Virus-like Particles as Vaccines for Allergen-Specific Therapy: An Overview of Current Developments
Abstract
1. Introduction
2. VLPs as Vaccine: Success Stories
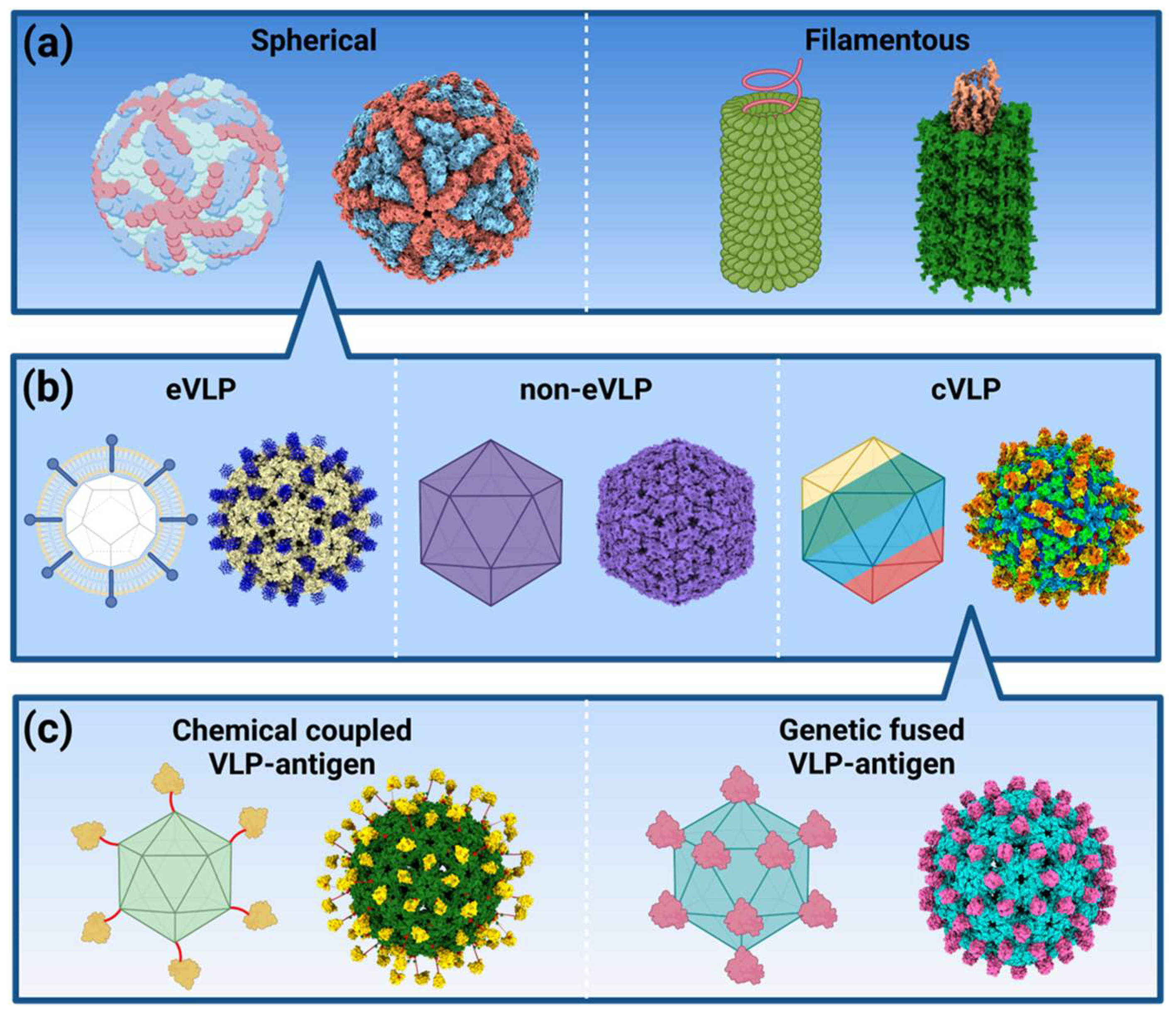
2.1. Structural Features
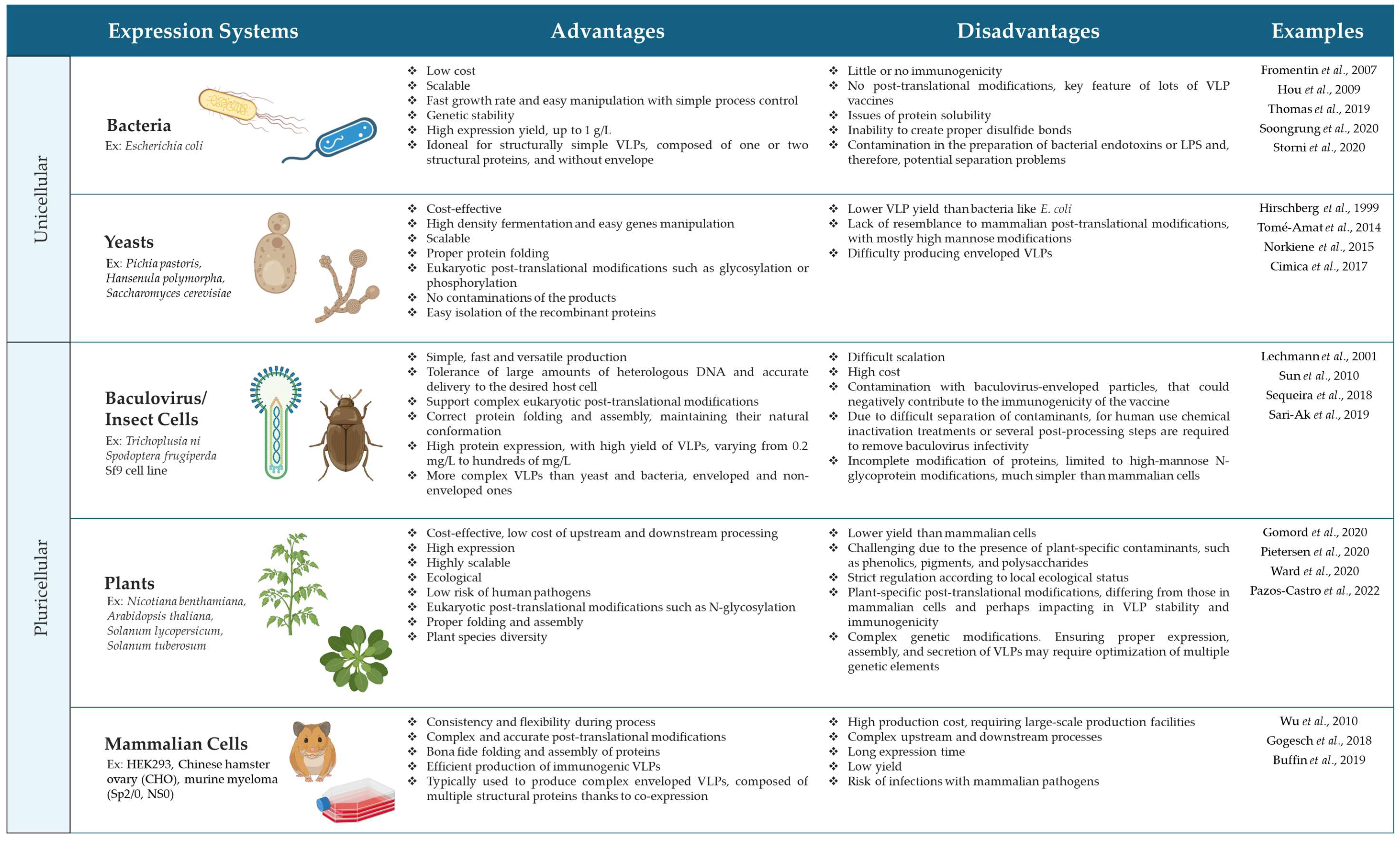
2.2. Challenges in the Production of VLPs
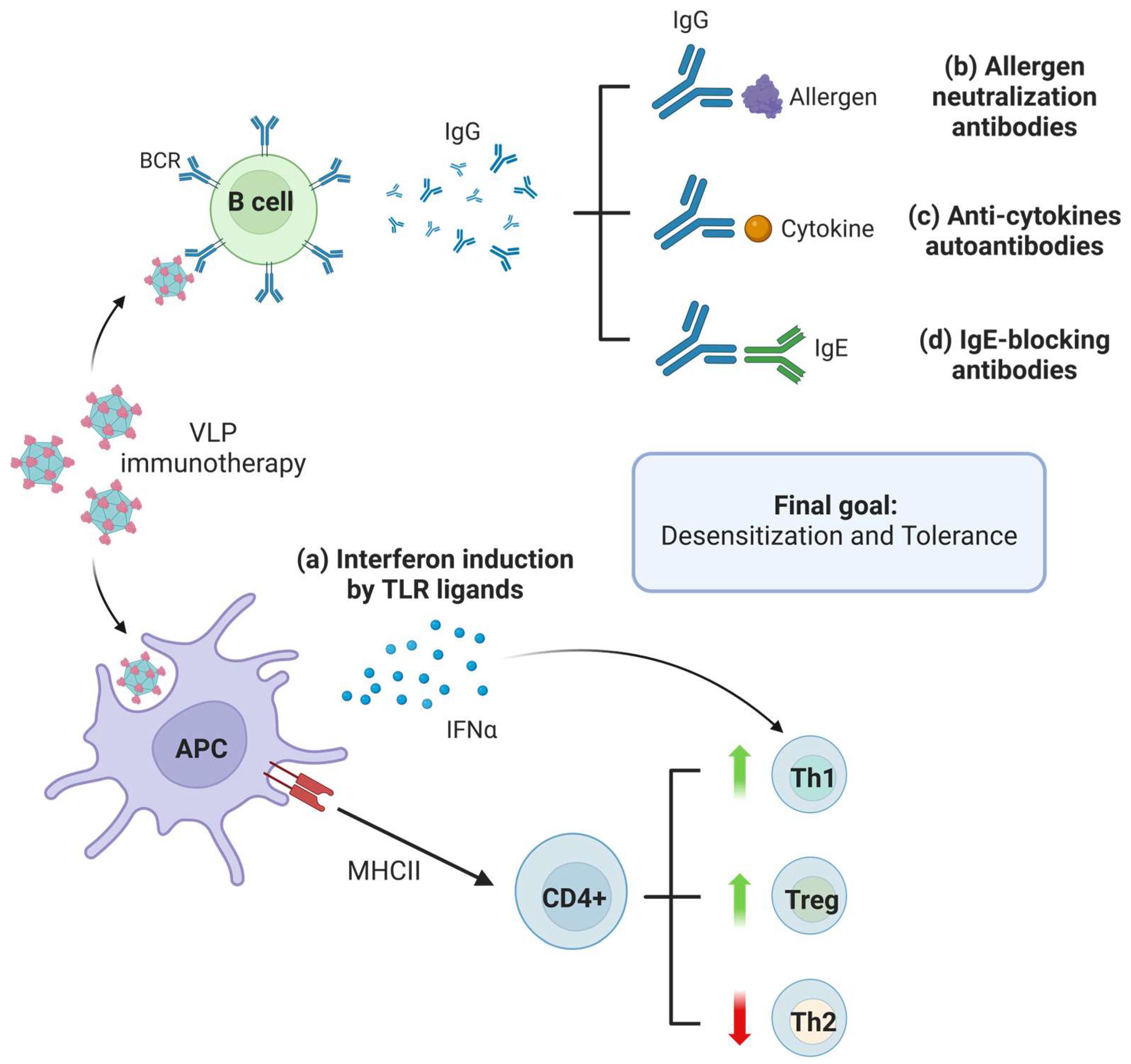
2.3. Immunological Mechanisms of VLPs
3. Application of VLPs in the Treatment of Allergic Diseases
3.1. Allergen-Dependent VLPs
| ALLERGEN-DEPENDENT | ||||
|---|---|---|---|---|
| VLP | Target | Organism | Observed Effects | Reference |
| Vaccine BM32 PreS domain of Hepatitis B Virus (HBV) | Phl p 1, 2, 5, 6 | Human phase II clinical trial | Increase in IgG4 allergen-specific antibodies No IgE levels enhanced | ClinicalTrials.gov Identifier: NCT01538979 |
| Monoley-murine-Leukemia Virus (MLV) | Art v 1 | Mouse | Surface exposed Art v 1 VLP induces allergen-specific antibodies Induction of Th1/Treg response | [103] |
| Monoley-murine-Leukemia Virus (MLV), displaying GM-CSF | Ova-derived peptides | Mouse | Expansion of CD11b+ cells within bone marrow Induction of antigen-specific CD4+ and CD8+ T-cell proliferation | [75] |
| Acinetobacter phage AP205 fused to SpyCatcher (SpyCatcher-VLP) | Der p 2 | Mouse | Blocking of allergen-specific IgG Prevention of specific IgE | [61] |
| HypoCat™ Cucumber Mosaic Virus engineered with tetanus toxoid universal T-cell epitope (CuMVTT) | Fel d 1 | Cat | Development of neutralizing antibodies against Fel d 1 Sustained specific IgG antibody response Reduction in symptoms in cat owners | [60,104] |
| Cucumber Mosaic Virus engineered with tetanus toxoid universal T-cell epitope (CuMVTT) | Ara h 1, 2, R | Mouse | Protection of peanut-sensitized mice against anaphylaxis to the whole peanut extract Induction of specific IgG antibodies | [64] |
| TM/CT domain of Influenza Virus hemagglutinin | Der p 2 | Mouse | Strong IgG response Low basophil degranulation of human sera | [72] |
| Hepatitis B core antigen (HBcAg) | Che a 3-derived peptide | Mouse | Lack of IgE-binding and basophil degranulation activity Induction of rChe a 3-related IgG antibody Low polcalcin-specific IgE | [105] |
| Turnip Mosaic Virus (TuMV) | Pru p 3 | Mouse | No adjuvants needed Reduction in allergen-specific IgE and IgG2a | [12] |
| Cucumber Mosaic Virus engineered with tetanus toxoid universal T-cell epitope (CuMVTT) | Ara h 2 | Mouse | Significant anti-Ara h 2 IgG response Confer systemic protection | [102] |
| PreS domain of Hepatitis B Virus (HBV) | Bet v 1/Mal d 1-derived peptides | Rabbit | Lack of IgE reactivity and allergenic activity Presence of neutralizing antibodies to both allergens at the same time | [106] |
| Cucumber Mosaic Virus engineered with tetanus toxoid universal T-cell epitope (CuMVTT) | Ara h 2 | Human phase I clinical trial | Recruiting candidates | ClinicalTrials.gov Identifier: NCT05476497 |
| ALLERGEN INDEPENDENT: Immunomodulation by TLR ligands | ||||
| Bacteriophage Qβ-derived VLP | CpG-motif G10 (TLR9 ligand) | Human, phase IIb clinical trial | Improvement of rhinoconjunctivitis symptoms in dust mite-allergic patients | ClinicalTrials.gov Identifier: NCT00800332 |
| Bacteriophage Qβ-derived VLP | CpG-motif G10 (TLR9 ligand) | Human, phase II clinical trial | Improvement of asthma symptoms and relief medications in allergic patients | ClinicalTrials.gov Identifier: NCT00890734 |
| ALLERGEN INDEPENDENT: Neutralize cytokines | ||||
| Hepatitis B core antigen (HBcAg) | Recombinant IL-13 peptide | Mouse | Partial suppression of induced airway remodeling features Production of anti-IL13 antibodies | [107] |
| Cucumber Mosaic Virus engineered with tetanus toxoid universal T-cell epitope (CuMVTT) | Recombinant IL-5 | Horse | Induction of neutralizing anti-IL-5 IgG Reduction in eosinophil inflammation in lesions Response maintained over a year | [108,109,110] |
| ALLERGEN INDEPENDENT: Neutralize allergen-specific IgE | ||||
| Bacteriophage Qβ-derived VLP | IgE peptides Y and P | Mouse | Strong antibody response to IgE peptides by TLR7 activation Production of blocking anti-IgE antibodies | [19] |
| Cucumber Mosaic Virus engineered with tetanus toxoid universal T-cell epitope (CuMVTT) | Synthetic mouse IgE-Fc fragments | Mouse | High amount of anti-IgE antibodies Less IgE bound to FcεRI on the surface of basophils | [111] |
3.2. Allergen-Independent VLPs
3.2.1. Immunomodulation by TLR Ligands
3.2.2. VLPs Coupled with Cytokines
3.2.3. Neutralizing/Blocking Antibodies against Allergen-Specific IgE
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Bartha, I.; Almulhem, N.; Santos, A.F. Feast for Thought: A Comprehensive Review of Food Allergy 2021–2023. J. Allergy Clin. Immunol. 2024, 153, 576–594. [Google Scholar] [CrossRef] [PubMed]
- Sampath, V.; Abrams, E.M.; Adlou, B.; Akdis, C.; Akdis, M.; Brough, H.A.; Chan, S.; Chatchatee, P.; Chinthrajah, R.S.; Cocco, R.R.; et al. Food Allergy across the Globe. J. Allergy Clin. Immunol. 2021, 148, 1347–1364. [Google Scholar] [CrossRef] [PubMed]
- Scheurer, S.; Van Ree, R.; Vieths, S. The Role of Lipid Transfer Proteins as Food and Pollen Allergens Outside the Mediterranean Area. Curr. Allergy Asthma Rep. 2021, 21, 7. [Google Scholar] [CrossRef]
- Missaoui, K.; Gonzalez-Klein, Z.; Pazos-Castro, D.; Hernandez-Ramirez, G.; Garrido-Arandia, M.; Brini, F.; Diaz-Perales, A.; Tome-Amat, J. Plant Non-Specific Lipid Transfer Proteins: An Overview. Plant Physiol. Biochem. 2022, 171, 115–127. [Google Scholar] [CrossRef]
- Tome-Amat, J.; Gonzalez-Klein, Z.; Pazos-Castro, D.; Resuela-Gonzalez, J.L.; Vilchez-Pinto, G.; Berreiros-Hortala, H.; Palacio-Garcia, L.; Fernandez-Bravo, S.; Esteban, V.; Diaz-Perales, A.; et al. Plant Lipid Transfer Proteins’ Ligand Enhances Allergic Sensitization to Non-related Proteins in Murine Models. Allergy 2024, 79, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Barber, D.; Diaz-Perales, A.; Escribese, M.M.; Kleine-Tebbe, J.; Matricardi, P.M.; Ollert, M.; Santos, A.F.; Sastre, J. Molecular Allergology and Its Impact in Specific Allergy Diagnosis and Therapy. Allergy 2021, 76, 3642–3658. [Google Scholar] [CrossRef]
- Pajno, G.B.; Fernandez-Rivas, M.; Arasi, S.; Roberts, G.; Akdis, C.A.; Alvaro-Lozano, M.; Beyer, K.; Bindslev-Jensen, C.; Burks, W.; Ebisawa, M.; et al. EAACI Guidelines on Allergen Immunotherapy: IgE-mediated Food Allergy. Allergy 2018, 73, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; Duschl, A.; Himly, M. Nanotechnology-Based Vaccines for Allergen-Specific Immunotherapy: Potentials and Challenges of Conventional and Novel Adjuvants under Research. Vaccines 2020, 8, 237. [Google Scholar] [CrossRef]
- Hughes, K.R.; Saunders, M.N.; Landers, J.J.; Janczak, K.W.; Turkistani, H.; Rad, L.M.; Miller, S.D.; Podojil, J.R.; Shea, L.D.; O’Konek, J.J. Masked Delivery of Allergen in Nanoparticles Safely Attenuates Anaphylactic Response in Murine Models of Peanut Allergy. Front. Allergy 2022, 3, 829605. [Google Scholar] [CrossRef]
- Sampath, V.; Sindher, S.B.; Alvarez Pinzon, A.M.; Nadeau, K.C. Can Food Allergy Be Cured? What Are the Future Prospects? Allergy 2020, 75, 1316–1326. [Google Scholar] [CrossRef]
- Bruton, K.; Koenig, J.F.E.; Phelps, A.; Jordana, M. Perturbations to Homeostasis in Experimental Models Revealed Innate Pathways Driving Food Allergy. Front. Immunol. 2020, 11, 603272. [Google Scholar] [CrossRef] [PubMed]
- Pazos-Castro, D.; Margain, C.; Gonzalez-Klein, Z.; Amores-Borge, M.; Yuste-Calvo, C.; Garrido-Arandia, M.; Zurita, L.; Esteban, V.; Tome-Amat, J.; Diaz-Perales, A.; et al. Suitability of Potyviral Recombinant Virus-like Particles Bearing a Complete Food Allergen for Immunotherapy Vaccines. Front. Immunol. 2022, 13, 986823. [Google Scholar] [CrossRef] [PubMed]
- Curin, M.; Khaitov, M.; Karaulov, A.; Namazova-Baranova, L.; Campana, R.; Garib, V.; Valenta, R. Next-Generation of Allergen-Specific Immunotherapies: Molecular Approaches. Curr. Allergy Asthma Rep. 2018, 18, 39. [Google Scholar] [CrossRef] [PubMed]
- Reguraman, N.; Hassani, A.; Philip, P.S.; Pich, D.; Hammerschmidt, W.; Khan, G. Assessing the Efficacy of VLP-Based Vaccine against Epstein-Barr Virus Using a Rabbit Model. Vaccines 2023, 11, 540. [Google Scholar] [CrossRef] [PubMed]
- Hemmati, F.; Hemmati-Dinarvand, M.; Karimzade, M.; Rutkowska, D.; Eskandari, M.H.; Khanizadeh, S.; Afsharifar, A. Plant-Derived VLP: A Worthy Platform to Produce Vaccine against SARS-CoV-2. Biotechnol. Lett. 2022, 44, 45–57. [Google Scholar] [CrossRef]
- Ikwuagwu, B.; Tullman-Ercek, D. Virus-like Particles for Drug Delivery: A Review of Methods and Applications. Curr. Opin. Biotechnol. 2022, 78, 102785. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, M.O.; Bachmann, M.F. Virus-like Particle Vaccinology, from Bench to Bedside. Cell. Mol. Immunol. 2022, 19, 993–1011. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhou, K.; Wang, Q. Tailoring the Self-Assembly Behaviors of Recombinant Tobacco Mosaic Virus by Rationally Introducing Covalent Bonding at the Protein–Protein Interface. Small 2016, 12, 4955–4959. [Google Scholar] [CrossRef]
- Akache, B.; Weeratna, R.; Deora, A.; Thorn, J.; Champion, B.; Merson, J.; Davis, H.; McCluskie, M. Anti-IgE Qb-VLP Conjugate Vaccine Self-Adjuvants through Activation of TLR7. Vaccines 2016, 4, 3. [Google Scholar] [CrossRef]
- Le, D.T.; Müller, K.M. In Vitro Assembly of Virus-Like Particles and Their Applications. Life 2021, 11, 334. [Google Scholar] [CrossRef]
- Chung, Y.H.; Cai, H.; Steinmetz, N.F. Viral Nanoparticles for Drug Delivery, Imaging, Immunotherapy, and Theranostic Applications. Adv. Drug Deliv. Rev. 2020, 156, 214–235. [Google Scholar] [CrossRef] [PubMed]
- Shahgolzari, M.; Pazhouhandeh, M.; Milani, M.; Yari Khosroushahi, A.; Fiering, S. Plant Viral Nanoparticles for Packaging and in Vivo Delivery of Bioactive Cargos. WIREs Nanomed. Nanobiotechnol. 2020, 12, e1629. [Google Scholar] [CrossRef]
- Jensen-Jarolim, E.; Bachmann, M.F.; Bonini, S.; Jacobsen, L.; Jutel, M.; Klimek, L.; Mahler, V.; Mösges, R.; Moingeon, P.; O’Hehir, R.E.; et al. State-of-the-art in Marketed Adjuvants and Formulations in Allergen Immunotherapy: A Position Paper of the European Academy of Allergy and Clinical Immunology (EAACI). Allergy 2020, 75, 746–760. [Google Scholar] [CrossRef] [PubMed]
- Nooraei, S.; Bahrulolum, H.; Hoseini, Z.S.; Katalani, C.; Hajizade, A.; Easton, A.J.; Ahmadian, G. Virus-like Particles: Preparation, Immunogenicity and Their Roles as Nanovaccines and Drug Nanocarriers. J. Nanobiotechnol. 2021, 19, 59. [Google Scholar] [CrossRef] [PubMed]
- Veneziano, R.; Moyer, T.J.; Stone, M.B.; Wamhoff, E.-C.; Read, B.J.; Mukherjee, S.; Shepherd, T.R.; Das, J.; Schief, W.R.; Irvine, D.J.; et al. Role of Nanoscale Antigen Organization on B-Cell Activation Probed Using DNA Origami. Nat. Nanotechnol. 2020, 15, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Zepeda-Cervantes, J.; Ramírez-Jarquín, J.O.; Vaca, L. Interaction Between Virus-Like Particles (VLPs) and Pattern Recognition Receptors (PRRs) From Dendritic Cells (DCs): Toward Better Engineering of VLPs. Front. Immunol. 2020, 11, 1100. [Google Scholar] [CrossRef]
- Zeltins, A.; West, J.; Zabel, F.; El Turabi, A.; Balke, I.; Haas, S.; Maudrich, M.; Storni, F.; Engeroff, P.; Jennings, G.T.; et al. Incorporation of Tetanus-Epitope into Virus-like Particles Achieves Vaccine Responses Even in Older Recipients in Models of Psoriasis, Alzheimer’s and Cat Allergy. npj Vaccines 2017, 2, 30. [Google Scholar] [CrossRef]
- Gonzalez-Castro, R.; Acero Galindo, G.; García Salcedo, Y.; Uribe Campero, L.; Vazquez Perez, V.; Carrillo-Tripp, M.; Gevorkian, G.; Gomez Lim, M.A. Plant-Based Chimeric HPV-Virus-like Particles Bearing Amyloid-β Epitopes Elicit Antibodies Able to Recognize Amyloid Plaques in APP-Tg Mouse and Alzheimer’s Disease Brains. Inflammopharmacology 2018, 26, 817–827. [Google Scholar] [CrossRef]
- Von Loga, I.S.; El-Turabi, A.; Jostins, L.; Miotla-Zarebska, J.; Mackay-Alderson, J.; Zeltins, A.; Parisi, I.; Bachmann, M.F.; Vincent, T.L. Active Immunisation Targeting Nerve Growth Factor Attenuates Chronic Pain Behaviour in Murine Osteoarthritis. Ann. Rheum. Dis. 2019, 78, 672–675. [Google Scholar] [CrossRef]
- Crossey, E.; Amar, M.J.A.; Sampson, M.; Peabody, J.; Schiller, J.T.; Chackerian, B.; Remaley, A.T. A Cholesterol-Lowering VLP Vaccine That Targets PCSK9. Vaccine 2015, 33, 5747–5755. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Rivera, O.A.; Shin, M.D.; Moreno-Gonzalez, M.A.; Pokorski, J.K.; Steinmetz, N.F. A Single-Dose Qβ VLP Vaccine against S100A9 Protein Reduces Atherosclerosis in a Preclinical Model. Adv. Ther. 2022, 5, 2200092. [Google Scholar] [CrossRef] [PubMed]
- Tomé-Amat, J.; Fleischer, L.; Parker, S.A.; Bardliving, C.L.; Batt, C.A. Secreted Production of Assembled Norovirus Virus-like Particles from Pichia Pastoris. Microb. Cell Fact. 2014, 13, 134. [Google Scholar] [CrossRef] [PubMed]
- Lizotte, P.H.; Wen, A.M.; Sheen, M.R.; Fields, J.; Rojanasopondist, P.; Steinmetz, N.F.; Fiering, S. In Situ Vaccination with Cowpea Mosaic Virus Nanoparticles Suppresses Metastatic Cancer. Nat. Nanotechnol. 2016, 11, 295–303. [Google Scholar] [CrossRef]
- Kim, K.R.; Lee, A.S.; Kim, S.M.; Heo, H.R.; Kim, C.S. Virus-like Nanoparticles as a Theranostic Platform for Cancer. Front. Bioeng. Biotechnol. 2023, 10, 1106767. [Google Scholar] [CrossRef] [PubMed]
- Pardi, N.; Weissman, D. Development of Vaccines and Antivirals for Combating Viral Pandemics. Nat. Biomed. Eng. 2020, 4, 1128–1133. [Google Scholar] [CrossRef]
- Naskalska, A.; Pyrć, K. Virus Like Particles as Immunogens and Universal Nanocarriers. Pol. J. Microbiol. 2015, 64, 3–13. [Google Scholar] [CrossRef]
- Anzaghe, M.; Schülke, S.; Scheurer, S. Virus-Like Particles as Carrier Systems to Enhance Immunomodulation in Allergen Immunotherapy. Curr. Allergy Asthma Rep. 2018, 18, 71. [Google Scholar] [CrossRef]
- Tariq, H.; Batool, S.; Asif, S.; Ali, M.; Abbasi, B.H. Virus-Like Particles: Revolutionary Platforms for Developing Vaccines Against Emerging Infectious Diseases. Front. Microbiol. 2022, 12, 790121. [Google Scholar] [CrossRef] [PubMed]
- Pitoiset, F.; Vazquez, T.; Bellier, B. Enveloped Virus-like Particle Platforms: Vaccines of the Future? Expert Rev. Vaccines 2015, 14, 913–915. [Google Scholar] [CrossRef][Green Version]
- Deng, F. Advances and Challenges in Enveloped Virus-like Particle (VLP)-Based Vaccines. J. Immunol. Sci. 2018, 2, 36–41. [Google Scholar] [CrossRef]
- Lua, L.H.L.; Connors, N.K.; Sainsbury, F.; Chuan, Y.P.; Wibowo, N.; Middelberg, A.P.J. Bioengineering Virus-like Particles as Vaccines. Biotechnol. Bioeng. 2014, 111, 425–440. [Google Scholar] [CrossRef] [PubMed]
- Pacios, L.F.; Sánchez, F.; Ponz, F. Intrinsic Disorder in the Dynamic Evolution of Structure, Stability, and Flexibility of Potyviral VLP Assemblies: A Computational Study. Int. J. Biol. Macromol. 2024, 254, 127798. [Google Scholar] [CrossRef]
- Rohovie, M.J.; Nagasawa, M.; Swartz, J.R. Virus-like Particles: Next-generation Nanoparticles for Targeted Therapeutic Delivery. Bioeng. Transla Med. 2017, 2, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, M.O.; Zha, L.; Cabral-Miranda, G.; Bachmann, M.F. Major Findings and Recent Advances in Virus–like Particle (VLP)-Based Vaccines. Semin. Immunol. 2017, 34, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Zhou, A.; Sun, X.; Sha, W.; Ai, K.; Pan, G.; Zhou, C.; Zhou, H.; Cong, H.; He, S. Immunogenicity of a Virus-Like-Particle Vaccine Containing Multiple Antigenic Epitopes of Toxoplasma Gondii Against Acute and Chronic Toxoplasmosis in Mice. Front. Immunol. 2019, 10, 592. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Banerjee, M.; Lua, L.H.; Rathore, A.S. Current Status and Future Challenges in Transitioning to Continuous Bioprocessing of Virus-like Particles. J. Chem. Technol. Biotechnol. 2022, 97, 2376–2385. [Google Scholar] [CrossRef]
- Charlton Hume, H.K.; Vidigal, J.; Carrondo, M.J.T.; Middelberg, A.P.J.; Roldão, A.; Lua, L.H.L. Synthetic Biology for Bioengineering Virus-like Particle Vaccines. Biotechnol. Bioeng. 2019, 116, 919–935. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, M.O.; Augusto, G.; Bachmann, M.F. The 3Ds in Virus-like Particle Based-vaccines: “Design, Delivery and Dynamics”. Immunol. Rev. 2020, 296, 155–168. [Google Scholar] [CrossRef]
- Syomin, B.V.; Ilyin, Y.V. Virus-Like Particles as an Instrument of Vaccine Production. Mol. Biol. 2019, 53, 323–334. [Google Scholar] [CrossRef]
- Vicente, T.; Roldão, A.; Peixoto, C.; Carrondo, M.J.T.; Alves, P.M. Large-Scale Production and Purification of VLP-Based Vaccines. J. Invertebr. Pathol. 2011, 107, S42–S48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xu, W.; Ma, X.; Sun, X.; Fan, J.; Wang, Y. Virus-like Particles as Antiviral Vaccine: Mechanism, Design, and Application. Biotechnol. Bioprocess Eng. 2023, 28, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Fuenmayor, J.; Gòdia, F.; Cervera, L. Production of Virus-like Particles for Vaccines. New Biotechnol. 2017, 39, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Wijewardhana, C.; Mann, J.F.S. Virus-Like Particle, Liposome, and Polymeric Particle-Based Vaccines against HIV-1. Front. Immunol. 2018, 9, 345. [Google Scholar] [CrossRef] [PubMed]
- Shirbaghaee, Z.; Bolhassani, A. Different Applications of Virus-like Particles in Biology and Medicine: Vaccination and Delivery Systems. Biopolymers 2016, 105, 113–132. [Google Scholar] [CrossRef] [PubMed]
- Masavuli, M.G.; Wijesundara, D.K.; Torresi, J.; Gowans, E.J.; Grubor-Bauk, B. Preclinical Development and Production of Virus-Like Particles As Vaccine Candidates for Hepatitis C. Front. Microbiol. 2017, 8, 2413. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, T.; Alves, A.; Lopes, A.; Carrondo, M.J.T.; Alves, P.M.; Cruz, P.E. Removal of Envelope Protein-free Retroviral Vectors by Anion-exchange Chromatography to Improve Product Quality. J. Sep. Sci. 2008, 31, 3509–3518. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.M.; Petiot, E.; Mullick, A.; Aucoin, M.G.; Henry, O.; Kamen, A.A. Critical Assessment of Influenza VLP Production in Sf9 and HEK293 Expression Systems. BMC Biotechnol. 2015, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Cervera, L.; Gòdia, F.; Tarrés-Freixas, F.; Aguilar-Gurrieri, C.; Carrillo, J.; Blanco, J.; Gutiérrez-Granados, S. Production of HIV-1-Based Virus-like Particles for Vaccination: Achievements and Limits. Appl. Microbiol. Biotechnol. 2019, 103, 7367–7384. [Google Scholar] [CrossRef]
- Zhao, D.; Sun, B.; Jiang, H.; Sun, S.; Kong, F.T.; Ma, Y.; Jiang, L.; Bai, L.; Chen, X.; Yang, P.; et al. Enterovirus71 Virus-like Particles Produced from Insect Cells and Purified by Multistep Chromatography Elicit Strong Humoral Immune Responses in Mice. J. Appl. Microbiol. 2015, 119, 1196–1205. [Google Scholar] [CrossRef] [PubMed]
- Thoms, F.; Jennings, G.T.; Maudrich, M.; Vogel, M.; Haas, S.; Zeltins, A.; Hofmann-Lehmann, R.; Riond, B.; Grossmann, J.; Hunziker, P.; et al. Immunization of Cats to Induce Neutralizing Antibodies against Fel d 1, the Major Feline Allergen in Human Subjects. J. Allergy Clin. Immunol. 2019, 144, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Soongrung, T.; Mongkorntanyatip, K.; Peepim, T.; Jitthamstaporn, S.; Pitakpolrat, P.; Kaewamatawong, T.; Janitzek, C.M.; Thrane, S.; Sander, A.F.; Jacquet, A. Virus-like Particles Displaying Major House Dust Mite Allergen Der p 2 for Prophylactic Allergen Immunotherapy. Allergy 2020, 75, 1232–1236. [Google Scholar] [CrossRef]
- Hou, L.; Wu, H.; Xu, L.; Yang, F. Expression and Self-Assembly of Virus-like Particles of Infectious Hypodermal and Hematopoietic Necrosis Virus in Escherichia coli. Arch. Virol. 2009, 154, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Fromentin, R.; Majeau, N.; Gagné, M.-E.L.; Boivin, A.; Duvignaud, J.-B.; Leclerc, D. A Method for in Vitro Assembly of Hepatitis C Virus Core Protein and for Screening of Inhibitors. Anal. Biochem. 2007, 366, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Storni, F.; Zeltins, A.; Balke, I.; Heath, M.D.; Kramer, M.F.; Skinner, M.A.; Zha, L.; Roesti, E.; Engeroff, P.; Muri, L.; et al. Vaccine against Peanut Allergy Based on Engineered Virus-like Particles Displaying Single Major Peanut Allergens. J. Allergy Clin. Immunol. 2020, 145, 1240–1253.e3. [Google Scholar] [CrossRef]
- Hirschberg, S.; Layton, G.T.; Harris, S.J.; Savage, N.; Dallman, M.J.; Lamb, J.R. CD4+ T Cells Induced by Virus-like Particles Expressing a Major T Cell Epitope down-Regulate IL-5 Production in an Ongoing Immune Response to Der p 1 Independently of IFN-γ Production. Int. Immunol. 1999, 11, 1927–1934. [Google Scholar] [CrossRef] [PubMed]
- Cimica, V.; Galarza, J.M. Adjuvant Formulations for Virus-like Particle (VLP) Based Vaccines. Clin. Immunol. 2017, 183, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Norkiene, M.; Stonyte, J.; Ziogiene, D.; Mazeike, E.; Sasnauskas, K.; Gedvilaite, A. Production of Recombinant VP1-Derived Virus-like Particles from Novel Human Polyomaviruses in Yeast. BMC Biotechnol. 2015, 15, 68. [Google Scholar] [CrossRef]
- Sari-Ak, D.; Bahrami, S.; Laska, M.J.; Drncova, P.; Fitzgerald, D.J.; Schaffitzel, C.; Garzoni, F.; Berger, I. High-Throughput Production of Influenza Virus-Like Particle (VLP) Array by Using VLP-FactoryTM, a MultiBac Baculoviral Genome Customized for Enveloped VLP Expression. In High-Throughput Protein Production and Purification; Vincentelli, R., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2019; Volume 2025, pp. 213–226. ISBN 978-1-4939-9623-0. [Google Scholar]
- Sequeira, D.P.; Correia, R.; Carrondo, M.J.T.; Roldão, A.; Teixeira, A.P.; Alves, P.M. Combining Stable Insect Cell Lines with Baculovirus-Mediated Expression for Multi-HA Influenza VLP Production. Vaccine 2018, 36, 3112–3123. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Carrion, R.; Ye, L.; Wen, Z.; Ro, Y.-T.; Brasky, K.; Ticer, A.E.; Schwegler, E.E.; Patterson, J.L.; Compans, R.W.; et al. Corrigendum to “Protection against Lethal Challenge by Ebola Virus-like Particles Produced in Insect Cells” [Virology 383 (2009) 12–21]. Virology 2010, 399, 186. [Google Scholar] [CrossRef]
- Lechmann, M. Hepatitis C Virus–like Particles Induce Virus-Specific Humoral and Cellular Immune Responses in Mice. Hepatology 2001, 34, 417–423. [Google Scholar] [CrossRef]
- Gomord, V.; Stordeur, V.; Fitchette, A.-C.; Fixman, E.D.; Tropper, G.; Garnier, L.; Desgagnes, R.; Viel, S.; Couillard, J.; Beauverger, G.; et al. Design, Production and Immunomodulatory Potency of a Novel Allergen Bioparticle. PLoS ONE 2020, 15, e0242867. [Google Scholar] [CrossRef]
- Pietersen, I.; Van Zyl, A.; Rybicki, E.; Hitzeroth, I. Novel Production of Bovine Papillomavirus Pseudovirions in Tobacco Plants. Pathogens 2020, 9, 996. [Google Scholar] [CrossRef]
- Ward, B.J.; Makarkov, A.; Séguin, A.; Pillet, S.; Trépanier, S.; Dhaliwall, J.; Libman, M.D.; Vesikari, T.; Landry, N. Efficacy, Immunogenicity, and Safety of a Plant-Derived, Quadrivalent, Virus-like Particle Influenza Vaccine in Adults (18–64 Years) and Older Adults (≥65 Years): Two Multicentre, Randomised Phase 3 Trials. Lancet 2020, 396, 1491–1503. [Google Scholar] [CrossRef] [PubMed]
- Gogesch, P.; Schülke, S.; Scheurer, S.; Mühlebach, M.D.; Waibler, Z. Modular MLV-VLPs Co-Displaying Ovalbumin Peptides and GM-CSF Effectively Induce Expansion of CD11b+ APC and Antigen-Specific T Cell Responses in Vitro. Mol. Immunol. 2018, 101, 19–28. [Google Scholar] [CrossRef]
- Buffin, S.; Peubez, I.; Barrière, F.; Nicolaï, M.-C.; Tapia, T.; Dhir, V.; Forma, E.; Sève, N.; Legastelois, I. Influenza A and B Virus-like Particles Produced in Mammalian Cells Are Highly Immunogenic and Induce Functional Antibodies. Vaccine 2019, 37, 6857–6867. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Yeh, Y.-C.; Yang, Y.-C.; Chou, C.; Liu, M.-T.; Wu, H.-S.; Chan, J.-T.; Hsiao, P.-W. Mammalian Expression of Virus-Like Particles for Advanced Mimicry of Authentic Influenza Virus. PLoS ONE 2010, 5, e9784. [Google Scholar] [CrossRef]
- Panasiuk, M.; Zimmer, K.; Czarnota, A.; Grzyb, K.; Narajczyk, M.; Peszyńska-Sularz, G.; Żołędowska, S.; Nidzworski, D.; Hovhannisyan, L.; Gromadzka, B. Immunization with Leishmania Tarentolae-Derived Norovirus Virus-like Particles Elicits High Humoral Response and Stimulates the Production of Neutralizing Antibodies. Microb. Cell Fact. 2021, 20, 186. [Google Scholar] [CrossRef] [PubMed]
- Foerster, J.; Molęda, A. Virus-Like Particle-Mediated Vaccination against Interleukin-13 May Harbour General Anti-Allergic Potential beyond Atopic Dermatitis. Viruses 2020, 12, 438. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, B.; Douglas, T. Development of Virus-like Particles for Diagnostic and Prophylactic Biomedical Applications. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2015, 7, 722–735. [Google Scholar] [CrossRef]
- Boisgérault, F.; Morón, G.; Leclerc, C. Virus-like Particles: A New Family of Delivery Systems. Expert Rev. Vaccines 2002, 1, 101–109. [Google Scholar] [CrossRef]
- Pattinson, D.J.; Apte, S.H.; Wibowo, N.; Rivera-Hernandez, T.; Groves, P.L.; Middelberg, A.P.J.; Doolan, D.L. Chimeric Virus-Like Particles and Capsomeres Induce Similar CD8+ T Cell Responses but Differ in Capacity to Induce CD4+ T Cell Responses and Antibody Responses. Front. Immunol. 2020, 11, 564627. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, M.F.; El-Turabi, A.; Fettelschoss-Gabriel, A.; Vogel, M. The Prospects of an Active Vaccine Against Asthma Targeting IL-5. Front. Microbiol. 2018, 9, 2522. [Google Scholar] [CrossRef] [PubMed]
- Klimek, L.; Kündig, T.; Kramer, M.F.; Guethoff, S.; Jensen-Jarolim, E.; Schmidt-Weber, C.B.; Palomares, O.; Mohsen, M.O.; Jakob, T.; Bachmann, M. Virus-like Particles (VLP) in Prophylaxis and Immunotherapy of Allergic Diseases. Allergo J. Int. 2018, 27, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Alvandi, N.; Rajabnejad, M.; Taghvaei, Z.; Esfandiari, N. New Generation of Viral Nanoparticles for Targeted Drug Delivery in Cancer Therapy. J. Drug Target. 2022, 30, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Fan, D.; Cao, Y.; Cao, M.; Wang, Y.; Cao, Y.; Gong, T. Nanomedicine in Cancer Therapy. Signal Transduct. Target. Ther. 2023, 8, 293. [Google Scholar] [CrossRef]
- Greiner, V.J.; Ronzon, F.; Larquet, E.; Desbat, B.; Estèves, C.; Bonvin, J.; Gréco, F.; Manin, C.; Klymchenko, A.S.; Mély, Y. The Structure of HBsAg Particles Is Not Modified upon Their Adsorption on Aluminium Hydroxide Gel. Vaccine 2012, 30, 5240–5245. [Google Scholar] [CrossRef] [PubMed]
- Moradi Vahdat, M.; Hemmati, F.; Ghorbani, A.; Rutkowska, D.; Afsharifar, A.; Eskandari, M.H.; Rezaei, N.; Niazi, A. Hepatitis B Core-Based Virus-like Particles: A Platform for Vaccine Development in Plants. Biotechnol. Rep. 2021, 29, e00605. [Google Scholar] [CrossRef] [PubMed]
- Venters, C.; Graham, W.; Cassidy, W. Recombivax-HB: Perspectives Past, Present and Future. Expert Rev. Vaccines 2004, 3, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Joe, C.C.D.; Chatterjee, S.; Lovrecz, G.; Adams, T.E.; Thaysen-Andersen, M.; Walsh, R.; Locarnini, S.A.; Smooker, P.; Netter, H.J. Glycoengineered Hepatitis B Virus-like Particles with Enhanced Immunogenicity. Vaccine 2020, 38, 3892–3901. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Mitoma, F.; Popovic, V.; Spaans, J.N. Assessment of Immunogenicity and Safety across Two Manufacturing Lots of a 3-Antigen Hepatitis B Vaccine, Sci-B-Vac®, Compared with Engerix-B® in Healthy Asian Adults: A Phase 3 Randomized Clinical Trial. Vaccine 2021, 39, 3892–3899. [Google Scholar] [CrossRef]
- Shi, L.; Sings, H.L.; Bryan, J.T.; Wang, B.; Wang, Y.; Mach, H.; Kosinski, M.; Washabaugh, M.W.; Sitrin, R.; Barr, E. GARDASIL®: Prophylactic Human Papillomavirus Vaccine Development—From Bench Top to Bed-Side. Clin. Pharmacol. Ther. 2007, 81, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Zhai, L.; Tumban, E. Gardasil-9: A Global Survey of Projected Efficacy. Antivir. Res. 2016, 130, 101–109. [Google Scholar] [CrossRef]
- Schwarz, T.F. Clinical Update of the AS04-Adjuvanted Human Papillomavirus-16/18 Cervical Cancer Vaccine, Cervarix®. Adv. Ther. 2009, 26, 983–998. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wei, M.; Pan, H.; Lin, Z.; Wang, K.; Weng, Z.; Zhu, Y.; Xin, L.; Zhang, J.; Li, S.; et al. Robust Manufacturing and Comprehensive Characterization of Recombinant Hepatitis E Virus-like Particles in Hecolin®. Vaccine 2014, 32, 4039–4050. [Google Scholar] [CrossRef] [PubMed]
- Laurens, M.B. RTS,S/AS01 Vaccine (MosquirixTM): An Overview. Hum. Vaccines Immunother. 2020, 16, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Pechsrichuang, P.; Namwongnao, S.; Jacquet, A. Bioengineering of Virus-like Particles for the Prevention or Treatment of Allergic Diseases. Allergy Asthma Immunol. Res. 2021, 13, 23. [Google Scholar] [CrossRef]
- Donaldson, B.; Lateef, Z.; Walker, G.F.; Young, S.L.; Ward, V.K. Virus-like Particle Vaccines: Immunology and Formulation for Clinical Translation. Expert Rev. Vaccines 2018, 17, 833–849. [Google Scholar] [CrossRef]
- Engeroff, P.; Caviezel, F.; Storni, F.; Thoms, F.; Vogel, M.; Bachmann, M.F. Allergens Displayed on Virus-like Particles Are Highly Immunogenic but Fail to Activate Human Mast Cells. Allergy 2018, 73, 341–349. [Google Scholar] [CrossRef]
- Kratzer, B.; Hofer, S.; Zabel, M.; Pickl, W.F. All the Small Things: How Virus-like Particles and Liposomes Modulate Allergic Immune Responses. Eur. J. Immunol. 2020, 50, 17–32. [Google Scholar] [CrossRef]
- Schmitz, N.; Dietmeier, K.; Bauer, M.; Maudrich, M.; Utzinger, S.; Muntwiler, S.; Saudan, P.; Bachmann, M.F. Displaying Fel D1 on Virus-like Particles Prevents Reactogenicity despite Greatly Enhanced Immunogenicity: A Novel Therapy for Cat Allergy. J. Exp. Med. 2009, 206, 1941–1955. [Google Scholar] [CrossRef]
- Sobczak, J.M.; Krenger, P.S.; Storni, F.; Mohsen, M.O.; Balke, I.; Reseviča, G.; Heath, M.D.; Carreno Velazquez, T.L.; Kramer, M.F.; Scott, C.J.W.; et al. The next Generation Virus-like Particle Platform for the Treatment of Peanut Allergy. Allergy 2023, 78, 1980–1996. [Google Scholar] [CrossRef]
- Kratzer, B.; Köhler, C.; Hofer, S.; Smole, U.; Trapin, D.; Iturri, J.; Pum, D.; Kienzl, P.; Elbe-Bürger, A.; Gattinger, P.; et al. Prevention of Allergy by Virus-like Nanoparticles (VNP) Delivering Shielded Versions of Major Allergens in a Humanized Murine Allergy Model. Allergy 2019, 74, 246–260. [Google Scholar] [CrossRef] [PubMed]
- Thoms, F.; Haas, S.; Erhart, A.; Nett, C.S.; Rüfenacht, S.; Graf, N.; Strods, A.; Patil, G.; Leenadevi, T.; Fontaine, M.C.; et al. Immunization of Cats against Fel d 1 Results in Reduced Allergic Symptoms of Owners. Viruses 2020, 12, 288. [Google Scholar] [CrossRef]
- Sani, M.Z.; Bargahi, A.; Momenzadeh, N.; Dehghani, P.; Moghadam, M.V.; Maleki, S.J.; Nabipour, I.; Shirkani, A.; Akhtari, J.; Hesamizadeh, K.; et al. Genetically Engineered Fusion of Allergen and Viral-like Particle Induces a More Effective Allergen-Specific Immune Response than a Combination of Them. Appl. Microbiol. Biotechnol. 2021, 105, 77–91. [Google Scholar] [CrossRef]
- Khaitov, M.; Shilovskiy, I.; Valenta, R.; Weber, M.; Korneev, A.; Tulaeva, I.; Gattinger, P.; Van Hage, M.; Hofer, G.; Konradsen, J.R.; et al. Recombinant PreS-fusion Protein Vaccine for Birch Pollen and Apple Allergy. Allergy 2024, 79, 1001–1017. [Google Scholar] [CrossRef]
- Ma, Y.; Halayko, A.J.; Basu, S.; Guan, Q.; Weiss, C.R.; Ma, A.G.; HayGlass, K.T.; Becker, A.B.; Warrington, R.J.; Peng, Z. Sustained Suppression of IL-13 by a Vaccine Attenuates Airway Inflammation and Remodeling in Mice. Am. J. Respir. Cell Mol. Biol. 2013, 48, 540–549. [Google Scholar] [CrossRef]
- Fettelschoss-Gabriel, A.; Fettelschoss, V.; Thoms, F.; Giese, C.; Daniel, M.; Olomski, F.; Kamarachev, J.; Birkmann, K.; Bühler, M.; Kummer, M.; et al. Treating Insect-Bite Hypersensitivity in Horses with Active Vaccination against IL-5. J. Allergy Clin. Immunol. 2018, 142, 1194–1205.e3. [Google Scholar] [CrossRef]
- Fettelschoss-Gabriel, A.; Fettelschoss, V.; Olomski, F.; Birkmann, K.; Thoms, F.; Bühler, M.; Kummer, M.; Zeltins, A.; Kündig, T.M.; Bachmann, M.F. Active Vaccination against Interleukin-5 as Long-term Treatment for Insect-bite Hypersensitivity in Horses. Allergy 2019, 74, 572–582. [Google Scholar] [CrossRef] [PubMed]
- Jonsdottir, S.; Fettelschoss, V.; Olomski, F.; Talker, S.C.; Mirkovitch, J.; Rhiner, T.; Birkmann, K.; Thoms, F.; Wagner, B.; Bachmann, M.F.; et al. Safety Profile of a Virus-Like Particle-Based Vaccine Targeting Self-Protein Interleukin-5 in Horses. Vaccines 2020, 8, 213. [Google Scholar] [CrossRef] [PubMed]
- Gharailoo, Z.; Plattner, K.; Augusto, G.; Engeroff, P.; Vogel, M.; Bachmann, M.F. Generation of a Virus-like Particles Based Vaccine against IgE. Allergy 2024, 16090. [Google Scholar] [CrossRef]
- Shamji, M.; Layhadi, J.; Turner, P.; Patel, N.; Parkin, R.; Oluwayi, K.; Rusyn, O.; Skinner, M.; Heath, M.; Kramer, M.; et al. Virus Like Particle (VLP) Based Peanut Allergen Immunotherapy Candidate Display A Decreased Activation And Histamine Release From CRTH2+ Basophils: A Proof of Concept Study. J. Allergy Clin. Immunol. 2022, 149, AB37. [Google Scholar] [CrossRef]
- Eckl-Dorna, J.; Weber, M.; Stanek, V.; Linhart, B.; Ristl, R.; Waltl, E.E.; Villazala-Merino, S.; Hummel, A.; Focke-Tejkl, M.; Froeschel, R.; et al. Two Years of Treatment with the Recombinant Grass Pollen Allergy Vaccine BM32 Induces a Continuously Increasing Allergen-Specific IgG4 Response. EBioMedicine 2019, 50, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Gerlich, W.H. “Dual Use”: The Anti-Allergy Vaccine BM32 and Its HBV Carrier Protein. EBioMedicine 2020, 60, 102998. [Google Scholar] [CrossRef] [PubMed]
- Asayama, K.; Kobayashi, T.; D’Alessandro-Gabazza, C.N.; Toda, M.; Yasuma, T.; Fujimoto, H.; Okano, T.; Saiki, H.; Takeshita, A.; Fujiwara, K.; et al. Protein S Protects against Allergic Bronchial Asthma by Modulating Th1/Th2 Balance. Allergy 2020, 75, 2267–2278. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Luo, X.; Zhang, Q.; He, X.; Zhang, Z.; Wang, X. Bifidobacterium Infantis Relieves Allergic Asthma in Mice by Regulating Th1/Th2. Med. Sci. Monit. 2020, 26, e920583-1. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Douglas, T. Bioinspired Approaches to Self-Assembly of Virus-like Particles: From Molecules to Materials. Acc. Chem. Res. 2022, 55, 1349–1359. [Google Scholar] [CrossRef] [PubMed]
- Klimek, L.; Bachmann, M.F.; Senti, G.; Kündig, T.M. Immunotherapy of Type-1 Allergies with Virus-like Particles and CpG-Motifs. Expert Rev. Clin. Immunol. 2014, 10, 1059–1067. [Google Scholar] [CrossRef]
- Krieg, A.M. Therapeutic Potential of Toll-like Receptor 9 Activation. Nat. Rev. Drug Discov. 2006, 5, 471–484. [Google Scholar] [CrossRef] [PubMed]
- Durham, S.R.; Shamji, M.H. Allergen Immunotherapy: Past, Present and Future. Nat. Rev. Immunol. 2023, 23, 317–328. [Google Scholar] [CrossRef]
- Senti, G.; Johansen, P.; Haug, S.; Bull, C.; Gottschaller, C.; Müller, P.; Pfister, T.; Maurer, P.; Bachmann, M.F.; Graf, N.; et al. Use of A-type CpG Oligodeoxynucleotides as an Adjuvant in Allergen-specific Immunotherapy in Humans: A Phase I/IIa Clinical Trial. Clin. Exp. Allergy 2009, 39, 562–570. [Google Scholar] [CrossRef]
- Klimek, L.; Willers, J.; Hammann-Haenni, A.; Pfaar, O.; Stocker, H.; Mueller, P.; Renner, W.A.; Bachmann, M.F. Assessment of Clinical Efficacy of CYT003-QbG10 in Patients with Allergic Rhinoconjunctivitis: A Phase IIb Study. Clin. Exp. Allergy 2011, 41, 1305–1312. [Google Scholar] [CrossRef]
- Beeh, K.-M.; Kanniess, F.; Wagner, F.; Schilder, C.; Naudts, I.; Hammann-Haenni, A.; Willers, J.; Stocker, H.; Mueller, P.; Bachmann, M.F.; et al. The Novel TLR-9 Agonist QbG10 Shows Clinical Efficacy in Persistent Allergic Asthma. J. Allergy Clin. Immunol. 2013, 131, 866–874. [Google Scholar] [CrossRef]
- Casale, T.B.; Cole, J.; Beck, E.; Vogelmeier, C.F.; Willers, J.; Lassen, C.; Hammann-Haenni, A.; Trokan, L.; Saudan, P.; Wechsler, M.E. CYT 003, a TLR 9 Agonist, in Persistent Allergic Asthma—A Randomized Placebo-controlled Phase 2b Study. Allergy 2015, 70, 1160–1168. [Google Scholar] [CrossRef] [PubMed]
- Chun, P.I.F.; Lehman, H. Current and Future Monoclonal Antibodies in the Treatment of Atopic Dermatitis. Clin. Rev. Allerg. Immunol. 2020, 59, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Orengo, J.M.; Radin, A.R.; Kamat, V.; Badithe, A.; Ben, L.H.; Bennett, B.L.; Zhong, S.; Birchard, D.; Limnander, A.; Rafique, A.; et al. Treating Cat Allergy with Monoclonal IgG Antibodies That Bind Allergen and Prevent IgE Engagement. Nat. Commun. 2018, 9, 1421. [Google Scholar] [CrossRef]
- Suber, J.; Zhang, Y.; Ye, P.; Guo, R.; Burks, A.W.; Kulis, M.D.; Smith, S.A.; Iweala, O.I. Novel Peanut-Specific Human IgE Monoclonal Antibodies Enable Screens for Inhibitors of the Effector Phase in Food Allergy. Front. Immunol. 2022, 13, 974374. [Google Scholar] [CrossRef]
- Ma, Y.; Hayglass, K.T.; Becker, A.B.; Halayko, A.J.; Basu, S.; Simons, F.E.R.; Peng, Z. Novel Cytokine Peptide-based Vaccines: An Interleukin-4 Vaccine Suppresses Airway Allergic Responses in Mice. Allergy 2007, 62, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Sonderegger, I.; Lipowsky, G.; Jennings, G.T.; Schmitz, N.; Landi, M.; Kopf, M.; Bachmann, M.F. Combined Vaccination against IL-5 and Eotaxin Blocks Eosinophilia in Mice. Vaccine 2010, 28, 3192–3200. [Google Scholar] [CrossRef] [PubMed]
- Long, Q.; Huang, W.; Yao, Y.; Yang, X.; Sun, W.; Jin, X.; Li, Y.; Chu, X.; Liu, C.; Peng, Z.; et al. Virus-like Particles Presenting Interleukin-33 Molecules: Immunization Characteristics and Potentials of Blocking IL-33/ST2 Pathway in Allergic Airway Inflammation. Hum. Vaccines Immunother. 2014, 10, 2303–2311. [Google Scholar] [CrossRef]
- Ryman, J.T.; Meibohm, B. Pharmacokinetics of Monoclonal Antibodies. CPT Pharmacom Syst. Pharma 2017, 6, 576–588. [Google Scholar] [CrossRef] [PubMed]
- Kueng, H.J.; Leb, V.M.; Haiderer, D.; Raposo, G.; Thery, C.; Derdak, S.V.; Schmetterer, K.G.; Neunkirchner, A.; Sillaber, C.; Seed, B.; et al. General Strategy for Decoration of Enveloped Viruses with Functionally Active Lipid-Modified Cytokines. J. Virol. 2007, 81, 8666–8676. [Google Scholar] [CrossRef]
- Ahmar Rauf, M.; Nisar, M.; Abdelhady, H.; Gavande, N.; Iyer, A.K. Nanomedicine Approaches to Reduce Cytokine Storms in Severe Infections. Drug Discov. Today 2022, 27, 103355. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Liu, Q.; Wang, Q.; Rector, E.; Ma, Y.; Warrington, R. Novel IgE Peptide-based Vaccine Prevents the Increase of IgE and Down-regulates Elevated IgE in Rodents. Clin. Exp. Allergy 2007, 37, 1040–1048. [Google Scholar] [CrossRef]
- Bachmann, M.F.; Jennings, G.T. Therapeutic Vaccines for Chronic Diseases: Successes and Technical Challenges. Philos. Trans. R. Soc. B 2011, 366, 2815–2822. [Google Scholar] [CrossRef]
- An, M.; Raguram, A.; Du, S.W.; Banskota, S.; Davis, J.R.; Newby, G.A.; Chen, P.Z.; Palczewski, K.; Liu, D.R. Engineered Virus-like Particles for Transient Delivery of Prime Editor Ribonucleoprotein Complexes in Vivo. Nat. Biotechnol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Zeltins, A. Construction and Characterization of Virus-Like Particles: A Review. Mol. Biotechnol. 2013, 53, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Kundig, T.; Senti, G.; Schnetzler, G.; Wolf, C.; Prinzvavricka, B.; Fulurija, A.; Hennecke, F.; Sladko, K.; Jennings, G.; Bachmann, M. Der p 1 Peptide on Virus-like Particles Is Safe and Highly Immunogenic in Healthy Adults. J. Allergy Clin. Immunol. 2006, 117, 1470–1476. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-J.; Kim, G.; Bae, J.-H.; Song, J.-J.; Kim, H.-S. A pH-Responsive Virus-Like Particle as a Protein Cage for a Targeted Delivery. Adv. Healthc. Mater. 2024, 13, e2302656. [Google Scholar] [CrossRef]
- Zehetner, L.; Széliová, D.; Kraus, B.; Graninger, M.; Zanghellini, J.; Hernandez Bort, J.A. Optimizing VLP Production in Gene Therapy: Opportunities and Challenges for in Silico Modeling. Biotechnol. J. 2023, 18, 2200636. [Google Scholar] [CrossRef]
- Mobini, S.; Chizari, M.; Mafakher, L.; Rismani, E.; Rismani, E. Computational Design of a Novel VLP-Based Vaccine for Hepatitis B Virus. Front. Immunol. 2020, 11, 2074. [Google Scholar] [CrossRef]
- López-Sagaseta, J.; Malito, E.; Rappuoli, R.; Bottomley, M.J. Self-Assembling Protein Nanoparticles in the Design of Vaccines. Comput. Struct. Biotechnol. J. 2016, 14, 58–68. [Google Scholar] [CrossRef]
- Grgacic, E.V.L.; Anderson, D.A. Virus-like Particles: Passport to Immune Recognition. Methods 2006, 40, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, M.F.; Jennings, G.T. Vaccine Delivery: A Matter of Size, Geometry, Kinetics and Molecular Patterns. Nat. Rev. Immunol. 2010, 10, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Sabree, S.A.; Voigt, A.P.; Blackwell, S.E.; Vishwakarma, A.; Chimenti, M.S.; Salem, A.K.; Weiner, G.J. Direct and Indirect Immune Effects of CMP-001, a Virus-like Particle Containing a TLR9 Agonist. J. Immunother. Cancer 2021, 9, e002484. [Google Scholar] [CrossRef] [PubMed]
- Lemke-Miltner, C.D.; Blackwell, S.E.; Yin, C.; Krug, A.E.; Morris, A.J.; Krieg, A.M.; Weiner, G.J. Antibody Opsonization of a TLR9 Agonist–Containing Virus-like Particle Enhances In Situ Immunization. J. Immunol. 2020, 204, 1386–1394. [Google Scholar] [CrossRef]
- Lin, Y.-J.; Zimmermann, J.; Schülke, S. Novel Adjuvants in Allergen-Specific Immunotherapy: Where Do We Stand? Front. Immunol. 2024, 15, 1348305. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berreiros-Hortala, H.; Vilchez-Pinto, G.; Diaz-Perales, A.; Garrido-Arandia, M.; Tome-Amat, J. Virus-like Particles as Vaccines for Allergen-Specific Therapy: An Overview of Current Developments. Int. J. Mol. Sci. 2024, 25, 7429. https://doi.org/10.3390/ijms25137429
Berreiros-Hortala H, Vilchez-Pinto G, Diaz-Perales A, Garrido-Arandia M, Tome-Amat J. Virus-like Particles as Vaccines for Allergen-Specific Therapy: An Overview of Current Developments. International Journal of Molecular Sciences. 2024; 25(13):7429. https://doi.org/10.3390/ijms25137429
Chicago/Turabian StyleBerreiros-Hortala, Helena, Gonzalo Vilchez-Pinto, Araceli Diaz-Perales, Maria Garrido-Arandia, and Jaime Tome-Amat. 2024. "Virus-like Particles as Vaccines for Allergen-Specific Therapy: An Overview of Current Developments" International Journal of Molecular Sciences 25, no. 13: 7429. https://doi.org/10.3390/ijms25137429
APA StyleBerreiros-Hortala, H., Vilchez-Pinto, G., Diaz-Perales, A., Garrido-Arandia, M., & Tome-Amat, J. (2024). Virus-like Particles as Vaccines for Allergen-Specific Therapy: An Overview of Current Developments. International Journal of Molecular Sciences, 25(13), 7429. https://doi.org/10.3390/ijms25137429







