Immunohistochemistry Screening of Different Tyrosine Kinase Receptors in Canine Solid Tumors—Part I: Proposal of a Receptor Panel to Predict Therapies
Abstract
1. Introduction
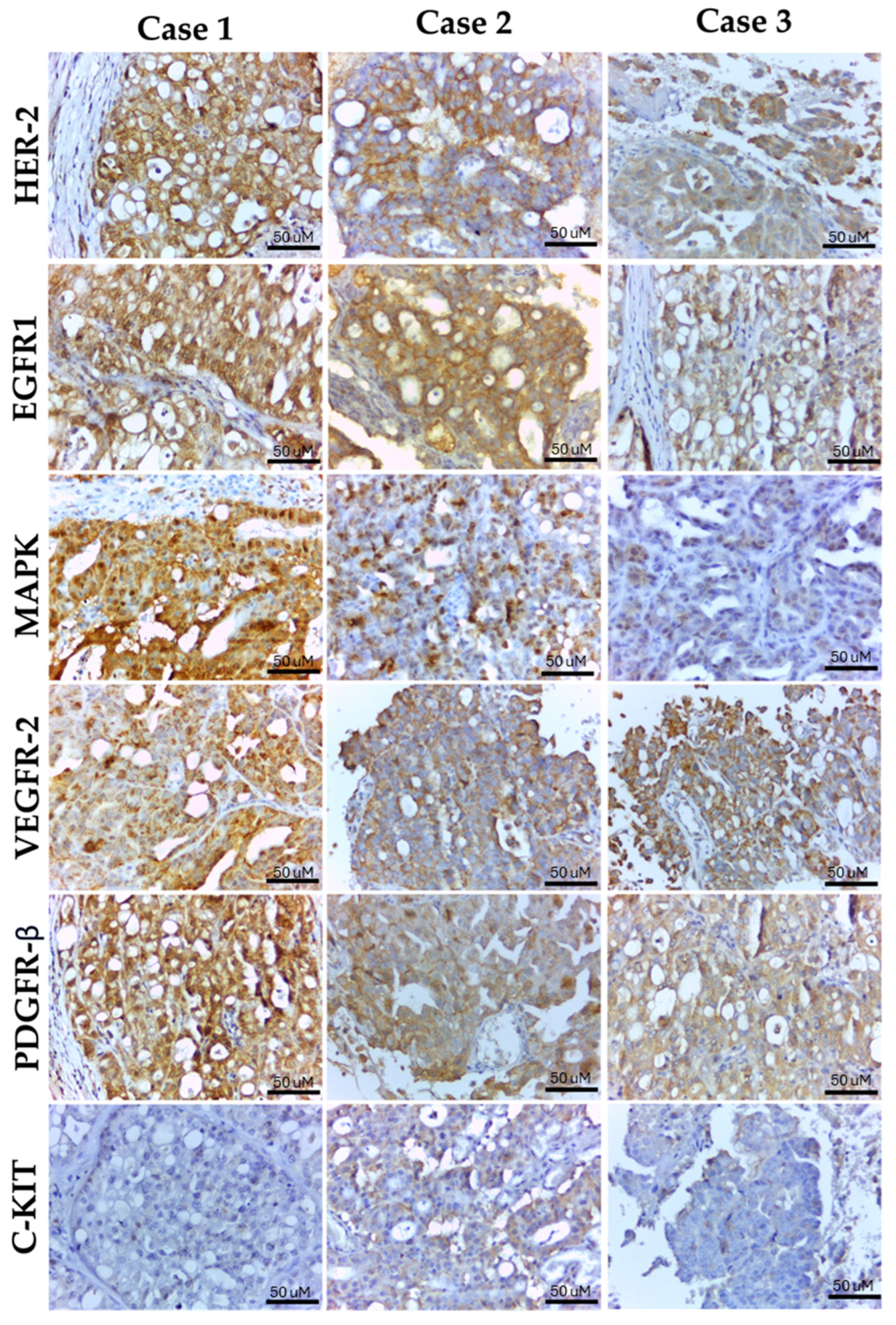
2. Results
3. Discussion
4. Materials and Methods
4.1. Screening of Different Tyrosine Kinase Receptors in Canine Solid Tumors
4.2. Selection of Solid Tumor Cases
4.3. Cross-Reactivity with Canine Tissue
4.4. Immunohistochemistry
4.5. Immunohistochemistry Analysis and Selection of the Tyrosine Kinase Inhibitors
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fonseca-Alves, C.; Palmieri, C.; Dagli, M.L.Z.; Laufer-Amorim, R. Editorial: Precision Medicine in Veterinary Oncology. Front. Vet. Sci. 2021, 8, 718891. [Google Scholar] [CrossRef]
- Ullrich, A.; Coussens, L.; Hayflick, J.S.; Dull, T.J.; Gray, A.; Tam, A.W.; Lee, J.; Yarden, Y.; Libermann, T.A.; Schlessinger, J.; et al. Human epidermal growth factor receptor cDNA sequence and aberrant expression of the amplified gene in A431 epidermoid carcinoma cells. Nature 1984, 309, 418–425. [Google Scholar] [CrossRef]
- Guo, P.; Pu, T.; Chen, S.; Qju, Y.; Zhong, X.; Zheng, H.; Chen, L.; Bu, H.; Ye, F. Breast cancers with EGFR and HER2 co-amplification favor distant metastasis and poor clinical outcome. Oncol. Lett. 2017, 14, 6562–6570. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rehmani, H.S.; Issaeva, N. EGFR in head and neck squamous cell carcinoma: Exploring possibilities of novel drug combinations. Ann. Transl. Med. 2020, 8, 813. [Google Scholar] [CrossRef]
- Gray, M.E.; Lee, S.; McDowell, A.L.; Erskine, M.; Loh, Q.T.M.; Grice, O.; Argyle, D.J.; Bergkvist, G.T. Dual targeting of EGFR and ERBB2 pathways produces a synergistic effect on cancer cell proliferation and migration in vitro. Vet. Comp. Oncol. 2017, 15, 890–909. [Google Scholar] [CrossRef] [PubMed]
- Mok, T.S.; Wu, Y.L.; Thongprasert, S.; Yang, C.H.; Chu, D.T.; Saijo, N.; Sunpaweravong, P.; Han, B.; Margono, B.; Ichinose, Y.; et al. Gefitinib or Carboplatin–Paclitaxel in Pulmonary Adenocarcinoma. N. Engl. J. Med. 2009, 361, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Sanguedolce, F.; Zanelli, M.; Palicelli, A.; Bisagni, A.; Zizzo, M.; Ascani, S.; Pedicillo, M.C.; Cormio, A.; Falagario, U.G.; Carrieri, G.; et al. HER2 expression in bladder cancer: A focused view on its diagnostic, prognostic, and predictive role. Int. J. Mol. Sci. 2023, 24, 3720. [Google Scholar] [CrossRef]
- Anderson, S.; Bartow, B.B.; Siegal, G.P.; Huang, X.; Wei, S. The dynamics of HER2-low expression during breast cancer progression. Breast Cancer Res. Treat. 2023, 201, 437–446. [Google Scholar] [CrossRef]
- McAfee, J.L.; Hoda, R.S.; Hoyle, C.; McCoy, L.; Sprague, C.; Reddy, C.A.; Koyfman, S.A.; Geiger, J.L.; Komforti, M.K.; Griffith, C.C. ERBB2 amplification and HER2 expression in salivary duct carcinoma: Evaluation of scoring guidelines and potential for expanded anti-HER2 therapy. Mod. Pathol. 2023, 7, 100273. [Google Scholar] [CrossRef]
- Bergkvist, G.T.; Yool, D.A. Epidermal growth factor receptor as a therapeutic target in veterinary oncology. Vet. Comp. Oncol. 2011, 9, 81–94. [Google Scholar] [CrossRef]
- Minke, J.M.; Schuuring, E.; Van Den Berghe, R.; Stolwijk, J.A.; Boonstra, J.; Cornelisse, C.; Hilkens, J.; Misdorp, W. Isolation of two distinct epithelial cell lines from a single feline mammary carcinoma with different tumorigenic potential in nude mice and expression different levels of epidermal growth factor receptors. Cancer Res. 1991, 51, 4028–4037. [Google Scholar] [PubMed]
- Wiese, D.; Thaiwong, T.; Yuzbasiyan-Gurkan, V.; Kiupel, M. Feline mammary basal-like adenocarcinomas: A potential model for human triple-negative breast cancer (TNBC) with basal-like subtype. BMC Cancer 2013, 13, 403. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, K.C.; Qurollo, B.A.; Rose, B.J.; Thamm, D.H. Epidermal growth factor enhances the malignant phenotype in canine mammary carcinoma cell lines. Vet. Comp. Oncol. 2011, 9, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.I.; Guimarães, M.J.; Pires, I.; Prada, J.; Silva-Carvalho, R.; Lopes, C.; Queiroga, F.L. EGFR and microvessel density in canine malignant mammary tumours. Res. Vet. Sci. 2013, 95, 1094–1099. [Google Scholar] [CrossRef] [PubMed]
- Muscatello, L.V.; Gobbo, F.; Di Oto, E.; Sarli, G.; De Maria, R.; De Leo, A.; Tallini, G.; Brunetti, B. HER2 Overexpression and Cytogenetical Patterns in Canine Mammary Carcinomas. Vet. Sci. 2022, 22, 583. [Google Scholar] [CrossRef] [PubMed]
- Leis-Filho, A.F.; Lainetti, P.D.; Kobayashi, P.E.; Palmieri, C.; Amorim, R.L.; Fonseca-Alves, C.E. Expression and prognostic significance of vascular endothelial growth factor-A (VEGF-A) and its receptor in canine prostate cancer. Prostate 2021, 81, 1021–1031. [Google Scholar] [CrossRef] [PubMed]
- Maeda, S.; Sakai, K.; Kaji, K.; Iio, A.; Nakazawa, M.; Motegi, T.; Yonezawa, T.; Momoi, Y. Lapatinib as first-line treatment for muscle-invasive urothelial carcinoma in dogs. Sci. Rep. 2022, 13, 4. [Google Scholar] [CrossRef] [PubMed]
- Lorch, G.; Sivaprakasam, K.; Zismann, V.; Perdigones, N.; Contente-Cuomo, T.; Nazareno, A.; Facista, S.; Wong, S.; Drenner, K.; Liang, W.S.; et al. Identification of Recurrent Activating HER2 Mutations in Primary Canine Pulmonary Adenocarcinoma. Clin. Cancer Res. 2019, 25, 5866–5877. [Google Scholar] [CrossRef] [PubMed]
- Stierer, M.; Rosen, H.; Weber, R.; Hanak, H.; Spona, J.; Tuchler, H. Immunohistochemical and biochemical measurement of estrogen and progesterone receptors in primary breast cancer. Correlation of histopathology and prognostic factors. Ann. Surg. 1993, 218, 13–21. [Google Scholar] [CrossRef]
- Zaha, D.C. Significance of immunohistochemistry in breast cancer. World J. Clin. Oncol. 2014, 10, 382–392. [Google Scholar] [CrossRef]
- Effi, A.B.; Aman, N.A.; Koui, B.S.; Koffi, K.D.; Traoré, Z.C.; Kouyate, M. Immunohistochemical determination of estrogen and progesterone receptors in breast cancer: Relationship with clinicopathologic factors in 302 patients in Ivory Coast. BMC Cancer 2017, 17, 115. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Krishnamurti, U.; Zhang, C.; Meisel, J.; Wei, Z.; Suo, A.; Aneja, R.; Li, Z.; Li, X. HER2 immunohistochemistry staining positivity is strongly predictive of tumor response to neoadjuvant chemotherapy in HER2 positive breast cancer. Pathol. Res. Pract. 2020, 216, 153155. [Google Scholar] [CrossRef] [PubMed]
- Allison, K.H.; Hammond, M.E.H.; Dowsett, M.; McKernin, S.E.; Carey, L.A.; Fitzgibbons, P.L.; Hayes, D.F.; Lakhani, S.R.; Chavez-MacGregor, M.; Perlmutter, J.; et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J. Clin. Oncol. 2020, 38, 1346–1366. [Google Scholar] [CrossRef] [PubMed]
- Mino-Kenudson, M. Immunohistochemistry for predictive biomarkers in non-small cell lung cancer. Transl. Lung Cancer Res. 2017, 6, 570–587. [Google Scholar] [CrossRef] [PubMed]
- Travaglino, A.; Raffone, A.; Saccone, G.; Insabato, L.; Mollo, A.; De Placido, G.; Zullo, F. Immunohistochemical predictive markers of response to conservative treatment of endometrial hyperplasia and early endometrial cancer: A systematic review. Acta Obstet. Gynecol. Scand. 2019, 98, 1086–1099. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Wang, L.; Li, H.; Zhang, Y.; Gao, Y.; Guo, G.; Liu, K.; Meng, Q.; Zhao, C.; Wang, D.; et al. Predictive Immunohistochemical Markers Related to Drug Selection for Patients Treated with Sunitinib or Sorafenib for Metastatic Renal Cell Cancer. Sci. Rep. 2016, 6, 30886. [Google Scholar] [CrossRef]
- Aupperle-Lellbach, H.; Kehl, A.; Brot, S.; Van der Weyden, L. Clinical use of molecular biomarkers in canine and feline oncology: Current and future. Vet. Sci. 2024, 11, 199. [Google Scholar] [CrossRef] [PubMed]
- Urie, B.K.; Russell, D.S.; Kisseberth, W.C.; London, C.A. Evaluation of expression and function of vascular endothelial growth factor receptor 2, platelet derived growth factor receptors-alpha and -beta, KIT, and RET in canine apocrine gland anal sac adenocarcinoma and thyroid carcinoma. BMC Vet. Res. 2012, 8, 67. [Google Scholar] [CrossRef] [PubMed]
- Harding, K.; De Mello Souza, C.H.; Shiomitsu, K.; Maxwell, E.; Bertran, J. C-kit, flt-3, PDGFR-β, and VEGFR2 expression in canine adrenal tumors and correlation with outcome following adrenalectomy. Can. J. Vet. Res. 2021, 85, 279–284. [Google Scholar]
- Setyo, L.C.; Donahoe, S.L.; Shearer, P.L.; Wang, P.; Krockenberger, M.B. Immunohistochemical analysis of expression of VEGFR2, KIT, PDGFR-β, and CDK4 in canine urothelial carcinoma. J. Vet. Diagn. Investig. 2023, 35, 109–115. [Google Scholar] [CrossRef]
- Gattino, F.; Maniscalco, L.; Iussich, S.; Biasato, I.; Martano, M.; Morello, E.; Gola, C.; Ruiz, Y.M.; Saeki, N.; Buracco, P.; et al. PDGFR-α, PDGFR-β, VEGFR-2 and CD117 expression in canine mammary tumours and evaluation of the in vitro effects of toceranib phosphate in neoplastic mammary cell lines. Vet. Rec. 2018, 183, 221. [Google Scholar] [CrossRef] [PubMed]
- London, C.A.; Hannah, A.L.; Zadovoskaya, R.; Chien, M.B.; Kollias-Baker, C.; Rosenberg, M.; Downing, S.; Post, G.; Boucher, J.; Shenoy, N.; et al. Phase I dose-escalating study of SU11654, a small molecule receptor tyrosine kinase inhibitor, in dogs with spontaneous malignancies. Clin. Cancer Res. 2003, 9, 2755–2768. [Google Scholar] [PubMed]
- LeBlanc, A.K.; Miller, A.N.; Galyon, G.D.; Moyers, T.D.; Long, M.J.; Stuckey, A.C.; Wall, J.S.; Morandi, F. Preliminary evaluation of serial (18) FDG-PET/CT to assess response to toceranib phosphate therapy in canine cancer. Vet. Radiol. Ultrasound 2012, 53, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, H.; Tanaka, T.; Mie, K.; Nishida, H.; Miura, N.; Akiyoshi, H. Assessment of postoperative adjuvant treatment using toceranib phosphate against adenocarcinoma in dogs. J. Vet. Intern. Med. 2020, 34, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Graziano, C. HER-2 breast assay, linked to Herceptin, wins FDA’s okay. CAP Today 1998, 12, 14–16. [Google Scholar]
- Wisecarver, J.L. HER-2/neu testing comes of age. Am. J. Clin. Pathol. 1999, 111, 299–301. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sakamoto, G.; Mitsuyama, S. New molecule-targeting therapy with herceptin (trastuzumab), an anti-HER2 (c-erB-2) monoclonal antibody. Breast Cancer 2000, 7, 350–357. [Google Scholar] [CrossRef]
- Tsuda, H.; Tani, Y.; Hasegawa, T.; Fukutomi, T. Concordance in judgments among c-erbB-2 (HER2/neu) overexpression detected by two immunohistochemical tests and gene amplification detected by Southern blot hybridization in breast carcinoma. Pathol. Int. 2001, 51, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Hatanaka, Y.; Hashizume, K.; Kamihara, Y.; Itoh, H.; Tsuda, H.; Osamura, R.Y.; Tani, Y. Quantitative immunohistochemical evaluation of HER2/neu expression with HercepTestTM in breast carcinoma by image analysis. Pathol. Int. 2001, 51, 33–36. [Google Scholar] [CrossRef]
- O’Malley, F.P.; Parkes, R.; Latta, E.; Tjan, S.; Zadro, T.; Mueller, R.; Arneson, N.; Blackstein, M.; Andrulis, I. Comparison of HER2/neu status assessed by quantitative polymerase chain reaction and immunohistochemistry. Am. J. Clin. Pathol. 2001, 115, 504–511. [Google Scholar] [CrossRef][Green Version]
- Nguyen, F.; Peña, L.; Ibisch, C.; Loussouarn, D.; Gama, A.; Rieder, N.; Belousov, A.; Campone, M.; Abadie, J. Canine invasive mammary carcinomas as models of human breast cancer. Part 1: Natural history and prognostic factors. Breast Cancer Res. Treat. 2018, 167, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Pastor, N.; Ezquerra, L.J.; Santella, M.; Caballé, N.C.; Tarazona, R.; Durán, M.E. Prognostic significance of immunohistochemical markers and histological classification in malignant canine mammary tumours. Vet. Comp. Oncol. 2020, 18, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Seung, B.J.; Cho, S.H.; Kim, S.H.; Lim, H.Y.; Sur, J.H. Quantitative analysis of HER2 mRNA expression by RNA in situ hybridization in canine mammary gland tumors: Comparison with immunohistochemistry analysis. PLoS ONE 2020, 15, e0229031. [Google Scholar] [CrossRef] [PubMed]
- Martin de las Mulas, J.; Ordás, J.; Millán, Y.; Fernández-Soria, V.; Ramón, C.S. Oncogene HER-2 in canine mammary gland carcinomas: An immunohistochemical and chromogenic in situ hybridization study. Breast Cancer Res. Treat. 2003, 80, 363–367. [Google Scholar] [CrossRef]
- Kobayashi, P.E.; Lainetti, P.F.; Leis-Filho, A.F.; Delella, F.K.; Carvalho, M.; Cury, S.S.; Carvalho, R.F.; Fonseca-Alves, C.E.; Laufer-Amorim, R. Transcriptome of Two Canine Prostate Cancer Cells Treated with Toceranib Phosphate Reveals Distinct Antitumor Profiles Associated with the PDGFR Pathway. Front. Vet. Sci. 2020, 7, 561212. [Google Scholar] [CrossRef] [PubMed]
- Walters, L.; Martin, O.; Price, J.; Sula, M.M. Expression of receptor tyrosine kinase targets PDGFR-β, VEGFR2 and KIT in canine transitional cell carcinoma. Vet. Comp. Oncol. 2018, 16, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Yokota, S.; Yonezawa, T.; Momoi, Y.; Maeda, S. Sorafenib inhibits tumor cell growth and angiogenesis in canine transitional cell carcinoma. Vet. Med. Sci. 2022, 84, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Sheppard-Olivares, S.; Bello, N.M.; Johannes, C.M.; Hocker, S.E.; Biller, B.; Husbands, B.; Snyder, E.; McMillan, M.; McKee, T.; Wouda, R.M. Toceranib phosphate in the management of canine insulinoma: A retrospective multicentre study of 30 cases (2009–2019). Vet. Rec. Open 2022, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Flesner, B.K.; Fletcher, J.M.; Smithee, T.; Boudreaux, B. Longterm survival and glycemic control with toceranib phosphate and prednisone for a metastatic canine insulinoma. J. Am. Anim. Hosp. Assoc. 2019, 55, e55105. [Google Scholar] [CrossRef]
- Buishand, F.O. Current Trends in Diagnosis, Treatment and Prognosis of Canine Insulinoma. Vet. Sci. 2022, 29, 540. [Google Scholar] [CrossRef]
- Ramos-Vara, J.A.; Kiupel, M.; Baszler, T.; Bliven, L.; Brodersen, B.; Chelack, B.; Czub, S.; Del Piero, F.; Dial, S.; Ehrhart, E.J.; et al. American Association of Veterinary Laboratory Diagnosticians Subcommittee on Standardization of Immunohistochemistry. Suggested guidelines for immunohistochemical techniques in veterinary diagnostic laboratories. J. Vet. Diagn. Investig. 2008, 20, 393–413. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Alves, C.E.; Kobayashi, P.E.; Palmieri, C.; Laufer-Amorim, R. Investigation of c-KIT and Ki67 expression in normal, preneoplastic and neoplastic canine prostate. BMC Vet. Res. 2017, 13, 380. [Google Scholar] [CrossRef] [PubMed]
- Maniscalco, L.; Iussich, S.; Morello, E.; Martano, M.; Biolatti, B.; Riondato, F.; Salda, L.D.; Romanucci, M.; Malatesta, D.; Bongiovanni, L.; et al. PDGFs and PDGFRs in canine osteosarcoma: New targets for innovative therapeutic strategies in comparative oncology. Vet. J. 2013, 195, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, M.; Sakai, K.; Maeda, S.; Chambers, J.K.; Yonezawa, T.; Matsuki, N.; Uchida, K.; Nakayama, H. Assessment of HER2 Expression in Canine Urothelial Carcinoma of the Urinary Bladder. Vet. Pathol. 2019, 56, 369–376. [Google Scholar] [CrossRef]
- Nuovo, G. False-positive results in diagnostic immunohistochemistry are related to horseradish peroxidase conjugates in commercially available assays. Ann. Diagn. Pathol. 2016, 25, 54–59. [Google Scholar] [CrossRef]
| ID | HER2 | EGFR-1 | VEGFR-2 | PDGFR-β | c-Kit | ERK1/ ERK2 |
|---|---|---|---|---|---|---|
| Prostatic Carcinomas | ||||||
| Case 1 | 0 | 0 | 2+ | 1+ | 0 | 0 |
| Case 2 | 2+ | 0 | 1+ | 0 | 0 | 0 |
| Case 3 | 2+ | 0 | 2+ | 0 | 0 | 0 |
| Case 4 | 2+ | 0 | 2+ | 0 | 0 | 0 |
| Case 5 | 3+ | 1+ | 3+ | 0 | 0 | 2+ |
| Case 6 | 3+ | 2+ | 3+ | 2+ | 0 | 2+ |
| Case 7 | 4+ | 3+ | 2+ | 2+ | 0 | 0 |
| Case 8 | 3+ | 2+ | 2+ | 2+ | 0 | 0 |
| Case 9 | 4+ | 3+ | 2+ | 1+ | 1+ | 0 |
| Case 10 | 3+ | 3+ | 4+ | 0 | 0 | 3+ |
| Case 11 | 2+ | 4+ | 3+ | 2+ | 0 | 1+ |
| Case 12 | 3+ | 3+ | 3+ | 2+ | 0 | 0 |
| Case 13 | 4+ | 3+ | 3+ | 0 | 0 | 0 |
| Case 14 | 4+ | 3+ | 4+ | 3+ | 0 | 4+ |
| Case 15 | 3+ | 3+ | 2+ | 2+ | 0 | 0 |
| Case 16 | 4+ | 2+ | 3+ | 2+ | 0 | 2+ |
| Case 17 | 3+ | 3+ | 4+ | 2+ | 0 | 1+ |
| Case 18 | 3+ | 3+ | 2+ | 0 | 0 | 1+ |
| Soft Tissue Sarcomas | ||||||
| Case 1 | 0 | 0 | 0 | 1+ | 0 | 0 |
| Case 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 4 | 0 | 0 | 1+ | 0 | 0 | 0 |
| Case 5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 6 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 7 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 8 | 0 | 0 | 1+ | 1+ | 0 | 0 |
| Case 9 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 10 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 11 | 0 | 0 | 1+ | 0 | 0 | 0 |
| Case 12 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 13 | 0 | 0 | 0 | 1+ | 0 | 0 |
| Case 14 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 15 | 0 | 0 | 2+ | 0 | 0 | 0 |
| Case 16 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 17 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 18 | 0 | 0 | 1+ | 2+ | 0 | 0 |
| Case 19 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 20 | 0 | 0 | 0 | 0 | 0 | 2+ |
| Case 21 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 22 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 23 | 0 | 0 | 0 | 1+ | 0 | 0 |
| Case 24 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 25 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 26 | 0 | 0 | 1+ | 0 | 0 | 0 |
| Case 27 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 28 | 0 | 0 | 0 | 0 | 0 | 1+ |
| Case 29 | 0 | 0 | 0 | 2+ | 0 | 0 |
| Case 30 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 31 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 32 | 0 | 0 | 1+ | 0 | 0 | 0 |
| Case 33 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 34 | 0 | 0 | 0 | 1+ | 0 | 1+ |
| Case 35 | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 36 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mammary Gland Carcinomas | ||||||
| Case 1 (comedocarcinoma) | 3+ | 2+ | 3+ | 2+ | 0 | 0 |
| Case 2 (solid carcinoma) | 3+ | 3+ | 3+ | 2+ | 0 | 0 |
| Case 3 (carcinoma in mixed tumor) | 0 | 1+ | 0 | 1+ | 0 | 0 |
| Case 4 (solid carcinoma) | 3+ | 2+ | 3+ | 0 | 0 | 2+ |
| Case 5 (Tubular carcinoma) | 0 | 1+ | 3+ | 0 | 0 | 0 |
| Case 6 (carcinoma in mixed tumor) | 0 | 0 | 4+ | 3+ | 0 | 0 |
| Case 7 (complex carcinoma) | 0 | 0 | 2+ | 3+ | 0 | 3+ |
| Case 8 (inflammatory carcinoma) | 0 | 1+ | 3+ | 1+ | 0 | 3+ |
| Case 9 (complex carcinoma) | 0 | 0 | 2+ | 1+ | 0 | 0 |
| Case 10 (tubular carcinoma) | 0 | 1+ | 2+ | 0 | 0 | 0 |
| Case 11 (complex carcinoma) | 3+ | 0 | 0 | 1+ | 0 | 1+ |
| Case 12 (tubular carcinoma) | 0 | 0 | 2+ | 0 | 0 | 0 |
| Case 13 (micropapillary carcinoma) | 3+ | 2+ | 1+ | 0 | 0 | 0 |
| Case 14 (inflammatory carcinoma) | 3+ | 2+ | 0 | 0 | 0 | 0 |
| Case 15 (carcinoma in mixed tumor) | 0 | 0 | 0 | 0 | 0 | 0 |
| Case 16 (solid carcinoma) | 4+ | 3+ | 4+ | 3+ | 0 | 2+ |
| Case 17 (solid carcinoma) | 2+ | 0 | 3+ | 1+ | 0 | 2+ |
| Case 18 (solid carcinoma) | 3+ | 2+ | 3+ | 2+ | 0 | 2+ |
| Case 19 (solid carcinoma) | 2+ | 2+ | 2+ | 0 | 0 | 1+ |
| Case 20 (solid carcinoma) | 3+ | 2+ | 3+ | 0 | 0 | 0 |
| Urothelial Bladder Carcinomas | ||||||
| Case 1 | 3+ | 3+ | 3+ | 0 | 1+ | 4+ |
| Case 2 | 4+ | 3+ | 3+ | 0 | 0 | 3+ |
| Case 3 | 3+ | 3+ | 2+ | 0 | 0 | 0 |
| Case 4 | 4+ | 3+ | 4+ | 0 | 0 | 4+ |
| Case 5 | 4+ | 3+ | 3+ | 0 | 1+ | 4+ |
| Case 6 | 3+ | 3+ | 0 | 1+ | 0 | 2+ |
| Endocrine/neuroendocrine Tumors | ||||||
| Case 1 (thyroid carcinoma) | 0 | 0 | 1+ | 3+ | 0 | 2+ |
| Case 2 (thyroid carcinoma) | 0 | 0 | 2+ | 1+ | 0 | 2+ |
| Case 3 (insulinoma) | 0 | 0 | 2+ | 0 | 0 | 0 |
| Case 4 (insulinoma) | 0 | 0 | 4+ | 2+ | 0 | 0 |
| Case 5 (mammary neuroendocrine carcinoma) | 0 | 0 | 1+ | 0 | 0 | 2+ |
| Case 6 (hepatic neuroendocrine carcinoma) | 0 | 0 | 4+ | 4+ | 0 | 4+ |
| Case 7 (pancreatic solid carcinoma) | 1+ | 1+ | 4+ | 1+ | 0 | 3+ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dos Anjos, D.S.; Civa, P.A.S.; Werner, J.; Vicente, I.S.T.; Fonseca-Alves, C.E. Immunohistochemistry Screening of Different Tyrosine Kinase Receptors in Canine Solid Tumors—Part I: Proposal of a Receptor Panel to Predict Therapies. Int. J. Mol. Sci. 2024, 25, 8438. https://doi.org/10.3390/ijms25158438
Dos Anjos DS, Civa PAS, Werner J, Vicente IST, Fonseca-Alves CE. Immunohistochemistry Screening of Different Tyrosine Kinase Receptors in Canine Solid Tumors—Part I: Proposal of a Receptor Panel to Predict Therapies. International Journal of Molecular Sciences. 2024; 25(15):8438. https://doi.org/10.3390/ijms25158438
Chicago/Turabian StyleDos Anjos, Denner Santos, Patrick Antônio Sonaglio Civa, Juliana Werner, Igor Simões Tiagua Vicente, and Carlos Eduardo Fonseca-Alves. 2024. "Immunohistochemistry Screening of Different Tyrosine Kinase Receptors in Canine Solid Tumors—Part I: Proposal of a Receptor Panel to Predict Therapies" International Journal of Molecular Sciences 25, no. 15: 8438. https://doi.org/10.3390/ijms25158438
APA StyleDos Anjos, D. S., Civa, P. A. S., Werner, J., Vicente, I. S. T., & Fonseca-Alves, C. E. (2024). Immunohistochemistry Screening of Different Tyrosine Kinase Receptors in Canine Solid Tumors—Part I: Proposal of a Receptor Panel to Predict Therapies. International Journal of Molecular Sciences, 25(15), 8438. https://doi.org/10.3390/ijms25158438






