Dipeptidyl Peptidase (DPP)-4 Inhibitors and Pituitary Adenylate Cyclase-Activating Polypeptide, a DPP-4 Substrate, Extend Neurite Outgrowth of Mouse Dorsal Root Ganglia Neurons: A Promising Approach in Diabetic Polyneuropathy Treatment
Abstract
1. Introduction
2. Results
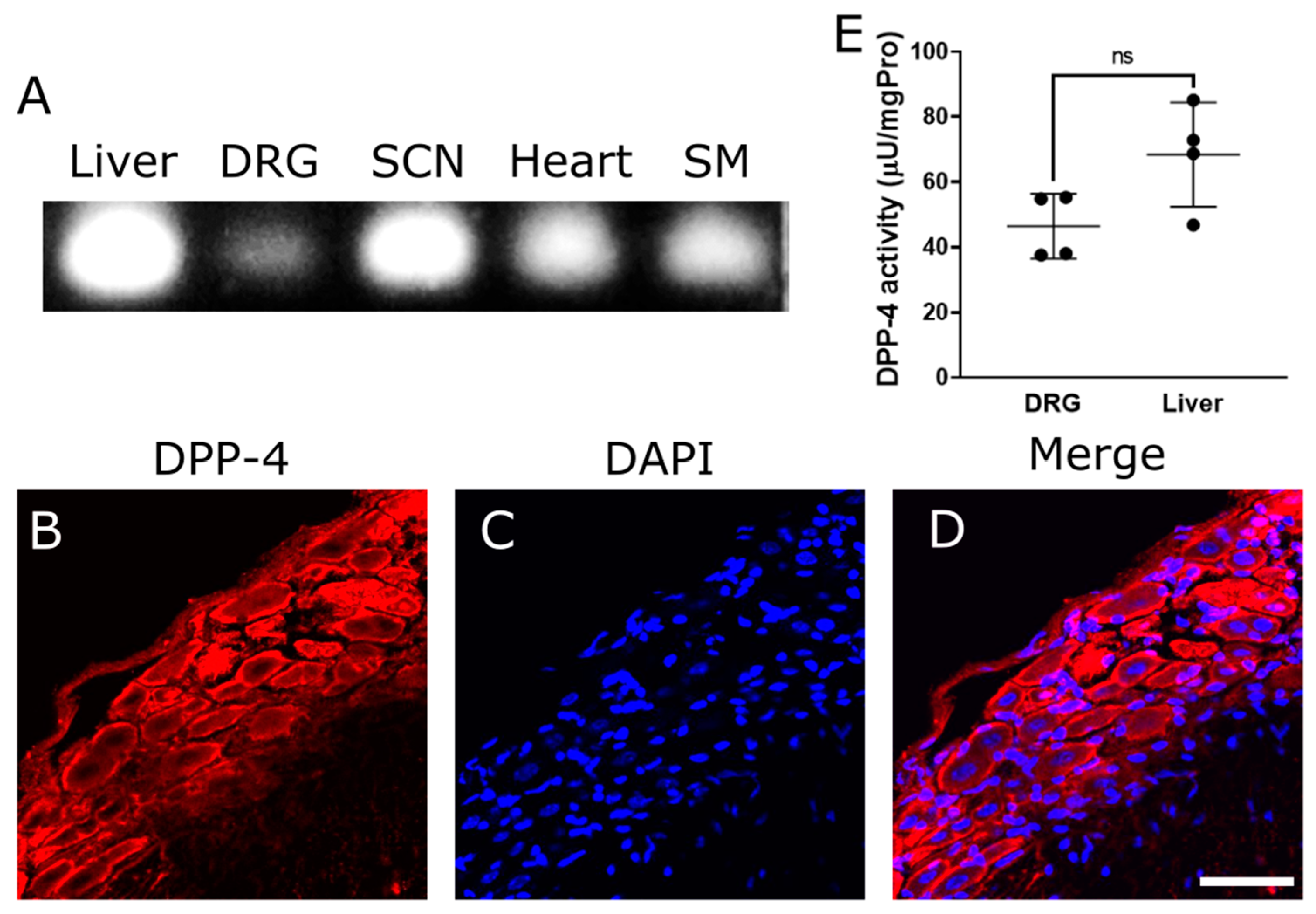
2.1. DPP-4 Expresses in Dorsal Root Ganglia (DRG)
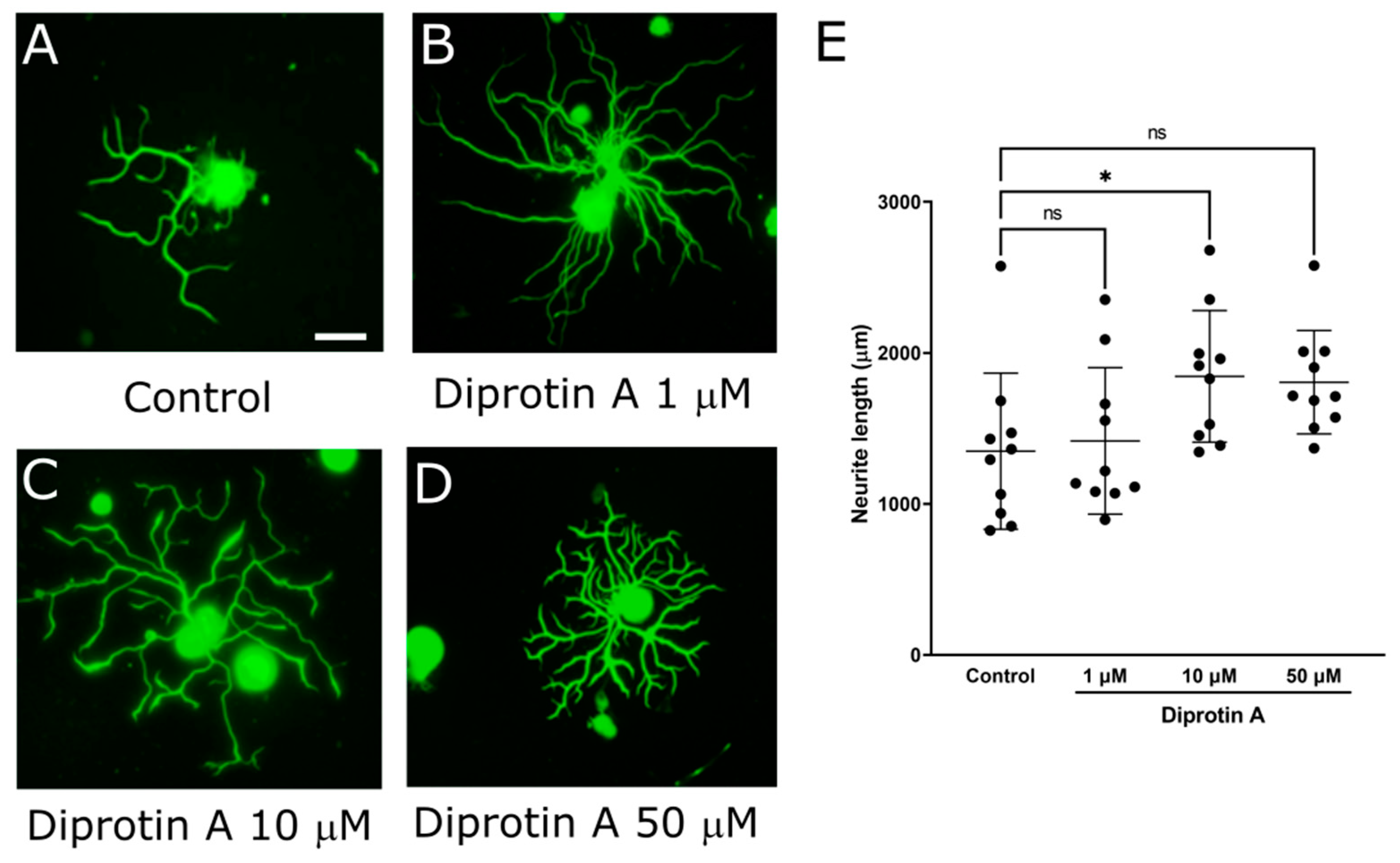
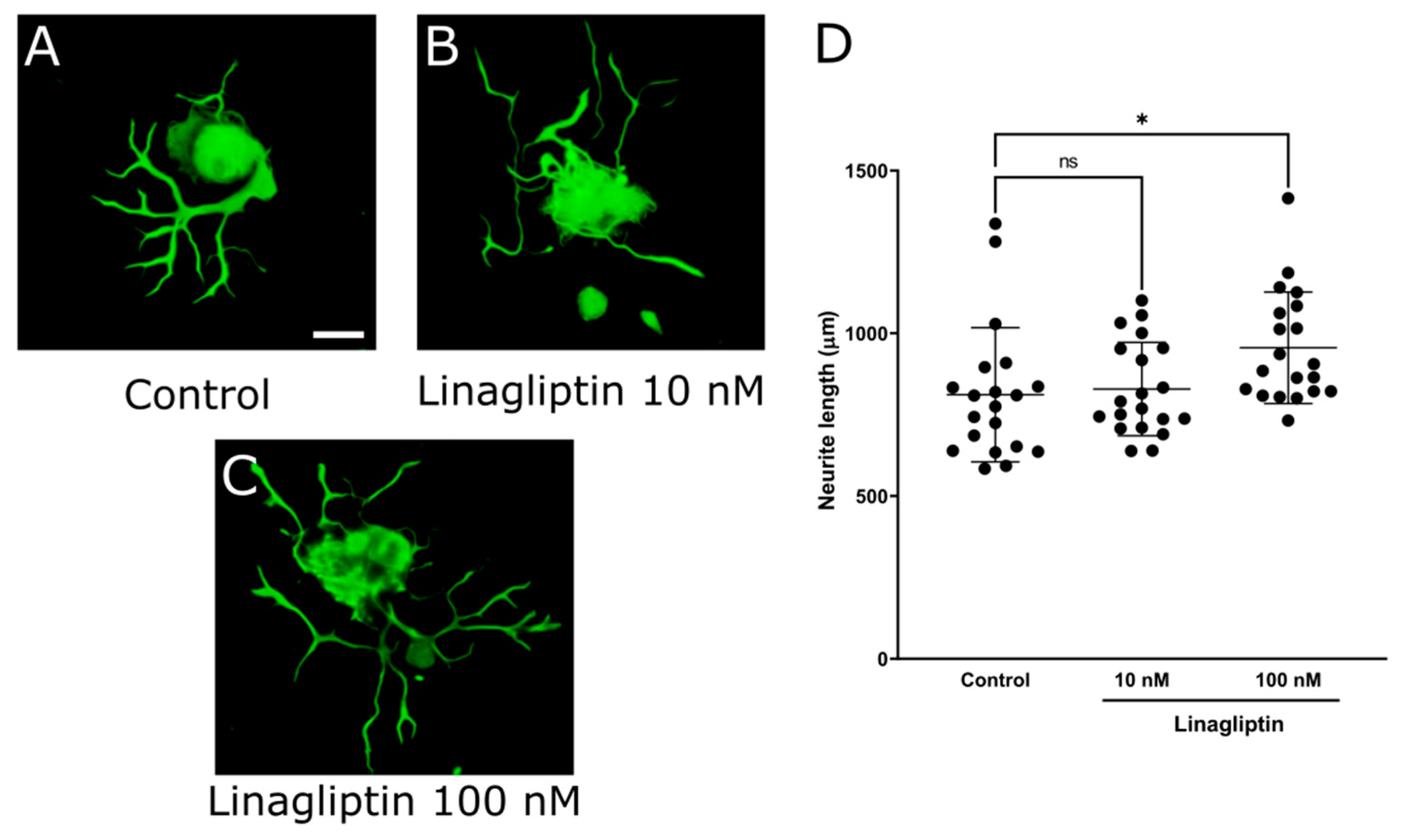
2.2. DPP-4 Inhibitors Promoted Neurite Outgrowth of DRG Primary Neurons
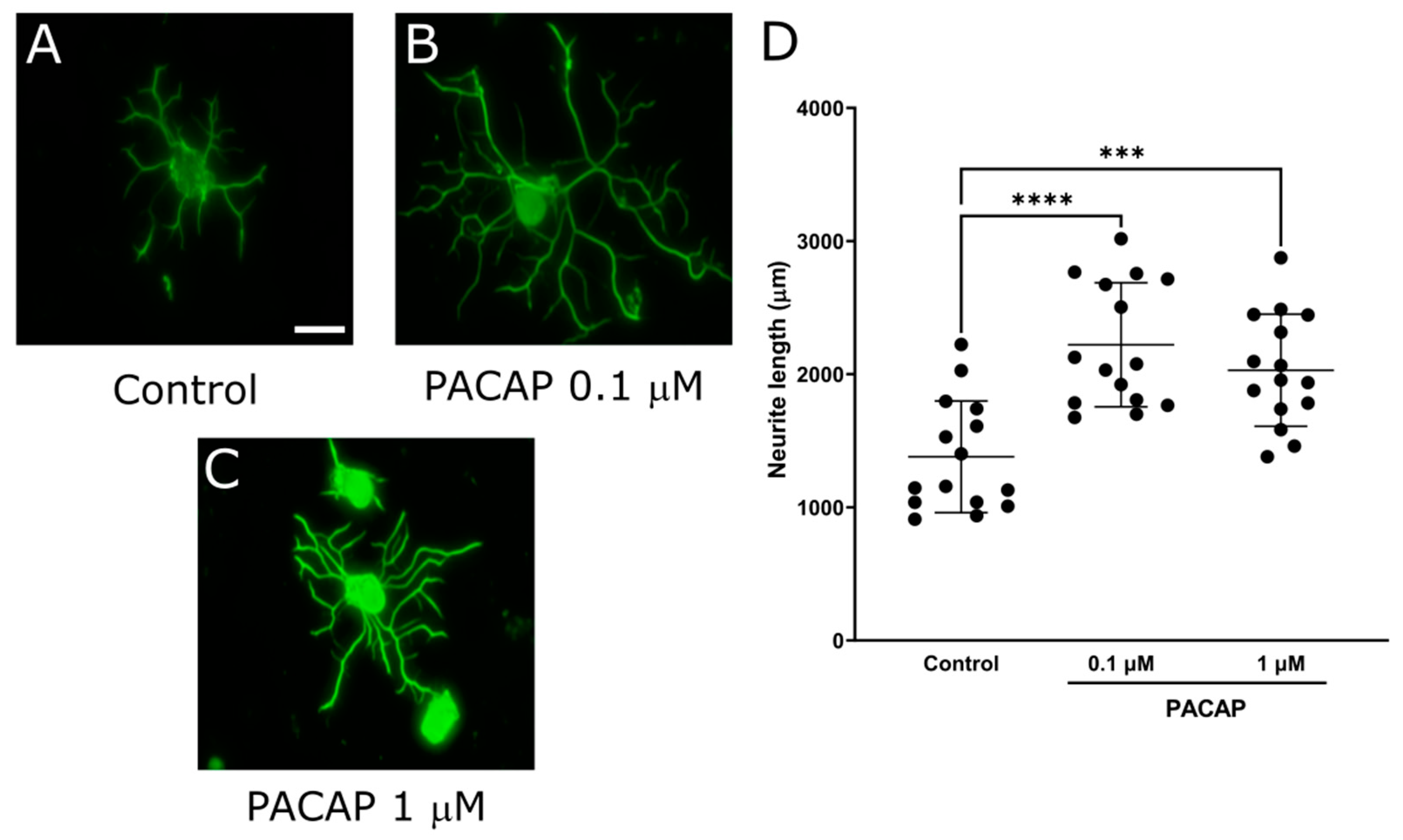
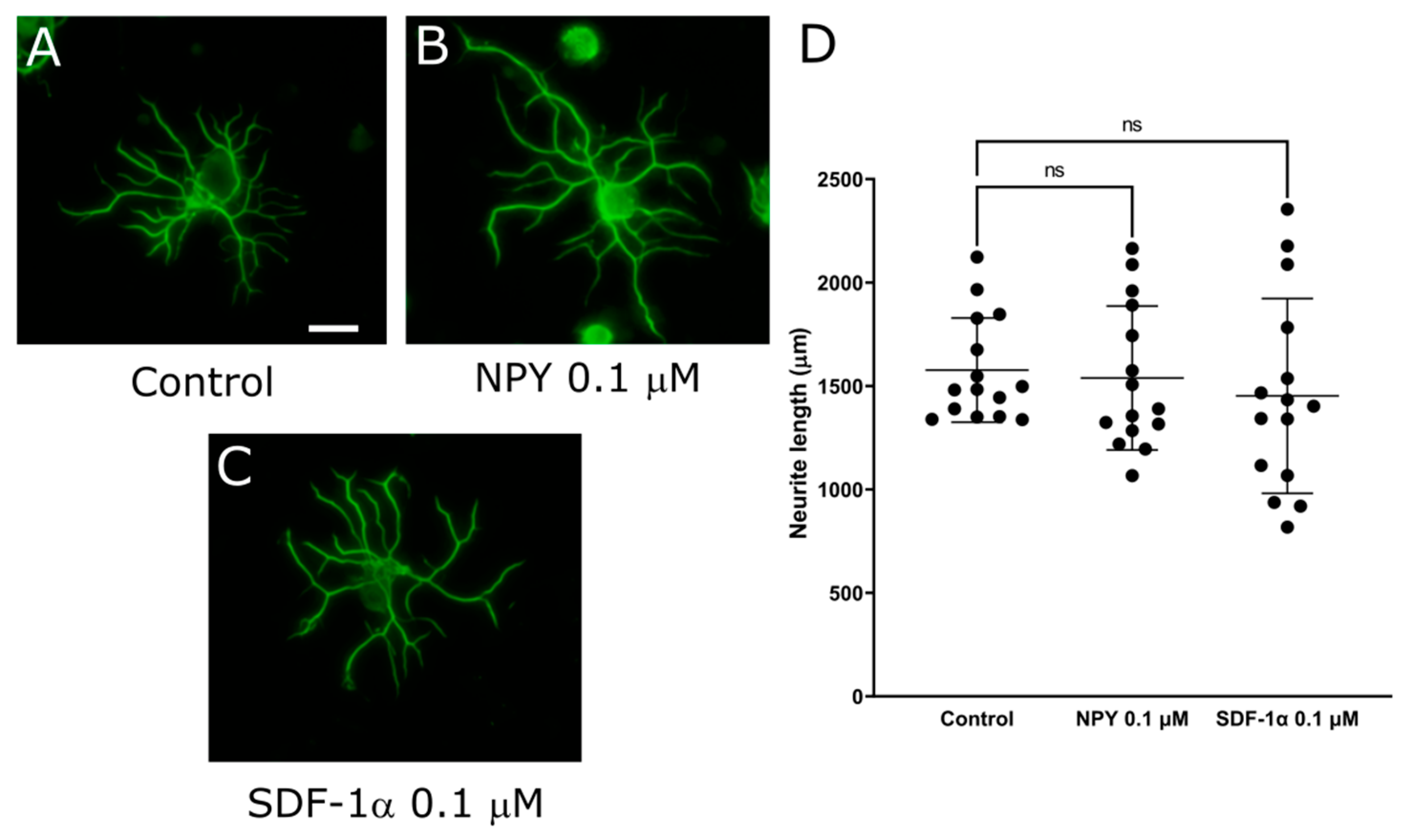
2.3. PACAP, DPP-4 Substrate, Promoted Neurite Outgrowth of DRG Primary Neurons
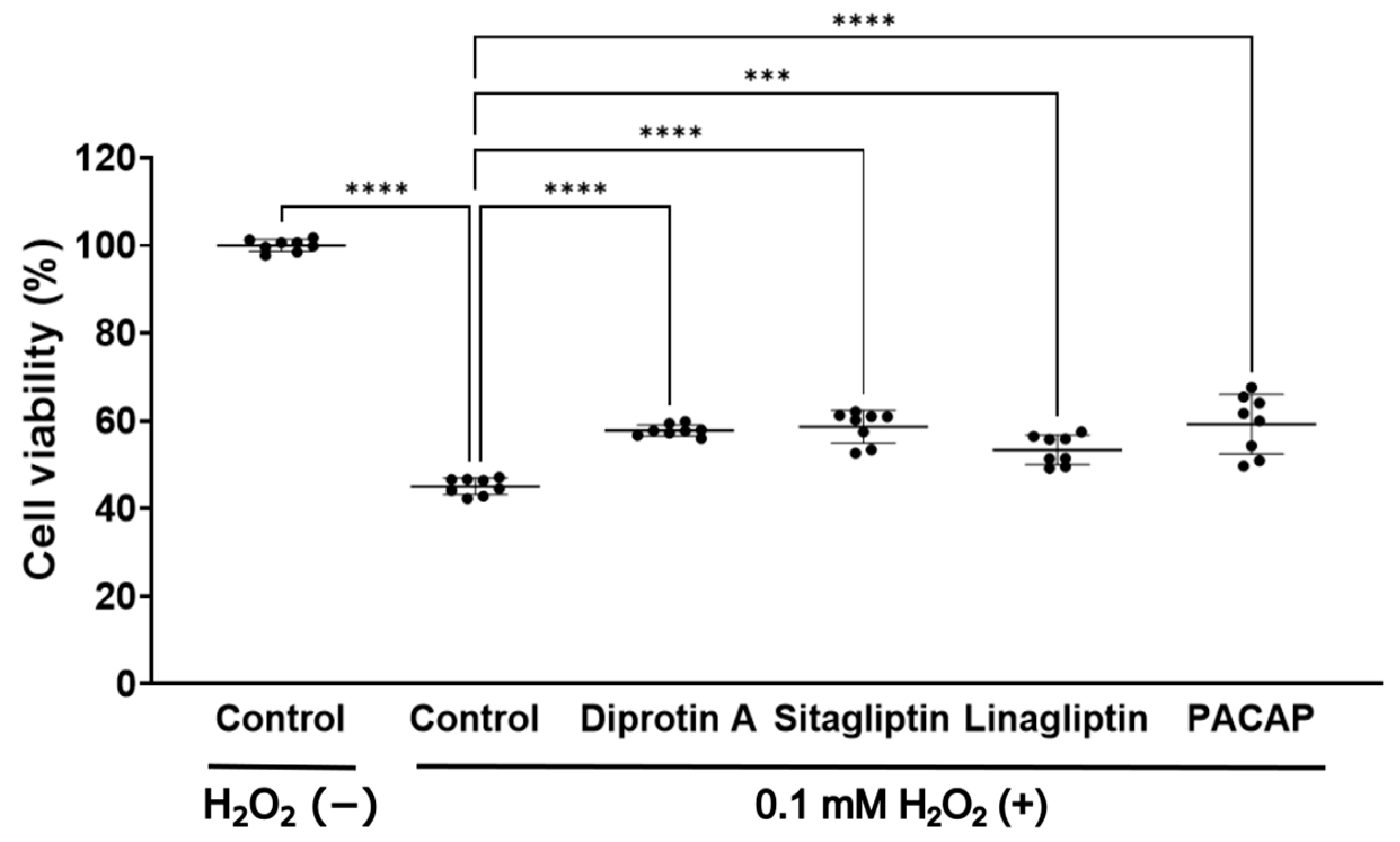
2.4. DPP-4 Inhibitors and PACAP Enhanced Cell Viability in 50B11 Cells, DRG Neuronal Cells
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Primary Culture of Dorsal Root Ganglion (DRG) Neurons and Evaluation of Neurite Outgrowth
4.3. DPP-4 mRNA Expression in DRG and Sciatic Nerves
4.4. Immunocytochemistry and Frozen Section Staining
4.5. DPP-4 Activity
4.6. MTT Assay
4.7. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dyck, P.J.; Kratz, K.M.; Karnes, J.L.; Litchy, W.J.; Klein, R.; Pach, J.M.; Wilson, D.M.; O’Brien, P.C.; Melton, L.J., 3rd; Service, F.J. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: The Rochester Diabetic Neuropathy Study. Neurology 1993, 43, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.J.; Asbury, A.K. Diabetic neuropathy. Ann. Neurol. 1984, 15, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Zochodne, D.W. Diabetic neuropathies: Features and mechanisms. Brain Pathol. 1999, 9, 369–391. [Google Scholar] [CrossRef] [PubMed]
- Toth, C.; Brussee, V.; Cheng, C.; Zochodne, D.W. Diabetes mellitus and the sensory neuron. J. Neuropathol. Exp. Neurol. 2004, 63, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, W.R.; Wendelschafer-Crabb, G.; Johnson, T. Quantitation of epidermal nerves in diabetic neuropathy. Neurology 1996, 47, 1042–1048. [Google Scholar] [CrossRef]
- Sullivan, K.A.; Hayes, J.M.; Wiggin, T.D.; Backus, C.; Su Oh, S.; Lentz, S.I.; Brosius, F., 3rd; Feldman, E.L. Mouse models of diabetic neuropathy. Neurobiol. Dis. 2007, 28, 276–285. [Google Scholar] [CrossRef]
- Johnson, M.S.; Ryals, J.M.; Wright, D.E. Early loss of peptidergic intraepidermal nerve fibers in an STZ-induced mouse model of insensate diabetic neuropathy. Pain 2008, 140, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Lennertz, R.C.; Medler, K.A.; Bain, J.L.; Wright, D.E.; Stucky, C.L. Impaired sensory nerve function and axon morphology in mice with diabetic neuropathy. J. Neurophysiol. 2011, 106, 905–914. [Google Scholar] [CrossRef]
- Zochodne, D.W. Diabetes mellitus and the peripheral nervous system: Manifestations and mechanisms. Muscle Nerve 2007, 36, 144–166. [Google Scholar] [CrossRef]
- Javed, S.; Petropoulos, I.N.; Alam, U.; Malik, R.A. Treatment of painful diabetic neuropathy. Ther. Adv. Chronic Dis. 2015, 6, 15–28. [Google Scholar] [CrossRef]
- Todorovic, S.M. Is Diabetic Nerve Pain Caused by Dysregulated Ion Channels in Sensory Neurons? Diabetes 2015, 64, 3987–3989. [Google Scholar] [CrossRef]
- Singh, R.; Kishore, L.; Kaur, N. Diabetic peripheral neuropathy: Current perspective and future directions. Pharmacol. Res. 2014, 80, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Farmer, K.L.; Li, C.; Dobrowsky, R.T. Diabetic peripheral neuropathy: Should a chaperone accompany our therapeutic approach? Pharmacol. Rev. 2012, 64, 880–900. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Zhou, S. Inflammation: Therapeutic targets for diabetic neuropathy. Mol. Neurobiol. 2014, 49, 536–546. [Google Scholar] [CrossRef]
- Kobayashi, M.; Zochodne, D.W. Diabetic neuropathy and the sensory neuron: New aspects of pathogenesis and their treatment implications. J. Diabetes Investig. 2018, 9, 1239–1254. [Google Scholar] [CrossRef]
- Kles, K.A.; Vinik, A.I. Pathophysiology and treatment of diabetic peripheral neuropathy: The case for diabetic neurovascular function as an essential component. Curr. Diabetes Rev. 2006, 2, 131–145. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Li, K.; Chen, Y.; Xie, J.; Wu, C.; Cui, C.; Deng, B. Oxidative Stress in Diabetic Peripheral Neuropathy: Pathway and Mechanism-Based Treatment. Mol. Neurobiol. 2023, 60, 4574–4594. [Google Scholar] [CrossRef]
- Estall, J.L.; Drucker, D.J. Glucagon and glucagon-like peptide receptors as drug targets. Curr. Pharm. Des. 2006, 12, 1731–1750. [Google Scholar] [CrossRef]
- Drucker, D.J.; Nauck, M.A. The incretin system: Glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 2006, 368, 1696–1705. [Google Scholar] [CrossRef]
- Lovshin, J.A.; Drucker, D.J. Incretin-based therapies for type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2009, 5, 262–269. [Google Scholar] [CrossRef]
- Green, B.D.; Flatt, P.R.; Bailey, C.J. Dipeptidyl peptidase IV (DPP IV) inhibitors: A newly emerging drug class for the treatment of type 2 diabetes. Diabetes Vasc. Dis. Res. 2006, 3, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Sebokova, E.; Christ, A.D.; Boehringer, M.; Mizrahi, J. Dipeptidyl peptidase IV inhibitors: The next generation of new promising therapies for the management of type 2 diabetes. Curr. Top. Med. Chem. 2007, 7, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Singhal, S.; Manikrao Patil, V.; Verma, S.; Masand, N. Recent advances and structure-activity relationship studies of DPP-4 inhibitors as anti-diabetic agents. Bioorg. Chem. 2024, 146, 107277. [Google Scholar] [CrossRef] [PubMed]
- Barreira da Silva, R.; Laird, M.E.; Yatim, N.; Fiette, L.; Ingersoll, M.A.; Albert, M.L. Dipeptidylpeptidase 4 inhibition enhances lymphocyte trafficking, improving both naturally occurring tumor immunity and immunotherapy. Nat. Immunol. 2015, 16, 850–858. [Google Scholar] [CrossRef] [PubMed]
- Shah, Z.; Kampfrath, T.; Deiuliis, J.A.; Zhong, J.; Pineda, C.; Ying, Z.; Xu, X.; Lu, B.; Moffatt-Bruce, S.; Durairaj, R.; et al. Long-term dipeptidyl-peptidase 4 inhibition reduces atherosclerosis and inflammation via effects on monocyte recruitment and chemotaxis. Circulation 2011, 124, 2338–2349. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Rao, X.; Deiuliis, J.; Braunstein, Z.; Narula, V.; Hazey, J.; Mikami, D.; Needleman, B.; Satoskar, A.R.; Rajagopalan, S. A potential role for dendritic cell/macrophage-expressing DPP4 in obesity-induced visceral inflammation. Diabetes 2013, 62, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Kanasaki, K.; Shi, S.; Kanasaki, M.; He, J.; Nagai, T.; Nakamura, Y.; Ishigaki, Y.; Kitada, M.; Srivastava, S.P.; Koya, D. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes 2014, 63, 2120–2131. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.; Hasegawa, Y.; Koibuchi, N.; Toyama, K.; Uekawa, K.; Nakagawa, T.; Lin, B.; Kim-Mitsuyama, S. DPP-4 inhibition with linagliptin ameliorates cognitive impairment and brain atrophy induced by transient cerebral ischemia in type 2 diabetic mice. Cardiovasc. Diabetol. 2015, 14, 54. [Google Scholar] [CrossRef] [PubMed]
- Kornelius, E.; Lin, C.L.; Chang, H.H.; Li, H.H.; Huang, W.N.; Yang, Y.S.; Lu, Y.L.; Peng, C.H.; Huang, C.N. DPP-4 Inhibitor Linagliptin Attenuates Aβ-induced Cytotoxicity through Activation of AMPK in Neuronal Cells. CNS Neurosci. Ther. 2015, 21, 549–557. [Google Scholar] [CrossRef]
- Seino, Y.; Yabe, D. Glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1: Incretin actions beyond the pancreas. J. Diabetes Investig. 2013, 4, 108–130. [Google Scholar] [CrossRef]
- Zhu, L.; Tamvakopoulos, C.; Xie, D.; Dragovic, J.; Shen, X.; Fenyk-Melody, J.E.; Schmidt, K.; Bagchi, A.; Griffin, P.R.; Thornberry, N.A.; et al. The role of dipeptidyl peptidase IV in the cleavage of glucagon family peptides: In vivo metabolism of pituitary adenylate cyclase activating polypeptide-(1-38). J. Biol. Chem. 2003, 278, 22418–22423. [Google Scholar] [CrossRef] [PubMed]
- Ahrén, B.; Hughes, T.E. Inhibition of dipeptidyl peptidase-4 augments insulin secretion in response to exogenously administered glucagon-like peptide-1, glucose-dependent insulinotropic polypeptide, pituitary adenylate cyclase-activating polypeptide, and gastrin-releasing peptide in mice. Endocrinology 2005, 146, 2055–2059. [Google Scholar] [CrossRef] [PubMed]
- Green, B.D.; Irwin, N.; Flatt, P.R. Pituitary adenylate cyclase-activating peptide (PACAP): Assessment of dipeptidyl peptidase IV degradation, insulin-releasing activity and antidiabetic potential. Peptides 2006, 27, 1349–1358. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Yu, T.; Lee, D.H. The nonglycemic actions of dipeptidyl peptidase-4 inhibitors. BioMed Res. Int. 2014, 2014, 368703. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, N.; Kolibabka, M.; Busch, S.; Bugert, P.; Kaiser, U.; Lin, J.; Fleming, T.; Morcos, M.; Klein, T.; Schlotterer, A.; et al. The DPP4 Inhibitor Linagliptin Protects from Experimental Diabetic Retinopathy. PLoS ONE 2016, 11, e0167853. [Google Scholar] [CrossRef]
- Avogaro, A.; Fadini, G.P. The pleiotropic cardiovascular effects of dipeptidyl peptidase-4 inhibitors. Br. J. Clin. Pharmacol. 2018, 84, 1686–1695. [Google Scholar] [CrossRef] [PubMed]
- Packer, M. Do DPP-4 Inhibitors Cause Heart Failure Events by Promoting Adrenergically Mediated Cardiotoxicity? Clues From Laboratory Models and Clinical Trials. Circ. Res. 2018, 122, 928–932. [Google Scholar] [CrossRef]
- Arimura, A. Perspectives on pituitary adenylate cyclase activating polypeptide (PACAP) in the neuroendocrine, endocrine, and nervous systems. Jpn J. Physiol. 1998, 48, 301–331. [Google Scholar] [CrossRef]
- Reichmann, F.; Holzer, P. Neuropeptide Y: A stressful review. Neuropeptides 2016, 55, 99–109. [Google Scholar] [CrossRef]
- Zou, Y.R.; Kottmann, A.H.; Kuroda, M.; Taniuchi, I.; Littman, D.R. Function of the chemokine receptor CXCR4 in haematopoiesis and in cerebellar development. Nature 1998, 393, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, Y.; Bito, H.; Furuyashiki, T.; Tsuji, T.; Takemoto-Kimura, S.; Kimura, K.; Nozaki, K.; Hashimoto, N.; Narumiya, S. Control of axon elongation via an SDF-1alpha/Rho/mDia pathway in cultured cerebellar granule neurons. J. Cell Biol. 2003, 161, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.Y.; Liu, W.J.; Park, J.H.; Baek, H.S.; Park, T.S. Effect of dipeptidyl peptidase-IV (DPP-IV) inhibitor (Vildagliptin) on peripheral nerves in streptozotocin-induced diabetic rats. Arch. Med. Res. 2009, 40, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.; Cervellini, I.; Porretta-Serapiglia, C.; Oggioni, N.; Burkey, B.; Ghezzi, P.; Cavaletti, G.; Lauria, G. Beneficial effects of PKF275-055, a novel, selective, orally bioavailable, long-acting dipeptidyl peptidase IV inhibitor in streptozotocin-induced diabetic peripheral neuropathy. J. Pharmacol. Exp. Ther. 2012, 340, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.K.; Sharma, A.; Kumari, R.; Kishore, K.; Sharma, D.; Srinivasan, B.P.; Singh, S.K.; Gaur, S.; Jatav, V.S.; Sharma, P.; et al. Sitagliptin, sitagliptin and metformin, or sitagliptin and amitriptyline attenuate streptozotocin-nicotinamide induced diabetic neuropathy in rats. J. Biomed. Res. 2012, 26, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Avogaro, A.; Fadini, G.P. The effects of dipeptidyl peptidase-4 inhibition on microvascular diabetes complications. Diabetes Care 2014, 37, 2884–2894. [Google Scholar] [CrossRef] [PubMed]
- Rónai, A.Z.; Király, K.; Szebeni, A.; Szemenyei, E.; Prohászka, Z.; Darula, Z.; Tóth, G.; Till, I.; Szalay, B.; Kató, E.; et al. Immunoreactive endomorphin 2 is generated extracellularly in rat isolated L4,5 dorsal root ganglia by DPP-IV. Regul. Pept. 2009, 157, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Mohiuddin, M.S.; Himeno, T.; Inoue, R.; Miura-Yura, E.; Yamada, Y.; Nakai-Shimoda, H.; Asano, S.; Kato, M.; Motegi, M.; Kondo, M.; et al. Glucagon-Like Peptide-1 Receptor Agonist Protects Dorsal Root Ganglion Neurons against Oxidative Insult. J. Diabetes Res. 2019, 2019, 9426014. [Google Scholar] [CrossRef] [PubMed]
- Mohiuddin, M.S.; Himeno, T.; Yamada, Y.; Morishita, Y.; Kondo, M.; Tsunekawa, S.; Kato, Y.; Nakamura, J.; Kamiya, H. Glucagon Prevents Cytotoxicity Induced by Methylglyoxal in a Rat Neuronal Cell Line Model. Biomolecules 2021, 11, 287. [Google Scholar] [CrossRef]
- Chen, W.; Mi, R.; Haughey, N.; Oz, M.; Höke, A. Immortalization and characterization of a nociceptive dorsal root ganglion sensory neuronal line. J. Peripher. Nerv. Syst. 2007, 12, 121–130. [Google Scholar] [CrossRef]
- Dusan, M.; Jastrow, C.; Alyce, M.M.; Yingkai, W.; Shashikanth, M.; Andelain, E.; Christine, B.M.; Stuart, B.M.; Oliver, B.G.; Michael, M.Z.; et al. Differentiation of the 50B11 dorsal ganglion cells into NGF and GDNF responsive nociceptor subtypes. Mol. Pain 2020, 16, 1744806920970368. [Google Scholar] [CrossRef]
- Himeno, T.; Kamiya, H.; Naruse, K.; Harada, N.; Ozaki, N.; Seino, Y.; Shibata, T.; Kondo, M.; Kato, J.; Okawa, T.; et al. Beneficial effects of exendin-4 on experimental polyneuropathy in diabetic mice. Diabetes 2011, 60, 2397–2406. [Google Scholar] [CrossRef] [PubMed]
- Monaghan, T.K.; Mackenzie, C.J.; Plevin, R.; Lutz, E.M. PACAP-38 induces neuronal differentiation of human SH-SY5Y neuroblastoma cells via cAMP-mediated activation of ERK and p38 MAP kinases. J. Neurochem. 2008, 104, 74–88. [Google Scholar] [CrossRef] [PubMed]
- Mabuchi, T.; Shintani, N.; Matsumura, S.; Okuda-Ashitaka, E.; Hashimoto, H.; Muratani, T.; Minami, T.; Baba, A.; Ito, S. Pituitary adenylate cyclase-activating polypeptide is required for the development of spinal sensitization and induction of neuropathic pain. J. Neurosci. 2004, 24, 7283–7291. [Google Scholar] [CrossRef] [PubMed]
- Vaudry, D.; Gonzalez, B.J.; Basille, M.; Yon, L.; Fournier, A.; Vaudry, H. Pituitary adenylate cyclase-activating polypeptide and its receptors: From structure to functions. Pharmacol. Rev. 2000, 52, 269–324. [Google Scholar] [PubMed]
- May, V.; Johnson, G.C.; Hammack, S.E.; Braas, K.M.; Parsons, R.L. PAC1 Receptor Internalization and Endosomal MEK/ERK Activation Is Essential for PACAP-Mediated Neuronal Excitability. J. Mol. Neurosci. 2021, 71, 1536–1542. [Google Scholar] [CrossRef]
- Motegi, M.; Himeno, T.; Nakai-Shimoda, H.; Inoue, R.; Ozeki, N.; Hayashi, Y.; Sasajima, S.; Mohiuddin, M.S.; Asano-Hayami, E.; Kato, M.; et al. Deficiency of glucagon gene-derived peptides induces peripheral polyneuropathy in mice. Biochem. Biophys. Res. Commun. 2020, 532, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.S.; Sundrum, T.; Hay, D.L. PACAP receptor pharmacology and agonist bias: Analysis in primary neurons and glia from the trigeminal ganglia and transfected cells. Br. J. Pharmacol. 2014, 171, 1521–1533. [Google Scholar] [CrossRef] [PubMed]
- Nakamachi, T.; Li, M.; Shioda, S.; Arimura, A. Signaling involved in pituitary adenylate cyclase-activating polypeptide-stimulated ADNP expression. Peptides 2006, 27, 1859–1864. [Google Scholar] [CrossRef] [PubMed]
- Nakamachi, T.; Nakamura, K.; Oshida, K.; Kagami, N.; Mori, H.; Watanabe, J.; Arata, S.; Yofu, S.; Endo, K.; Wada, Y.; et al. Pituitary adenylate cyclase-activating polypeptide (PACAP) stimulates proliferation of reactive astrocytes in vitro. J. Mol. Neurosci. 2011, 43, 16–21. [Google Scholar] [CrossRef]
- Michel, M.C.; Beck-Sickinger, A.; Cox, H.; Doods, H.N.; Herzog, H.; Larhammar, D.; Quirion, R.; Schwartz, T.; Westfall, T. XVI. International Union of Pharmacology recommendations for the nomenclature of neuropeptide Y, peptide YY, and pancreatic polypeptide receptors. Pharmacol. Rev. 1998, 50, 143–150. [Google Scholar] [PubMed]
- Vaudry, D.; Falluel-Morel, A.; Bourgault, S.; Basille, M.; Burel, D.; Wurtz, O.; Fournier, A.; Chow, B.K.; Hashimoto, H.; Galas, L.; et al. Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol. Rev. 2009, 61, 283–357. [Google Scholar] [CrossRef] [PubMed]
- Farnham, M.M.; Lung, M.S.; Tallapragada, V.J.; Pilowsky, P.M. PACAP causes PAC1/VPAC2 receptor mediated hypertension and sympathoexcitation in normal and hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2012, 303, H910–H917. [Google Scholar] [CrossRef] [PubMed]
- Horvath, G.; Opper, B.; Reglodi, D. The Neuropeptide Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP) is Protective in Inflammation and Oxidative Stress-Induced Damage in the Kidney. Int. J. Mol. Sci. 2019, 20, 4944. [Google Scholar] [CrossRef] [PubMed]
- Fehér, M.; Márton, Z.; Szabó, Á.; Kocsa, J.; Kormos, V.; Hunyady, Á.; Kovács, L.; Ujvári, B.; Berta, G.; Farkas, J.; et al. Downregulation of PACAP and the PAC1 Receptor in the Basal Ganglia, Substantia Nigra and Centrally Projecting Edinger-Westphal Nucleus in the Rotenone model of Parkinson’s Disease. Int. J. Mol. Sci. 2023, 24, 11843. [Google Scholar] [CrossRef] [PubMed]
- Banks, W.A.; Uchida, D.; Arimura, A.; Somogyvári-Vigh, A.; Shioda, S. Transport of pituitary adenylate cyclase-activating polypeptide across the blood-brain barrier and the prevention of ischemia-induced death of hippocampal neurons. Ann. N. Y. Acad. Sci. 1996, 805, 270–277, discussion 277–279. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamaguchi, M.; Noda-Asano, S.; Inoue, R.; Himeno, T.; Motegi, M.; Hayami, T.; Nakai-Shimoda, H.; Kono, A.; Sasajima, S.; Miura-Yura, E.; et al. Dipeptidyl Peptidase (DPP)-4 Inhibitors and Pituitary Adenylate Cyclase-Activating Polypeptide, a DPP-4 Substrate, Extend Neurite Outgrowth of Mouse Dorsal Root Ganglia Neurons: A Promising Approach in Diabetic Polyneuropathy Treatment. Int. J. Mol. Sci. 2024, 25, 8881. https://doi.org/10.3390/ijms25168881
Yamaguchi M, Noda-Asano S, Inoue R, Himeno T, Motegi M, Hayami T, Nakai-Shimoda H, Kono A, Sasajima S, Miura-Yura E, et al. Dipeptidyl Peptidase (DPP)-4 Inhibitors and Pituitary Adenylate Cyclase-Activating Polypeptide, a DPP-4 Substrate, Extend Neurite Outgrowth of Mouse Dorsal Root Ganglia Neurons: A Promising Approach in Diabetic Polyneuropathy Treatment. International Journal of Molecular Sciences. 2024; 25(16):8881. https://doi.org/10.3390/ijms25168881
Chicago/Turabian StyleYamaguchi, Masahiro, Saeko Noda-Asano, Rieko Inoue, Tatsuhito Himeno, Mikio Motegi, Tomohide Hayami, Hiromi Nakai-Shimoda, Ayumi Kono, Sachiko Sasajima, Emiri Miura-Yura, and et al. 2024. "Dipeptidyl Peptidase (DPP)-4 Inhibitors and Pituitary Adenylate Cyclase-Activating Polypeptide, a DPP-4 Substrate, Extend Neurite Outgrowth of Mouse Dorsal Root Ganglia Neurons: A Promising Approach in Diabetic Polyneuropathy Treatment" International Journal of Molecular Sciences 25, no. 16: 8881. https://doi.org/10.3390/ijms25168881
APA StyleYamaguchi, M., Noda-Asano, S., Inoue, R., Himeno, T., Motegi, M., Hayami, T., Nakai-Shimoda, H., Kono, A., Sasajima, S., Miura-Yura, E., Morishita, Y., Kondo, M., Tsunekawa, S., Kato, Y., Kato, K., Naruse, K., Nakamura, J., & Kamiya, H. (2024). Dipeptidyl Peptidase (DPP)-4 Inhibitors and Pituitary Adenylate Cyclase-Activating Polypeptide, a DPP-4 Substrate, Extend Neurite Outgrowth of Mouse Dorsal Root Ganglia Neurons: A Promising Approach in Diabetic Polyneuropathy Treatment. International Journal of Molecular Sciences, 25(16), 8881. https://doi.org/10.3390/ijms25168881





