Disclosing the Novel Protective Mechanisms of Ocrelizumab in Multiple Sclerosis: The Role of PKC Beta and Its Down-Stream Targets
Abstract
1. Introduction
2. Results
2.1. Demographic and Clinical Characteristics of MS Patients and HC
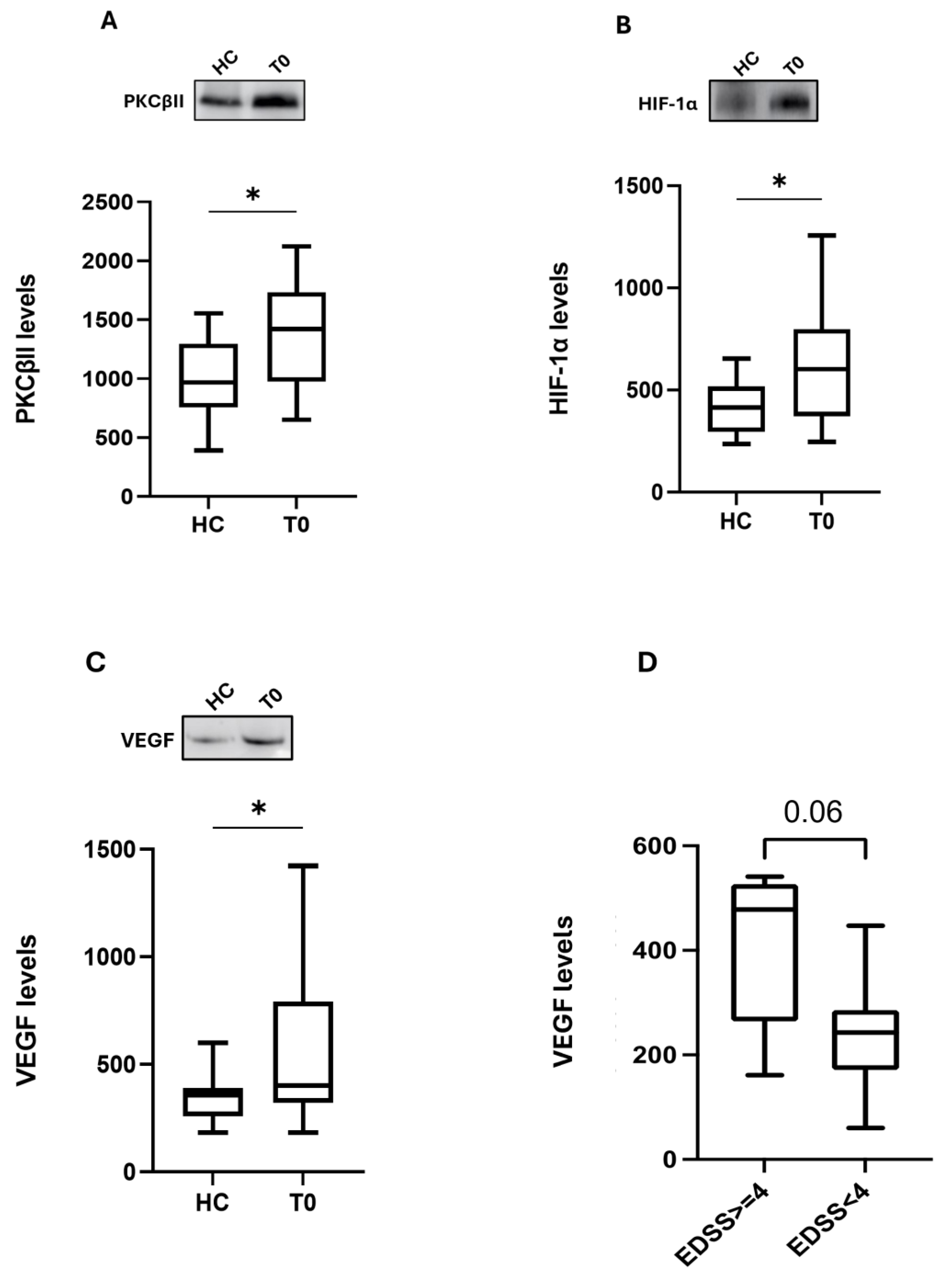
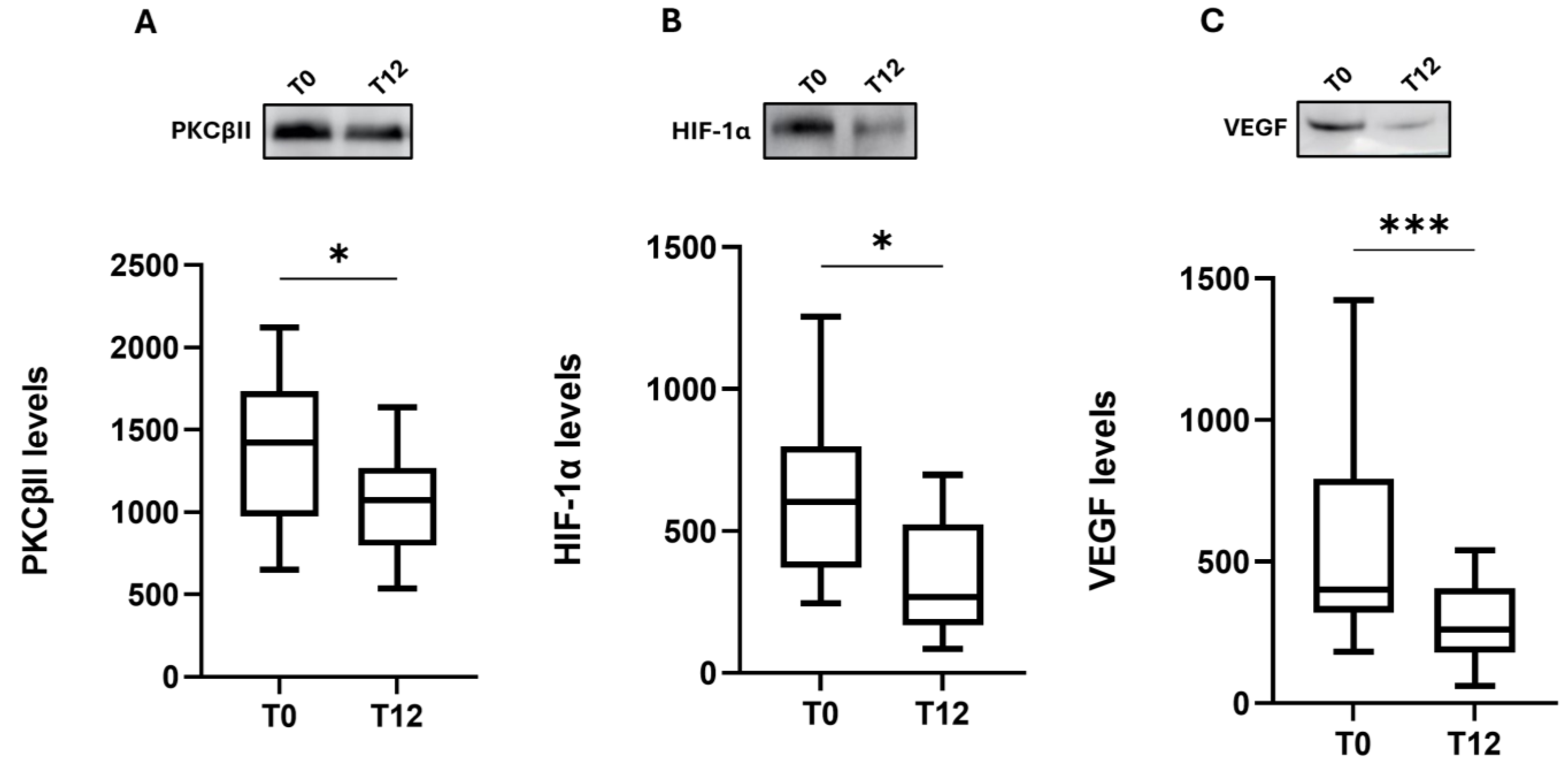
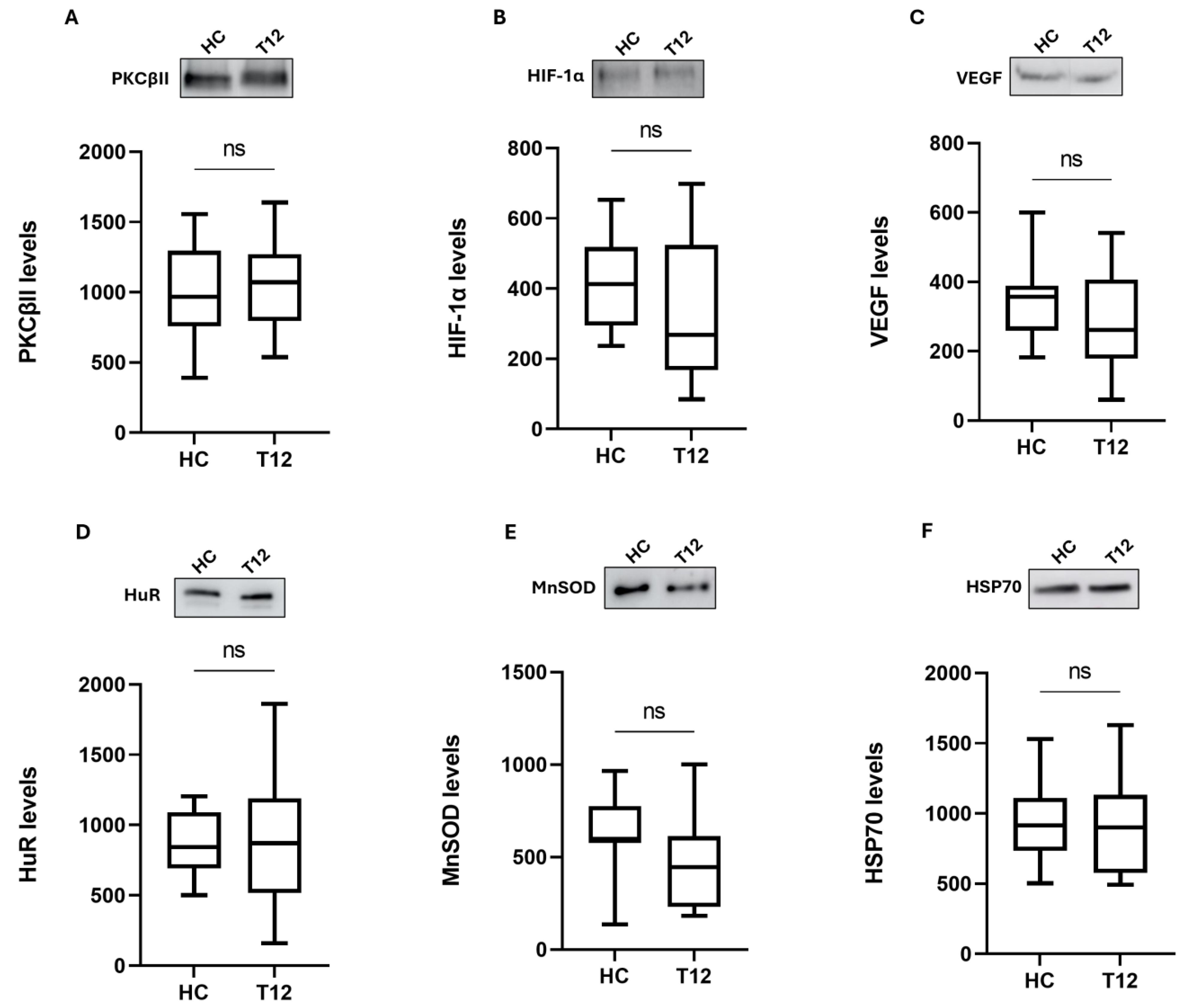
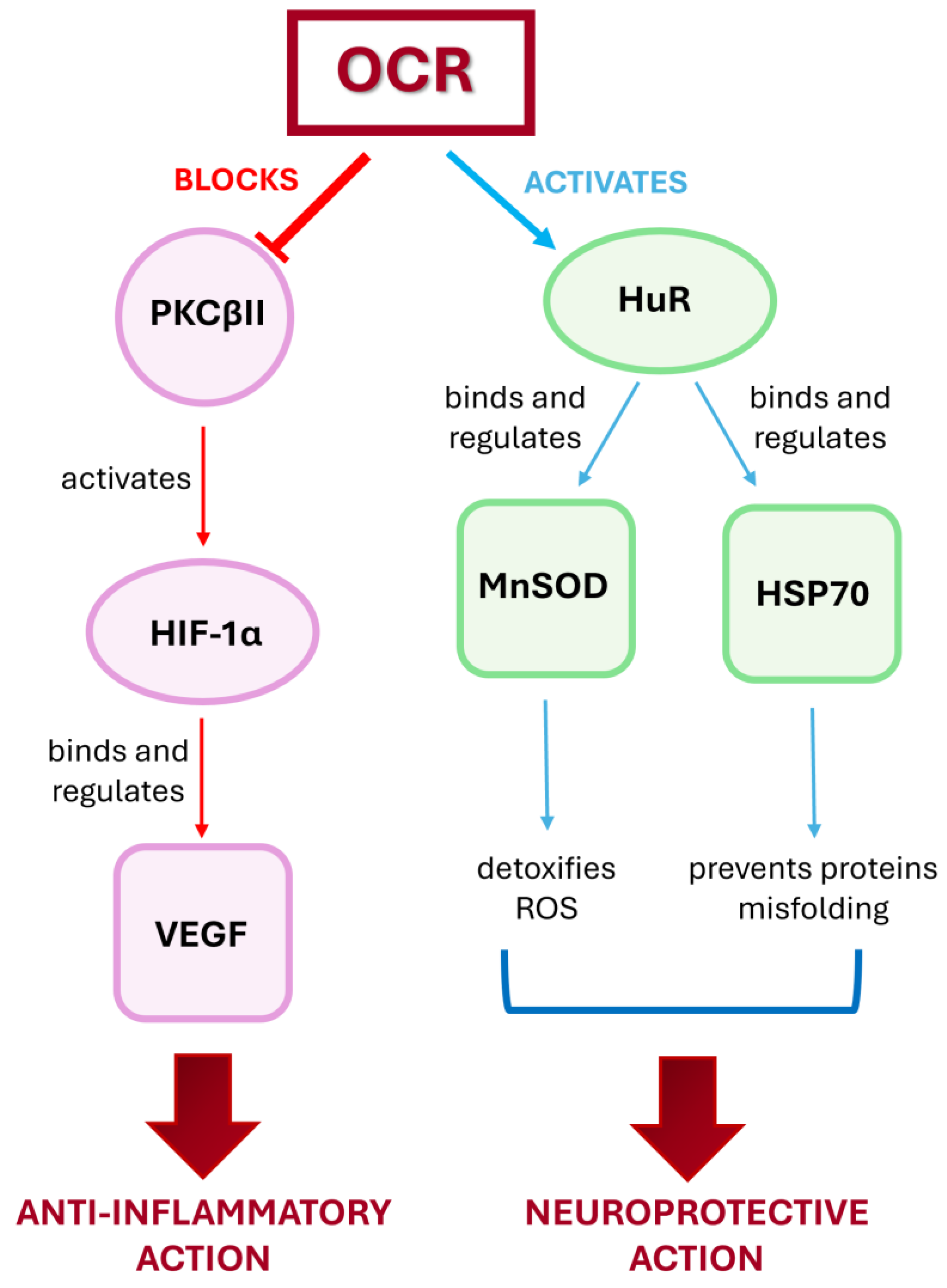
2.2. Effect of Ocrelizumab Treatment on the PKCβII/HIF-1α/VEGF Inflammatory Cascade in PBMCs
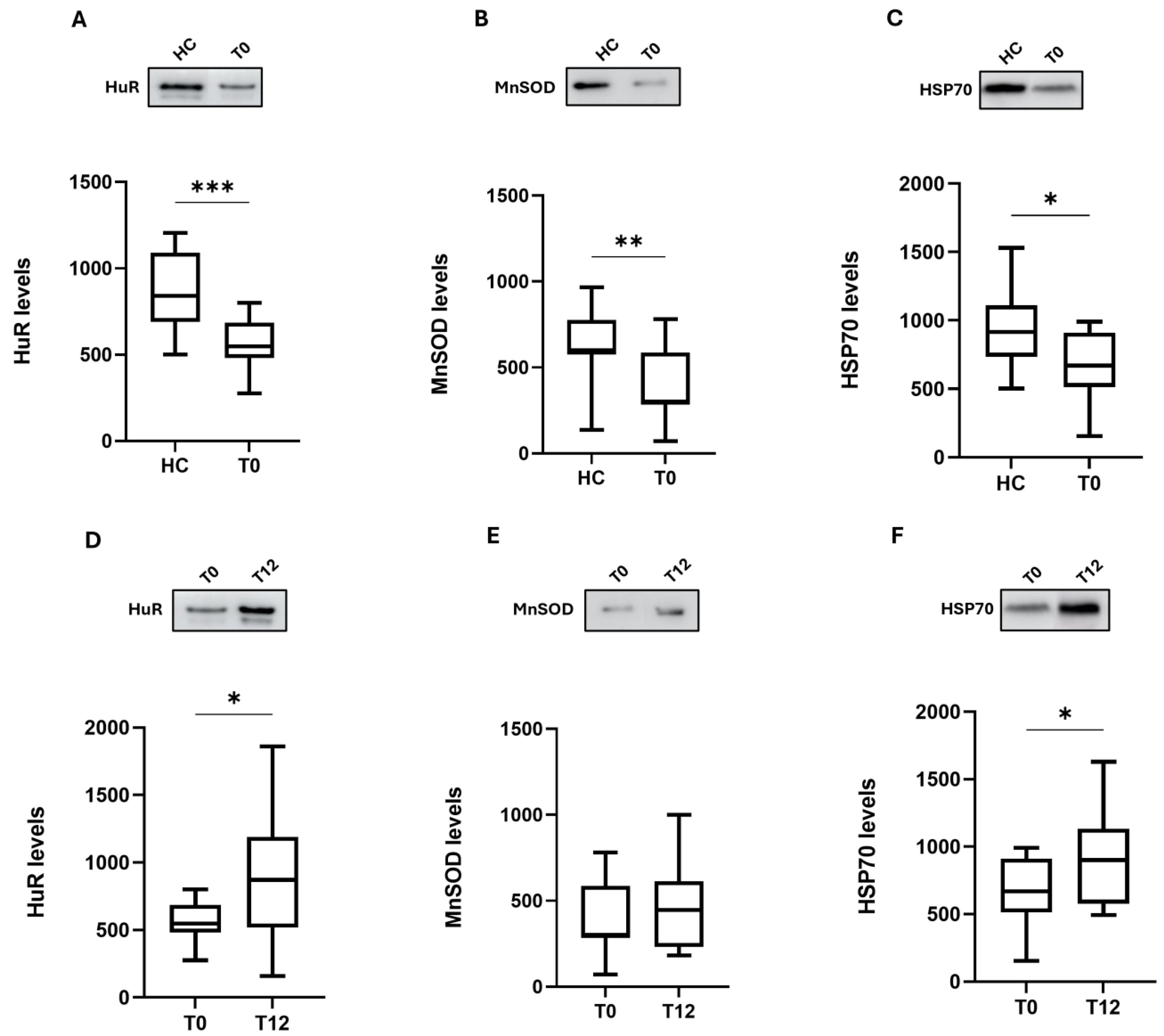
2.3. Effect of Ocrelizumab Treatment on the HuR, MnSOD, and HSP70 Antioxidant Pathways in PBMCs
3. Discussion
4. Materials and Methods
4.1. Subjects
Clinical Data
4.2. PBMCs Isolation from Whole Blood
4.3. Western Blotting
4.4. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dobson, R.; Giovannoni, G. Multiple Sclerosis—A review. Eur. J. Neurol. 2019, 26, 27–40. [Google Scholar] [CrossRef]
- Hauser, S.L.; Cree, B.A.C. Treatment of Multiple Sclerosis: A Review. Am. J. Med. 2020, 133, 1380–1390.e2. [Google Scholar] [CrossRef]
- Calabrese, M.; Preziosa, P.; Scalfari, A.; Colato, E.; Marastoni, D.; Absinta, M.; Battaglini, M.; De Stefano, N.; Di Filippo, M.; Hametner, S.; et al. Determinants and Biomarkers of Progression Independent of Relapses in Multiple Sclerosis. Ann. Neurol. 2024, 96, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Mulero, P.; Midaglia, L.; Montalban, X. Ocrelizumab: A New Milestone in Multiple Sclerosis Therapy. Ther. Adv. Neurol. Disord. 2018, 11, 175628641877302. [Google Scholar] [CrossRef]
- Jelcic, I.; Al Nimer, F.; Wang, J.; Lentsch, V.; Planas, R.; Jelcic, I.; Madjovski, A.; Ruhrmann, S.; Faigle, W.; Frauenknecht, K.; et al. Memory B Cells Activate Brain-Homing, Autoreactive CD4+ T Cells in Multiple Sclerosis. Cell 2018, 175, 85–100.e23. [Google Scholar] [CrossRef] [PubMed]
- Michel, L.; Touil, H.; Pikor, N.B.; Gommerman, J.L.; Prat, A.; Bar-Or, A. B Cells in the Multiple Sclerosis Central Nervous System: Trafficking and Contribution to CNS-Compartmentalized Inflammation. Front. Immunol. 2015, 6, 636. [Google Scholar] [CrossRef]
- Hauser, S.L.; Bar-Or, A.; Comi, G.; Giovannoni, G.; Hartung, H.-P.; Hemmer, B.; Lublin, F.; Montalban, X.; Rammohan, K.W.; Selmaj, K.; et al. Ocrelizumab versus Interferon Beta-1a in Relapsing Multiple Sclerosis. N. Engl. J. Med. 2017, 376, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Montalban, X.; Hauser, S.L.; Kappos, L.; Arnold, D.L.; Bar-Or, A.; Comi, G.; De Seze, J.; Giovannoni, G.; Hartung, H.-P.; Hemmer, B.; et al. Ocrelizumab versus Placebo in Primary Progressive Multiple Sclerosis. N. Engl. J. Med. 2017, 376, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.; Oswald, E.; Wong, H.K.; Vural, A.; Yilmaz, V.; Tüzün, E.; Türkoğlu, R.; Straub, T.; Meinl, I.; Thaler, F.; et al. Ocrelizumab Treatment Modulates B-Cell Regulating Factors in Multiple Sclerosis. Neurol. Neuroimmunol. Neuroinflamm. 2023, 10, e200083. [Google Scholar] [CrossRef]
- Li, R.; Rezk, A.; Miyazaki, Y.; Hilgenberg, E.; Touil, H.; Shen, P.; Moore, C.S.; Michel, L.; Althekair, F.; Rajasekharan, S.; et al. Proinflammatory GM-CSF–Producing B Cells in Multiple Sclerosis and B Cell Depletion Therapy. Sci. Transl. Med. 2015, 7, 310ra166. [Google Scholar] [CrossRef]
- Riley, J.K.; Sliwkowski, M.X. CD20: A Gene in Search of a Function. Semin. Oncol. 2000, 27, 17–24. [Google Scholar] [PubMed]
- Smith, M.R. Rituximab (Monoclonal Anti-CD20 Antibody): Mechanisms of Action and Resistance. Oncogene 2003, 22, 7359–7368. [Google Scholar] [CrossRef] [PubMed]
- Leseux, L.; Laurent, G.; Laurent, C.; Rigo, M.; Blanc, A.; Olive, D.; Bezombes, C. PKC ζ–mTOR Pathway: A New Target for Rituximab Therapy in Follicular Lymphoma. Blood 2008, 111, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Fahmideh, F.; Marchesi, N.; Campagnoli, L.I.M.; Landini, L.; Caramella, C.; Barbieri, A.; Govoni, S.; Pascale, A. Effect of Troxerutin in Counteracting Hyperglycemia-Induced VEGF Upregulation in Endothelial Cells: A New Option to Target Early Stages of Diabetic Retinopathy? Front. Pharmacol. 2022, 13, 951833. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Shen, X.; Lin, L.; Leitges, M.; Rosario, R.; Zou, Y.S.; Yan, S.F. PKCβ Promotes Vascular Inflammation and Acceleration of Atherosclerosis in Diabetic ApoE Null Mice. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 1779–1787. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shu, Y.; Hassan, F.; Coppola, V.; Baskin, K.K.; Han, X.; Mehta, N.K.; Ostrowski, M.C.; Mehta, K.D. Hepatocyte-Specific PKCβ Deficiency Protects against High-Fat Diet-Induced Nonalcoholic Hepatic Steatosis. Mol. Metab. 2021, 44, 101133. [Google Scholar] [CrossRef] [PubMed]
- Amadio, M.; Scapagnini, G.; Lupo, G.; Drago, F.; Govoni, S.; Pascale, A. PKCβII/HuR/VEGF: A New Molecular Cascade in Retinal Pericytes for the Regulation of VEGF Gene Expression. Pharmacol. Res. 2008, 57, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; Ozaki, I.; Matsuhashi, S.; Kuwashiro, T.; Takahashi, H.; Anzai, K.; Mizuta, T. Mechanisms of PKC-Mediated Enhancement of HIF-1α Activity and its Inhibition by Vitamin K2 in Hepatocellular Carcinoma Cells. Int. J. Mol. Sci. 2019, 20, 1022. [Google Scholar] [CrossRef]
- Forsythe, J.A.; Jiang, B.-H.; Iyer, N.V.; Agani, F.; Leung, S.W.; Koos, R.D.; Semenza, G.L. Activation of Vascular Endothelial Growth Factor Gene Transcription by Hypoxia-Inducible Factor 1. Mol. Cell. Biol. 1996, 16, 4604–4613. [Google Scholar] [CrossRef]
- Pagé, E.L.; Robitaille, G.A.; Pouysségur, J.; Richard, D.E. Induction of Hypoxia-Inducible Factor-1α by Transcriptional and Translational Mechanisms. J. Biol. Chem. 2002, 277, 48403–48409. [Google Scholar] [CrossRef]
- Tham, E.; Gielen, A.W.; Khademi, M.; Martin, C.; Piehl, F. Decreased Expression of VEGF-A in Rat Experimental Autoimmune Encephalomyelitis and in Cerebrospinal Fluid Mononuclear Cells from Patients with Multiple Sclerosis. Scand. J. Immunol. 2006, 64, 609–622. [Google Scholar] [CrossRef]
- Girolamo, F.; Coppola, C.; Ribatti, D.; Trojano, M. Angiogenesis in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis. Acta Neuropathol. Commun. 2014, 2, 84. [Google Scholar] [CrossRef]
- Iacobaeus, E.; Amoudruz, P.; Ström, M.; Khademi, M.; Brundin, L.; Hillert, J.; Kockum, I.; Malmström, V.; Olsson, T.; Tham, E.; et al. The Expression of VEGF—A Is Down Regulated in Peripheral Blood Mononuclear Cells of Patients with Secondary Progressive Multiple Sclerosis. PLoS ONE 2011, 6, e19138. [Google Scholar] [CrossRef]
- Minagar, A.; Alexander, J.S. Blood-Brain Barrier Disruption in Multiple Sclerosis. Mult. Scler. J. 2003, 9, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Pascale, A.; Govoni, S. The Complex World of Post-Transcriptional Mechanisms: Is Their Deregulation a Common Link for Diseases? Focus on ELAV-like RNA-Binding Proteins. Cell. Mol. Life Sci. 2012, 69, 501–517. [Google Scholar] [CrossRef]
- Srikantan, S.; Gorospe, M. HuR Function in Disease. Front. Biosci. Landmark Ed. 2012, 17, 189–205. [Google Scholar] [CrossRef]
- Ramos-González, E.J.; Bitzer-Quintero, O.K.; Ortiz, G.; Hernández-Cruz, J.J.; Ramírez-Jirano, L.J. Relationship between Inflammation and Oxidative Stress and Its Effect on Multiple Sclerosis. Neurología 2021, 3, S0213485321002632. [Google Scholar] [CrossRef]
- Pegoretti, V.; Swanson, K.A.; Bethea, J.R.; Probert, L.; Eisel, U.L.M.; Fischer, R. Inflammation and Oxidative Stress in Multiple Sclerosis: Consequences for Therapy Development. Oxid. Med. Cell. Longev. 2020, 2020, 7191080. [Google Scholar] [CrossRef] [PubMed]
- Marciano, F.; Vajro, P. Oxidative Stress and Gut Microbiota. In Gastrointestinal Tissue; Elsevier: Amsterdam, The Netherlands, 2017; pp. 113–123. ISBN 978-0-12-805377-5. [Google Scholar]
- Kokoszka, J.E.; Coskun, P.; Esposito, L.A.; Wallace, D.C. Increased Mitochondrial Oxidative Stress in the Sod2 (+/-) Mouse Results in the Age-Related Decline of Mitochondrial Function Culminating in Increased Apoptosis. Proc. Natl. Acad. Sci. USA 2001, 98, 2278–2283. [Google Scholar] [CrossRef]
- Amadio, M.; Scapagnini, G.; Laforenza, U.; Intrieri, M.; Romeo, L.; Govoni, S.; Pascale, A. Post-Transcriptional Regulation of HSP70 Expression Following Oxidative Stress in SH-SY5Y Cells: The Potential Involvement of the RNA-Binding Protein HuR. Curr. Pharm. Des. 2008, 14, 2651–2658. [Google Scholar] [CrossRef] [PubMed]
- Kalmar, B.; Greensmith, L. Induction of Heat Shock Proteins for Protection against Oxidative Stress. Adv. Drug Deliv. Rev. 2009, 61, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Mansilla, M.J.; Comabella, M.; Río, J.; Castilló, J.; Castillo, M.; Martin, R.; Montalban, X.; Espejo, C. Up-Regulation of Inducible Heat Shock Protein-70 Expression in Multiple Sclerosis Patients. Autoimmunity 2014, 47, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Mayer, M.P. Chaperone Dynamics and Molecular Mechanism. Trends Biochem. Sci. 2013, 38, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Amadio, M.; Bucolo, C.; Leggio, G.M.; Drago, F.; Govoni, S.; Pascale, A. The PKCβ/HuR/VEGF Pathway in Diabetic Retinopathy. Biochem. Pharmacol. 2010, 80, 1230–1237. [Google Scholar] [CrossRef] [PubMed]
- Mallucci, G.; Marchesi, N.; Campagnoli, L.I.M.; Boschi, F.; Fahmideh, F.; Fusco, S.; Tavazzi, E.; Govoni, S.; Bergamaschi, R.; Pascale, A. Evidence for Novel Cell Defense Mechanisms Sustained by Dimethyl Fumarate in Multiple Sclerosis Patients: The HuR/SOD2 Cascade. Mult. Scler. Relat. Disord. 2022, 68, 104197. [Google Scholar] [CrossRef] [PubMed]
- Pistono, C.; Monti, M.C.; Marchesi, N.; Boiocchi, C.; Campagnoli, L.I.M.; Morlotti, D.; Cuccia, M.; Govoni, S.; Montomoli, C.; Mallucci, G.; et al. Unraveling a New Player in Multiple Sclerosis Pathogenesis: The RNA-Binding Protein HuR. Mult. Scler. Relat. Disord. 2020, 41, 102048. [Google Scholar] [CrossRef] [PubMed]
- Rigor, R.R.; Hawkins, B.T.; Miller, D.S. Activation of PKC Isoform β I at the Blood–Brain Barrier Rapidly Decreases P-Glycoprotein Activity and Enhances Drug Delivery to the Brain. J. Cereb. Blood Flow Metab. 2010, 30, 1373–1383. [Google Scholar] [CrossRef] [PubMed]
- Willis, C.L.; Meske, D.S.; Davis, T.P. Protein Kinase C Activation Modulates Reversible Increase in Cortical Blood–Brain Barrier Permeability and Tight Junction Protein Expression during Hypoxia and Posthypoxic Reoxygenation. J. Cereb. Blood Flow Metab. 2010, 30, 1847–1859. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-A.; Park, S.L.; Kim, M.-Y.; Lee, S.H.; Baik, E.J.; Moon, C.-H.; Jung, Y.-S. ole of PKCβII and PKCδ in Blood–Brain Barrier Permeability during Aglycemic Hypoxia. Neurosci. Lett. 2010, 468, 254–258. [Google Scholar] [CrossRef]
- Lanz, T.V.; Becker, S.; Osswald, M.; Bittner, S.; Schuhmann, M.K.; Opitz, C.A.; Gaikwad, S.; Wiestler, B.; Litzenburger, U.M.; Sahm, F.; et al. Protein Kinase Cβ as a Therapeutic Target Stabilizing Blood–Brain Barrier Disruption in Experimental Autoimmune Encephalomyelitis. Proc. Natl. Acad. Sci. USA 2013, 110, 14735–14740. [Google Scholar] [CrossRef]
- Ahluwalia, A.; S Tarnawski, A. Critical Role of Hypoxia Sensor—HIF-1α; in VEGF Gene Activation. Implications for Angiogenesis and Tissue Injury Healing. Curr. Med. Chem. 2012, 19, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Graeber, T.G.; Osmanian, C.; Jacks, T.; Housman, D.E.; Koch, C.J.; Lowe, S.W.; Giaccia, A.J. Hypoxia-Mediated Selection of Cells with Diminished Apoptotic Potential in Solid Tumours. Nature 1996, 379, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Roscoe, W.A.; Welsh, M.E.; Carter, D.E.; Karlik, S.J. VEGF and Angiogenesis in Acute and Chronic MOG(35–55) Peptide Induced EAE. J. Neuroimmunol. 2009, 209, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, H. Hypoxia-like Tissue Injury as a Component of Multiple Sclerosis Lesions. J. Neurol. Sci. 2003, 206, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Moran, E.P.; Wang, Z.; Chen, J.; Sapieha, P.; Smith, L.E.H.; Ma, J. Neurovascular Cross Talk in Diabetic Retinopathy: Pathophysiological Roles and Therapeutic Implications. Am. J. Physiol.-Heart Circ. Physiol. 2016, 311, H738–H749. [Google Scholar] [CrossRef] [PubMed]
- Chapouly, C.; Tadesse Argaw, A.; Horng, S.; Castro, K.; Zhang, J.; Asp, L.; Loo, H.; Laitman, B.M.; Mariani, J.N.; Straus Farber, R.; et al. Astrocytic TYMP and VEGFA Drive Blood–Brain Barrier Opening in Inflammatory Central Nervous System. Brain 2015, 138, 1548–1567. [Google Scholar] [CrossRef] [PubMed]
- Di Girolamo, F.; D’Amato, A.; Lante, I.; Signore, F.; Muraca, M.; Putignani, L. Farm Animal Serum Proteomics and Impact on Human Health. Int. J. Mol. Sci. 2014, 15, 15396–15411. [Google Scholar] [CrossRef]
- Theoharides, T.C.; Konstantinidou, A.D. Corticotropin-Releasing Hormone and the Blood-Brain-Barrier. Front. Biosci. 2007, 12, 1615. [Google Scholar] [CrossRef]
- Amini Harandi, A.; Siavoshi, F.; Shirzadeh Barough, S.; Amini Harandi, A.; Pakdaman, H.; Sahraian, M.A.; Fathtabar, Z.; Mohammadi, F.; Karamiani, F.; Ardehali, S.H. Vascular Endothelial Growth Factor as a Predictive and Prognostic Biomarker for Multiple Sclerosis. Neuroimmunomodulation 2022, 29, 476–485. [Google Scholar] [CrossRef]
- Lange, C.; Storkebaum, E.; De Almodóvar, C.R.; Dewerchin, M.; Carmeliet, P. Vascular Endothelial Growth Factor: A Neurovascular Target in Neurological Diseases. Nat. Rev. Neurol. 2016, 12, 439–454. [Google Scholar] [CrossRef] [PubMed]
- Rajdev, S.; Hara, K.; Kokubo, Y.; Mestril, R.; Dillmann, W.; Weinstein, P.R.; Sharp, F.R. Mice Overexpressing Rat Heat Shock Protein 70 Are Protected against Cerebral Infarction. Ann. Neurol. 2000, 47, 782–791. [Google Scholar] [CrossRef] [PubMed]
- Mansilla, M.J.; Montalban, X.; Espejo, C. Heat Shock Protein 70: Roles in Multiple Sclerosis. Mol. Med. 2012, 18, 1018–1028. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.L.; Brosnan, C.F.; Raine, C.S. Experimental Autoimmune Encephalomyelitis. Qualitative and Semiquantitative Differences in Heat Shock Protein 60 Expression in the Central Nervous System. J. Immunol. 1995, 154, 3548–3556. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of Multiple Sclerosis: 2017 Revisions of the McDonald Criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Rae-Grant, A.; Day, G.S.; Marrie, R.A.; Rabinstein, A.; Cree, B.A.C.; Gronseth, G.S.; Haboubi, M.; Halper, J.; Hosey, J.P.; Jones, D.E.; et al. Practice Guideline Recommendations Summary: Disease-Modifying Therapies for Adults with Multiple Sclerosis: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018, 90, 777–788. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating Neurologic Impairment in Multiple Sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 1983, 33, 1444. [Google Scholar] [CrossRef] [PubMed]
- Roxburgh, R.H.S.R.; Seaman, S.R.; Masterman, T.; Hensiek, A.E.; Sawcer, S.J.; Vukusic, S.; Achiti, I.; Confavreux, C.; Coustans, M.; le Page, E.; et al. Multiple Sclerosis Severity Score: Using Disability and Disease Duration to Rate Disease Severity. Neurology 2005, 64, 1144–1151. [Google Scholar] [CrossRef]
- Rigotti, D.; Gass, A.; Achtnichts, L.; Inglese, M.; Babb, J.; Naegelin, Y.; Hirsch, J.; Amann, M.; Kappos, L.; Gonen, O. Multiple Sclerosis Severity Scale and Whole-Brain N -Acetylaspartate Concentration for Patients’ Assessment. Mult. Scler. J. 2012, 18, 98–107. [Google Scholar] [CrossRef]
| MS Patients | Healthy Controls | |
|---|---|---|
| N = 17 | N = 17 | |
| Age (years) | 42.17 ± 8.44 | 42.00 ± 9.26 |
| Sex (F/M ratio) | 1.80 | 1.80 |
| MS duration (years) | 10.05 ± 9.26 | |
| EDSS (N = 17) | 2.79 ±1.70 | |
| EDSS < 4 | N 12 (70.6%) | |
| EDSS > 4 | N 5 (29.4%) | |
| MSSS (N = 17) | 4.24 ± 3.07 | |
| Mild MS (MSSS < 3, N = 7) | 1.12 ± 0.61 | |
| Moderate/severe MS (MSSS ≥ 3, N = 10) | 6.42 ± 1.90 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campagnoli, L.I.M.; Ahmad, L.; Marchesi, N.; Greco, G.; Boschi, F.; Masi, F.; Mallucci, G.; Bergamaschi, R.; Colombo, E.; Pascale, A. Disclosing the Novel Protective Mechanisms of Ocrelizumab in Multiple Sclerosis: The Role of PKC Beta and Its Down-Stream Targets. Int. J. Mol. Sci. 2024, 25, 8923. https://doi.org/10.3390/ijms25168923
Campagnoli LIM, Ahmad L, Marchesi N, Greco G, Boschi F, Masi F, Mallucci G, Bergamaschi R, Colombo E, Pascale A. Disclosing the Novel Protective Mechanisms of Ocrelizumab in Multiple Sclerosis: The Role of PKC Beta and Its Down-Stream Targets. International Journal of Molecular Sciences. 2024; 25(16):8923. https://doi.org/10.3390/ijms25168923
Chicago/Turabian StyleCampagnoli, Lucrezia Irene Maria, Lara Ahmad, Nicoletta Marchesi, Giacomo Greco, Federica Boschi, Francesco Masi, Giulia Mallucci, Roberto Bergamaschi, Elena Colombo, and Alessia Pascale. 2024. "Disclosing the Novel Protective Mechanisms of Ocrelizumab in Multiple Sclerosis: The Role of PKC Beta and Its Down-Stream Targets" International Journal of Molecular Sciences 25, no. 16: 8923. https://doi.org/10.3390/ijms25168923
APA StyleCampagnoli, L. I. M., Ahmad, L., Marchesi, N., Greco, G., Boschi, F., Masi, F., Mallucci, G., Bergamaschi, R., Colombo, E., & Pascale, A. (2024). Disclosing the Novel Protective Mechanisms of Ocrelizumab in Multiple Sclerosis: The Role of PKC Beta and Its Down-Stream Targets. International Journal of Molecular Sciences, 25(16), 8923. https://doi.org/10.3390/ijms25168923







