Antinociceptive Behavior, Glutamine/Glutamate, and Neopterin in Early-Stage Streptozotocin-Induced Diabetic Neuropathy in Liraglutide-Treated Mice under a Standard or Enriched Environment
Abstract
1. Introduction
2. Results
2.1. Body Weight Gain/Loss during the Trial
2.2. Antinociceptive Behavior
2.2.1. Formalin Test
2.2.2. Von Frey Test
2.3. Biochemistry
2.3.1. Blood Glucose
2.3.2. Serum Neopterin
2.3.3. Glutamine/Glutamate
3. Discussion
3.1. Short-Term Effect of Liraglutide in Streptozotocin-Induced Type 1 Diabetes
3.2. Short-Term Effect of Liraglutide in Antinociceptive Behavior in Streptozotocin-Induced Diabetic Neuropathy
3.3. Short-Term Liraglutide Treatment Demonstrates Different Behavior Antinociceptive Effects in the Formalin Test in Standard or EE-Reared Mice
3.4. Short-Term Liraglutide Treatment Effects on Neopterin and Glutamine-to-Glutamate Ratio
3.5. Limitations
4. Materials and Methods
4.1. Chemicals and Kits
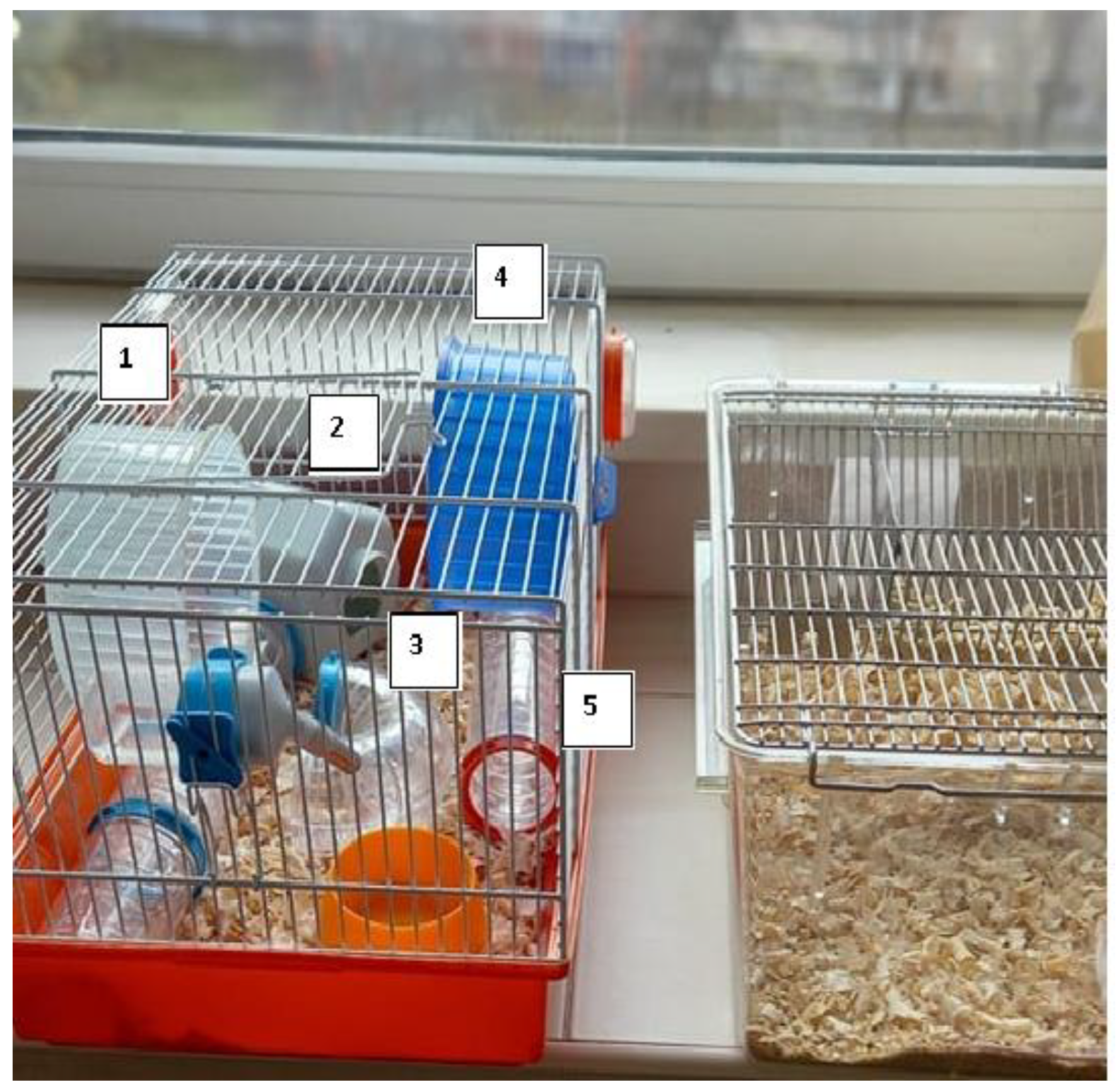
4.2. Experimental Design
- C—control group raised under standard conditions in standard Plexiglas cages (n = 12).
- D—a group with developed diabetes, grown in standard conditions in standard Plexiglas cages (n = 12).
- DLS—a group with developed diabetes, bred in standard Plexiglas cages and treated with liraglutide (n = 12).
- DLE—a group with developed diabetes, bred in an EE, treated with liraglutide (n = 12).
4.3. Body Weight Gain/Loss during the Trial
4.4. Behavior Tests
4.4.1. Formalin Test
4.4.2. Von Frey Test (Dynamic Plantar Aesthesiometer)
4.5. Biochemistry
4.5.1. Pre-Analytical Stage
4.5.2. Blood Glucose Testing
4.5.3. Neopterin Evaluation
4.5.4. Glutamine/Glutamate Evaluation
4.6. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sandireddy, R.; Yerra, V.G.; Areti, A.; Komirishetty, P.; Kumar, A. Neuroinflammation and Oxidative Stress in Diabetic Neuropathy: Futuristic Strategies Based on These Targets. Int. J. Endocrinol. 2014, 2014, 674987. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, P.D.; Sakowski, S.A.; Feldman, E.L. Mouse Models of Diabetic Neuropathy. ILAR J. 2014, 54, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Hu, Z.; Luo, Y.; Liu, Y.; Luo, W.; Du, X.; Luo, Z.; Hu, J.; Peng, S. Diabetic Peripheral Neuropathy: Pathogenetic Mechanisms and Treatment. Front. Endocrinol. 2024, 14, 1265372. [Google Scholar] [CrossRef] [PubMed]
- Papachristoforou, E.; Lambadiari, V.; Maratou, E.; Makrilakis, K. Association of Glycemic Indices (Hyperglycemia, Glucose Variability, and Hypoglycemia) with Oxidative Stress and Diabetic Complications. J. Diabetes Res. 2020, 2020, 7489795. [Google Scholar] [CrossRef]
- Goldney, J.; Sargeant, J.A.; Davies, M.J. Incretins and Microvascular Complications of Diabetes: Neuropathy, Nephropathy, Retinopathy and Microangiopathy. Diabetologia 2023, 66, 1832–1845. [Google Scholar] [CrossRef]
- Zhao, M.; Li, C.H.; Liu, Y.L. Toll-like Receptor (TLR)-2/4 Expression in Retinal Ganglion Cells in a High-Glucose Environment and Its Implications. Genet. Mol. Res. 2016, 15, 23–41. [Google Scholar] [CrossRef]
- Pascale, M.R.D.; Bruzzese, G.; Crimi, E.; Grimaldi, V.; Liguori, A.; Brongo, S.; Barbieri, M.; Picascia, A.; Schiano, C.; Sommese, L.; et al. Severe Type 2 Diabetes Induces Reversible Modifications of Endothelial Progenitor Cells Which Are Ameliorate by Glycemic Control. Int. J. Stem Cells 2016, 9, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Nellaiappan, K.; Preeti, K.; Khatri, D.K.; Singh, S.B. Diabetic Complications: An Update on Pathobiology and TherapeuticStrategies. Curr. Diabetes Rev. 2022, 18, e030821192146. [Google Scholar] [CrossRef]
- Madonna, R.; Balistreri, C.R.; Geng, Y.-J.; De Caterina, R. Diabetic Microangiopathy: Pathogenetic Insights and Novel Therapeutic Approaches. Vascul. Pharmacol. 2017, 90, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J.; Holst, J.J. The Expanding Incretin Universe: From Basic Biology to Clinical Translation. Diabetologia 2023, 66, 1765–1779. [Google Scholar] [CrossRef]
- Yaribeygi, H.; Maleki, M.; Sathyapalan, T.; Jamialahmadi, T.; Sahebkar, A. Antioxidative Potentials of Incretin-Based Medications: A Review of Molecular Mechanisms. Oxid. Med. Cell. Longev. 2021, 2021, 9959320. [Google Scholar] [CrossRef]
- Helmstädter, J.; Frenis, K.; Filippou, K.; Grill, A.; Dib, M.; Kalinovic, S.; Pawelke, F.; Kus, K.; Kröller-Schön, S.; Oelze, M.; et al. Endothelial GLP-1 (Glucagon-Like Peptide-1) Receptor Mediates Cardiovascular Protection by Liraglutide In Mice With Experimental Arterial Hypertension. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 145–158. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; She, M.; Xu, M.; Chen, H.; Li, J.; Chen, X.; Zheng, D.; Liu, J.; Chen, S.; Zhu, J.; et al. GLP-1 Treatment Protects Endothelial Cells from Oxidative Stress-Induced Autophagy and Endothelial Dysfunction. Int. J. Biol. Sci. 2018, 14, 1696–1708. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.; Chen, J.; Zhao, L.; Ma, H. Analysis of the Effect of Liraglutide on Glycemic Variability in Patients with Type 2 Diabetes. Endocr. J. 2020, 67, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Dimitrios, P.; Michael, D.; Vasilios, K.; Konstantinos, S.; Konstantinos, I.; Ioanna, Z.; Konstantinos, P.; Spyridon, B.; Asterios, K. Liraglutide as Adjunct to Insulin Treatment in Patients with Type 1 Diabetes: A Systematic Review and Meta-Analysis. Curr. Diabetes Rev. 2020, 16, 313–326. [Google Scholar] [CrossRef]
- Moustafa, P.E.; Abdelkader, N.F.; El Awdan, S.A.; El-Shabrawy, O.A.; Zaki, H.F. Liraglutide Ameliorated Peripheral Neuropathy in Diabetic Rats: Involvement of Oxidative Stress, Inflammation and Extracellular Matrix Remodeling. J. Neurochem. 2018, 146, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Brock, C.; Hansen, C.S.; Karmisholt, J.; Møller, H.J.; Juhl, A.; Farmer, A.D.; Drewes, A.M.; Riahi, S.; Lervang, H.H.; Jakobsen, P.E.; et al. Liraglutide Treatment Reduced Interleukin-6 in Adults with Type 1 Diabetes but Did Not Improve Established Autonomic or Polyneuropathy. Br. J. Clin. Pharmacol. 2019, 85, 2512–2523. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, K.; Chikamoto, A.; Hsu, J.C.-N.; Tochinai, R.; Sekizawa, S.; Yamamoto, M.; Kuwahara, M. Effects of Environmental Enrichment on Autonomic Nervous Activity in NSY Mice. Exp. Anim. 2020, 69, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Dorfman, D.; Aranda, M.L.; Rosenstein, R.E. Enriched Environment Protects the Optic Nerve from Early Diabetes-Induced Damage in Adult Rats. PLoS ONE 2015, 10, e0136637. [Google Scholar] [CrossRef] [PubMed]
- Cutuli, D.; Landolfo, E.; Petrosini, L.; Gelfo, F. Environmental Enrichment Effects on the Brain-Derived Neurotrophic Factor Expression in Healthy Condition, Alzheimer’s Disease, and Other Neurodegenerative Disorders. J. Alzheimers Dis. 2022, 85, 975–992. [Google Scholar] [CrossRef]
- Zheng, X.; Qi, Y.; Bi, L.; Shi, W.; Zhang, Y.; Zhao, D.; Hu, S.; Li, M.; Li, Q. Effects of Exercise on Blood Glucose and Glycemic Variability in Type 2 Diabetic Patients with Dawn Phenomenon. BioMed Res. Int. 2020, 2020, 6408724. [Google Scholar] [CrossRef]
- Munan, M.; Oliveira, C.L.P.; Marcotte-Chénard, A.; Rees, J.L.; Prado, C.M.; Riesco, E.; Boulé, N.G. Acute and Chronic Effects of Exercise on Continuous Glucose Monitoring Outcomes in Type 2 Diabetes: A Meta-Analysis. Front. Endocrinol. 2020, 11, 495. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yang, X.; Sun, B.; Zhu, C. Perspectives of Glycemic Variability in Diabetic Neuropathy: A Comprehensive Review. Commun. Biol. 2021, 4, 1366. [Google Scholar] [CrossRef]
- Cooper, D.D.; Frenguelli, B.G. The Influence of Sensory Experience on the Glutamatergic Synapse. Neuropharmacology 2021, 193, 108620. [Google Scholar] [CrossRef] [PubMed]
- Salim, S. Oxidative Stress and the Central Nervous System. J. Pharmacol. Exp. Ther. 2017, 360, 201–205. [Google Scholar] [CrossRef]
- Maher, P.; Van Leyen, K.; Dey, P.N.; Honrath, B.; Dolga, A.; Methner, A. The Role of Ca2+ in Cell Death Caused by Oxidative Glutamate Toxicity and Ferroptosis. Cell Calcium 2018, 70, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Lewerenz, J.; Ates, G.; Methner, A.; Conrad, M.; Maher, P. Oxytosis/Ferroptosis—(Re-) Emerging Roles for Oxidative Stress-Dependent Non-Apoptotic Cell Death in Diseases of the Central Nervous System. Front. Neurosci. 2018, 12, 214. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Wang, K.; Lin, R.; Mu, F.; Cui, J.; Tao, X.; Weng, Y.; Wang, J. Influence of Glutamine Metabolism on Diabetes Development:A Scientometric Review. Heliyon 2024, 10, e25258. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.M.; Pei, H.; Sandoval, D.A.; Seeley, R.J.; Chang, R.B.; Liberles, S.D.; Olson, D.P. Liraglutide Modulates Appetite and Body Weight Through Glucagon-Like Peptide 1 Receptor–Expressing Glutamatergic Neurons. Diabetes 2018, 67, 1538–1548. [Google Scholar] [CrossRef] [PubMed]
- Elbarbary, N.S.; Ismail, E.A.R.; El-Hilaly, R.A.; Ahmed, F.S. Role of Neopterin as a Biochemical Marker for Peripheral Neuropathy in Pediatric Patients with Type 1 Diabetes: Relation to Nerve Conduction Studies. Int. Immunopharmacol. 2018, 59, 68–75. [Google Scholar] [CrossRef]
- Ghisoni, K.; Martins, R.D.P.; Barbeito, L.; Latini, A. Neopterin as a Potential Cytoprotective Brain Molecule. J. Psychiatr. Res. 2015, 71, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Deuis, J.R.; Dvorakova, L.S.; Vetter, I. Methods Used to Evaluate Pain Behaviors in Rodents. Front. Mol. Neurosci. 2017, 10, 284. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Poudel, A.; Chandramani-Shivalingappa, P.; Xu, B.; Welchko, R.; Li, L. Liraglutide Induces Beige Fat Development and Promotes Mitochondrial Function in Diet Induced Obesity Mice Partially through AMPK-SIRT-1-PGC1-α Cell Signaling Pathway. Endocrine 2019, 64, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Cernea, S. The Role of Incretin Therapy at Different Stages of Diabetes. Rev. Diabet. Stud. 2011, 8, 323–338. [Google Scholar] [CrossRef] [PubMed]
- Eleazu, C.O.; Eleazu, K.C.; Chukwuma, S.; Essien, U.N. Review of the Mechanism of Cell Death Resulting from Streptozotocin Challenge in Experimental Animals, Its Practical Use and Potential Risk to Humans. J. Diabetes Metab. Disord. 2013, 12, 60. [Google Scholar] [CrossRef] [PubMed]
- Junod, A.; Lambert, A.E.; Orci, L.; Pictet, R.; Gonet, A.E.; Renold, A.E. Studies of the Diabetogenic Action of Streptozotocin. Exp. Biol. Med. 1967, 126, 201–205. [Google Scholar] [CrossRef]
- Kentner, A.C.; Speno, A.V.; Doucette, J.; Roderick, R.C. The Contribution of Environmental Enrichment to Phenotypic Variation in Mice and Rats. eneuro 2021, 8, ENEURO.0539-20.2021. [Google Scholar] [CrossRef]
- Murakami, T.; Iwanaga, T.; Ogawa, Y.; Fujita, Y.; Sato, E.; Yoshitomi, H.; Sunada, Y.; Nakamura, A. Development of Sensory Neuropathy in Streptozotocin-induced Diabetic Mice. Brain Behav. 2013, 3, 35–41. [Google Scholar] [CrossRef] [PubMed]
- López-Cano, M.; Fernández-Dueñas, V.; Llebaria, A.; Ciruela, F. Formalin Murine Model of Pain. Bio-Protocol 2017, 7, e2628. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.; Klemm, F.; Kichko, T.I.; Sauer, S.K.; Kistner, K.; Riedl, B.; Raboisson, P.; Luo, L.; Babes, A.; Kocher, L.; et al. The Formalin Test Does Not Probe Inflammatory Pain but Excitotoxicity in Rodent Skin. Physiol. Rep. 2022, 10, e15194. [Google Scholar] [CrossRef]
- Ratuski, A.S.; Weary, D.M. Environmental Enrichment for Rats and Mice Housed in Laboratories: A Metareview. Animals 2022, 12, 414. [Google Scholar] [CrossRef] [PubMed]
- Slivicki, R.A.; Mali, S.S.; Hohmann, A.G. Voluntary Exercise Reduces Both Chemotherapy-Induced Neuropathic Nociception and Deficits in Hippocampal Cellular Proliferation in a Mouse Model of Paclitaxel-Induced Peripheral Neuropathy. Neurobiol. Pain 2019, 6, 100035. [Google Scholar] [CrossRef] [PubMed]
- Parent-Vachon, M.; Vachon, P. Environmental Enrichment Alleviates Chronic Pain in Rats Following a Spared Nerve Injury to Induce Neuropathic Pain. A Preliminary Study. Vet. Med. Res. Rep. 2018, 9, 69–72. [Google Scholar] [CrossRef]
- Tai, W.L.; Sun, L.; Li, H.; Gu, P.; Joosten, E.A.; Cheung, C.W. Additive Effects of Environmental Enrichment and Ketamine on Neuropathic Pain Relief by Reducing Glutamatergic Activation in Spinal Cord Injury in Rats. Front. Neurosci. 2021, 15, 635187. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhang, G.; Jia, M.; Xie, Z.; Yang, J.; Shen, J.; Zhou, Z. Environmental Enrichment Improves Pain Sensitivity, Depression-like Phenotype, and Memory Deficit in Mice with Neuropathic Pain: Role of NPAS4. Psychopharmacology 2019, 236, 1999–2014. [Google Scholar] [CrossRef]
- Qi, L.; Gao, R.; Chen, Z.; Lin, D.; Liu, Z.; Wang, L.; Lin, L.; Liu, X.; Liu, X.; Liu, L. Liraglutide Reduces Oxidative Stress and Improves Energy Metabolism in Methylglyoxal-Induced SH-SY5Y Cells. NeuroToxicology 2022, 92, 166–179. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Zhao, Y.; Xu, L.; Li, W.; Zhang, H.; Ping, F.; Li, Y. Liraglutide Attenuates Hepatic Oxidative Stress, Inflammation, and Apoptosis in Streptozotocin-Induced Diabetic Mice by Modulating the Wnt/β-Catenin Signaling Pathway. Mediators Inflamm. 2023, 2023, 8974960. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, M.; Abate, N.; Chandalia, M.; Rizvi, A.A.; Giglio, R.V.; Nikolic, D.; Marino Gammazza, A.; Barbagallo, I.; Isenovic, E.R.; Banach, M.; et al. Liraglutide Reduces Oxidative Stress And Restores Heme Oxygenase-1 and Ghrelin Levels in Patients with Type 2 Diabetes: A Prospective Pilot Study. J. Clin. Endocrinol. Metab. 2015, 100, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Oh, S.; Kim, E.-K. Glucagon-like Peptide-1 Analog Liraglutide Leads to Multiple Metabolic Alterations in Diet-Induced Obese Mice. J. Biol. Chem. 2022, 298, 102682. [Google Scholar] [CrossRef]
- Darmaun, D.; Torres-Santiago, L.; Mauras, N. Glutamine and Type 1 Diabetes Mellitus: Is There a Role in Glycemic Control? Curr. Opin. Clin. Nutr. Metab. Care 2019, 22, 91–95. [Google Scholar] [CrossRef]
- Dickson, I. Intestinal Gluconeogenesis Prevents Hepatic Steatosis. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 316. [Google Scholar] [CrossRef]
- Gautier-Stein, A.; Rajas, F.; Mithieux, G. Intestinal Gluconeogenesis and Protein Diet: Future Directions. Proc. Nutr. Soc. 2021, 80, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Lutchmansingh, F.K.; Hsu, J.W.; Bennett, F.I.; Badaloo, A.V.; McFarlane-Anderson, N.; Gordon-Strachan, G.M.; Wright-Pascoe, R.A.; Jahoor, F.; Boyne, M.S. Glutathione Metabolism in Type 2 Diabetes and Its Relationship with Microvascular Complications and Glycemia. PLoS ONE 2018, 13, e0198626. [Google Scholar] [CrossRef]
- Badole, S.L.; Jangam, G.B.; Chaudhari, S.M.; Ghule, A.E.; Zanwar, A.A. L-Glutamine Supplementation Prevents the Development of Experimental Diabetic Cardiomyopathy in Streptozotocin-Nicotinamide Induced Diabetic Rats. PLoS ONE 2014, 9, e92697. [Google Scholar] [CrossRef] [PubMed]
- Curis, E.; Nicolis, I.; Moinard, C.; Osowska, S.; Zerrouk, N.; Bénazeth, S.; Cynober, L. Almost All about Citrulline in Mammals. Amino Acids 2005, 29, 177. [Google Scholar] [CrossRef]
- Kurohane Kaneko, Y.; Ishikawa, T. Dual Role of Nitric Oxide in Pancreatic β-Cells. J. Pharmacol. Sci. 2013, 123, 295–300. [Google Scholar] [CrossRef]
- Greenfield, J.R.; Farooqi, I.S.; Keogh, J.M.; Henning, E.; Habib, A.M.; Blackwood, A.; Reimann, F.; Holst, J.J.; Gribble, F.M. Oral Glutamine Increases Circulating Glucagon-like Peptide 1, Glucagon, and Insulin Concentrations in Lean, Obese, and Type 2 Diabetic Subjects. Am. J. Clin. Nutr. 2009, 89, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.E.; Shcherbina, L.; Al-Majdoub, M.; Vishnu, N.; Arroyo, C.B.; Aste Carrara, J.; Wollheim, C.B.; Fex, M.; Mulder, H.; Wierup, N.; et al. Glutamine-Elicited Secretion of Glucagon-Like Peptide 1 Is Governed by an Activated Glutamate Dehydrogenase. Diabetes 2018, 67, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Hohnholt, M.C.; Andersen, V.H.; Andersen, J.V.; Christensen, S.K.; Karaca, M.; Maechler, P.; Waagepetersen, H.S. Glutamate Dehydrogenase Is Essential to Sustain Neuronal Oxidative Energy Metabolism during Stimulation. J. Cereb. Blood Flow Metab. 2018, 38, 1754–1768. [Google Scholar] [CrossRef]
- Walls, A.B.; Waagepetersen, H.S.; Bak, L.K.; Schousboe, A.; Sonnewald, U. The Glutamine–Glutamate/GABA Cycle: Function, Regional Differences in Glutamate and GABA Production and Effects of Interference with GABA Metabolism. Neurochem. Res. 2015, 40, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Hedrington, M.S.; Mikeladze, M.; Tate, D.B.; Younk, L.M.; Davis, I.; Davis, S.N. Effects of γ-Aminobutyric Acid A Receptor Activation on Counterregulatory Responses to Subsequent Exercise in Individuals With Type 1 Diabetes. Diabetes 2016, 65, 2754–2759. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Lipton, S.A. Preventing Ca2+-Mediated Nitrosative Stress in Neurodegenerative Diseases: Possible Pharmacological Strategies. Cell Calcium 2010, 47, 190–197. [Google Scholar] [CrossRef]
- Brennan, A.M.; Won Suh, S.; Joon Won, S.; Narasimhan, P.; Kauppinen, T.M.; Lee, H.; Edling, Y.; Chan, P.H.; Swanson, R.A. NADPH Oxidase Is the Primary Source of Superoxide Induced by NMDA Receptor Activation. Nat. Neurosci. 2009, 12, 857–863. [Google Scholar] [CrossRef] [PubMed]
- De Paula Martins, R.; Ghisoni, K.; Lim, C.K.; Aguiar, A.S.; Guillemin, G.J.; Latini, A. Neopterin Preconditioning Prevents Inflammasome Activation in Mammalian Astrocytes. Free Radic. Biol. Med. 2018, 115, 371–382. [Google Scholar] [CrossRef]
- Meurot, C.; Martin, C.; Sudre, L.; Breton, J.; Bougault, C.; Rattenbach, R.; Bismuth, K.; Jacques, C.; Berenbaum, F. Liraglutide, a Glucagon-like Peptide 1 Receptor Agonist, Exerts Analgesic, Anti-Inflammatory and Anti-Degradative Actions in Osteoarthritis. Sci. Rep. 2022, 12, 1567. [Google Scholar] [CrossRef] [PubMed]
- Alkan, A.A.; Arslan, B.; Özcan, D.; Tekin, K. Serum Neopterin and Orexin-A Levels in Different Stages of Diabetic Retinopathy. Clin. Exp. Optom. 2024, 107, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cutaș, A.; Drugan, C.; Roman, G.; Rusu, A.; Cătană, C.S.; Achimaș-Cadariu, A.; Drugan, T. Evaluation of Chitotriosidase and Neopterin as Biomarkers of Microvascular Complications in Patients with Type 1 Diabetes Mellitus. Diagnostics 2021, 11, 263. [Google Scholar] [CrossRef]
- Salem, I.A.; Abdulsattar, S.A.; Alrubaye, H.F. Evaluation of Neopterin as a Neuroinflammatory Marker for Peripheral Neuropathy in Type 2 Diabetic Patients. Al-Rafidain J. Med. Sci. 2023, 5, S183–S188. [Google Scholar] [CrossRef]
- Al-Nimer, M.S.; Dezayee, Z.M. Assessment of Serum Neopterin as an Inflammatory and Cardiovascular Marker in Type 1 and 2 Diabetes Complicated by Diabetic Foot Syndrome: A Comparative Study. Clin. Diabetol. 2018, 7, 91–96. [Google Scholar] [CrossRef]
- Gieseg, S.P.; Baxter-Parker, G.; Lindsay, A. Neopterin, Inflammation, and Oxidative Stress: What Could We Be Missing? Antioxidants 2018, 7, 80. [Google Scholar] [CrossRef]
- Nikolova, S.; Lee, Y.S.; Lee, Y.-S.; Kim, J. Rac1-NADPH Oxidase-Regulated Generation of Reactive Oxygen Species Mediates Glutamate-Induced Apoptosis in SH-SY5Y Human Neuroblastoma Cells. Free Radic. Res. 2005, 39, 1295–1304. [Google Scholar] [CrossRef]
- Furman, B.L. Streptozotocin-Induced Diabetic Models in Mice and Rats. Curr. Protoc. Pharmacol. 2015, 70, 5–47. [Google Scholar] [CrossRef]
- Knudsen, L.B. Liraglutide: The Therapeutic Promise from Animal Models: Liraglutide: The Therapeutic Promise from Animal Models. Int. J. Clin. Pract. 2010, 64, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, L.; Li, L.; Hölscher, C. Neuroprotective Effects of the Novel GLP-1 Long Acting Analogue Semaglutide in the MPTP Parkinson’s Disease Mouse Model. Neuropeptides 2018, 71, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Kubota, K.; Nakano, M.; Kobayashi, E.; Mizue, Y.; Chikenji, T.; Otani, M.; Nagaishi, K.; Fujimiya, M. An Enriched Environment Prevents Diabetes-Induced Cognitive Impairment in Rats by Enhancing Exosomal miR-146a Secretion from Endogenous Bone Marrow-Derived Mesenchymal Stem Cells. PLoS ONE 2018, 13, e0204252. [Google Scholar] [CrossRef]
- Beauquis, J.; Roig, P.; De Nicola, A.F.; Saravia, F. Short-Term Environmental Enrichment Enhances Adult Neurogenesis, Vascular Network and Dendritic Complexity in the Hippocampus of Type 1 Diabetic Mice. PLoS ONE 2010, 5, e13993. [Google Scholar] [CrossRef]


| Groups | Time | Body Weight (g) | Weight Gain/Loss (g) | % from the Initial BW Value for Each Mouse |
|---|---|---|---|---|
| C | Start | 33.00 (30.25 ÷ 34.00) | ||
| End | 33.00 (31.00 ÷ 34.00) | 1.00 (0.00 ÷ 2.00) | +3.03 (−2.14 ÷ 5.27) | |
| D | Start | 33.50 (30.50 ÷ 35.50) | ||
| End | 28.00 * (26.00 ÷ 30.00) | −5.50 * (−8.50 ÷ −3.50) | −14.30 * (−21.71 ÷ −10.34) | |
| DLS | Start | 33.00 (30.25 ÷ −35.00) | ||
| End | 29.00 (25.00 ÷ 33.50) | −3.50 * (−7.00 ÷ 0.00) | −9.38 * (−27.19 ÷ +3.00) | |
| DLE | Start | 34.00 (31.00 ÷ 35.50) | ||
| End | 30.00 (25.00 ÷ 32.00) | −3.50 * (−5.00 ÷ −2.50) | −16.12 * (−19.30 ÷ −9.38) |
| Groups | Formalin Test (s) | Von Frey Test | q | |
|---|---|---|---|---|
| 0–5 min | 20–30 min | (grams) | (s) | |
| C (n = 12) | 108.25 ± 37.79 | 10.00 (8.00–13.00) | 8.48 ± 1.90 | 3.40 ± 0.74 |
| D (n = 12) | 147.92 * ± 35.64 | 33.00 (10.00–124.00) | 7.59 ± 1.35 | 3.00 ± 0.55 |
| DLS (n = 12) | 91.83 ** *** ± 34.70 | 29.00 (2.25–41.50) | 6.58 # ± 1.36 | 2.55 ### ± 0.55 |
| DLE (n = 12) | 64.50 ***** ± 35.80 | 2.00 ***** (0.00–11.00) | 5.96 ## ± 1.58 | 2.30 #### ± 0.62 |
| Groups | Glucose (mmol/L) | Neopterin (ng/mL) | Glutamine/Glutamate |
|---|---|---|---|
| C (n = 12) | 12.65 * (10.55–13.55) | 5.92 ± 1.31 | 2.00 ± 1.04 |
| D (n = 12) | 29.5 * (16.65–33.30) | 9.58 ** ± 1.68 | 1.17 ± 0.50 |
| DLS (n = 12) | 24.5 * (16.60–33.30) | 5.83 ± 1.75 | 2.67 *** ± 1.23 |
| DLE (n = 12) | 30.65 * (23.05–33.30) | 5.92 ± 1.73 | 2.75 **** ± 0.96 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gateva, P.; Hristov, M.; Ivanova, N.; Vasileva, D.; Ivanova, A.; Sabit, Z.; Bogdanov, T.; Apostolova, S.; Tzoneva, R. Antinociceptive Behavior, Glutamine/Glutamate, and Neopterin in Early-Stage Streptozotocin-Induced Diabetic Neuropathy in Liraglutide-Treated Mice under a Standard or Enriched Environment. Int. J. Mol. Sci. 2024, 25, 10786. https://doi.org/10.3390/ijms251910786
Gateva P, Hristov M, Ivanova N, Vasileva D, Ivanova A, Sabit Z, Bogdanov T, Apostolova S, Tzoneva R. Antinociceptive Behavior, Glutamine/Glutamate, and Neopterin in Early-Stage Streptozotocin-Induced Diabetic Neuropathy in Liraglutide-Treated Mice under a Standard or Enriched Environment. International Journal of Molecular Sciences. 2024; 25(19):10786. https://doi.org/10.3390/ijms251910786
Chicago/Turabian StyleGateva, Pavlina, Milen Hristov, Natasha Ivanova, Debora Vasileva, Alexandrina Ivanova, Zafer Sabit, Todor Bogdanov, Sonia Apostolova, and Rumiana Tzoneva. 2024. "Antinociceptive Behavior, Glutamine/Glutamate, and Neopterin in Early-Stage Streptozotocin-Induced Diabetic Neuropathy in Liraglutide-Treated Mice under a Standard or Enriched Environment" International Journal of Molecular Sciences 25, no. 19: 10786. https://doi.org/10.3390/ijms251910786
APA StyleGateva, P., Hristov, M., Ivanova, N., Vasileva, D., Ivanova, A., Sabit, Z., Bogdanov, T., Apostolova, S., & Tzoneva, R. (2024). Antinociceptive Behavior, Glutamine/Glutamate, and Neopterin in Early-Stage Streptozotocin-Induced Diabetic Neuropathy in Liraglutide-Treated Mice under a Standard or Enriched Environment. International Journal of Molecular Sciences, 25(19), 10786. https://doi.org/10.3390/ijms251910786









