The Effect of Tryptophan-to-Tyrosine Mutation at Position 61 of the Nonstructural Protein of Severe Fever with Thrombocytopenia Syndrome Virus on Viral Replication through Autophagosome Modulation
Abstract
:1. Introduction
2. Results
2.1. NS Expression Induces the Formation of Autophagosomes and Increases Replication
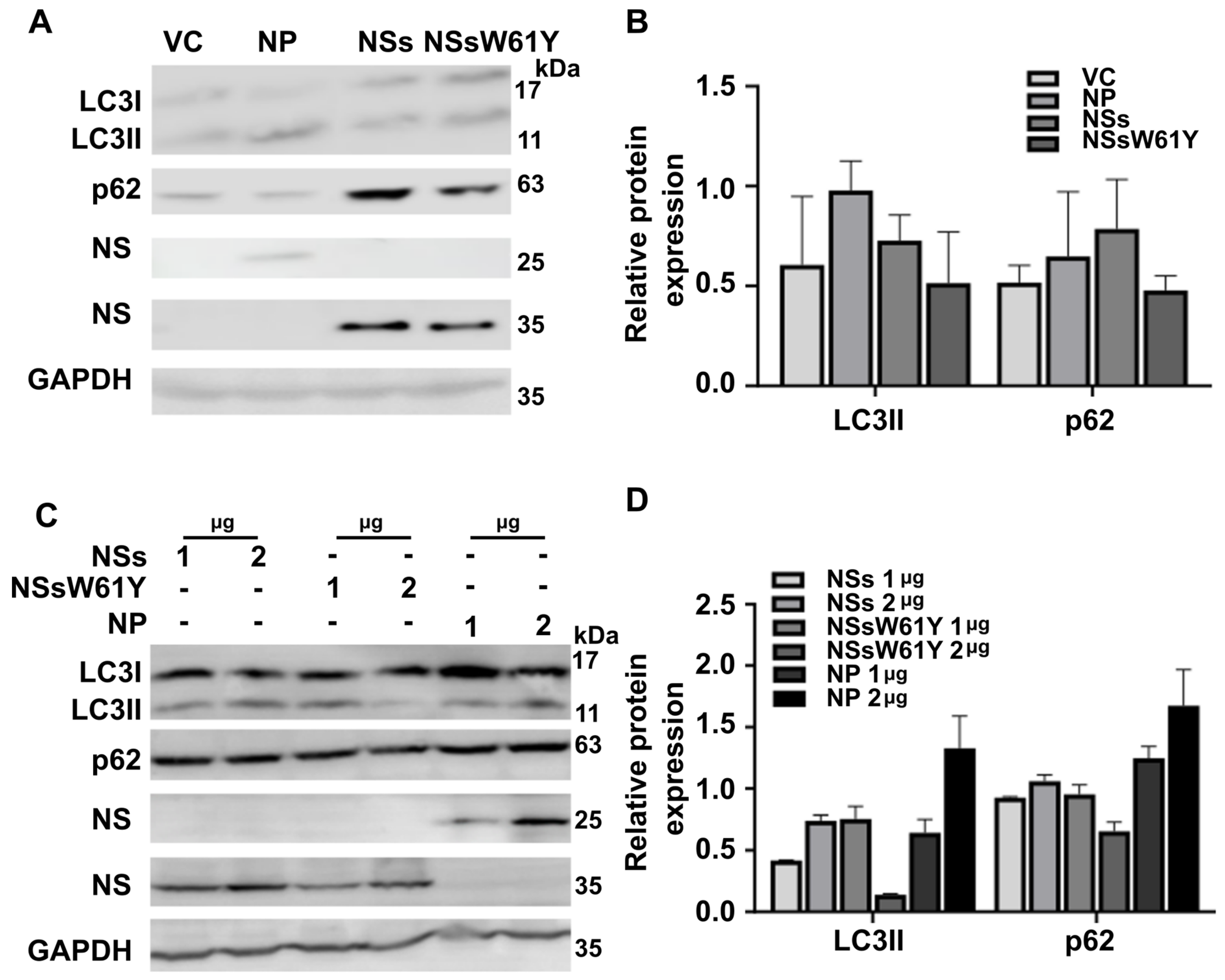
2.2. Autophagosome Marker Levels Are Downregulated by NSsW61Y Expression
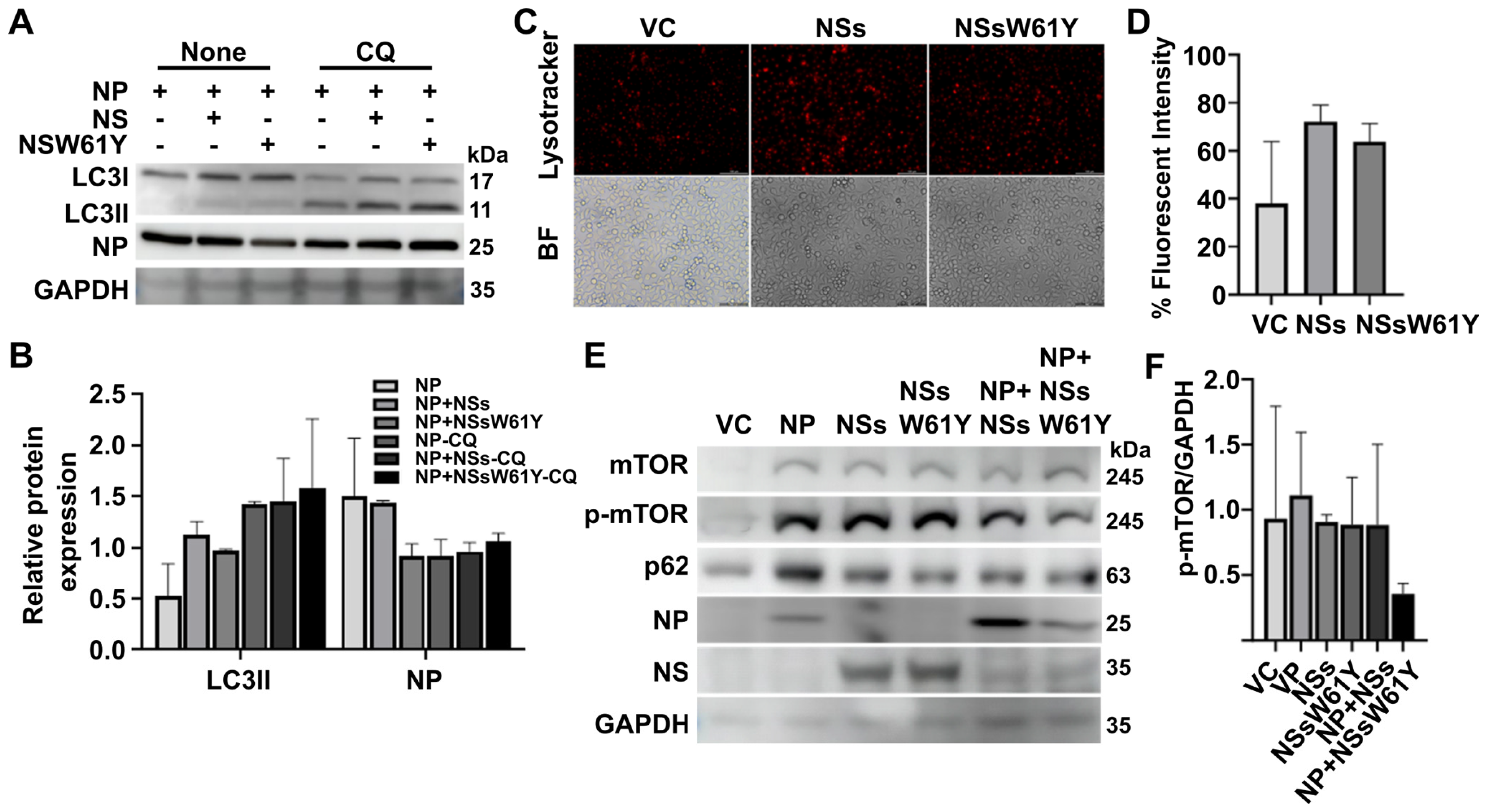
2.3. Effect of NSsW61Y on Autophagy Related to the Lysosome-Dependent Degradation Pathway
2.4. The Relationship between SFTSV NSsW61Y and mTOR-Dependent Autophagy
3. Discussion
4. Materials and Methods
4.1. Cell Culture and virus Propagation
4.2. Antibodies and Reagents
4.3. Plasmids and Transient Transfection
4.4. Western Blot Analysis
4.5. LysoTracker Deep Red Staining and Immunofluorescence Microscopy
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, S.-W.; Han, M.-G.; Yun, S.-M.; Park, C.; Lee, W.-J.; Ryou, J. Severe fever with thrombocytopenia syndrome virus, South Korea, 2013. Emerg. Infect. Dis. 2014, 20, 1880. [Google Scholar] [CrossRef]
- Casel, M.A.; Park, S.J.; Choi, Y.K. Severe fever with thrombocytopenia syndrome virus: Emerging novel phlebovirus and their control strategy. Exp. Mol. Med. 2021, 53, 713–722. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Y.; Zhao, L.; Li, B.; Yu, H.; Wen, H.; Yu, X.-J. An emerging hemorrhagic fever in China caused by a novel bunyavirus SFTSV. Sci. China Life Sci. 2013, 56, 697–700. [Google Scholar] [CrossRef]
- Suzuki, T.; Sato, Y.; Sano, K.; Arashiro, T.; Katano, H.; Nakajima, N.; Shimojima, M.; Kataoka, M.; Takahashi, K.; Wada, Y. Severe fever with thrombocytopenia syndrome virus targets B cells in lethal human infections. J. Clin. Investig. 2020, 130, 799–812. [Google Scholar] [CrossRef]
- Seo, J.-W.; Kim, D.; Yun, N.; Kim, D.-M. Clinical update of severe fever with thrombocytopenia syndrome. Viruses 2021, 13, 1213. [Google Scholar] [CrossRef]
- Yang, T.; Huang, H.; Jiang, L.; Li, J. Overview of the immunological mechanism underlying severe fever with thrombocytopenia syndrome. Int. J. Mol. Med. 2022, 50(3), 1–12. [Google Scholar] [CrossRef]
- Wu, Y.-X.; Yang, X.; Leng, Y.; Li, J.-C.; Yuan, L.; Wang, Z.; Fan, X.-J.; Yuan, C.; Liu, W.; Li, H. Human-to-human transmission of severe fever with thrombocytopenia syndrome virus through potential ocular exposure to infectious blood. Int. J. Infect. Dis. 2022, 123, 80–83. [Google Scholar] [CrossRef]
- Wei, X.; Li, S.; Lu, Y.; Qiu, L.; Xu, N.; Guo, X.; Chen, M.; Liang, H.; Cheng, D.; Zhao, L. Severe fever with thrombocytopenia syndrome virus aerosol infection in C57/BL6 mice. Virology 2023, 581, 58–62. [Google Scholar] [CrossRef]
- Ning, Y.-J.; Feng, K.; Min, Y.-Q.; Cao, W.-C.; Wang, M.; Deng, F.; Hu, Z.; Wang, H. Disruption of type I interferon signaling by the nonstructural protein of severe fever with thrombocytopenia syndrome virus via the hijacking of STAT2 and STAT1 into inclusion bodies. J. Virol. 2015, 89, 4227–4236. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Lu, G.; Wen, L.; Luo, P.; Huang, Y.; Liang, R.; Tang, K.; Qin, Z.; Chan, C.C.-Y.; Chik, K.K.-H. Severe fever with thrombocytopenia syndrome virus (SFTSV)-host interactome screen identifies viral nucleoprotein-associated host factors as potential antiviral targets. Comput. Struct. Biotechnol. J. 2021, 19, 5568–5577. [Google Scholar] [CrossRef] [PubMed]
- Shoji-Kawata, S.; Levine, B. Autophagy, antiviral immunity, and viral countermeasures. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2009, 1793, 1478–1484. [Google Scholar] [CrossRef]
- Liu, S.; Su, Y.; Lu, Z.; Zou, X.; Xu, L.; Teng, Y.; Wang, Z.; Wang, T. The SFTSV Nonstructural Proteins Induce Autophagy to Promote Viral Replication via Interaction with Vimentin. J. Virol. 2023, 97, e00302–e00323. [Google Scholar] [CrossRef]
- Shao, Z.; Borde, C.; Quignon, F.; Escargueil, A.; Maréchal, V. Epstein–Barr Virus BALF0 and BALF1 Modulate Autophagy. Viruses 2019, 11, 1099. [Google Scholar] [CrossRef]
- Chan, S.T.; Ou, J.-h.J. Hepatitis C virus-induced autophagy and host innate immune response. Viruses 2017, 9, 224. [Google Scholar] [CrossRef]
- Gerada, C.; Ryan, K.M. Autophagy, the innate immune response and cancer. Mol. Oncol. 2020, 14, 1913–1929. [Google Scholar] [CrossRef]
- Park, J.-Y.; Sivasankar, C.; Kirthika, P.; Prabhu, D.; Lee, J.H. Non-Structural Protein-W61 as a Novel Target in Severe Fever with Thrombocytopenia Syndrome Virus (SFTSV): An In-Vitro and In-Silico Study on Protein-Protein Interactions with Nucleoprotein and Viral Replication. Viruses 2023, 15, 1963. [Google Scholar] [CrossRef]
- Yan, J.-m.; Zhang, W.-k.; Yan, L.-n.; Jiao, Y.-J.; Zhou, C.-m.; Yu, X.-j. Bunyavirus SFTSV exploits autophagic flux for viral assembly and egress. Autophagy 2022, 18, 1599–1612. [Google Scholar] [CrossRef]
- Feng, K.; Zhang, H.; Jiang, Z.; Zhou, M.; Min, Y.Q.; Deng, F.; Li, P.; Wang, H.; Ning, Y.J. SFTS bunyavirus NSs protein sequestrates mTOR into inclusion bodies and deregulates mTOR-ULK1 signaling, provoking pro-viral autophagy. J. Med. Virol. 2023, 95, e28371. [Google Scholar] [CrossRef]
- Bik, E.; Mateuszuk, L.; Orleanska, J.; Baranska, M.; Chlopicki, S.; Majzner, K. Chloroquine-induced accumulation of autophagosomes and lipids in the endothelium. Int. J. Mol. Sci. 2021, 22, 2401. [Google Scholar] [CrossRef] [PubMed]
- Mauthe, M.; Orhon, I.; Rocchi, C.; Zhou, X.; Luhr, M.; Hijlkema, K.-J.; Coppes, R.P.; Engedal, N.; Mari, M.; Reggiori, F. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy 2018, 14, 1435–1455. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Dellibovi-Ragheb, T.A.; Kerviel, A.; Pak, E.; Qiu, Q.; Fisher, M.; Takvorian, P.M.; Bleck, C.; Hsu, V.W.; Fehr, A.R. β-Coronaviruses use lysosomes for egress instead of the biosynthetic secretory pathway. Cell 2020, 183, 1520–1535.e1514. [Google Scholar] [CrossRef] [PubMed]
- Fogel, J.L.; Thein, T.Z.T.; Mariani, F.V. Use of LysoTracker to detect programmed cell death in embryos and differentiating embryonic stem cells. JoVE (J. Vis. Exp.) 2012, 68, e4254. [Google Scholar]
- Munson, M.J.; Ganley, I.G. MTOR, PIK3C3, and autophagy: Signaling the beginning from the end. Autophagy 2015, 11, 2375–2376. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.C.; Guan, K.-L. mTOR: A pharmacologic target for autophagy regulation. J. Clin. Investig. 2015, 125, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Alers, S.; Löffler, A.S.; Wesselborg, S.; Stork, B. Role of AMPK-mTOR-Ulk1/2 in the regulation of autophagy: Cross talk, shortcuts, and feedbacks. Mol. Cell. Biol. 2012, 32, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Galluzzi, L.; Zitvogel, L.; Kroemer, G. Autophagy and cellular immune responses. Immunity 2013, 39, 211–227. [Google Scholar] [CrossRef] [PubMed]
- Jackson, W.T.; Giddings Jr, T.H.; Taylor, M.P.; Mulinyawe, S.; Rabinovitch, M.; Kopito, R.R.; Kirkegaard, K. Subversion of cellular autophagosomal machinery by RNA viruses. PLoS Biol. 2005, 3, e156. [Google Scholar] [CrossRef] [PubMed]
- Ke, P.-Y.; Chen, S.S.-L. Autophagy: A novel guardian of HCV against innate immune response. Autophagy 2011, 7, 533–535. [Google Scholar] [CrossRef]
- Romeo, M.A.; Masuelli, L.; Gaeta, A.; Nazzari, C.; Granato, M.; Gilardini Montani, M.S.; Faggioni, A.; Cirone, M. Impact of HHV-6A and HHV-6B lytic infection on autophagy and endoplasmic reticulum stress. J. Gen. Virol. 2019, 100, 89–98. [Google Scholar] [CrossRef]
- Nowag, H.; Guhl, B.; Thriene, K.; Romao, S.; Ziegler, U.; Dengjel, J.; Münz, C. Macroautophagy proteins assist Epstein Barr virus production and get incorporated into the virus particles. EBioMedicine 2014, 1, 116–125. [Google Scholar] [CrossRef]
- Granato, M.; Santarelli, R.; Farina, A.; Gonnella, R.; Lotti, L.V.; Faggioni, A.; Cirone, M. Epstein-barr virus blocks the autophagic flux and appropriates the autophagic machinery to enhance viral replication. J. Virol. 2014, 88, 12715–12726. [Google Scholar] [CrossRef]
- Sir, D.; Ou, J.-h.J. Autophagy in viral replication and pathogenesis. Mol. Cells 2010, 29, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Liu, M.-m.; Lei, X.-y.; Yu, X.-j. SFTS phlebovirus promotes LC3-II accumulation and nonstructural protein of SFTS phlebovirus co-localizes with autophagy proteins. Sci. Rep. 2018, 8, 5287. [Google Scholar] [CrossRef]
- Pi, S.; Seng-Libi, L.; Xao-Ping, D. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed. Environ. Sci. 2003, 16, 246–255. [Google Scholar]
- Lin, H.-T.; Tsai, H.-Y.; Liu, C.-P.; Yuan, T.T.-T. Comparability of bovine virus titers obtained by TCID50/mL and FAID50/mL. J. Virol. Methods 2010, 165, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-Y.; Hewawaduge, C.; Sivasankar, C.; Lloren, K.K.S.; Oh, B.; So, M.Y.; Lee, J.H. An mRNA-Based Multiple Antigenic Gene Expression System Delivered by Engineered Salmonella for Severe Fever with Thrombocytopenia Syndrome and Assessment of Its Immunogenicity and Protection Using a Human DC-SIGN-Transduced Mouse Model. Pharmaceutics 2023, 15, 1339. [Google Scholar] [CrossRef]
- Jinyong, Z.; Xiaoli, Z.; Weijun, Z.; Ying, G.; Gang, G.; Xuhu, M.; Quanming, Z. Fusion expression and immunogenicity of Bordetella pertussis PTS1-FHA protein: Implications for the vaccine development. Mol. Biol. Rep. 2011, 38, 1957–1963. [Google Scholar] [CrossRef]
- Shi, B.; Xue, M.; Wang, Y.; Wang, Y.; Li, D.; Zhao, X.; Li, X. An improved method for increasing the efficiency of gene transfection and transduction. Int. J. Physiol. Pathophysiol. Pharmacol. 2018, 10, 95. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-Y.; Senevirathne, A.; Lloren, K.K.S.; Lee, J.H. The Effect of Tryptophan-to-Tyrosine Mutation at Position 61 of the Nonstructural Protein of Severe Fever with Thrombocytopenia Syndrome Virus on Viral Replication through Autophagosome Modulation. Int. J. Mol. Sci. 2024, 25, 6394. https://doi.org/10.3390/ijms25126394
Park J-Y, Senevirathne A, Lloren KKS, Lee JH. The Effect of Tryptophan-to-Tyrosine Mutation at Position 61 of the Nonstructural Protein of Severe Fever with Thrombocytopenia Syndrome Virus on Viral Replication through Autophagosome Modulation. International Journal of Molecular Sciences. 2024; 25(12):6394. https://doi.org/10.3390/ijms25126394
Chicago/Turabian StylePark, Ji-Young, Amal Senevirathne, Khristine Kaith S. Lloren, and John Hwa Lee. 2024. "The Effect of Tryptophan-to-Tyrosine Mutation at Position 61 of the Nonstructural Protein of Severe Fever with Thrombocytopenia Syndrome Virus on Viral Replication through Autophagosome Modulation" International Journal of Molecular Sciences 25, no. 12: 6394. https://doi.org/10.3390/ijms25126394





