World J. 2011, 11, 320–339. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.W. Adenosine A2A receptor agonists as anti-inflammatory agents. Curr. Opin. Investig. Drugs 2003, 4, 1313–1319. [Google Scholar] [PubMed]
- Corriden, R.; Insel, P.A. New insights regarding the regulation of chemotaxis by nucleotides, adenosine, and their receptors. Purinergic Signal. 2012, 8, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.J.; Chen, C.Q.; Gu, X.H. [Effect of adenosine triphosphate on type I collagen mineralization in hard tissue]. Zhonghua Kou Qiang Yi Xue Za Zhi 2019, 54, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Lee, J.K.; Jung, J.W.; Baek, S.W.; Kim, J.H.; Heo, Y.; Kim, T.H.; Han, D.K. Promotion of Bone Regeneration Using Bioinspired PLGA/MH/ECM Scaffold Combined with Bioactive PDRN. Materials 2021, 14, 4149. [Google Scholar] [CrossRef] [PubMed]
- Fredholm, B.B.; AP, I.J.; Jacobson, K.A.; Klotz, K.N.; Linden, J. International Union of Pharmacology. XXV. Nomenclature and classification of adenosine receptors. Pharmacol. Rev. 2001, 53, 527–552. [Google Scholar] [PubMed]
- Fredholm, B.B.; Chern, Y.; Franco, R.; Sitkovsky, M. Aspects of the general biology of adenosine A2A signaling. Prog. Neurobiol. 2007, 83, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Gharibi, B.; Abraham, A.A.; Ham, J.; Evans, B.A.J. Contrasting effects of A1 and A2b adenosine receptors on adipogenesis. Int. J. Obes. 2012, 36, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Che, J.; Chan, E.S.; Cronstein, B.N. Adenosine A2A receptor occupancy stimulates collagen expression by hepatic stellate cells via pathways involving protein kinase A, Src, and extracellular signal-regulated kinases 1/2 signaling cascade or p38 mitogen-activated protein kinase signaling pathway. Mol. Pharmacol. 2007, 72, 1626–1636. [Google Scholar] [CrossRef]
- Csoka, B.; Nemeth, Z.H.; Virag, L.; Gergely, P.; Leibovich, S.J.; Pacher, P.; Sun, C.X.; Blackburn, M.R.; Vizi, E.S.; Deitch, E.A.; et al. A2A adenosine receptors and C/EBPbeta are crucially required for IL-10 production by macrophages exposed to Escherichia coli. Blood 2007, 110, 2685–2695. [Google Scholar] [CrossRef]
- Mazzon, E.; Esposito, E.; Impellizzeri, D.; Di Paole, R.; Melani, A.; Bramanti, P.; Pedata, F.; Cuzzocrea, S. CGS 21680, an agonist of the adenosine (A2A) receptor, reduces progression of murine type II collagen-induced arthritis. J. Rheumatol. 2011, 38, 2119–2129. [Google Scholar] [CrossRef] [PubMed]
- Mediero, A.; Kara, F.M.; Wilder, T.; Cronstein, B.N. Adenosine A(2A) receptor ligation inhibits osteoclast formation. Am. J. Pathol. 2012, 180, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Yegutkin, G.G. Nucleotide- and nucleoside-converting ectoenzymes: Important modulators of purinergic signalling cascade. Biochim. Biophys. Acta 2008, 1783, 673–694. [Google Scholar] [CrossRef]
- Borea, P.A.; Varani, K.; Vincenzi, F.; Baraldi, P.G.; Tabrizi, M.A.; Merighi, S.; Gessi, S. The A3 adenosine receptor: History and perspectives. Pharmacol. Rev. 2015, 67, 74–102. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.D.; Bekisz, J.M.; Corciulo, C.; Mediero, A.; Coelho, P.G.; Witek, L.; Flores, R.L.; Cronstein, B.N. Local delivery of adenosine receptor agonists to promote bone regeneration and defect healing. Adv. Drug Deliv. Rev. 2019, 146, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Hasko, G.; Cronstein, B.N. Adenosine: An endogenous regulator of innate immunity. Trends Immunol. 2004, 25, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.F.; Eltzschig, H.K.; Fredholm, B.B. Adenosine receptors as drug targets—What are the challenges? Nat. Rev. Drug Discov. 2013, 12, 265–286. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Chu, X.; Deng, F.; Tong, L.; Tong, G.; Yi, Y.; Liu, J.; Tang, J.; Tang, Y.; Xia, Y.; et al. The adenosine A2b receptor promotes tumor progression of bladder urothelial carcinoma by enhancing MAPK signaling pathway. Oncotarget 2017, 8, 48755–48768. [Google Scholar] [CrossRef] [PubMed]
- Cronstein, B.N. Adenosine receptors and fibrosis: A translational review. F1000 Biol. Rep. 2011, 3, 21. [Google Scholar] [CrossRef]
- Parker, R.B.; McCollam, P.L. Adenosine in the episodic treatment of paroxysmal supraventricular tachycardia. Clin. Pharm. 1990, 9, 261–271. [Google Scholar]
- Cheng, X.; Cheng, G.; Xing, X.; Yin, C.; Cheng, Y.; Zhou, X.; Jiang, S.; Tao, F.; Deng, H.; Li, Z. Controlled release of adenosine from core-shell nanofibers to promote bone regeneration through STAT3 signaling pathway. J. Control Release 2020, 319, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Vergara, M.J.; Benalcazar-Jalkh, E.B.; Nayak, V.V.; Bergamo, E.T.P.; Cronstein, B.; Zetola, A.L.; Weiss, F.P.; Grossi, J.R.A.; Deliberador, T.M.; Coelho, P.G.; et al. Employing Indirect Adenosine 2(A) Receptors (A(2A)R) to Enhance Osseointegration of Titanium Devices: A Pre-Clinical Study. J. Funct. Biomater. 2023, 14, 308. [Google Scholar] [CrossRef]
- DeMitchell-Rodriguez, E.M.; Shen, C.; Nayak, V.V.; Tovar, N.; Witek, L.; Torroni, A.; Yarholar, L.M.; Cronstein, B.N.; Flores, R.L.; Coelho, P.G. Engineering 3D Printed Bioceramic Scaffolds to Reconstruct Critical-Sized Calvaria Defects in a Skeletally Immature Pig Model. Plast. Reconstr. Surg. 2023, 152, 270e–280e. [Google Scholar] [CrossRef]
- Lopez, C.D.; Coelho, P.G.; Witek, L.; Torroni, A.; Greenberg, M.I.; Cuadrado, D.L.; Guarino, A.M.; Bekisz, J.M.; Cronstein, B.N.; Flores, R.L. Regeneration of a Pediatric Alveolar Cleft Model Using Three-Dimensionally Printed Bioceramic Scaffolds and Osteogenic Agents: Comparison of Dipyridamole and rhBMP-2. Plast. Reconstr. Surg. 2019, 144, 358–370. [Google Scholar] [CrossRef]
- Wang, M.M.; Flores, R.L.; Witek, L.; Torroni, A.; Ibrahim, A.; Wang, Z.; Liss, H.A.; Cronstein, B.N.; Lopez, C.D.; Maliha, S.G.; et al. Dipyridamole-loaded 3D-printed bioceramic scaffolds stimulate pediatric bone regeneration in vivo without disruption of craniofacial growth through facial maturity. Sci. Rep. 2019, 9, 18439. [Google Scholar] [CrossRef]
- Lopez, C.D.; Diaz-Siso, J.R.; Witek, L.; Bekisz, J.M.; Gil, L.F.; Cronstein, B.N.; Flores, R.L.; Torroni, A.; Rodriguez, E.D.; Coelho, P.G. Dipyridamole Augments Three-Dimensionally Printed Bioactive Ceramic Scaffolds to Regenerate Craniofacial Bone. Plast. Reconstr. Surg. 2019, 143, 1408–1419. [Google Scholar] [CrossRef] [PubMed]
- Maliha, S.G.; Lopez, C.D.; Coelho, P.G.; Witek, L.; Cox, M.; Meskin, A.; Rusi, S.; Torroni, A.; Cronstein, B.N.; Flores, R.L. Bone Tissue Engineering in the Growing Calvaria Using Dipyridamole-Coated, Three-Dimensionally-Printed Bioceramic Scaffolds: Construct Optimization and Effects on Cranial Suture Patency. Plast. Reconstr. Surg. 2020, 145, 337e–347e. [Google Scholar] [CrossRef]
- Witek, L.; Alifarag, A.M.; Tovar, N.; Lopez, C.D.; Cronstein, B.N.; Rodriguez, E.D.; Coelho, P.G. Repair of Critical-Sized Long Bone Defects Using Dipyridamole-Augmented 3D-Printed Bioactive Ceramic Scaffolds. J Orthop. Res 2019, 37, 2499–2507. [Google Scholar] [CrossRef] [PubMed]
- Mediero, A.; Wilder, T.; Reddy, V.S.; Cheng, Q.; Tovar, N.; Coelho, P.G.; Witek, L.; Whatling, C.; Cronstein, B.N. Ticagrelor regulates osteoblast and osteoclast function and promotes bone formation in vivo via an adenosine-dependent mechanism. FASEB J. 2016, 30, 3887–3900. [Google Scholar] [CrossRef]
- Kobat, M.A.; Dundar, S.; Bozoglan, A.; Gelen, M.A.; Artas, G.; Kirtay, M.; Tasdemir, I.; Karasu, M.; Habek, O. Evaluation of the Effects of Dual Antiplatelet Therapy on Guided Bone Regeneration in Peri-Implant Bone Defect. J. Craniofac. Surg. 2023, 34, 1590–1594. [Google Scholar] [CrossRef]
- Takedachi, M.; Oohara, H.; Smith, B.J.; Iyama, M.; Kobashi, M.; Maeda, K.; Long, C.L.; Humphrey, M.B.; Stoecker, B.J.; Toyosawa, S.; et al. CD73-generated adenosine promotes osteoblast differentiation. J. Cell. Physiol. 2012, 227, 2622–2631. [Google Scholar] [CrossRef] [PubMed]
- Bradaschia-Correa, V.; Josephson, A.M.; Egol, A.J.; Mizrahi, M.M.; Leclerc, K.; Huo, J.; Cronstein, B.N.; Leucht, P. Ecto-5′-nucleotidase (CD73) regulates bone formation and remodeling during intramembranous bone repair in aging mice. Tissue Cell 2017, 49, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.V.; Liu, M.; Kwon, S.K.; Iida, M.; Gong, Y.; Sangaj, N.; Varghese, S. Dysregulation of ectonucleotidase-mediated extracellular adenosine during postmenopausal bone loss. Sci. Adv. 2019, 5, eaax1387. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.; Breitbach, M.; Schildberg, F.A.; Hesse, M.; Fleischmann, B.K. Bone marrow CD73(+) mesenchymal stem cells display increased stemness in vitro and promote fracture healing in vivo. Bone Rep. 2021, 15, 101133. [Google Scholar] [CrossRef] [PubMed]
- Hinton, D.J.; McGee-Lawrence, M.E.; Lee, M.R.; Kwong, H.K.; Westendorf, J.J.; Choi, D.S. Aberrant bone density in aging mice lacking the adenosine transporter ENT1. PLoS ONE 2014, 9, e88818. [Google Scholar] [CrossRef] [PubMed]
- Ii, H.; Warraich, S.; Tenn, N.; Quinonez, D.; Holdsworth, D.W.; Hammond, J.R.; Dixon, S.J.; Seguin, C.A. Disruption of biomineralization pathways in spinal tissues of a mouse model of diffuse idiopathic skeletal hyperostosis. Bone 2016, 90, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, G.; Compagno, M.; Belisario, D.C.; Bracci, C.; Genova, T.; Mussano, F.; Vitale, M.; Horenstein, A.; Malavasi, F.; Ferracini, R.; et al. CD73/Adenosine Pathway Involvement in the Interaction of Non-Small Cell Lung Cancer Stem Cells and Bone Cells in the Pre-Metastatic Niche. Int. J. Mol. Sci. 2022, 23, 5126. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Wilder, T.; Cronstein, B.N. Rolofylline, an adenosine A1 receptor antagonist, inhibits osteoclast differentiation as an inverse agonist. Br. J. Pharmacol. 2013, 170, 1167–1176. [Google Scholar] [CrossRef] [PubMed]
- Tesch, A.M.; MacDonald, M.H.; Kollias-Baker, C.; Benton, H.P. Effects of an adenosine kinase inhibitor and an adenosine deaminase inhibitor on accumulation of extracellular adenosine by equine articular chondrocytes. Am. J. Vet. Res. 2002, 63, 1512–1519. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, S.S.; Zaki, H.F.; Raafat, S.N. The Effect of Clopidogrel and Ticagrelor on Human Adipose Mesenchymal Stem Cell Osteogenic Differentiation Potential: In Vitro Comparative Study. Adv. Pharmacol. Pharm. Sci. 2024, 2024, 2990670. [Google Scholar] [CrossRef]
- Lopez, C.D.; Diaz-Siso, J.R.; Bekisz, J.M.; Witek, L.; Tovar, N.; Gil, L.F.; Cronstein, B.N.; Flores, R.L.; Rodriguez, E.D.; Coelho, P.G. Dipyridamole Releasing 3D Printed Bioactive Ceramic Scaffolds with Osseoconductive Geometries Promote Craniofacial Bone Regeneration. Plast. Reconstr. Surg.–Glob. Open 2017, 5, 178–179. [Google Scholar] [CrossRef]
- Bekisz, J.M.; Flores, R.L.; Witek, L.; Lopez, C.D.; Runyan, C.M.; Torroni, A.; Cronstein, B.N.; Coelho, P.G. Dipyridamole enhances osteogenesis of three-dimensionally printed bioactive ceramic scaffolds in calvarial defects. J. Cranio-Maxillofac. Surg. 2018, 46, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Bekisz, J.M.; Lopez, C.D.; Corciulo, C.; Mediero, A.; Coelho, P.G.; Witek, L.; Flores, R.L.; Cronstein, B.N. The Role of Adenosine Receptor Activation in Attenuating Cartilaginous Inflammation. Inflammation 2018, 41, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Maliha, S.G.; Lopez, C.D.; Cox, M.E.; Witek, L.; Gendy, F.G.; Torroni, A.; Cronstein, B.N.; Flores, R.L.; Coelho, P.G. Bone Tissue Engineering of the Pediatric Calvarium and Alveolus using Dipyridamole-coated 3D-Printed Bioactive Ceramic Scaffolds. Plast. Reconstr. Surg.–Glob. Open 2018, 6, 80–81. [Google Scholar] [CrossRef]
- Lopez, C.D.; Witek, L.; Torroni, A.; Flores, R.L.; Demissie, D.B.; Young, S.; Cronstein, B.N.; Coelho, P.G. The role of 3D printing in treating craniomaxillofacial congenital anomalies. Birth Defects Res. 2018, 110, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.D.; Coelho, P.G.; Witek, L.; Torroni, A.; Greenberg, M.I.; Cuadrado, D.L.; Guarino, A.M.; Haque, A.J.; Cronstein, B.N.; Flores, R.L. Osteogenic Effects of Dipyridamole Versus rhBMP-2 Using 3D-Printed Bioceramic Scaffolds in a Growing Alveolar Cleft Model. Plast. Reconstr. Surg.–Glob. Open 2018, 6, 133–134. [Google Scholar] [CrossRef]
- Witek, L.; Colon, R.R.; Wang, M.M.; Torroni, A.; Young, S.; Melville, J.; Lopez, C.D.; Flores, R.L.; Cronstein, B.N.; Coelho, P.G. Tissue-engineered alloplastic scaffolds for reconstruction of alveolar defects. In Handbook of Tissue Engineering Scaffolds: Volume One; Elsevier: Amsterdam, The Netherlands, 2019; pp. 505–520. [Google Scholar]
- Lopez, C.D.; Witek, L.; Flores, R.L.; Torroni, A.; Rodriguez, E.D.; Cronstein, B.N.; Coelho, P.G. 3D printing and adenosine receptor activation for craniomaxillofacial regeneration. In Regenerative Strategies for Maxillary and Mandibular Reconstruction: A Practical Guide; Springer: Cham, Switzerland, 2019; pp. 255–267. [Google Scholar]
- Shen, C.; Witek, L.; Flores, R.L.; Tovar, N.; Torroni, A.; Coelho, P.G.; Kasper, F.K.; Wong, M.; Young, S. Three-dimensional printing for craniofacial bone tissue engineering. Tissue Eng. Part A 2020, 26, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Xu, J.; Han, X.-H.; Cui, F.-Z.; Zhang, D.-S.; Huang, S.-Y. Clinical efficacy of mineralized collagen (MC) versus anorganic bovine bone (Bio-Oss) for immediate implant placement in esthetic area: A single-center retrospective study. BMC Oral Health 2021, 21, 390. [Google Scholar] [CrossRef] [PubMed]
- Fama, C.; Kaye, G.J.; Flores, R.; Lopez, C.D.; Bekisz, J.M.; Torroni, A.; Tovar, N.; Coelho, P.G.; Witek, L. Three-Dimensionally-printed bioactive ceramic scaffolds: Construct effects on bone regeneration. J. Craniofac. Surg. 2021, 32, 1177–1181. [Google Scholar] [CrossRef]
- Maliha, S.G.; Lopez, C.D.; Coelho, P.G.; Witek, L.; Cox, M.; Meskin, A.; Rusi, S.; Torroni, A.; Cronstein, B.N.; Flores, R.L. Bone tissue engineering in the growing calvaria: A 3D printed bioceramic scaffold to reconstruct critical-sized defects in a skeletally immature pig model. Plast. Reconstr. Surg. 2020, 145, 337e–347e. [Google Scholar] [CrossRef]
- Nayak, V.V.; Slavin, B.; Bergamo, E.T.; Boczar, D.; Slavin, B.R.; Runyan, C.M.; Tovar, N.; Witek, L.; Coelho, P.G. Bone tissue engineering (BTE) of the craniofacial skeleton, Part I: Evolution and optimization of 3D-printed scaffolds for repair of defects. J. Craniofac. Surg. 2023, 34, 2016–2025. [Google Scholar] [CrossRef]
- Nayak, V.V.; Slavin, B.V.; Bergamo, E.T.; Torroni, A.; Runyan, C.M.; Flores, R.L.; Kasper, F.K.; Young, S.; Coelho, P.G.; Witek, L. Three-dimensional printing bioceramic scaffolds using direct-ink-writing for craniomaxillofacial bone regeneration. Tissue Eng. Part C Methods 2023, 29, 332–345. [Google Scholar] [CrossRef] [PubMed]
- Nayak, V.V.; Boczar, D.; Coelho, P.G.; Torroni, A.; Runyan, C.M.; Melville, J.C.; Young, S.; Cronstein, B.; Flores, R.L.; Witek, L. Innovative Treatment Modalities for Craniofacial Reconstruction. In Advancements and Innovations in OMFS, ENT, and Facial Plastic Surgery; Springer: Cham, Switzerland, 2023; pp. 291–308. [Google Scholar]
- Slavin, B.V.; Ehlen, Q.T.; Costello, J.P.; Nayak, V.V.; Bonfante, E.A.; Benalcázar Jalkh, E.B.; Runyan, C.M.; Witek, L.; Coelho, P.G. 3D Printing Applications for Craniomaxillofacial Reconstruction: A Sweeping Review. ACS Biomater. Sci. Eng. 2023, 9, 6586–6609. [Google Scholar] [CrossRef]
- Slavin, B.V.; Nayak, V.V.; Boczar, D.; Bergamo, E.T.; Slavin, B.R.; Yarholar, L.M.; Torroni, A.; Coelho, P.G.; Witek, L. Bone Tissue Engineering (BTE) of the Craniofacial Skeleton, Part II: Translational Potential of 3D-Printed Scaffolds for Defect Repair. J. Craniofacial Surg. 2024, 35, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Allahham, M.; Lerman, A.; Atar, D.; Birnbaum, Y. Why Not Dipyridamole: A Review of Current Guidelines and Re-evaluation of Utility in the Modern Era. Cardiovasc. Drugs Ther. 2022, 36, 525–532. [Google Scholar] [CrossRef]
- Barlas, R.S.; Loke, Y.K.; Mamas, M.A.; Bettencourt-Silva, J.H.; Ford, I.; Clark, A.B.; Bowles, K.M.; Metcalf, A.K.; Potter, J.F.; Myint, P.K. Effect of Antiplatelet Therapy (Aspirin + Dipyridamole Versus Clopidogrel) on Mortality Outcome in Ischemic Stroke. Am. J. Cardiol. 2018, 122, 1085–1090. [Google Scholar] [CrossRef]
- Balakumar, P.; Nyo, Y.H.; Renushia, R.; Raaginey, D.; Oh, A.N.; Varatharajan, R.; Dhanaraj, S.A. Classical and pleiotropic actions of dipyridamole: Not enough light to illuminate the dark tunnel? Pharmacol. Res. 2014, 87, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Weber, R.; Brenck, J.; Diener, H.C. Antiplatelet therapy in cerebrovascular disorders. In Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2012; pp. 519–546. [Google Scholar] [CrossRef]
- Harker, L.A.; Kadatz, R.A. Mechanism of action of dipyridamole. Thromb. Res. Suppl. 1983, 4, 39–46. [Google Scholar] [CrossRef]
- Llamas-Granda, P.; Martin-Rodriguez, L.; Largo, R.; Herrero-Beaumont, G.; Mediero, A. Tenofovir Modulates Semaphorin 4D Signaling and Regulates Bone Homeostasis, Which Can Be Counteracted by Dipyridamole and Adenosine A2A Receptor. Int. J. Mol. Sci. 2021, 22, 11490. [Google Scholar] [CrossRef]
- Mediero, A.; Frenkel, S.R.; Wilder, T.; He, W.; Mazumder, A.; Cronstein, B.N. Adenosine A2A receptor activation prevents wear particle-induced osteolysis. Sci. Transl. Med. 2012, 4, 135ra165. [Google Scholar] [CrossRef]
- Panther, E.; Idzko, M.; Herouy, Y.; Rheinen, H.; Gebicke-Haerter, P.J.; Mrowietz, U.; Dichmann, S.; Norgauer, J. Expression and function of adenosine receptors in human dendritic cells. FASEB J. 2001, 15, 1963–1970. [Google Scholar] [CrossRef] [PubMed]
- Sumaya, W.; Storey, R.F. Ticagrelor: Effects Beyond the P2Y(12) Receptor. Interv. Cardiol. Clin. 2017, 6, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Verdoia, M.; Pergolini, P.; Rolla, R.; Sartori, C.; Nardin, M.; Schaffer, A.; Barbieri, L.; Daffara, V.; Marino, P.; Bellomo, G.; et al. Vitamin D levels and high-residual platelet reactivity in patients receiving dual antiplatelet therapy with clopidogrel or ticagrelor. Platelets 2016, 27, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.R.; Zhang, X.; Hau, R.K.; Jilek, J.L.; Jennings, E.Q.; Galligan, J.J.; Foil, D.H.; Zorn, K.M.; Ekins, S.; Wright, S.H.; et al. Predicting Drug Interactions with Human Equilibrative Nucleoside Transporters 1 and 2 Using Functional Knockout Cell Lines and Bayesian Modeling. Mol. Pharmacol. 2021, 99, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Jouan, E.; Moreau, A.; Bruyere, A.; Alim, K.; Denizot, C.; Parmentier, Y.; Fardel, O. Differential Inhibition of Equilibrative Nucleoside Transporter 1 (ENT1) Activity by Tyrosine Kinase Inhibitors. Eur. J. Drug Metab. Pharmacokinet. 2021, 46, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Soto, L.M.S.; Wang, H.; Katz, M.H.; Prakash, L.R.; Kim, M.; Tzeng, C.D.; Lee, J.E.; Wolff, R.A.; Huang, Y.; et al. Overexpression of CD73 in pancreatic ductal adenocarcinoma is associated with immunosuppressive tumor microenvironment and poor survival. Pancreatology 2021, 21, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.M.; Cho, H.; Kim, T.M.; Kim, Y.; Jeon, S.; Bychkov, A.; Jung, C.K. CD73 Overexpression Promotes Progression and Recurrence of Papillary Thyroid Carcinoma. Cancers 2020, 12, 3042. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.L.; Shen, M.N.; Hu, B.; Wang, B.L.; Yang, W.J.; Lv, L.H.; Wang, H.; Zhou, Y.; Jin, A.L.; Sun, Y.F.; et al. CD73 promotes hepatocellular carcinoma progression and metastasis via activating PI3K/AKT signaling by inducing Rap1-mediated membrane localization of P110beta and predicts poor prognosis. J. Hematol. Oncol. 2019, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Cristalli, G.; Costanzi, S.; Lambertucci, C.; Lupidi, G.; Vittori, S.; Volpini, R.; Camaioni, E. Adenosine deaminase: Functional implications and different classes of inhibitors. Med. Res. Rev. 2001, 21, 105–128. [Google Scholar] [CrossRef]
- Boison, D. Adenosine kinase: Exploitation for therapeutic gain. Pharmacol. Rev. 2013, 65, 906–943. [Google Scholar] [CrossRef]
- Sauer, A.V.; Mrak, E.; Hernandez, R.J.; Zacchi, E.; Cavani, F.; Casiraghi, M.; Grunebaum, E.; Roifman, C.M.; Cervi, M.C.; Ambrosi, A.; et al. ADA-deficient SCID is associated with a specific microenvironment and bone phenotype characterized by RANKL/OPG imbalance and osteoblast insufficiency. Blood 2009, 114, 3216–3226. [Google Scholar] [CrossRef] [PubMed]
- Strazzulla, L.C.; Cronstein, B.N. Regulation of bone and cartilage by adenosine signaling. Purinergic Signal. 2016, 12, 583–593. [Google Scholar] [CrossRef]
- Manson, D.; Diamond, L.; Oudjhane, K.; Hussain, F.B.; Roifman, C.; Grunebaum, E. Characteristic scapular and rib changes on chest radiographs of children with ADA-deficiency SCIDS in the first year of life. Pediatr. Radiol. 2013, 43, 589–592. [Google Scholar] [CrossRef] [PubMed]
- Flinn, A.M.; Gennery, A.R. Adenosine deaminase deficiency: A review. Orphanet J. Rare Dis. 2018, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Liao, H.; Yu, H.P.; Song, W.; Zhang, G.; Lu, B.; Zhu, Y.J.; Yu, W.; He, Y. Amorphous calcium phosphate nanoparticles using adenosine triphosphate as an organic phosphorus source for promoting tendon-bone healing. J. Nanobiotechnol. 2021, 19, 270. [Google Scholar] [CrossRef] [PubMed]
- Hoque, J.; Zeng, Y.; Newman, H.; Gonzales, G.; Lee, C.; Varghese, S. Microgel-Assisted Delivery of Adenosine to Accelerate Fracture Healing. ACS Biomater. Sci. Eng. 2022, 8, 4863–4872. [Google Scholar] [CrossRef] [PubMed]
- Cronstein, B.N.; Angle, S.R. Purines and Adenosine Receptors in Osteoarthritis. Biomolecules 2023, 13, 1760. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Corciulo, C.; Arabagian, S.; Ulman, A.; Cronstein, B.N. Adenosine-Functionalized Biodegradable PLA-b-PEG Nanoparticles Ameliorate Osteoarthritis in Rats. Sci. Rep. 2019, 9, 7430. [Google Scholar] [CrossRef] [PubMed]
- Corciulo, C.; Castro, C.M.; Coughlin, T.; Jacob, S.; Li, Z.; Fenyo, D.; Rifkin, D.B.; Kennedy, O.D.; Cronstein, B.N. Intraarticular injection of liposomal adenosine reduces cartilage damage in established murine and rat models of osteoarthritis. Sci. Rep. 2020, 10, 13477. [Google Scholar] [CrossRef]
- Corciulo, C.; Lendhey, M.; Wilder, T.; Schoen, H.; Cornelissen, A.S.; Chang, G.; Kennedy, O.D.; Cronstein, B.N. Endogenous adenosine maintains cartilage homeostasis and exogenous adenosine inhibits osteoarthritis progression. Nat. Commun. 2017, 8, 15019. [Google Scholar] [CrossRef]
- Cheng, G.; Yin, C.; Tu, H.; Jiang, S.; Wang, Q.; Zhou, X.; Xing, X.; Xie, C.; Shi, X.; Du, Y.; et al. Controlled Co-delivery of Growth Factors through Layer-by-Layer Assembly of Core-Shell Nanofibers for Improving Bone Regeneration. ACS Nano 2019, 13, 6372–6382. [Google Scholar] [CrossRef] [PubMed]
- Torres-Giner, S.; Martinez-Abad, A.; Gimeno-Alcañiz, J.V.; Ocio, M.J.; Lagaron, J.M. Controlled Delivery of Gentamicin Antibiotic from Bioactive Electrospun Polylactide-Based Ultrathin Fibers. Adv. Eng. Mater. 2012, 14, B112–B122. [Google Scholar] [CrossRef]
- Li, P. 3D bioprinting: Regulation, innovation, and patents. In 3D Bioprinting for Reconstructive Surgery; Elsevier: Amsterdam, The Netherlands, 2018; pp. 217–231. [Google Scholar]
- Murphy, S.V.; De Coppi, P.; Atala, A. Opportunities and challenges of translational 3D bioprinting. Nat. Biomed. Eng. 2020, 4, 370–380. [Google Scholar] [CrossRef] [PubMed]


| Drug | Target | Species | Location | Results | Reference |
|---|---|---|---|---|---|
| NA | A2A | Mice (n = 14) | Femur | A2A knockout mice showed significantly lower ratios of bone volume to total volume with decreased bone mineral density and bone mineral content. | [52] |
| DIPY | ENT-1 | Sheep (n = 15) | Vertebrae | The DIPY scaffold provided increased osteointegration three weeks postoperatively, while no differences were seen six or twelve weeks postoperatively. | [62] |
| DIPY | ENT-1 | Pig (n = 14) | Calvarium | DIPY scaffolds increased bone growth relative to control, while maintaining native bone mechanics. No ectopic bone growth or excessive inflammation was seen. | [63] |
| DIPY | ENT-1 | Rabbit (n = 18) | Alveolus | DIPY-coated scaffolds had statistically similar bone regeneration to rhBMP-2-coated scaffolds, while avoiding early suture fusion associated with rhBMP-2. There were no mechanical differences between bones. | [64] |
| DIPY | ENT-1 | Rabbit (n = 16) | Calvarium/Alveolus | DIPY scaffolds promoted osteogenic growth better than autologous bone grafts, with mechanical properties, vascularization, and organization comparable to native bone. DIPY scaffolds did not result in premature closure of craniofacial sutures or disruption of facial symmetry. | [65] |
| DIPY | ENT-1 | Mice (n = 120) | Calvarium | DIPY enhanced bone regeneration with increased osteoblasts and decreased osteoclasts relative to controls. DIPY showed accelerated bone regeneration relative to BMP-2 treatment. A2A knockout mice did not show enhanced bone regeneration with DIPY. | [17] |
| DIPY | ENT-1 | Rabbit (n = 15) | Mandible | The DIPY treatment group demonstrated the most bone regeneration relative to control and collagen groups with no inflammatory response. | [66] |
| DIPY | ENT-1 | Rabbit (n = 16) | Calvarium | DIPY-treated scaffolds demonstrated significantly more bone growth than control groups. No ectopic bone formation was noted in the DIPY-treated group. | [67] |
| DIPY | ENT-1 | Rabbit (n = 24) | Radius | 3D-printed scaffolds treated with DIPY showed increased bone regeneration in a dose-dependent manner, while maintaining the biomechanical properties of native bone. | [68] |
| Ticagrelor | ENT-1 | Mice (n = 120) | Calvarium | Increased bone area, bone volume, and bone mineral density with an increase in alkaline phosphatase expression. | [69] |
| Ticagrelor | ENT-1 | Rats (n = 40) | Tibia | Higher, but not statistically significant, new bone formation relative to implants treated with acetylsalicylic icracid, clopidogrel, or prasugrel. | [70] |
| NA | CD73 | Mice | Femur/Tibia | CD73 knockout mice had lower bone mineral density, reduced trabecular bone volume, and decreased trabecular thickness. They exhibited decreased osteoblast differentiation. | [71] |
| NA | CD73 | Mice (n = 20) | Tibia | CD73 knockout mice exhibited delayed bone regeneration and decreased bone matrix deposition with decreased callus size following fracture. These mice had reduced cell proliferation, alkaline phosphatase activity, and osteoclast numbers, suggesting that CD73 may be necessary to induce osteoblast activity and stimulate bone regeneration. | [72] |
| BAY 60-6583 | A2B | Mice (n = 12) | Vertebrae | Osteoporotic animals (secondary to low estradiol) exhibit decreased CD73 and CD39 with lower extracellular adenosine. An A2B agonist, BAY 60-6583, was administered and showed decreased vertebral and femoral bone loss with increased bone density despite no changes in CD73/39 expression. | [73] |
| CD73(+) mesenchymal stem cells (MSCs) | CD73 | Mice (n = 15) | Femur | MSCs expressing CD73 contributed to the endochondral ossification process immediately after fracture and continued to differentiate into osteoblasts and subsequently osteocytes throughout the fracture healing process. CD73+ cells were also found to contribute to neovascularization at the fracture site. CD73+ MSCs were grafted at the fracture site, showing increased bone callus and lamellar bone formation. | [74] |
| NA | ENT-1 | Mice (n = 18) | NA | ENT-1 knockout mice showed reduced bone density and bone mineral density relative to controls in the thoracic and lumbar spine and femur. ENT-1 knockout mice were also found to have increased TRAP expression in long bones. | [75] |
| NA | ENT-1 | Mice (n = 16) | Vertebrae | ENT-1 knockout mice showed increased calcification and hypermineralization of intravertebral discs. | [76] |
| Target | Drug | Cell Line | Location | Results | Reference |
|---|---|---|---|---|---|
| ENT-1 | Ticagrelor | Bone marrow cells | Femur/Tibia | Inhibited osteoclastogenesis in an adenosine concentration-dependent manner with decreased receptor activator of NF-κB ligand (RANKL) expression and increased osteoprotegerin expression. | [69] |
| CD73 | NA | Osteoblasts | Calvarium | CD73-deficient osteoblasts exhibited decreased alkaline phosphatase expression with delayed calcification. Over-expression of CD73 led to accelerated osteoblast differentiation and increased adenosine receptor expression, which was stimulated by A2B signaling. | [71] |
| CD73/39 | NA | Bone marrow cells | Femur/Tibia/Humerus/Radius/Ulna/Vertebra | Bone marrow cells from osteoporotic bones (estradiol deficient) showed decreased expression of CD73 and CD39 with a significant decrease in extracellular adenosine. Increased extracellular adenosine and A2B signaling were shown to promote osteoblastogenesis, decrease osteoclast differentiation, and reduce osteoclast transcription factor and TRAP. | [73] |
| CD73 | Anti-CD73 monoclonal antibody (moAb)/adenosine 5′-(α,β-methylene) diphosphate (APCP) | Cancer stem cells/Osteoblasts/Osteoclasts | NA | Higher levels of CD73 were discovered in osteoblasts versus osteoclasts, leading to higher adenosine production by osteoblasts. Osteoclasts primarily expressed A3, while osteoclasts and osteoblasts expressed A1 and A2A. Osteoblasts expressed A2B. Both anti-CD73 moAb and APCP blocked CD73, decreasing adenosine concentrations. | [77] |
| A1 | Rolofylline | Bone marrow cells | Femur/Tibia | Rolofylline blocked A1 and suppressed osteoclast differentiation, demonstrated by decreased expression of osteoclast-specific genes. This effect remained even in CD39 and CD73 deficient mice, indicating that A1 is the primary component for osteoclast differentiation. | [78] |
| CD73 | CD73 MSCs | Bone marrow cells | Femur/Tibia | CD73+ MSCs showed increased plasticity and osteogenic potential relative to the CD73- counterparts. | [74] |
| ENT-1 | CGS21680/DIPY | Osteoclasts | Femur/Tibia | Activation of A2A by CGS21680 inhibited osteoclastogenesis in a dose-dependent manner. A2A agonism decreased bone resorption and resulted in decreased concentrations of IL-1B. | [52] |
| ENT-1 | CGS21680/DIPY | Osteoblasts/Osteoclasts | Calvarium | CGS21680 and DIPY inhibited osteoclasts, decreasing cathepsin K and RANK, while activating osteoblasts, showing increased levels of osteocalcin and osteonectin expression. | [17] |
| Adenosine Deaminase | Erythro-9-(2-hydroxy-3-nonyl) adenine hydrochloride (EHNA) | Chondrocytes | MTP/MCP Joints | Administration of EHNA did not significantly increase the extracellular concentration of adenosine. However, EHNA in combination with 5′-iodotubercidin (ITU) demonstrated a synergistic effect and largely increased concentrations of adenosine. | [79] |
| Adenosine Kinase | ITU | Chondrocytes | MTP/MCP Joints | ITU administration demonstrated significant increases in extracellular adenosine in a time-dependent manner. | [79] |
| ENT-1 | NA | Annulus Fibrosus Cells | Intravertebral Discs | ENT-1 knockout cells from the annulus fibrosus displayed hyper mineralization and increased alkaline phosphatase activity, resulting in calcifications. | [76] |
| ENT-1 | Ticagrelor | MSCs | Adipose Tissue | MSCs in the ticagrelor group demonstrated increased extracellular matrix formation, increased alkaline phosphatase activity, and decreased IL-6 and TNF-α expression. | [80] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ehlen, Q.T.; Mirsky, N.A.; Slavin, B.V.; Parra, M.; Nayak, V.V.; Cronstein, B.; Witek, L.; Coelho, P.G. Translational Experimental Basis of Indirect Adenosine Receptor Agonist Stimulation for Bone Regeneration: A Review. Int. J. Mol. Sci. 2024, 25, 6104. https://doi.org/10.3390/ijms25116104
Ehlen QT, Mirsky NA, Slavin BV, Parra M, Nayak VV, Cronstein B, Witek L, Coelho PG. Translational Experimental Basis of Indirect Adenosine Receptor Agonist Stimulation for Bone Regeneration: A Review. International Journal of Molecular Sciences. 2024; 25(11):6104. https://doi.org/10.3390/ijms25116104
Chicago/Turabian StyleEhlen, Quinn T., Nicholas A. Mirsky, Blaire V. Slavin, Marcelo Parra, Vasudev Vivekanand Nayak, Bruce Cronstein, Lukasz Witek, and Paulo G. Coelho. 2024. "Translational Experimental Basis of Indirect Adenosine Receptor Agonist Stimulation for Bone Regeneration: A Review" International Journal of Molecular Sciences 25, no. 11: 6104. https://doi.org/10.3390/ijms25116104





