Monoamine Oxidase Contributes to Valvular Oxidative Stress: A Prospective Observational Pilot Study in Patients with Severe Mitral Regurgitation
Abstract
1. Introduction
2. Results
2.1. Both MAO-A and -B Isoforms Are Present and Their Expression Increase in Response to ANG2 in Pathological Human Mitral Valves
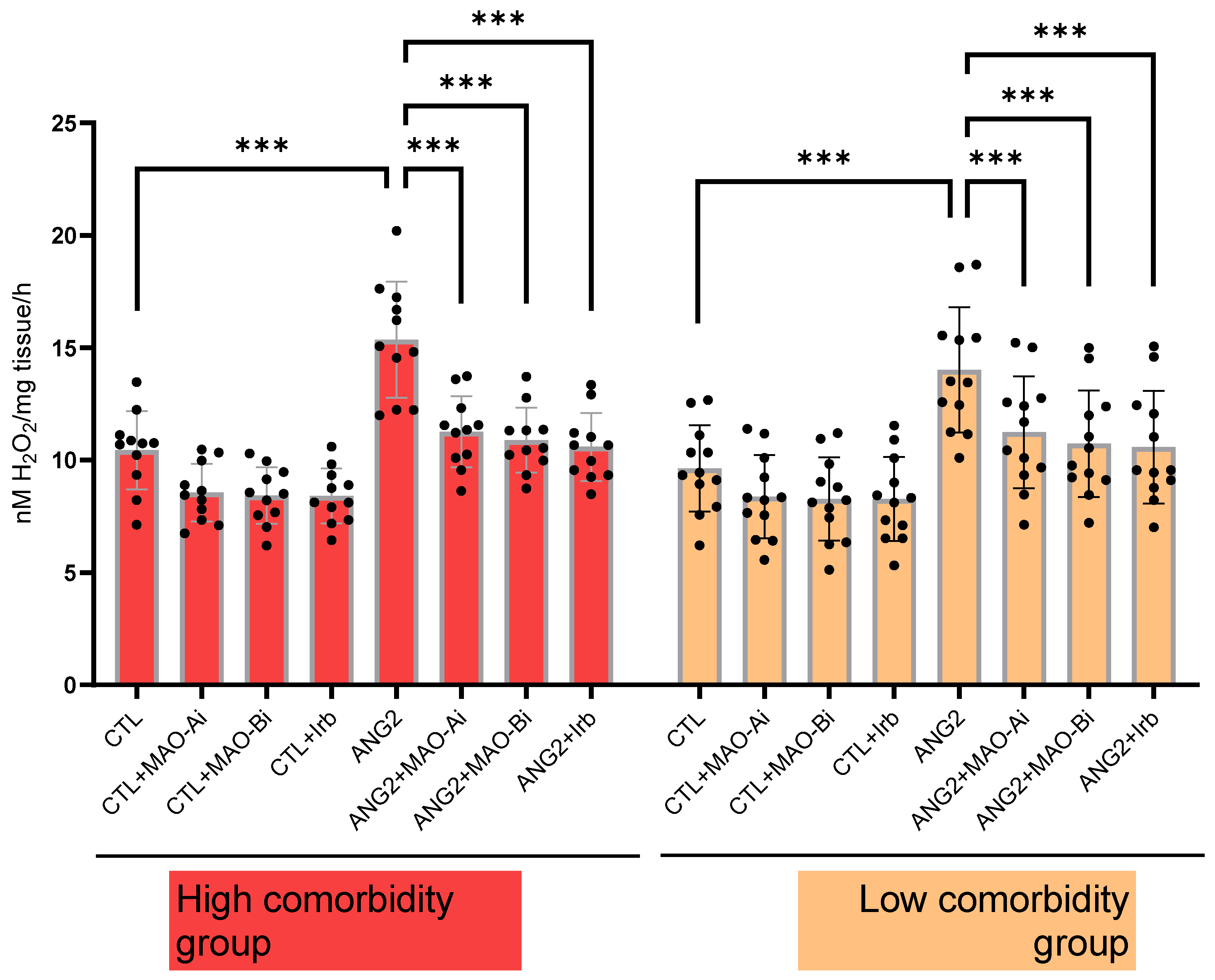
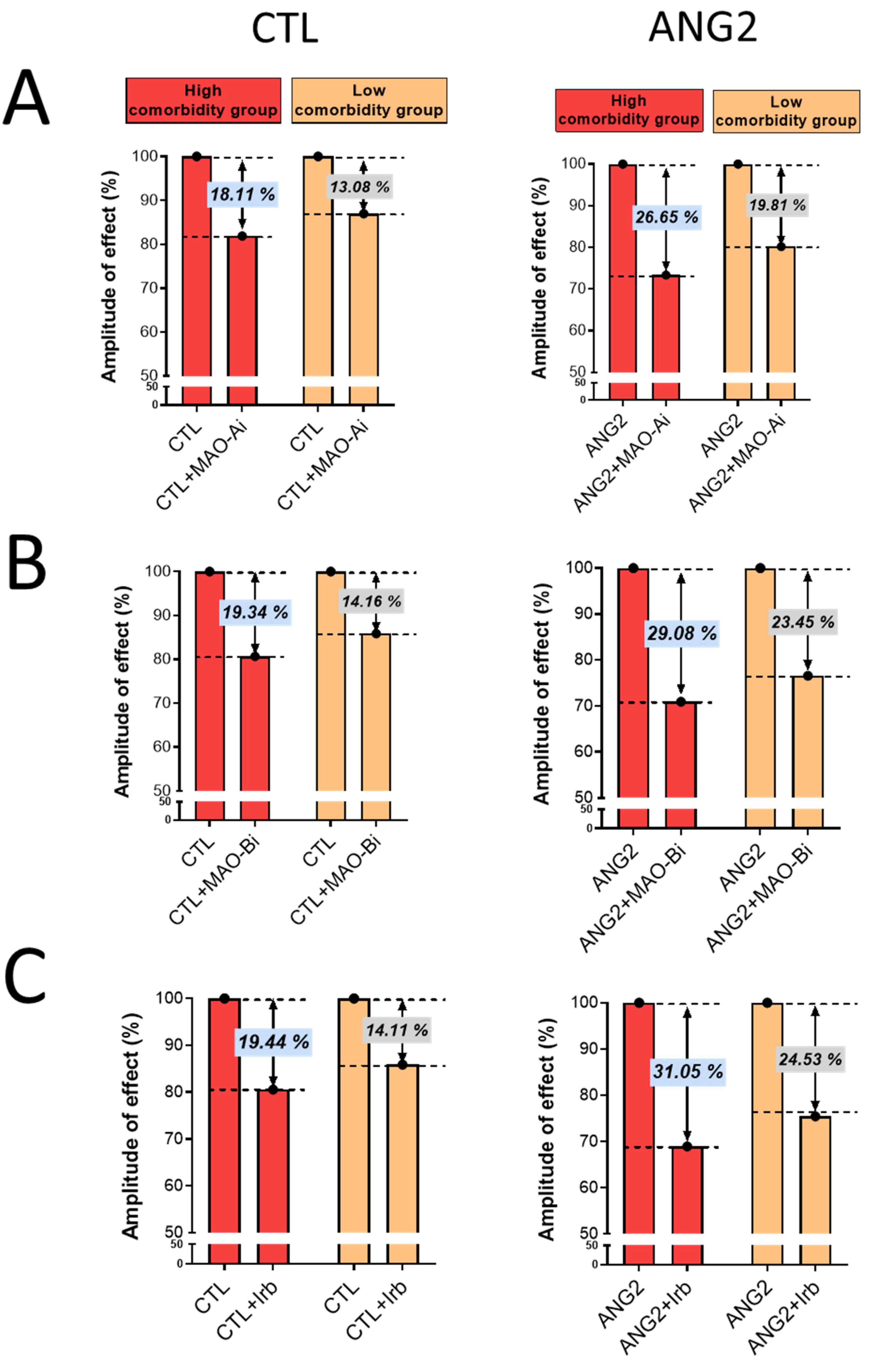
2.2. Angiotensin 2 Increased Valvular ROS Generation, an Effect Mitigated by MAO Inhibitors and the Angiotensin Receptor Blocker (ARB), Irbesartan
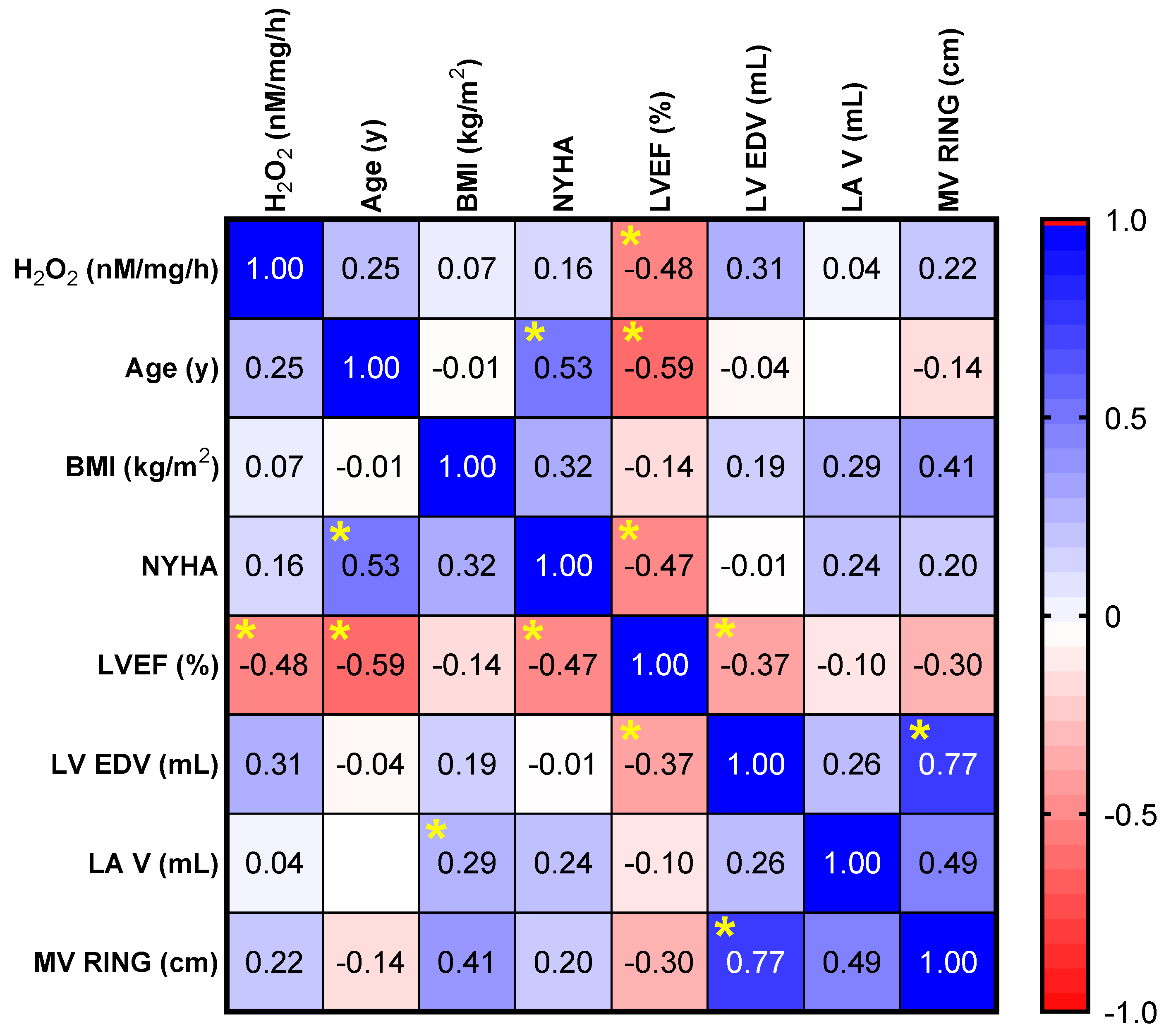
2.3. Assessment of Correlations between Valvular Oxidative Stress and Clinical and Echocardiographic Parameters
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Study Design
4.2. Preliminary Patient Evaluation
4.3. Tissue Culture
4.4. Immune Fluorescence Studies
4.5. Oxidative Stress Assessment by Means of Ferrous Iron Xylenol Orange Oxidation Assay
4.6. Real-Time Polymerase Chain Reaction (RT-PCR)
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iung, B.; Baron, G.; Butchart, E.G.; Delahaye, F.; Gohlke-Bärwolf, C.; Levang, O.W.; Tornos, P.; Vanoverschelde, J.L.; Vermeer, F.; Boersma, E.; et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur. Heart J. 2003, 24, 1231–1243. [Google Scholar] [CrossRef] [PubMed]
- Santangelo, G.; Bursi, F.; Faggiano, A.; Moscardelli, S.; Simeoli, P.S.; Guazzi, M.; Lorusso, R.; Carugo, S.; Faggiano, P. The Global Burden of Valvular Heart Disease: From Clinical Epidemiology to Management. J. Clin. Med. 2023, 12, 2178. [Google Scholar] [CrossRef] [PubMed]
- Gammie, J.S.; Chikwe, J.; Badhwar, V.; Thibault, D.P.; Vemulapalli, S.; Thourani, V.H.; Gillinov, M.; Adams, D.H.; Rankin, J.S.; Ghoreishi, M.; et al. Isolated Mitral Valve Surgery: The Society of Thoracic Surgeons Adult Cardiac Surgery Database Analysis. Ann. Thorac. Surg. 2018, 106, 716–727. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Luo, J.; Tian, X.; Zhao, Y.; Li, Y.; Wu, X. Progress in Understanding Oxidative Stress, Aging, and Aging-Related Diseases. Antioxidants 2024, 13, 394. [Google Scholar] [CrossRef] [PubMed]
- Dubois-Deruy, E.; Peugnet, V.; Turkieh, A.; Pinet, F. Oxidative Stress in Cardiovascular Diseases. Antioxidants 2020, 9, 864. [Google Scholar] [CrossRef]
- Sn, V.P.; Jaramillo, A.P.; Yasir, M.; Hussein, S.; Singareddy, S.; Iyer, N.; Nath, T.S. Hyperuricemia and Its Association With the Severity and Complications of Congestive Heart Failure: A Systematic Review. Cureus 2023, 15, e45246. [Google Scholar] [CrossRef]
- Cipriano, A.; Viviano, M.; Feoli, A.; Milite, C.; Sarno, G.; Castellano, S.; Sbardella, G. NADPH Oxidases: From Molecular Mechanisms to Current Inhibitors. J. Med. Chem. 2023, 66, 11632–11655. [Google Scholar] [CrossRef]
- Brandes, R.P.; Weissmann, N.; Schröder, K. Nox family NADPH oxidases: Molecular mechanisms of activation. Free Radic. Biol. Med. 2014, 76, 208–226. [Google Scholar] [CrossRef]
- Stamerra, C.A.; Di Giosia, P.; Giorgini, P.; Ferri, C.; Sukhorukov, V.N.; Sahebkar, A. Mitochondrial Dysfunction and Cardiovascular Disease: Pathophysiology and Emerging Therapies. Oxidative Med. Cell. Longev. 2022, 2022, 9530007. [Google Scholar] [CrossRef]
- Binda, C.; Mattevi, A.; Edmondson, D.E. Structural properties of human monoamine oxidases A and B. Int. Rev. Neurobiol. 2011, 100, 1–11. [Google Scholar] [CrossRef]
- Sturza, A.; Leisegang, M.S.; Babelova, A.; Schroder, K.; Benkhoff, S.; Loot, A.E.; Fleming, I.; Schulz, R.; Muntean, D.M.; Brandes, R.P. Monoamine oxidases are mediators of endothelial dysfunction in the mouse aorta. Hypertension 2013, 62, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Kaludercic, N.; Arusei, R.J.; Di Lisa, F. Recent advances on the role of monoamine oxidases in cardiac pathophysiology. Basic Res. Cardiol. 2023, 118, 41. [Google Scholar] [CrossRef] [PubMed]
- Kaludercic, N.; Carpi, A.; Menabò, R.; Di Lisa, F.; Paolocci, N. Monoamine oxidases (MAO) in the pathogenesis of heart failure and ischemia/reperfusion injury. Biochim. Biophys. Acta 2011, 1813, 1323–1332. [Google Scholar] [CrossRef] [PubMed]
- Sturza, A.; Duicu, O.M.; Vaduva, A.; Danila, M.D.; Noveanu, L.; Varro, A.; Muntean, D.M. Monoamine oxidases are novel sources of cardiovascular oxidative stress in experimental diabetes. Can. J. Physiol. Pharmacol. 2015, 93, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Ostadkarampour, M.; Putnins, E.E. Monoamine Oxidase Inhibitors: A Review of Their Anti-Inflammatory Therapeutic Potential and Mechanisms of Action. Front. Pharmacol. 2021, 12, 676239. [Google Scholar] [CrossRef]
- Di Lisa, F.; Kaludercic, N.; Carpi, A.; Menabò, R.; Giorgio, M. Mitochondria and vascular pathology. Pharmacol. Rep. 2009, 61, 123–130. [Google Scholar] [CrossRef]
- Schulz, R.; Schlüter, K.D. Importance of Mitochondria in Cardiac Pathologies: Focus on Uncoupling Proteins and Monoamine Oxidases. Int. J. Mol. Sci. 2023, 24, 6459. [Google Scholar] [CrossRef]
- Knittel, J.; Itani, N.; Schreckenberg, R.; Heger, J.; Rohrbach, S.; Schulz, R.; Schlüter, K.D. Monoamine Oxidase A Contributes to Serotonin-But Not Norepinephrine-Dependent Damage of Rat Ventricular Myocytes. Biomolecules 2023, 13, 1013. [Google Scholar] [CrossRef]
- Kaludercic, N.; Mialet-Perez, J.; Paolocci, N.; Parini, A.; Di Lisa, F. Monoamine oxidases as sources of oxidants in the heart. J. Mol. Cell. Cardiol. 2014, 73, 34–42. [Google Scholar] [CrossRef]
- Shi, Q.; Malik, H.; Crawford, R.M.; Streeter, J.; Wang, J.; Huo, R.; Shih, J.C.; Chen, B.; Hall, D.; Abel, E.D.; et al. Cardiac MAO-A inhibition protects against catecholamine-induced ventricular arrhythmias via enhanced diastolic calcium control. Cardiovasc. Res. 2024, 120, 596–611. [Google Scholar] [CrossRef]
- Wu, C.H.; Mohammadmoradi, S.; Chen, J.Z.; Sawada, H.; Daugherty, A.; Lu, H.S. Renin-Angiotensin System and Cardiovascular Functions. Arterioscler. Thromb. Vasc. Biol. 2018, 38, e108–e116. [Google Scholar] [CrossRef] [PubMed]
- Khatib, R.; Joseph, P.; Briel, M.; Yusuf, S.; Healey, J. Blockade of the renin-angiotensin-aldosterone system (RAAS) for primary prevention of non-valvular atrial fibrillation: A systematic review and meta analysis of randomized controlled trials. Int. J. Cardiol. 2013, 165, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Fernández, B.E.; Domínguez, A.E. Angiotensin II increases MAO activity in rat central nervous system. Rev. Esp. Fisiol. 1991, 47, 37–40. [Google Scholar] [PubMed]
- Lascu, A.; Ionică, L.N.; Buriman, D.G.; Merce, A.P.; Deaconu, L.; Borza, C.; Crețu, O.M.; Sturza, A.; Muntean, D.M.; Feier, H.B. Metformin and empagliflozin modulate monoamine oxidase-related oxidative stress and improve vascular function in human mammary arteries. Mol. Cell. Biochem. 2023, 478, 1939–1947. [Google Scholar] [CrossRef] [PubMed]
- Manni, M.E.; Zazzeri, M.; Musilli, C.; Bigagli, E.; Lodovici, M.; Raimondi, L. Exposure of cardiomyocytes to angiotensin II induces over-activation of monoamine oxidase type A: Implications in heart failure. Eur. J. Pharmacol. 2013, 718, 271–276. [Google Scholar] [CrossRef]
- Rouzaud-Laborde, C.; Delmas, C.; Pizzinat, N.; Tortosa, F.; Garcia, C.; Mialet-Perez, J.; Payrastre, B.; Sié, P.; Spreux-Varoquaux, O.; Sallerin, B.; et al. Platelet activation and arterial peripheral serotonin turnover in cardiac remodeling associated to aortic stenosis. Am. J. Hematol. 2015, 90, 15–19. [Google Scholar] [CrossRef]
- Lascu, A.; Șoșdean, R.; Ionică, L.N.; Pescariu, A.S.; Petrescu, L.; Ionac, A.; Luca, C.T.; Sturza, A.; Feier, H.B. Monoamine Oxidase (MAO) Is Expressed at the Level of Mitral Valve with Severe Regurgitation in Hypertrophic Obstructive Cardiomyopathy: A Case Report. Medicina 2022, 58, 1844. [Google Scholar] [CrossRef]
- Goldberg, E.; Grau, J.B.; Fortier, J.H.; Salvati, E.; Levy, R.J.; Ferrari, G. Serotonin and catecholamines in the development and progression of heart valve diseases. Cardiovasc. Res. 2017, 113, 849–857. [Google Scholar] [CrossRef]
- Pimentel, D.R.; Amin, J.K.; Xiao, L.; Miller, T.; Viereck, J.; Oliver-Krasinski, J.; Baliga, R.; Wang, J.; Siwik, D.A.; Singh, K.; et al. Reactive oxygen species mediate amplitude-dependent hypertrophic and apoptotic responses to mechanical stretch in cardiac myocytes. Circ. Res. 2001, 89, 453–460. [Google Scholar] [CrossRef]
- Zhang, Y.; Murugesan, P.; Huang, K.; Cai, H. NADPH oxidases and oxidase crosstalk in cardiovascular diseases: Novel therapeutic targets. Nat. Rev. Cardiol. 2020, 17, 170–194. [Google Scholar] [CrossRef]
- Daiber, A.; Steven, S.; Vujacic-Mirski, K.; Kalinovic, S.; Oelze, M.; Di Lisa, F.; Münzel, T. Regulation of Vascular Function and Inflammation via Cross Talk of Reactive Oxygen and Nitrogen Species from Mitochondria or NADPH Oxidase-Implications for Diabetes Progression. Int. J. Mol. Sci. 2020, 21, 3405. [Google Scholar] [CrossRef]
- Youn, J.Y.; Zhang, J.; Zhang, Y.; Chen, H.; Liu, D.; Ping, P.; Weiss, J.N.; Cai, H. Oxidative stress in atrial fibrillation: An emerging role of NADPH oxidase. J. Mol. Cell. Cardiol. 2013, 62, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.P.; Chen, M.C.; Liu, W.H.; Yang, C.H.; Chen, C.J.; Chen, Y.L.; Pan, K.L.; Tsai, T.H.; Chang, H.W. Atrial myocardial nox2 containing NADPH oxidase activity contribution to oxidative stress in mitral regurgitation: Potential mechanism for atrial remodeling. Cardiovasc. Pathol. 2011, 20, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Gladden, J.D.; Ahmed, M.I.; Litovsky, S.H.; Schiros, C.G.; Lloyd, S.G.; Gupta, H.; Denney, T.S., Jr.; Darley-Usmar, V.; McGiffin, D.C.; Dell’Italia, L.J. Oxidative stress and myocardial remodeling in chronic mitral regurgitation. Am. J. Med. Sci. 2011, 342, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Hagler, M.A.; Hadley, T.M.; Zhang, H.; Mehra, K.; Roos, C.M.; Schaff, H.V.; Suri, R.M.; Miller, J.D. TGF-β signalling and reactive oxygen species drive fibrosis and matrix remodelling in myxomatous mitral valves. Cardiovasc. Res. 2013, 99, 175–184. [Google Scholar] [CrossRef]
- Songia, P.; Porro, B.; Chiesa, M.; Myasoedova, V.; Alamanni, F.; Tremoli, E.; Poggio, P. Identification of Patients Affected by Mitral Valve Prolapse with Severe Regurgitation: A Multivariable Regression Model. Oxidative Med. Cell. Longev. 2017, 2017, 6838921. [Google Scholar] [CrossRef]
- Anderson, E.J.; Efird, J.T.; Davies, S.W.; O’Neal, W.T.; Darden, T.M.; Thayne, K.A.; Katunga, L.A.; Kindell, L.C.; Ferguson, T.B.; Anderson, C.A.; et al. Monoamine oxidase is a major determinant of redox balance in human atrial myocardium and is associated with postoperative atrial fibrillation. J. Am. Heart Assoc. 2014, 3, e000713. [Google Scholar] [CrossRef]
- Reina-Couto, M.; Afonso, J.; Carvalho, J.; Morgado, L.; Ronchi, F.A.; de Oliveira Leite, A.P.; Dias, C.C.; Casarini, D.E.; Bettencourt, P.; Albino-Teixeira, A.; et al. Interrelationship between renin-angiotensin-aldosterone system and oxidative stress in chronic heart failure patients with or without renal impairment. Biomed. Pharmacother. 2021, 133, 110938. [Google Scholar] [CrossRef]
- Dikalov, S.I.; Dikalova, A.E.; Bikineyeva, A.T.; Schmidt, H.H.; Harrison, D.G.; Griendling, K.K. Distinct roles of Nox1 and Nox4 in basal and angiotensin II-stimulated superoxide and hydrogen peroxide production. Free Radic. Biol. Med. 2008, 45, 1340–1351. [Google Scholar] [CrossRef]
- Kruithof, B.P.T.; Paardekooper, L.; Hiemstra, Y.L.; Goumans, M.J.; Palmen, M.; Delgado, V.; Klautz, R.J.M.; Ajmone Marsan, N. Stress-induced remodelling of the mitral valve: A model for leaflet thickening and superimposed tissue formation in mitral valve disease. Cardiovasc. Res. 2020, 116, 931–943. [Google Scholar] [CrossRef]
- Oyama, M.A.; Elliott, C.; Loughran, K.A.; Kossar, A.P.; Castillero, E.; Levy, R.J.; Ferrari, G. Comparative pathology of human and canine myxomatous mitral valve degeneration: 5HT and TGF-β mechanisms. Cardiovasc. Pathol. 2020, 46, 107196. [Google Scholar] [CrossRef] [PubMed]
- Peña-Silva, R.A.; Miller, J.D.; Chu, Y.; Heistad, D.D. Serotonin produces monoamine oxidase-dependent oxidative stress in human heart valves. Am. J. Physiol. Circ. Physiol. 2009, 297, H1354–H1360. [Google Scholar] [CrossRef] [PubMed]
- Higashi, Y. Roles of Oxidative Stress and Inflammation in Vascular Endothelial Dysfunction-Related Disease. Antioxidants 2022, 11, 1958. [Google Scholar] [CrossRef]
- Levine, R.A.; Hagége, A.A.; Judge, D.P.; Padala, M.; Dal-Bianco, J.P.; Aikawa, E.; Beaudoin, J.; Bischoff, J.; Bouatia-Naji, N.; Bruneval, P.; et al. Mitral valve disease—Morphology and mechanisms. Nat. Rev. Cardiol. 2015, 12, 689–710. [Google Scholar] [CrossRef] [PubMed]
- Eleid, M.F.; Nkomo, V.T.; Pislaru, S.V.; Gersh, B.J. Valvular Heart Disease: New Concepts in Pathophysiology and Therapeutic Approaches. Annu. Rev. Med. 2023, 74, 155–170. [Google Scholar] [CrossRef]
- Asgar, A.W.; Mack, M.J.; Stone, G.W. Secondary mitral regurgitation in heart failure: Pathophysiology, prognosis, and therapeutic considerations. J. Am. Coll. Cardiol. 2015, 65, 1231–1248. [Google Scholar] [CrossRef]
- Schoen, F.J. Evolving concepts of cardiac valve dynamics: The continuum of development, functional structure, pathobiology, and tissue engineering. Circulation 2008, 118, 1864–1880. [Google Scholar] [CrossRef]
- Corporan, D.; Onohara, D.; Amedi, A.; Saadeh, M.; Guyton, R.A.; Kumar, S.; Padala, M. Hemodynamic and transcriptomic studies suggest early left ventricular dysfunction in a preclinical model of severe mitral regurgitation. J. Thorac. Cardiovasc. Surg. 2021, 161, 961–976.e22. [Google Scholar] [CrossRef]
- Topilsky, Y. Mitral Regurgitation: Anatomy, Physiology, and Pathophysiology-Lessons Learned From Surgery and Cardiac Imaging. Front. Cardiovasc. Med. 2020, 7, 84. [Google Scholar] [CrossRef]
- Tsutsui, H.; Shimokawa, T.; Miura, T.; Takama, M.; Nishinaka, T.; Terada, T.; Yamagata, M.; Yukimura, T. Effect of monoamine oxidase inhibitors on ischaemia/reperfusion-induced acute kidney injury in rats. Eur. J. Pharmacol. 2018, 818, 38–42. [Google Scholar] [CrossRef]
- Dominguez, J.; Troncoso, P.; Martinez, L. Monoamine oxidase inhibition prevents ischemia reperfusion damage in rat kidneys. Transplant. Proc. 1995, 27, 1839–1842. [Google Scholar]
- Sturza, A.; Popoiu, C.M.; Ionică, M.; Duicu, O.M.; Olariu, S.; Muntean, D.M.; Boia, E.S. Monoamine Oxidase-Related Vascular Oxidative Stress in Diseases Associated with Inflammatory Burden. Oxidative Med. Cell. Longev. 2019, 2019, 8954201. [Google Scholar] [CrossRef] [PubMed]
- Niveta, J.P.S.; John, C.M.; Arockiasamy, S. Monoamine oxidase mediated oxidative stress: A potential molecular and biochemical crux in the pathogenesis of obesity. Mol. Biol. Rep. 2023, 51, 29. [Google Scholar] [CrossRef] [PubMed]
- Sturza, A.; Muntean, D.M.; Crețu, O.M. Monoamine Oxidase, Obesity and Related Comorbidities: Discovering Bonds. In Cellular and Biochemical Mechanisms of Obesity; Tappia, P.S., Ramjiawan, B., Dhalla, N.S., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 199–213. [Google Scholar] [CrossRef]
- Maggiorani, D.; Manzella, N.; Edmondson, D.E.; Mattevi, A.; Parini, A.; Binda, C.; Mialet-Perez, J. Monoamine Oxidases, Oxidative Stress, and Altered Mitochondrial Dynamics in Cardiac Ageing. Oxid. Med. Cell. Longev. 2017, 2017, 3017947. [Google Scholar] [CrossRef] [PubMed]
- Zorov, D.B.; Juhaszova, M.; Sollott, S.J. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol. Rev. 2014, 94, 909–950. [Google Scholar] [CrossRef]
- Rhee, S.G.; Chang, T.-S.; Jeong, W.; Kang, D. Methods for Detection and Measurement of Hydrogen Peroxide Inside and Outside of Cells. Mol. Cells 2010, 29, 539–549. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Lancellotti, P.; Tribouilloy, C.; Hagendorff, A.; Popescu, B.A.; Edvardsen, T.; Pierard, L.A.; Badano, L.; Zamorano, J.L. Recommendations for the echocardiographic assessment of native valvular regurgitation: An executive summary from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 611–644. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Tsang, W.; Adams, D.H.; Agricola, E.; Buck, T.; Faletra, F.F.; Franke, A.; Hung, J.; de Isla, L.P.; et al. EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. Eur. Heart J. Cardiovasc. Imaging 2012, 13, 1–46. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]


| Clinical Parameter | |
|---|---|
| Age, years, mean ± STD | 62.8 ± 12.62 |
| Sex, M/F, n (%) | 20 (66.66%)/10 (33.33%) |
| Body mass index, kg/m2, mean ± STD | 28.26 ± 4.02 |
| NYHA class | |
| II | 10 (33.33%) |
| III | 20 (66.66%) |
| Atrial fibrillation, n (%) | 11 (36.66%) |
| Arterial hypertension, n (%) | 22 (73.33%) |
| Diabetes mellitus, n (%) | 2 (6.66%) |
| Chronic kidney disease, n (%) | 1 (3.33%) |
| Coronary artery disease, n (%) | 6 (20%) |
| Obesity, n (%) | 10 (33.33%) |
| Dyslipidemia, n (%) | 13 (43.33%) |
| Smoking, n (%) | 5 (16.66%) |
| Medication | |
| RAAS inhibitors, n (%) | 7 (23.33%) |
| Beta-blockers, n (%) | 20 (66.66%) |
| MRI, n (%) | 21 (70%) |
| Statins, n (%) | 11 (36.66%) |
| Antidiabetic drugs, n (%) | 2 (6.66%) |
| Insulin, n (%) | 0 (0%) |
| Blood Test | |
|---|---|
| Leukocytes, n/mm3 | 7505.33 ± 1841.45 |
| Hemoglobin, g/dL | 14.22 ± 1.44 |
| Erythrocytes sedimentation rate, mm/h | 13.53 ± 10.33 |
| Creatinine, mg/dL | 0.96 ± 0.17 |
| Aspartate aminotransferase, IU/L | 23.93 ± 6.9 |
| Alanine aminotransferase, IU/L | 26.86 ± 13.03 |
| Fasting blood glucose, mg/dL | 101.73 ± 15.88 |
| Total cholesterol, mg/dL | 177.8 ± 47.63 |
| LDL cholesterol, mg/dL | 110.73 ± 37.11 |
| Triglycerides, mg/dL | 155.66 ± 117.71 |
| Echocardiographic Parameter | |
|---|---|
| LV EDD, mm | 5.42 ± 0.73 |
| Indexed LV EDD, mm/m2 | 2.83 ± 0.42 |
| LV EDV, mL | 156.1 ± 51.55 |
| Indexed LV EDV, mL/m2 | 81.25 ± 26.42 |
| LV EF, % | 55.16 ± 8.9 |
| LVPW, mm | 1.07 ± 0.16 |
| IVS, mm | 1.21 ± 0.26 |
| LA antero-posterior diameter, mm | 4.99 ± 0.65 |
| LA volume, mL | 131.23 ± 46.16 |
| Indexed LA volume, mL/m2 | 68.01 ± 22.09 |
| Mitral valve ring diameter, mm | 4.20 ± 0.61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Șoșdean, R.; Dănilă, M.D.; Ionică, L.N.; Pescariu, A.S.; Mircea, M.; Ionac, A.; Mornoș, C.; Luca, C.T.; Feier, H.B.; Muntean, D.M.; et al. Monoamine Oxidase Contributes to Valvular Oxidative Stress: A Prospective Observational Pilot Study in Patients with Severe Mitral Regurgitation. Int. J. Mol. Sci. 2024, 25, 10307. https://doi.org/10.3390/ijms251910307
Șoșdean R, Dănilă MD, Ionică LN, Pescariu AS, Mircea M, Ionac A, Mornoș C, Luca CT, Feier HB, Muntean DM, et al. Monoamine Oxidase Contributes to Valvular Oxidative Stress: A Prospective Observational Pilot Study in Patients with Severe Mitral Regurgitation. International Journal of Molecular Sciences. 2024; 25(19):10307. https://doi.org/10.3390/ijms251910307
Chicago/Turabian StyleȘoșdean, Raluca, Maria D. Dănilă, Loredana N. Ionică, Alexandru S. Pescariu, Monica Mircea, Adina Ionac, Cristian Mornoș, Constantin T. Luca, Horea B. Feier, Danina M. Muntean, and et al. 2024. "Monoamine Oxidase Contributes to Valvular Oxidative Stress: A Prospective Observational Pilot Study in Patients with Severe Mitral Regurgitation" International Journal of Molecular Sciences 25, no. 19: 10307. https://doi.org/10.3390/ijms251910307
APA StyleȘoșdean, R., Dănilă, M. D., Ionică, L. N., Pescariu, A. S., Mircea, M., Ionac, A., Mornoș, C., Luca, C. T., Feier, H. B., Muntean, D. M., & Sturza, A. (2024). Monoamine Oxidase Contributes to Valvular Oxidative Stress: A Prospective Observational Pilot Study in Patients with Severe Mitral Regurgitation. International Journal of Molecular Sciences, 25(19), 10307. https://doi.org/10.3390/ijms251910307







