Biallelic Loss of 7q34 (TRB) and 9p21.3 (CDKN2A/2B) in Adult Ph-Negative Acute T-Lymphoblastic Leukemia
Abstract
1. Introduction
2. Results
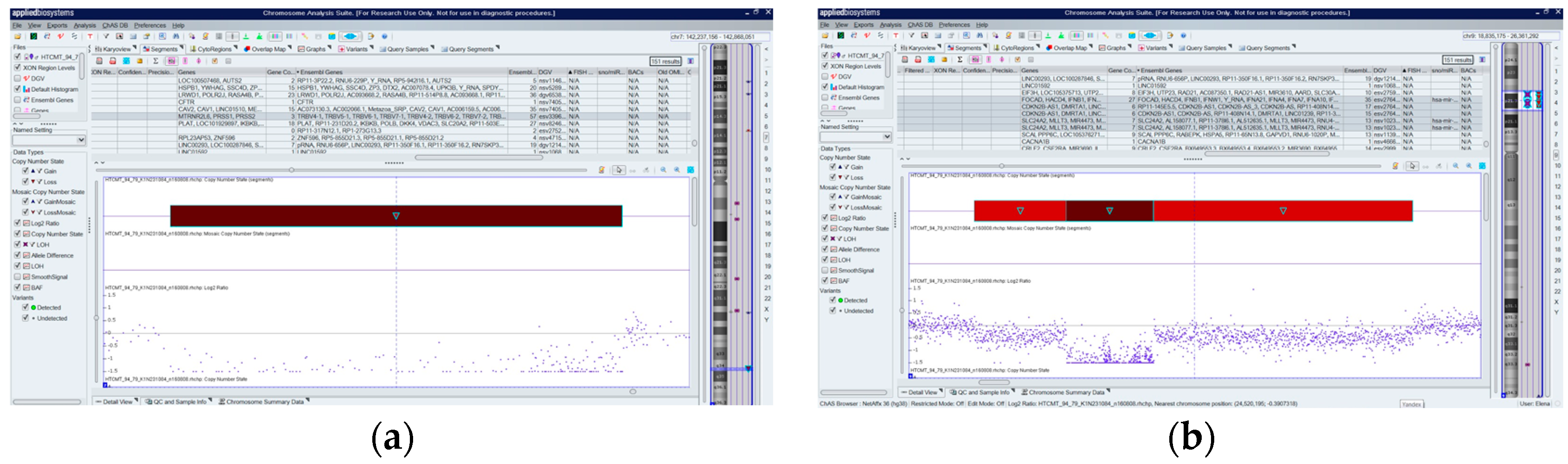
2.1. Biallelic Deletions in the Study Cohort
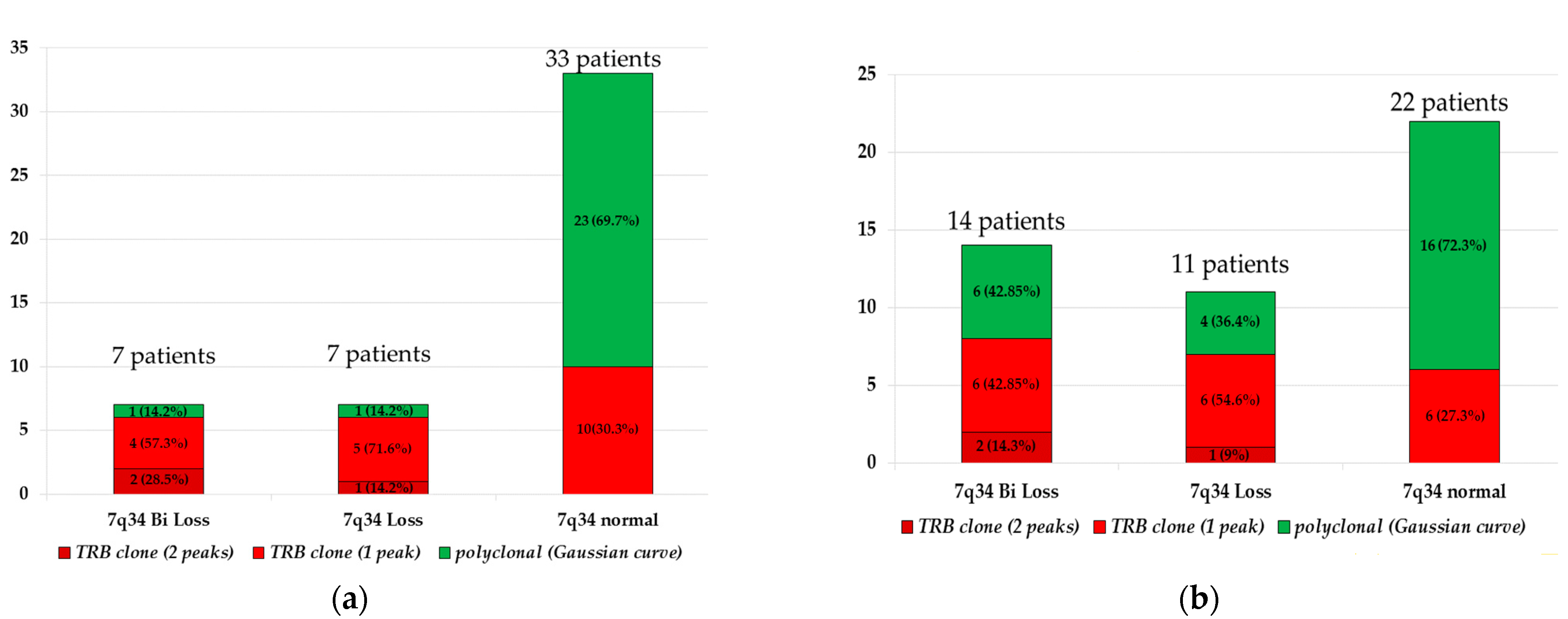
2.2. Association between 7q34 Loss and Clonal TRB Rearrangement
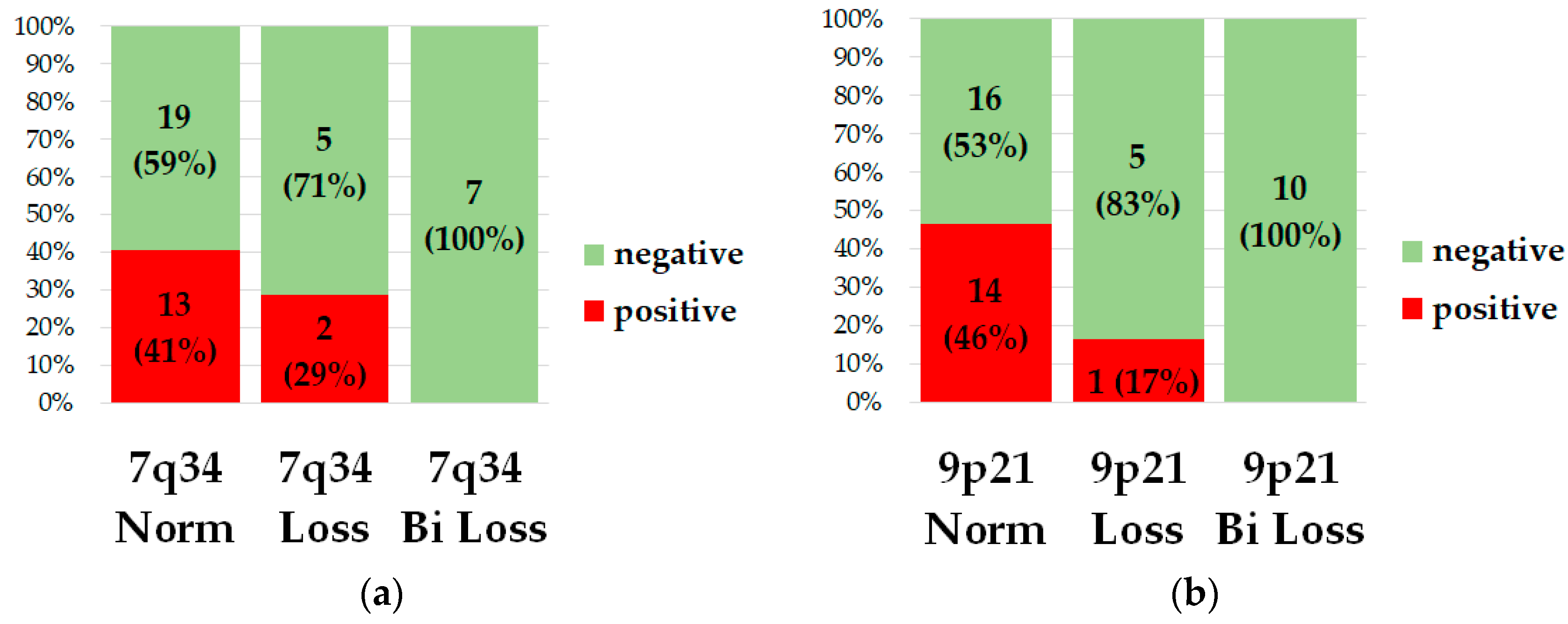
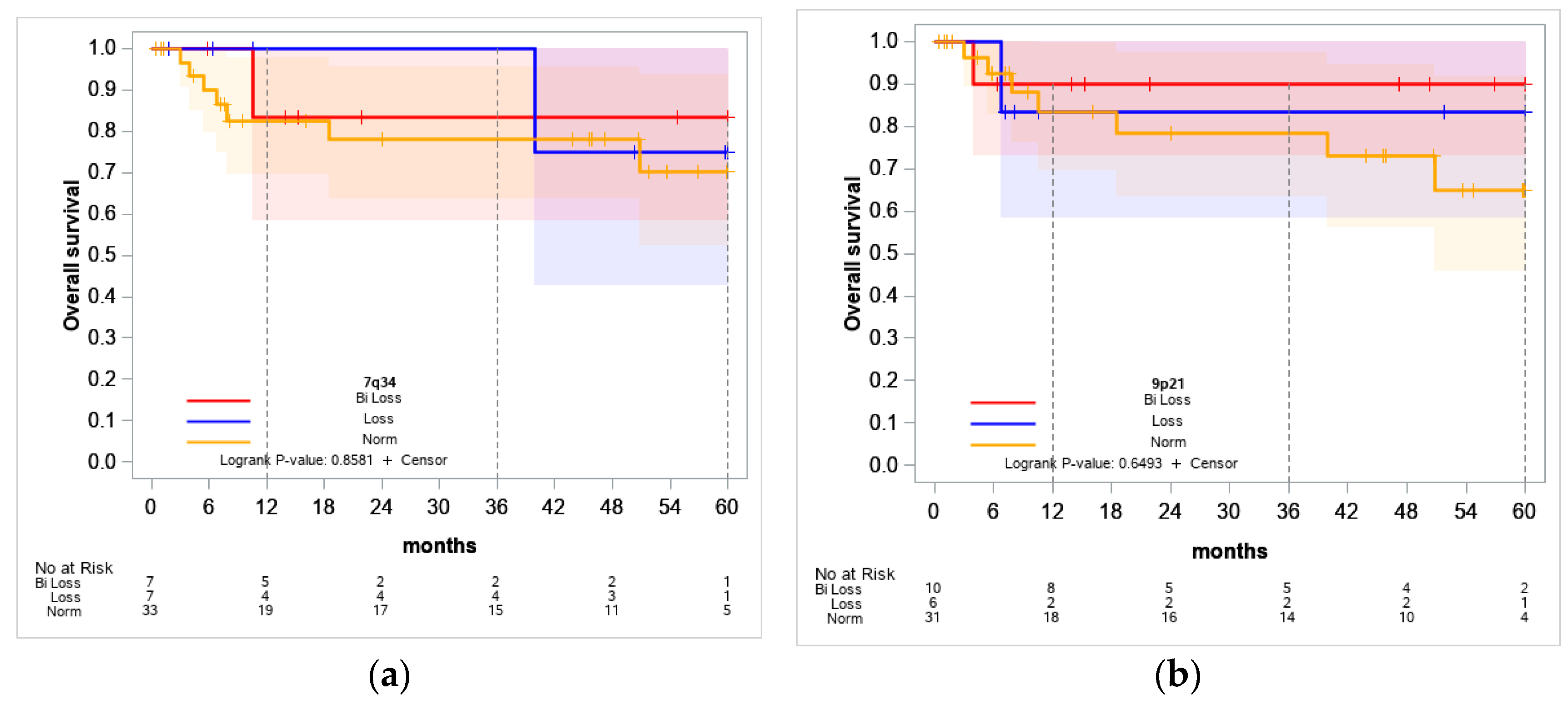
2.3. Association between 7q34 and 9p21.3 Losses and MRD Status at Day 70
3. Discussion
4. Materials and Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gianni, F.; Belver, L.; Ferrando, A. The Genetics and Mechanisms of T-Cell Acute Lymphoblastic Leukemia. Cold Spring Harb. Perspect. Med. 2020, 10, a035246. [Google Scholar] [CrossRef] [PubMed]
- De Bie, J.; Quessada, J.; Tueur, G.; Lefebvre, C.; Luquet, I.; Toujani, S.; Cuccuini, W.; Lafage-Pochitaloff, M.; Michaux, L. Cytogenetics in the management of T-cell acute lymphoblastic leukemia (T-ALL): Guidelines from the Groupe Francophone de Cytogénétique Hématologique (GFCH). Curr. Res. Transl. Med. 2023, 71, 103431. [Google Scholar] [CrossRef] [PubMed]
- Girardi, T.; Vicente, C.; Cools, J.; De Keersmaecker, K. The genetics and molecular biology of T-ALL. Blood 2017, 129, 1113–1123. [Google Scholar] [CrossRef] [PubMed]
- Van Vlierberghe, P.; Ambesi-Impiombato, A.; De Keersmaecker, K.; Hadler, M.; Paietta, E.; Tallman, M.S.; Rowe, J.M.; Forne, C.; Rue, M.; Ferrando, A.A. Prognostic relevance of integrated genetic profiling in adult T-cell acute lymphoblastic leukemia. Blood 2013, 122, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Parovichnikova, E.N.; Aleshina, O.A.; Troitskaya, V.V.; Chabaeva, Y.A.; Sokolov, A.N.; Isinova, G.A.; Kotova, E.S.; Akhmerzaeva, Z.H.; Klyasova, G.A.; Galtseva, I.V.; et al. Comparison of the treatment results in adult patients with acute Ph-negative lymphoblastic leukemia on protocols of the Russian multicenter studies ALL-2009 and ALL-2016. Russ. J. Hematol. Transfusiol. 2022, 67, 460–477. (In Russian) [Google Scholar] [CrossRef]
- Schoumans, J.; Suela, J.; Hastings, R.; Muehlematter, D.; Rack, K.; van den Berg, E.; Berna Beverloo, H.; Stevens-Kroef, M. Guidelines for genomic array analysis in acquired haematological neoplastic disorders. Genes Chromosomes Cancer 2016, 55, 480–491. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, P.R.; Andersen, E.F.; Brown, T.R.; Horner, V.L.; Horwitz, J.; Rehder, C.W.; Rudy, N.L.; Robin, N.H.; Thorland, E.C.; On behalf of the Acmg Laboratory Quality Assurance Committee. Interpretation and reporting of large regions of homozygosity and suspected consanguinity/uniparental disomy, 2021 revision: A technical standard of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. Off. J. Am. Coll. Med. Genet. 2022, 24, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Kuang, P.; Liu, T. Prognostic significance of CDKN2A/B deletions in acute lymphoblastic leukaemia: A meta-analysis. Ann. Med. 2019, 51, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.P.; Zhou, Y.L.; Huang, X.; Zhang, Y.; Qian, J.J.; Li, J.H.; Li, X.Y.; Li, C.Y.; Lou, Y.J.; Mai, W.Y.; et al. CDKN2A deletions are associated with poor outcomes in 101 adults with T-cell acute lymphoblastic leukemia. Am. J. Hematol. 2021, 96, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Remke, M.; Pfister, S.; Kox, C.; Toedt, G.; Becker, N.; Benner, A.; Werft, W.; Breit, S.; Liu, S.; Engel, F.; et al. High-resolution genomic profiling of childhood T-ALL reveals frequent copy-number alterations affecting the TGF-beta and PI3K-AKT pathways and deletions at 6q15-16.1 as a genomic marker for unfavorable early treatment response. Blood 2009, 114, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- TRB T Cell Receptor Beta Locus [Homo Sapiens (Human)] Gene ID: 6957. Available online: https://www.ncbi.nlm.nih.gov/gene/6957 (accessed on 17 August 2024).
- Risinskaya, N.; Gladysheva, M.; Abdulpatakhov, A.; Chabaeva, Y.; Surimova, V.; Aleshina, O.; Yushkova, A.; Dubova, O.; Kapranov, N.; Galtseva, I.; et al. DNA Copy Number Alterations and Copy Neutral Loss of Heterozygosity in Adult Ph-Negative Acute B-Lymphoblastic Leukemia: Focus on the Genes Involved. Int. J. Mol. Sci. 2023, 24, 17602. [Google Scholar] [CrossRef] [PubMed]
- Raimondi, S. Acute T-type lymphoblastic leukemia (T-ALL). Atlas Genet. Cytogenet. Oncol. Hematol. 2007, 11, 328–339. Available online: http://atlasgeneticsoncology.org/haematological/1374/t-lineage-acute-lymphoblastic-leukemia-(t-all) (accessed on 20 August 2024).
- Yamamoto, K.; Nakamachi, Y.; Yakushijin, K.; Miyata, Y.; Okamura, A.; Kawano, S.; Matsuoka, H.; Minami, H. A novel TRB@/NOTCH1 fusion gene in T-cell lymphoblastic lymphoma with t(7;9)(q34;q34). Eur. J. Haematol. 2013, 90, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Bardelli, V.; Arniani, S.; Pierini, V.; Di Giacomo, D.; Pierini, T.; Gorello, P.; Mecucci, C.; La Starza, R. T-Cell Acute Lymphoblastic Leukemia: Biomarkers and Their Clinical Usefulness. Genes 2021, 12, 1118. [Google Scholar] [CrossRef]
- Homminga, I.; Vuerhard, M.J.; Langerak, A.W.; Buijs-Gladdines, J.; Pieters, R.; Meijerink, J.P. Characterization of a pediatric T-cell acute lymphoblastic leukemia patient with simultaneous LYL1 and LMO2 rearrangements. Haematologica 2012, 97, 258–261. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Müller, J.; Walter, W.; Haferlach, C.; Müller, H.; Fuhrmann, I.; Müller, M.L.; Ruge, H.; Meggendorfer, M.; Kern, W.; Haferlach, T.; et al. How T-lymphoblastic leukemia can be classified based on genetics using standard diagnostic techniques enhanced by whole genome sequencing. Leukemia 2023, 37, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Pasquini, A.; Ciolli, G.; Mannelli, F.; Scappini, B.; Gianfaldoni, G.; Pilerci, S.; Fasano, L.; Quinti, E.; Paradiso, V.; Crupi, F.; et al. ALL-256 Nelarabine, Etoposide, and Cyclophosphamide for Adult T Cell Acute Lymphoblastic Leukemia/Lymphoma Relapsing After Pediatric-Inspired Frontline Approaches: Report of 3 Cases From a Real-Life Setting. Acute Lymphoblastic Leuk. 2023, 23 (Suppl. S1), S242–S243. [Google Scholar] [CrossRef]
- McGowan-Jordan, J.; Ros, J. ISCN 2020: An International System for Human Cytogenomic Nomenclature, 1st ed.; S. Karger AG: Basel, Switzerland, 2020. [Google Scholar]
- Porwit-MacDonald, A.; Björklund, E.; Lánczky, A.; Tsao, L.; Fioretos, T.; Bahram, F.; Book, M.; Wang, Y.-H.; Kim, W.Y.; Hasselblom, S.; et al. Genomic features of T-cell acute lymphoblastic leukemia patients harboring NUP214-ABL1 or ETV6-JAK2 fusions. Blood Cancer J. 2022, 12, 7. [Google Scholar]
- van Dongen, J.J.; Langerak, A.W.; Brüggemann, M.; Evans, P.A.; Hummel, M.; Lavender, F.L.; Delabesse, E.; Davi, F.; Schuuring, E.; García-Sanz, R.; et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: Report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 2003, 17, 2257–2317. [Google Scholar] [CrossRef] [PubMed]


| Parameters | T-ALL (n = 47) |
|---|---|
| Male:Female | 34:13 |
| Age, median | 33 (19–53) years |
| Leukocytes, 109/L | 44.59 (0.95–833.94) |
| LDH | 1 207 (154–20,064) |
| Blast cells in peripheral blood, % | 75 (0–97) |
| Blast cells in the bone marrow, % | 86 (5.2–100) |
| Immunophenotype, EGIL, WHO | T-I 6 (12.7%) |
| T-II 16 (34%) | |
| T-III 21 (44.6%) | |
| T-IV 1 (2.1%) MPAL(T-myelo) 3 (6.4%) | |
| Standard cytogenetics | 47 |
| +mitosis | 44 (93.6%) |
| −mitosis | 3 (6.4%) |
| Karyotype | 44 |
| Normal | 20 (20.0%) |
| Abnormal: | 24 (80.0%) |
| CNS leukemia | 10 (21.3%) |
| Extramedullary disease | 34 (72.3%) |
| MRD-status (+70 day) | 46 |
| MRD+ | 13 |
| MRD− | 33 |
| CR: | |
| After 2nd induction (+70 day) | 16 |
| Refractory disease | 14 |
| Early Death | 1 |
| Patient# | Age | Gender | Immunophenotype | % of Blast Cells in Bone Marrow | 9p21.3 (Start-End Position of Genomic Coordinates) | 7q34 (Start-End Position of Genomic Coordinates) | 12p13.2 (Start-End Position of Genomic Coordinates) | 13q14.2 (Start-End Position of Genomic Coordinates) |
|---|---|---|---|---|---|---|---|---|
| 12 | 47 | m | T-III | 80.1 | 9p21.3(21972814_22025494)x0 | 7q34(142610489_142796623)x0 | ||
| 14 | 40 | m | T-II | 84.9 | 7q34(142538468_142787265)x0, 7q34q36.1(142792254_151451166)x1 | |||
| 15 | 23 | m | T-III | 96.5 | 7q34(142438198_142787265)x0 | |||
| 23 | 41 | m | T-II | 81.2 | 9p24.3p13.3(204082_33290534)x2 hmz, 9p21.3(21682143_22103814)x0 | 7q34(142659319_142785320)x0 | ||
| 26 | 20 | m | T-III | 94.9 | 9p21.3(21471728_22313094)x0 | 7q34(142637680_142796623)x0 | 13q14.2(48411504_48496038)x0 | |
| 27 | 40 | m | T-III | 87.5 | 9p22.1p21.3(19703574_20908514)x1, 9p21.3(20914896_22056500)x0, 9p21.3(22061616_25458801)x1 | 7q34(142309952_142795256)x0 * | ||
| 28 | 42 | f | T-III | 61.5 | 9p21.3(21052665_21865843)x1, 9p21.3(21866502_21996864)x0, 9p21.3(21998037_25552602)x1 | |||
| 30 | 54 | f | T-II | 86 | 12p13.2(11592806_11983676)x0 | |||
| 36 | 40 | m | T-II | 38 | 9p24.3p21.3(204083_21635941)x1 [0.76], 9p21.3(20272224_22647015)x0 [0.5], 9p21.3p13.1(22681778_38780194)x1 [0.76] | |||
| 38 | 21 | f | T-III | 59.3 | 9p24.3p21.3(204082_21905380)x1, 9p21.3(21909980_22233512)x0, 9p21.3p11.2(22238596_40880243)x1 | |||
| 43 | 33 | f | T-III | 89.3 | 9p24.3p21.3(203862_20710799)x1, 9p21.3(20719868_22088261)x0, 9p21.3p11.2(22283154_41008724)x1 | |||
| 44 | 30 | f | T-III | 71 | 7q34(142353951_142785767)x0 | |||
| 45 | 29 | m | T-II | 94.8 | 9p22.3p21.3(14432343_22130515)x1, 9p21.3p21.2(22137086_25938431)x0, 9p21.2q13(25944009_67986968)x1 | |||
| 46 | 23 | m | T-III | 66 | 9p21.3(21720109_22502487)x0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Risinskaya, N.; Abdulpatakhov, A.; Chabaeva, Y.; Aleshina, O.; Gladysheva, M.; Nikulina, E.; Bolshakov, I.; Yushkova, A.; Dubova, O.; Vasileva, A.; et al. Biallelic Loss of 7q34 (TRB) and 9p21.3 (CDKN2A/2B) in Adult Ph-Negative Acute T-Lymphoblastic Leukemia. Int. J. Mol. Sci. 2024, 25, 10482. https://doi.org/10.3390/ijms251910482
Risinskaya N, Abdulpatakhov A, Chabaeva Y, Aleshina O, Gladysheva M, Nikulina E, Bolshakov I, Yushkova A, Dubova O, Vasileva A, et al. Biallelic Loss of 7q34 (TRB) and 9p21.3 (CDKN2A/2B) in Adult Ph-Negative Acute T-Lymphoblastic Leukemia. International Journal of Molecular Sciences. 2024; 25(19):10482. https://doi.org/10.3390/ijms251910482
Chicago/Turabian StyleRisinskaya, Natalya, Abdulpatakh Abdulpatakhov, Yulia Chabaeva, Olga Aleshina, Maria Gladysheva, Elena Nikulina, Ivan Bolshakov, Anna Yushkova, Olga Dubova, Anastasia Vasileva, and et al. 2024. "Biallelic Loss of 7q34 (TRB) and 9p21.3 (CDKN2A/2B) in Adult Ph-Negative Acute T-Lymphoblastic Leukemia" International Journal of Molecular Sciences 25, no. 19: 10482. https://doi.org/10.3390/ijms251910482
APA StyleRisinskaya, N., Abdulpatakhov, A., Chabaeva, Y., Aleshina, O., Gladysheva, M., Nikulina, E., Bolshakov, I., Yushkova, A., Dubova, O., Vasileva, A., Obukhova, T., Julhakyan, H., Kapranov, N., Galtseva, I., Kulikov, S., Sudarikov, A., & Parovichnikova, E. (2024). Biallelic Loss of 7q34 (TRB) and 9p21.3 (CDKN2A/2B) in Adult Ph-Negative Acute T-Lymphoblastic Leukemia. International Journal of Molecular Sciences, 25(19), 10482. https://doi.org/10.3390/ijms251910482





