The Human OCTN Sub-Family: Gene and Protein Structure, Expression, and Regulation
Abstract
1. Introduction
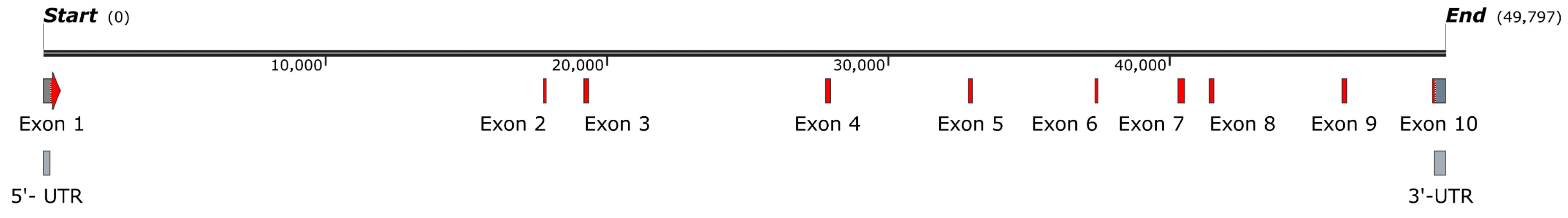
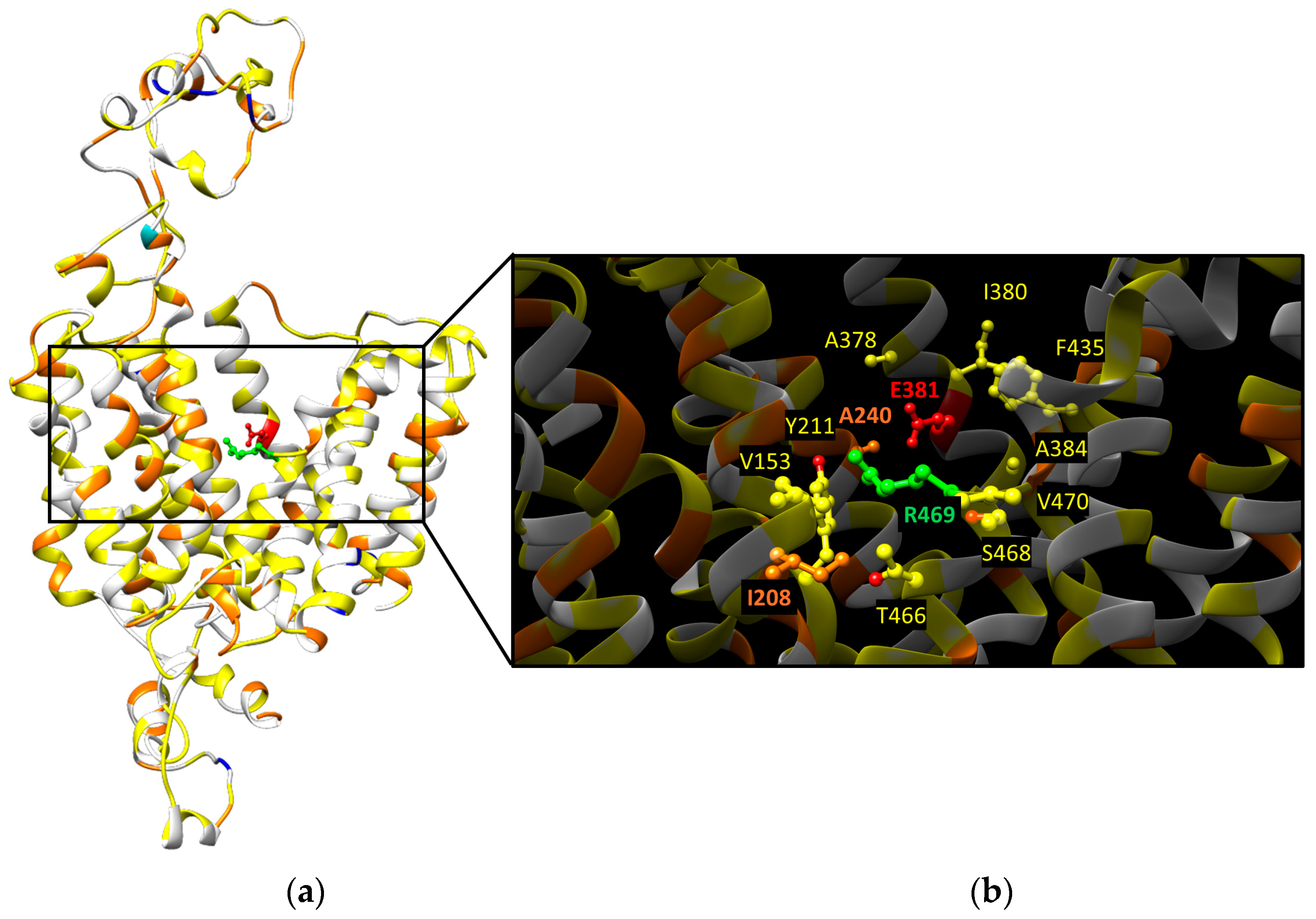
2. SLC22A4/OCTN1 Gene and Protein
2.1. OCTN1 Gene Variants (SNPs)
2.2. OCTN1 Transport Mechanisms
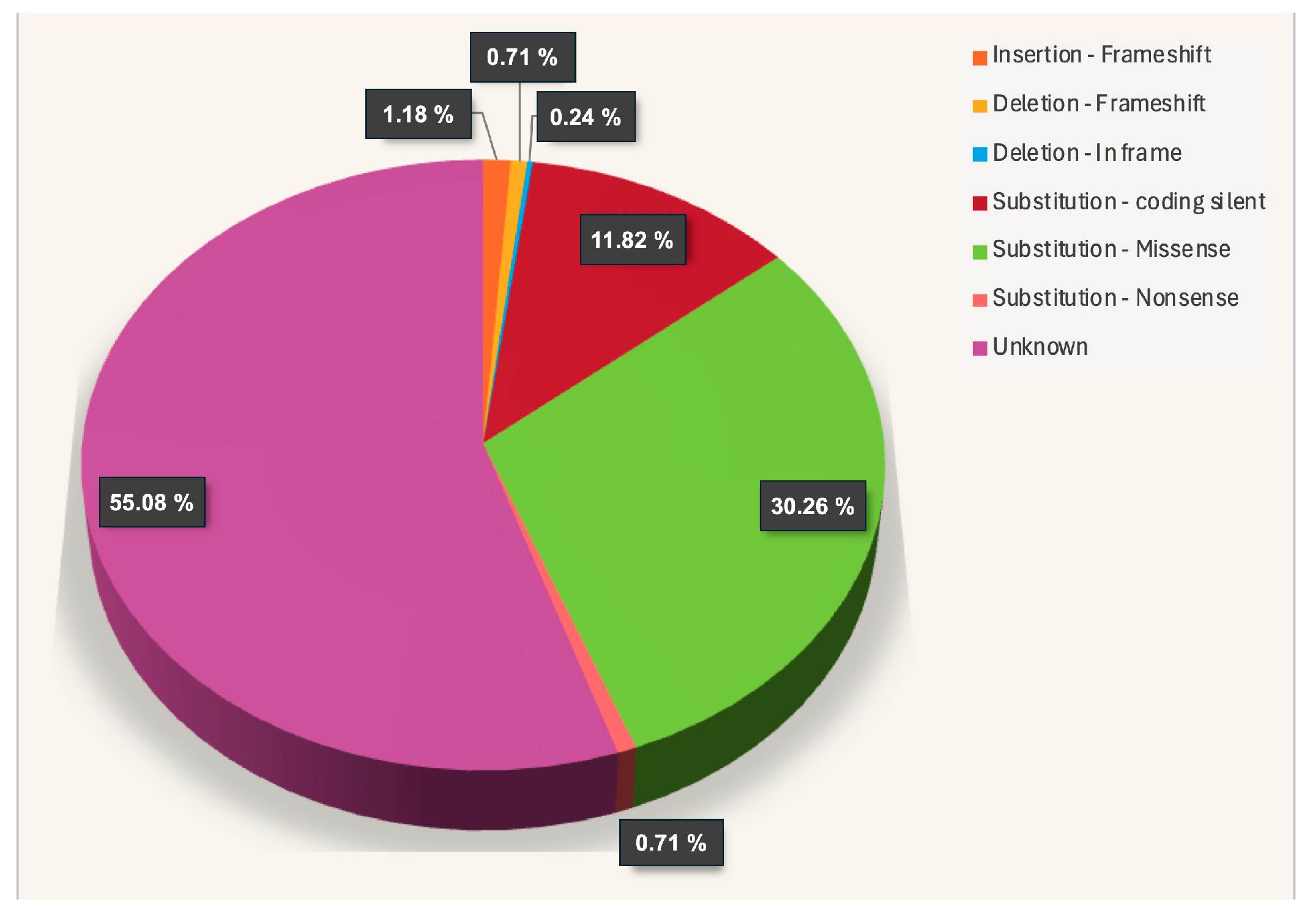
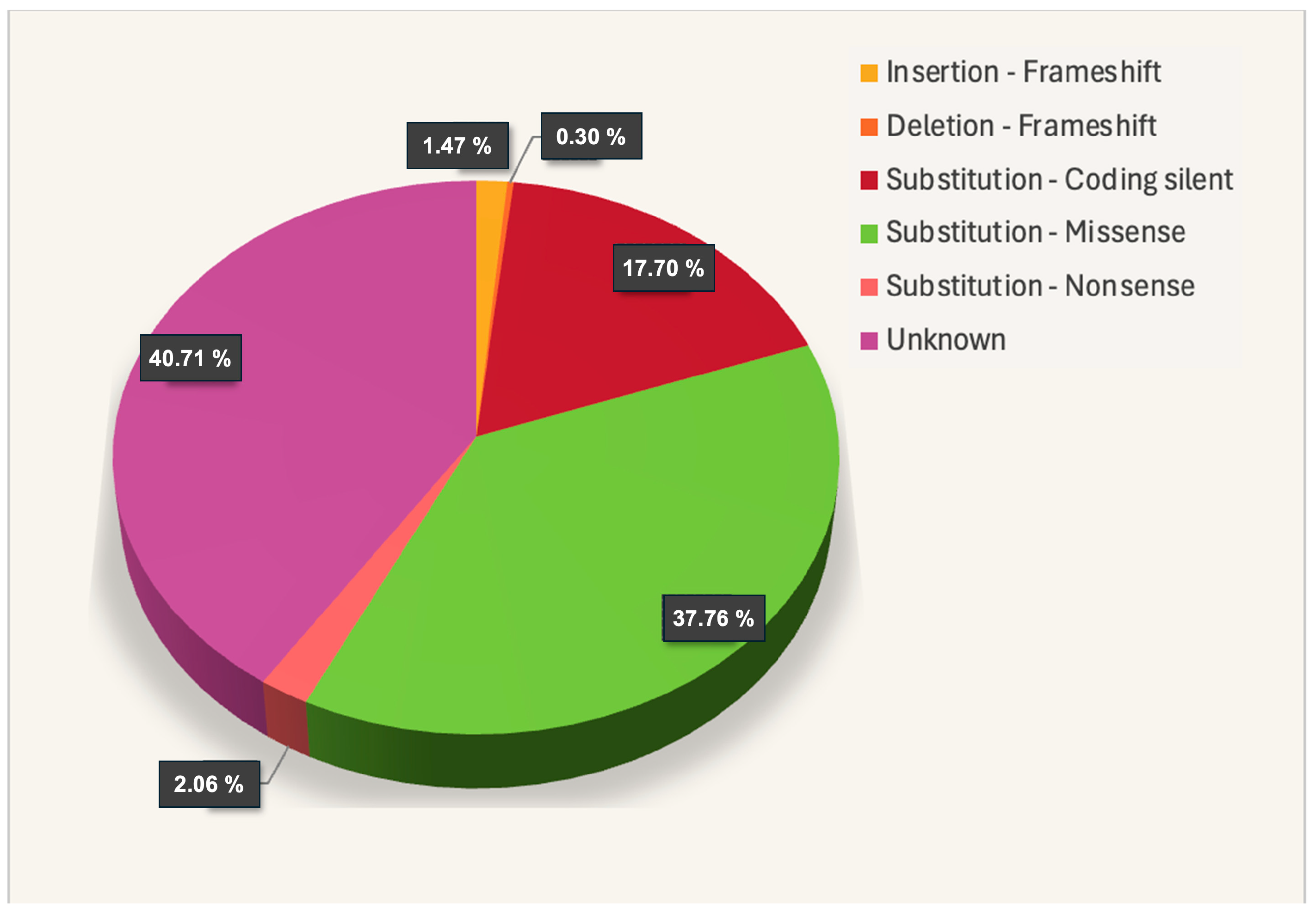
2.3. OCTN1 Somatic Mutations
2.4. OCTN1 Promoter/Enhancer
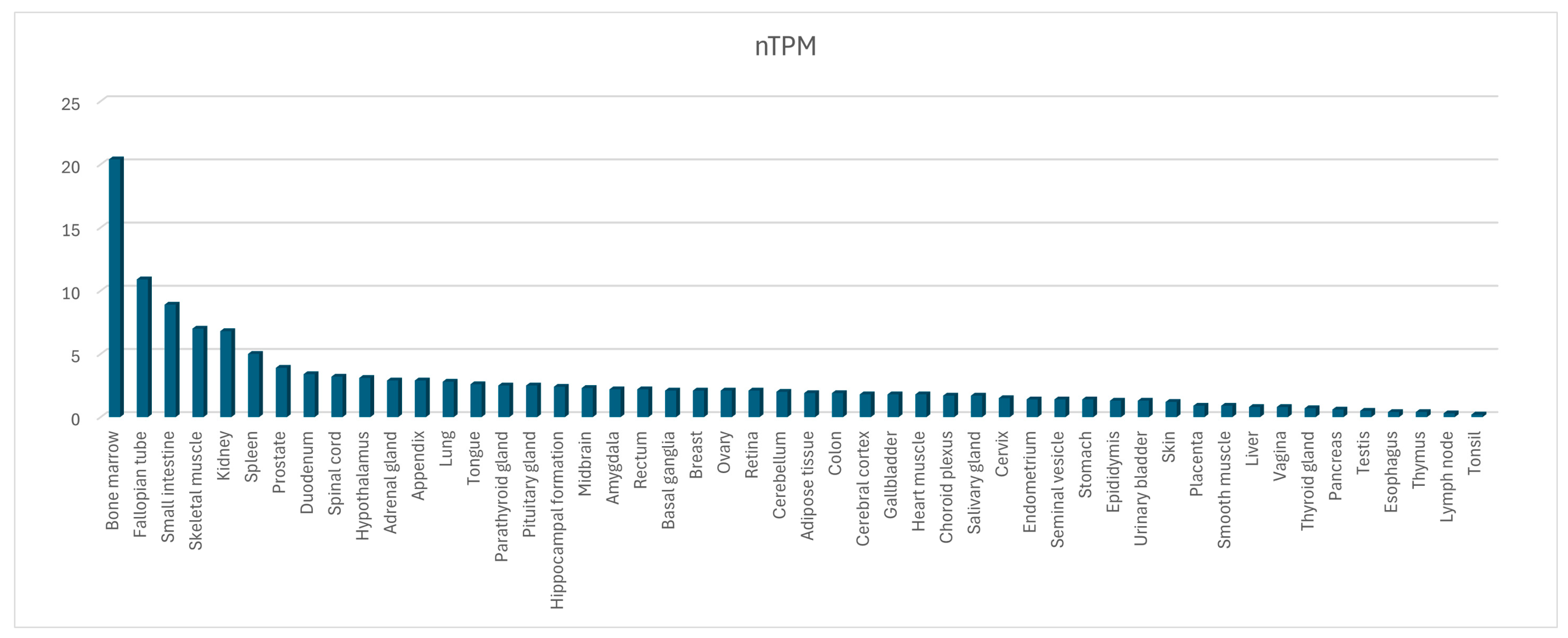
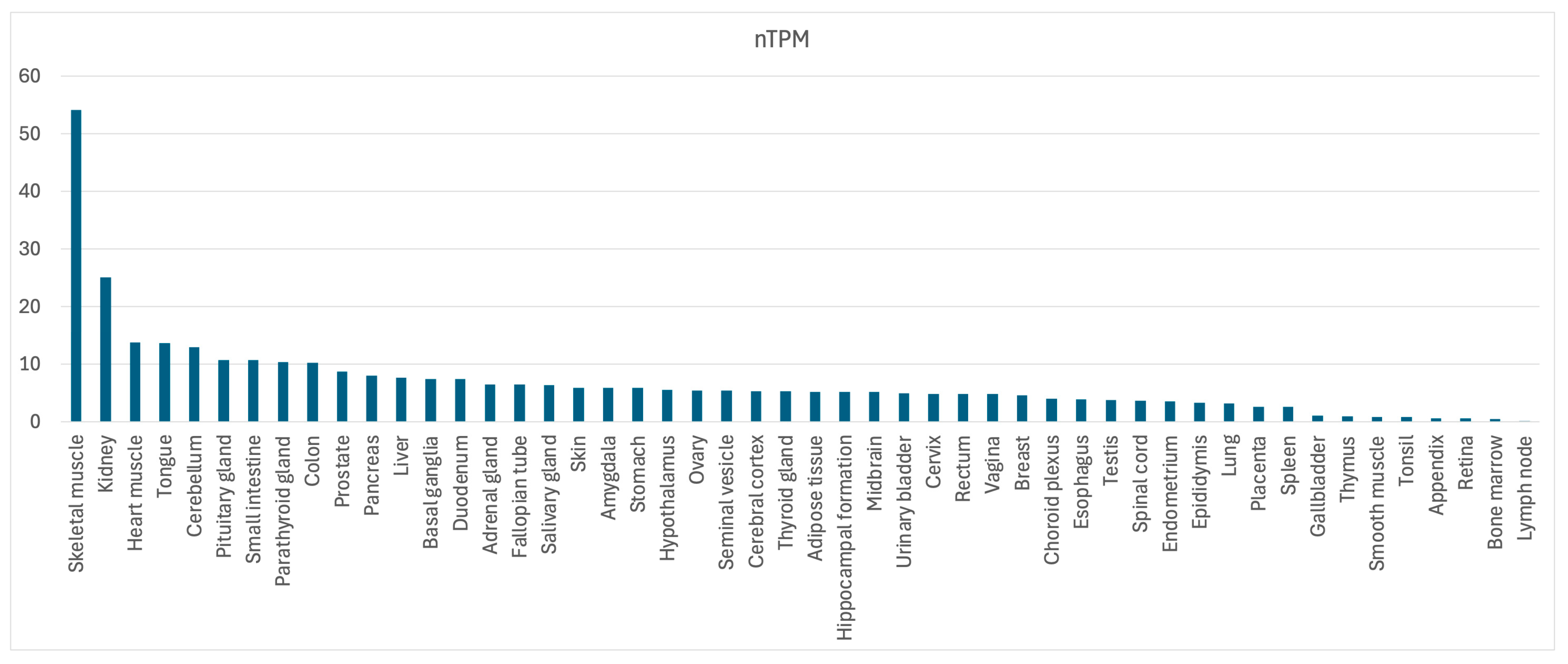
2.5. OCTN1 Gene and Protein Expression and Regulation
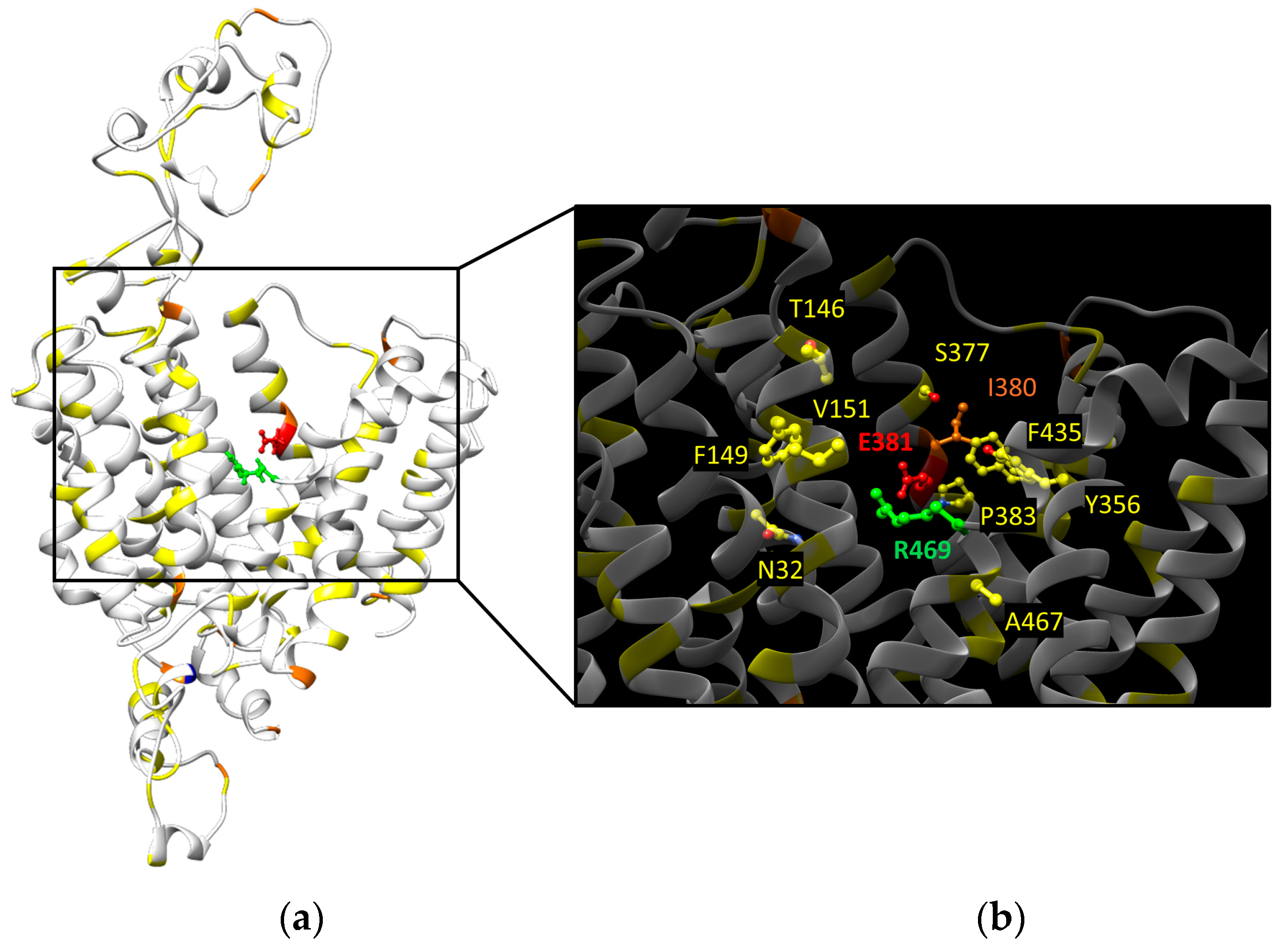
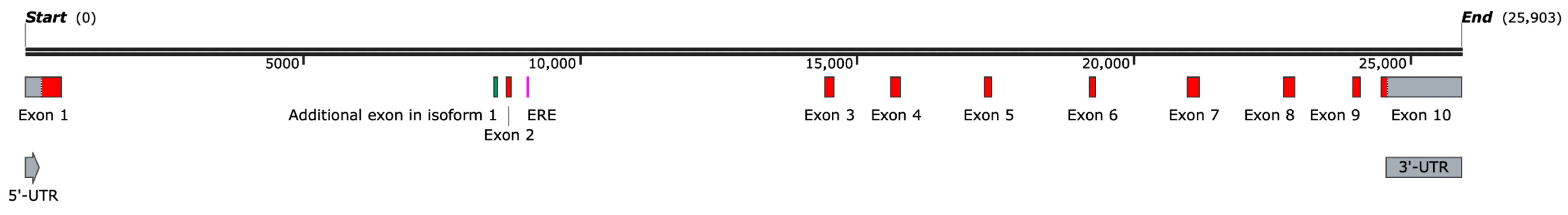
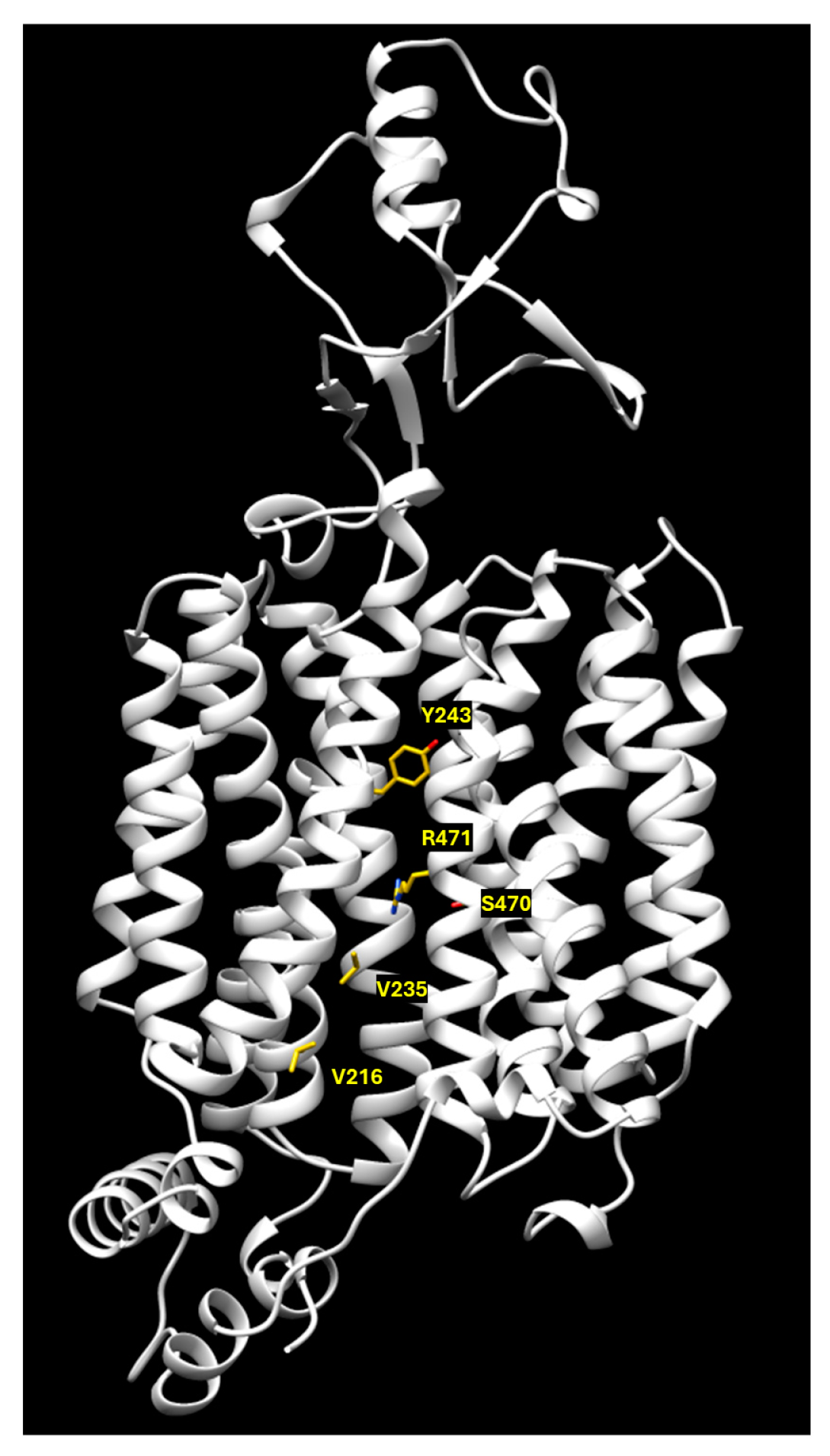
3. SLC22A5/OCTN2 Gene and Protein
3.1. OCTN2 Gene Variants (SNPs)
3.2. OCTN2 Transport Mechanism
3.3. OCTN2 Somatic Mutations
3.4. OCTN2 Promoter/Enhancer
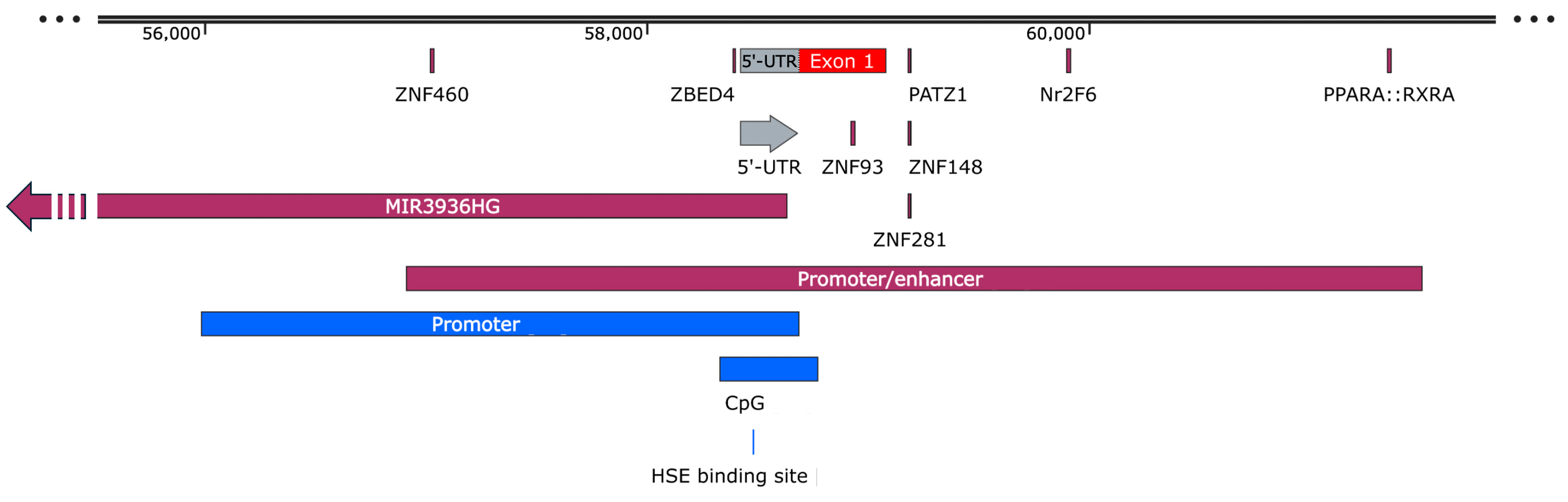
3.5. OCTN2 Gene and Protein Expression and Regulation
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ferrada, E.; Superti-Furga, G. A structure and evolutionary-based classification of solute carriers. iScience 2022, 25, 105096. [Google Scholar] [CrossRef] [PubMed]
- Dobson, L.; Remenyi, I.; Tusnady, G.E. The human transmembrane proteome. Biol. Direct 2015, 10, 31. [Google Scholar] [CrossRef] [PubMed]
- Koepsell, H. Organic Cation Transporters in Health and Disease. Pharmacol. Rev. 2020, 72, 253–319. [Google Scholar] [CrossRef] [PubMed]
- Suo, Y.; Wright, N.J.; Guterres, H.; Fedor, J.G.; Butay, K.J.; Borgnia, M.J.; Im, W.; Lee, S.Y. Molecular basis of polyspecific drug and xenobiotic recognition by OCT1 and OCT2. Nat. Struct. Mol. Biol. 2023, 30, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Khanppnavar, B.; Maier, J.; Herborg, F.; Gradisch, R.; Lazzarin, E.; Luethi, D.; Yang, J.W.; Qi, C.; Holy, M.; Jantsch, K.; et al. Structural basis of organic cation transporter-3 inhibition. Nat. Commun. 2022, 13, 6714. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.C.; Sobti, M.; Quinn, A.; Smith, N.J.; Brown, S.H.J.; Vandenberg, J.I.; Ryan, R.M.; O’Mara, M.L.; Stewart, A.G. Structural basis of promiscuous substrate transport by Organic Cation Transporter 1. Nat. Commun. 2023, 14, 6374. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhu, A.; Kong, F.; Chen, J.; Lan, B.; He, G.; Gao, K.; Cheng, L.; Sun, X.; Yan, C.; et al. Structural insights into human organic cation transporter 1 transport and inhibition. Cell Discov. 2024, 10, 30. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.L.; Kato, T.; Kuteyi, G.; Sitsel, O.; Newstead, S. Molecular basis for selective uptake and elimination of organic anions in the kidney by OAT1. Nat. Struct. Mol. Biol. 2023, 30, 1786–1793. [Google Scholar] [CrossRef] [PubMed]
- Pochini, L.; Barone, F.; Console, L.; Brunocilla, C.; Galluccio, M.; Scalise, M.; Indiveri, C. OCTN1 (SLC22A4) displays two different transport pathways for organic cations or zwitterions. Biochim. Biophys. Acta Biomembr. 2024, 1866, 184263. [Google Scholar] [CrossRef]
- Tamai, I. Pharmacological and pathophysiological roles of carnitine/organic cation transporters (OCTNs: SLC22A4, SLC22A5 and Slc22a21). Biopharm. Drug Dispos. 2013, 34, 29–44. [Google Scholar] [CrossRef]
- Enomoto, A.; Wempe, M.F.; Tsuchida, H.; Shin, H.J.; Cha, S.H.; Anzai, N.; Goto, A.; Sakamoto, A.; Niwa, T.; Kanai, Y.; et al. Molecular identification of a novel carnitine transporter specific to human testis. Insights into the mechanism of carnitine recognition. J. Biol. Chem. 2002, 277, 36262–36271. [Google Scholar] [CrossRef] [PubMed]
- Galluccio, M.; Mazza, T.; Scalise, M.; Sarubbi, M.C.; Indiveri, C. Bacterial over-expression of functionally active human CT2 (SLC22A16) carnitine transporter. Mol. Biol. Rep. 2022, 49, 8185–8193. [Google Scholar] [CrossRef] [PubMed]
- Koepsell, H.; Endou, H. The SLC22 drug transporter family. Pflügers Arch. 2004, 447, 666–676. [Google Scholar] [CrossRef] [PubMed]
- Pochini, L.; Galluccio, M.; Console, L.; Scalise, M.; Eberini, I.; Indiveri, C. Inflammation and Organic Cation Transporters Novel (OCTNs). Biomolecules 2024, 14, 392. [Google Scholar] [CrossRef] [PubMed]
- Pochini, L.; Galluccio, M.; Scalise, M.; Console, L.; Pappacoda, G.; Indiveri, C. OCTN1: A Widely Studied but Still Enigmatic Organic Cation Transporter Linked to Human Pathology and Drug Interactions. Int. J. Mol. Sci. 2022, 23, 914. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto-Furusho, J.K.; Mendivil, E.J.; Villeda-Ramirez, M.A.; Fonseca-Camarillo, G.; Barreto-Zuniga, R. Gene expression of carnitine organic cation transporters 1 and 2 (OCTN) is downregulated in patients with ulcerative colitis. Inflamm. Bowel Dis. 2011, 17, 2205–2206. [Google Scholar] [CrossRef] [PubMed]
- Rioux, J.D.; Silverberg, M.S.; Daly, M.J.; Steinhart, A.H.; McLeod, R.S.; Griffiths, A.M.; Green, T.; Brettin, T.S.; Stone, V.; Bull, S.B.; et al. Genomewide search in Canadian families with inflammatory bowel disease reveals two novel susceptibility loci. Am. J. Hum. Genet. 2000, 66, 1863–1870. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Jung, E.S.; Kong, K.A.; Park, E.M.; Cheon, J.H.; Choi, J.H. Identification of OCTN2 variants and their association with phenotypes of Crohn’s disease in a Korean population. Sci. Rep. 2016, 6, 22887. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.R.; Richbart, S.D.; Merritt, J.C.; Brown, K.C.; Nolan, N.A.; Akers, A.T.; Lau, J.K.; Robateau, Z.R.; Miles, S.L.; Dasgupta, P. Acetylcholine signaling system in progression of lung cancers. Pharmacol. Ther. 2019, 194, 222–254. [Google Scholar] [CrossRef]
- Shibbani, K.; Fahed, A.C.; Al-Shaar, L.; Arabi, M.; Nemer, G.; Bitar, F.; Majdalani, M. Primary carnitine deficiency: Novel mutations and insights into the cardiac phenotype. Clin. Genet. 2014, 85, 127–137. [Google Scholar] [CrossRef]
- Nezu, J.; Tamai, I.; Oku, A.; Ohashi, R.; Yabuuchi, H.; Hashimoto, N.; Nikaido, H.; Sai, Y.; Koizumi, A.; Shoji, Y.; et al. Primary systemic carnitine deficiency is caused by mutations in a gene encoding sodium ion-dependent carnitine transporter. Nat. Genet. 1999, 21, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Stanley, C.A. Carnitine deficiency disorders in children. Ann. N. Y. Acad. Sci. 2004, 1033, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Frigeni, M.; Balakrishnan, B.; Yin, X.; Calderon, F.R.O.; Mao, R.; Pasquali, M.; Longo, N. Functional and molecular studies in primary carnitine deficiency. Hum. Mutat. 2017, 38, 1684–1699. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.L.; Ganapathy, V.; Wu, X.; Hui, J.; Seth, P.; Yuen, P.M.; Wanders, R.J.; Fok, T.F.; Hjelm, N.M. Mutations of OCTN2, an organic cation/carnitine transporter, lead to deficient cellular carnitine uptake in primary carnitine deficiency. Hum. Mol. Genet. 1999, 8, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Tokuhiro, S.; Yamada, R.; Chang, X.; Suzuki, A.; Kochi, Y.; Sawada, T.; Suzuki, M.; Nagasaki, M.; Ohtsuki, M.; Ono, M.; et al. An intronic SNP in a RUNX1 binding site of SLC22A4, encoding an organic cation transporter, is associated with rheumatoid arthritis. Nat. Genet. 2003, 35, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Rioux, J.D.; Daly, M.J.; Silverberg, M.S.; Lindblad, K.; Steinhart, H.; Cohen, Z.; Delmonte, T.; Kocher, K.; Miller, K.; Guschwan, S.; et al. Genetic variation in the 5q31 cytokine gene cluster confers susceptibility to Crohn disease. Nat. Genet. 2001, 29, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Peltekova, V.D.; Wintle, R.F.; Rubin, L.A.; Amos, C.I.; Huang, Q.; Gu, X.; Newman, B.; Van Oene, M.; Cescon, D.; Greenberg, G.; et al. Functional variants of OCTN cation transporter genes are associated with Crohn disease. Nat. Genet. 2004, 36, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, X.; Yang, H.; Wu, D.; Wang, L.; Qian, J. Contribution of the IBD5 locus to inflammatory bowel disease: A meta-analysis. Hum. Genet. 2011, 129, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Pochini, L.; Scalise, M.; Galluccio, M.; Pani, G.; Siminovitch, K.A.; Indiveri, C. The human OCTN1 (SLC22A4) reconstituted in liposomes catalyzes acetylcholine transport which is defective in the mutant L503F associated to the Crohn’s disease. Biochim. Biophys. Acta 2012, 1818, 559–565. [Google Scholar] [CrossRef]
- Wagner, J.; Sim, W.H.; Ellis, J.A.; Ong, E.K.; Catto-Smith, A.G.; Cameron, D.J.; Bishop, R.F.; Kirkwood, C.D. Interaction of Crohn’s disease susceptibility genes in an Australian paediatric cohort. PLoS ONE 2010, 5, e15376. [Google Scholar] [CrossRef]
- Santiago, J.L.; Martinez, A.; de la Calle, H.; Fernandez-Arquero, M.; Figueredo, M.A.; de la Concha, E.G.; Urcelay, E. Evidence for the association of the SLC22A4 and SLC22A5 genes with type 1 diabetes: A case control study. BMC Med. Genet. 2006, 7, 54. [Google Scholar] [CrossRef] [PubMed]
- Klaassen, C.D.; Aleksunes, L.M. Xenobiotic, bile acid, and cholesterol transporters: Function and regulation. Pharmacol. Rev. 2010, 62, 1–96. [Google Scholar] [CrossRef] [PubMed]
- Pochini, L.; Galluccio, M.; Scalise, M.; Console, L.; Indiveri, C. OCTN: A Small Transporter Subfamily with Great Relevance to Human Pathophysiology, Drug Discovery, and Diagnostics. SLAS Discov. 2019, 24, 89–110. [Google Scholar] [CrossRef] [PubMed]
- Rattray, N.J.W.; Trivedi, D.K.; Xu, Y.; Chandola, T.; Johnson, C.H.; Marshall, A.D.; Mekli, K.; Rattray, Z.; Tampubolon, G.; Vanhoutte, B.; et al. Metabolic dysregulation in vitamin E and carnitine shuttle energy mechanisms associate with human frailty. Nat. Commun. 2019, 10, 5027. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Han, D.J.; Kim, B.H.; Yoo, J.; Kim, H.J.; Wu, H.G.; Kim, K.S.; Kim, H.S.; Han, I.; Moon, K.C.; et al. Whole-Genome Sequencing Reveals Mutational Signatures Related to Radiation-Induced Sarcomas and DNA-Damage-Repair Pathways. Mod. Pathol. 2023, 36, 100004. [Google Scholar] [CrossRef] [PubMed]
- Maeda, T.; Hirayama, M.; Kobayashi, D.; Miyazawa, K.; Tamai, I. Mechanism of the regulation of organic cation/carnitine transporter 1 (SLC22A4) by rheumatoid arthritis-associated transcriptional factor RUNX1 and inflammatory cytokines. Drug Metab. Dispos. 2007, 35, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Tahara, H.; Yee, S.W.; Urban, T.J.; Hesselson, S.; Castro, R.A.; Kawamoto, M.; Stryke, D.; Johns, S.J.; Ferrin, T.E.; Kwok, P.Y.; et al. Functional genetic variation in the basal promoter of the organic cation/carnitine transporters OCTN1 (SLC22A4) and OCTN2 (SLC22A5). J. Pharmacol. Exp. Ther. 2009, 329, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.S.; Park, H.J.; Kong, K.A.; Choi, J.H.; Cheon, J.H. Association study between OCTN1 functional haplotypes and Crohn’s disease in a Korean population. Korean J. Physiol. Pharmacol. 2017, 21, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Angelini, S.; Soverini, S.; Ravegnini, G.; Barnett, M.; Turrini, E.; Thornquist, M.; Pane, F.; Hughes, T.P.; White, D.L.; Radich, J.; et al. Association between imatinib transporters and metabolizing enzymes genotype and response in newly diagnosed chronic myeloid leukemia patients receiving imatinib therapy. Haematologica 2013, 98, 193–200. [Google Scholar] [CrossRef]
- Machova Polakova, K.; Albeer, A.; Polivkova, V.; Krutska, M.; Vlcanova, K.; Curik, N.; Fabarius, A.; Klamova, H.; Spiess, B.; Waller, C.F.; et al. The SNP rs460089 in the gene promoter of the drug transporter OCTN1 has prognostic value for treatment-free remission in chronic myeloid leukemia patients treated with imatinib. Leukemia 2024, 38, 318–325. [Google Scholar] [CrossRef]
- Fishilevich, S.; Nudel, R.; Rappaport, N.; Hadar, R.; Plaschkes, I.; Iny Stein, T.; Rosen, N.; Kohn, A.; Twik, M.; Safran, M.; et al. GeneHancer: Genome-wide integration of enhancers and target genes in GeneCards. Database 2017, 2017, bax028. [Google Scholar] [CrossRef] [PubMed]
- Rauluseviciute, I.; Riudavets-Puig, R.; Blanc-Mathieu, R.; Castro-Mondragon, J.A.; Ferenc, K.; Kumar, V.; Lemma, R.B.; Lucas, J.; Cheneby, J.; Baranasic, D.; et al. JASPAR 2024: 20th anniversary of the open-access database of transcription factor binding profiles. Nucleic Acids Res. 2024, 52, D174–D182. [Google Scholar] [CrossRef] [PubMed]
- Tamai, I.; Yabuuchi, H.; Nezu, J.; Sai, Y.; Oku, A.; Shimane, M.; Tsuji, A. Cloning and characterization of a novel human pH-dependent organic cation transporter, OCTN1. FEBS Lett. 1997, 419, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Liao, B.; Wang, J.; Yuan, Y.; Luo, H.; Ouyang, X. Biological roles of SLC16A1-AS1 lncRNA and its clinical impacts in tumors. Cancer Cell Int. 2024, 24, 122. [Google Scholar] [CrossRef] [PubMed]
- Magdy, T.; Jouni, M.; Kuo, H.H.; Weddle, C.J.; Lyra-Leite, D.; Fonoudi, H.; Romero-Tejeda, M.; Gharib, M.; Javed, H.; Fajardo, G.; et al. Identification of Drug Transporter Genomic Variants and Inhibitors That Protect Against Doxorubicin-Induced Cardiotoxicity. Circulation 2022, 145, 279–294. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, D.; Aizawa, S.; Maeda, T.; Tsuboi, I.; Yabuuchi, H.; Nezu, J.; Tsuji, A.; Tamai, I. Expression of organic cation transporter OCTN1 in hematopoietic cells during erythroid differentiation. Exp. Hematol. 2004, 32, 1156–1162. [Google Scholar] [CrossRef] [PubMed]
- Longo, N. Primary Carnitine Deficiency and Newborn Screening for Disorders of the Carnitine Cycle. Ann. Nutr. Metab. 2016, 68 (Suppl. S3), 5–9. [Google Scholar] [CrossRef]
- Koleske, M.L.; McInnes, G.; Brown, J.E.H.; Thomas, N.; Hutchinson, K.; Chin, M.Y.; Koehl, A.; Arkin, M.R.; Schlessinger, A.; Gallagher, R.C.; et al. Functional genomics of OCTN2 variants informs protein-specific variant effect predictor for Carnitine Transporter Deficiency. Proc. Natl. Acad. Sci. USA 2022, 119, e2210247119. [Google Scholar] [CrossRef]
- Tamai, I.; Ohashi, R.; Nezu, J.; Yabuuchi, H.; Oku, A.; Shimane, M.; Sai, Y.; Tsuji, A. Molecular and functional identification of sodium ion-dependent, high affinity human carnitine transporter OCTN2. J. Biol. Chem. 1998, 273, 20378–20382. [Google Scholar] [CrossRef]
- Maekawa, S.; Mori, D.; Nishiya, T.; Takikawa, O.; Horinouchi, T.; Nishimoto, A.; Kajita, E.; Miwa, S. OCTN2VT, a splice variant of OCTN2, does not transport carnitine because of the retention in the endoplasmic reticulum caused by insertion of 24 amino acids in the first extracellular loop of OCTN2. Biochim. Biophys. Acta 2007, 1773, 1000–1006. [Google Scholar] [CrossRef]
- Pochini, L.; Scalise, M.; Galluccio, M.; Indiveri, C. OCTN cation transporters in health and disease: Role as drug targets and assay development. J. Biomol. Screen. 2013, 18, 851–867. [Google Scholar] [CrossRef] [PubMed]
- Ganapathy, M.E.; Huang, W.; Rajan, D.P.; Carter, A.L.; Sugawara, M.; Iseki, K.; Leibach, F.H.; Ganapathy, V. beta-lactam antibiotics as substrates for OCTN2, an organic cation/carnitine transporter. J. Biol. Chem. 2000, 275, 1699–1707. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, S.; Okamura, N.; Sakamoto, S.; Hasegawa, H.; Norikura, R.; Kanaoka, E.; Takahashi, K.; Horie, K.; Sakamoto, K.; Baba, T. Role of Na+/L-carnitine transporter (OCTN2) in renal handling of pivaloylcarnitine and valproylcarnitine formed during pivalic acid-containing prodrugs and valproic acid treatment. Drug Metab. Pharmacokinet. 2008, 23, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Nakahara, S.; Arimura, Y.; Saito, K.; Goto, A.; Motoya, S.; Shinomura, Y.; Miyamoto, A.; Imai, K. Association of SLC22A4/5 polymorphisms with steroid responsiveness of inflammatory bowel disease in Japan. Dis. Colon Rectum 2008, 51, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Heintzman, N.D.; Stuart, R.K.; Hon, G.; Fu, Y.; Ching, C.W.; Hawkins, R.D.; Barrera, L.O.; Van Calcar, S.; Qu, C.; Ching, K.A.; et al. Distinct and predictive chromatin signatures of transcriptional promoters and enhancers in the human genome. Nat. Genet. 2007, 39, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Qu, Q.; Qu, J.; Zhan, M.; Wu, L.X.; Zhang, Y.W.; Lou, X.Y.; Fu, L.J.; Zhou, H.H. Different involvement of promoter methylation in the expression of organic cation/carnitine transporter 2 (OCTN2) in cancer cell lines. PLoS ONE 2013, 8, e76474. [Google Scholar] [CrossRef] [PubMed]
- He, R.Z.; Luo, D.X.; Mo, Y.Y. Emerging roles of lncRNAs in the post-transcriptional regulation in cancer. Genes Dis. 2019, 6, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.H.; Shen, W.; Sun, H.; Migawa, M.T.; Vickers, T.A.; Crooke, S.T. Translation efficiency of mRNAs is increased by antisense oligonucleotides targeting upstream open reading frames. Nat. Biotechnol. 2016, 34, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Shu, Y. Transcriptional Regulation of Solute Carrier (SLC) Drug Transporters. Drug Metab. Dispos. 2022, 50, 1238–1250. [Google Scholar] [CrossRef]
- Oscarson, M.; Zanger, U.M.; Rifki, O.F.; Klein, K.; Eichelbaum, M.; Meyer, U.A. Transcriptional profiling of genes induced in the livers of patients treated with carbamazepine. Clin. Pharmacol. Ther. 2006, 80, 440–456. [Google Scholar] [CrossRef]
- Paul, H.S.; Adibi, S.A. Paradoxical effects of clofibrate on liver and muscle metabolism in rats. Induction of myotonia and alteration of fatty acid and glucose oxidation. J. Clin. Investig. 1979, 64, 405–412. [Google Scholar] [CrossRef]
- Luci, S.; Geissler, S.; Konig, B.; Koch, A.; Stangl, G.I.; Hirche, F.; Eder, K. PPARalpha agonists up-regulate organic cation transporters in rat liver cells. Biochem. Biophys. Res. Commun. 2006, 350, 704–708. [Google Scholar] [CrossRef]
- Schoonjans, K.; Peinado-Onsurbe, J.; Lefebvre, A.M.; Heyman, R.A.; Briggs, M.; Deeb, S.; Staels, B.; Auwerx, J. PPARalpha and PPARgamma activators direct a distinct tissue-specific transcriptional response via a PPRE in the lipoprotein lipase gene. EMBO J. 1996, 15, 5336–5348. [Google Scholar] [CrossRef] [PubMed]
- Ringseis, R.; Posel, S.; Hirche, F.; Eder, K. Treatment with pharmacological peroxisome proliferator-activated receptor alpha agonist clofibrate causes upregulation of organic cation transporter 2 in liver and small intestine of rats. Pharmacol. Res. 2007, 56, 175–183. [Google Scholar] [CrossRef]
- van Vlies, N.; Wanders, R.J.; Vaz, F.M. Measurement of carnitine biosynthesis enzyme activities by tandem mass spectrometry: Differences between the mouse and the rat. Anal. Biochem. 2006, 354, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Ringseis, R.; Luci, S.; Spielmann, J.; Kluge, H.; Fischer, M.; Geissler, S.; Wen, G.; Hirche, F.; Eder, K. Clofibrate treatment up-regulates novel organic cation transporter (OCTN)-2 in tissues of pigs as a model of non-proliferating species. Eur. J. Pharmacol. 2008, 583, 11–17. [Google Scholar] [CrossRef]
- D’Argenio, G.; Petillo, O.; Margarucci, S.; Torpedine, A.; Calarco, A.; Koverech, A.; Boccia, A.; Paolella, G.; Peluso, G. Colon OCTN2 gene expression is up-regulated by peroxisome proliferator-activated receptor gamma in humans and mice and contributes to local and systemic carnitine homeostasis. J. Biol. Chem. 2010, 285, 27078–27087. [Google Scholar] [CrossRef] [PubMed]
- Grube, M.; Meyer Zu Schwabedissen, H.; Draber, K.; Prager, D.; Moritz, K.U.; Linnemann, K.; Fusch, C.; Jedlitschky, G.; Kroemer, H.K. Expression, localization, and function of the carnitine transporter octn2 (slc22a5) in human placenta. Drug Metab. Dispos. 2005, 33, 31–37. [Google Scholar] [CrossRef]
- Huang, F.D.; Kung, F.L.; Tseng, Y.C.; Chen, M.R.; Chan, H.S.; Lin, C.J. Regulation of protein expression and function of octn2 in forskolin-induced syncytialization in BeWo Cells. Placenta 2009, 30, 187–194. [Google Scholar] [CrossRef]
- Chang, T.T.; Shyu, M.K.; Huang, M.C.; Hsu, C.C.; Yeh, S.Y.; Chen, M.R.; Lin, C.J. Hypoxia-mediated down-regulation of OCTN2 and PPARalpha expression in human placentas and in BeWo cells. Mol. Pharm. 2011, 8, 117–125. [Google Scholar] [CrossRef]
- Eder, K.; Ringseis, R. The role of peroxisome proliferator-activated receptor alpha in transcriptional regulation of novel organic cation transporters. Eur. J. Pharmacol. 2010, 628, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Fink, M.A.; Paland, H.; Herzog, S.; Grube, M.; Vogelgesang, S.; Weitmann, K.; Bialke, A.; Hoffmann, W.; Rauch, B.H.; Schroeder, H.W.S.; et al. L-Carnitine-Mediated Tumor Cell Protection and Poor Patient Survival Associated with OCTN2 Overexpression in Glioblastoma Multiforme. Clin. Cancer Res. 2019, 25, 2874–2886. [Google Scholar] [CrossRef] [PubMed]
- Elsnerova, K.; Mohelnikova-Duchonova, B.; Cerovska, E.; Ehrlichova, M.; Gut, I.; Rob, L.; Skapa, P.; Hruda, M.; Bartakova, A.; Bouda, J.; et al. Gene expression of membrane transporters: Importance for prognosis and progression of ovarian carcinoma. Oncol. Rep. 2016, 35, 2159–2170. [Google Scholar] [CrossRef] [PubMed]
- Scalise, M.; Galluccio, M.; Accardi, R.; Cornet, I.; Tommasino, M.; Indiveri, C. Human OCTN2 (SLC22A5) is down-regulated in virus- and nonvirus-mediated cancer. Cell Biochem. Funct. 2012, 30, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Uray, I.P.; Mazumdar, A.; Mayer, J.A.; Brown, P.H. SLC22A5/OCTN2 expression in breast cancer is induced by estrogen via a novel intronic estrogen-response element (ERE). Breast Cancer Res. Treat. 2012, 134, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Papierniak-Wygladala, A.; Lamch, W.; Jurewicz, E.; Nalecz, K.A. The activity and surface presence of organic cation/carnitine transporter OCTN2 (SLC22A5) in breast cancer cells depends on AKT kinase. Arch. Biochem. Biophys. 2023, 742, 109616. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.; Okubo, H.; Morishige, J.I.; Xu, P.; Hasan, N.; Nagata, N.; Ando, H. Lenvatinib causes reduced expression of carnitine/organic cation transporter 2 and carnitine deficiency in the skeletal muscle of rats. Toxicol. Lett. 2022, 366, 17–25. [Google Scholar] [CrossRef]
- Juraszek, B.; Nalecz, K.A. SLC22A5 (OCTN2) Carnitine Transporter-Indispensable for Cell Metabolism, a Jekyll and Hyde of Human Cancer. Molecules 2019, 25, 14. [Google Scholar] [CrossRef]
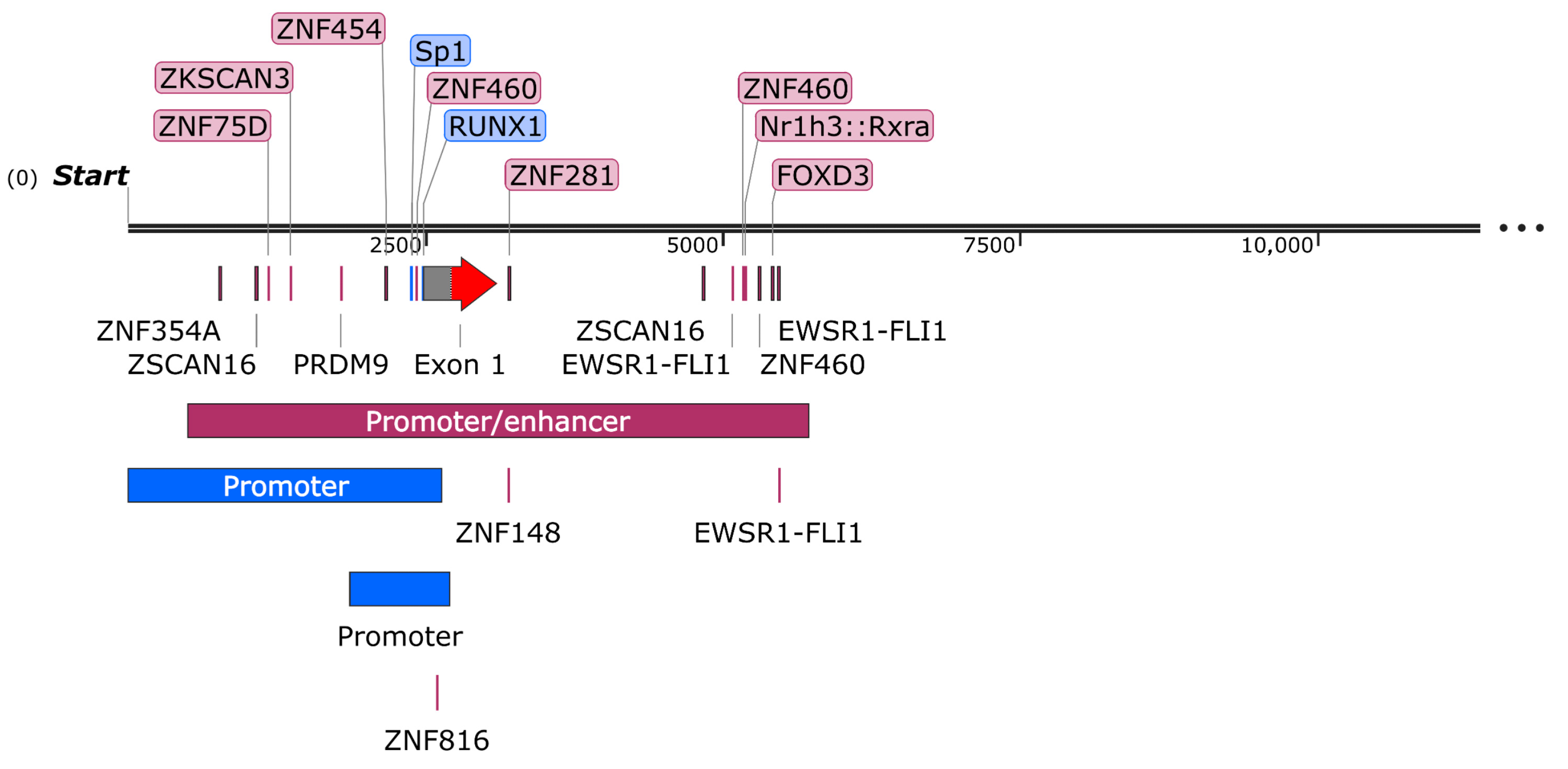
| Transcription Factor | JASPAR Score | Genomic Position | Binding Site Size |
|---|---|---|---|
| ZNF354A | 637 | chr5:132292671-132292690 | 20 |
| ZSCAN16 | 670 602 | chr5:132292976-132292993 chr5:132296737-132296754 | 18 |
| ZNF75D | 607 | chr5:132293083-132293094 | 12 |
| ZKSCAN3 | 608 | chr5:132293266-132293279 | 14 |
| PRDM9 | 657 | chr5:132293697-132293716 | 20 |
| ZNF454 | 636 | chr5:132294069-132294085 | 17 |
| ZNF460 | 668 621 745 | chr5:132294326-132294341 chr5:132297073-132297088 chr5:132297208-132297223 | 16 |
| ZNF816 | 605 | chr5:132294499-132294513 | 15 |
| ZNF281 | 602 | chr5:132295107-132295116 | 10 |
| ZNF148 | 602 | chr5:132295107-132295116 | 10 |
| EWSR1-FLI1 | 628 616 728 | chr5:132296985-132297002 chr5:132297372-132297389 chr5:132297376-132297393 | 18 |
| Nr1h3::Rxra | 603 | chr5:132297093-132297108 | 16 |
| FOXD3 | 602 | chr5:132297318-132297331 | 14 |
| Gene Symbol | Database | Transcript | Length (nt) |
|---|---|---|---|
| SLC22A4 | NCBI/Gene | NM_003059.3 | 2234 |
| SLC22A4 | NCBI/Gene | XM_006714675.5 | 2130 |
| SLC22A4 | NCBI/Gene | XM_011543589.3 | 1958 |
| SLC22A4 | NCBI/Gene | XM_047417594.1 | 1788 |
| SLC22A4 | NCBI/Gene | XM_017009776.2 | 1821 |
| SLC22A4 | Ensembl | ENST00000491257.1 | 564 |
| SLC22A4 | Ensembl | ENST00000425923.1 | 463 |
| Transcription Factor | JASPAR Score | Genomic Position | Binding Site Size |
|---|---|---|---|
| ZNF460 | 776 | chr5:132368308-132368323 | 16 |
| ZBED4 | 602 | chr5:132369676-132369685 | 10 |
| ZNF93 | 633 | chr5:132370212-132370225 | 14 |
| PATZ1 | 614 | chr5:132370470-132370480 | 11 |
| ZNF281 | 602 | chr5:132370471-132370480 | 10 |
| ZNF148 | 602 | chr5:132370471-132370480 | 10 |
| Nr2F6 | 600 | chr5:132371186-132371200 | 15 |
| PPARA::RXRA | 717 | chr5:132372636-132372652 | 17 |
| Gene Symbol | Database | Transcript | Trasncript Length (nt) | Protein Length (aa) |
|---|---|---|---|---|
| SLC22A5 | NCBI/Gene | NM_001308122.2 | 3349 | 581 |
| SLC22A5 | NCBI/Gene | NM_003060.4 | 3277 | 557 |
| SLC22A5 | NCBI/Gene | XM_017009778.3 | 1570 | 381 |
| SLC22A5 | NCBI/Gene | XM_047417595.1 | 1788 | 374 |
| SLC22A5 | NCBI/Gene | XM_047417596.1 | 8198 | 353 |
| SLC22A5 | NCBI/Gene | XM_011543590.3 | 2495 | 351 |
| SLC22A5 | NCBI/Gene | XM_047417597.1 | 1295 | 308 |
| SLC22A5 | NCBI/Gene | XM_047417598.1 | 1289 | 306 |
| SLC22A5 | Ensembl | ENST00000693308.1 | 3146 | 573 |
| SLC22A5 | Ensembl | ENST00000692413.1 | 3080 | 551 |
| SLC22A5 | Ensembl | ENST00000689271.1 | 2945 | 506 |
| SLC22A5 | Ensembl | ENST00000415928.6 | 1873 | 431 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galluccio, M.; Tripicchio, M.; Pochini, L. The Human OCTN Sub-Family: Gene and Protein Structure, Expression, and Regulation. Int. J. Mol. Sci. 2024, 25, 8743. https://doi.org/10.3390/ijms25168743
Galluccio M, Tripicchio M, Pochini L. The Human OCTN Sub-Family: Gene and Protein Structure, Expression, and Regulation. International Journal of Molecular Sciences. 2024; 25(16):8743. https://doi.org/10.3390/ijms25168743
Chicago/Turabian StyleGalluccio, Michele, Martina Tripicchio, and Lorena Pochini. 2024. "The Human OCTN Sub-Family: Gene and Protein Structure, Expression, and Regulation" International Journal of Molecular Sciences 25, no. 16: 8743. https://doi.org/10.3390/ijms25168743
APA StyleGalluccio, M., Tripicchio, M., & Pochini, L. (2024). The Human OCTN Sub-Family: Gene and Protein Structure, Expression, and Regulation. International Journal of Molecular Sciences, 25(16), 8743. https://doi.org/10.3390/ijms25168743








