The Advantage of Targeted Next-Generation Sequencing over qPCR in Testing for Druggable EGFR Variants in Non-Small-Cell Lung Cancer
Abstract
:1. Introduction
2. Results
2.1. Overall Performance of qPCR and NGS Assays
2.1.1. Cobas EGFR Mutation Test v2
2.1.2. TruSight Tumor 15 Assay
2.2. The NGS Detection Limit in DNA Reference Material
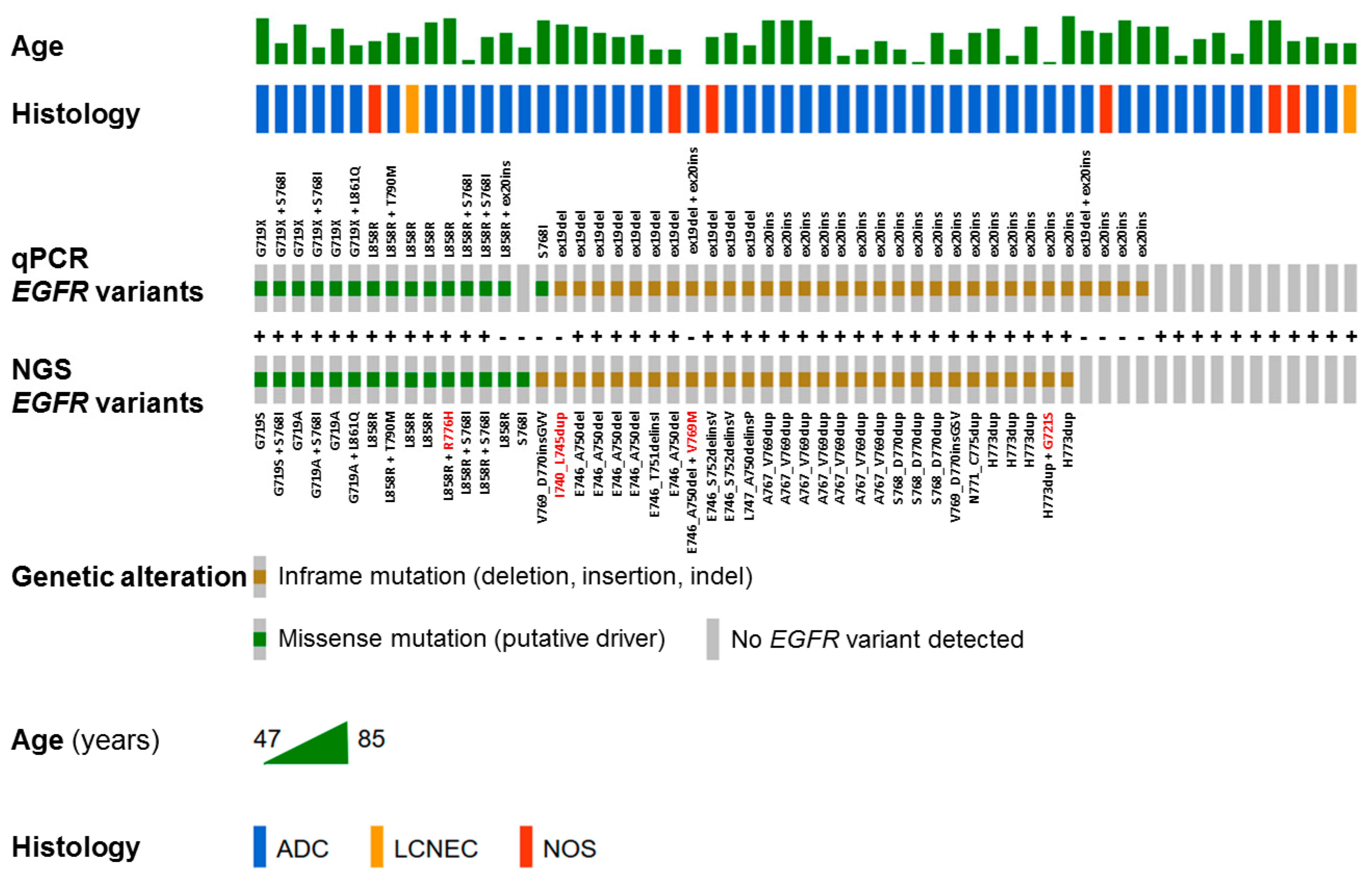
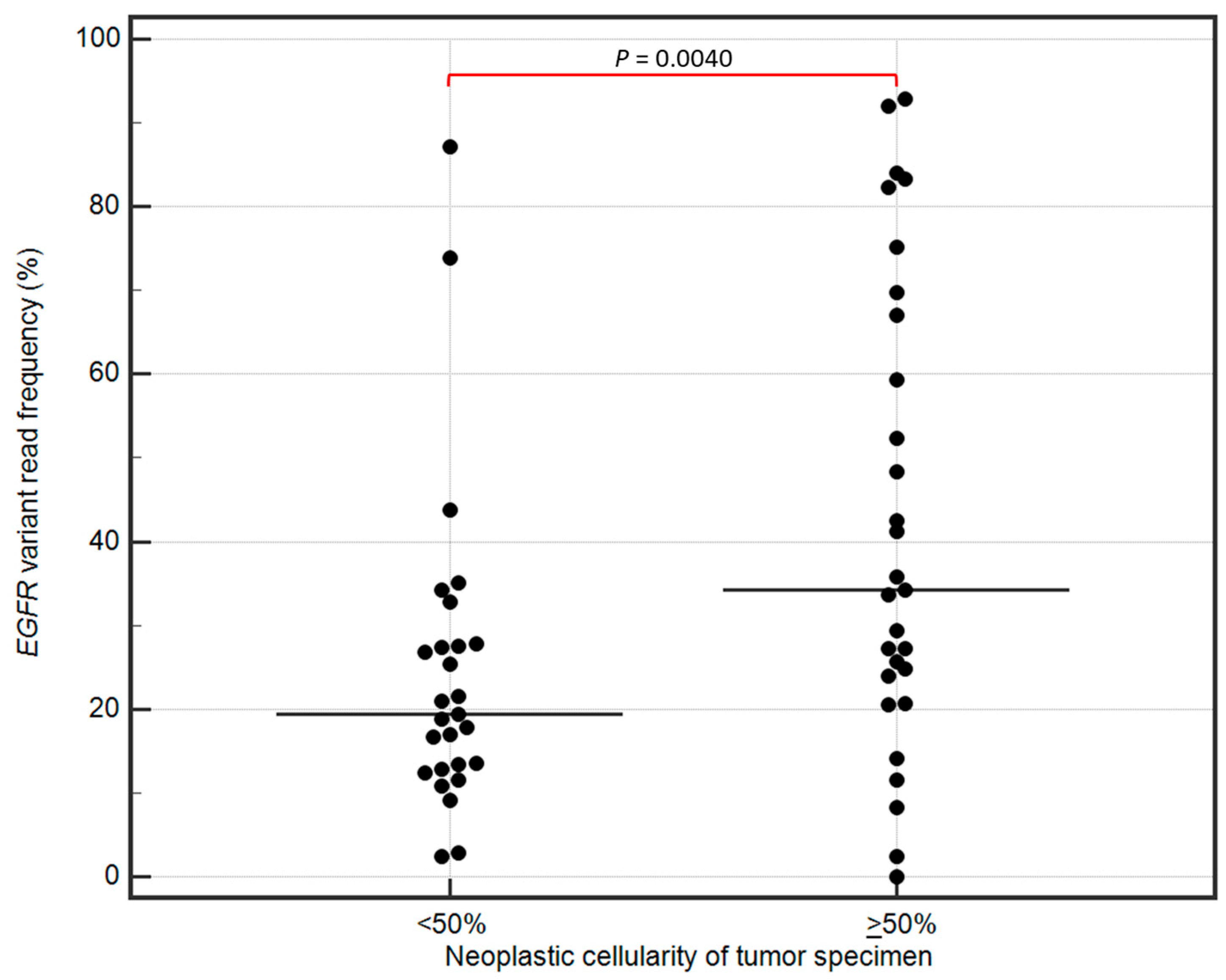
2.3. The Detection of EGFR Variants in Clinical Samples by qPCR and NGS Assays
2.4. Other Gene Variants Detected in Clinical Samples by NGS
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Clinical Tumor Specimens
4.3. Lung Cancer Cell Lines and In Vitro Culture Conditions
4.4. DNA Extraction
4.5. Biosynthetic DNA Reference Material
4.6. Biological DNA Reference Material
4.7. EGFR Mutation Analysis in Clinical Samples by Multiplex qPCR
4.8. NGS Analysis of Gene Variants in Cell Lines and Clinical Samples
4.9. Bioinformatics and Computational Analysis of NGS Output Data
4.10. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, Y.L.; Yuan, J.Q.; Wang, K.F.; Fu, X.H.; Han, X.R.; Threapleton, D.; Yang, Z.Y.; Mao, C.; Tang, J.L. The prevalence of EGFR mutation in patients with non-small cell lung cancer: A systematic review and meta-analysis. Oncotarget 2016, 7, 78985–78993. [Google Scholar] [CrossRef] [PubMed]
- Midha, A.; Dearden, S.; McCormack, R. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: A systematic review and global map by ethnicity (mutMapII). Am. J. Cancer. Res. 2015, 5, 2892–2911. [Google Scholar] [PubMed]
- Melosky, B.; Kambartel, K.; Hantschel, M.; Bennetts, M.; Nickens, D.J.; Brinkmann, J.; Kayser, A.; Moran, M.; Cappuzzo, F. Worldwide Prevalence of Epidermal Growth Factor Receptor Mutations in Non-Small Cell Lung Cancer: A Meta-Analysis. Mol. Diagn. Ther. 2022, 26, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Yeh, P.; Chen, H.; Andrews, J.; Naser, R.; Pao, W.; Horn, L. DNA-Mutation Inventory to Refine and Enhance Cancer Treatment (DIRECT): A catalog of clinically relevant cancer mutations to enable genome-directed anticancer therapy. Clin. Cancer. Res. 2013, 19, 1894–1901. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.; Garassino, M.C.; Mok, T.; Mitsudomi, T. Treatment strategies and outcomes for patients with EGFR-mutant non-small cell lung cancer resistant to EGFR tyrosine kinase inhibitors: Focus on novel therapies. Lung Cancer 2022, 170, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Olivier, T.; Prasad, V. Amivantamab and Mobocertinib in Exon 20 insertions EGFR Mutant Lung Cancer, Challenge To The Current Guidelines. Transl. Oncol. 2022, 23, 101475. [Google Scholar] [CrossRef] [PubMed]
- Khaddour, K.; Jonna, S.; Deneka, A.; Patel, J.D.; Abazeed, M.E.; Golemis, E.; Borghaei, H.; Boumber, Y. Targeting the Epidermal Growth Factor Receptor in EGFR-Mutated Lung Cancer: Current and Emerging Therapies. Cancers 2021, 13, 3164. [Google Scholar] [CrossRef] [PubMed]
- Kazdal, D.; Hofman, V.; Christopoulos, P.; Ilie, M.; Stenzinger, A.; Hofman, P. Fusion-positive non-small cell lung carcinoma: Biological principles, clinical practice, and diagnostic implications. Genes Chromosomes Cancer 2022, 61, 244–260. [Google Scholar] [CrossRef] [PubMed]
- Khoo, C.; Rogers, T.M.; Fellowes, A.; Bell, A.; Fox, S. Molecular methods for somatic mutation testing in lung adenocarcinoma: EGFR and beyond. Transl. Lung Cancer Res. 2015, 4, 126–141. [Google Scholar] [CrossRef]
- Villaruz, L.C.; Socinski, M.A.; Weiss, J. Guidance for clinicians and patients with non-small cell lung cancer in the time of precision medicine. Front. Oncol. 2023, 13, 1124167. [Google Scholar] [CrossRef]
- Garinet, S.; Lupo, A.; Denize, T.; Loyaux, R.; Timsit, S.; Gazeau, B.; Fabre, E.; Maaradji, Z.; Gibault, L.; Giroux-Leprieur, E.; et al. Successive next-generation sequencing strategy for optimal fusion gene detection in non-small-cell lung cancer in clinical practice. Pathology 2024, 56, 702–709. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.M.; Hackett, J.M.; Plestina, S. Unlocking Access to Broad Molecular Profiling: Benefits, Barriers, and Policy Solutions. Public Health Genom. 2021, 25, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Best, M.C.; Bartley, N.; Napier, C.E.; Fisher, A.; Ballinger, M.L.; Thomas, D.M.; Goldstein, D.; Tucker, K.; Biesecker, B.B.; Butow, P. Return of comprehensive tumour genomic profiling results to advanced cancer patients: A qualitative study. Support. Care Cancer 2022, 30, 8201–8210. [Google Scholar] [CrossRef] [PubMed]
- Rao, W.; Guo, L.; Ling, Y.; Dong, L.; Li, W.; Ying, J.; Li, W. Developing an effective quality evaluation strategy of next-generation sequencing for accurate detecting non-small cell lung cancer samples with variable characteristics: A real-world clinical practice. J. Cancer Res. Clin. Oncol. 2023, 149, 4889–4897. [Google Scholar] [CrossRef]
- Malapelle, U.; Sirera, R.; Jantus-Lewintre, E.; Reclusa, P.; Calabuig-Farinas, S.; Blasco, A.; Pisapia, P.; Rolfo, C.; Camps, C. Profile of the Roche cobas(R) EGFR mutation test v2 for non-small cell lung cancer. Expert Rev. Mol. Diagn. 2017, 17, 209–215. [Google Scholar] [CrossRef]
- US Food & Drug Administration—Cobas EGFR Mutation Test V2. 2016. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150047c.pdf (accessed on 15 May 2024).
- Cobas EGFR Mutation Test–P120019. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P120019 (accessed on 15 May 2024).
- Cobas EGFR Mutation Test V2–P150047. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P150047 (accessed on 15 May 2024).
- Lim, S.M.; Syn, N.L.; Cho, B.C.; Soo, R.A. Acquired resistance to EGFR targeted therapy in non-small cell lung cancer: Mechanisms and therapeutic strategies. Cancer Treat. Rev. 2018, 65, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kwapisz, D. The first liquid biopsy test approved. Is it a new era of mutation testing for non-small cell lung cancer? Ann. Transl. Med. 2017, 5, 46. [Google Scholar] [CrossRef]
- Cobas EGFR Mutation Test V2. 2016. Available online: http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm504540.htm. (accessed on 15 May 2024).
- Lopez-Rios, F.; Angulo, B.; Gomez, B.; Mair, D.; Martinez, R.; Conde, E.; Shieh, F.; Tsai, J.; Vaks, J.; Current, R.; et al. Comparison of molecular testing methods for the detection of EGFR mutations in formalin-fixed paraffin-embedded tissue specimens of non-small cell lung cancer. J. Clin. Pathol. 2013, 66, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Evrard, S.M.; Taranchon-Clermont, E.; Rouquette, I.; Murray, S.; Dintner, S.; Nam-Apostolopoulos, Y.C.; Bellosillo, B.; Varela-Rodriguez, M.; Nadal, E.; Wiedorn, K.H.; et al. Multicenter Evaluation of the Fully Automated PCR-Based Idylla EGFR Mutation Assay on Formalin-Fixed, Paraffin-Embedded Tissue of Human Lung Cancer. J. Mol. Diagn. 2019, 21, 1010–1024. [Google Scholar] [CrossRef]
- Uchibori, K.; Takano, N.; Manabe, R.; Tsugitomi, R.; Ogusu, S.; Tozuka, T.; Sakamoto, H.; Yoshida, H.; Amino, Y.; Ariyasu, R.; et al. Clinical influence of switching companion diagnostic tests for EGFR-TKs from Therascreen to Cobas v2. Thorac. Cancer 2021, 12, 906–913. [Google Scholar] [CrossRef]
- Thress, K.S.; Brant, R.; Carr, T.H.; Dearden, S.; Jenkins, S.; Brown, H.; Hammett, T.; Cantarini, M.; Barrett, J.C. EGFR mutation detection in ctDNA from NSCLC patient plasma: A cross-platform comparison of leading technologies to support the clinical development of AZD9291. Lung Cancer 2015, 90, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Hagiwara, K.; Han, B.; Tjulandin, S.; Grohe, C.; Yokoi, T.; Morabito, A.; Novello, S.; Arriola, E.; Molinier, O.; et al. ctDNA Determination of EGFR Mutation Status in European and Japanese Patients with Advanced NSCLC: The ASSESS Study. J. Thorac. Oncol. 2016, 11, 1682–1689. [Google Scholar] [CrossRef] [PubMed]
- Romero, A.; Jantus-Lewintre, E.; Garcia-Pelaez, B.; Royuela, A.; Insa, A.; Cruz, P.; Collazo, A.; Perez Altozano, J.; Vidal, O.J.; Diz, P.; et al. Comprehensive cross-platform comparison of methods for non-invasive EGFR mutation testing: Results of the RING observational trial. Mol. Oncol. 2021, 15, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Szpechcinski, A.; Bryl, M.; Wojcik, P.; Czyzewicz, G.; Wojda, E.; Rudzinski, P.; Duk, K.; Moes-Sosnowska, J.; Maszkowska-Kopij, K.; Langfort, R.; et al. Detection of EGFR mutations in liquid biopsy samples using allele-specific quantitative PCR: A comparative real-world evaluation of two popular diagnostic systems. Adv. Med. Sci. 2021, 66, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Galffy, G.; Morocz, E.; Korompay, R.; Hecz, R.; Bujdoso, R.; Puskas, R.; Lovas, T.; Gaspar, E.; Yahya, K.; Kiraly, P.; et al. Targeted therapeutic options in early and metastatic NSCLC-overview. Pathol. Oncol. Res. 2024, 30, 1611715. [Google Scholar] [CrossRef]
- Hess, L.M.; Krein, P.M.; Haldane, D.; Han, Y.; Sireci, A.N. Biomarker Testing for Patients With Advanced/Metastatic Nonsquamous NSCLC in the United States of America, 2015 to 2021. JTO Clin. Res. Rep. 2022, 3, 100336. [Google Scholar] [CrossRef]
- Liam, C.K.; Mallawathantri, S.; Fong, K.M. Is tissue still the issue in detecting molecular alterations in lung cancer? Respirology 2020, 25, 933–943. [Google Scholar] [CrossRef] [PubMed]
- Schmid, K.; Oehl, N.; Wrba, F.; Pirker, R.; Pirker, C.; Filipits, M. EGFR/KRAS/BRAF mutations in primary lung adenocarcinomas and corresponding locoregional lymph node metastases. Clin. Cancer Res. 2009, 15, 4554–4560. [Google Scholar] [CrossRef] [PubMed]
- Vaeyens, F.; Hetzel, J.-P.; Mernberger, M.; Eggermont, C.; Olsen, C.; Maes, K.; Vlaeminck, J.; Hes, F.; Pichler, M.; Giron, P.; et al. Variant-Specific Landscape of Mutual Exclusivity Among BRAF, EGFR, and KRAS Oncogenes in Human Cancer. medRxiv 2023. [Google Scholar] [CrossRef]
- O’Donnell, P.; Ferguson, J.; Shyu, J.; Current, R.; Rehage, T.; Tsai, J.; Christensen, M.; Tran, H.B.; Chien, S.S.; Shieh, F.; et al. Analytic performance studies and clinical reproducibility of a real-time PCR assay for the detection of epidermal growth factor receptor gene mutations in formalin-fixed paraffin-embedded tissue specimens of non-small cell lung cancer. BMC Cancer 2013, 13, 210. [Google Scholar] [CrossRef]
- Suda, K.; Sakai, K.; Ohira, T.; Chikugo, T.; Satou, T.; Matsubayashi, J.; Nagao, T.; Ikeda, N.; Tsutani, Y.; Mitsudomi, T.; et al. Performance of Ultra-Rapid Idylla EGFR Mutation Test in Non-Small-Cell Lung Cancer and Its Potential at Clinical Molecular Screening. Cancers 2023, 15, 2648. [Google Scholar] [CrossRef]
- Kanaoka, K.; Tamiya, A.; Inagaki, Y.; Taniguchi, Y.; Nakao, K.; Takeda, M.; Matsuda, Y.; Okishio, K.; Shimizu, S. Possible False Results With cobas ((R)) EGFR Mutation Test v2 and Oncomine Dx Target Test for EGFR Mutation. Anticancer Res. 2023, 43, 2771–2776. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, N.I.; Cagle, P.T.; Beasley, M.B.; Chitale, D.A.; Dacic, S.; Giaccone, G.; Jenkins, R.B.; Kwiatkowski, D.J.; Saldivar, J.S.; Squire, J.; et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: Guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J. Thorac. Oncol. 2013, 8, 823–859. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, P.; Sheath, K.L.; Tin, S.T.; Khwaounjoo, P.; Aye, P.S.; Li, A.; Laking, G.R.; Kingston, N.J.; Lewis, C.A.; Mark Elwood, J.; et al. Lung cancer mutation testing: A clinical retesting study of agreement between a real-time PCR and a mass spectrometry test. Oncotarget 2017, 8, 101437–101451. [Google Scholar] [CrossRef] [PubMed]
- Park, I.H.; Son, D.S.; Choi, Y.L.; Choi, J.H.; Park, J.E.; Jeon, Y.J.; Cho, M.; Kim, H.K.; Choi, Y.S.; Shim, Y.M.; et al. Clinical Validation of the Unparalleled Sensitivity of the Novel Allele-Discriminating Priming System Technology-Based EGFR Mutation Assay in Patients with Operable Non-Small Cell Lung Cancer. Cancer Res. Treat. 2024, 56, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Kimura, H.; Ohira, T.; Uchida, O.; Matsubayashi, J.; Shimizu, S.; Nagao, T.; Ikeda, N.; Nishio, K. Analytical performance of the cobas EGFR mutation assay for Japanese non-small-cell lung cancer. Lung Cancer 2014, 83, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.I.; Ho, H.L.; Yeh, Y.C.; Chiu, C.H.; Chou, T.Y. Epidermal growth factor receptor mutations in non-small cell lung cancer undetected by high-sensitivity allele-specific real-time polymerase chain reaction-based assays. J. Chin. Med. Assoc. 2020, 83, 345–349. [Google Scholar] [CrossRef]
- Stoler, N.; Nekrutenko, A. Sequencing error profiles of Illumina sequencing instruments. NAR Genom Bioinform 2021, 3, lqab019. [Google Scholar] [CrossRef] [PubMed]
- OLGEN Coverage Limit Calculator. Available online: http://app.olgen.cz/clc/ (accessed on 15 May 2024).
- Petrackova, A.; Vasinek, M.; Sedlarikova, L.; Dyskova, T.; Schneiderova, P.; Novosad, T.; Papajik, T.; Kriegova, E. Standardization of Sequencing Coverage Depth in NGS: Recommendation for Detection of Clonal and Subclonal Mutations in Cancer Diagnostics. Front. Oncol. 2019, 9, 851. [Google Scholar] [CrossRef]
- Deans, Z.C.; Costa, J.L.; Cree, I.; Dequeker, E.; Edsjo, A.; Henderson, S.; Hummel, M.; Ligtenberg, M.J.; Loddo, M.; Machado, J.C.; et al. Integration of next-generation sequencing in clinical diagnostic molecular pathology laboratories for analysis of solid tumours; an expert opinion on behalf of IQN Path ASBL. Virchows Arch. 2017, 470, 5–20. [Google Scholar] [CrossRef]
- D’Haene, N.; Le Mercier, M.; De Neve, N.; Blanchard, O.; Delaunoy, M.; El Housni, H.; Dessars, B.; Heimann, P.; Remmelink, M.; Demetter, P.; et al. Clinical Validation of Targeted Next Generation Sequencing for Colon and Lung Cancers. PLoS ONE 2015, 10, e0138245. [Google Scholar] [CrossRef]
- Jennings, L.J.; Arcila, M.E.; Corless, C.; Kamel-Reid, S.; Lubin, I.M.; Pfeifer, J.; Temple-Smolkin, R.L.; Voelkerding, K.V.; Nikiforova, M.N. Guidelines for Validation of Next-Generation Sequencing-Based Oncology Panels: A Joint Consensus Recommendation of the Association for Molecular Pathology and College of American Pathologists. J. Mol. Diagn. 2017, 19, 341–365. [Google Scholar] [CrossRef]
- Lazzari, C.; Bulotta, A.; Cangi, M.G.; Bucci, G.; Pecciarini, L.; Bonfiglio, S.; Lorusso, V.; Ippati, S.; Arrigoni, G.; Grassini, G.; et al. Next Generation Sequencing in Non-Small Cell Lung Cancer: Pitfalls and Opportunities. Diagnostics 2020, 10, 1092. [Google Scholar] [CrossRef]
- Huang, L.T.; Zhang, S.L.; Han, C.B.; Ma, J.T. Impact of EGFR exon 19 deletion subtypes on clinical outcomes in EGFR-TKI-Treated advanced non-small-cell lung cancer. Lung Cancer 2022, 166, 9–16. [Google Scholar] [CrossRef]
- Xu, C.W.; Lei, L.; Wang, W.X.; Lin, L.; Zhu, Y.C.; Wang, H.; Miao, L.Y.; Wang, L.P.; Zhuang, W.; Fang, M.Y.; et al. Molecular Characteristics and Clinical Outcomes of EGFR Exon 19 C-Helix Deletion in Non-Small Cell Lung Cancer and Response to EGFR TKIs. Transl. Oncol. 2020, 13, 100791. [Google Scholar] [CrossRef]
- Boscolo Bielo, L.; Trapani, D.; Repetto, M.; Crimini, E.; Valenza, C.; Belli, C.; Criscitiello, C.; Marra, A.; Subbiah, V.; Curigliano, G. Variant allele frequency: A decision-making tool in precision oncology? Trends Cancer 2023, 9, 1058–1068. [Google Scholar] [CrossRef]
- Friedlaender, A.; Tsantoulis, P.; Chevallier, M.; De Vito, C.; Addeo, A. The Impact of Variant Allele Frequency in EGFR Mutated NSCLC Patients on Targeted Therapy. Front. Oncol. 2021, 11, 644472. [Google Scholar] [CrossRef]
- Gieszer, B.; Megyesfalvi, Z.; Dulai, V.; Papay, J.; Kovalszky, I.; Timar, J.; Fillinger, J.; Harko, T.; Pipek, O.; Teglasi, V.; et al. EGFR variant allele frequency predicts EGFR-TKI efficacy in lung adenocarcinoma: A multicenter study. Transl. Lung Cancer Res. 2021, 10, 662–674. [Google Scholar] [CrossRef]
- Katakura, S.; Murakami, S.; Kanako, S.; Ryota, U.; Tetsuro, K.; Terufumi, K.; Tomoyuki, Y.; Haruhiro, S. MO29-1 The relationship between EGFR variant allele frequency and efficacy of osimertinib in EGFR mutation-positive NSCLC. Ann. Oncol. 2022, 33, S500. [Google Scholar] [CrossRef]
- Moes-Sosnowska, J.; Szpechcinski, A.; Chorostowska-Wynimko, J. Clinical significance of TP53 alterations in advanced NSCLC patients treated with EGFR, ALK and ROS1 tyrosine kinase inhibitors: An update. Tumour. Biol. 2024, 46, S309–S325. [Google Scholar] [CrossRef]
- Hou, H.; Qin, K.; Liang, Y.; Zhang, C.; Liu, D.; Jiang, H.; Liu, K.; Zhu, J.; Lv, H.; Li, T.; et al. Concurrent TP53 mutations predict poor outcomes of EGFR-TKI treatments in Chinese patients with advanced NSCLC. Cancer Manag. Res. 2019, 11, 5665–5675. [Google Scholar] [CrossRef]
- Roeper, J.; Christopoulos, P.; Falk, M.; Heukamp, L.C.; Tiemann, M.; Stenzinger, A.; Thomas, M.; Griesinger, F. TP53 co-mutations as an independent prognostic factor in 2nd and further line therapy-EGFR mutated non-small cell lung cancer IV patients treated with osimertinib. Transl. Lung Cancer Res. 2022, 11, 4–13. [Google Scholar] [CrossRef]
- Zhou, X.; Cai, L.; Liu, J.; Hua, X.; Zhang, Y.; Zhao, H.; Wang, B.; Li, B.; Gai, P. Analyzing EGFR mutations and their association with clinicopathological characteristics and prognosis of patients with lung adenocarcinoma. Oncol. Lett. 2018, 16, 362–370. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, H.; Yang, S.; Yang, Y.; Wu, Y.; He, Z.; Ma, S.; Mo, Y.; Chen, H.; Wang, Q.; et al. EGFR mutation types and abundance were associated with the overall survival of advanced lung adenocarcinoma patients receiving first-line tyrosine kinase inhibitors. J. Thorac. Dis. 2022, 14, 2254–2267. [Google Scholar] [CrossRef]
- WHO Classification of Tumours Editorial Board. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart; International Agency for Research on Cancer (IARC): Lyons, France, 2015. [Google Scholar]
- WHO Classification of Tumours Editorial Board. Thoracic Tumours, 5th ed.; International Agency for Research on Cancer: Lyon, France, 2021. [Google Scholar]
- Brierley, J.; Gospodarowicz, M.; Wittekind, C. TNM Classification of Malignant Tumours; Wiley: Chichester, UK, 2017. [Google Scholar]
- Hendriks, L.E.; Kerr, K.M.; Menis, J.; Mok, T.S.; Nestle, U.; Passaro, A.; Peters, S.; Planchard, D.; Smit, E.F.; Solomon, B.J.; et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2023, 34, 339–357. [Google Scholar] [CrossRef]
- Bronner, I.F.; Quail, M.A.; Turner, D.J.; Swerdlow, H. Improved Protocols for Illumina Sequencing. Curr. Protoc. Hum. Genet. 2014, 79, 18.2.1–18.2.42. [Google Scholar] [CrossRef]
- Froyen, G.; Le Mercier, M.; Lierman, E.; Vandepoele, K.; Nollet, F.; Boone, E.; Van der Meulen, J.; Jacobs, K.; Lambin, S.; Vander Borght, S.; et al. Standardization of Somatic Variant Classifications in Solid and Haematological Tumours by a Two-Level Approach of Biological and Clinical Classes: An Initiative of the Belgian ComPerMed Expert Panel. Cancers 2019, 11, 2030. [Google Scholar] [CrossRef]
- Hébrant, A.; Froyen, G.; Maes, B.; Salgado, R.; Le Mercier, M.; D’Haene, N.; De Keersmaecker, S.; Claes, K.; Van der Meulen, J.; Aftimos, P.; et al. The Belgian next generation sequencing guidelines for haematological and solid tumours. Belg. J. Med. Oncol. 2017, 11, 56–67. [Google Scholar]
- Landrum, M.J.; Lee, J.M.; Riley, G.R.; Jang, W.; Rubinstein, W.S.; Church, D.M.; Maglott, D.R. ClinVar: Public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 2014, 42, D980–D985. [Google Scholar] [CrossRef]
- Kopanos, C.; Tsiolkas, V.; Kouris, A.; Chapple, C.E.; Albarca Aguilera, M.; Meyer, R.; Massouras, A. VarSome: The human genomic variant search engine. Bioinformatics 2019, 35, 1978–1980. [Google Scholar] [CrossRef]
- den Dunnen, J.T.; Dalgleish, R.; Maglott, D.R.; Hart, R.K.; Greenblatt, M.S.; McGowan-Jordan, J.; Roux, A.F.; Smith, T.; Antonarakis, S.E.; Taschner, P.E. HGVS Recommendations for the Description of Sequence Variants: 2016 Update. Hum. Mutat. 2016, 37, 564–569. [Google Scholar] [CrossRef]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B.E.; Sumer, S.O.; Aksoy, B.A.; Jacobsen, A.; Byrne, C.J.; Heuer, M.L.; Larsson, E.; et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012, 2, 401–404. [Google Scholar] [CrossRef]
- Gao, J.; Aksoy, B.A.; Dogrusoz, U.; Dresdner, G.; Gross, B.; Sumer, S.O.; Sun, Y.; Jacobsen, A.; Sinha, R.; Larsson, E.; et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 2013, 6, pl1. [Google Scholar] [CrossRef]
- Simundic, A.M. Measures of Diagnostic Accuracy: Basic Definitions. EJIFCC 2009, 19, 203–211. [Google Scholar]
- Ranganathan, P.; Pramesh, C.S.; Aggarwal, R. Common pitfalls in statistical analysis: Measures of agreement. Perspect. Clin. Res. 2017, 8, 187–191. [Google Scholar] [CrossRef]
- Teixeira, M.R.; Oliveira, J.; Borralho, P.; Fernandes, M.G.O.; Almodovar, T.; Fernandes, I.; Macedo, D.; Ferreira, A.; Barroso, A.; Teixeira, E.; et al. Portuguese Consensus Recommendations for Next-Generation Sequencing of Lung Cancer, Rare Tumors, and Cancers of Unknown Primary Origin in Clinical Practice. Acta Med. Port. 2022, 35, 677–690. [Google Scholar] [CrossRef]
- Malapelle, U.; Donne, A.D.; Pagni, F.; Fraggetta, F.; Rocco, E.G.; Pasello, G.; Perrone, G.; Pepe, F.; Vatrano, S.; Pignata, S.; et al. Standardized and simplified reporting of next-generation sequencing results in advanced non-small-cell lung cancer: Practical indications from an Italian multidisciplinary group. Crit. Rev. Oncol. Hematol. 2024, 193, 104217. [Google Scholar] [CrossRef]
- Isla, D.; Lozano, M.D.; Paz-Ares, L.; Salas, C.; de Castro, J.; Conde, E.; Felip, E.; Gomez-Roman, J.; Garrido, P.; Belen Enguita, A. New update to the guidelines on testing predictive biomarkers in non-small-cell lung cancer: A National Consensus of the Spanish Society of Pathology and the Spanish Society of Medical Oncology. Rev. Esp. Patol. 2023, 56, 97–112. [Google Scholar] [CrossRef]
- Hatanaka, Y.; Kuwata, T.; Morii, E.; Kanai, Y.; Ichikawa, H.; Kubo, T.; Hatanaka, K.C.; Sakai, K.; Nishio, K.; Fujii, S.; et al. The Japanese Society of Pathology Practical Guidelines on the handling of pathological tissue samples for cancer genomic medicine. Pathol. Int. 2021, 71, 725–740. [Google Scholar] [CrossRef]
- Chang, S.; Shim, H.S.; Kim, T.J.; Choi, Y.L.; Kim, W.S.; Shin, D.H.; Kim, L.; Park, H.S.; Lee, G.K.; Lee, C.H.; et al. Molecular biomarker testing for non-small cell lung cancer: Consensus statement of the Korean Cardiopulmonary Pathology Study Group. J. Pathol. Transl. Med. 2021, 55, 181–191. [Google Scholar] [CrossRef]
- Mosele, M.F.; Westphalen, C.B.; Stenzinger, A.; Barlesi, F.; Bayle, A.; Bieche, I.; Bonastre, J.; Castro, E.; Dienstmann, R.; Kramer, A.; et al. Recommendations for the use of next-generation sequencing (NGS) for patients with advanced cancer in 2024: A report from the ESMO Precision Medicine Working Group. Ann. Oncol. 2024, 35, 588–606. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Coldren, C.; Karunamurthy, A.; Kip, N.S.; Klee, E.W.; Lincoln, S.E.; Leon, A.; Pullambhatla, M.; Temple-Smolkin, R.L.; Voelkerding, K.V.; et al. Standards and Guidelines for Validating Next-Generation Sequencing Bioinformatics Pipelines: A Joint Recommendation of the Association for Molecular Pathology and the College of American Pathologists. J. Mol. Diagn. 2018, 20, 4–27. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, N.I.; Cagle, P.T.; Aisner, D.L.; Arcila, M.E.; Beasley, M.B.; Bernicker, E.H.; Colasacco, C.; Dacic, S.; Hirsch, F.R.; Kerr, K.; et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. Arch. Pathol. Lab. Med. 2018, 142, 321–346. [Google Scholar] [CrossRef]
| Reference DNA Material | NGS TST15 Results | ||||||
|---|---|---|---|---|---|---|---|
| Gene | HGVSc | HGVSp | COSMIC ID | Average Allele Frequency | Detection Status [Yes/No] | Total Read Depth * | Variant Read Frequency * |
| Biosynthetic DNA reference material (Seraseq) | |||||||
| EGFR | c.2236_2250del | p.(Glu746_Ala750del) | COSM6225 | 3.5% | Yes | 1283 | 3.50% |
| c.2310_2311insGGT | p.(Asp770_Asn771insGly) | COSM12378 | 3.3% | Yes | 5320 | 2.28% | |
| c.2369C > T | p.(Thr790Met) | COSM6240 | 3.3% | Yes | 5325 | 2.26% | |
| c.2573T > G | p.(Leu858Arg) | COSM6224 | 7.3% | Yes | 468 | 2.56% | |
| Biological DNA reference material (NSCLC cell lines) | |||||||
| EGFR | c.2236_2250del | p.(Glu746_Ala750del) | COSM6225 | 10% | Yes | 1719 | 14.54% |
| 5% | Yes | 1665 | 5.35% | ||||
| 2.5% | Yes | 1508 | 4.91% | ||||
| 1% | Yes | 1535 | 2.41% | ||||
| EGFR | c.2369C > T | p.(Thr790Met) | COSM6240 | 10% | Yes | 10,925 | 15.13% |
| 5% | Yes | 9955 | 7.47% | ||||
| 2.5% | Yes | 8250 | 4.73% | ||||
| 1% | Yes | 9990 | 1.4% | ||||
| EGFR | c.2573T > G | p.(Leu858Arg) | COSM6224 | 10% | Yes | 440 | 16.82% |
| 5% | Yes | 510 | 5.1% | ||||
| 2.5% | Yes | 568 | 2.46% | ||||
| 1% | Yes | 502 | 3.19% | ||||
| Sample No. | Cobas qPCR Result | NGS Result (HGVSp) | Explanation of Discrepancy | EGFR-TKI Administered |
|---|---|---|---|---|
| 7 | ex19del | p.(Ile740_Lys745dup) | Rare exon 19 insertion erroneously interpreted as deletion by cobas due to mismatch in probe binding site. Sensitizing EGFR mutation. | osimertinib |
| 14 | ex19del | p.(Glu746_Ala750del) | Concordant. | gefitinib |
| ex20ins | n/d | False-positive result in cobas analysis. Variant EGFR c.2305G > A p.(Val769Met) detected in NGS analysis is possible cause of mismatch at position 2305 falsely interpreted as ex20ins by cobas. Repeated cobas analysis of new FFPET section returned no ex20ins. | ||
| 18 | ex19del | n/d | Both results false-positive in cobas analysis. Repeated cobas analysis of new FFPET section returned no ex19del and no ex20ins. | No |
| ex20ins | n/d | |||
| 19 | n/d | p.(Ser768Ile) | Discordant results. No tumor tissue available to repeat test. | No |
| 24 | ex20ins | n/d | False-positive result in cobas analysis. No tumor tissue available to repeat cobas analysis. In NGS analysis BRAF p.(Val600Glu) present (mutually exclusive with EGFR mutations). | No |
| 32 | S768I | p.(Val769_Asp770insGlyValVal) | Discordant results. No tumor tissue available to repeat test. The proximity of ex20ins to the S768I may be a possible cause of mismatch at position 768. | No * |
| 39 | ex20ins | n/d | False-positive result in cobas analysis. No tumor tissue available to repeat test. | No |
| 40 | ex20ins | n/d | False-positive result in cobas analysis. No tumor tissue available to repeat test. KRAS p.(Gly12Cys) present and mutually exclusive with EGFR mutations. | No ** |
| 48 | L858R | p.(Leu858Arg) | Concordant. | osimertinib |
| ex20ins | n/d | False-positive result in cobas analysis. Repeated cobas analysis of new FFPET section returned no ex20ins. |
| Characteristics | n (%) | |
|---|---|---|
| NSCLC patients | 59 (100%) | |
| Median age (range), years | 68 (47–85) | |
| Sex | ||
| Female | 37/59 (63%) | |
| Male | 22/59 (37%) | |
| Histology (WHO) | ||
| ADC | 51/59 (86.5%) | |
| LCNEC | 2/59 (3.5%) | |
| NOS | 6/59 (10%) | |
| Stage IIIb–IV (TNM) | 59/59 (100%) | |
| EGFR mutation status | ||
| No mutation detected | 15/59 (25.5%) | |
| Exon 18 p.(Gly719Ala/Cys/Ser) | 6/59 (10%) | |
| Exon 19 deletion | 10/59 (17%) | |
| Exon 20 insertion | 18/59 (30.5%) | |
| Exon 20 p.(Thr790Met) | 1/59 (1.5%) | |
| Exon 21 p.(Leu858Arg) | 8/59 (13.5%) | |
| Other | 7/59 (12%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szpechcinski, A.; Moes-Sosnowska, J.; Skronska, P.; Lechowicz, U.; Pelc, M.; Szolkowska, M.; Rudzinski, P.; Wojda, E.; Maszkowska-Kopij, K.; Langfort, R.; et al. The Advantage of Targeted Next-Generation Sequencing over qPCR in Testing for Druggable EGFR Variants in Non-Small-Cell Lung Cancer. Int. J. Mol. Sci. 2024, 25, 7908. https://doi.org/10.3390/ijms25147908
Szpechcinski A, Moes-Sosnowska J, Skronska P, Lechowicz U, Pelc M, Szolkowska M, Rudzinski P, Wojda E, Maszkowska-Kopij K, Langfort R, et al. The Advantage of Targeted Next-Generation Sequencing over qPCR in Testing for Druggable EGFR Variants in Non-Small-Cell Lung Cancer. International Journal of Molecular Sciences. 2024; 25(14):7908. https://doi.org/10.3390/ijms25147908
Chicago/Turabian StyleSzpechcinski, Adam, Joanna Moes-Sosnowska, Paulina Skronska, Urszula Lechowicz, Magdalena Pelc, Malgorzata Szolkowska, Piotr Rudzinski, Emil Wojda, Krystyna Maszkowska-Kopij, Renata Langfort, and et al. 2024. "The Advantage of Targeted Next-Generation Sequencing over qPCR in Testing for Druggable EGFR Variants in Non-Small-Cell Lung Cancer" International Journal of Molecular Sciences 25, no. 14: 7908. https://doi.org/10.3390/ijms25147908
APA StyleSzpechcinski, A., Moes-Sosnowska, J., Skronska, P., Lechowicz, U., Pelc, M., Szolkowska, M., Rudzinski, P., Wojda, E., Maszkowska-Kopij, K., Langfort, R., Orlowski, T., Sliwinski, P., Polaczek, M., & Chorostowska-Wynimko, J. (2024). The Advantage of Targeted Next-Generation Sequencing over qPCR in Testing for Druggable EGFR Variants in Non-Small-Cell Lung Cancer. International Journal of Molecular Sciences, 25(14), 7908. https://doi.org/10.3390/ijms25147908








