Markers of Metabolic Abnormalities in Vitiligo Patients
Abstract
:1. Introduction
2. Results
2.1. Evaluation of Common Metabolic Syndrome Components
2.2. Elevated Inflammatory Markers in the Serum of Vitiligo Patients
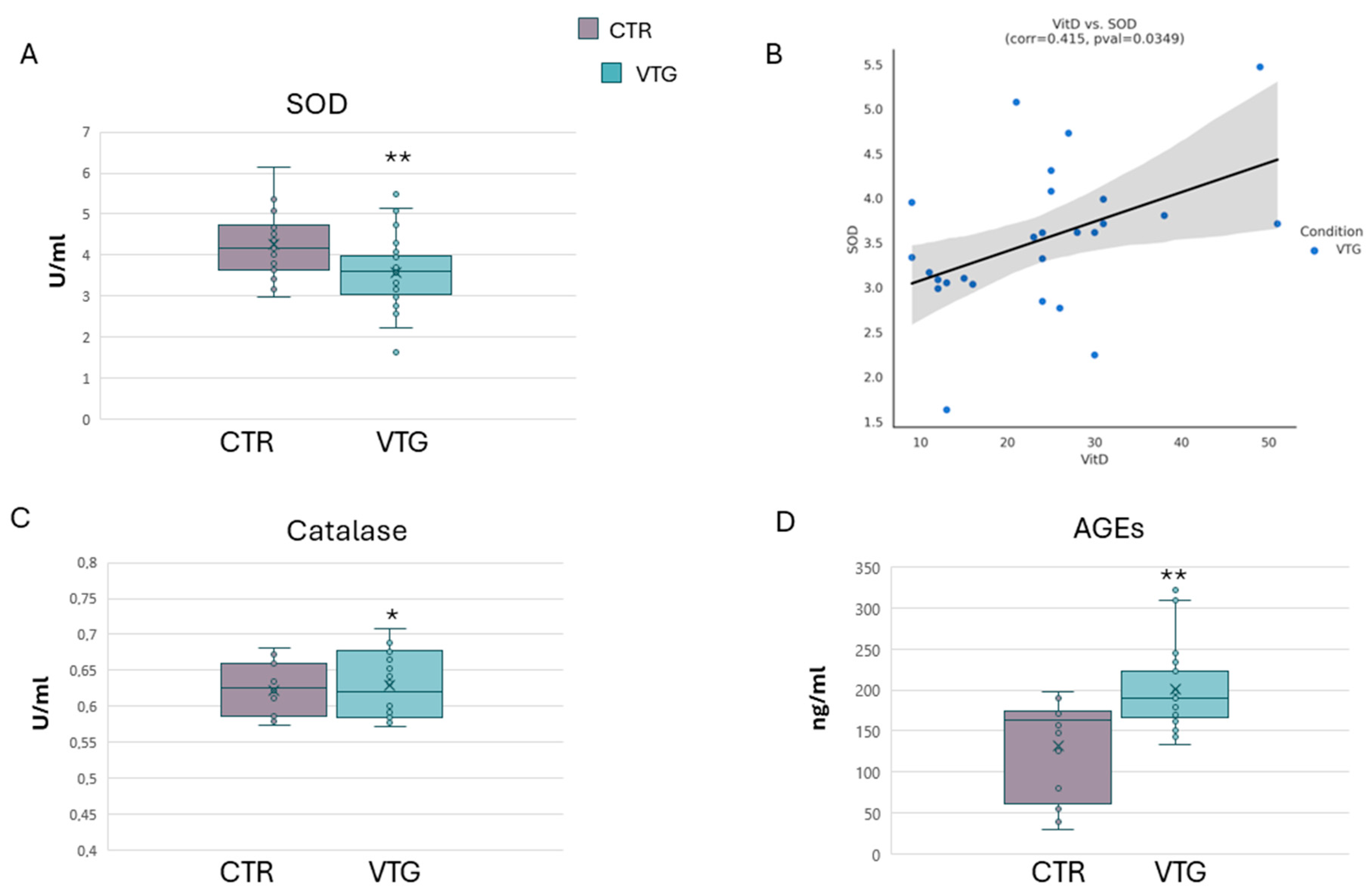
2.3. Assessment of Oxidative Stress Indicators in Vitiligo
2.4. Vitiligo Circulating Fatty Acid Composition
3. Discussion
4. Material and Methods
4.1. Patients
4.2. Blood Sampling
4.3. Immunoenzymatic and Colorimetric Assays
4.4. Extraction and Derivatization of Plasma Fatty Acids
4.5. GCMS Analysis of Plasma Fatty Acids
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ezzedine, K.; Eleftheriadou, V.; Whitton, M.; van Geel, N. Vitiligo. Lancet 2015, 386, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Bergqvist, C.; Ezzedine, K. Vitiligo: A Focus on Pathogenesis and its Therapeutic Implications. J. Dermatol. 2021, 48, 252–270. [Google Scholar] [CrossRef] [PubMed]
- Picardo, M.; Dell’Anna, M.L.; Ezzedine, K.; Hamzavi, I.; Harris, J.E.; Parsad, D.; Taieb, A. Vitiligo. Nat. Rev. Dis. Primers 2015, 1, 15011. [Google Scholar] [CrossRef] [PubMed]
- Mason, P.J. Vitiligo: The Psychosocial Effects. MedSurg Nurs. 1997, 6, 216–218, 232. [Google Scholar]
- Lyu, C.; Sun, Y. Immunometabolism in the Pathogenesis of Vitiligo. Front. Immunol. 2022, 13, 1055958. [Google Scholar] [CrossRef]
- Pietrzak, A.; Bartosińska, J.; Hercogová, J.; Lotti, T.M.; Chodorowska, G. Metabolic Syndrome in Vitiligo. Dermatol. Ther. 2012, 25 (Suppl. S1), 41. [Google Scholar] [CrossRef]
- Marchioro, H.Z.; Silva de Castro, C.C.; Fava, V.M.; Sakiyama, P.H.; Dellatorre, G.; Miot, H.A. Update on the Pathogenesis of Vitiligo. An. Bras. Dermatol. 2022, 97, 478–490. [Google Scholar] [CrossRef]
- Katz, E.L.; Harris, J.E. Translational Research in Vitiligo. Front. Immunol. 2021, 12, 624517. [Google Scholar] [CrossRef]
- Frisoli, M.L.; Essien, K.; Harris, J.E. Vitiligo: Mechanisms of Pathogenesis and Treatment. Annu. Rev. Immunol. 2020, 38, 621–648. [Google Scholar] [CrossRef]
- Karadag, A.S.; Tutal, E.; Ertugrul, D.T. Insulin Resistance is Increased in Patients with Vitiligo. Acta Derm. Venereol. 2011, 91, 541–544. [Google Scholar] [CrossRef]
- D’Arino, A.; Picardo, M.; Truglio, M.; Pacifico, A.; Iacovelli, P. Metabolic Comorbidities in Vitiligo: A Brief Review and Report of New Data from a Single-Center Experience. Int. J. Mol. Sci. 2021, 22, 8820. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Samson, S.L.; Garber, A.J. Metabolic Syndrome. Endocrinol. Metab. Clin. N. Am. 2014, 43, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Gisondi, P.; Fostini, A.C.; Fossà, I.; Girolomoni, G.; Targher, G. Psoriasis and the Metabolic Syndrome. Clin. Dermatol. 2018, 36, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Zhu, Y.; Zou, S.; Zhou, P.; Hu, Y.; Zhao, Q.; Gu, L.; Zhang, H.; Wang, Z.; Li, J. Metabolic Syndrome and Psoriasis: Mechanisms and Future Directions. Front. Immunol. 2021, 12, 711060. [Google Scholar] [CrossRef]
- Agarwal, K.; Das, S.; Kumar, R.; De, A. Psoriasis and its Association with Metabolic Syndrome. Indian J. Dermatol. 2023, 68, 274–277. [Google Scholar] [CrossRef]
- Tanacan, E.; Atakan, N. Higher Incidence of Metabolic Syndrome Components in Vitiligo Patients: A Prospective Cross-Sectional Study. An. Bras. Dermatol. 2020, 95, 165–172. [Google Scholar] [CrossRef]
- Hu, Z.; Wang, T. Beyond Skin White Spots: Vitiligo and Associated Comorbidities. Front. Med. 2023, 10, 1072837. [Google Scholar] [CrossRef]
- Xia, J.; Melian, C.; Guo, W.; Usmani, H.; Clark, R.; Lozeau, D. Vitiligo and Metabolic Syndrome: Systematic Review and Meta-Analysis. JMIR Dermatol. 2022, 5, e34772. [Google Scholar] [CrossRef]
- Shen, C.; Gao, J.; Sheng, Y.; Dou, J.; Zhou, F.; Zheng, X.; Ko, R.; Tang, X.; Zhu, C.; Yin, X.; et al. Genetic Susceptibility to Vitiligo: GWAS Approaches for Identifying Vitiligo Susceptibility Genes and Loci. Front. Genet. 2016, 7, 3. [Google Scholar] [CrossRef]
- Randhawa, M.; Huff, T.; Valencia, J.C.; Younossi, Z.; Chandhoke, V.; Hearing, V.J.; Baranova, A. Evidence for the Ectopic Synthesis of Melanin in Human Adipose Tissue. FASEB J. 2009, 23, 835–843. [Google Scholar] [CrossRef] [PubMed]
- Page, S.; Chandhoke, V.; Baranova, A. Melanin and Melanogenesis in Adipose Tissue: Possible Mechanisms for Abating Oxidative Stress and Inflammation? Obes. Rev. 2011, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Dell’Anna, M.L.; Urbanelli, S.; Mastrofrancesco, A.; Camera, E.; Iacovelli, P.; Leone, G.; Manini, P.; D’Ischia, M.; Picardo, M. Alterations of Mitochondria in Peripheral Blood Mononuclear Cells of Vitiligo Patients. Pigment Cell Res. 2003, 16, 553–559. [Google Scholar] [CrossRef]
- Bellei, B.; Pitisci, A.; Ottaviani, M.; Ludovici, M.; Cota, C.; Luzi, F.; Dell’Anna, M.L.; Picardo, M. Vitiligo: A Possible Model of Degenerative Diseases. PLoS ONE 2013, 8, e59782. [Google Scholar] [CrossRef] [PubMed]
- Dell’Anna, M.L.; Ottaviani, M.; Kovacs, D.; Mirabilii, S.; Brown, D.A.; Cota, C.; Migliano, E.; Bastonini, E.; Bellei, B.; Cardinali, G.; et al. Energetic Mitochondrial Failing in Vitiligo and Possible Rescue by Cardiolipin. Sci. Rep. 2017, 7, 13663–13665. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, D.; Bastonini, E.; Ottaviani, M.; Cota, C.; Migliano, E.; Dell’Anna, M.L.; Picardo, M. Vitiligo Skin: Exploring the Dermal Compartment. J. Investig. Dermatol. 2018, 138, 394–404. [Google Scholar] [CrossRef]
- Papaccio, F.; Bellei, B.; Ottaviani, M.; D’Arino, A.; Truglio, M.; Caputo, S.; Cigliana, G.; Sciuto, L.; Migliano, E.; Pacifico, A.; et al. A Possible Modulator of Vitiligo Metabolic Impairment: Rethinking a PPARγ Agonist. Cells 2022, 11, 3583. [Google Scholar] [CrossRef]
- Ataş, H.; Gönül, M. Increased Risk of Metabolic Syndrome in Patients with Vitiligo. Balk. Med. J. 2017, 34, 219–225. [Google Scholar] [CrossRef]
- Namazi, N.; Amani, M.; Haghighatkhah, H.R.; Noori, E.; Abdollahimajd, F. Increased Risk of Subclinical Atherosclerosis and Metabolic Syndrome in Patients with Vitiligo: A Real Association or a Coincidence? Dermatol. Ther. 2021, 34, e14803. [Google Scholar] [CrossRef]
- Tsai, T.; Kuo, C.; Huang, Y. Serum Homocysteine, Folate, and Vitamin B(12) Levels in Patients with Vitiligo and their Potential Roles as Disease Activity Biomarkers: A Systematic Review and Meta-Analysis. J. Am. Acad. Dermatol. 2019, 80, 646–654.e5. [Google Scholar] [CrossRef]
- Hasibuan, D.R.U.; Putra, I.B.; Jusuf, N.K. Correlation between Serum Homocysteine and Vitiligo Area Scoring Index. Open Access Maced J. Med. Sci. 2017, 5, 332–334. [Google Scholar] [CrossRef] [PubMed]
- Rehman, K.; Akash, M.S.H. Mechanisms of Inflammatory Responses and Development of Insulin Resistance: How are they Interlinked? J. Biomed. Sci. 2016, 23, 87. [Google Scholar] [CrossRef] [PubMed]
- Moretti, S.; Spallanzani, A.; Amato, L.; Hautmann, G.; Gallerani, I.; Fabiani, M.; Fabbri, P. New Insights into the Pathogenesis of Vitiligo: Imbalance of Epidermal Cytokines at Sites of Lesions. Pigment Cell Res. 2002, 15, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, M.; El-Mofty, M.; Anbar, T.; Rasheed, H.; Esmat, S.; Al-Tawdy, A.; Fawzy, M.M.; Abdel-Halim, D.; Hegazy, R.; Gawdat, H.; et al. CXCL-10 and Interleukin-6 are Reliable Serum Markers for Vitiligo Activity: A Multicenter Cross-Sectional Study. Pigment Cell Melanoma Res. 2018, 31, 330–336. [Google Scholar] [CrossRef]
- Khan, R.; Gupta, S.; Sharma, A. Circulatory Levels of T-Cell Cytokines (Interleukin [IL]-2, IL-4, IL-17, and Transforming Growth Factor-Β) in Patients with Vitiligo. J. Am. Acad. Dermatol. 2012, 66, 510–511. [Google Scholar] [CrossRef]
- Esmaeili, B.; Rezaee, S.A.R.; Layegh, P.; Tavakkol Afshari, J.; Dye, P.; Ghayoor Karimiani, E.; Kalalinia, F.; Rafatpanah, H. Expression of IL-17 and COX2 Gene in Peripheral Blood Leukocytes of Vitiligo Patients. Iran. J. Allergy Asthma Immunol. 2011, 10, 81–89. [Google Scholar]
- Bassiouny, D.A.; Shaker, O. Role of Interleukin-17 in the Pathogenesis of Vitiligo. Clin. Exp. Dermatol. 2011, 36, 292–297. [Google Scholar] [CrossRef]
- Elela, M.A.; Hegazy, R.A.; Fawzy, M.M.; Rashed, L.A.; Rasheed, H. Interleukin 17, Interleukin 22 and FoxP3 Expression in Tissue and Serum of Non-Segmental Vitiligo: A Case- Controlled Study on Eighty-Four Patients. Eur. J. Dermatol. 2013, 23, 350–355. [Google Scholar] [CrossRef]
- Fischer, F.; Schulte, H.; Mohan, S.; Tataru, M.; Köhler, E.; Assmann, G.; von Eckardstein, A. Associations of Insulin-Like Growth Factors, Insulin-Like Growth Factor Binding Proteins and Acid-Labile Subunit with Coronary Heart Disease. Clin. Endocrinol. 2004, 61, 595–602. [Google Scholar] [CrossRef]
- Halliwell, B.; Murcia, M.A.; Chirico, S.; Aruoma, O.I. Free Radicals and Antioxidants in Food and In Vivo: What they do and how they Work. Crit. Rev. Food Sci. Nutr. 1995, 35, 7–20. [Google Scholar] [CrossRef]
- Rahman, I.; Biswas, S.K.; Kode, A. Oxidant and Antioxidant Balance in the Airways and Airway Diseases. Eur. J. Pharmacol. 2006, 533, 222–239. [Google Scholar] [CrossRef] [PubMed]
- Carillon, J.; Rouanet, J.; Cristol, J.; Brion, R. Superoxide Dismutase Administration, a Potential Therapy Against Oxidative Stress Related Diseases: Several Routes of Supplementation and Proposal of an Original Mechanism of Action. Pharm. Res. 2013, 30, 2718–2728. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Wu, Y.; Li, L.; Cai, Y.; Liu, M.; Gao, X.; Chen, H. Meta-Analysis of the Association between Vitiligo and the Level of Superoxide Dismutase Or Malondialdehyde. Clin. Exp. Dermatol. 2017, 42, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Mathachan, S.R.; Khurana, A.; Gautam, R.K.; Kulhari, A.; Sharma, L.; Sardana, K. Does Oxidative Stress Correlate with Disease Activity and Severity in Vitiligo? An Analytical Study. J. Cosmet. Dermatol. 2021, 20, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Kassab, A.; Khalij, Y.; Ayed, Y.; Dar-Odeh, N.; Kokandi, A.A.; Denguezli, M.; Youssef, M. Serum Inflammatory and Oxidative Stress Markers in Patients with Vitiligo. J. Clin. Med. 2023, 12, 5861. [Google Scholar] [CrossRef]
- Bickers, D.R.; Athar, M. Oxidative Stress in the Pathogenesis of Skin Disease. J. Investig. Dermatol. 2006, 126, 2565–2575. [Google Scholar] [CrossRef]
- Chang, W.; Ko, C. The Role of Oxidative Stress in Vitiligo: An Update on its Pathogenesis and Therapeutic Implications. Cells 2023, 12, 936. [Google Scholar] [CrossRef]
- Vaccaro, M.; Bagnato, G.; Cristani, M.; Borgia, F.; Spatari, G.; Tigano, V.; Saja, A.; Guarneri, F.; Cannavò, S.P.; Gangemi, S. Oxidation Products are Increased in Patients Affected by Non-Segmental Generalized Vitiligo. Arch. Dermatol. Res. 2017, 309, 485–490. [Google Scholar] [CrossRef]
- Planas, A.; Simó-Servat, O.; Hernández, C.; Simó, R. Advanced Glycations End Products in the Skin as Biomarkers of Cardiovascular Risk in Type 2 Diabetes. Int. J. Mol. Sci. 2022, 23, 6234. [Google Scholar] [CrossRef]
- Parwani, K.; Mandal, P. Role of Advanced Glycation End Products and Insulin Resistance in Diabetic Nephropathy. Arch. Physiol. Biochem. 2023, 129, 95–107. [Google Scholar] [CrossRef]
- Simopoulos, A.P. Essential Fatty Acids in Health and Chronic Disease. Am. J. Clin. Nutr. 1999, 70, 560S–569S. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C.; Grimble, R.F. Polyunsaturated Fatty Acids, Inflammation and Immunity. Eur. J. Clin. Nutr. 2002, 56 (Suppl. S3), 14. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. Polyunsaturated Fatty Acids and Inflammation. Prostaglandins Leukot. Essent. Fatty Acids 2006, 75, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Abdelmagid, S.A.; Clarke, S.E.; Nielsen, D.E.; Badawi, A.; El-Sohemy, A.; Mutch, D.M.; Ma, D.W.L. Comprehensive Profiling of Plasma Fatty Acid Concentrations in Young Healthy Canadian Adults. PLoS ONE 2015, 10, e0116195. [Google Scholar] [CrossRef] [PubMed]
- Salama, A.H.; Alnemr, L.; Khan, A.R.; Alfakeer, H.; Aleem, Z.; Ali-Alkhateeb, M. Unveiling the Unseen Struggles: A Comprehensive Review of Vitiligo’s Psychological, Social, and Quality of Life Impacts. Cureus 2023, 15, e45030. [Google Scholar] [CrossRef]
- Singh, S.; Singh, U.; Pandey, S.S. Increased Level of Serum Homocysteine in Vitiligo. J. Clin. Lab. Anal. 2011, 25, 110–112. [Google Scholar] [CrossRef]
- Ataş, H.; Cemil, B.Ç.; Gönül, M.; Baştürk, E.; Çiçek, E. Serum Levels of Homocysteine, Folate and Vitamin B12 in Patients with Vitiligo before and After Treatment with Narrow Band Ultraviolet B Phototherapy and in a Group of Controls. J. Photochem. Photobiol. B. 2015, 148, 174–180. [Google Scholar] [CrossRef]
- Bhatti, J.S.; Bhatti, G.K.; Reddy, P.H. Mitochondrial Dysfunction and Oxidative Stress in Metabolic Disorders—A Step Towards Mitochondria Based Therapeutic Strategies. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 1066–1077. [Google Scholar] [CrossRef]
- Mascarenhas, M.R.M.; Oliveira, M.d.C.; Oliveira, L.F.d.; Magalhães, A.S.; Machado, P.R.L. Clinical Profile of Vitiligo Patients and Relationship with Immuno-Inflammatory Markers. An. Bras. Dermatol. 2024, 99, 196–201. [Google Scholar] [CrossRef]
- Singh, R.K.; Lee, K.M.; Vujkovic-Cvijin, I.; Ucmak, D.; Farahnik, B.; Abrouk, M.; Nakamura, M.; Zhu, T.H.; Bhutani, T.; Wei, M.; et al. The Role of IL-17 in Vitiligo: A Review. Autoimmun. Rev. 2016, 15, 397–404. [Google Scholar] [CrossRef]
- Le, T.V.T.; Ngoc Phan, H.; Dang, T.N.; Pham, L.D. Increased Circulatory Interleukin-17A Levels in Patients with Progressive and Leukotrichial Vitiligo. Dermatol. Res. Pract. 2021, 2021, 5524566. [Google Scholar] [CrossRef] [PubMed]
- Acharya, P.; Mathur, M. Interleukin-17 Level in Patients with Vitiligo: A Systematic Review and Meta-Analysis. Australas. J. Dermatol. 2020, 61, e208–e212. [Google Scholar] [CrossRef] [PubMed]
- Osman, A.M.; Mukhtar, M.M.; Bakheit, K.H.; Hamdan, H.Z. Plasma Levels of Interleukin-17, Interleukin-23, and Transforming Growth Factor-Β in Sudanese Patients with Vitiligo: A Case-Control Study. Indian J. Dermatol. 2015, 60, 635. [Google Scholar] [CrossRef] [PubMed]
- Sravani, P.V.; Babu, N.K.; Gopal, K.V.T.; Rao, G.R.R.; Rao, A.R.; Moorthy, B.; Rao, T.R. Determination of Oxidative Stress in Vitiligo by Measuring Superoxide Dismutase and Catalase Levels in Vitiliginous and Non-Vitiliginous Skin. Indian J. Dermatol. Venereol. Leprol. 2009, 75, 268–271. [Google Scholar] [PubMed]
- Jain, A.; Mal, J.; Mehndiratta, V.; Chander, R.; Patra, S.K. Study of Oxidative Stress in Vitiligo. Indian. J. Clin. Biochem. 2011, 26, 78–81. [Google Scholar] [CrossRef]
- Ozel Turkcu, U.; Solak Tekin, N.; Gokdogan Edgunlu, T.; Karakas Celik, S.; Oner, S. The Association of FOXO3A Gene Polymorphisms with Serum FOXO3A Levels and Oxidative Stress Markers in Vitiligo Patients. Gene 2014, 536, 129–134. [Google Scholar] [CrossRef]
- Speeckaert, R.; van Geel, N. Vitiligo: An Update on Pathophysiology and Treatment Options. Am. J. Clin. Dermatol. 2017, 18, 733–744. [Google Scholar] [CrossRef]
- Koca, R.; Armutcu, F.; Altinyazar, H.C.; Gürel, A. Oxidant-Antioxidant Enzymes and Lipid Peroxidation in Generalized Vitiligo. Clin. Exp. Dermatol. 2004, 29, 406–409. [Google Scholar] [CrossRef]
- Khan, R.; Satyam, A.; Gupta, S.; Sharma, V.K.; Sharma, A. Circulatory Levels of Antioxidants and Lipid Peroxidation in Indian Patients with Generalized and Localized Vitiligo. Arch. Dermatol. Res. 2009, 301, 731–737. [Google Scholar] [CrossRef]
- Al-Shobaili, H.A. Update on the Genetics Characterization of Vitiligo. Int. J. Health Sci. 2011, 5, 167–179. [Google Scholar]
- Zhang, X.; Chen, J.; Liu, J. The Genetic Concept of Vitiligo. J. Dermatol. Sci. 2005, 39, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Gopal, K.V.T.; Rao, G.R.; Kumar, Y.H. Increased Prevalence of Thyroid Dysfunction and Diabetes Mellitus in Indian Vitiligo Patients: A Case-Control Study. Indian Dermatol. Online J. 2014, 5, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Afkhami-Ardekani, M.; Ghadiri-Anari, A.; Ebrahimzadeh-Ardakani, M.; Zaji, N. Prevalence of Vitiligo among Type 2 Diabetic Patients in an Iranian Population. Int. J. Dermatol. 2014, 53, 956–958. [Google Scholar] [CrossRef] [PubMed]
- Raveendra, L.; Hemavathi, R.N.; Rajgopal, S. A Study of Vitiligo in Type 2 Diabetic Patients. Indian J. Dermatol. 2017, 62, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.; Lin, M.; Huang, Y.; Hou, T. The Association between Vitiligo and Diabetes Mellitus: A Systematic Review and Meta-Analysis. J. Am. Acad. Dermatol. 2019, 81, 1442–1445. [Google Scholar] [CrossRef]
- Khalid, M.; Petroianu, G.; Adem, A. Advanced Glycation End Products and Diabetes Mellitus: Mechanisms and Perspectives. Biomolecules 2022, 12, 542. [Google Scholar] [CrossRef]
- Singh, V.P.; Bali, A.; Singh, N.; Jaggi, A.S. Advanced Glycation End Products and Diabetic Complications. Korean J. Physiol. Pharmacol. 2014, 18, 1–14. [Google Scholar] [CrossRef]
- Lee, J.; Yun, J.; Ko, S. Advanced Glycation End Products and their Effect on Vascular Complications in Type 2 Diabetes Mellitus. Nutrients 2022, 14, 3086. [Google Scholar] [CrossRef]
- Denisenko, Y.K.; Kytikova, O.Y.; Novgorodtseva, T.P.; Antonyuk, M.V.; Gvozdenko, T.A.; Kantur, T.A. Lipid-Induced Mechanisms of Metabolic Syndrome. J. Obes. 2020, 2020, 5762395. [Google Scholar] [CrossRef]
- Serhan, C.N.; Chiang, N.; Dalli, J. New Pro-Resolving N-3 Mediators Bridge Resolution of Infectious Inflammation to Tissue Regeneration. Mol. Aspects Med. 2018, 64, 1–17. [Google Scholar] [CrossRef]
- Gilroy, D.W.; Bishop-Bailey, D. Lipid Mediators in Immune Regulation and Resolution. Br. J. Pharmacol. 2019, 176, 1009–1023. [Google Scholar] [CrossRef] [PubMed]
- Lepretti, M.; Martucciello, S.; Burgos Aceves, M.A.; Putti, R.; Lionetti, L. Omega-3 Fatty Acids and Insulin Resistance: Focus on the Regulation of Mitochondria and Endoplasmic Reticulum Stress. Nutrients 2018, 10, 350. [Google Scholar] [CrossRef] [PubMed]
- Albracht-Schulte, K.; Kalupahana, N.S.; Ramalingam, L.; Wang, S.; Rahman, S.M.; Robert-McComb, J.; Moustaid-Moussa, N. Omega-3 Fatty Acids in Obesity and Metabolic Syndrome: A Mechanistic Update. J. Nutr. Biochem. 2018, 58, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Nigam, A.; Frasure-Smith, N.; Lespérance, F.; Julien, P. Relationship between N-3 and N-6 Plasma Fatty Acid Levels and Insulin Resistance in Coronary Patients with and without Metabolic Syndrome. Nutr. Metab. Cardiovasc. Dis. 2009, 19, 264–270. [Google Scholar] [CrossRef]
- Mayneris-Perxachs, J.; Guerendiain, M.; Castellote, A.I.; Estruch, R.; Covas, M.I.; Fitó, M.; Salas-Salvadó, J.; Martínez-González, M.A.; Aros, F.; Lamuela-Raventós, R.M.; et al. Plasma Fatty Acid Composition, Estimated Desaturase Activities, and their Relation with the Metabolic Syndrome in a Population at High Risk of Cardiovascular Disease. Clin. Nutr. 2014, 33, 90–97. [Google Scholar] [CrossRef]
- Zhu, Y.; Tchkonia, T.; Pirtskhalava, T.; Gower, A.C.; Ding, H.; Giorgadze, N.; Palmer, A.K.; Ikeno, Y.; Hubbard, G.B.; Lenburg, M.; et al. The Achilles’ Heel of Senescent Cells: From Transcriptome to Senolytic Drugs. Aging Cell 2015, 14, 644–658. [Google Scholar] [CrossRef]
- Ezzedine, K.; Lim, H.W.; Suzuki, T.; Katayama, I.; Hamzavi, I.; Lan, C.C.; Goh, B.K.; Anbar, T.; Silva de Castro, C.; Lee, A.Y.; et al. Revised Classification/Nomenclature of Vitiligo and Related Issues: The Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2012, 25, E1–E13. [Google Scholar] [CrossRef]
- Chiu, H.; Kuo, C. Gas Chromatography-Mass Spectrometry-Based Analytical Strategies for Fatty Acid Analysis in Biological Samples. J. Food Drug Anal. 2020, 28, 60–73. [Google Scholar] [CrossRef]
- Lepoittevin, M.; Blancart-Remaury, Q.; Kerforne, T.; Pellerin, L.; Hauet, T.; Thuillier, R. Comparison between 5 Extractions Methods in either Plasma Or Serum to Determine the Optimal Extraction and Matrix Combination for Human Metabolomics. Cell. Mol. Biol. Lett. 2023, 28, 43. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papaccio, F.; Ottaviani, M.; Truglio, M.; D’Arino, A.; Caputo, S.; Pacifico, A.; Iacovelli, P.; Di Nardo, A.; Picardo, M.; Bellei, B. Markers of Metabolic Abnormalities in Vitiligo Patients. Int. J. Mol. Sci. 2024, 25, 10201. https://doi.org/10.3390/ijms251810201
Papaccio F, Ottaviani M, Truglio M, D’Arino A, Caputo S, Pacifico A, Iacovelli P, Di Nardo A, Picardo M, Bellei B. Markers of Metabolic Abnormalities in Vitiligo Patients. International Journal of Molecular Sciences. 2024; 25(18):10201. https://doi.org/10.3390/ijms251810201
Chicago/Turabian StylePapaccio, Federica, Monica Ottaviani, Mauro Truglio, Andrea D’Arino, Silvia Caputo, Alessia Pacifico, Paolo Iacovelli, Anna Di Nardo, Mauro Picardo, and Barbara Bellei. 2024. "Markers of Metabolic Abnormalities in Vitiligo Patients" International Journal of Molecular Sciences 25, no. 18: 10201. https://doi.org/10.3390/ijms251810201






